Abstract
Background and study aims: Biliary and pancreatic diseases are common in the elderly; however, few studies have addressed the occurrence of adverse events in elderly patients undergoing endoscopic retrograde cholangiopancreatography (ERCP). Our objective was to determine the incidence rates of specific adverse events in this group and calculate incidence rate ratios (IRRs) for selected comparison groups.
Patients and methods: Bibliographical searches were conducted in Medline, EMBASE, and Cochrane library databases. The studies included documented the incidence of adverse events (perforation, pancreatitis, bleeding, cholangitis, cardiopulmonary adverse events, mortality) in patients aged ≥ 65 who underwent ERCP. Pooled incidence rates were calculated for each reported adverse event and IRRs were determined for available comparison groups. A parallel analysis was performed in patients aged ≥ 80 and ≥ 90.
Results: Our literature search yielded 7429 articles, of which 69 studies met our inclusion criteria. Pooled incidence rates for adverse events (per 1000 ERCPs) in patients aged ≥ 65 were as follows: perforation 3.8 (95 %CI 1.8 – 7.0), pancreatitis 13.1 (95 %CI 11.0 – 15.5), bleeding 7.7 (95 %CI 5.7 – 10.1), cholangitis 16.1 (95 %CI 11.7 – 21.7), cardiopulmonary events 3.7 (95 %CI 1.5 – 7.6), and death 7.1 (95 %CI 5.2 – 9.4). Patients ≥ 65 had lower rates of pancreatitis (IRR 0.3, 95 %CI 0.3 – 0.4) compared with younger patients. Octogenarians had higher rates of death (IRR 2.4, 95 %CI 1.3 – 4.5) compared with younger patients, whereas nonagenarians had increased rates of bleeding (IRR 2.4, 95 %CI 1.1 – 5.2), cardiopulmonary events (IRR 3.7, 95 %CI 1.0 – 13.9), and death (IRR 3.8, 95 %CI 1.0 – 14.4).
Conclusions ERCP appears to be safe in elderly patients, except in the very elderly who are at higher risk of some adverse events. These data on adverse event rates can help to inform clinical decision-making, the consent process, and comparative effectiveness analyses.
Introduction
The elderly population of the United States is predicted to double from 35 to 71 million people in the next 30 years 1 At the same time, diseases such as choledocholithiasis and malignancy, and the postoperative management of adverse events following biliary surgery 2 3 are all more prevalent in the elderly population 4 5. Therefore, the incidence of biliary and pancreatic diseases will continue to rise, along with the rise in our aging population. Endoscopic retrograde cholangiopancreatography (ERCP) is a diagnostic and therapeutic procedure that can directly treat many of these pancreaticobiliary diseases and can represent a safer alternative to surgery for the elderly in some circumstances 6. However, ERCP is not without risk, with a reported adverse event rate of 5 % – 10 % 7 8 and a mortality rate of 0.3 % – 0.5 % 7 9. Moreover, these risks may be exacerbated by age, and their consequences may be more severe and protracted in the elderly. With the dramatic rise in the elderly population, it is anticipated that ERCP will be in greater demand for this group of patients in the next few years. As a result, it is vital to better understand ERCP adverse events in the elderly, in order to balance the risks and benefits and to provide better information for older patients so they can make more informed decisions about undergoing ERCP.
Currently, there is a dearth of literature on ERCP and adverse events in the elderly, but there have been several studies published suggesting that ERCP is safe in patients aged ≥ 65 years 5 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29. However, most of these studies are small, and in many cases they focus on one adverse event only, thereby limiting the generalizability of their conclusions. To our knowledge, no systematic review or meta-analysis comparing elderly and non-elderly patients with respect to adverse events following ERCP has been performed. Because of this gap in the literature, we aimed to determine the incidence rates for specific adverse events in elderly patients undergoing ERCP and to calculate specific incidence rate ratios of ERCP adverse events between younger and older patients.
Patients/materials and methods
Study population
We performed a systematic review of computerized bibliography databases for studies that included elderly patients who underwent ERCP and that had reported adverse events. Elderly was defined using the World Health Organization’s definition of patients 65 years of age and older.
Literature search
We searched computerized bibliography databases including MEDLINE (1950 to August 1, 2012), EMBASE (1980 to August 1, 2012), and Cochrane Review Library (1992 to August 1, 2012). Search terms included “ERCP” and “elderly” combined with any of the following key words/MeSH headings: “adverse event(s),” “complications,” or specific adverse events related to ERCP including “abdominal pain,” “pancreatitis,” “perforation(s),” “bleeding,” “post-sphincterotomy bleeding,” “cholangitis,” “cardiovascular adverse event(s),” “respiratory adverse event(s),” “hospitalization(s),” or “death(s).” The references of all retrieved articles were reviewed to identify additional studies. Lastly, a manual search of abstracts submitted to Digestive Diseases Week and the American College of Gastroenterology Annual Conference (2001 – 2012) was performed.
Inclusion and exclusion criteria
Studies were included if adverse events related to the performance of an ERCP in patients 65 years of age and older were reported and could be abstracted. ERCPs performed in both the outpatient and inpatient setting were included, as were both diagnostic and therapeutic procedures. Three age strata were present in the literature: the elderly (≥ 65), octogenarians (≥ 80), and nonagenarians (≥ 90). Articles were limited to randomized, controlled trials and cohort studies (prospective and retrospective) with no restriction on language.
Data abstraction
Data on the following six categories of adverse events were abstracted from the full articles:
(i) pancreatitis
(ii) perforation
(iii) bleeding (including post-sphincterotomy bleeding)
(iv) cholangitis
(v) cardiopulmonary adverse events
(vi) mortality related to the performance of the ERCP
Adverse events were identified and attributed to the performance of the ERCP by the authors of each study. The following definitions were used for each specific adverse event that was abstracted. Pancreatitis was defined as the onset of new abdominal pain, with at least a three-fold elevation of serum amylase or lipase levels, at least 24 hours after the procedure, which required more than 1 night of hospitalization. Perforation was defined as retroperitoneal or bowel-wall perforation, as evidenced by any imaging technique. Bleeding adverse events were defined as clinical evidence of hemorrhage, with a decrease in hemoglobin > 2 g/dL or the need for endoscopic or transfusion treatment. Cholangitis was defined as a temperature of more than 38 °C for 24 – 48 hours occurring after the procedure and thought to have a biliary cause, without evidence of other concomitant infections. Cardiopulmonary adverse events included myocardial infarction, cerebrovascular accident, congestive heart failure, cardiac/respiratory arrest, arrhythmia, hypoxemia (oxygen saturation < 90 %), hypotension (systolic blood pressure < 90 mmHg), bradycardia (heart rate < 60 beats/minute), tachycardia (heart rate > 110 beats/minute), or vasovagal response, all of which had to be attributed to the performance of an ERCP.
Of note, we did not use established consensus criteria, such as the Cotton classification 30, in developing the definitions of adverse events for our study. Unfortunately, in the available literature on the adverse events of ERCP in the elderly, the level of detail required by the Cotton classification, such as the number of days that a symptom persisted or how long a patient was hospitalized, was not present in the vast majority of studies, hence less stringent criteria were employed.
Secondary data abstracted included the type of center where the study was performed, trainee involvement, the use of general anesthesia, and cannulation rate of the major papilla. Two authors (L. W. D and L. L.) independently screened and reviewed all titles, abstracts, and full articles for eligibility. If there was a discrepancy between the two reviewers, M.S. also reviewed the article and a consensus was then reached among all three authors.
Statistical analysis
Adverse event primary outcomes were selected a priori based on their clinical importance and included pancreatitis, perforation, bleeding (including post-sphincterotomy bleeding), cholangitis, cardiopulmonary adverse events, and mortality. We used the assessments made by the authors of each included article with regards to whether each of the adverse events was directly related to the performance of an ERCP.
First, the incidence rate of each primary outcome (using pooled data for each specific adverse event) was calculated (adverse event per 1000 ERCPs). Incidence rate calculations were performed for three age strata: (i) patients ≥ 65 years, (ii) patients ≥ 80 years, and (iii) patients ≥ 90 years. These age strata were selected because studies in the available literature involving adverse events and ERCPs were mostly categorized according to these three age strata. Incidence rates and the 95 % confidence intervals (CIs) were calculated using the binomial distribution.
Second, a meta-analysis was performed to examine the association between different age strata and the incidence rates of selected ERCP adverse events. In the meta-analysis, we analyzed pancreatitis, perforation, bleeding, cholangitis, cardiopulmonary adverse events, and mortality, with respect to the following grouping of patients: (i) ≥ 65 versus < 65, (ii) ≥ 80 versus < 80, and (iii) ≥ 90 versus < 90. Studies were assigned weights based on their sample size (number of included ERCPs) as a function of the statistical test. The primary analysis was performed using the random-effects model. Incidence rate ratios (IRRs) with 95 %CIs were calculated for each analysis. A statistically significant result was observed with a 95 %CI and a P value < 0.05. Not all studies used for incidence rate calculations were included in the meta-analysis because some studies did not have a younger age group with which to make a comparison 14 17 19 23 24 27 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50.
Third, sensitivity analyses were attempted to assess the effect of known or potential risk factors on specific adverse events in the elderly. Risk factors considered for the sensitivity analyses included performance of a pancreatogram, having a precut preformed, suspected sphincter of Oddi dysfunction (SOD), cannulation rate, trainee involvement, center type, presence of one or more comorbid medical conditions, and use of aspirin/nonsteroidal anti-inflammatory drugs, anticoagulants, or antiplatelet agents. However, sensitivity analyses could not be performed for specific ERCP adverse events as data on individual risk factors could not be stratified by both age and adverse event. Instead, the relationships between the rates of relevant risk factors and rates of adverse events were examined using a Spearman’s rank correlation coefficient.
Heterogeneity was calculated using a χ2 test with n – 1 degrees of freedom, where n represents the number of studies included with P < 0.10 representing significant heterogeneity. Kendall’s tau was determined, and a funnel plot constructed to test for publication bias. All statistical analyses were calculated using Stata software version 11.0 (StataCorp, College station, Texas, USA).
Results
Our initial search strategy yielded 7429 articles. After initial title and abstract review, 711 articles remained for full manuscript review. A total of 642 articles were excluded with the most frequent reason being that both the number of ERCPs and specific number of adverse events could not be abstracted from the articles and stratified into any of the three age strata (Fig. 1).
Fig. 1.
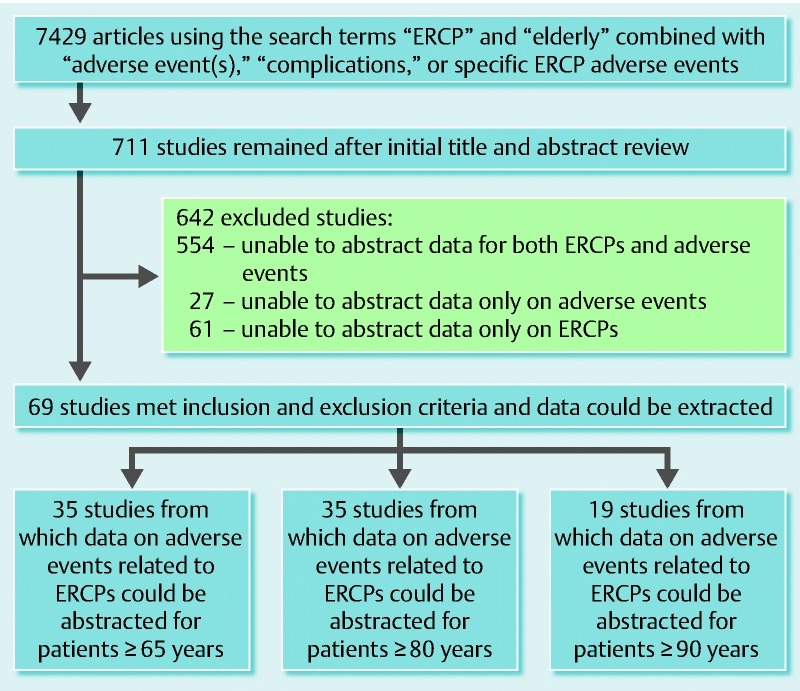
Flow chart of the inclusion and exclusion of studies for the systematic review and meta-analysis of adverse events in older patients undergoing endoscopic retrograde cholangiopancreatography (ERCP). Note: data from the included studies could be abstracted for more than two age stratifications.
Characteristics of included studies
There were 69 articles included in the study. Of the included studies, there were three randomized controlled studies, 37 prospective cohort studies, and 29 retrospective cohort studies. There were 35 studies from which data could be abstracted on patients over 65 6 13 19 23 31 32 33 34 35 47 51 52 53 54 55 56 57 58 59 60 61 62 63 64 65 66 67 68 69 70 71 72 73 74 75 and over 80 5 6 10 11 14 15 20 25 26 28 31 33 36 37 38 39 40 41 48 49 55 56 57 60 64 66 67 69 71 75 76 77 78 79 80 in which 10 286 and 4036 ERCPs had been performed, respectively; 19 studies were available from which data could be abstracted on patients over 90 10 11 17 20 24 27 42 43 44 45 46 50 57 60 64 69 78 81 82 and these involved 742 ERCPs. A majority of included studies were performed at academic centers (91.2 %) and involved trainees (89.2 %), and a third of cases had anesthetic support (31.3 %). The mean rate for cannulation of the common bile duct was 95.3 % among the included studies.
Systematic review of ERCP adverse event incidence rates in elderly patients
Patients over the age of 65 years
Table 1 represents a summary of the pooled incidence rates for specific adverse events related to ERCP and stratified by age. With respect to individual adverse events in patients aged ≥ 65 years of age, the rate of pancreatitis was 13.1 /1000 ERCPs (95 %CI 11.0 – 15.5) 13 19 23 31 32 33 34 35 47 51 52 53 54 55 56 58 59 60 61 62 63 64 66 67 68 69 70 72 73 74 75 83, perforation rate was 3.8 /1000 ERCPs (95 %CI 1.8 – 7.0) 13 19 23 31 32 33 34 35 47 51 52 53 55 58 59 60 61 62 63 64 66 67 68 69 72 74 75 83, and bleeding rate was 7.7 /1000 ERCPs (95 %CI 5.7 – 10.1) 13 19 23 31 32 33 34 35 47 51 52 53 55 56 58 59 60 61 62 63 64 66 67 68 69 70 72 74 75 83. Cholangitis was the most frequent adverse event reported in the literature for patients ≥ 65 (16.1 /1000 ERCPs, 95 %CI 11.7 – 21.7) 13 19 23 31 32 33 34 35 47 51 52 53 55 58 59 60 61 62 63 64 65 66 67 69 71 72 74 75 83.
Table 1. Summary of incidence rates for specific adverse events related to endoscopic retrograde cholangiopancreatography (ERCP) stratified by age.
| Age | Number of adverse events/number of ERCPs (%) | Incidence rate per 1000 ERCPs (95 % CI) |
| ≥ 65 years | ||
| Pancreatitis | 133/10 146 (1.3) | 13.1 (11.0 – 15.5) |
| Perforation | 10/2630 (0.4) | 3.8 (1.8 – 7.0) |
| Bleeding | 50/6506 (0.8) | 7.7 (5.7 – 10.1) |
| Cholangitis | 43 /2664 (1.6) | 16.1 (11.7 – 21.7) |
| Cardiopulmonary | 7/1903 (0.4) | 3.7 (1.5 – 7.6) |
| Death | 47 /6614 (0.7) | 7.1 (5.2 – 9.4) |
| ≥ 80 years | ||
| Pancreatitis | 65/3586 (1.8) | 18.1 (14.0 – 23.0) |
| Perforation | 11/2462 (0.4) | 4.5 (2.2 – 8.0) |
| Bleeding | 35/3157 (1.1) | 11.1 (7.7 – 15.4) |
| Cholangitis | 10/2446 (0.4) | 4.1 (2.0 – 7.5) |
| Cardiopulmonary | 52/1313 (4.0) | 39.6 (29.7 – 51.6) |
| Death | 22/3605 (0.6) | 6.1 (3.8 – 9.2) |
| ≥ 90 years | ||
| Pancreatitis | 9/735 (1.2) | 12.2 (5.6 – 23.1) |
| Perforation | 1/741 (0.1) | 1.3 (0 – 7.5) |
| Bleeding | 21/735 (2.9) | 28.6 (17.8 – 43.3) |
| Cholangitis | 5 /735 (0.7) | 6.8 (2.2 – 15.8) |
| Cardiopulmonary | 6/726 (0.8) | 8.3 (3.0 – 17.9) |
| Death | 2/742 (0.3) | 2.7 (0.3 – 9.7) |
CI, confidence interval.
Patients over the ages of 80 and 90 years
Varying adverse event incidence rates were observed in patients aged ≥ 80 and ≥ 90 years (Table 1). The lowest adverse event incidence rates in octogenarians were for perforation and cholangitis, while cardiopulmonary adverse events were the most frequently reported 10 11 14 15 25 28 31 33 36 38 40 48 49 55 60 64 66 67 69 75 76 77 83. Additionally, the mortality rate was 6.1 deaths/1000 ERCPs (95 %CI 3.8 – 9.2) 5 10 11 14 15 20 25 26 28 31 33 36 37 38 40 41 48 49 55 56 57 60 64 66 67 69 75 76 77 78 79 83, with 22 documented deaths among 32 of the studies involving octogenarians. Lastly, among patients ≥ 90, the most frequent adverse event was bleeding with an incidence rate of 28.6/1000 ERCPs (95 %CI 17.8 – 43.3) 10 11 17 20 24 27 42 43 44 45 46 50 60 64 69 81 82, with perforation and mortality rates being the lowest at 1.3 perforations/1000 ERCPs (95 %CI 0 – 7.5) 10 11 17 20 24 27 42 43 44 45 46 50 60 64 69 78 81 82 and 2.7 deaths/1000 ERCPs (95 %CI 0.3 – 9.7) 10 11 17 20 24 27 42 43 44 45 46 50 57 60 64 69 78 81 82, respectively, in this age group.
Meta-analysis for adverse events in elderly patients undergoing ERCP
Older age appeared to modify the risk of developing specific ERCP adverse events. In contrast to the incidence rate calculations above, there were far fewer studies included in the meta-analyses because some of the studies did not include patients in a younger age group with which to make comparisons. Patients ≥ 65 years of age were 70 % less likely to have an episode of post-ERCP pancreatitis compared with younger patients (IRR 0.3; 95 %CI 0.3 – 0.4; P = 0.7 for heterogeneity) 13 52 54 56 58 59 61 62 63 67 73 74 75 (Fig. 2).
Fig. 2.
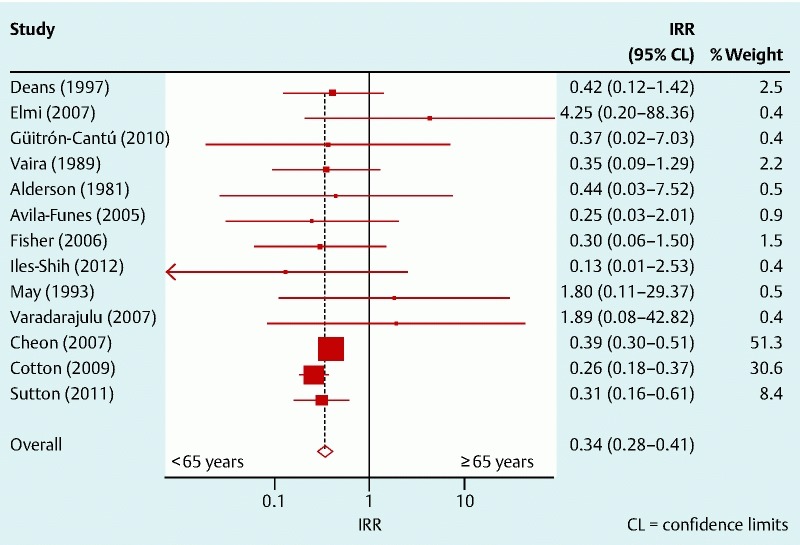
Incidence rate ratio for the development of post-endoscopic retrograde cholangiopancreatography (ERCP) pancreatitis among patients aged ≥ 65 years and < 65 years.
Nonagenarians had the highest risk of having an adverse event related to an ERCP. Bleeding (IRR 2.4; 95 %CI 1.1 – 5.2; P = 0.4 for heterogeneity) 10 11 20 60 64 69 81 82 (Fig. 3), cardiopulmonary adverse events (IRR 3.7; 95 %CI 1.0 – 13.9; P = 0.7 for heterogeneity) 69 81 (Fig. 4), and mortality (IRR 3.8; 95 %CI 1.0 – 14.4; P = 0.8 for heterogeneity) 10 20 57 60 (Fig. 5) were all significantly more elevated in patients ≥ 90 years of age compared with patients < 90. Lastly, octogenarians had a more than a two-fold risk of procedure-related death (IRR 2.4; 95 %CI 1.3 – 4.5; P = 0.9 for heterogeneity) 5 10 15 31 56 57 60 75 compared with patients < 80 (Fig. 5). There was no significant difference between elderly patients (in all three age strata) and younger patients with respect to perforation, cholangitis, and all adverse events combined.
Fig. 3.
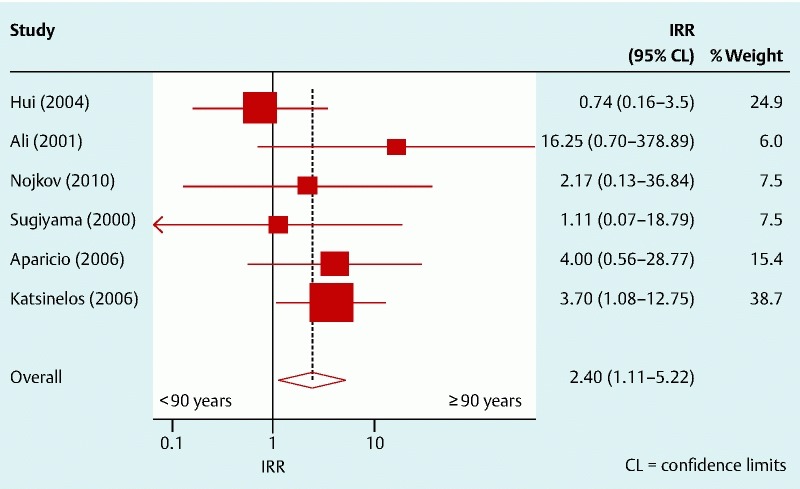
Incidence rate ratio for the development of bleeding after an endoscopic retrograde cholangiopancreatography (ERCP) among patients aged ≥ 90 years and < 90 years.
Fig. 4.
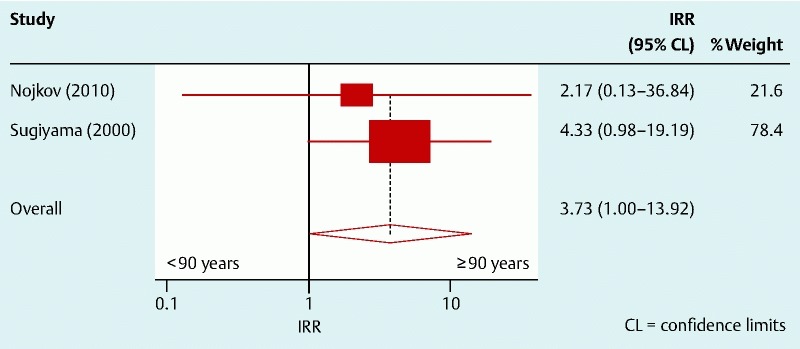
Incidence rate ratio for the development of cardiopulmonary adverse events after an endoscopic retrograde cholangiopancreatography (ERCP) among patients aged ≥ 90 years and < 90 years.
Fig. 5.
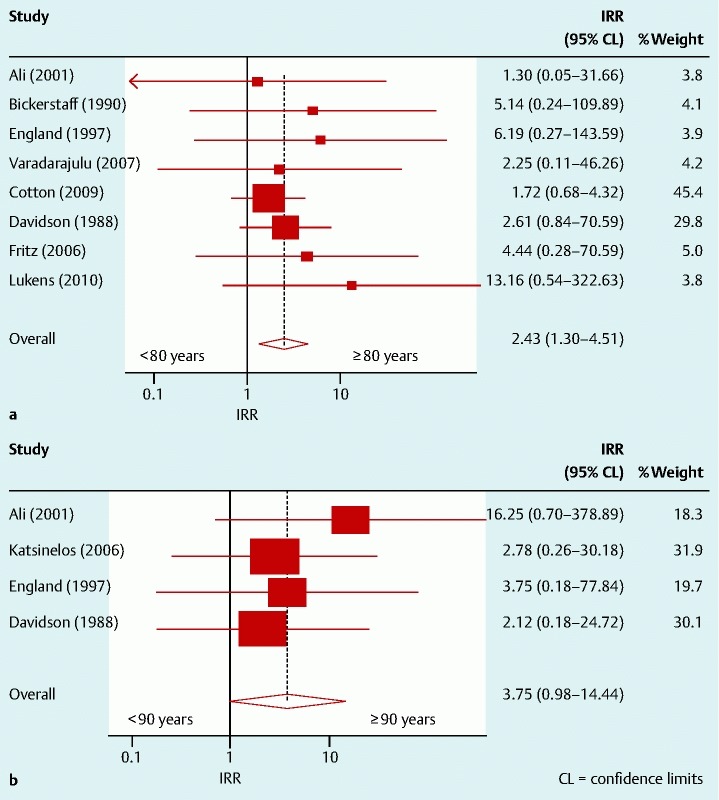
Incidence rate ratio for mortality related to the performance of an endoscopic retrograde cholangiopancreatography (ERCP) among patients aged: a ≥ 80 years and < 80 years; b ≥ 90 years and < 90 years.
Visual inspection of the funnel plots and statistical analysis showed no evidence of significant publication bias.
Individual risk factors and the development of ERCP adverse events
Several risk factors were correlated with ERCP adverse events based on age as shown in Table 2. In the elderly, suspected SOD was positively correlated with pancreatitis (Rs 0.3, P = 0.02), while the cannulation rate was inversely correlated with pancreatitis (Rs – 0.5, P = 0.001). A similar pattern existed in the non-elderly, except that no correlation was evident between cannulation rate and pancreatitis. Furthermore, a negative correlation existed between cannulation rate and the risk of perforation (Rs – 0.5, P = 0.005) in the elderly, with a less robust relationship in the non-elderly (Rs – 0.4, p = 0.06). Lastly, having a precut performed was positively correlated with bleeding risk in the elderly (Rs 0.9, P < 0.001). Data on all other risk factors either showed no relationship or there was insufficient data present.
Table 2. Correlation between age and individual risk factors related to specific endoscopic retrograde cholangiopancreatography (ERCP) adverse events.
| Adverse event | Patients aged ≥ 65 years | Patients aged < 65 years | ||
| Spearman’s rho | P value | Spearman’s rho | P value | |
| Pancreatitis | ||||
| Sphincter of Oddi dysfunction suspected | 0.3 | 0.02 | 0.3 | 0.05 |
| Cannulation rate | – 0.5 | 0.001 | – 0.3 | 0.1 |
| Perforation | ||||
| Cannulation rate | – 0.5 | 0.005 | – 0.4 | 0.06 |
| Bleeding | ||||
| Precut performed | 0.9 | < 0.001 | No relationship | |
Discussion
As individuals live longer, information regarding age-based differences with respect to developing ERCP-related adverse events will be increasingly important for patients and providers. Our study had two important findings. First, we have demonstrated that the incidence and risk of developing specific adverse events during ERCP varies by age. For example, among octogenarians, cardiopulmonary adverse events were by far the most frequent type of adverse event, whereas nonagenarians had more adverse events related to bleeding. Second, we found that age appears to modify the risk of developing some ERCP-related adverse events and particularly increased the risk of certain events. Nonagenarians were at higher risk of ERCP-related bleeding and cardiopulmonary adverse events, while both octogenarians and nonagenarians had an increased mortality risk. Such information can be informative in deciding if ERCP is the best course of action in elderly patients and should be integrated into our discussions with patients and families during the informed consent process.
ERCP is one of the more invasive endoscopic procedures, with higher adverse events when compared with other procedures performed by gastroenterologists. However, reported adverse event rates for ERCP in the literature vary extensively, span several decades, and provide little information with respect to the role played by age. Pancreatitis is the most common adverse event, with a reported incidence of 35/1000 ERCPs, but the range varies widely from 16 – 157/1000. The less common adverse events vary as follows: perforation 1 – 6/1000, bleeding 12 – 15/1000, cholangitis and cardiopulmonary adverse events both 10 /1000, and mortality 2 – 5/1000 9. Our calculated adverse event incidence rates for patients aged ≥ 65 fell within the ranges for most of these reported rates in the literature, suggesting that ERCP is safe in the elderly 5 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29.
Interestingly, in contrast to the previous literature, pancreatitis was not the most common adverse event seen in elderly patients; instead, bleeding and cardiopulmonary adverse events dominated. Moreover, cardiopulmonary adverse events in patients aged ≥ 80, most of which were transient, and bleeding in patients aged ≥ 90 were significantly higher than previously reported rates. Several factors may explain these findings including that these patients may have: a higher number or more severe comorbid medical conditions 84, were taking a higher number of prescribed medications 85, or showed greater sensitivity to sedation, as may occur in the very elderly.
Our study illustrates several important findings with respect to age and post-ERCP pancreatitis. First, increasing age appears to have a protective role against the development of post-ERCP pancreatitis. Our finding that patients over 65 were at significantly lower risk of developing post-ERCP pancreatitis (nearly 70 %) compared with younger patients is in concordance with published data 5 8 10 22 54 73. It is unclear why the elderly appear to be at lower risk of pancreatitis, but increased pancreatic atrophy, increased pancreatic fibrosis, or reduced levels of pancreatic enzyme secretion may explain such findings 5.
Second, our data confirm that specific factors related both to the patient and the endoscopist can lead to the development of post-ERCP pancreatitis and may be further influenced by age. Our data agreed with the widely observed correlations between post-ERCP pancreatitis and suspected SOD, and difficult cannulation 56 86 87 88. In our study, these correlations were seen more prominently in the elderly, with difficult cannulation being the most powerful predictor. Difficult cannulation of the common bile duct may be more frequent in the elderly owing to altered anatomy from previous surgery, higher rates of duodenal diverticulum 14, or scarring of the major papilla from the passage of small stones over time.
Surprisingly in our analysis the performance of pancreatograms did not correlate with the development of post-ERCP pancreatitis. These findings are in contrast to previous studies 8 54 56 86 87 89; yet this observation may be related to the number of pancreatograms performed or the endoscopists’ level of experience, neither of which we were able to account for in our data abstraction. Overall, the elderly were at lower risk of experiencing post-ERCP pancreatitis, but some factors such as suspected SOD and difficult cannulation added to this risk in elderly patients.
Additionally, our research illustrates that the very elderly, in particular patients over 90, are at greater risk of certain ERCP-related adverse events, specifically bleeding and cardiopulmonary adverse events. Nonagenarians had twice the risk of bleeding compared with younger patients, which may be due to the increased prevalence in this age group of coagulopathy, the taking of medications that could increase bleeding risk, big stones that require a larger sphincterotomy and more therapeutic maneuvers 59, and/or periampullary diverticulum 14.
Along the same lines, nonagenarians in our meta-analysis also had a nearly four-fold increase in the risk of cardiopulmonary adverse events compared with younger patients. This finding may reflect a greater incidence and severity of comorbid medical conditions in the very elderly, or that very elderly patients may have longer procedure times owing to more therapy during an ERCP. As an example, the association between older age and common bile duct stones that are difficult to remove has been well reported 20, and this can lead to longer procedure times and potentially more sedation being administered in the elderly. Furthermore, studies have shown that older patients are at increased risk of myocardial injury if ERCP is prolonged for > 30 minutes 61. Our findings suggest that special care needs to be taken in patients aged ≥ 90 before they undergo ERCP, and that strategies need to be employed to minimize these two adverse events.
Finally, our study sheds light on mortality risk and ERCP with respect to age. Mortality is a rare adverse event in patients undergoing ERCP, but our meta-analysis interestingly demonstrated a trend of increasing mortality in the very elderly: a two-fold increase in octogenarians and nearly a four-fold increase in nonagenarians when compared with younger patients. These findings are concerning and should make endoscopists pause.
The elevated mortality rate may be driven by several factors: an increase in comorbid medical conditions 90 91, polypharmacy in the very elderly 92, poor functional status and frailty 93, a more acute presentation of the illness, and/or higher incidence rates for other adverse events that can lead to death. This trend has not been reported in the literature, most likely because previous studies have been of smaller size; however, the strength of our systematic review and meta-analysis is that pooling data together from a large number of studies can help to reduce such limitations. Therefore, despite adverse events being low, mortality rates in the elderly are higher when compared with their younger counterparts, and this serves to further alert clinicians to the fact that the elderly may be more susceptible to adverse outcomes following ERCP and that such risks need to be considered when deciding if ERCP is warranted.
Several limitations exist with our study. First, other factors in addition to age may have contributed to our observation of increased incidence rates of adverse events related to ERCP. Although age may serve as a surrogate for risk, the true mediator of risk, such as the number and severity of comorbid medical conditions, could not be accounted for in our study. Also the use of anticoagulants and nonsteroidal or anti-platelet agents were not routinely reported in our studies; such information would have been useful to determine whether their use correlated with an increased risk of bleeding in this patient population. Moreover, data on the nature of the ERCP, whether elective or emergent and diagnostic or therapeutic, could not be abstracted and may have played a role in the development of adverse events.
Second, we could not assess other adverse events such as cholecystitis, abdominal pain, and hospitalizations. In many cases, these were not consistently reported, could not be abstracted from the studies examined, or were documented only in case reports. Third, among the data on death post-ERCP, the causes of death, as well as the patient’s comorbid medical conditions, were not present in the majority of studies, which made it difficult to determine if the deaths in these cases were truly attributable to the performance of an ERCP. Therefore, the mortality rate we report may in fact be lower than the true rate. Fourth, it was difficult to compare our pooled incidence rates for each adverse event among each of the three age strata given that the data was abstracted from several different studies. For example, there were only four studies in which data could be abstracted on specific adverse events for all three age strata.
In addition, we excluded studies that did not specifically mention adverse events because we were unable to be certain whether there had not been any adverse events or whether the authors had chosen not to mention them in their article. By doing this, we could have overestimated the rate of adverse events reported in our analysis. Clearly, larger studies that focus on the risk factors for elderly patients undergoing ERCP are needed in order to more accurately determine the incidence rates for specific adverse events in each age strata. Such information would then allow one to make more robust comparisons among each age group with respect to the incidence of specific adverse events.
Also, over 90 % of the ERCPs in our study were performed at academic medical centers and nearly a third were performed with anesthetic support, so our results may not be generalizable to ERCPs performed in the community. However, within the last decade there has been an increasing trend toward having ERCPs performed at centers of excellence, many of which are located at large academic centers and are similar to the institutions in our study. Lastly, a further limitation of our study is that few studies were available in which meta-analyses could be performed with respect to specific adverse events, which again limits the generalizability of our results.
In summary, our study highlights that while ERCP was relatively safe in the elderly, the very elderly were at greatest risk of having an adverse event. While patients aged ≥ 65 were at lower risk of developing ERCP-related pancreatitis, octogenarians and nonagenarians had an increased risk of other ERCP-related adverse events. Nonagenarians were, in particular, at higher risk of bleeding and cardiopulmonary adverse events, and the risk of mortality rose steeply after the age of 80 when compared with younger patients. Our data on the risk of performing ERCP in older patients, specifically in very elderly patients, should be integrated into the discussions that we have with our patients and their families, including the informed consent process, as well as into decision algorithms with regard to the utility of performing an ERCP.
Funding
This work was supported by a grant from the National Cancer Institute K23 CA157929 (MS).
Note
Lukejohn Day (conception and design; analysis and interpretation of data for the article; critical revision of the article for important intellectual content; final approval of the article).
Lisa Lin (analysis and interpretation of data for the article; critical revision of the article for important intellectual content; final approval of the article).
Ma Somsouk (conception and design; analysis and interpretation of data for the article; critical revision of the article for important intellectual content; final approval of the article).
Competing interests: None
Lukejohn W. Day, MD and Lisa Lin, MD are the first authors.
References
- 1.CDC Trends in aging: United states and worldwide MMWR; 2003. Accessed on August 1, 2013 at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5206a2.htm [PubMed]
- 2.Baron T H, Mallery J S, Hirota W K. et al. The role of endoscopy in the evaluation and treatment of patients with pancreaticobiliary malignancy. Gastrointest Endosc. 2003;58:643–649. doi: 10.1016/s0016-5107(03)01994-1. [DOI] [PubMed] [Google Scholar]
- 3.Costamagna G Shah S K Tringali A Current management of postoperative complications and benign biliary strictures Gastrointest Endosc Clin N Am 200313635–648.ix ix [DOI] [PubMed] [Google Scholar]
- 4.Harness J K, Strodel W E, Talsma S E. Symptomatic biliary tract disease in the elderly patient. Am Surg. 1986;52:442–445. [PubMed] [Google Scholar]
- 5.Lukens F J, Howell D A, Upender S. et al. ERCP in the very elderly: outcomes among patients older than eighty. Dig Dis Sci. 2010;55:847–851. doi: 10.1007/s10620-009-0784-6. [DOI] [PubMed] [Google Scholar]
- 6.Siegel J H, Kasmin F E. Biliary tract diseases in the elderly: management and outcomes. Gut. 1997;41:433–435. doi: 10.1136/gut.41.4.433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Andriulli A, Loperfido S, Napolitano G. et al. Incidence rates of post-ERCP complications: a systematic survey of prospective studies. Am J Gastroenterol. 2007;102:1781–1788. doi: 10.1111/j.1572-0241.2007.01279.x. [DOI] [PubMed] [Google Scholar]
- 8.Freeman M L Nelson D B Sherman S et al. Complications of endoscopic biliary sphincterotomy N Engl J Med 1996335909–918.PubMed [DOI] [PubMed] [Google Scholar]
- 9.Anderson M A, Fisher L, Jain R. et al. Complications of ERCP. Gastrointest Endosc. 2012;75:467–473. doi: 10.1016/j.gie.2011.07.010. [DOI] [PubMed] [Google Scholar]
- 10.Ali M Ward G Staley D et al. A retrospective study of the safety and efficacy of ERCP in octogenarians Dig Dis Sci 201156586–590.PubMed [DOI] [PubMed] [Google Scholar]
- 11.Aparicio D PS, Sakai C M, Bueno T. et al. Analysis of the role of endoscopic retrograde cholangiopancreatography (ERCP) as a therapeutic method for the elderly. Gastrenterologia Endoscopia Digestiva. 2007;26:31–35. [Google Scholar]
- 12.Ashton C E, McNabb W R, Wilkinson M L. et al. Endoscopic retrograde cholangiopancreatography in elderly patients. Age Ageing. 1998;27:683–688. doi: 10.1093/ageing/27.6.683. [DOI] [PubMed] [Google Scholar]
- 13.Avila-Funes J A, Montaño-Loza A, Zepeda-Gómez S. et al. Endoscopic retrograde cholangiopancreatography in the elderly. Rev Invest Clin. 2005;57:666–670. [PubMed] [Google Scholar]
- 14.Chong V H, Yim H B, Lim C C. Endoscopic retrograde cholangiopancreatography in the elderly: outcomes, safety and complications. Singapore Med J. 2005;46:621–626. [PubMed] [Google Scholar]
- 15.Fritz E, Kirchgatterer A, Hubner D. et al. ERCP is safe and effective in patients 80 years of age and older compared with younger patients. Gastrointest Endosc. 2006;64:899–905. doi: 10.1016/j.gie.2006.05.010. [DOI] [PubMed] [Google Scholar]
- 16.Hammerle C W, Chung M J, Pandey A. et al. Complications of therapeutic endoscopic retrograde cholangiopancreatography in the elderly: A prospective analysis. Gastrointest Endosc. 2010;71:AB162–AB163. [Google Scholar]
- 17.Hisai H, Tanaka I, Abe S. et al. Efficacy and safety of ERCP procedures in patients 90 years of age and older. J Gastroenterol Hepatol. 2010;25:A62–A63. [Google Scholar]
- 18.Hu K C, Chu C H, Shih S C. et al. Safety and efficacy of endoscopic retrograde cholangiopancreatography in patients 85 years of age and older. Journal of Internal Medicine of Taiwan. 2006;17:233–239. [Google Scholar]
- 19.Hu K C Chang W H Chu C H et al. Findings and risk factors of early mortality of endoscopic retrograde cholangiopancreatography in different cohorts of elderly patients J Am Geriatr Soc 2009571839–1843.PubMed [DOI] [PubMed] [Google Scholar]
- 20.Katsinelos P, Paroutoglou G, Kountouras J. et al. Efficacy and safety of therapeutic ERCP in patients 90 years of age and older. Gastrointest Endosc. 2006;63:417–423. doi: 10.1016/j.gie.2005.09.051. [DOI] [PubMed] [Google Scholar]
- 21.Kim J E, Cha B H, Lee S H. et al. [Safety and efficacy of endoscopic retrograde cholangiopancreatograpy in very elderly patients] Korean J Gastroenterol. 2011;57:237–242. doi: 10.4166/2011.57.4.237. [DOI] [PubMed] [Google Scholar]
- 22.Köklü S, Parlak E, Yüksel O. et al. Endoscopic retrograde cholangiopancreatography in the elderly: a prospective and comparative study. Age Ageing. 2005;34:572–577. doi: 10.1093/ageing/afi180. [DOI] [PubMed] [Google Scholar]
- 23.MacMahon M, Walsh T N, Brennan P. et al. Endoscopic retrograde cholangiopancreatography in the elderly: a single unit audit. Gerontology. 1993;39:28–32. doi: 10.1159/000213511. [DOI] [PubMed] [Google Scholar]
- 24.Mitchell R M, O’Connor F, Dickey W. Endoscopic retrograde cholangiopancreatography is safe and effective in patients 90 years of age and older. J Clin Gastroenterol. 2003;36:72–74. doi: 10.1097/00004836-200301000-00019. [DOI] [PubMed] [Google Scholar]
- 25.Obana T, Fujita N, Noda Y. et al. Efficacy and safety of therapeutic ERCP for the elderly with choledocholithiasis: comparison with younger patients. Intern Med. 2010;49:1935–1941. doi: 10.2169/internalmedicine.49.3660. [DOI] [PubMed] [Google Scholar]
- 26.Riphaus A, Stergiou N, Wehrmann T. ERCP in octogenerians: a safe and efficient investigation. Age Ageing. 2008;37:595–599. doi: 10.1093/ageing/afn119. [DOI] [PubMed] [Google Scholar]
- 27.Rodríguez-González F J, Naranjo-Rodríguez A, Mata-Tapia I. et al. ERCP in patients 90 years of age and older. Gastrointest Endosc. 2003;58:220–225. doi: 10.1067/mge.2003.363. [DOI] [PubMed] [Google Scholar]
- 28.Talar-Wojnarowska R, Szulc G, Woźniak B. et al. Assessment of frequency and safety of endoscopic retrograde cholangiopancreatography in patients over 80 years of age. Pol Arch Med Wewn. 2009;119:136–140. [PubMed] [Google Scholar]
- 29.Zuckerman M Garcia C Lopez O et al. ERCP in the elderly J Gastroenterol Hepatol 2011263621175791 [Google Scholar]
- 30.Cotton P B, Lehman G, Vennes J. et al. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383–393. doi: 10.1016/s0016-5107(91)70740-2. [DOI] [PubMed] [Google Scholar]
- 31.Bickerstaff K I, Berry A R, Chapman R W. et al. Endoscopic sphincterotomy for the palliation of ampullary carcinoma. Br J Surg. 1990;77:160–162. doi: 10.1002/bjs.1800770215. [DOI] [PubMed] [Google Scholar]
- 32.Boytchev I, Pelletier G, Prat F. et al. [Late biliary complications after endoscopic sphincterotomy for common bile duct stones in patients older than 65 years of age with gallbladder in situ] Gastroenterol Clin Biol. 2000;24:995–1000. [PubMed] [Google Scholar]
- 33.Cappell M S. Endoscopic retrograde cholangiopancreatography with endoscopic sphincterotomy for symptomatic choledocholithiasis after recent myocardial infarction. Am J Gastroenterol. 1996;91:1827–1831. [PubMed] [Google Scholar]
- 34.Croker J R, Williams S G, Charlton M. et al. Endoscopic therapy for bile duct stones in a geriatric population. Postgrad Med J. 1992;68:457–460. doi: 10.1136/pgmj.68.800.457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lee T H, Han J H, Kim H J. et al. Is the addition of choleretic agents in multiple double-pigtail biliary stents effective for difficult common bile duct stones in elderly patients? A prospective, multicenter study. Gastrointest Endosc. 2011;74:96–102. doi: 10.1016/j.gie.2011.03.005. [DOI] [PubMed] [Google Scholar]
- 36.Arthur J D, Edwards P R, Chagla L S. Management of gallstone disease in the elderly. Ann R Coll Surg Engl. 2003;85:91–96. doi: 10.1308/003588403321219849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Riphaus A, Stergiou N, Wehrmann T. Sedation with propofol for routine ERCP in high-risk octogenarians: a randomized, controlled study. Am J Gastroenterol. 2005;100:1957–1963. doi: 10.1111/j.1572-0241.2005.41672.x. [DOI] [PubMed] [Google Scholar]
- 38.Scapa E, Berant A, Leibovitz A. et al. Endoscopic retrograde cholangiopancreatography in octogenarians. J Clin Gastroenterol. 1996;22:21–22. doi: 10.1097/00004836-199601000-00006. [DOI] [PubMed] [Google Scholar]
- 39.Testoni P A, Giussani A, Vailati C. et al. Precut sphincterotomy, repeated cannulation and post-ERCP pancreatitis in patients with bile duct stone disease. Dig Liver Dis. 2011;43:792–796. doi: 10.1016/j.dld.2011.05.010. [DOI] [PubMed] [Google Scholar]
- 40.Tobal D, Tobal F. Endoscopy in the elderly. Findings justify risks? Gastrointest Endosc. 2010;71:AB216. [Google Scholar]
- 41.Wang X F, Zhou X P, Li S G. et al. Rational therapy for elderly patients aged over 80 with acute obstructive suppurative cholangitis. World Chin J Digestology. 2008;16:3005–3008. [Google Scholar]
- 42.Garcia-Cano Lizcano J, Gonzalez Martin J A, Taberna Arana L. et al. [Therapeutic biliary endoscopy in patients over 90 years of age] Med Interna. 2002;19:409–411. [PubMed] [Google Scholar]
- 43.Grönroos J M, Salminen P, Laine S. et al. Feasibility of ERCP procedures in patients 90 years of age and older. J Clin Gastroenterol. 2010;44:227–228. doi: 10.1097/MCG.0b013e3181b3830f. [DOI] [PubMed] [Google Scholar]
- 44.Horiuchi A, Nakayama Y, Tanaka N. et al. Propofol sedation for endoscopic procedures in patients 90 years of age and older. Digestion. 2008;78:20–23. doi: 10.1159/000151765. [DOI] [PubMed] [Google Scholar]
- 45.Huguet J M, Sempere J, Bort I. et al. [Complications of endoscopic retrograde cholangiopancreatography in patients aged more than 90 years old] Gastroenterol Hepatol. 2005;28:263–266. doi: 10.1157/13074059. [DOI] [PubMed] [Google Scholar]
- 46.Salminen P, Grönroos J M. Anesthesiologist assistance in endoscopic retrograde cholangiopancreatography procedures in the elderly: is it worthwhile? J Laparoendosc Adv Surg Tech A. 2011;21:517–519. doi: 10.1089/lap.2010.0527. [DOI] [PubMed] [Google Scholar]
- 47.Vracko J, Markovic S, Wiechel K L. Conservative treatment versus endoscopic sphincterotomy in the initial management of acute cholecystitis in elderly patients at high surgical risk. Endoscopy. 2006;38:773–778. doi: 10.1055/s-2006-925448. [DOI] [PubMed] [Google Scholar]
- 48.Cocking J B, Ferguson A, Mukherjee S K. et al. Short-acting general anaesthesia facilitates therapeutic ERCP in frail elderly patients with benign extra-hepatic biliary disease. Eur J Gastroenterol Hepatol. 2000;12:451–454. doi: 10.1097/00042737-200012040-00014. [DOI] [PubMed] [Google Scholar]
- 49.Thomopoulos K C, Vagenas K, Assimakopoulos S F. et al. Endoscopic retrogade cholangiopancreatography is safe and effective method for diagnosis and treatment of biliary and pancreatic disorders in octogenarians. Acta Gastroenterol Belg. 2007;70:199–202. [PubMed] [Google Scholar]
- 50.Grönroos J M. Clinical success of ERCP procedures in nonagenarian patients with bile duct stones. Minim Invasive Ther Allied Technol. 2011;20:146–149. doi: 10.3109/13645706.2010.530825. [DOI] [PubMed] [Google Scholar]
- 51.Akkiz H, Akinoglu A, Colakoglu S. et al. Endoscopic management of biliary hydatid disease. Can J Surg. 1996;39:287–292. [PMC free article] [PubMed] [Google Scholar]
- 52.Alderson D, Lavelle M I, Venables C W. Endoscopic sphincterotomy before pancreaticoduodenectomy for ampullary carcinoma. Br Med J (Clin Res Ed) 1981;282:1109–1111. doi: 10.1136/bmj.282.6270.1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bajaj J S, Spinelli K S, Dua K S. Postoperative management of noniatrogenic traumatic bile duct injuries: role of endoscopic retrograde cholangiopancreaticography. Surg Endosc. 2006;20:974–977. doi: 10.1007/s00464-005-0472-3. [DOI] [PubMed] [Google Scholar]
- 54.Cheon Y K, Cho K B, Watkins J L. et al. Frequency and severity of post-ERCP pancreatitis correlated with extent of pancreatic ductal opacification. Gastrointest Endosc. 2007;65:385–393. doi: 10.1016/j.gie.2006.10.021. [DOI] [PubMed] [Google Scholar]
- 55.Chow S, Bosco J J, Heiss F W. et al. Successful treatment of post-cholecystectomy bile leaks using nasobiliary tube drainage and sphincterotomy. Am J Gastroenterol. 1997;92:1839–1843. [PubMed] [Google Scholar]
- 56.Cotton P B, Garrow D A, Gallagher J. et al. Risk factors for complications after ERCP: a multivariate analysis of 11,497 procedures over 12 years. Gastrointest Endosc. 2009;70:80–88. doi: 10.1016/j.gie.2008.10.039. [DOI] [PubMed] [Google Scholar]
- 57.Davidson B R, Neoptolemos J P, Carr-Locke D L. Endoscopic sphincterotomy for common bile duct calculi in patients with gall bladder in situ considered unfit for surgery. Gut. 1988;29:114–120. doi: 10.1136/gut.29.1.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Deans G T, Sedman P, Martin D F. et al. Are complications of endoscopic sphincterotomy age related? Gut. 1997;41:545–548. doi: 10.1136/gut.41.4.545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Elmi F, Silverman W B. Outcome of ERCP in the management of duct-to-duct anastomotic strictures in orthotopic liver transplant. Dig Dis Sci. 2007;52:2346–2350. doi: 10.1007/s10620-006-9142-0. [DOI] [PubMed] [Google Scholar]
- 60.England R E, Martin D F. Endoscopic management of Mirizzi’s syndrome. Gut. 1997;40:272–276. doi: 10.1136/gut.40.2.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Fisher L, Fisher A, Thomson A. Cardiopulmonary complications of ERCP in older patients. Gastrointest Endosc. 2006;63:948–955. doi: 10.1016/j.gie.2005.09.020. [DOI] [PubMed] [Google Scholar]
- 62.Güitrón-Cantú A, Adalid-Martínez R, Gutiérrez-Bermúdez J A. et al. [In Process Citation] Rev Gastroenterol Mex. 2010;75:267–272. [PubMed] [Google Scholar]
- 63.Iles-Shih L, Hilden K, Adler D G. Combined ERCP and EUS in one session is safe in elderly patients when compared to non-elderly patients: outcomes in 206 combined procedures. Dig Dis Sci. 2012;57:1949–1953. doi: 10.1007/s10620-012-2135-2. [DOI] [PubMed] [Google Scholar]
- 64.Itoi T, Ishii K, Itokawa F. et al. Large balloon papillary dilation for removal of bile duct stones in patients who have undergone a billroth ii gastrectomy. Dig Endosc. 2010;22:S98–S102. doi: 10.1111/j.1443-1661.2010.00955.x. [DOI] [PubMed] [Google Scholar]
- 65.Kim H J, Choi H S, Park J H. et al. Factors influencing the technical difficulty of endoscopic clearance of bile duct stones. Gastrointest Endosc. 2007;66:1154–1160. doi: 10.1016/j.gie.2007.04.033. [DOI] [PubMed] [Google Scholar]
- 66.Kogure H, Tsujino T, Yagioka H. et al. Self-expandable metallic stents for malignant biliary obstruction with an anomalous pancreaticobiliary junction. Surg Endosc. 2008;22:787–791. doi: 10.1007/s00464-007-9482-7. [DOI] [PubMed] [Google Scholar]
- 67.May G R, Cotton P B, Edmunds S E. et al. Removal of stones from the bile duct at ERCP without sphincterotomy. Gastrointest Endosc. 1993;39:749–754. doi: 10.1016/s0016-5107(93)70258-8. [DOI] [PubMed] [Google Scholar]
- 68.Morelli J, Mulcahy H E, Willner I R. et al. Long-term outcomes for patients with post-liver transplant anastomotic biliary strictures treated by endoscopic stent placement. Gastrointest Endosc. 2003;58:374–379. doi: 10.1067/s0016-5107(03)00011-7. [DOI] [PubMed] [Google Scholar]
- 69.Nojkov B, Cappell M S. Safety and efficacy of ERCP after recent myocardial infarction or unstable angina. Gastrointest Endosc. 2010;72:870–880. doi: 10.1016/j.gie.2010.06.024. [DOI] [PubMed] [Google Scholar]
- 70.Paik W H, Park Y S, Hwang J H. et al. Palliative treatment with self-expandable metallic stents in patients with advanced type III or IV hilar cholangiocarcinoma: a percutaneous versus endoscopic approach. Gastrointest Endosc. 2009;69:55–62. doi: 10.1016/j.gie.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 71.Sharara A I, El Hajj I I, Mroueh M. et al. Prophylaxis with ertapenem in patients with obstructive jaundice undergoing endoscopic retrograde cholangiopancreatography: safety, efficacy, and biliary penetration. South Med J. 2011;104:189–194. doi: 10.1097/SMJ.0b013e318205de10. [DOI] [PubMed] [Google Scholar]
- 72.Sherman S, Shaked A, Cryer H M. et al. Endoscopic management of biliary fistulas complicating liver transplantation and other hepatobiliary operations. Ann Surg. 1993;218:167–175. doi: 10.1097/00000658-199308000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Sutton V R, Hong M K, Thomas P R. Using the 4-hour Post-ERCP amylase level to predict post-ERCP pancreatitis. JOP. 2011;12:372–376. [PubMed] [Google Scholar]
- 74.Vaira D, D’Anna L, Ainley C. et al. Endoscopic sphincterotomy in 1000 consecutive patients. Lancet. 1989;2:431–434. doi: 10.1016/s0140-6736(89)90602-8. [DOI] [PubMed] [Google Scholar]
- 75.Varadarajulu S, Eloubeidi M A, Wilcox C M. Prospective evaluation of indeterminate ERCP findings by intraductal ultrasound. J Gastroenterol Hepatol. 2007;22:2086–2092. doi: 10.1111/j.1440-1746.2006.04823.x. [DOI] [PubMed] [Google Scholar]
- 76.Kouklakis G, Gatopoulou A, Lirantzopoulos N. et al. Evaluation of guide wire cannulation technique in elderly patients with choledocholithiasis. J Gastrointestin Liver Dis. 2009;18:185–188. [PubMed] [Google Scholar]
- 77.Murata A, Motomura Y, Akahoshi K. et al. Therapeutic ERCP for choledocholithiasis in patients 80 years of age and older. J Clin Gastroenterol. 2009;43:289–290. doi: 10.1097/MCG.0b013e318165dc94. [DOI] [PubMed] [Google Scholar]
- 78.Pisello F, Geraci G, Li Volsi F. et al. Permanent stenting in “unextractable” common bile duct stones in high risk patients. A prospective randomized study comparing two different stents. Langenbecks Arch Surg. 2008;393:857–863. doi: 10.1007/s00423-008-0388-1. [DOI] [PubMed] [Google Scholar]
- 79.Straja D, Daha C, Simion L. [Endoscopic sphincterotomy in the treatment of common bile duct benign lesions (experience with 100 cases)] Chirurgia (Bucur) 2001;96:521–526. [PubMed] [Google Scholar]
- 80.Thomas P R, Sengupta S. Prediction of pancreatitis following endoscopic retrograde cholangiopancreatography by the 4-h post procedure amylase level. J Gastroenterol Hepatol. 2001;16:923–926. doi: 10.1046/j.1440-1746.2001.02547.x. [DOI] [PubMed] [Google Scholar]
- 81.Sugiyama M, Atomi Y. Endoscopic sphincterotomy for bile duct stones in patients 90 years of age and older. Gastrointest Endosc. 2000;52:187–191. doi: 10.1067/mge.2000.107285. [DOI] [PubMed] [Google Scholar]
- 82.Hui C K, Liu C L, Lai K C. et al. Outcome of emergency ERCP for acute cholangitis in patients 90 years of age and older. Aliment Pharmacol Ther. 2004;19:1153–1158. doi: 10.1111/j.1365-2036.2004.01962.x. [DOI] [PubMed] [Google Scholar]
- 83.Siegel J H. Duodenoscopic sphincterotomy in the treatment of the “sump syndrome”. Dig Dis Sci. 1981;26:922–928. doi: 10.1007/BF01309498. [DOI] [PubMed] [Google Scholar]
- 84.Yancik R. Cancer burden in the aged: an epidemiologic and demographic overview. Cancer. 1997;80:1273–1283. [PubMed] [Google Scholar]
- 85.Fulton M M, Allen E R. Polypharmacy in the elderly: a literature review. J Am Acad Nurse Pract. 2005;17:123–132. doi: 10.1111/j.1041-2972.2005.0020.x. [DOI] [PubMed] [Google Scholar]
- 86.Masci E, Toti G, Mariani A. et al. Complications of diagnostic and therapeutic ERCP: a prospective multicenter study. Am J Gastroenterol. 2001;96:417–423. doi: 10.1111/j.1572-0241.2001.03594.x. [DOI] [PubMed] [Google Scholar]
- 87.Freeman M L, DiSario J A, Nelson D B. et al. Risk factors for post-ERCP pancreatitis: a prospective, multicenter study. Gastrointest Endosc. 2001;54:425–434. doi: 10.1067/mge.2001.117550. [DOI] [PubMed] [Google Scholar]
- 88.Freeman M L. Adverse outcomes of endoscopic retrograde cholangiopancreatography. Rev Gastroenterol Disord. 2002;2:147–168. [PubMed] [Google Scholar]
- 89.Cheng C L, Sherman S, Watkins J L. et al. Risk factors for post-ERCP pancreatitis: a prospective multicenter study. Am J Gastroenterol. 2006;101:139–147. doi: 10.1111/j.1572-0241.2006.00380.x. [DOI] [PubMed] [Google Scholar]
- 90.Guiding principles for the care of older adults with multimorbidity: an approach for clinicians. Guiding principles for the care of older adults with multimorbidity: an approach for clinicians: American Geriatrics Society Expert Panel on the Care of Older Adults with Multimorbidity. J Am Geriatr Soc. 2012;60:E1–E25. doi: 10.1111/j.1532-5415.2012.04188.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Uijen A A, van de Lisdonk E H. Multimorbidity in primary care: prevalence and trend over the last 20 years. Eur J Gen Pract. 2008;14 01:28–32. doi: 10.1080/13814780802436093. [DOI] [PubMed] [Google Scholar]
- 92.Hajjar E R, Cafiero A C, Hanlon J T. Polypharmacy in elderly patients. Am J Geriatr Pharmacother. 2007;5:345–351. doi: 10.1016/j.amjopharm.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 93.Clegg A, Young J, Iliffe S. et al. Frailty in elderly people. Lancet. 2013;381:752–762. doi: 10.1016/S0140-6736(12)62167-9. [DOI] [PMC free article] [PubMed] [Google Scholar]


