Abstract
Introduction
Thyroglossal duct cyst carcinomas are extremely rare and their clinical presentation is similar to that of benign cysts. The diagnosis is based on physical examination, laboratory tests, and most importantly multiple imaging techniques (ultrasonography, computed tomography and magnetic resonance imaging), and fine needle aspiration cytology.
Presentation of case
We report a very unusual case of a tall cell variant of papillary carcinoma arising in a thyroglossal duct cyst in association with a follicular variant of papillary microcarcinoma and a tall cell variant of papillary carcinoma arising from the thyroid gland.
Discussion
Although rarely described in the medical literature, ectopic thyroid tissue present in the thyroglossal duct cyst could be involved in the development of a poorly differentiated carcinoma. The frequent observation of an associated primitive thyroid carcinoma makes surgical management of thyroid gland controversial.
Conclusion
For the optimal management of this rare pathological condition, a comprehensive preoperative evaluation and meticulous intra-operative appraisal are fundamental.
Keywords: Thyroglossal duct cyst, Papillary carcinoma, Tall cell carcinoma, Thyroidectomy, Sistrunk procedure
Abbreviations: TDCC, thyroglossal duct cyst carcinoma; US, ultrasonography; CT, computed tomography; MRI, magnetic resonance imaging
Highlights
-
•
TDCCs are uncommon but usually with a good prognosis.
-
•
An association with thyroid primitive carcinoma is frequently observed.
-
•
An extremely rare TDCC variant with a poor prognosis associated with two synchronous foci of thyroid carcinoma is reported.
-
•
Surgical management of the thyroid gland within treatment plan is controversial.
-
•
An accurate preoperative evaluation is mandatory for an optimal management.
1. Introduction
The thyroid gland originates from a median endodermal thickening in the floor of the primordial pharynx at the base of the tongue. This thickening soon becomes a small outpouching that descends into the neck during its maturation. This thyroid primordium is connected to the tongue by the thyroglossal duct a narrow epithelial tube that degenerates and disappears before the definitive development of the thyroid gland. Various thyroid pathologies are known both in thyroid gland and in the ectopic thyroid tissue [1].
The thyroglossal duct cyst is a cystic expansion occurring due to an abnormality in thyroid development resulting from the defective obliteration of the duct during embryogenesis. A persistent thyroglossal duct is usually a benign condition, but in some cases it may undergo dilatation and be responsible for cyst formation, which clinically presents as a mass arising along the thyroglossal tract [2]. This abnormality occurs in around 7% of the population [3] and it represents the most common congenital anomaly of the neck resulting in more than 75% of median neck swellings in childhood. Between 1.5 and 45% of cases show the presence of ectopic thyroid tissue [2,4].
The development of a carcinoma of the thyroglossal duct cysts is rather rare, occurring in approx. 1% of cases. The median age at presentation is 40 years and females are affected more often than men with a 3:2 ratio [5,6]. The peak incidence is in the third decade for women and sixth decade for men and it presents an overall age and sex distribution similar to that of thyroid carcinoma. Regional lymph node metastases are less common in the thyroglossal duct cyst papillary carcinoma compared to a primary cancer of the thyroid, with an incidence <8% [2]. Furthermore, papillary duct cyst carcinoma rarely presents distant metastases and its prognosis is similar to that of the thyroid papillary carcinoma.
The vast majority of thyroid cancers concern papillary carcinomas (79.9%), followed by much fewer cases of follicular or mixed follicular-papillary (9.5%), squamous cell carcinomas (7.6%), anaplastic carcinomas (0.6%), and Hürthle cell carcinomas (0.6%) [7]. No reports of medullary carcinoma exist to date, probably due to the fact that C cells originate from the last pharyngeal pouch, supporting the theory of the primitive genesis of carcinomas arising in ectopic thyroid tissue rather than from the metastatic diffusion of thyroid carcinoma through the thyroglossal duct [8]. On the other hand, a synchronous papillary carcinoma on the thyroglossal duct cyst and on the thyroid gland can be explained as a multi-focus manifestation of the tumor and not as metastatic foci [9]. An association with primitive thyroid papillary carcinoma is observed in about 25–40% of patients undergoing total thyroidectomy as part of their surgical treatment [6,9].
Papillary carcinoma is therefore the most frequent malignancy arising from ectopic thyroid tissue of this remnant; moreover, a tall cell variant is extremely rare and shows a rather poor prognosis. Compared with classical papillary thyroid carcinoma, tall cell variant had a higher rate of extrathyroidal extension (53.6% vs. 30.2%), and a poorer 5-year disease-specific survival (81.9% vs. 97.8%) [10]. Differential diagnosis includes Hürthle cell variant, oncocytic papillary carcinoma and Warthin-like papillary carcinoma [9,11].
To date, only one case of tall cell carcinoma arising in a thyroglossal duct cyst has been reported in the medical literature [11]. Here, we present a remarkable case of tall cell carcinoma arising in a thyroglossal duct cyst associated with a follicular variant of papillary microcarcinoma and a tall cell variant of papillary carcinoma of the thyroid gland.
2. Presentation of case
A 77-year-old Caucasian woman was admitted to our Department with recent onset (2 months) of a median neck swelling.
She did not have any obstructive symptoms, such as dysphagia, dyspnoea, stridor or dysphonia.
The patient had a history of essential hypertension, dyslipidemia and type 2 diabetes mellitus. She had also been hospitalized in the past for a transient ischemic attack.
Physical examination revealed a voluminous swelling of about 8 cm, extending from the hyoid region to the jugular notch and laterally within the anterior margin of the sternocleidomastoid muscle. The swelling was oval in shape and with a smooth surface; it was mobile, firm and painless (Fig. 1).
Fig. 1.

Preoperative image: the large cervical swelling is visible.
Thyroid functional tests (serum thyroxine, triiodothyronine and thyroid stimulating hormone), calcitonin and thyroid antibodies were within normal limits.
A preoperative ultrasound neck evaluation showed a voluminous anterior midline neck mass of about 7–8 cm with an inhomogeneous echostructure and an isoechoic solid component (largest diameter of about 3–4 cm); high intranodular flow by Doppler analysis was associated with an hypoechoic solid nodule at the level of the thyroid isthmus of the thyroid gland with microcalcifications inside. No regional suspect nodes were identified.
The results of fine needle aspiration cytology suggested possible malignancy.
Intralesional thyroglobulin levels were 27.550 ng/ml (normal values: <10 ng/ml).
The patient underwent mass and thyroglossal duct excision and total thyroidectomy. Parathyroid glands and recurrent laryngeal nerves were identified and preserved.
The surgical specimen included a skin lozenge with midline neck mass and the thyroid gland (Fig. 2).
Fig. 2.

Surgical specimen: thyroid, neoplasm, thyroglossal duct along with a lozenge of skin.
Microscopic examination revealed the presence of an infiltrative tall cell variant of papillary carcinoma, arising in the thyroglossal duct cyst in conjuction with a follicular variant of papillary microcarcinoma of the left thyroid lobe and a peri-isthmic tall cell variant of papillary carcinoma (Figs. 3–5). No evidence of cervical lymph node metastases was found.
Fig. 3.
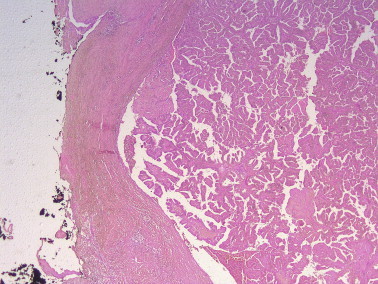
HE x2.5. Panoramic magnification view of the tumor. Papillary architecture. The surgical margin is shown in black.
Fig. 4.
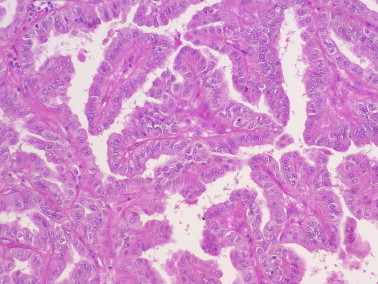
HE x25. Tall cell morphology and papillary architettural pattern.
Fig. 5.
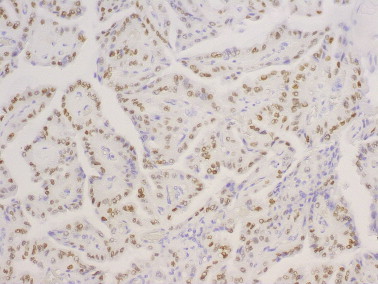
TTF1 x25. Neoplastic cell immunostained for TTF1 (nuclear expression).
The patient then underwent radioiodine ablation therapy (106 mCi).
Thyroglobulin level after radioiodine ablative therapy was <0.20 ng/ml (normal values: 0.73–84.00 ng/ml).
The surveillance work-up performed during the follow-up included thyroglobulin measurements (thyroglobulin: <0.20 ng/ml) and neck ultrasounds (negative). No evidence of persistent, recurrent or metastatic disease was found.
The patient continues to be disease free at 43 months post-surgery.
3. Discussion
Controversies still exist about the pathogenesis, the diagnosis, and the treatment of thyroglossal duct cyst carcinomas. Some authors consider a thyroglossal duct to provide a natural way through which occult tumors can spread and recommend total thyroidectomy with neck dissection, while others consider radical excision as the treatment of choice for thyroglossal duct cyst carcinomas due to its origin [6,12]. The distinction between a primary carcinoma arising in ectopic thyroid tissue and thyroid neoplasm metastasis is often difficult to establish, yet it is crucial to ascertain for the treatment plan.
Preoperative evaluation of thyroglossal duct cyst includes physical examination, imaging studies, and fine needle aspiration cytology. The clinical presentation of thyroglossal duct cyst carcinomas is similar to that of benign thyroglossal duct cysts in terms of growth, localization, size, and consistency. A rapid increase in size or the presence of a firm palpable mass may be signs of malignancy, although definitive diagnosis is made by pathological analysis of the surgical specimen. The role of fine needle aspiration cytology is not always decisive due to inadequate sampling, thus it may only help diagnosis in some cases. On the other hand, imaging studies (US, CT, NMI) can show the lesion characteristics (cystic, solid, capsulated, vascularized) associated with features of invasion, and thus play a crucial role in the diagnosis and preoperative evaluation of the extent of malignancy, helping in its staging and consequently in the treatment plan [13].
In this context, the microscopic evaluation of a surgical specimen plays a crucial role in diagnostic process in order to differentiate carcinomas from benign lesions arising in thyroglossal duct [2].
In addition to diagnostic difficulties, surgical management of the thyroid gland is controversial and the subject of much debate within the international medical community. In the opinion of some authors the Sistrunk procedure would be the treatment of choice for both thyroglossal duct cysts and carcinomas arising in ectopic thyroid tissue without neoplasms in the thyroid gland, followed by strict follow-up consisting essentially in periodic neck ultrasound [3]. Other authors suggest a more aggressive approach associating to Sistrunk procedure a total thyroidectomy followed by radioiodine ablative therapy [3].
The high incidence of associated thyroid carcinoma requires that total thyroidectomy is evaluated as a necessary part of a treatment plan [14–16]. For this reason, a thorough preoperative evaluation of the thyroid gland is crucial, including clinical examination, laboratory tests, ultrasonography and fine needle aspiration cytology.
Although cyst removal by Sistrunk procedure remains the treatment of choice for thyroglossal duct cyst carcinomas, the extent of surgical treatment depends on the degree of tumor involvement as detected during the preoperative evaluation and on the operating table [6].
In the present case, considering the extent of the swelling, the outcome of preoperative ultrasound and the intraoperative appearance of the thyroid, total thyroidectomy was deemed to be the best treatment strategy.
The postoperative treatment plan for the patient required radioiodine ablative therapy as it is taken up by thyroglossal duct remnant tissue and recommended to all patients with thyroglossal duct cyst carcinoma without thyroid gland.
4. Conclusion
This paper reports a rare case of an uncommon variant of papillary carcinoma with a poor prognosis, together with the coexistence of a follicular variant of papillary microcarcinoma and a tall cell variant of papillary carcinoma of the thyroid gland.
For the optimal management of this rare pathological condition, a comprehensive preoperative evaluation and meticulous intra-operative appraisal are fundamental.
Consent
Informed written consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review from the Editor-in-Chief of this journal on request.
Conflict of interest statement
None.
Funding
None.
Ethical approval
The study was approved by ethics committee of the University of Cagliari.
Research registration unique identifying number (UIN)
Researchregistry129.
ISRCTN
None.
Author contribution
Luca Gordini: study design, data interpretation, drafting the article.
Francesco Podda: data collection, data analysis.
Fabio Medas: data collection, data analysis.
Maria Letizia Lai: drafting the article, histopathological analysis.
Alessandro Longheu: data collection, data analysis.
Giuseppe Pisano: revising the article, data analysis.
Pietro Giorgio Calò: study concept, revising the article, operation of the patient.
Guarantor
None.
References
- 1.Fumarola A., Trimboli P., Cavaliere R., Coletta I., Veltri A., Di Fiore A. Thyroid papillary carcinoma arising in ectopic thyroid tissue within a neck branchial cyst. WJSO. 2006;4:24–27. doi: 10.1186/1477-7819-4-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Allard R.H.B. The thyroglossal cyst. Head Neck Surg. 1982;5:134–146. doi: 10.1002/hed.2890050209. [DOI] [PubMed] [Google Scholar]
- 3.Mesolella M., Ricciardello F., Cavaliere M., Iengo M., Galli V., Galli J. Papillary carcinoma arising in a submental-intralingual thyroglossal duct cyst. Acta. Otorhinolaryngol. Ital. 2010;30:313–316. [PMC free article] [PubMed] [Google Scholar]
- 4.Organ G.M., Organ C.H. Thyroid gland and surgery of the thyroglossal duct: exercise in applied embryology. World J. Surg. 2000;24:886–890. doi: 10.1007/s002680010172. [DOI] [PubMed] [Google Scholar]
- 5.Doshi S.V., Cruz R.M., Hilsinger R.L. Thyroglossal duct carcinoma: a large case series. Ann. Otol. Rhinol. Laryngol. 2001;110:734–738. doi: 10.1177/000348940111000807. [DOI] [PubMed] [Google Scholar]
- 6.Asti J., Duskova J., Kraus J., Vicek P., Kodet R., Lastuvka P. Coincidence of thyroid tumor and thyroglossal duct remnants. Review of literature and presentations of 3 cases. Tumori. 2003;89:314–320. doi: 10.1177/030089160308900316. [DOI] [PubMed] [Google Scholar]
- 7.Weiss S.D., Orlich C.C. Primary papillary carcinoma of a thyroglossal duct cyst; report of a case and literature review. Br. J. Surg. 1991;78:87–89. doi: 10.1002/bjs.1800780127. [DOI] [PubMed] [Google Scholar]
- 8.Rossi E.D., Martini M., Straccia P., Cocomazzi A., Pennacchia I., Revelli L. Thyroglossal duct cyst cancer most likely arises from a thyroid gland remnant. Virchows. Arch. 2014;465:67–72. doi: 10.1007/s00428-014-1583-9. [DOI] [PubMed] [Google Scholar]
- 9.Joseph T.J., Komorowski R.A. Thyroglossal duct carcinoma. Hum. Pathol. 1975;6:717–729. doi: 10.1016/s0046-8177(75)80080-3. [DOI] [PubMed] [Google Scholar]
- 10.Morris L.G.T., Shaha A.R., Tuttle R.M., Sikora A.G., Ganly I. Tall cell variant of papillary carcinoma: a matched-pair analysis of survival. Thyroid. 2010;20:153–158. doi: 10.1089/thy.2009.0352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Köybaşioğlu F., Simşek G.G., Onal B.U. Tall cell variant of papillary carcinoma arising from a thyroglossal cyst: report of a case with diagnosis by fine needle aspiration cytology. Acta. Cytol. 2006;50:221–224. doi: 10.1159/000325937. [DOI] [PubMed] [Google Scholar]
- 12.Kennedy T.L., Whitaker M., Wadih G. Thyroglossal duct carcinoma: a rational approach to management. Laryngoscope. 1998;108:1154–1158. doi: 10.1097/00005537-199808000-00010. [DOI] [PubMed] [Google Scholar]
- 13.Gebbia V., Di Gregorio C., Attard M. Thyroglossal duct cyst carcinoma with concurrent thyroid carcinoma: a case report. JMCR. 2008;2:132–135. doi: 10.1186/1752-1947-2-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Calò P.G., Medas F., Loi G., Erdas E., Pisano G., Nicolosi A. Differentiated thyroid cancer in the elderly: our experience. Int. J. Surg. 2014;12(Suppl. 2):S140–S143. doi: 10.1016/j.ijsu.2014.08.362. [DOI] [PubMed] [Google Scholar]
- 15.Calò P.G., Medas F., Pisano G., Boi F., Baghino G., Mariotti S. Differentiated thyroid cancer: indications and extent of central neck dissection-our experience. Int. J. Surg. Oncol. 2013;2013:625193. doi: 10.1155/2013/625193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Calò P.G., Pisano G., Medas F., Marcialis J., Gordini L., Erdas E. Total thyroidectomy without prophylactic central neck dissection in clinically node-negative papillary thyroid cancer: is it an adequate treatment? World J. Surg. Oncol. 2014;12:152. doi: 10.1186/1477-7819-12-152. [DOI] [PMC free article] [PubMed] [Google Scholar]


