Abstract
Background and aims: Patient’s posture change is commonly employed by a colonoscopist to achieve complete examination. We studied whether patient’s posture (left-lateral decubitus vs supine) influenced the success rate of ileal intubation.
Patients and methods: In this prospective open-label randomized study performed in the Endoscopy Suite of a tertiary-care center, all adult outpatients referred for colonoscopy, in whom cecal intubation was achieved and who satisfied predefined inclusion criteria, were randomized to undergo ileal intubation in either of the above two postures. Colonoscopy (EC-201 WL, Fujinon) was performed after overnight poly-ethylene-glycol preparation, under conscious sedation and continuous pulse-oxymetry monitoring. After confirming cecal intubation, patients were randomized for ileal intubation. Success was defined by visualization of ileal mucosa or villi (confirmed by digital photography) and was attempted until limited by pain and/or time of ≥ 6 min.
Results: Of 320 eligible patients, 217 patients (150 males) were randomized, 106 to left-lateral decubitus and 111 to supine posture. At baseline, the two groups were evenly matched. Successful ileal intubation was achieved in 145 (66.8 %) patients overall, significantly higher in the supine posture (74.8 % versus 58.5 %; P = 0.014). On multivariate analysis, supine posture (P = 0.02), average/good right-colon preparation (P < 0.01), non-thin-lipped ileocecal (IC) valve (P < 0.001) and younger age (P = 0.02) were independent predictors of success. Positive ileal findings were recorded in 13 (9 %) patients.
Conclusion: Ileoscopy is more successful in supine than in left-lateral decubitus posture. Age, bowel preparation and type of IC valve also determine success.
Introduction
Since its introduction into clinical practice in the late 1960 s, colonoscopy has now become a standard procedure 1 2. After the initial report of successful ileal intubation during colonoscopy, 3 ileoscopy is often recommended by some in unselected patients undergoing colonoscopy 4 or at least in those patients presenting with diarrhea or suspected Inflammatory Bowel Disease (IBD) or intestinal tuberculosis (ITB) 5 6 7 8 9 10. In addition, identification of the ileocecal (IC) valve and ileal mucosa documents completeness of full length colonoscopy 11 12.
However, various difficulties are encountered during ileoscopy. The IC valve may be difficult to locate when it is hidden behind large semilunar folds or if excess air is insufflated with stretching of the lumen or if the valve is papillary in form and flush with the wall 1 13. In various studies, the success of ileoscopy, without any special maneuvers, varies from 77.8 % to 81.3 %, with a time required to insert the scope into the ileum of, on average, 3.4 min (range: 30 s to 10 min) 14 15 16. Despite this, with various endoscopic maneuvers, it is possible to successfully intubate the terminal ileum in a significant number of patients 16.
During colonoscopy, the endoscopist employs various maneuvers, including changing the patient’s posture, to achieve complete colonoscopic examination 1 13 16. If one position fails, another is attempted. Posture change has also been reported to increase the success rate of ileal intubation, with the supine posture often bringing the IC valve to a 6 – 7 o’clock position (Fig. 1) 16 17. However, there has been no randomized trial which has shown that a particular posture of the patient increases the success rate of ileoscopy.
Fig. 1.
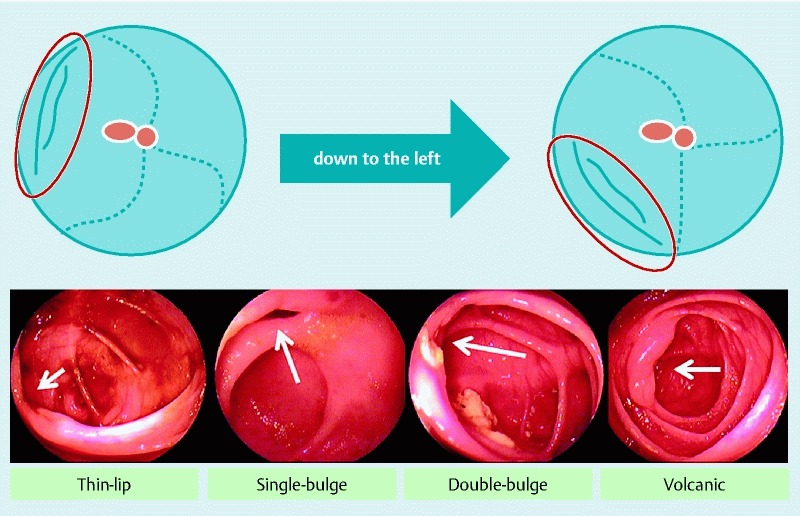
Upper panel shows the “down to left” position taken by the IC valve when shifting the patient’s posture from left-lateral decubitus to supine. Lower panel shows the four types of IC valve.
The present study was performed to determine the impact of the patient’s posture (left lateral vs supine position) on the success rate of ileal intubation. In addition, we also assessed the yield (clinically relevant positive findings) of ileal intubation and the predictors of successful terminal ileal intubation.
Patients and Methods
Study Design
All outpatients (> 12 years old) referred for colonoscopy between June and December 2010 were eligible for entry into the study provided they did not have the following conditions: 1) acute fulminant colitis; 2) acute intestinal obstruction; 3) suspected intestinal perforation; 4) peritonitis; 5) pregnancy; 6) severe cardio-respiratory disease (ASA grade > II); 7) decompensated liver disease; 8) recent pelvic or colonic surgery (in the last 6 months); 9) large aortic or iliac artery aneurysm; 10) Human Immunodeficiency Virus (HIV) infection; and 11) were non-consenting.
Colonoscopy was performed in the Endoscopy Suite of the School of Digestive and Liver Diseases (SDLD), IPGME & R, Kolkata, a tertiary referral-cum-teaching hospital with a videocolonoscope (EC-201 WL, Fujinon) by endoscopists with different skill levels, including third-year gastroenterology trainees and departmental consultants, under conscious sedation with titrated intravenous midazolam (dose: 0.05 – 0.1 mg/kg) while the patients were monitored by continuous pulse oxymetry (Draco-oxy Biptronics Plethysmogram).
Randomization
In this randomized, open-label study, patients were randomized to undergo ileal intubation, either in the left-lateral decubitus (LL) or supine (S) posture, after the cecum had been successfully intubated by a 1:1 randomization (equal proportions) by the sealed envelope method. An independent statistician generated random numbers on a computer using SPSS 13.0 for Windows (SPSS Inc, Chicago, Ill). He prepared hundreds of sealed envelopes containing random numbers for allocation, which had equal odd – even proportions. An odd number allocated the patient to the LL posture group and an even number to the S posture group. An assistant nurse opened the envelopes just after completion of cecal intubation at colonoscopy.
Sample-size calculation
This was done with the free software G*Power 3.0.10 (Universität Kiel, Germany). Based on the literature, the reported success of ileoscopy without any maneuver was taken to be ~ 80 %. 14 15 16 Expecting at least a 15 % increase in success at ileal intubation after changing the patient’s posture to supine, the sample size required using Fisher’s exact 2-sided test to detect a statistically significant difference (α-error probability = 0.05) was 216 (108 in each group) with 90 % power (β-error = 0.1).
Procedure
Colonoscopy and preparation
Patients were advised to take clear liquid on the night prior to colonoscopy. Bowel preparation was done by taking two tablets of Bisacodyl (Tablet Dalculax 10 mg) at bedtime on the night before colonoscopy and a standard poly-ethylene glycol (PEG) preparation (containing 118.0 g PEG, 2.93 g sodium chloride, 1.48 g potassium chloride, 3.37 g sodium bicarbonate, 11.3 g anhydrous bicarbonate; ColopegTM, J.B. Chemicals & Pharmaceuticals Ltd, India) in the early morning on the day of colonoscopy. Adequacy of bowel preparation was assessed by the validated Boston Bowel Preparation Scale (BBPS or “bee-bops”) 18.
Colonoscopy was started in the LL posture. The endoscopist was allowed to apply all maneuvers to successfully intubate the cecum, which was confirmed by standard landmarks, i. e., appendicular orifice, IC valve and transillumination 11. The shape (Fig. 1) and position of the IC valve were recorded.
Ileoscopy and randomization
After confirmation of cecal intubation and with the scope shortened and de-looped, patients were randomized to either the LL or S position if they satisfied the predefined inclusion criteria. Then terminal ileal intubation was attempted. Partial suction and scope maneuvers for ileal intubation were allowed 13. Use of anti-peristalsis agents, biopsy forceps (as an “anchor” to facilitate IC valve intubation), and intubation in the retroflexed position were not allowed. If the ileum was not intubated within 6 min, 19 it was considered a failure and the study end point was reached. Further attempts at ileoscopy were at the discretion of the endoscopist.
Outcome measures
The primary outcome was whether ileal intubation was achieved or not within the stipulated 6 min. The other outcomes that were recorded were: 1) time taken to intubate the ileum; 2) depth of ileal intubation; and 3) presence or absence of ileal pathology.
Successful ileal intubation was defined as visualization of the ileal mucosa or villi (confirmed by digital photography). 20 Time to ileal intubation was calculated from the first attempts, after randomization, until visualization of the ileal mucosa, and was limited by pain or time ≤ 6 min.19 After ileal intubation, ileal exploration was performed with minimal air insufflation and was limited by pain and/or length of the colonoscope. Depth of ileoscopy was calculated at the time of withdrawal of the scope, from the furthest point reached in the ileum to the IC valve. Any abnormal finding was recorded and biopsies were taken, if deemed necessary, by the performing endoscopist.
Patient tolerability of ileoscopy was rated by a three-point score: 0, no pain; 1, pain not limiting the procedure; 2, pain limiting the procedure 19. All adverse events were recorded including hypoxia, tachy- and/or bradycardia.
Ethical clearance and statistical analysis
Each patient’s data were meticulously recorded by one of the investigators (MA) in a structured proforma. Written informed consent about the study protocol was taken from each patient before colonoscopy and the study was approved by the Institutional Ethics Committee (IEC).
All statistical analyses were performed on an intention-to-treat basis. Mean, median, standard deviation (SD), standard error of the mean (SEM), range and proportions were calculated, as appropriate. Categorical variables were analyzed using the χ2 test with the Yates correction or Fisher’s exact test, as appropriate. Continuous variables were compared using the Student’s t-test. Multivariate analysis, to identify the predictors of successful ileal intubation, was done by binary logistic regression analysis using variables found to be significant on univariate analysis (P < 0.05). Statistical analysis was done using SPSSTM (Version 13 for Windows) software. A P-value of < 0.05 was considered to be statistically significant.
Results
Between June 1 and December 31, 2010, of the 653 patients referred for colonoscopy, 623 (95.4 %) had successful cecal intubation. Of the 653 patients, 320 (49 %) were eligible for inclusion (Fig. 2). Of these, 217 (67.8 %; 150 males), were randomized, 106 and 111 undergoing ileoscopy in the left-lateral decubitus and supine posture, respectively (Fig. 2: CONSORT Diagram).
Fig. 2.
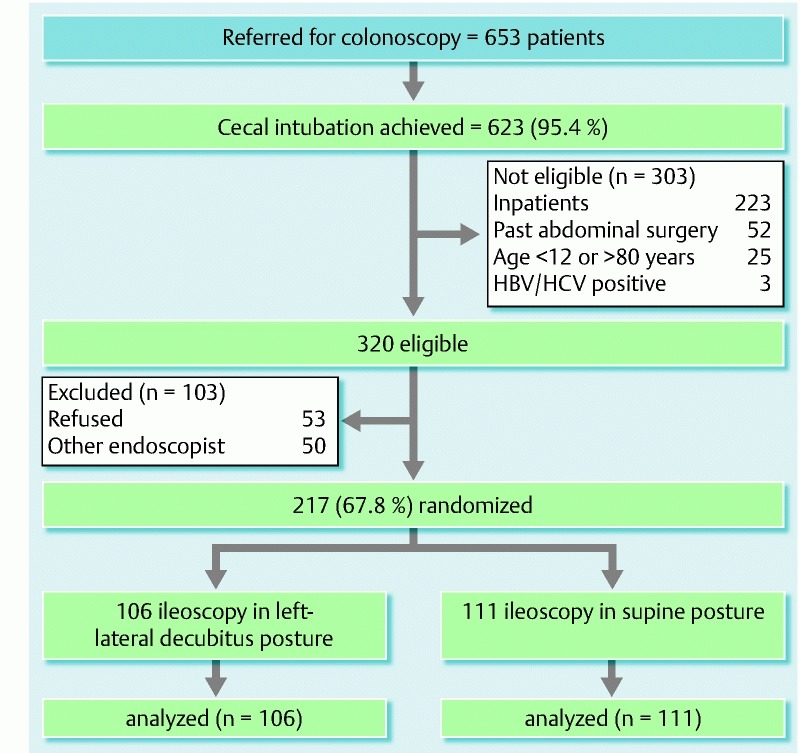
Flowchart of the study population.
At baseline (Table 1), the two groups were evenly matched with respect to demography, degree of colonic preparation, type of IC valve, indication for attempted colonoscopy, and the endoscopist performing the procedure. Endoscopist 1 (JD) was senior with > 15 years’ experience in colonoscopy doing > 70 ileoscopies per year. Endoscopist 2 (SB) and 3 (RS) had > 3 years’ experience in colonoscopy while endoscopist 4 (MA) had > 2 years’ experience in colonoscopy. Endoscopist 2, 3 and 4 had already done > 100 ileoscopies, more than twice the number regarded as necessary to achieve competence 19.
Table 1. Baseline characteristics of the two groups.
| Left lateral decubitus (n = 106) |
Supine (n = 111) |
P-value | |
| Age (mean ± SEM) | 40.7 ± 1.5 | 39.8 ± 1.4 | 0.7 |
| Male (%) | 69 | 69 | 1.0 |
| R-colon preparation (BBPS) [%] | 0.5 | ||
| Sub-optimal (score = 1) | 23 | 22 | |
| Average (score = 2) | 50 | 44 | |
| Good (score = 3) | 27 | 34 | |
| IC valve type (%) | 0.3 | ||
| Thin-lipped (n = 70) | 39 | 30 | |
| Single-bulged (n = 42) | 19 | 21 | |
| Double-bulged (n = 66) | 32 | 31 | |
| Volcanic (n = 31) | 10 | 18 | |
| Indication (%) | 0.3 | ||
| Bleeding P/R | 37 | 26 | |
| Diarrhea | 10 | 14 | |
| Anemia | 6 | 14 | |
| SAIO | 12 | 10 | |
| FBD | 12 | 13 | |
| Endoscopist (%) | 0.7 | ||
| No 1 | 13 | 9 | |
| No 2 | 27 | 24 | |
| No 3 | 14 | 15 | |
| No 4 | 46 | 52 |
P/R, per rectal; SAIO, subacute intestinal obstruction; FBD, functional bowel disorder AU: Please check that FBD has been defined correctly.
Overall, the primary end point, i. e., successful ileal intubation, was achieved in 145 of 217 (66.8 %) patients, significantly more often in the supine (74.8 %) versus the left-lateral decubitus (58.5 %) posture (P = 0.014). The predominant reason for failure in 69 patients was inability to intubate the ileum in the stipulated predetermined time of ≤ 6 min (n = 55, 80 %) alone or combined with poor right colon preparation (n = 9, 13 %).
Among the secondary outcomes (Table 2), the median time taken for ileal intubation was 74.0 s (range: 2 to 349 s) overall, with a longer time required in LL posture versus S posture, which did not achieve statistical significance. The mean (± SEM) depth of ileal intubation was 8.4 ± 0.3 cm overall, with no difference between the two groups. No major adverse event developed in any of the patients in the trial. Among the minor adverse events, there was no difference between the two groups with respect to pain, hypoxia and bradycardia. Only asymptomatic tachycardia was significantly more common in the supine posture ( Table 2).
Table 2. Secondary outcome measures in the two groups.
| Total | Left lateral decubitus (n = 106) |
Supine (n = 111) |
P-value | |
| Successful ileal intubation, n (%) | 145 (66.8) | 62 (58.5) | 83 (74.8) | 0.014 |
|
Depth of ileal intubation
(cm; mean ± SEM) |
8.4 ± 0.3 | 8.6 ± 0.4 | 8.2 ± 0.3 | 0.5 |
|
Time to ileal intubation
(s; median, range) |
74.0 (2 – 349) |
84.5 (2 – 310) |
71.0 (4 – 349) |
0.3 |
| Patient-perceived pain (%) | 0.3 | |||
| Nil | 93 | 90 | 95 | |
| Present, not limiting | 7 | 10 | 5 | |
| Adverse events (%) | ||||
| Hypoxia | 2 | 2 | 2 | 1.0 |
| Tachycardia | 16 | 9 | 22 | 0.015 |
| Bradycardia | 0.5 | 1.0 | 0 | 0.5 |
Clinically relevant findings were recorded in 13 (9 %) patients in whom successful ileoscopy was performed: a small bowel source of bleeding was confirmed in 2; ulcers ± nodularity ± strictures were seen in 8 patients (Tuberculosis 5; Crohn’s 1; Idiopathic 2); terminal ileal nodularity in 1 and polyp in another 1 patient.
On univariate analysis, in addition to supine posture, successful ileal intubation was more frequent in younger patients (mean ± SEM: 38.0 ± 1.2 vs 44.7 ± 1.9 years; P < 0.01), in those with better right-colon preparation (BBPS average and/or good vs suboptimal: 72 % vs 48 %; P < 0.01) and in those who did not have a thin-lipped IC valve (other types vs thin-lipped: 79 % vs 43 %; P < 0.0001). Sex, endoscopist and other factors were not significant in univariate analysis.
On multivariate analysis, age (OR 0.97; 95 % CI: 0.95 – 0.99), supine posture (OR 2.2; 95 % CI: 1.1 – 4.3), average and/or good BBPS of right colon (OR 4.1; 95 % CI: 1.9 – 8.9) and IC valve type that was not thin-lipped (OR 5.1; 95 % CI: 2.6 – 9.8) were independent predictors of successful ileal intubation (Table 3).
Table 3. Univariate and multivariate analysis of the factors associated with successful ileal intubation.
| Univariate | Multivariate | ||||
| Success (n = 145) |
Failure (n = 72) |
P-value | OR (95 % CI) |
P-value | |
| Age (mean ± SEM) | 38.0 ± 1.2 | 44.7 ± 1.9 | 0.002 | 0.97 (0.95 – 0.99) |
0.02 |
| Male (%) | 71 | 65 | 0.4 | ||
| R-colon preparation (BBPS) [%] | 0.007 | ||||
| Sub-optimal (score = 1) | 16 | 35 | 1 | ||
| Average/Good (score = 2 /3) | 84 | 65 | 4.1 (1.9 – 8.9) |
< 0.0001 | |
| Patient posture (%) | 0.014 | 0.02 | |||
| Left lateral | 43 | 61 | 1 | ||
| Supine | 57 | 39 | 2.2 (1.1 – 4.3) |
||
| IC valve type (%) | < 0.0001 | < 0.0001 | |||
| Thin-lipped | 22 | 58 | 1 | ||
| Others | 78 | 42 | 5.0 (2.6 – 9.8) |
||
| Indication (%) | 0.6 | ||||
| Bleeding P/R | 28 | 37 | |||
| Diarrhea | 13 | 10 | |||
| Anemia | 10 | 10 | |||
| SAIO | 12 | 8 | |||
| FBD | 12 | 12 | |||
| Endoscopist (%) | 0.2 | ||||
| No 1 | 9 | 15 | |||
| No 2 | 26 | 24 | |||
| No 3 | 17 | 8 | |||
| No 4 | 48 | 53 | |||
When analyzing the independent predictors of successful ileal intubation separately in the LL and S postures, by multivariate analysis, age, degree of right-colon preparation and type of IC-valve were significant independent predictors of ileal intubation in the LL posture, whereas the latter two alone were significant independent predictors of ileal intubation in the S posture (data not shown).
Discussion
This prospective randomized trial demonstrated that, within a predetermined stipulated time frame, ileal intubation is significantly more successful in the supine than in the left-lateral decubitus posture. Moreover, in addition to supine posture, younger age, better right colon preparation and type of IC valve (non-thin-lipped) are independent predictors of successful ileal intubation. The major strengths of our study are its prospective randomized nature, sample-size generation, blinded allocation and analysis, using predefined stringent criteria for success and failure and use of a well-validated bowel preparation score.
There have been very few studies about the technical feasibility of terminal ileoscopy during colonoscopy 14 16 17 with most of the studies predominantly focusing on the yield of ileoscopy and/or ileal biopsies 5 6 7 8 9 10 21 22 23 24. Most endoscopists intubate the terminal ileum in the left-lateral decubitus posture with the ileocecal valve in the 6 – 7 o’clock position, using downward deflection and anticlockwise torque while withdrawing from the cecal cone 16. Prospective studies have shown that the ileum is successfully intubated in this position in 65 – 78 % of patients, depending on the training level of endoscopists 16 19 25. Shifting the posture to supine, however, achieves an ileoscopy completion rate of > 95 %. 16 19 It is against this background that our trial conclusively demonstrates that the supine posture is technically the easier posture to intubate the terminal ileum, with a higher success rate.
While our analysis was ongoing, another randomized trial was published that showed that the prone posture is equivalent to the left-lateral decubitus posture with regard to the frequency of ileal intubation achieved, albeit within a shorter time 26. However, that trial did not stratify or analyze the confounding factors such as endoscopist, bowel preparation and IC valve morphology 26.
In addition to posture, we also found that age, degree of right-colon preparation and morphology of IC valve are independent predictors of ileal intubation success. Younger age was associated with increased success at ileal intubation overall, and especially in left lateral decubitus posture. Age was not an independent predictor of ileal intubation success in the supine posture. The quality of right-colon preparation was an independent predictor of success overall, as well as in both postures independently. This is to be expected as good bowel preparation is an important determinant of technical success in colonoscopy and in any colonoscopic procedure.
In compliance with a previous study, the morphology of the IC valve was an independent predictor of ileal intubation success. 19 The thin-lipped type of valve is difficult to intubate as it is less distensible and often flush with the semicircular fold of the cecum.
One drawback in our study was the lower rate of successful ileal intubation overall (~ 67 %). Although this was well within the range reported in the literature, the major reason (~ 80 %) for failure was the inability to intubate the ileum within the stipulated time frame of ≤ 6 min. We had stipulated a cut-off time of 6 min, in compliance with a previous study, and in addition, this is double the average time required to intubate the ileum according to the literature 19. Thus, in a prospective controlled trial setting with a time-pressure, the rate of success might be lower for complex visuo-spatio-psychomotor procedures such as colonoscopy and ileoscopy 27. Moreover, our population was predominantly male and had a higher prevalence of the difficult thin-lipped type of IC-valve vis-à-vis, the Italian population reported in the literature 20. This could also have contributed to the lower rate of success.
Reviewing the literature, we found two studies that prospectively assessed the technical success of ileoscopy during colonoscopy. In the first study, overall success was achieved in 79 %, with a longer time (mean: 3.4 min; range: 30 s to 10 min) and no difference between endoscopists having different levels of training 14. In the second study, ileoscopy, performed by a single colonoscopist, was achieved without any intervention in 77.8 %, which increased to ~ 97 % when changing the posture to supine and/or use of an anti-peristalsis agent (Hyoscine-n-butyl bromide) in one-fifth of patients, respectively 16. The median time taken for intubation was 55 s (range: 2 – 1140 s) 16, not much different from our rates. Moreover, we did not use any anti-peristalsis agent which is proven to facilitate ease of ileal intubation 28.
One of the biggest impediments to the technical success of colonoscopy is the result of “looping” in the tortuous and often redundant areas of the colon, especially the sigmoid and transverse colon 29 30 31. We speculate that the same should hold for ileoscopy, as it is difficult to intubate the terminal ileum if the colonoscope is not de-looped. Older age is one of the risk factors for increased looping, which is reflected in our study by the decreased success at ileoscopy in older age 31. Posture change is one of the maneuvers that successfully de-loops the colon, especially in the sigmoid and transverse colon 30. We speculate that this might be the reason for the increased success of ileoscopy in the supine vis-à-vis the left lateral decubitus posture.
In conclusion, this randomized controlled trial proves that ileal intubation is more successful in supine than left-lateral decubitus posture. Age, bowel preparation and type of IC valve also determine successful ileoscopy.
Footnotes
Competing interests: None
References
- 1.Williams C, Teague R. Colonoscopy. Gut. 1973;14:990–1003. doi: 10.1136/gut.14.12.990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cotton P B Williams C B(ed.)Colonoscopy and Flexible Sigmoidoscopy. Practical Gastrointestinal EndoscopyFifth edition.Oxford, UK: Blackwell Publishing Ltd; 200383–171. [Google Scholar]
- 3.Nagasako K, Yazawa C, Takemoto T. Biopsy of the terminal ileum. Gastrointest Endosc. 1972;19:7–10. doi: 10.1016/s0016-5107(72)73931-0. [DOI] [PubMed] [Google Scholar]
- 4.Baillie J. Oxford: Butterworth-Heinemann Ltd; 1992. Gastrointestinal Endoscopy, Basic Principles and Practice; pp. 79–80. [Google Scholar]
- 5.Bhasin D K, Goenka M K, Dhavan S. et al. Diagnostic value of ileoscopy: a report from India. J Clin Gastroenterol. 2000;31:144–146. doi: 10.1097/00004836-200009000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Geboes K, Ectors N, D’Haens G. et al. Is ileoscopy with biopsy worthwhile in patients presenting with symptoms of inflammatory bowel disease? Am J Gastroenterol. 1998;93:201–206. doi: 10.1111/j.1572-0241.1998.00201.x. [DOI] [PubMed] [Google Scholar]
- 7.Morini S, Lorenzetti R, Stella F. et al. Retrograde ileoscopy in chronic nonbloody diarrhea: a prospective, case-control study. Am J Gastroenterol. 2003;98:1512–1515. doi: 10.1111/j.1572-0241.2003.07523.x. [DOI] [PubMed] [Google Scholar]
- 8.Jeong S H, Lee K J, Kim Y B. et al. Diagnostic value of terminal ileum intubation during colonoscopy. J Gastroenterol Hepatol. 2008;23:51–55. doi: 10.1111/j.1440-1746.2007.05151.x. [DOI] [PubMed] [Google Scholar]
- 9.Yusoff I F, Ormonde D G, Hoffman N E. Routine colonic mucosal biopsy and ileoscopy increases diagnostic yield in patients undergoing colonoscopy for diarrhea. J Gastroenterol Hepatol. 2002;17:276–280. doi: 10.1046/j.1440-1746.2002.02686.x. [DOI] [PubMed] [Google Scholar]
- 10.Misra S P, Dwivedi M, Misra V. et al. Endoscopic biopsies from normal-appearing terminal ileum and cecum in patients with suspected colonic tuberculosis. Endoscopy. 2004;36:612–616. doi: 10.1055/s-2004-814518. [DOI] [PubMed] [Google Scholar]
- 11.Cirocco W C, Rusin L C. The reliability of cecal landmarks during colonoscopy. Surg Endosc. 1993;7:33–36. doi: 10.1007/BF00591234. [DOI] [PubMed] [Google Scholar]
- 12.Powell N, Knight H, Dunn J. et al. Images of the terminal ileum are more convincing than cecal images for verifying the extent of colonoscopy. Endoscopy. 2011;43:196–201. doi: 10.1055/s-0030-1256174. [DOI] [PubMed] [Google Scholar]
- 13.Sakai YSection 6, Chapter 81Second edition.Philadelphia, PA: WB Saunders; 1999 [Google Scholar]
- 14.Kundrotas L W, Clement D J, Kubik C M. et al. A prospective evaluation of successful terminal ileum intubation during routine colonoscopy. Gastrointest Endosc. 1994;40:544–546. doi: 10.1016/s0016-5107(94)70249-7. [DOI] [PubMed] [Google Scholar]
- 15.Börsch G, Schmidt G. Endoscopy of the terminal ileum. Diagnostic yield in 400 consecutive examinations. Dis Colon Rectum. 1985;28:499–501. doi: 10.1007/BF02554095. [DOI] [PubMed] [Google Scholar]
- 16.Ansari A, Soon S Y, Saunders B P. et al. A prospective study of the technical feasibility of ileoscopy at colonoscopy. Scand J Gastroenterol. 2003;38:1184–1186. doi: 10.1080/00365520310006018. [DOI] [PubMed] [Google Scholar]
- 17.Chen M, Khanduja K S. Intubation of the ileocecal valve made easy. Dis Colon Rectum. 1997;40:494–496. doi: 10.1007/BF02258398. [DOI] [PubMed] [Google Scholar]
- 18.Lai E J, Calderwood A H, Doros G. et al. The Boston Bowel Preparation Scale: A valid and reliable instrument for colonoscopy-oriented research. Gastrointest Endosc. 2009;69:620–625. doi: 10.1016/j.gie.2008.05.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Iacopini G, Frontespezi S, Vitale M A. et al. Routine ileoscopy at colonoscopy: a prospective evaluation of learning curve and skill-keeping line. Gastrointest Endosc. 2006;63:250–256. doi: 10.1016/j.gie.2005.09.029. [DOI] [PubMed] [Google Scholar]
- 20.Powell N, Hayee B H, Yeoh D PK. et al. Terminal ileal photography or biopsy to verify total colonoscopy: does the endoscope agree with the microscope? Gastrointest Endosc. 2007;66:320–325. doi: 10.1016/j.gie.2007.02.039. [DOI] [PubMed] [Google Scholar]
- 21.Kennedy G, Larson D, Wolff B. et al. Routine ileal intubation during screening colonoscopy: a useful maneuver? Surg Endosc. 2008;22:2606–2608. doi: 10.1007/s00464-008-9843-x. [DOI] [PubMed] [Google Scholar]
- 22.Yoong K KY, Heymann T. It is not worthwhile to perform ileoscopy on all patients. Surg Endosc. 2006;20:809–811. doi: 10.1007/s00464-005-0426-9. [DOI] [PubMed] [Google Scholar]
- 23.McHugh J B, Appelman H D, McKenna B J. The diagnostic value of endoscopic terminal ileum biopsies. Am J Gastroenterol. 2007;102:1084–1089. doi: 10.1111/j.1572-0241.2007.01194.x. [DOI] [PubMed] [Google Scholar]
- 24.Melton S D, Feagins L A, Saboorian M H. et al. Ileal biopsy: Clinical indications, endoscopic and histopathologic findings in 10,000 patients. Dig Liver Dis. 2011;43:199–203. doi: 10.1016/j.dld.2010.08.004. [DOI] [PubMed] [Google Scholar]
- 25.Cherian S, Singh P. Is routine ileoscopy useful? An observational study of procedure times, diagnostic yield, and learning curve. . Am J Gastroenterol. 2004;99:2324–2329. doi: 10.1111/j.1572-0241.2004.40730.x. [DOI] [PubMed] [Google Scholar]
- 26.De Silva A P, Kumarasena R S, Perera Keragala S D. et al. The prone 12 o’clock position reduces ileal intubation time during colonoscopy compared to the left lateral 6 o’clock (standard) position. BMC Gastroenterol. 2011;11:89. doi: 10.1186/1471-230X-11-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Poolton J M, Wilson M R, Malhotra N. et al. A comparison of evaluation, time pressure, and multitasking as stressors of psychomotor operative performance. Surgery. 2011;149:776–782. doi: 10.1016/j.surg.2010.12.005. [DOI] [PubMed] [Google Scholar]
- 28.Misra S P, Dwivedi M. Role of intravenously administered hyoscine butyl bromide in retrograde terminal ileoscopy: a randomized, double-blinded, placebo-controlled trial. World J Gastroenterol. 2007;13:1820–1823. doi: 10.3748/wjg.v13.i12.1820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rex D K. Achieving cecal intubation in the very difficult colon. Gastrointest Endosc. 2008;67:938–944. doi: 10.1016/j.gie.2007.12.028. [DOI] [PubMed] [Google Scholar]
- 30.Shah S G, Saunders B P, Brooker J C. et al. Magnetic imaging of colonoscopy: an audit of looping, accuracy and ancillary maneuvers. Gastrointest Endosc. 2000;52:1–8. doi: 10.1067/mge.2000.107296. [DOI] [PubMed] [Google Scholar]
- 31.Shah H A, Paszat L F, Saskin R. et al. Factors associated with incomplete colonoscopy: a population-based study. Gastroenterology. 2007;132:2297–2303. doi: 10.1053/j.gastro.2007.03.032. [DOI] [PubMed] [Google Scholar]


