Abstract
Objective
To describe the development and evaluation of an observation system to assess the process of mother-infant feeding interaction relevant to infant neuro-behavioral regulation: the Mother-Infant Feeding Tool.
Design
Secondary analysis.
Setting
Special care nursery just before discharge and in the home at 1 and 4 months postterm age.
Participants
Forty-three mother-infant dyads.
Methods
Videotaped feeding interactions were examined to assess regulatory processes of mother-infant interaction. Data were collected at three times over the infant’s first 4 postterm months: before the infant’s discharge from the special care nursery and at 1 and 4 months postterm age in the home.
Results
Across all three data points mothers rarely talked to their infants.
Conclusion
Further testing is needed, but the Mother-Infant Feeding Tool shows promise in assessing very early mother-infant feeding interactions.
Keywords: preterm infant feeding, mother-infant interaction, preterm infants
Early maternal and infant-feeding behaviors are important because of their frequency and their regulatory effects on nutrient intake and infant development (Anand & Scalzo, 2000; DeWitt et al., 1997; Valenzuela, 1997). These regulatory effects are derived from infant physiological, neuromotor, behavioral, attentional, and emotional responses to maternal behavior. Interactive feeding behaviors are particularly important for mothers of premature infants because of the infants’ needs for feeding support. Early feeding interactions may strengthen adaptive feeding behaviors or reinforce maladaptive feeding behaviors of both the mother and the infant. Adaptive maternal feeding behavior is positive in affect and is sensitive and responsive to the infant’s signals of need for protection, nurturance, and comfort (DeWitt et al.).
A mother who is sensitive recognizes her infant’s cues and responds accordingly. Adaptive infant feeding behavior is organized and regulated in a manner that supports participation in the feeding within the limits of developmental capacities. Over time, patterns of mother-infant feeding interaction may modify the development of the premature infant’s brain pathways associated with social, cognitive, emotional, and behavioral participation in the goal-directed activity of feeding (Als et al., 2004; Anand & Scalzo, 2000). Little is known about the very early feeding interactions of mothers and their preterm infants’ that occur during the first quarter of the first postterm year.
Neural pathways of the brain involved in emotional and social function begin to develop in the first months of life (Champagne & Curley, 2005; Schore, 2001). A substantial amount of brain maturation occurs during infancy. The repeated interactions that an infant experiences during feeding are incorporated into and shape neural development. The neural pathways that develop are central to regulation of physiological, arousal, and motoric processes and conditions as well as behavioral adaptations during feeding. Examples of behavioral adaptations include sucking, swallowing, and breathing in a coordinated manner. Mothers of prematurely born infants will have a more challenging job of supporting their infants when they begin to nipple feed than mothers of full-term infants, given the younger infants’ neurodevelopmental limitations in sucking, swallowing, and breathing. Not all premature infants will have coordination at the time they begin nipple feeding. The neuro-behavioral development that occurs is the basis of the infant’s long-lasting regulatory strategies (Anand & Scalzo, 2000).
It is important to study the process involved in the very early feeding interaction of mothers and their prematurely born infants because of its effect on neuro-behavioral development. A process is a series of actions, changes, or functions bringing about a result, such as feeding. However, little is known about feeding interactions that begin before prematurely born infants are yet term age and continue through the early months of the first postterm year. Available instruments to assess very early feeding interactions are lacking in features to assess the regulatory process of mothers and infants. The purpose of this article is to describe the development and evaluation of an observation system to assess the process of mother-infant feeding interaction relevant to infant neuro-behavioral regulation.
Feeding is considered the most complex and highly organized behavior of very young infants (Osofsky, 1976). Studying the regulatory processes of mother-infant feeding interactions will help clinicians and researchers gain a better understanding of the structure of feeding interactions. A description of the process involved in mother-infant feeding interactions will inform the observer about interactive behavior of the mother in the context of the infant’s behavior and vice versa and provide a basis for elucidating the effect of the behavior of one member of the dyad on the other. Once researchers and clinicians understand the process, interventions can be developed to aid the dyad in becoming more adaptive in their feeding behavior.
Adaptive feeding behaviors for the mother are sensitive to the infant’s signals, responsive to needs, and supportive of the regulatory process. An extensive body of research has examined mother-infant interactive behavior (Coyl, Roggman, & Newland, 2002; Davis, Edwards, & Mohay, 2003; Feldman & Eidelman, 2006; Forcada-Guex, Pierrehumbert, Borghini, Moessinger, & Muller-Nix, 2006; Harel, Oppenheim, & Tirosh, 1999; Holditch-Davis, Cox, Miles & Belyea, 2003; Holditch-Davis, Miles, & Belyea, 2000). However, these studies have not focused on the regulatory aspects of the adaptive or maladaptive qualities of mother-infant interactive behavior during feeding. To date, instruments to assess the process of regulation during feeding for premature infants and their mothers are lacking.
Regulatory Aspects of Mother-Infant Interaction
The synactive theory of development (Als, 1982; Als et al., 2004) and attachment theory (Bowlby, 1988) provided the theoretical underpinnings for an observational tool to describe prematurely born infants interacting with their mothers during feeding. According to Als and Gilkerson (1995), infant behavior is a function of four subsystems. The subsystems include the autonomic, motor, behavioral, and attentional systems. The synactive theory suggests that mothers of preterm infants assist their infants to meet regulatory goals by providing sensitive and responsive care. This care is contingent upon the infant’s physiological and motor stability as well as attentional and behavioral adaptations to the feeding.
Bowlby (1982) postulated that throughout infancy, the infant must have a close relationship with a warm, nurturing, consistent caregiver to ensure protection in the face of both internal changes and external challenges. The mother helps protect the infant’s airway during feeding and provides comfort by aiding the infant in maintaining regulated behavioral, emotional, and physiological processes. Research has shown that maternal sensitivity to infant signals and timely and appropriate responsiveness to the infant’s signals, pacing, and preferences are associated with positive infant developmental outcomes (Ainsworth, 1983; Egeland & Farber, 1984; Isabella, 1993; Mertesacker, Bade, Haverkock, & Pauli-Pott, 2004). Maternal sensitive and responsive behaviors during feeding are important for infant feeding outcomes (DeWitt et al., 1997; Pridham, Brown, Clark, Sondel, & Green, 2002; Thoyre & Brown, 2004; Valenzuela, 1997). Infant regulated feeding behaviors have been found to depend on the mother’s ability to modify the environment when needed and to directly support the infant’s feeding (Brown & Pridham, 2007). Infant behaviors regulate those of the mother and the mother’s caregiving behaviors in turn regulate those of the infant (Barnard, Bee, & Hammond, 1984; Osofsky & O’Connell,1972).
Premature infants’ immature regulatory systems make it difficult to process stimulation, and their cues for support in regulating input may not be clear to their mothers (Barnard et al., 1984; Davis et al., 2003; Singer et al., 2003; Thoyre & Carlson, 2003a). Consequently, premature infants have been found to be less attentive, less expressive, and fussier than term infants (Davis et al.; Wolf et al., 2002). As a result of immaturity, these infants may experience physiological, neuromotor, and behavioral disorganization during feeding. This disorganization is just one of the challenges mothers face when feeding their premature infants. Prematurely born infants also have poor coordination of their breathing and swallowing (Vice & Gewolb, 2008) and waning energy levels during feeding (Thoyre, 2001; Thoyre & Carlson, 2003b). In order to respond appropriately and in a timely manner, mothers of preterm infants must be familiar with the infant’s cues during feeding and aware of the infant’s ability to coordinate sucking, swallowing, and breathing.
Observational Tools for Examination of Mother-Infant Feeding Interactions
The most widely used tools currently available to measure mother-infant feeding interactions are scales that give a score on specific qualities for an entire feeding. One widely used measure is the Nursing Child Assessment Feeding Scales (NCAF) (Barnard, 1978). The NCAF consists of 50 items for assessment of four parental subscales (sensitivity to infant cues, response to infant distress, social-emotional growth fostering, and cognitive growth fostering). The NCAF also includes 16 items for assessment of two infant scales (clarity of cues and responsiveness to the caregiver). All items are scored on a binary scale (observed or not observed). The NCAF has been used widely as a clinical screening instrument and in research studies to characterize the extent to which parental and infant feeding behaviors are adaptive, as determined by total parent or infant scores or by subscale scores. The NCAF is not structured to permit assessment of regulatory processes of parent and infant as they are engaged in interaction. That is, the scale is not designed to code behavior of one member of the dyad in context of the other member’s behavior. A binary system provides information about who needs intervention but does not provide detailed information about the behaviors that warrant attention and intervention.
Similarly, the feeding checklist (MacPhee & Schneider, 1996) can be used to target parents or infants who need support, but it does not provide detailed information about the behaviors that warrant professional attention and intervention. The feeding checklist is a 25-item binary scale. The items reflect the caregiver’s ability to respond to infant cues and the infant’s ability to provide clear signals. In contrast to the NCAF, the feeding checklist exclusively addresses the qualities of the feeding as a nutritional task.
In addition to binary scales that mark the presence or absence of behaviors, researchers also use global rating scales to assess feeding interactions. Global rating scales attempt to capture the individual’s behavior in the identified ordered series of categories by assigning a numerical value to each category. Likert-type rating scales are typically used. Global measures utilize subjective estimates of quantity rather than direct counts of behaviors as used in event-based or micro-analytic measures. Global measures are particularly suitable where observers are required to summarize across behaviors or across the interaction process (Margolin et al., 1998). Instruments that provide a global rating are not designed to describe the process that goes on during the interaction.
The feeding scale (Chatoor, Getson, Menvielle, & Brasseaux, 1997) provides a global rating of mother-infant/toddler interactions based on the analysis of a videotaped feeding interaction. The scale has 46 items (26 maternal items and 20 infant items) and five subscales. The subscales include the following: dyadic reciprocity, dyadic conflict, talk and distraction, struggle for control, and maternal noncontingency. Mother-infant behaviors are rated from 20 minutes of a videotaped feeding on a 4-point Likert scale on how often and how intensely each of the behaviors occurred. The feeding scale is designed to characterize the quality of the relationship. The scale has not been used with infants less than 5 weeks of age, and it is not designed for observations of the process of interaction.
The Assessment of Mother-Infant Sensitivity Scale (AMIS) (Price,1983) was developed to measure the quality of early mother-infant feeding interactions in the infant’s first 4 months. The AMIS contains 25 items scored from 1 to 5 on a Likert scale, with higher values indicating higher sensitivity. Fifteen items evaluate maternal behavior, 7 evaluate infant behavior, and 3 evaluate dyadic behavior. Maternal items are holding/handling, social/affective, and feeding/caregiving behavior. Infant items are mood/affect, vocalization, and posture. Dyadic items include regulation of feeding, initiation, and synchrony in response to pleasurable affect. Mother-infant feeding interactions are videotaped and the entire feeding is scored. The AMIS identifies areas of less sensitive maternal behavior; however, maternal behavior is not scored in context of the infant’s needs. For example, an infant may cease to feed with coordinated sucking, swallowing, and breathing with the mother’s talking during feeding. The mother may receive a score of 5, indicating she is highly sensitive and her speech is warmly affectionate and loving. However, her vocalization may not be well timed, an attribute of her behavior that the AMIS is not designed to record. Because it is not structured to examine either the infant’s antecedent behavior or the mother’s response to the infant’s behavior, the AMIS has limited usefulness in designing interventions tailored to a mother-infant dyad, including sensitive timing of maternal behavior.
The Parent Child Early Relational Assessment (PCERA) (Clark, 1999) consists of 65 items (29 parental, 27 infant, and 8 dyad), each of which is scored on a 5-point rating scale defined by the intensity, frequency, or duration of the quality of behavior. Each scale assesses an affective and behavioral characteristic that the parent and infant each bring to the interaction. The PCERA permits description of qualities of social-emotional as well as task-related behavior during feeding; however, it does not permit a description of the process of mother and infant interaction throughout the feeding.
Despite the available research on mother-infant feeding interaction, there are no instruments designed specifically to describe the very early feeding process of parents and their very young infants, including the process of newly oral-feeding preterm infants in a special care nursery. In particular, an observational system to describe infant regulation or dysregulation, the parent behavioral context of the regulated or dysregulated behavior, and the sequence of parental and infant behaviors in which regulated or dysregulated behavior occurs, resolves, or is maintained has not been available to date. Regulation refers to maintaining internal goals (emotional, behavioral, physiological, and neuromotoric homeostasis) and external goals (interaction with the environment). For example, infants who are regulated during feeding will suck, swallow, and breathe in a coordinated manner. Dysregulation refers to ineffective regulation such as infants choking because they are trying to breathe and swallow simultaneously.
The premature infant’s immature neuromotor development puts her/him at risk for dysregulation during feeding. For example the infant’s ability to coordinate swallowing with respiration is immature, putting the airway at risk (Gewolb & Vice, 2006). Therefore, an observational tool to identify areas where mothers need of support early on would be beneficial. An observational tool to assess mothers and their premature infants during feeding was developed to address this gap. The Mother-Infant Feeding Tool (MIFT) is a real-time, coding scheme that was designed to capture the regulatory process of mother-infant feeding interactions. This article describes the characteristics and method of application of the MIFT and examines the reliability and validity of the MIFT using videotaped feeding interactions of mothers and their prematurely born infants before and after discharge from the special care nursery.
Method
Study of mother-infant interaction using the MIFT
In this secondary analysis, videotaped feeding interactions were examined to assess regulatory processes of mother-infant interaction. Data were collected at three times over the infant’s first 4 post-term months: before the infant’s discharge from the special care nursery and at 1 and 4 months post-term age (PTA) in the home. Institutional review board approval was obtained from the institutional review boards of the university and all three participating hospitals.
Participants
The original sample for this study was recruited from one large central city hospital and two smaller hospitals that served both an urban and a rural area. The sample consisted of 43 mother-premature infant dyads. The inclusion criteria for the mothers were age 17 years or older and ability to speak and read English. Inclusion criteria for the infants were less than 35 weeks gestation at birth, appropriate weight for gestational age, no major congenital malformations, and no known drug exposure. Infants with an intraventricular bleed greater than Grade II were not included. Infants with bronchopulmonary dysplasia were not excluded. Both breast- and bottle-fed infants were included; however, the breastfeeding sample was small.
Procedure
Clinical and systematic observations of videotaped feedings were used to begin the development of the MIFT. This method was undertaken by the investigators to describe the real-time behavior of mother and infant in relation to each other during feeding. Numerous videotapes of mothers and infants were watched to develop the coding system. To establish face and content validity, experts in mother-infant interaction reviewed the coding scheme and their input was used to refine the items.
Videotapes of mothers and infants feeding were digitized and then stored on the computer’s hard drive so they could be opened for coding. The system used (Observer) is computer-based and offers a systematic means of observing and recording behavior as it occurs in real-time from videotape recordings. The coding analysis is done by replaying the digitized video recording and entering observational codes into the computer as they are identified. The coding may then be checked against the videotape and corrections may be made.
In this computerized system, the initial state in each category is marked and change in behavior can be noted with a precision of milliseconds. For each feeding session, the Observer coding provided the temporal sequence of the events (in seconds), the total duration of each event, and the temporal relationship between two different classes of events (e.g., between maternal behavior and infant regulation).
Measures
The MIFT
The MIFT is coded from videotaped feeding interactions. The mother and infant codes and their definitions are included in Tables 1 and 2, respectively. Codes are of two types: (a) momentary events, producing frequency counts; and (b) continuous codes, producing duration in seconds. Mother and infant behaviors are coded independently. Behavior in each category that cannot be determined due to poor camera angle or lighting is coded as “unable to determine.” The continuous codes are mutually exclusive and exhaustive within categories. Both maternal and infant behaviors are described by continuous codes that are co-occurring.
Table 1.
Mother Code Definitions
| Monitoring | |
| Monitoring | Observes feed; initiates, continues, or ends the feeding with infant signs; breastfeeding mothers may pull the breast back to observe feeding |
| Unfocused | Briefly glances away; is distracted; carries on conversation with another person; attention is elsewhere |
| Supportive feeding | |
| Supporting feeding | Supports infant in feeding position (infant can bring hands to midline, has chin tucked, positions neck in a neutral position for optimal breathing, rewraps infant to provide support, waits for infant to open mouth before inserting nipple |
| Not supporting | Does not support infant’s position or allow infant to initiate feeding |
| Unable to determine | Unclear; unable to determine if mother’s actions were supportive |
| Supportive environment | |
| Supportive environment | Manipulates the environment to make feeding more pleasurable; turns down the lights; moves away from a light source |
| Not supportive | Does not manipulate the environment |
| Verbal | |
| Normal talk | Talks about anything other than feeding with normal voice quality |
| Supportive talk | Praises infant, encourages infant, motherese |
| Harsh | Commands infant; there is sharpness to her voice |
| Talk to others | Talks to anyone other than infant with normal voice quality |
| Harsh others | Speaks harsh to anyone other than infant |
| Nonverbal | Does not speak |
| Vestibular stimulation | |
| Rocking | Moves infant forward or backward; rocks or bounces infant |
| No movement | Does not move infant |
| Position change | Changes infant’s position (e.g., from feeding position to burping position);once movement is complete |
| Reposition self | Changes her position (arm or body) |
| Touching | |
| Gentle | Gentle rubbing or patting including during burping, kissing, wiping, or tickling |
| Rough | Touching that has a harsh, jerky quality and includes rough patting or rubbing during burping |
| No touch | Not rubbing or patting infant |
| Feeding | |
| Nipple in | Nipple fully seated in infant’s mouth |
| Nipple out | Space is seen between nipple and infant’s mouth |
| Active feeding | |
| Tongue &/or cheek support | Applies tongue and/or cheek support |
| No tongue &/or cheek | Does not apply tongue and/or cheek support |
| Jiggling | Jiggles bottle in infant’s mouth |
| Pulling/pushing | Pulls or pushes nipple in and out of infant’s mouth |
| Roots infant | Touches or strokes infants lips or cheeks |
| Repositions nipple | Repositions nipple (turns bottle) |
| Tips nipple back | Slows flow or stops flow by tipping nipple back |
| Opens mouth | Pulls the chin down to open the infant’s mouth |
| Repositions infant’s head | Repositions infant’s head |
| Rough | Repositioning is rough, sudden, jerky, may elicit startle |
| Gentle | Repositioning is gentle, slow |
Note. Any mother behavior that lasts <2 s is not coded.
Table 2.
Infant Code Definitions
| Infant muscle tone | |
| Regulated tone | Partially contracted state of the limbs, flexion, midline positioning |
| Dysregulated tone | Hypotonic or hypertonic muscle tone, tremors, flailing, startle, finger splaying |
| Unable tone | Unable to determine infant tone. Infant may be swaddled and arms and legs cannot be seen and infant face may not be visible to determine tone in cheeks. |
| Infant physiologic indices | |
| Regulated physiology | Pink with patterned breathing |
| Unregulated physiology | Dysregulated breathing, includes signs of nonhomeostatic autonomic functioning, including pallor, grunting, or use of accessory muscles for breathing |
| Unable physiology | Unable to determine infant breathing or color |
| Infant behavior | |
| Regulated behavior | Infant feeding smoothly; not pulling away from bottle or mother; turns to bottle, opens mouth with tongue down |
| Dysregulated behavior | A change in behavior including averting, pulling/turning away/resisting, body language, including closed/fisted hands in the context of signs of disorganization; has the quality of the infant attempting to protect him/herself |
| Unable behavior | Unable to determine if infant’s behavior is regulated or not; infant’s hands may be swaddled and not visible; unable to determine if infant is pulling away from mom |
| Infant emotional | |
| Regulated emotional | Infant’s face is relaxed |
| Dysregulated emotional | Facial expressions, including raised eyebrows, frowning, grimacing, crying |
| Unable emotional | Unable to see infant’s face to determine regulation |
| Sucking/swallowing | |
| Regulated sucking | Actively sucking and swallowing |
| Dysregulated swallow | Infant is coughing, choking, or multiple swallowing |
| Not sucking | Not sucking |
| Unable to determine | Unable to determine if infant is sucking |
| Dribbling | |
| Dribbling | Formula is seen escaping from infant’s mouth |
| Not dribbling | Formula cannot be seen escaping from infant’s mouth |
| Unable to determine | Cannot determine if formula is escaping from infant’s mouth |
| Indices of arousal | |
| Open/half-lidded | Infant’s eyes are open, half open |
| Closed | Infant’s eyes are closed |
| Unable to determine | Unable to see infant’s face |
The infant is assessed as being regulated or dysregulated in each of four areas: muscle tone, physiological indices, behavior, and emotion. In addition to regulation, infant sucking/swallowing, dribbling, and indices of arousal are assessed. These seven infant codes were chosen because each category defines an area of observable behavior that has clinical meaning. In addition, they are areas of behavior that a mother could observe and respond to.
Maternal behavior is described with seven categories of behaviors: monitoring behavior, supportive behavior, verbal behavior, vestibular stimulation, touching, feeding, and active feeding. These maternal behaviors were chosen because they were observed in the context of the feeding. These are also behaviors identified in the literature as clinically important and the range of social-emotional and task-related behaviors that are likely to be observed during the feeding of a young infant, including a preterm infant.
Coding begins when the mother presents the nipple to the infant. The infant may be in a regulated or a dysregulated condition before the feeding begins; a code from each coding category is selected. For example, the infant may be coded as not sucking, eyes open, and having regulated tone, behavior, physiological indices, and emotions. The mother may be coded as monitoring, supporting, not talking, not moving, not touching, no tongue and/or cheek support, and nipple out. As the feeding proceeds, codes are changed within each category as maternal or infant behaviors change.
All videotapes were coded by one coder trained in the MIFT. A second coder trained to 80% reliability coded a random 20% of the videotapes. Reliability was measured using percent agreement and Cohen’s κ. After all videos were coded reliability and concurrent validity was assessed. To assess concurrent validity, correlations between PCERA scale scores and the frequency or duration of specific codes in the MIFT were calculated.
Parent Child Early Relational Assessment
The PCERA was used in this study to examine the validity of the MIFT. The PCERA is a 65-item observational rating scale that was designed to assess the amount, duration, and intensity of interactional behavior, assessed comprehensively in terms of social-emotional and task-related qualities. These qualities capture the major features of mother-infant interaction identified in the literature (Clark, Hyde, Essex, & Klein, 1997; Grych & Clark, 1999). Clark identified six scales (two maternal, two infant, and two dyadic) consisting of PCERA items on theoretical grounds and factor analysis of data obtained from mothers and healthy infants during feeding at 4 months infant age (Clark, 1999;Clark et al.). Each item is rated on a scale of 1 to 5; 1 = behavior of clinical concern and 5 = regulated, adaptive behavior.
Two PCERA subscales derived from theoretical literature and factor analysis (Clark, 1999) were used in this study to describe maternal interactive behavior. The first of two subscales, Positive Affective Involvement and Sensitivity/Responsiveness (PAISR), includes 16 items to rate maternal sensitivity and responsiveness to the infant’s cues, warmth and kindness of tone of voice, expression of positive affect and enjoyment, competence in structuring and mediating of the environment to support nutrient intake and a positive feeding experience, visual regard, and mirroring of the infant’s feelings. The second subscale, regulation of Affect and behavior (RAB), includes 14 items to rate how competently a mother structures a feeding and mediates the infant’s feeding environment and provides a positive and well-regulated social-emotional experience for her infant. Items in the RAB subscale also describe a mother’s curtailment of such behaviors as talking with an angry tone of voice, expressing a negative attitude, behaving intrusively, handling the infant roughly or abruptly, and responding inflexibly.
Two PCERA subscales were used to describe infant adaptive feeding behavior. The first subscale, Infant Positive Affect, Communication and Social Skills (IPACS), includes 12 items to rate the quality of attention, motoric and communicative skills, social initiative, and responsiveness. The second sub-scale, Infant Regulation of Behavior and Affect (IRBA) includes 11 items for describing the infant’s expression of negative affect, fearfulness or tension, irritability, soberness, avoiding or averting behavior, attention to feeding, and interest in the environment.
A trained coder who was blind to the study hypotheses and who did not know the families coded 100% of the videotapes. To determine intercoder reliability, the first author, who was trained to 80% reliability in coding PCERA items, independently coded a random sample of 20% of the videotapes. The second 5 minute portion of the videotaped feeding was used to rate the items. Alpha coefficient ranges for the four scales, each assessed at the three data collection points, were as follows: PAISR, .96 to 97; RAB, .93 to .95; IPACS, .85 to .89; and IRAB, .88 to .89.
Analysis
Data were analyzed using descriptive statistics to examine the distribution of maternal and infant behaviors. Pearson’s r was used to examine the relationship among all the variables. Intra-rater reliability was checked throughout the coding period. For inter-rater reliability, a coder was trained to a minimum of 80% reliability. Each time, the two-trained observers entered the same code with less than 2 seconds of difference between the two entries, agreement was tallied; otherwise, disagreement was tallied. Using a random sample of 20 videotapes, inter-rater reliability was examined and κ coefficients computed separately for infant and maternal behaviors.
Results
Description of Participants
The average age at birth for the infants was 30 weeks (SD = 3.1). There were 22 male (51%) and 21 female (49%) infants in the study. Sixteen infants (37%) stayed in the hospital 9 weeks or more. The average age of the mothers was 29 years (SD = 6.9). Twenty-nine parents (67%) were married and 21 households (49%) had an income greater than $50,000. Nineteen mothers (44%) had an associate’s degree or higher. The average age of the father was 30.5 years (SD = 6.3 years) and average age of the mother was 29.4 years (SD = 6.5 years). The majority of the mothers and fathers were White (n = 31, 72% and n = 30, 70%, respectively). Demographic characteristics of the families are shown in Table 3.
Table 3.
Demographic Data on Mothers and Infants
| n | % | |
|---|---|---|
| Mother’s ethnicity | ||
| Asian American | 2 | 4.7 |
| European American | 31 | 72.1 |
| African American | 6 | 14.0 |
| Latino | 2 | 4.7 |
| Mixed | 2 | 4.7 |
| Income | ||
| < 10,000 | 4 | 9.3 |
| 10,000–19,999 | 4 | 9.3 |
| 20,000–34,999 | 4 | 9.3 |
| 35,000–49,999 | 6 | 14 |
| >50,000 | 21 | 48.8 |
| Missing | 4 | 9.3 |
| Infant birth weight (g) | ||
| <1,000 | 9 | 21 |
| 1,000–1,500 | 11 | 26 |
| 1,501–2,000 | 10 | 23 |
| 2,001–2,500 | 11 | 26 |
| >2,500 | 2 | 4 |
| Gestational age (weeks) | ||
| <26 | 7 | 16 |
| 27–28 | 11 | 26 |
| 29–30 | 3 | 7 |
| 31–32 | 12 | 28 |
| 33–34 | 10 | 23 |
| Gender | ||
| Male | 22 | 51 |
| Female | 21 | 49 |
The Coded Interaction Process
The process of mother-infant interaction, coded with the MIFT on the Observer system, is illustrated by an episode of infant dysregulation in (Figure 1). Figure 1 reads starting on the column at the left and contains all the mother-infant categories. The colored bars in the middle column show the duration of each behavior that has been coded in seconds and what behaviors were ongoing at any specific second. The set of columns on the right shows what colors represent each behavior. The coded interaction process displayed in the middle column is read by identifying what maternal and infant behaviors were concurrently happening. The interaction shown in Figure 1 is read by examining the colored bars. For example, at approximately 5 seconds the mother opened the infant’s mouth shown by blue vertical line on the brown bar (8th row) and inserts the nipple, shown by a green vertical bar (5th row). The infant immediately becomes dysregulated in behavior and tone. The dysregulation is shown in the 11th and 12th row by the change in color from green to purple and by the change in color from light green to purple. The mother takes the nipple out of the infant’s mouth, shown in the 5th row by the change in color from green to purple, and the infant becomes regulated again, shown by the change in color on the 12th row from purple to light green. Intervention for this mother could include helping her to root her infant and to wait for the infant to indicate readiness for the nipple by opening the mouth.
Figure 1.
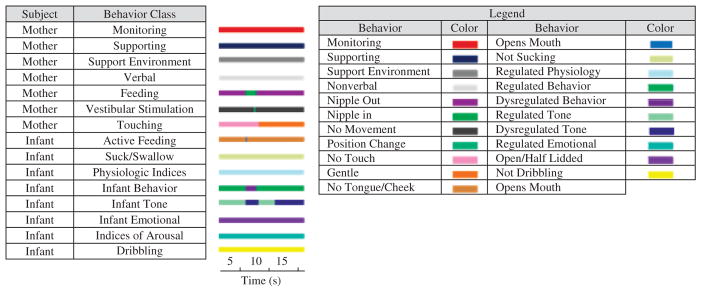
Example of infant dysregulation
Frequency and Percent of Duration of Specific Maternal and Infant Behaviors
Table 4 includes the total number of events and the percent of feeding time (nipple in to nipple out) for a few select behaviors at each of the observation time points (near discharge [Time 1], at 1 month PTA [Time 2], and at 4 months PTA [Time 3]). Mothers spent less time monitoring and more time supporting their infants in an optimal feeding position as the infants grew older. Mothers spent more of the feeding time not focused on the infant or the feeding as the infant grew older. Across all three data collection points mothers rarely talked to their infants during feeding. Mothers also spent less time jiggling and pushing/pulling the nipple as their infant’s grew older. Infants spent less time having dysregulated behavior and tone as they grew older. Infants spent more time with their eyes open during the feeding as they grew older.
Table 4.
Total Number and Percent of Feeding Time of Selected Coded Behavior
| Variables | Total Number Time 1 Mean (SD) |
Percent of Feeding Time 1 Mean (SD) |
Total Number Time 2 Mean (SD) |
Percent of Feeding Time 2 Mean (SD) |
Total Number Time 3 Mean (SD) |
Percent of Feeding Time 3 Mean (SD) |
|---|---|---|---|---|---|---|
| Monitoring | 92.46 | 81.34 | 83.78 | |||
| (8.44) | (22.12) | (17.50) | ||||
| Supportive | 94.96 | 96.65 | 99.68 | |||
| (18.54) | (6.20) | (1.99) | ||||
| Normal talk | 1.16 | 4.85 | 6.37 | |||
| (0.74) | (8.60) | (8.05) | ||||
| Supportive talk | 1.09 | 0.00 | 0.00 | |||
| (6.95) | (0.00) | (0.00) | ||||
| Nonverbal | 90.73 | 91.23 | 90.97 | |||
| (9.85) | (11.13) | (9.10) | ||||
| Nipple in | 100 | 100 | 100 | |||
| (0.09) | (0.07) | (0.07) | ||||
| No movement | 98.82 | 86.46 | 84.89 | |||
| (3.85) | (26.59) | (28.46) | ||||
| No touch | 93.41 | 91.99 | 93.48 | |||
| (14.71) | (13.80) | (8.82) | ||||
| No tongue and cheek support | 98.08 | 99.93 | 100 | |||
| (3.59) | (0.34) | (0.07) | ||||
| Jiggle | 9.40 | n/a | 4.87 | n/a | 3.51 | n/a |
| (20.97) | (9.31) | (8.08) | ||||
| Push/pull | 10.40 | n/a | 8.33 | n/a | 3.21 | n/a |
| Nipple | (28.17) | (30.34) | (6.52) | |||
| Roots | 27.00 | n/a | 4.26 | n/a | 0.92 | n/a |
| (35.79) | (6.18) | (2.23) | ||||
| Supportive environment | 84.89 | 99.68 | 94.70 | |||
| (35.43) | (1.66) | (22.62) | ||||
| Regulated physiological indices | 100 | 93.22 | 94.68 | |||
| (0.09) | (24.09) | (22.62) | ||||
| Regulated behavior | 33.16 | 73.30 | 80.25 | |||
| (39.36) | (32.48) | (29.79) | ||||
| Unable to determine behavior | 61.59 | 26.26 | 19.62 | |||
| 41.14 | (32.19) | (29.80) | ||||
| Regulated tone | 33.33 | 72.38 | 80.04 | |||
| (37.60) | (32.49) | (27.45) | ||||
| Unable to determine tone | 58.73 | 25.53 | 18.26 | |||
| (41.16) | (31.74) | (27.87) | ||||
| Regulated emotions | 65.76 | 72.32 | 77.97 | |||
| (42.84) | (40.27) | (34.97) | ||||
| Eyes open | 24.35 | 42.10 | 54.56 | |||
| (36.11) | (39.26) | (39.91) | ||||
| Eyes closed | 24.35 | 24.72 | 11.57 | |||
| (36.11) | (33.24) | (22.09) | ||||
| Unable to determine dribbling | 75.97 | 80.51 | 83.36 | |||
| (35.09) | (33.29) | (31.32) |
Kappa values for infant behaviors ranged from .51 to .83, whereas κ values for mother behaviors ranged from .73 to .94. Combined κ ranged from .73 to .86 for a single session. The combined percent agreement for maternal and infant variables was 80.7% with a range of 74.7 to 87.0.
The percent of time infants were dysregulated behaviorally was significantly and positively correlated with maternal behaviors of pushing/pulling and repositioning the nipple (r =.49 and .32, respectively). The percent of time the infant was dysregulated physiologically was significantly and positively correlated with maternal behaviors of jiggling the nipple (r =.36). The percent of time infants were dysregulated emotionally was significantly and positively correlated with maternal behaviors of pushing/pulling and repositioning the nipple (r =.44 and .36). The percent of time infants had dysregulated tone was significantly and positively correlated with jiggling the nipple (r =.44).
Significant correlations were found between PCERA subscales and specific codes of the MIFT. Mothers’ positive affect, involvement, responsiveness, and sensitivity (PAISR) were significantly and negatively associated with infants’ dysregulated sucking (r =−.30). The mother’s PAISR and RAB were also significantly and positively associated with maternal talking (r =.58). Infants’ positive affective communication and social skills were significantly and negatively associated with maternal nonverbal interactions (r =−0.30). The IRBA was not correlated with any of the MIFT codes.
Discussion
The MIFT is an observational coding system that enables description of the process involved in mother-infant feeding interactions. Specifically, the MIFT permits description of the sequence of mother and infant feeding interactive behaviors in relation to each other. In addition, the MIFT allows researchers to examine what elicits dysregulation in the infant, how dysregulation progresses, and how it is resolves. The Observer coding program allows visual examination of the sequence of mother and infant behaviors during an episode of infant dysregulation.
The MIFT enables researchers and health care personnel to evaluate mother-infant interaction processes likely to be relevant and even central to the development of the infant’s feeding skills and the early mother-infant relationship. The tool will enable clinicians to look at specific episodes of infant dysregulation in an effort to identify specific behaviors that are clinically useful. For example, a clinician may notice that the mother and infant have difficulty initiating a feeding. The clinician may videotape the feeding interaction but only analyze the beginning of the feeding. This part of the feeding interaction could be played back and discussed with the mother as part of a feeding intervention. The identification of maternal behaviors that are regulating or dysregulating for a specific infant provides a means of individualizing care. The tool also gives the clinician labels to use with parents to describe what is occurring.
Limitations
Despite the limited number of breastfeeding dyads, the researchers found that breastfeeding mothers engaged in all the same behaviors as the bottle-feeding mother except chin and/or cheek support. A larger sample of breastfeeding mothers may identify additional codes. This was a secondary analysis of videotaped feeding interactions between mothers and their prematurely born infants, and only one camcorder was used to capture the dyad. If a second camcorder was used to capture the infant’s behaviors, the inability to determine codes may be reduced or eliminated.
Conclusions
The MIFT can be helpful to researchers and clinicians who intend to understand the process of feeding and how mothers and infants coregulate infant feeding behavior. Future plans for testing the MIFT will include using a larger sample of breast-feeding dyads and examining the tool with older pre-term and full-term infants. Future studies will also examine very early, as soon as the infant begins to nipple, and follow the dyad until 4 months corrected age. Use of the MIFT will aid researchers in identifying and addressing questions concerning the sequence and contingencies of feeding behaviors that may make a difference in the adaptiveness of the feeding process and in feeding outcomes. Through early assessment of maternal and infant processes of regulation as they occur in real time during feeding interaction, areas of concern for mother-infant dyads can be evaluated and addressed and mothers can be given specific information concerning support of the infant’s neuromotor, behavioral, physiological, and emotional regulation during feeding.
Acknowledgments
Supported by the National Institute of Nursing Research, NRSA Award F31NR007703, Merck Foundation, Wisconsin Nurses Association, Sigma Theta Tau Beta Eta at Large, Helen Denne Schulte Fund, Virginia Horn Henry Foundation, and the Interventions to Prevent and Manage Chronic Illness T-32 NR07091.
Contributor Information
Lisa F. Brown, Assistant professor in the School of Nursing, Virginia Commonwealth University, Richmond, VA.
Suzanne Thoyre, Associate professor in the School of Nursing, University of North Carolina, Chapel Hill, NC.
Karen Pridham, Professor emeritus from the School of Nursing, University of Wisconsin-Madison, Madison, WI.
Christine Schubert, Assistant professor in the School of Medicine, Virginia Commonwealth University, Richmond, VA.
References
- Ainsworth M. Patterns of infant-mother attachment as related to maternal care: The early history and their contribution to continuity. In: Magnusson D, Allen VL, editors. Human development: An interactional perspective. New York: Academic Press; 1983. pp. 35–55. [Google Scholar]
- Als H. The unfolding of behavioral organization in the face of biological violation. In: Tronick E, editor. Social interchange in infancy: Affect, cognition, and communication. Baltimore: University Park Press; 1982. pp. 125–160. [Google Scholar]
- Als H, Duffy FH, McAnulty GB, Rivkin MJ, Vajapeyam S, Mulkern RV, et al. Early experience alters brain function and structure. Pediatrics. 2004;113:846–857. doi: 10.1542/peds.113.4.846. [DOI] [PubMed] [Google Scholar]
- Als H, Gilkerson L. Developmentally supportive care in the NICU. Zero to Three. 1995;15:2–10. [Google Scholar]
- Anand KJ, Scalzo FM. Can adverse neonatal experiences alter brain development and subsequent behavior? Biology of the Neonate. 2000;77:69–82. doi: 10.1159/000014197. [DOI] [PubMed] [Google Scholar]
- Barnard K. Nursing child assessment feeding scale. Seattle, WA: University of Washington, School of Nursing; 1978. [Google Scholar]
- Barnard K, Bee H, Hammond M. Developmental changes in maternal interactions with term and preterm infants. Infant Behavior and Development. 1984;7:101–113. [Google Scholar]
- Bowlby J. Attachment and loss. New York: Basic Books; 1982. [Google Scholar]
- Bowlby J. A secure base: Parent-child attachment and healthy human development. New York: Basic Books; 1988. [Google Scholar]
- Brown L, Pridham K. The effect of maternal depressive symptoms and early maternal feeding behavior on later infant feeding behavior. Newborn and Infant Nursing Review. 2007;7:56–63. doi: 10.1053/j.nainr.2006.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Champagne FA, Curley JP. How social experiences influence the brain. Current Opinion in Neurobiology. 2005;15:704–709. doi: 10.1016/j.conb.2005.10.001. [DOI] [PubMed] [Google Scholar]
- Chatoor I, Getson P, Menvielle E, Brasseaux C. A feeding scale for research and clinical practice to assess mother-infant interactions in the first three years of life. Infant Mental Health Journal. 1997;18:76–91. [Google Scholar]
- Clark R. The parent-child early relational assessment. A factorial validity study. Emotional and Psychological Measurement. 1999;59:821–846. [Google Scholar]
- Clark R, Hyde JS, Essex MJ, Klein MH. Length of maternity leave and quality of mother-infant interactions. Child Development. 1997;68:364–383. doi: 10.1111/j.1467-8624.1997.tb01945.x. [DOI] [PubMed] [Google Scholar]
- Coyl D, Roggman L, Newland L. Stress, maternal depression, and negative mother-infant interaction in relation to infant attachment. Infant Mental Health Journal. 2002;23:145–163. [Google Scholar]
- Davis L, Edwards H, Mohay H. Mother-infant interaction in premature infants at three months after nursery discharge. International Journal of Nursing Practice. 2003;9:374–381. doi: 10.1046/j.1440-172x.2003.00447.x. [DOI] [PubMed] [Google Scholar]
- DeWitt SJ, Sparks JW, Swank PB, Smith K, Denson SE, Landry SH. Physical growth of low birthweight infants in the first year of life: Impact of maternal behaviors. Early Human Development. 1997;47:19–34. doi: 10.1016/s0378-3782(96)01757-4. [DOI] [PubMed] [Google Scholar]
- Egeland B, Farber EA. Infant-mother attachment: Factors related to its development and changes over time. Child Development. 1984;55:753–771. [PubMed] [Google Scholar]
- Feldman R, Eidelman AI. Neonatal state organization, neuro-maturation, mother-infant interaction, and cognitive development in small-for-gestational-age premature infants. Pediatrics. 2006;118:e869–e878. doi: 10.1542/peds.2005-2040. [DOI] [PubMed] [Google Scholar]
- Forcada-Guex M, Pierrehumbert B, Borghini A, Moessinger A, Muller-Nix C. Early dyadic patterns of mother-infant interactions and outcomes of prematurity at 18 months. Pediatrics. 2006;118:E107–E114. doi: 10.1542/peds.2005-1145. [DOI] [PubMed] [Google Scholar]
- Gewolb IH, Vice FL. Maturational changes in the rhythms, patterning, and coordination of respiration and swallow during feeding in preterm and term infants. Developmental Medicine and Child Neurology. 2006;48:589–594. doi: 10.1017/S001216220600123X. [DOI] [PubMed] [Google Scholar]
- Grych JH, Clark R. Maternal employment and development of the father-infant relationship in the first year. Developmental Psychology. 1999;35:893–903. doi: 10.1037//0012-1649.35.4.893. [DOI] [PubMed] [Google Scholar]
- Harel J, Oppenheim D, Tirosh E. Associations between mother-child interaction and children’s later self and mother feature knowledge. Infant Mental Health Journal. 1999;20:123–137. [Google Scholar]
- Holditch-Davis D, Cox MF, Miles MS, Belyea M. Mother-infant interactions of medically fragile infants and non-chronically ill premature infants. Research in Nursing and Health. 2003;26:300–311. doi: 10.1002/nur.10095. [DOI] [PubMed] [Google Scholar]
- Holditch-Davis D, Miles MS, Belyea M. Feeding and non-feeding interactions of mothers and prematures. Western Journal of Nursing Research. 2000;22:320–334. doi: 10.1177/01939450022044449. [DOI] [PubMed] [Google Scholar]
- Isabella RA. Origins of attachment: Maternal interactive behavior across the first year. Child Development. 1993;64:605–621. doi: 10.1111/j.1467-8624.1993.tb02931.x. [DOI] [PubMed] [Google Scholar]
- MacPhee M, Schneider J. A clinical tool for nonorganic failure-to-thrive feeding interactions. Journal of Pediatric Nursing. 1996;11:29–39. doi: 10.1016/S0882-5963(96)80035-2. [DOI] [PubMed] [Google Scholar]
- Margolin G, Oliver PH, Gordis EB, O’Hearn HG, Medina AM, Ghosh CM, et al. The nuts and bolts of behavioral observation of marital and family interaction. Clinical Child and Family Psychology Review. 1998;1:195–213. doi: 10.1023/a:1022608117322. [DOI] [PubMed] [Google Scholar]
- Mertesacker B, Bade U, Haverkock A, Pauli-Pott U. Predicting maternal reactivity/sensitivity: The role of infant emotionality, maternal depressiveness/anxiety, and social support. Infant Mental Health Journal. 2004;25:47–61. [Google Scholar]
- Osofsky JD. Neonatal characteristics and mother-infant interaction in two observational situations. Child Development. 1976;47:1138–1147. [PubMed] [Google Scholar]
- Osofsky JD, O’Connell EJ. Parent-child interaction: Daughters’ effects upon mothers’ and fathers’ behaviors. Developmental Psychology. 1972;7:157–168. [Google Scholar]
- Price GM. Sensitivity in mother-infant interactions: The AMIS scale. Infant Behavior and Development. 1983;6:353–360. [Google Scholar]
- Pridham KF, Brown R, Clark R, Sondel S, Green C. Infant and caregiving factors affecting weight-for-age and motor development of full-term and premature infants at 1 year post-term. Research in Nursing and Health. 2002;25:394–410. doi: 10.1002/nur.10047. [DOI] [PubMed] [Google Scholar]
- Schore AN. Effects of a secure attachment relationship on right brain development, affect regulation, and infant mental health. Infant Mental Health Journal. 2001;22:7–66. [Google Scholar]
- Singer LT, Fulton S, Davillier M, Koshy D, Salvator A, Baley JE. Effects of infant risk status and maternal psychological distress on maternal-infant interactions during the first year of life. Journal of Developmental and Behavioral Pediatrics. 2003;24:233–241. doi: 10.1097/00004703-200308000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thoyre SM. Challenges mothers identify in bottle feeding their preterm infants. Neonatal Network. 2001;20:41–50. doi: 10.1891/0730-0832.20.1.45. [DOI] [PubMed] [Google Scholar]
- Thoyre SM, Brown RL. Factors contributing to preterm infant engagement during bottle-feeding. Nursing Research. 2004;53:304–313. doi: 10.1097/00006199-200409000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thoyre SM, Carlson J. Occurrence of oxygen desaturation events during preterm infant bottle feeding near discharge. Early Human Development. 2003a;72:25–36. doi: 10.1016/s0378-3782(03)00008-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thoyre SM, Carlson JR. Preterm infants’ behavioural indicators of oxygen decline during bottle feeding. Journal of Advanced Nursing. 2003b;43:631–641. doi: 10.1046/j.1365-2648.2003.02762.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valenzuela M. Maternal sensitivity in a developing society: The context of urban poverty and infant chronic undernutrition. Developmental Psychology. 1997;33:845–855. doi: 10.1037//0012-1649.33.5.845. [DOI] [PubMed] [Google Scholar]
- Vice FL, Gewolb IH. Respiratory patterns and strategies during feeding in preterm infants. Developmental Medicine and Child Neurology. 2008;50:467–472. doi: 10.1111/j.1469-8749.2008.02065.x. [DOI] [PubMed] [Google Scholar]
- Wolf MJ, Koldewijn K, Beelen A, Smit B, Hedlund R, de Groot IJ. Neurobehavioral and developmental profile of very low birthweight preterm infants in early infancy. Acta Paediatrica. 2002;91:930–938. doi: 10.1080/080352502760148667. [DOI] [PubMed] [Google Scholar]


