Abstract
Background and study aims: Discontinuation of all antiplatelet agents before endoscopic procedures may cause serious complications in some patients. The aim of this study was to evaluate the hemorrhagic risk of post-endoscopic submucosal dissection (ESD) in patients on antiplatelet therapy (APT).
Patients and methods: The subjects were 350 patients (377 lesions) who underwent gastric ESD between January 2007 and July 2013. The patients were categorized based on antiplatelet therapies. The primary outcome was post-ESD bleeding. Multivariate analysis was performed to identify independent risk factors for post-ESD bleeding.
Results: The patients were categorized into three groups: (1) no APT, 261 patients with 281 lesions; (2) single APT, 58 patients with 63 lesions (53 patients with low dose aspirin [LDA] and 5 patients with a thienopyridine); and (3) dual APT (DAPT), 31 patients with 33 lesions (DAPT with LDA and a thienopyridine). Post-ESD bleeding occurred in 16 of 261 patients in the no APT group (6.1 %), 9 of 58 patients in the single APT group (15.5 %), and 11 of 31 patients in the DAPT group (35.5 %). In multivariate analysis with a Cox proportional hazards model in the no APT and single APT groups, APT (HR 2.7, 95 %CI 1.1 – 6.6, P = 0.03) and diameter of the resected specimen of 40 mm or greater (HR 2.7, 95 %CI 1.2 – 5.9, P = 0.01) were significant risk factors for post-ESD bleeding. In multivariate analysis in the no APT and DAPT groups, DAPT was the only significant risk factor for post-ESD bleeding (HR 16.3, 95 %CI 3.4 – 78.2, P < 0.01). Continuous LDA was not a significant risk factor for post-ESD bleeding in both analyses (HR 0.8, 95 %CI 0.2 – 3.6, P = 0.72 in the no APT and single APT groups; HR 1.0, 95 %CI 0.2 – 5.1, P = 0.95 in the no APT and DAPT groups).
Conclusions: APT increased the risk for post-ESD bleeding, and DAPT markedly increased the risk for bleeding. Continuous LDA did not produce an additional hemorrhagic risk in all patients treated with APT. Thus, patients treated with APT should be careful monitored for post-ESD bleeding, and LDA should not be interrupted in patients with a high thromboembolic risk.
Introduction
Antiplatelet therapy (APT) with low dose aspirin (LDA) and/or thienopyridines is increasingly used because of the aging of patients. This change has occurred simultaneously with increased drug-eluting stent (DES) use in percutaneous coronary intervention (PCI). Recent guidelines indicate that patients with coronary artery stents should receive dual antiplatelet therapy (DAPT) with LDA plus thienopyridines for 1 year after placement of a DES, and that LDA should be continued for life 1.
Endoscopic submucosal dissection (ESD) is an effective treatment for early gastric cancers 2 3, but the management of APT in patients undergoing ESD has not been established. In the guidelines for the management of antithrombotic agents in endoscopic procedures published by the American Society for Gastrointestinal Endoscopy 4 and the British Society of Gastroenterology 5, the continuation of LDA is recommended for patients undergoing all endoscopic procedures, but ESD is not mentioned. The European Society of Gastrointestinal Endoscopy guidelines 6 recommend discontinuation of all APT, including LDA, in high risk endoscopic procedures, including endoscopic mucosal resection, ESD, ampullary resection, endoscopic sphincterotomy with large-balloon papillary dilation, and fine-needle aspiration biopsy of a cystic lesion with endoscopic ultrasonography.
In January 2014, the Japan Gastroenterological Endoscopy Society published new guidelines for the management of anticoagulation therapy and APT in patients undergoing endoscopic procedures 7. These guidelines indicate that LDA and cilostazol can be continued in high risk endoscopic procedures, including ESD. We have performed gastric ESD without interrupting LDA in all patients with high thromboembolic risk since 2007. In this study, we investigate the relationship between post-ESD bleeding and the status of APT.
Patients and methods
A total of 385 patients with 414 lesions underwent gastric ESD for gastric neoplasms (362 early gastric cancers and 52 gastric adenomas) at Shin-Tokyo Hospital in Chiba, Japan, between January 2007 and July 2013. Patients on anticoagulants (24 patients with 26 lesions) or cilostazol (10 patients with 10 lesions) were excluded from the study to allow evaluation of the effects of LDA and thienopyridines. One patient who underwent surgery for post-ESD perforation on the day after ESD was also excluded, leaving 350 patients (377 lesions) for inclusion in the study (Fig. 1). Single APT was used in 58 patients (63 lesions), including LDA in 53 patients (57 lesions) and a thienopyridine in 5 patients (6 lesions). LDA was continued in 14 of 58 patients treated with single APT. DAPT (a thienopyridine plus LDA) was used in 31 patients (33 lesions), and LDA was continued in 24 of 31 patients treated with DAPT. Ticlopidine and clopidogrel are permitted thienopyridines in Japan, and these drugs were used in 11 and 25, respectively, of 36 patients treated with a thienopyridine (in 5 patients as single APT and in 31 in DAPT).
Fig. 1.
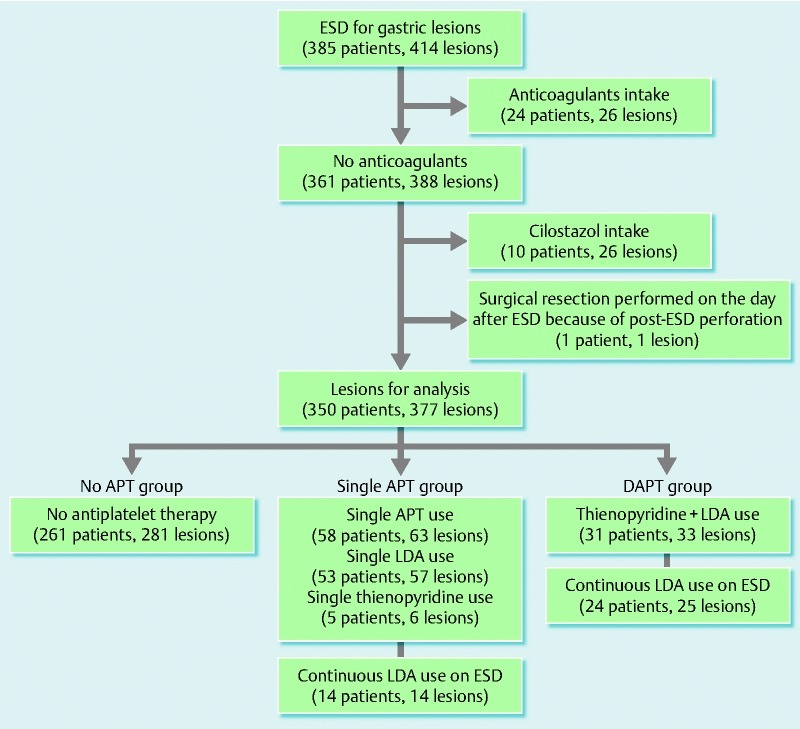
Lesions and use of antiplatelet drugs. Patients treated with anticoagulants, cilostazol, and surgical resection were excluded. A total of 350 patients were included in the analysis. The patients were divided into groups based on their use of antiplatelet therapies (APTs). In the single APT group, 53 patients received low dose aspirin (LDA), and 5 patients received a thienopyridine. LDA was continued during endoscopic submucosal dissection (ESD) in 14 of 58 patients in the single APT group and 24 of 31 patients in the dual APT (DAPT) group.
All patients were informed about the risks and benefits of ESD, with a focus on the increased risk for bleeding and possible need for blood transfusion with the continuous use of antiplatelet drugs, and the risk for thromboembolic complications with cessation of antiplatelet drugs. Written informed consent was obtained before ESD was performed.
Schedules of the interruption and resumption of antiplatelet drugs in each group are summarized in Fig. 2. Periods of interruption of antiplatelet drugs were based on a previous study in Japan 8. Patients with DES placement, recent bare metal stent (BMS) placement (within 3 months), and recent cerebrovascular attack or carotid artery stent placement (within 3 months) were considered to be at high thromboembolic risk, and LDA was continued around the time of ESD. Patients in whom a mechanical cardiac valve had been placed were excluded from the study based on treatment with anticoagulants. The risks of interruption of antiplatelet drugs were discussed with the cardiologists and neurosurgeons who had prescribed these drugs.
Fig. 2.
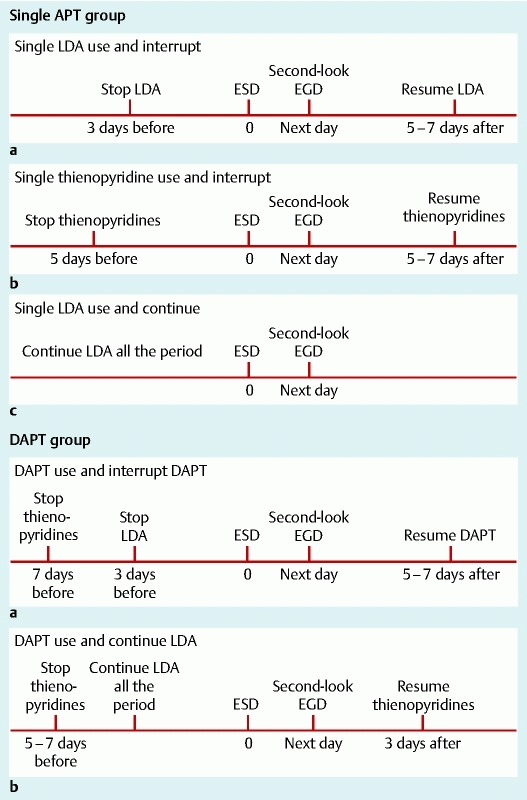
Schedules of interruption and resumption of antiplatelet drugs in each group. Antiplatelet drugs were interrupted based on the thromboembolic risk of the patients. Single low dose aspirin (LDA) was stopped 3 days before endoscopic submucosal dissection (ESD) and restarted 5 to 7 days after ESD. A single thienopyridine was stopped 5 days before ESD and restarted 5 to 7 days after ESD. If the thromboembolic risk was high, LDA was continued throughout the period. In patients on dual antiplatelet therapy (DAPT), thienopyridines were stopped 7 days before ESD, LDA was stopped 3 days before ESD, and DAPT was restarted 5 to 7 days after ESD. In patients with a high thromboembolic risk, thienopyridines were stopped 5 to 7 days before ESD and restarted 3 days after ESD, and LDA was continued throughout the period. Periods of interruption of APT were based on a previous study in Japan 8. EGD, esophagogastroduodenoscopy.
Endoscopic procedures and management
All ESD procedures were carried out by endoscopists with extensive experience in ESD (most of them by S.T. and Y.M.) using a regular video endoscope (GIF-Q260J; Olympus Medical Systems, Tokyo, Japan) and a multibending endoscope (GIF-2TQ260M; Olympus Medical Systems) with distal attachments (D-201-11804 for GIF-Q260 J and D-201-13404 for GIF-2TQ260M; Olympus Medical Systems). For ESD devices, a Flex Knife (KD-630 L) and Dual Knife (KD-650 L) were mainly used, and an IT knife2 (KD-611 L) and Hook Knife (KD-620LR) were additionally used (all from Olympus Medical Systems). The electrical generator was an ICC200 (Erbe, Tübingen, Germany) with settings of endocut effect 3, 120 W for mucosal incision and of forced coagulation effect 3, 50 W for submucosal dissection. Hemostasis was achieved by using hot biopsy forceps (Radial Jaw 3; Boston Scientific, Natick, Massachusetts, USA) with soft coagulation at 70 W and/or endoclips (HX-610-135 and HX-610-135S; Olympus Medical Systems). All visible vessels of the post-ESD ulcer were thoroughly burned out with the hot biopsy forceps immediately after the completion of ESD.
In 9 patients with chronic renal failure who were on hemodialysis, ESD was done on the day after hemodialysis, and hemodialysis was restarted 2 days after ESD. For hemodialysis after ESD, nafamostat mesilate was used as a substitute for heparin for 1 week. All patients underwent second-look endoscopies on the day after ESD, and preventive hemostasis with hot biopsy forceps and/or endoclips was done if needed. Because proton pump inhibitors are effective for preventing post-ESD bleeding 9 10, all patients received 10 mg of omeprazole intravenously twice a day on the day of ESD and the following day. After the second-look endoscopy, a liquid diet was started in the evening of the day after ESD. Oral rabeprazole was started at a dosage of 10 mg twice daily 2 days after ESD and continued for at least 30 days. Hemoglobin levels, platelets counts, and coagulation parameters (international normalized ratio of prothrombin time [PT-INR]) were checked within 1 month before ESD, and the hemoglobin levels were also checked on the morning after ESD. Patients were hospitalized for 7 days and checked for signs of post-ESD bleeding. At discharge, all patients received a careful explanation of the signs of gastric bleeding and were asked to visit the hospital immediately when they noticed any sign. All patients were also asked to visit the outpatient clinic 30 days after ESD for follow-up of their condition.
Post-ESD ulcer size
The maximum diameter of the resected specimen was used to represent the size of the post-ESD ulcer because this size is difficult to measure. A diameter of 40 mm or greater has previously been found to be a significant risk factor for post-ESD bleeding 11 12 13, so we used a cutoff value of 40 mm or greater to classify the diameter of the resected specimen.
Post-ESD bleeding
Urgent endoscopy and blood analysis were immediately performed when a patient showed any signs of bleeding (hematemesis, melena, or an acute decrease of blood pressure with tachycardia). Post-ESD bleeding was defined as bleeding from a post-ESD ulcer, confirmed by urgent endoscopy. Bleeding within 7 days after ESD was defined as early-onset post-ESD bleeding, and bleeding 8 days or more after ESD was defined as late-onset post-ESD bleeding.
Outcome measures
The primary outcome was significant post-ESD bleeding confirmed with endoscopy. Secondary outcomes included other hemorrhagic complications (cerebral bleeding or gastrointestinal tract bleeding except post-ESD bleeding) and thromboembolic complications (cerebral infarction, transient ischemic attack, acute myocardial infarction, pulmonary embolism, or deep vein thrombosis) observed from the first day of APT interruption to 30 days after ESD.
Data analysis
The patients were divided into three groups based on the status of APT: (1) no APT, no history of administration of antiplatelet drugs; (2) single APT, administration of LDA alone or a thienopyridine alone; and (3) DAPT, administration of a thienopyridine with LDA. In the single APT and DAPT groups, LDA was continued in patients with high thromboembolic risk, but thienopyridines were interrupted according to the schedule based on thromboembolic risk. To evaluate the effects of other factors, the following variables were analyzed: age (< 65 or ≥ 65 years old), sex, comorbidities (coronary artery disease, peripheral artery disease, atrial fibrillation, cerebrovascular disease, diabetes mellitus, chronic renal failure with hemodialysis, and liver cirrhosis); hemoglobin levels (< 12 or ≥ 12 g/dL) and platelet cell counts (< 100 or ≥ 100 × 109/L) before ESD (within 1 month); coagulation parameters (PT-INR > 1.20 or ≤ 1.20) before ESD (within 1 month), pathologic diagnosis of the resected lesion (presence or absence of early gastric cancer); diameter of the resected specimen (< 40 or ≥ 40 mm); location of the lesion (upper, middle, or lower third); and status of APT. We used a cutoff of less than 12 g/dL for classification of the hemoglobin level based on the World Health Organization definition of anemia for adult women, a cutoff of less than 100 × 109/L for platelet cell counts because this indicates moderate thrombocytopenia, and a cutoff of more than 1.20 for the PT-INR because the normal range is 0.8 to 1.2. In 25 patients, 2 lesions were resected in 1 ESD procedure, and in 1 patient, 3 lesions were resected in 1 procedure. In these patients, the largest lesion or the lesion in which post-ESD bleeding occurred was used for analysis.
Statistical analysis
Continuous variables are reported as means, standard deviation, and range, and categorical variables as frequency and percentage. Data for each drug-related group (single APT and DAPT groups) were compared with those for the no APT group. Qualitative variables were compared with Fisher’s exact test or the chi-squared test, and quantitative variables with the unpaired Student’s t test. To evaluate the risk for bleeding after ESD, univariate analysis with a log-rank test and multivariate analysis with a Cox proportional hazards regression model were used. To avoid type I statistical error, fewer than three variables with a P value of less than 0.05 in univariate analysis were examined in the Cox hazards model to identify independent factors associated with post-ESD bleeding. Data were analyzed with StatView Version 5 (SAS Institute, Cary, North Carolina, USA). Differences were considered significant at a P value of less than 0.05.
Results
Baseline characteristics
A total of 350 patients (377 lesions) were analyzed in the study. The patients were divided into three groups based on the status of administration of antiplatelet drugs: no APT (n = 261), single APT (n = 58), and DAPT (n = 31). The baseline characteristics in each group are shown in Table 1. Patients in the single APT group were older than those in the no APT group, and the percentage of male patients was lower in the no APT group. In the single APT and DAPT groups, 67.2 % and 93.6 %, respectively, of patients had coronary artery disease, which were much higher rates than that in the no APT group (6.1 %). The numbers of patients with comorbid peripheral artery disease and cerebrovascular disease were higher in the single APT and DAPT groups. The number of patients with comorbid diabetes mellitus was higher in the DAPT group than in the no APT group. Few patients had chronic renal failure, and there was no significant difference among the groups. Liver cirrhosis was also rare, and no patients had liver cirrhosis in the single APT and DAPT groups. The pre-ESD hemoglobin level was higher in the no APT group, the PT-INR was higher in the DAPT group, and the platelet counts did not differ significantly among the groups.
Table 1. Baseline characteristics of patients before endoscopic submucosal dissection of a gastric neoplasm.
| (A) No APT group (n = 261) | (B) Single APT group (n = 58) | (C) DAPT group (n = 31) |
A vs. B P value | A vs. C P value | |
| Age, mean(range, SD), years | 71.0(36 – 92, 8.2) | 75.1(61 – 89, 6.2) | 72.8(52 – 86, 8.7) | < 0.01 | 0.25 |
| Male sex, No. (%) | 180 (69.0) | 48 (82.8) | 29 (93.5) | 0.04 | < 0.01 |
| Coronary artery disease, No. (%) | 16 (6.1) | 39 (67.2) | 29 (93.6) | < 0.01 | < 0.01 |
| Post PCI (BMS) | 2 (0.8) | 8 (13.8) | 8 (25.8) | < 0.01 | < 0.01 |
| Post PCI (DES) | 0 (0) | 9 (15.5) | 19 (61.3) | < 0.01 | < 0.01 |
| Peripheral artery disease, No. (%) | 3 (1.1) | 4 (6.9) | 3 (9.7) | 0.02 | 0.02 |
| Atrial fibrillation, No. (%) | 8 (3.1) | 5 (8.6) | 1 (3.2) | 0.07 | > 0.99 |
| Past cerebral infarction, No. (%) | 4 (1.5) | 18 (31.0) | 3 (9.7) | < 0.01 | 0.03 |
| Diabetes mellitus, No. (%) | 22 (8.4) | 10 (17.2) | 9 (29.0) | 0.05 | < 0.01 |
| Chronic renal failure with hemodialysis, No. (%) | 6 (2.3) | 2 (3.5) | 1 (3.2) | 0.64 | 0.54 |
| Liver cirrhosis, No. (%) | 8 (3.1) | 0 (0) | 0 (0) | 0.36 | > 0.99 |
| Pre-ESD Hb, mean(range, SD), g/dL | 13.4(6.7 – 17.8, 1.7) | 12.8(8.2 – 16.7, 2.1) | 12.1(7.7 – 16.2, 2.0) | 0.01 | < 0.01 |
| Pre-ESD platelets, mean(range, SD), × 109/L | 216(81 – 392, 60) | 216(126 – 372, 52) | 228(141 – 430, 57) | 0.96 | 0.31 |
| Pre-ESD PT-INR, mean(range, SD) | 1.00(0.8 – 1.4, 0.08) | 0.99(0.8 – 1.2, 0.08) | 1.03(0.9 – 1.2, 0.10) | 0.68 | 0.03 |
APT, antiplatelet therapy; DAPT, dual antiplatelet therapy; SD, standard deviation; PCI, percutaneous coronary intervention; BMS, bare metal stent; DES, drug-eluting stent; Hb, hemoglobin; ESD, endoscopic submucosal dissection; PT-INR, international normalized ratio of prothrombin time.Note: Age was older in the single APT group. Percentages of male patients and comorbid arteriosclerotic diseases were higher in the single APT and DAPT groups. Percentage of comorbid diabetes mellitus was higher in the DAPT group. Hemoglobin levels before ESD were lower in the single APT and DAPT groups, but the platelet counts did not differ significantly among the groups. The PT-INR was higher in the DAPT group.
Endoscopic treatment outcomes
Endoscopic treatment outcomes are shown in Table 2. The location of the resected lesion and maximum diameter of the resected specimen did not differ significantly among the groups. Hemoglobin levels after ESD were higher in the no APT group. Rates of post-ESD bleeding were significantly higher in the single APT and DAPT groups than in the no APT group, and the rate of late-onset post-ESD bleeding (bleeding ≥ 8 days after ESD) was higher in the DAPT group. The relationship between antiplatelet therapies and the onset day of post-ESD bleeding is shown in Fig. 3. The rate of the need for blood transfusion was also higher in the single APT group (8.6 %, P < 0.01) and the DAPT group (19.4 %, P < 0.01) than in the no APT group (1.1 %).
Table 2. Treatment outcomes of patients after endoscopic submucosal dissection of a gastric neoplasm.
| (A) No APT group(n = 261) | (B) Single APT group(n = 58) | (C) DAPT group(n = 31) | A vs. B P value | A vs. C P value | |
| Diameter of resected specimen(range, SD), mm | 34.1(6 – 95, 14.1) | 35.6(14 – 90, 15.3) | 37.6(12 – 98, 19.1) | 0.47 | 0.22 |
| Diameter of resected specimen ≥ 40 mm, No. (%) | 73 (28.0) | 20 (34.5) | 11 (35.5) | 0.34 | 0.40 |
| Location of resected lesion, No. | L : M : U = 93 : 100 : 68 | L : M : U = 22 : 20 : 16 | L : M : U = 6 : 16 : 9 | 0.86 | 0.17 |
| Post-ESD Hb, mean(range, SD), g/dL | 12.9(6.5 – 16.6, 1.6) | 12.5(8.2 – 16.1, 2.0) | 12.1(8.6 – 14.6, 1.7) | 0.07 | < 0.01 |
| Post-ESD bleeding, No. (%) | 16 (6.1) | 9 (15.5) | 11 (35.5) | 0.03 | < 0.01 |
| Days after ESD of post-ESD bleeding(range, SD), days | 3.8(0 – 11, 3.6) | 7.3(0 – 16, 5.1) | 8.5(1 – 15, 5.0) | 0.06 | 0.01 |
| Late-onset post-ESD bleeding (≥ 8 days)(percentage all of post-ESD bleeding), No. (%) | 3 (18.8) | 4 (44.4) | 7 (63.6) | 0.20 | 0.04 |
| Blood transfusion, No. (%) | 3 (1.1) | 5 (8.6) | 6 (19.4) | < 0.01 | < 0.01 |
APT, antiplatelet therapy; DAPT, dual antiplatelet therapy; SD, standard deviation; L, lower; M, middle; U, upper; ESD, endoscopic submucosal dissection; Hb, hemoglobin.Note: Unpaired Student’s t test, Fisher’s exact test, and chi-squared test were used.Post-ESD bleeding occurred more frequently in the single APT and DAPT groups, and late-onset bleeding was significantly more common in the DAPT group. The requirement for blood transfusion was also higher in the single APT and DAPT groups. The locations of the resected lesions did not differ significantly among the groups.
Fig. 3.
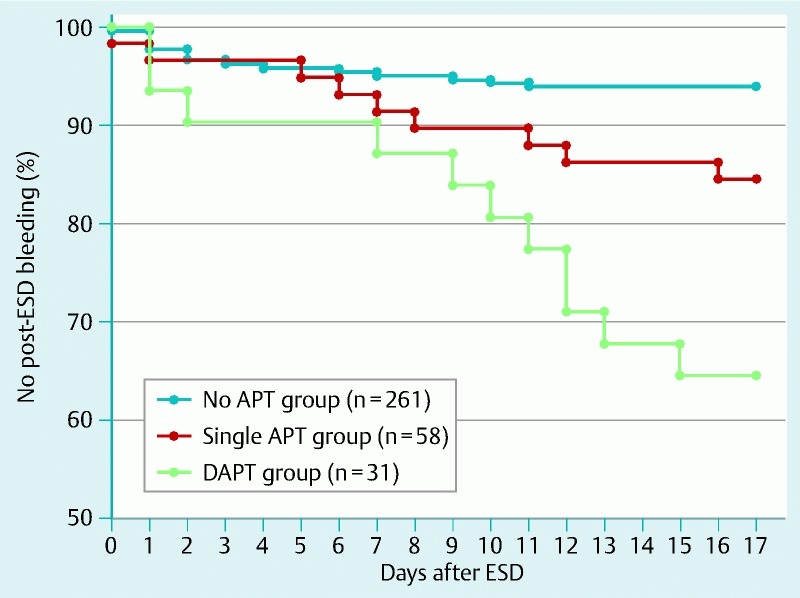
Relationships between antiplatelet therapies and onset of post-endoscopic submucosal dissection (post-ESD) bleeding. The Kaplan–Meier curves show relationships between antiplatelet therapies and the onset of post-ESD bleeding. Late-onset post-ESD bleeding (≥ 8 days after ESD) was most frequent in the dual antiplatelet therapy (DAPT) group.
Primary outcome
The primary outcome (post-ESD bleeding) occurred in 16 of 261 patients (6.1 %) in the no APT group, 9 of 58 patients (15.5 %, P = 0.03 compared with no APT) in the single APT group, and 11 of 31 patients (35.5 %, P < 0.01 compared with no APT) in the DAPT group (Table 2). In the single APT group, post-ESD bleeding occurred in 9 of 53 patients treated with LDA, but in none of the 5 patients treated with a thienopyridine.
Secondary outcomes
Secondary outcomes did not occur from the day before ESD until 30 days after ESD.
Risk factors for post-ESD bleeding
Post-ESD bleeding occurred in 16 of 261 patients in the no APT group, 9 of 58 patients in the single APT group, and 11 of 31 patients in the DAPT group. Univariate comparison of the 25 patients with post-ESD bleeding and 294 patients without bleeding in the no APT and single APT groups showed that chronic renal failure with hemodialysis (P < 0.01), single APT (LDA or thienopyridine, P = 0.02), and diameter of the resected specimen of 40 mm or greater (P = 0.01) were significant risk factors for post-ESD bleeding (Table 3). However, only 8 of the 350 patients had chronic renal failure with hemodialysis, and this factor was excluded from multivariate analysis. In the Cox proportional hazards regression model, single APT (HR 2.7, 95 %CI 1.1 – 6.6, P = 0.03), and diameter of the resected specimen of 40 mm or greater (HR 2.7, 95 %CI 1.2 – 5.9, P = 0.01) were significant risk factors for post-ESD bleeding, but continuous LDA (HR 0.8, 95 %CI 0.2 – 3.6, P = 0.72) was not a significant risk factor (Table 4).
Table 3. Univariate analysis of post-ESD bleeding. Comparison of lesions with and without post-ESD bleeding in the no APT and single APT groups.
| Post-ESD bleeding(25 patients) | No bleeding(294 patients) | P value | |
| Age ≥ 65 years, No. (%) | 21 (84.0) | 233 (79.3) | 0.58 |
| Male sex, No. (%) | 20 (80.0) | 208 (70.7) | 0.33 |
| Comorbidity, No. (%) | |||
| Coronary artery disease | 7 (28.0) | 48 (16.3) | 0.14 |
| Peripheral artery disease | 0 | 7 (2.3) | NA |
| Atrial fibrillation | 0 | 13 (4.4) | NA |
| Cerebrovascular disease | 2 (8.0) | 20 (6.8) | 0.87 |
| Diabetes mellitus | 2 (8.0) | 30 (10.2) | 0.74 |
| Chronic renal failure with hemodialysis | 4 (16.0) | 4 (1.4) | < 0.01 |
| Liver cirrhosis | 0 | 8 (2.7) | NA |
| Single APT, No. (%) | 9 (36.0) | 49 (16.7) | 0.02 |
| Continuous LDA, No. (%) | 2 (8.0) | 12 (4.1) | 0.38 |
| Diameter of resected specimen ≥ 40 mm, No. (%) | 13 (52.0) | 80 (27.2) | 0.01 |
| Early gastric cancer, No. (%) | 23 (92.0) | 255 (86.7) | 0.44 |
| Location of lesion, No. (%) | 0.40 | ||
| Lower | 9 (36.0) | 106 (36.1) | |
| Middle | 12 (48.0) | 108 (36.7) | |
| Upper | 4 (16.0) | 80 (27.2) | |
| Pre-ESD Hb < 12 g/dL, No. (%) | 7 (28.0) | 54 (18.4) | 0.23 |
| Pre-ESD platelet count < 100 × 109/L, No. (%) | 0 | 3 (1.0) | NA |
| Pre-ESD PT-INR > 1.20 s, No. (%) | 0 | 8 (2.7) | NA |
ESD, endoscopic submucosal dissection; APT, antiplatelet therapy; LDA, low dose aspirin; Hb, hemoglobin; PT-INR, international normalized ratio of prothrombin time.Note: The log-rank test was used.Comorbid chronic renal failure with hemodialysis, single APT, and diameter of the resected specimen ≥ 40 mm were significant risk factors in univariate analysis.
Table 4. Multivariate analysis of post-ESD bleeding with a Cox proportional hazards regression model in the no APT and single APT groups.
| Hazard ratio | 95 % Confidence interval | P value | |
| Single APT | 2.7 | 1.1 – 6.6 | 0.03 |
| Continuous LDA | 0.8 | 0.2 – 3.6 | 0.72 |
| Diameter of resected specimen ≥ 40 mm | 2.7 | 1.2 – 5.9 | 0.01 |
APT, antiplatelet therapy; LDA, low dose aspirin; Note: The Cox proportional hazards regression model was used.Single APT and a diameter of the resected specimen ≥ 40 mm were significant risk factors for post-ESD bleeding, but continuous LDA was not a significant risk factor for post-ESD bleeding.
Univariate comparison of the 27 patients with post-ESD bleeding and 265 patients without bleeding in the no APT and DAPT groups showed that comorbid coronary artery disease (P < 0.01), chronic renal failure with hemodialysis (P < 0.01), DAPT (P < 0.01), and continuous LDA (P < 0.01) were significant risk factors for post-ESD bleeding (Table 5). Again, only 7 of the 292 patients had chronic renal failure with hemodialysis, and this factor was excluded from multivariate analysis. In the Cox proportional hazards regression model, DAPT (HR 16.3, 95 %CI 3.4 – 78.2, P < 0.01) was a significant risk factor for post-ESD bleeding, but continuous LDA (HR 1.0, 95 %CI 0.2 – 5.1, P = 0.95) and comorbid coronary artery disease (HR 0.4, 95 %CI 0.1 – 2.3, P = 0.27) were not significant risk factors (Table 6).
Table 5. Univariate analysis of post-ESD bleeding. Comparison of lesions with and without post-ESD bleeding in the no APT and DAPT groups.
| Post-ESD bleeding(27 patients) | No bleeding(265 patients) | P value | |
| Age ≥ 65 years, No. (%) | 21 (77.8) | 202 (76.2) | 0.88 |
| Male sex, No. (%) | 21 (77.8) | 188 (70.9) | 0.47 |
| Comorbidity, No. (%) | |||
| Coronary artery disease | 10 (37.0) | 35 (13.2) | < 0.01 |
| Peripheral artery disease | 1 (3.7) | 5 (1.9) | 0.49 |
| Atrial fibrillation | 1 (3.7) | 8 (3.0) | 0.87 |
| Cerebrovascular disease | 2 (7.4) | 5 (1.9) | 0.07 |
| Diabetes mellitus | 5 (18.5) | 26 (9.8) | 0.15 |
| Chronic renal failure with hemodialysis | 4 (14.8) | 3 (1.1) | < 0.01 |
| Liver cirrhosis | 0 | 8 (3.0) | NA |
| DAPT, No. (%) | 11 (40.7) | 20 (7.5) | < 0.01 |
| Continuous LDA, No. (%) | 8 (29.6) | 16 (6.0) | < 0.01 |
| Diameter of resected specimen ≥ 40 mm, No. (%) | 10 (37.0) | 74 (27.9) | 0.32 |
| Early gastric cancer, No. (%) | 26 (96.3) | 225 (84.9) | 0.11 |
| Location of lesion, No. (%) | 0.40 | ||
| Lower | 8 (29.6) | 91 (34.3) | |
| Middle | 14 (51.9) | 102 (38.5) | |
| Upper | 5 (18.5) | 72 (27.2) | |
| Pre-ESD Hb < 12.0 g/dL, No. (%) | 6 (22.2) | 44 (16.6) | 0.44 |
| Pre-ESD platelet count < 100 × 109/L, No. (%) | 0 | 3 (1.1) | NA |
| Pre-ESD PT-INR > 1.20 , No. (%) | 2 (7.4) | 6 (2.3) | 0.14 |
ESD, endoscopic submucosal dissection; APT, antiplatelet therapy; DAPT, dual antiplatelet therapy; LDA, low dose aspirin; Hb, hemoglobin; PT-INR, international normalized ratio of prothrombin time.Note: The log-rank test was used.Comorbid coronary artery disease, chronic renal failure with hemodialysis, DAPT, and continuous LDA were significant risk factors for post-ESD bleeding.
Table 6. Multivariate analysis of post-ESD bleeding with a Cox proportional hazards regression model in the no APT and DAPT groups.
| Hazard ratio | 95 % Confidence interval | P value | |
| DAPT | 16.3 | 3.4 – 78.2 | < 0.01 |
| Continuous LDA | 1.0 | 0.2 – 5.1 | 0.95 |
| Coronary artery disease | 0.4 | 0.1 – 2.3 | 0.27 |
ESD, endoscopic submucosal dissection; APT, antiplatelet therapy; DAPT, dual antiplatelet therapy; LDA, low dose aspirin.Note: The Cox proportional hazards regression model was used.DAPT was a significant risk factor for post-ESD bleeding, but continuous LDA and comorbid coronary artery disease were not significant risk factors for post-ESD bleeding.
Overall, these results show that APT and a diameter of the resected specimen of 40 mm or greater were significant risk factors for post-ESD bleeding. DAPT markedly increased the bleeding risk, but continuous LDA was not a significant risk factor for post-ESD bleeding.
Complications of ESD and management
One patient underwent surgery because of post-ESD perforation. Post-ESD bleeding occurred in 36 patients, but all of these patients recovered with endoscopic treatment and did not require surgery or radiologic intervention. In the patients receiving continuous LDA, LDA was continued after endoscopic treatment for post-ESD bleeding. In the DAPT group, the period from ESD to the onset of post-ESD bleeding was longer (8.5 vs. 3.8 days, P = 0.01) and the rate of late-onset bleeding was higher (63.6 % vs. 18.8 %, P = 0.04) than in the no APT group (Table 2).
Discussion
The results of this study show that APT (especially DAPT) and a diameter of the resected specimen of 40 mm or greater are significant risk factors for post-ESD bleeding, but that continuous LDA is not a significant risk factor for post-ESD bleeding. Concerning the onset time of post-ESD bleeding, late-onset post-ESD bleeding (≥ 8 days after ESD) occurred most frequently in patients on DAPT. We continued LDA around the time of ESD and resumed thienopyridines 3 days after ESD to prevent thromboembolic complication after DES placement based on the American Heart Association guidelines 1, but the strong antiplatelet action of a thienopyridine combined with aspirin seemed to increase post-ESD bleeding. The requirement for blood transfusion was higher in the single APT group and the DAPT group than in the no APT group. Thus, the antiplatelet action of resumed APT and delayed endoscopic hemostasis after discharge may increase the need for blood transfusion. Delayed resumption of thienopyridines may be useful to decrease post-ESD bleeding, but a thrombotic event after DES placement can cause acute coronary syndrome and be fatal. Endoscopic hemostasis and blood transfusion are required when post-ESD bleeding occurs, but this will rarely be fatal and is safe for patients. Only 9 patients were on hemodialysis, but post-ESD bleeding occurred in 5 of them. Concomitant chronic renal failure and hemodialysis were excluded from the multivariate analysis because of the small number of patients, but this combination may be associated with a high risk for post-ESD bleeding.
There have been several reports on hemorrhagic risk after ESD in patients on APT 12 13 14 15, but the effect of APT is still uncertain. Lim et al. found that continuous APT did not increase the risk for bleeding 12, whereas Cho et al. showed that continuous LDA increased the risk for post-ESD bleeding 14. In these reports, interruption of APT within 7 days was considered to be continuous APT, and patients treated with DAPT were included in the LDA group. In contrast, in the current study, interruption and continuation of LDA were clearly separated, and patients treated with single APT were also clearly separated from those who received DAPT. In patients with a high thromboembolic risk, we continued LDA around the time of ESD and interrupted thienopyridines for only 8 to 10 days, based on American Heart Association guidelines for APT after coronary stenting 1. This short period of interruption of thienopyridines and combination use with aspirin may cause increased post-ESD bleeding and an increased need for blood transfusion, but a long period of DAPT interruption may increase the risk for acute coronary syndrome after DES placement 16 17 18 19. Thus, we continued LDA during ESD and also resumed thienopyridines as soon as possible after ESD, despite the high risk for post-ESD bleeding.
Koh et al. found that a specimen size larger than 40 mm was the only independent risk factor for overall post-ESD bleeding, and that oral antithrombotic therapy was an independent risk factor for delayed bleeding 13. In the study of Koh et al., antithrombotic drug therapy was interrupted preoperatively and restarted immediately after second-look endoscopy 13. This situation is similar to the increase in late-onset bleeding after thienopyridines were restarted in patients on DAPT in the current study, and the strong antiplatelet action of thienopyridines is thought to affect post-ESD bleeding. For lesion size, we identified the diameter of the resected specimen (almost the same as the diameter of the post-ESD ulceration) as a risk factor for post-ESD. The specimen diameter and diameter of the post-ESD ulcer were previously found to be risk factors for bleeding in three other studies 11 12 14. Thus, the diameter of the resected specimen (diameter of the ESD ulcer) was identified as a risk factor for post-ESD bleeding in four previous independent studies 11 12 13 14 and in this study, and it can be considered to be a certain risk factor.
Takeuchi et al. found that combination therapy of LDA with warfarin and a longer ESD duration were significant risk factors for post-ESD bleeding 15. Antithrombotic therapy was interrupted preoperatively and restarted on the day after ESD, but the combination of antiplatelet and anticoagulation drugs increased the risk for post-ESD bleeding 15. We did not investigate the effect of anticoagulation therapy, but the strong antithrombotic action of a combination of antiplatelet and anticoagulation drugs may increase the risk for post-ESD bleeding. This is similar to what occurred in the DAPT group in the current study and suggests that the resumption of multiple antithrombotic therapies should be delayed to prevent post-ESD bleeding. The duration of ESD is affected by many factors, including size of the lesion, location of the lesion, technical skill of the endoscopist, the endoscopic device used, and whether or not hemorrhage occurs during ESD. In the current study, we did not investigate the duration of ESD because it is affected by many factors, but it may be a possible risk factor for post-ESD bleeding.
This study was carried out as a retrospective review in a single center with a limited number of patients, particularly those treated with a single thienopyridine (only 5 patients). Thus, a prospective, randomized, multicenter study is required to confirm the findings. Within these limitations, the results of the study suggest that LDA should not be interrupted if the thromboembolic risk is high, and that post-ESD bleeding should be carefully monitored in patients who are being treated with APT (especially with DAPT), have large gastric lesions, or are on hemodialysis. The resumption of thienopyridines after ESD should be delayed if possible, but thromboembolic risk must be considered, and in some cases thienopyridines should be resumed as soon as possible to prevent fatal complications.
Acknowledgment
We would like to thank the members of TARC (Teikyo Academic Research Center) for their help with the statistical analysis and the reviewers for their comments and suggestions.
Footnotes
Competing interests: None
References
- 1.Grines C L, Bonow R O, Casey D E. et al. Prevention of premature discontinuation of dual antiplatelet therapy in patients with coronary artery stents: a science advisory from the American Heart Association, American College of Cardiology, Society for Cardiovascular Angiography and Interventions, American College of Surgeons, and American Dental Association, with representation from the American College of Physicians. Circulation. 2007;115:813–818. doi: 10.1161/CIRCULATIONAHA.106.180944. [DOI] [PubMed] [Google Scholar]
- 2.Oda I, Saito D, Tada M. et al. A multicenter retrospective study of endoscopic resection for early gastric cancer. Gastric Cancer. 2006;9:262–270. doi: 10.1007/s10120-006-0389-0. [DOI] [PubMed] [Google Scholar]
- 3.Gotoda T, Yamamoto H, Soetikno R M. et al. Endoscopic submucosal dissection of early gastric cancer. J Gastroenterol. 2006;41:929–942. doi: 10.1007/s00535-006-1954-3. [DOI] [PubMed] [Google Scholar]
- 4.Anderson M A, Ben-Menachem T, Gan S I. et al. Management of antithrombotic agents for endoscopic procedures. Gastrointest Endosc. 2009;70:1060–1070. doi: 10.1016/j.gie.2009.09.040. [DOI] [PubMed] [Google Scholar]
- 5.Veitch A M, Baglin T P, Gershlich A H. et al. Guidelines for the management of anticoagulant and antiplatelet therapy in patients undergoing endoscopic procedures. Gut. 2008;57:1322–1329. doi: 10.1136/gut.2007.142497. [DOI] [PubMed] [Google Scholar]
- 6.Boustière C, Veitch A, Vanbiervliet G. et al. Endoscopy and antiplatelet agents. European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2011;43:445–458. doi: 10.1055/s-0030-1256317. [DOI] [PubMed] [Google Scholar]
- 7.Fujimoto K, Fujishiro M, Kato M. et al. Guidelines for gastroenterological endoscopy in patients undergoing antithrombotic treatment. Dig Endosc. 2014;26:1–14. doi: 10.1111/den.12183. [DOI] [PubMed] [Google Scholar]
- 8.Tamai Y, Komatsu T, Takami H. et al. Management of antiplatelet therapy for endoscopic procedures: optimal cessation period of antiplatelet therapy for Japanese. Dig Endosc. 2007;19:161–166. [Google Scholar]
- 9.Uedo N, Takeuchi Y, Yamada T. et al. Effect of a proton pump inhibitor or an H2-receptor antagonist on prevention of bleeding from ulcer after endoscopic submucosal dissection of early gastric cancer: a prospective randomized controlled trial. Am J Gastroenterol. 2007;102:1610–1616. doi: 10.1111/j.1572-0241.2007.01197.x. [DOI] [PubMed] [Google Scholar]
- 10.Yang Z, Wu Q, Liu Z. et al. Proton pump inhibitors versus histamine-2-receptor antagonists for the management of iatrogenic gastric ulcer after endoscopic mucosal resection or endoscopic submucosal dissection: a meta-analysis of randomized trials. Digestion. 2011;84:315–320. doi: 10.1159/000331138. [DOI] [PubMed] [Google Scholar]
- 11.Okada K, Yamamoto Y, Kasuga A. et al. Risk factors for delayed bleeding after endoscopic submucosal dissection for gastric neoplasm. Surg Endosc. 2011;25:98–107. doi: 10.1007/s00464-010-1137-4. [DOI] [PubMed] [Google Scholar]
- 12.Lim J H, Kim S G, Kim J W. et al. Do antiplatelets increase the risk of bleeding after endoscopic submucosal dissection of gastric neoplasms? Gastrointest Endosc. 2012;75:719–727. doi: 10.1016/j.gie.2011.11.034. [DOI] [PubMed] [Google Scholar]
- 13.Koh R, Hirasawa K, Yahara S. et al. Antithrombotic drugs are risk factors for delayed postoperative bleeding after endoscopic submucosal dissection for gastric neoplasms. Gastrointest Endosc. 2013;78:476–483. doi: 10.1016/j.gie.2013.03.008. [DOI] [PubMed] [Google Scholar]
- 14.Cho S J, Choi I J, Kim C G. et al. Aspirin use and bleeding risk after endoscopic submucosal dissection in patients with gastric neoplasms. Endoscopy. 2012;44:114–121. doi: 10.1055/s-0031-1291459. [DOI] [PubMed] [Google Scholar]
- 15.Takeuchi T, Ota K, Harada S. et al. The postoperative bleeding rate and its risk factors in patients on antithrombotic therapy who undergo gastric endoscopic submucosal dissection. BMC Gastroenterol. 2013;13:136. doi: 10.1186/1471-230X-13-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McFadden E P, Stabile E, Regar E. et al. Late thrombosis in drug-eluting coronary stents after discontinuation of antiplatelet therapy. Lancet. 2004;364:1519–1521. doi: 10.1016/S0140-6736(04)17275-9. [DOI] [PubMed] [Google Scholar]
- 17.Spertus J A, Kettelkamp R, Vance C. et al. Prevalence, predictors, and outcomes of premature discontinuation of thienopyridine therapy after drug-eluting stent placement: results from the PREMIER registry. Circulation. 2006;113:2803–2809. doi: 10.1161/CIRCULATIONAHA.106.618066. [DOI] [PubMed] [Google Scholar]
- 18.Pfisterer M, Brunner-La Rocca H P, Buser P T. et al. Late clinical events after clopidogrel discontinuation may limit the benefit of drug-eluting stents: an observational study of drug-eluting versus bare-metal stents. J Am Coll Cardiol. 2006;48:2584–2591. doi: 10.1016/j.jacc.2006.10.026. [DOI] [PubMed] [Google Scholar]
- 19.Eisenstein E L, Anstrom K J, Kong D F. et al. Clopidogrel use and long-term clinical outcomes after drug-eluting stent implantation. JAMA. 2007;297:159–168. doi: 10.1001/jama.297.2.joc60179. [DOI] [PubMed] [Google Scholar]


