Summary
Lysosomal α-galactosidase A (α-Gal) is the enzyme deficient in Fabry disease (FD), an X-linked glycosphingolipidosis caused by pathogenic mutations affecting the GLA gene. The early-onset, multi-systemic FD classical phenotype is associated with absent or severe enzyme deficiency, as measured by in vitro assays, but patients with higher levels of residual α-Gal activity may have later-onset, more organ-restricted clinical presentations.
A change in the codon 118 of the wild-type α-Gal sequence, replacing basic arginine by a potentially sulfhydryl-binding cysteine residue – GLA p.(Arg118Cys) –, has been recurrently described in large FD screening studies of high-risk patients. Although the Cys118 allele is associated with high residual α-Gal activity in vitro, it has been classified as a pathogenic mutation, mainly on the basis of theoretical arguments about the chemistry of the cysteine residue. However its pathogenicity has never been convincingly demonstrated by pathology criteria.
We reviewed the clinical, biochemical and histopathology data obtained from 22 individuals of Portuguese and Spanish ancestry carrying the Cys118 allele, including 3 homozygous females. Cases were identified either on the differential diagnosis of possible FD manifestations and on case-finding studies (n=11; 4 males), or on unbiased cascade screening of probands’ close relatives (n=11; 3 males). Overall, those data strongly suggest that the GLA p.(Arg118Cys) variant does not segregate with FD clinical phenotypes in a Mendelian fashion, but might be a modulator of the multifactorial risk of cerebrovascular disease, since the allelic frequency in stroke patients was 0.0087 (p=0.0185 vs the general population). The Cys118 allelic frequency in healthy Portuguese adults (n=696) has been estimated as 0.001, therefore not qualifying for “rare” condition.
Keywords: Fabry disease, α-galactosidase A, GLA gene, variant p.(Arg118Cys)
1. Introduction
Alpha-galactosidase A (α-Gal; EC 3.2.1.22), the lysosomal hydrolase deficient in Fabry disease (FD, OMIM #301500), is a homodimeric glycoprotein encoded by the GLA gene, which is located on the long arm of the X chromosome [1–3]. Decreased α-Gal activity in humans leads to accumulation of neutral glycosphingolipids (GSL) with terminal α-galactosyl residues, predominantly globotriaosylceramide (Gb3 or GL-3), in many different types of cells and in body fluids. The severity of the clinical phenotype in affected males is broadly related to residual α-Gal activity: the lower the enzyme activity, the earlier is the age of onset, and more severe and multi-systemic are the clinical manifestations. In classic FD, caused by complete absence or marked deficiency of α-Gal activity, the vascular endothelium and smooth muscle cells, the peripheral and autonomic nervous systems, the kidneys, the heart and the brain are major sites of pathology, and the affected males usually become symptomatic during childhood or adolescence [1, 3]. In patients with higher levels of residual α-Gal activity, the resultant phenotypes are more organ-restricted, usually to the heart, and have a much later clinical onset, frequently in mid-adulthood [3]. Like other X-linked genetic disorders, males with FD are more severely affected than females, many of whom have limited organ involvement or remain asymptomatic, although a few may in rare instances express the severe phenotype of the disease [4].
More than 750 different pathogenic GLA mutations are reported in “The Human Gene Mutation Database (HGMD®)” [http://www.hgmd.cf.ac.uk/ac/gene.php?gene=GLA, last accessed on August 1, 2014], of which about 2/3 are missense or nonsense point mutations. Most of the pathogenic GLA mutations are private to single families [5].
The mature α-Gal monomers have 12 cysteine (Cys) residues, at positions 52, 56, 63, 90, 94, 142, 172, 174, 202, 223, 378, 382 in the polypeptide chain [2]. Five disulfide bonds, between cysteine residues at positions 52–94, 56–63, 142–172, 202–223 and 378–382, are important for the stabilization of the three-dimensional structure of the enzyme; furthermore, the 142–172 disulfide contributes to the α-Gal catalytic site. The Cys90 and Cys174 residues are unpaired. An additional cysteine (Cys12) is removed from the monomer during the post-translational enzyme maturation, as part of the signal peptide.
Missense mutations affecting any one of the cysteines that form the disulfide bonds of the wild-type α-Gal structure are associated with the classic FD phenotype, and show negligible or very low residual enzyme activity [6–24], attesting their importance for normal enzyme function. Missense mutations involving the Cys12 or Cys90 residues have never been reported in FD patients. So far, two missense variants have been described that affect GLA Cys174, respectively changing the wild-type cysteine to arginine (Arg) or glycine (Gly) [http://www.hgmd.cf.ac.uk/ac/gene.php?gene=GLA, http://www.genomed.org/lovd2/variants.php?select_db=GLA&action=view_all, last accessed on August 1, 2014]. While mutation p.(Cys174Arg) is reportedly associated with classic FD [25], p.(Cys174Gly) is still classified as a single nucleotide polymorphism (SNP) at the Short Genetic Variations database (dbSNP) of the National Center for Biotechnology Information (NCBI; National Library of Medicine, Bethesda, MD, USA; http://www.ncbi.nlm.nih.gov/projects/SNP/snp_ref.cgi?rs=181562693, last accessed on August 1, 2014]. However, GLA p.(Cys174Gly) has recently been identified in a patient presenting with an unusual late-onset renal variant of FD [26], raising doubts about its clinical benignity [27].
Several missense mutations that introduce an extra cysteine into the amino acid sequence of α-Gal have been identified in FD patients. As the additional thiol can interfere with the correct formation of the 5 disulfide bonds critical to the α-Gal structure, such mutations are theoretically severe and expected to lead to classic FD. However, by comparison with mutations substituting other amino acids at the same positions (Table 1), it seems more likely that the functional impact of these mutations depends more on their location on the three-dimensional structure of the protein than on the specific amino acid change.
Table 1.
List of GLA gene mutations in amino acid positions where mutations to cysteine have also been reported.
| Amino acid residue position |
Wild-type amino acid |
Clinical phenotype of mutation to cysteine |
Described mutations other than to cysteine |
|---|---|---|---|
| 112 | Arg | Classical | His(a) / Ser |
| 162 | Trp | Classical | Arg |
| 171 | Gly | Classical | Arg / Asp |
| 216 | Tyr | Classical | Asp |
| 226 | Trp | Unknown(b) | Arg |
| 235 | Ser | Classical | Phe |
| 236 | Trp | Classical | Arg / Leu |
| 271 | Gly | Classical | Ser / Val |
| 287 | Trp | Classical | Gly |
| 297 | Ser | Classical | Phe |
| 360 | Gly | Classical | Asp / Ser |
| 363 | Arg | Classical | His |
Amino acid positions in the α-galactosidase A monomer are sequentially counted from the methionine residue coded by the mRNA start codon which, by convention, is numbered as position 1.
Mutation p.(Arg112His) has been consistently associated with late-onset cardiac variant of Fabry disease.
Mutation p.(Trp226Cys) was identified in a 16-year-old boy with the classical phenotype of Fabry disease, segregating in cis with mutation p.(Arg227Ter); as this nonsense mutation is known to cause a severe deficiency of α-galactosidase A activity, leading to classic Fabry disease, the intrinsic severity of the cysteine mutation has not been defined.
Amino acid names are abbreviated according to the three-letter code:
Arg = arginine; Asp = aspartate; Cys = cysteine; Gly = glycine; His = histidine; Leu = leucine ; Phe = phenylalanine; Ser = serine; Trp = tryptophan; Tyr = tyrosine; Val = valine.
A cysteine-involving GLA SNP variant of uncertain pathogenicity (allelic variant of uncertain significance, VUS) results from the cytosine to thymine transition (C>T) at a CpG dinucleotide in codon 118 (c.352C>T), leading to the non-conservative replacement of a basic arginine in the wild-type α-Gal sequence by an uncharged polar, sulfhydryl-containing, cysteine residue — p.(Arg118Cys), or p.R118C in the single letter code. This SNP was originally identified in a Portuguese family [Oliveira JP, poster presentation; 5th European Round Table on Fabry Disease, 2004], but its first description in a peer-reviewed article was with the results of a large-scale Italian newborn screening of FD, published in 2006 [28]. Subsequently, the GLA p.(Arg118Cys) variant was recurrently identified in large FD case-finding studies among patients with stroke, left ventricular hypertrophy (LVH) or on chronic dialysis, carried out in different European populations [29–32] (summarized in Table 2) and in Brazil [33].
Table 2.
Summary of the large Fabry disease case-finding studies among high-risk patient populations which have identified individuals carrying the GLA p.(Arg118Cys) sequence variant. Comparison with the Portuguese general population.
| Study | Location | Disease screened and patient enrollment conditions |
Cohort size and demographic features |
Screening method | Cases found | Reference (year) |
|---|---|---|---|---|---|---|
| “General Portuguese population screening” | ||||||
| Portugal | Volunteer medical students, fertile males and bone marrow donors | 696 [M: 360 (52%) / F: 336 (48%)] Age: 18–45y |
Direct sequencing of PCR or RT-PCR products | 1/696= 0.14% M: xy F: xy |
Present publication | |
| “Screening genetic conditions in Portuguese young stroke patients –PORTYSTROKE” | ||||||
| Portugal | Stroke Age range: 18–55y (first stroke, incident, unselected) |
493 [M: 300 (61%) / F: 193 (39%)] Mean age: 45y |
Direct sequencing of PCR or RT-PCR products | 6/493= 1.22% M: 46y, 45y, 42y F: 40y, 39y, 33y |
[29] 2010 |
|
| Screening for Fabry Disease among patients undergoing hemodialysis in Spain | ||||||
| Spain | ESRD/HD (prevalent, unselected) |
911 [M: 543(60%) / F: 368(40%)] Mean ages: M = 66y /F = 67y |
DBS α-Gal assay;cut-off for genetic analyses: M <48%(N) / F <80%(N) →DHPLC / GLA variants confirmed on direct sequencing of PCR products | 4/911= 0.44% M: 83y, 72y F: 50y, 47y |
[30] 2010 |
|
| “European Anderson-Fabry Disease survey” | ||||||
| Europe | Unexplained LVH (LVWT ≥15mm) Age: M >35y / F >40y (prevalent) |
1386 [M: 886 (64%)/F: 500 (36%)] Mean age: 58y |
DHPLC / GLAvariants confirmed on direct sequencing of PCR products | 1/1386= 0.07% F: 45y |
[31] 2011 |
|
| “Stroke in Young Fabry Patients – SIFAP” | ||||||
| Europe (mainly northern and central European countries) | Stroke Age range: 18–55y (incident, unselected) |
5023 [M: 2962 (59%)/ F: 2061 (41%)] Median age: 46y |
Direct sequencing of PCR products | 1/5023= 0.02% (*) |
[32] 2013 |
|
GLA: α-galactosidase A gene; α-Gal: α-galactosidase A.
ESRD/HD: end-stage renal disease on hemodialysis. LVH: left ventricular hypertrophy; LVWT: left ventricular wall thickness.
M: male / F: female; y: age in years.
presumably only one case, but no demographic or clinical details were reported.
PCR: polymerase chain reaction; RT-PCR: reverse transcription polymerase chain reaction. DHPLC: denaturing high performance liquid chromatography, used for first-tier rapid mutation screening. DBS: dried blood spot on filter paper.%(N):percent of the normal mean.
Molecular modeling (Figure 1) showed that GLA Cys118 does not alter the active site of the enzyme, therefore not interfering with its catalytic mechanism, and can be accommodated within the crystal structure of the α-Gal protein [28]. These data are comparable to those of other GLA mutations associated with later-onset FD phenotypes and led to the prediction that the α-Gal p.(Arg118Cys) might have altered stability, making it a potential candidate for rescue by pharmacological chaperones. In COS-7 cells transiently transfected with a mutant GLA Cys118 cDNA construct, the intracellular α-Gal residual activity was 29% of the mean transiently expressed Arg118 wild-type activity, increasing 1.1 fold following incubation with the chaperone deoxygalactonojirimycin (DGJ) [28]. Notably, the α-Gal p.Arg118Cys response to incubation with DGJ was several orders of magnitude lower than structurally similar GLA mutations and merely 5% more than the wild-type enzyme.
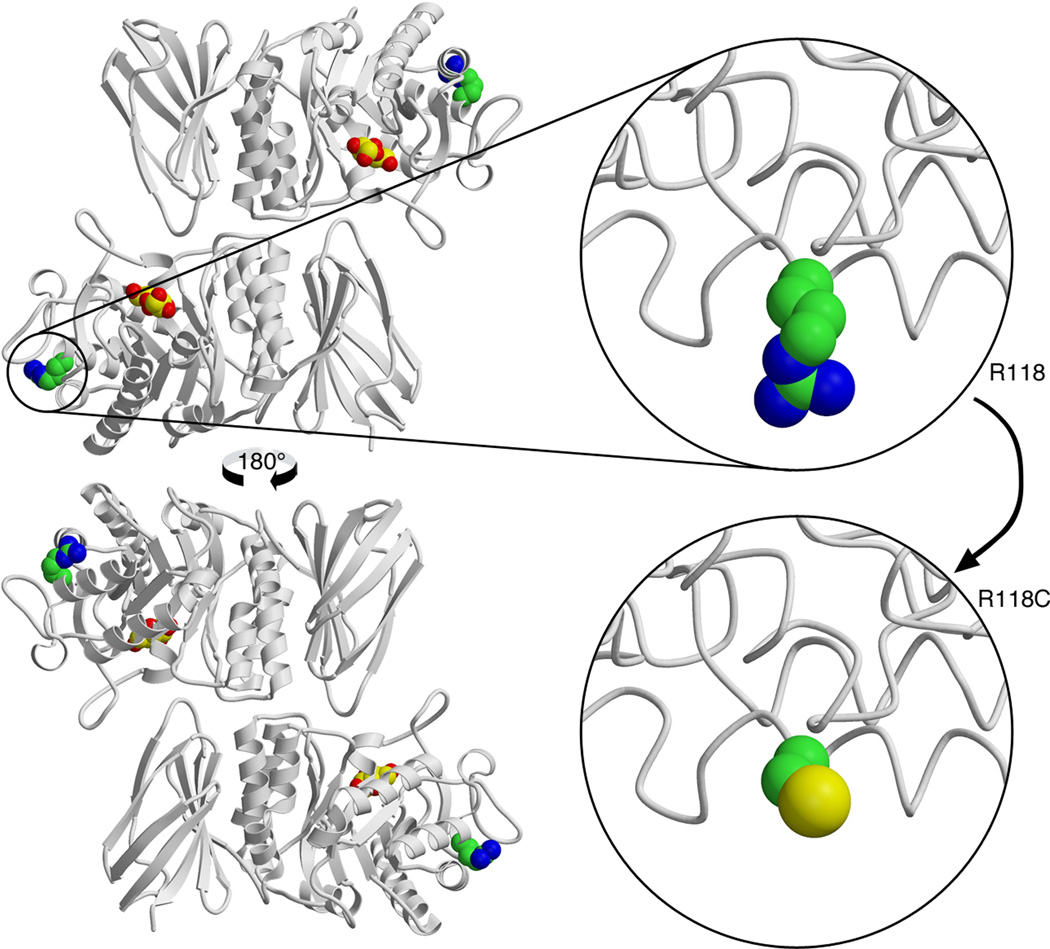
Figure 1.
Molecular structure of the wild-type mature human α-galactosidase A enzyme and modeling of the p.(Arg118Cys) variant: the change to cysteine is easily accommodated in the three-dimensional structure of the enzyme because the arginine is a surface residue and there is plenty of room to substitute the cysteine side chain. However, the cysteine side chain has different chemistry, which can interfere with the correct folding of the disulfide bonds required for the structure, or it could interfere with the binding of other molecules – like the chaperones BiP (binding immunoglobulin protein) and calnexin –, that are required for the folding and trafficking of the α-galactosidase A the lysosome. The structural prediction is that the protein should be active when it folds, but the efficiency of folding and trafficking will be reduced. This is consistent with the results of in vitro overexpression experiments [28].
At the dbSNP GLA c.352C>T is identified as a single nucleotide variation of uncertain clinical significance [http://www.ncbi.nlm.nih.gov/projects/SNP/snp_ref.cgi?rs=148158093, last accessed on August 1, 2014], with conflicting clinical data provided by different submitters. The frequency of the minor allele in the North-American population is estimated as 0.001 [https://esp.gs.washington.edu]. On bioinformatic analyses with different softwares, GLA p.Arg118Cys is predicted to be a “polymorphism” by MutationTaster [http://www.mutationtaster.org/], “benign” by PolyPhen-2 [http://www.mutationtaster.org/] and “deleterious” by SIFT [http://sift.jcvi.org/], whereas Panther scores [http://www.pantherdb.org/tools/csnpScore.do] are marginally suggestive that it may have a deleterious effect on protein function. It is of note that another mutation at the same codon, leading to the replacement of arginine by histidine (His), p.(Arg118His), is uniformly predicted to be non-pathogenic.
Because of the ascertainment bias inherent to genetic screenings of high-risk patient cohorts, cascade family studies and careful clinical evaluation of unbiasedly diagnosed subjects are an important approach for the elucidation of the actual contribution of VUS to human disease. Herein, we report the clinical phenotypes observed in a series of individuals and families of Iberian (Portuguese and Spanish) ancestry carrying the GLA Cys118 allele, and genetic epidemiology data collected in the Portuguese population.
2. Patients, Materials and Methods
Portuguese and Spanish individuals carrying the GLA Cys118 variant allele, as well as a Portuguese family emigrated in France, were identified either (i) on the differential diagnostic workup of individual patients presenting with possible clinical manifestations of FD; (ii) on systematic screenings of large cohorts of patients at high-risk for FD carried out in Portugal and Spain; and (iii) on cascade genetic screening of probands’ close relatives (including a patient identified through screening for FD in a cohort of patients with hypertrophic cardiomyopathies in France). The relevant demographic, clinical, laboratory and imaging data were retrospectively collected by systematic review of existing medical records. Particular attention was specifically paid to possible manifestations of FD, including dermatological (e.g., hypohidrosis, angiokeratomas), neuropathic (e.g., acroparesthesias), ophthalmological (e.g., cornea verticillata, conjunctival and retinal vascular abnormalities), cerebrovascular (e.g. transient ischemic attack, stroke, brain imaging abnormalities), cardiac (e.g., arrhythmias, LVH, ischemic heart disease) and renal (e.g., proteinuria, azotemia). Representative pathology illustrations were prepared from archive tissue biopsies and electron micrographs.
Plasma Gb3 concentration was estimated by a densitometric method, following thin-layer chromatography separation. To determine the Gb3/sphingomyelin molar ratio in the urinary sediment, Gb3 and sphingomyelin were quantified densitometrically after high-performance thin-layer chromatography, in centrifuged urine samples. Urinary Gb3 was measured by high-performance liquid chromatography (LC) coupled to tandem mass spectrometry (MS/MS), and lyso-Gb3 in plasma and urine samples were measured by ultra-performance LC-MS/MS, working in positive electrospray ionization mode.
The DXS8020, DXS8034, DXS8089, DXS8063 and DXS8096 microsatellite sequence-tagged sites (STS), spanning ≈3cM around the GLA gene, were used for haplotyping. Briefly, the relevant STS were amplified in two multiplex polymerase chain reactions (PCR) with 6-FAM™ fluorescent dye-labeled forward primers (Thermo Fisher Scientific; Waltham, MA, USA), according to their annealing temperatures, and the corresponding PCR amplicons were analyzed with an ABI 3500 Genetic Analyzer (Applied Biosystems, Life Technologies; Foster City, CA, USA), using the GeneMapper® software version 4.1 (Applied Biosystems).
A commercial multiplex-ligation probe amplification kit (SALSA MLPA P159-A3 GLA probemix; MRC-Holland; Amsterdam, the Netherlands) was used to screen for GLA gene duplications/deletions in females carrying the GLA Cys118 allele in apparent homozygosity. Statistical analyses were carried out with GraphPad Prism, version 5.0 (GraphPad Software, Inc.; La Jolla, CA, USA).
3. Results
3.1. Clinical data from the original patient and family
We have first identified GLA p.(Arg118Cys) on the genetic workup of a 26-year-old female who had been referred to the Dermatology clinic with an extensive, symmetrically distributed eruption of angiokeratomas in the buttocks and proximal thighs (Figure 2a), that she reported to have initially noticed four years before (clinical details published elsewhere) [34]. The clinical diagnosis of Fabry angiokeratomas was further supported by the light-microscopy (LM) findings on a biopsy of the affected skin (Figure 2b). The α-Gal A activity was within the normal control values, both in leukocytes (44 nmol/h/mg; normal range: 36–80) and in plasma (12.8 nmol/h/ml; normal range: 6.2–19.4), but the Gb3 concentration was slightly elevated in plasma (15.02 µg/ml; normal range: 0.67–10.66).
Figure 2.
A.
Detail of the eruption of angiokeratomas observed in a 26-year-old woman heterozygous for the GLA p.(Arg118Cys) sequence variant. The angiokeratomas localized exclusively to the buttocks and proximal thighs and had a symmetrical distribution. This patient was the proband of the first Portuguese family in whom the GLA p.(Arg118Cys) variant was identified.
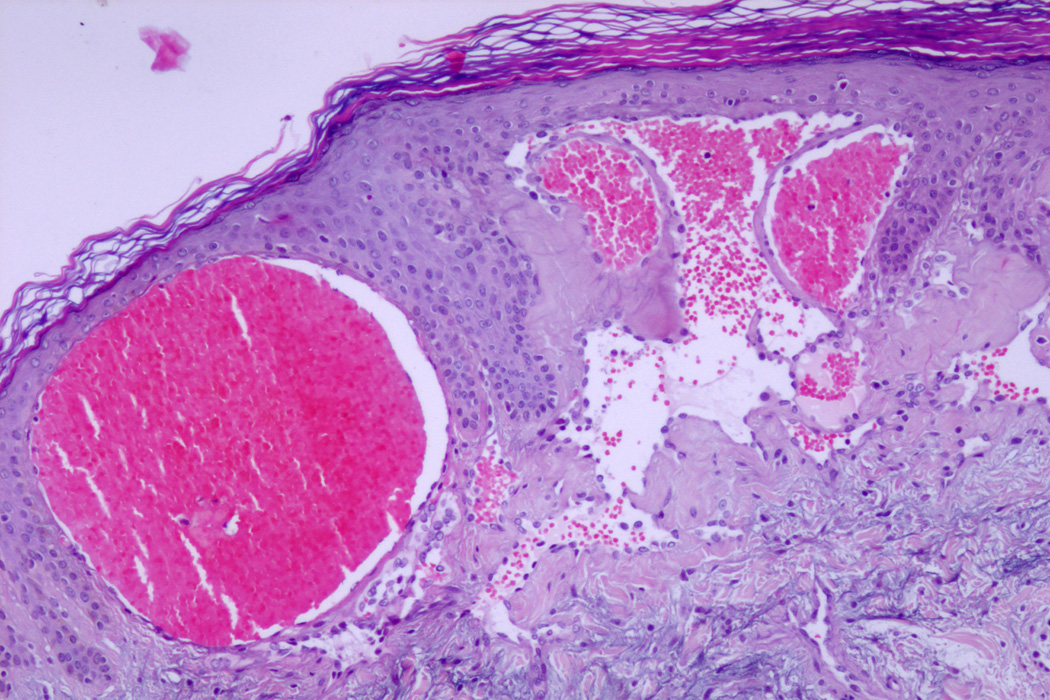
B.
Light-microscopy histopathology of the skin biopsy obtained from that patient. There is subepidermal proliferation of telangiectatic vessels lined by thin endothelial cells and surrounded by collarettes of thickened rete ridges. The dilated vascular spaces are filled with blood or thrombosed. The corneal layer is moderately thickened, showing mild parakeratosis.
The patient additionally reported a 13-year-long history of steroid-resistant nephrotic syndrome but she had remained normotensive, her serum creatinine (sCr) was within the normal (0.68 mg/dl) and examination of the urine sediment was unremarkable. The kidney ultrasound scan showed no abnormalities. The patient specifically denied past history or any current symptoms of neuropathic involvement, of abnormal sweating, and of cardiac or cerebrovascular disease. Slit-lamp ophthalmological examination did not reveal the corneal dystrophy or the conjunctival and retinal microvascular lesions typical of classical FD. The electrocardiogram (ECG) showed incomplete right bundle branch block (RBBB) but the echocardiogram was normal.
At age 13 years, the diagnostic workup for causes of secondary nephrotic syndrome had been negative. The kidney biopsy disclosed a mesangial proliferative glomerulonephritis, with no immune deposits visible on immunofluorescence microscopy. The baseline glomerular ultrastructural pathology could not be examined due to the lack of glomeruli on the sample processed for electron microscopy (EM) study. Since the nephrotic syndrome did not respond to standard immunosuppressive protocols, non-specific treatment with an angiotensin converting enzyme inhibitor (ACEi), with dose titrated according to proteinuria.
Considering the possibility of having missed the diagnosis of FD nephropathy on the LM examination of the first kidney biopsy, and the theoretical hypothesis of unilateral or focal kidney involvement, Gb3/sphingomyelin concentration ratio in a voided bladder urine specimen and in specimens collected from each of the ureters, with no evidence of increased urinary Gb3 excretion (bladder <0.01, left kidney <0.01, right kidney =0.04; normal controls <0.3). A second kidney biopsy was eventually obtained at age 29 years, from the right kidney. On LM examination, the renal pathology was similar to that described in the first biopsy. In addition, the toluidine blue-stained semi-thin scout sections for EM did not show any GSL inclusions, and no “myelin figure” and/or “zebra body” deposits that might be suggestive of FD nephropathy could be identified on the ultrastructural examination. On retrospective immunohistochemical study of this kidney biopsy with a murine anti-Gb3 antibody, Gb3 immunoreactivity was identified only in a few tubular cells, which is a staining pattern similar to that observed in the kidney tissue of control subjects [35]. At age 37 years, the plasma lyso-Gb3 and the urinary Gb3 levels remained within normal range.
Family screening showed the patient had inherited the GLA Cys118 allele from her father and that none of her father’s two brothers and two sisters who were still alive and accepted to be genotyped carried the variant allele; two of her father’s sisters had died during childhood and an older brother had died in his early eighties. Neither of these, nor the remaining brother who was not genotyped, had any clinical manifestations of FD. The proband’s paternal grandmother had died in the late 8th decade, possibly from complications of type 2 diabetes mellitus (DM2). Four of the proband’s 5 living paternal uncles and aunts, as well as her grandfather, also had history of DM2.
The proband’s father was initially evaluated at age 55 years and reported the following major medical problems: (i) DM2 diagnosed at age 39 years; (ii) hypertension, on treatment with an ACEi since age 51 years; (iii) mild mixed hyperlipidemia; (iv) long-lasting history of chronic alcohol abuse, with alcoholic liver disease confirmed on a liver biopsy at age 51 years; (v) bilateral carpal tunnel syndrome, confirmed on electromyography. He also had history of sinus bradycardia, first detected on a routine ECG obtained at age 40 years. About 5 years later he was evaluated at the cardiology clinic for the persistence of sinus bradycardia and newly diagnosed complete RBBB, but was eventually discharged because no evidence of an underlying cardiac pathology could be found.
An echocardiographic study performed at age 56 years showed mild LVH, with interventricular septal thickness of 13 mm and posterior wall thickness of 12 mm, and with a transvalvular mitral flow pattern suggestive of diastolic dysfunction. Results of exercise stress ECG testing and 24-hour continuous ambulatory ECG monitoring were unremarkable. A cardiac biopsy was obtained for differential diagnosis of LVH: although the myocardial tissue appeared histologically normal, without hypertrophy or vacuolization of cardiomyocytes and with no interstitial fibrosis, the EM examination showed small myelin figures within rare cardiomyocytes (Figure 3). He had no history of clinical manifestations of classical FD, including angiokeratomas, childhood-onset acroparesthesias or hypohidrosis, and the slit-lamp ophthalmological examination was normal. His baseline sCr was normal (0.79 mg/dl), the urinalysis did not show proteinuria or abnormalities of the urinary sediment, and a kidney ultrasound scan was unremarkable. The α-Gal activity was within the low-normal range, both in leukocytes (25 nmol/h/mg; normal range: 22–73) and in plasma (3 nmol/h/ml; normal range: 2.0–21.0). The plasma lyso-Gb3 and the urinary Gb3 levels, measured at age 64 years, were within the normal range.
Figure 3.
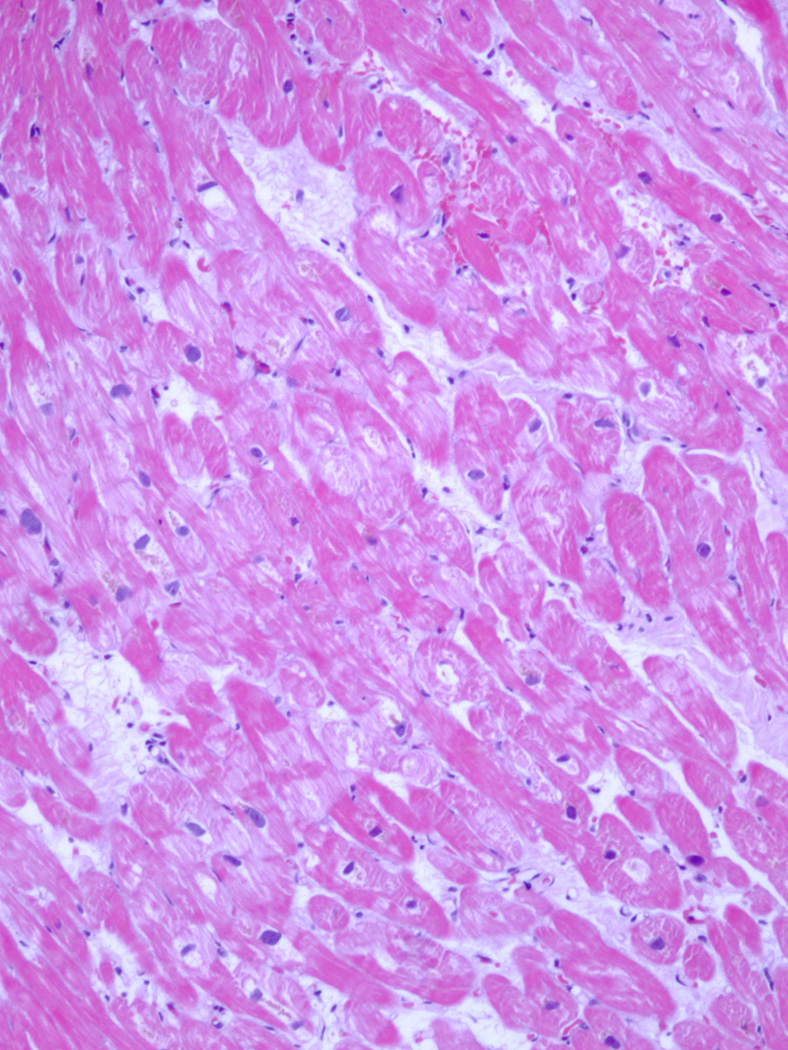
A.
Light microscopy of an endomyocardial biopsy taken from the right ventricle of a 56-year-old man hemizygous for the GLA p.(Arg118Cys) sequence variant. None of the typical features of Fabry disease cardiomyopathy – e.g. cardiomyocyte hypertrophy or vacuolation, enlarged nuclei or fiber branching and disarray –, are observed in this section.
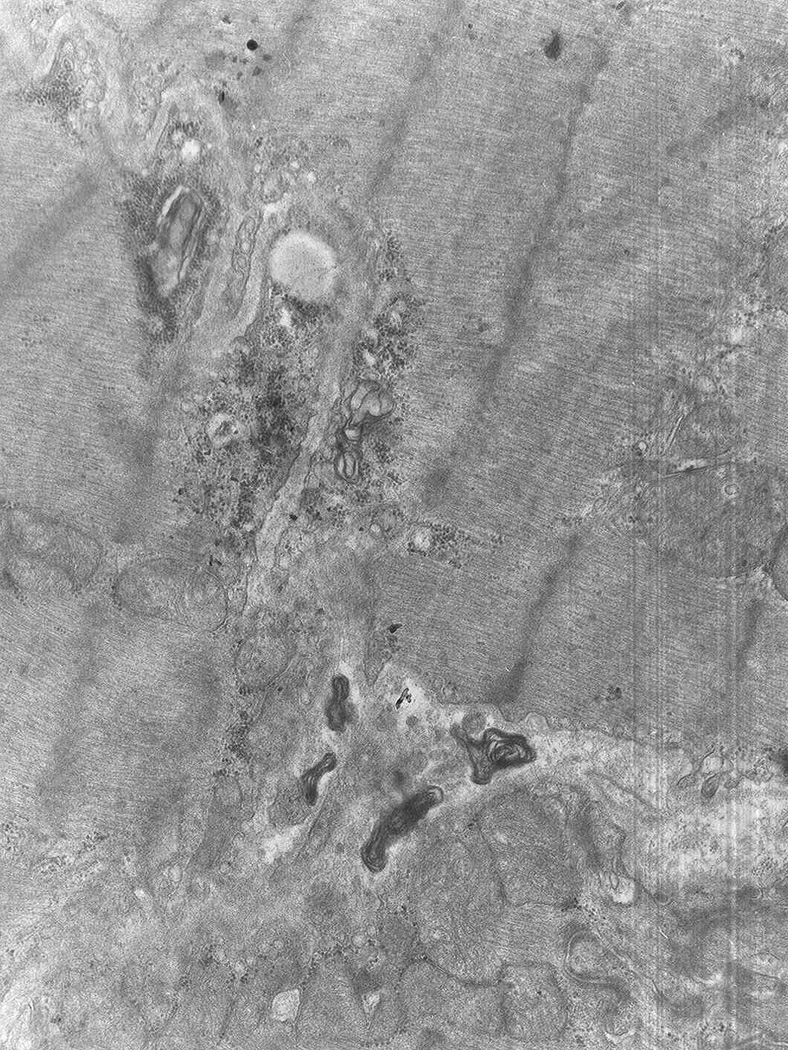
B.
An electron microphotograph of the endomyocardial biopsy of the same patient also does not show any cardiomyocyte inclusions typical of Fabry disease, i.e. with the ultrastructural morphology of “zebra body” or “myelin figure”.
Along 10 years of follow-up, neither the proband nor her father had any major clinical events attributable to FD, or evidence of cardiac or renal disease progression. On ACEi treatment, the proband’s urinary albumin/creatinine ratio was <250 mg/g. At the age of 34 years, two small hyperintense foci were visible at left frontal subcortical and right subinsular locations, on a brain magnetic resonance imaging (MRI). Her father’s brain MRI, obtained at age 61 years, showed multiple hyperintense white matter lesions (WML) located to the periventricular area, and in the corona radiata and centrum semiovale.
3.2. Clinical data from the PORTYSTROKE study
Three males and three females carrying the GLA Cys118 allele were identified in the PORTYSTROKE study [29] (Table 2). The mutation screening method in the Portuguese study was by genotyping, and the plasma and leukocyte α-Gal activities were measured as a second step in all patients who carried a GLA gene variant. This was a major difference in comparison to other previous or contemporary large case-finding studies carried out in southern European countries, either in non-selected male neonates [28] or in high-risk patient series [30], that have also identified individuals carrying the p.(Arg118Cys) variant, because the latter have used the αGal activity measured in dried blood spots (DBS) on filter paper as the screening assay, and only those cases with residual enzyme activity below a predefined cut-off level were subsequently genotyped.
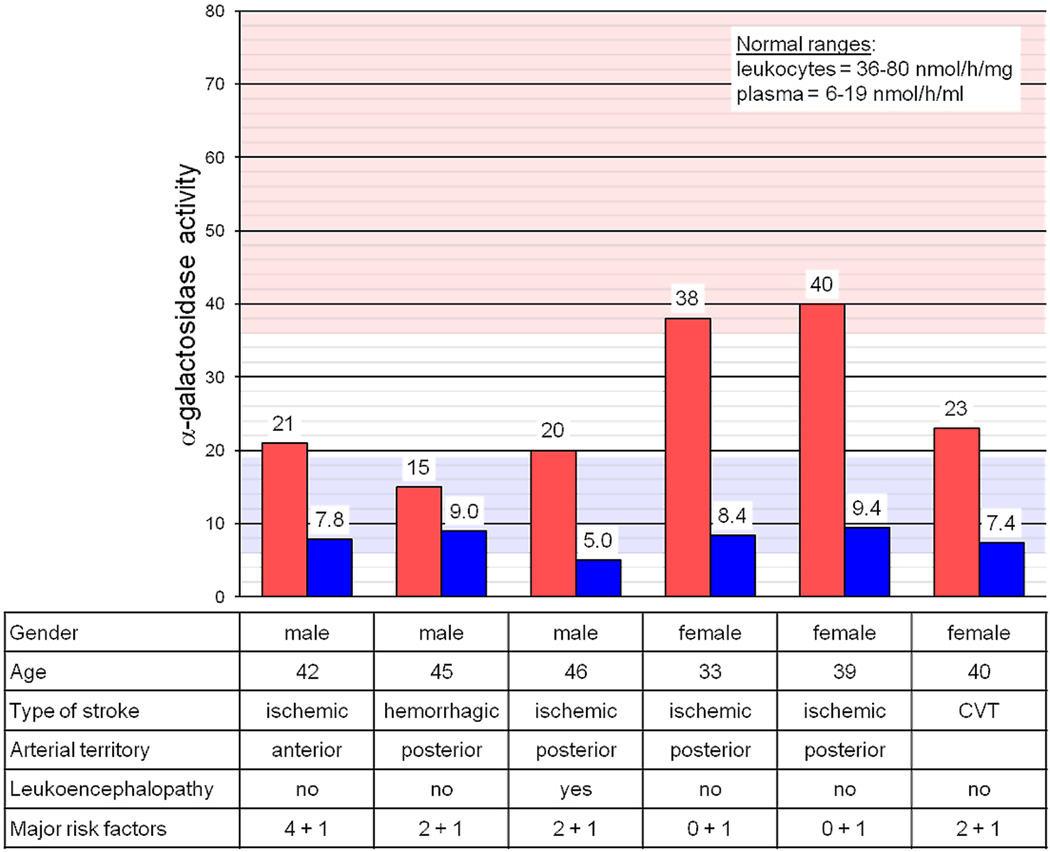
The demographic and clinical features of the 6 patients carrying the Cys118 alelle, and the corresponding results of the α-Gal assays in leukocytes and plasma, are summarized in Figure 4. The average residual leukocyte and plasma α-Gal activities in males and females were, respectively, 18.7 nmol/h/mg (32% of the control mean) and 7.3 nmol/h/ml (58% of the control mean), and 33.7 nmol/h/mg (58% of the control mean) and 8.4 nmol/h/ml (67% of the control mean). Interestingly, the female with the lowest residual leukocyte α-Gal activity (corresponding to ≈60% of the average activity of the other two females) carried the g.1170C>T/c.10C>T SNP of the GLA 5’-untranslated region (5’UTR), which is known to be associated with lower α-Gal activity levels in leukocytes [36, 37].
Figure 4.
Demographic and clinical features of the 6 stroke patients carrying the GLA p.(Arg118Cys) sequence variant that were identified in the PORTYSTROKE study, together with corresponding results of α-galactosidase A assays in leukocytes and plasma.
The pink and light-blue background areas are the normal reference ranges, respectively for the leukocyte and the plasma α-galactosidase A assays.
The numbers of major risk factors for stroke that coexisted in each patient are presented as follows: hypertension, hyperlipidemia, diabetes mellitus and smoking are summed up before and alcohol consumption and oral contraception are summed up after the plus sign.
CVT: cerebral venous thrombosis.
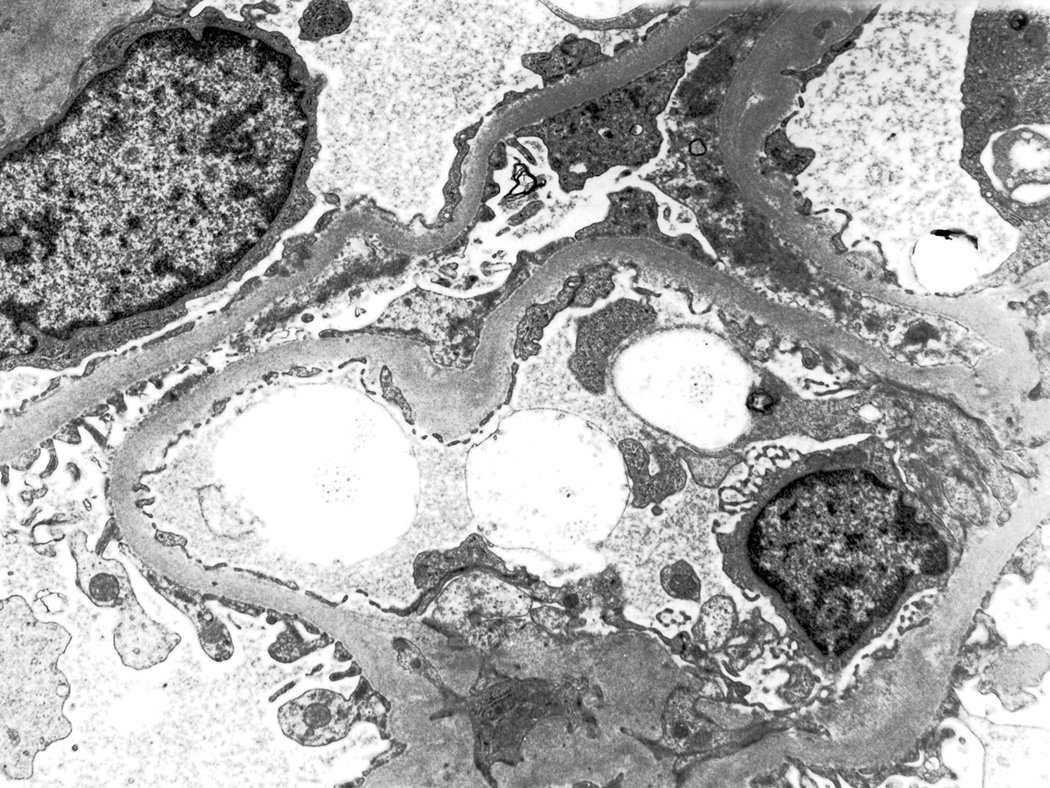
All the males had multiple major cardiovascular risk factors. The youngest of them, who had DM2 and presented mild proteinuria, underwent a kidney biopsy to exclude Fabry nephropathy: LM examination was diagnostic of diabetic nephropathy and the EM study did not show any typical GSL inclusions (Figure 5). None of the three male probands showed LVH on echocardiographic examination. None of the patients had family history suggestive of FD but the two females presenting with ischemic stroke had family histories of stroke. Three of the families were referred for genetic screening of the proband’s living first-degree relatives. Maternal inheritance was confirmed in the two families where the proband’s parents were available for genotyping: the two transmitting mothers of the GLA Cys118 allele were in good health, respectively at ages 70 and 69 years, with no clinical manifestations attributable to FD. AO: specify whether serum creatinine, albuminuria, ECG, echocardiogram, brain MRI normal or not performed.
Figure 5.
Electron micrograph of the kidney biopsy of a 42-year-old man with type 2 diabetes mellitus, hemizygous for the GLA p.(Arg118Cys) sequence variant, identified in the PORTYSTROKE study. The patient presented with mild proteinuria and a kidney biopsy was obtained for the differential diagnosis with diabetic nephropathy. Light microscopy examination was diagnostic of diabetic nephropathy and the electron microscopy study did not show any intracellular inclusions with the “zebra body” or “myelin figure” morphology, typical of Fabry disease nephropathy.
3.2.1. Post-hoc epidemiological analyses of the PORTYSTROKE patient cohort
By screening DNA samples of 360 males and 336 females, aged 18–45 years, from healthy cohorts of volunteer medical students, fertile males and bone marrow donors, the 95% confidence interval (95% CI) for the allelic frequency of GLA Cys118 in the general Portuguese population was estimated between <0.0001–0.006. As compared to the control population, the allelic frequency of the GLA Cys118 allele was significantly higher among the stroke patients, irrespective of gender (=0.0087, 95% CI: 0.004–0.019; Fisher’s exact test, p=0.0185).
However, when the PORTYSTROKE patients aged 45 years or less (n=204; 118 males) were entered as cases in a pair-matched case-control analysis, with healthy adult bone marrow donors used as gender- and age-matched controls, the estimated odds ratio (OR) for the risk of stroke among carriers of GLA Cys118 did not reach statistical significance (OR = 5.0, 95%CI: 0.56–236.5; McNemar’s test, p=0.22).
Remarkably, the frequency of the GLA c.937G>T SNP, that causes the replacement of aspartic acid (Asp) by tyrosine (Tyr) in codon 313 – i.e., p.(Asp313Tyr) or D313Y, which has been characterized as a non-pathogenic allele, causing a ”pseudodeficiency” of α-Gal activity in plasma [21] –, was significantly higher among male stroke patients than in controls (≈0.009 versus ≈0.002; Fisher’s exact test, p=0.026). Also of note is the observation that the minor allelic frequencies (MAF) of GLA p.(Arg118Cys) and p.(Asp313Tyr) in the general Portuguese population did not significantly differ (1/1032 versus 2/1032; Fisher’s exact test, p=1.0).
3.3. Clinical study of a Portuguese family emigrated in France
An asymptomatic 54-year-old male of Portuguese ancestry was serendipitously found to carry the GLA Cys118 allele, on cascade screening of first-degree relatives of a 59-year-old male diagnosed with FD-associated hypertrophic cardiomyopathy (HCM). The proband had been identified in a French case-finding study of incident patients with LVH of unknown cause [38], using DBS α-Gal activity as the screening method, and was subsequently shown to be hemizygous for the GLA mutation c.337T>C, that changes the translation of codon 113 from phenylalanine (Phe) to leucine (Leu) – i.e., p.(Phe113Leu) –, known to be associated with the cardiac variant of FD [2]. Genotyping of a proband’s younger brother, presenting the unusual value of 45% residual α-Gal activity in the leukocyte enzyme assay, unexpectedly revealed that he did not carry the p.(Phe113Leu) mutation but instead was hemizygous for of the GLA p.(Arg118Cys) variant.
This individual reported no past medical history or current symptoms of FD. On physical examination, there were no angiokeratomas or cornea verticillata. The sCr level was within the normal range, with an estimated glomerular filtration rate (GFR) of 96 ml/min/1.73m2 [CKD-EPI equation; http://www.kidney.org/professionals/kdoqi/gfr_calculator.cfm], and the urinalysis did not reveal proteinuria AO: be more specific? urinary albumin/creatinine ratio was <30 mg/g?. Additional diagnostic workup included brain MRI, on which neither lacunar infarction nor hyperintense WML were found; cardiac MRI, which showed a left ventricle of normal thickness, both at the posterior wall (7 mm) and interventricular septum (9 mm); and 51Cr-EDTA radioisotope measurement of GFR, which was normal for age (84 ml/min/1.73m2). On the basis of this diagnostic workup, it was decided not to start enzyme replacement therapy.
The mother of both individuals, who most probably was an obligate compound heterozygote p.(Phe113Leu)/p.(Arg118Cys), has recently passed away at the age of 87 years, in the absence of significant health problems that might be related to α-Gal deficiency.
3.4. The Spanish cohort
The demographic, genetic and clinical features observed in 11 individuals carrying the GLA p.(Arg118Cys) variant, belonging to 4 apparently unrelated Spanish families, are summarized in Table 3. All 4 probands, who were aged between 50 and 82 years, were ascertained on FD screening as a possible cause for left ventricular hypertrophy; remarkably, only one of the probands was a male. A female proband additionally had supraventricular tachycardia, pathological albuminuria and angiokeratoma at age 50, but no histological demonstration of the FD origin of these alterations was available. In two families, cascade genetic screening led to the identification of one male and 6 females in three consecutive generations, who also carried the GLA Cys118 allele. None of these unbiasedly ascertained individuals manifested LVH, proteinuric chronic kidney disease or any other signs or symptoms that, at their age group, might be unequivocally attributable to α-Gal deficiency. Three related women were Cys118/Cys118 homozygotes. Two sisters, respectively aged 60 and 51 years and the third was a cousin, aged 67. The older of the two sisters was started on enzyme replacement therapy following the abnormal result of the 24-hour Holter monitoring and the finding of WML on brain MRI. In the homozygote females, the residual α-Gal activity on the DBS assay ranged between 25–33% of the normal average.
Table 3.
Demographic, genetic and clinical features observed in Spanish individuals carrying the GLA p.(Arg118Cys) variant.
| Family tree entry |
Gender / age (Y) |
α-Gal activity | GLA gene | CNS | Heart | Kidney | Eye | Other symptoms and comorbidities. | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (% normal) DBS / plasma |
R118C | 5’UTR | Brain MRI | LVH | IVS (mm) echo / MRI |
Holter monitoring |
sCr / eGFR |
UACR (mg/g) |
||||
| Family 1 | ||||||||||||
| F1:P (II:1) | M / 51 | 38 / ND | + | WT | Normal | Yes | 15 / 14 | SVPB | 0.8 / 103 | 11 | Normal | No. |
| (I:2) | F / 81 | 77 / 83 | + / − | WT | ND | NA | ND / ND | ND | 0.93 / 58 | 2.8 | Cataracts | Primary biliary cirrhosis. |
| (II:3) | F / 48 | 69 / 39 | + / − | WT | Normal | No | 9 / 8 | Normal | 0.8 / 87 | 4 | NA | Hypohidrosis. Goiter. Hypercholesterolemia. |
| (III:4) | F / 15 | 64 / 74 | + / − | WT | ND | NA | ND / ND | ND | 0.7 / 130 | 1.9 | NA | |
| Family 2 | ||||||||||||
| F2:P | F / 50 | 50 / 46 | + / − | WT | ND | Yes | 18 / 15 | SVT | 1.2 / 53 | 486.3 | NA | Angiokeratoma. Hypertension. |
| Family 3 | ||||||||||||
| F3:P (II:1) | F / 55 | 100 / 37 | + / − | WT | Normal | No | 8 / 15.5 | Normal | 0.84 / 78 | 0.3 | NA | Depression. Limb pain. Dyspnea, palpitations; cardiac catheterization at age 53Y, with no evidence of CAD. |
| Family 4 | ||||||||||||
| F4:P (II:5) | F / 82 | 55 / ND | + / − | ND | Cerebral small vessel disease | Yes | 16 / ND | Pacemaker (AV block) | 1.7 / 28 | ND / (uPr = 300 mg/dl) | NA | Orthopnea (NYHA, stage 2). Pulmonary hypertension. Multiple myeloma. |
| (III:1) | F / 67 | 25 / ND | + / + | ND | Parenchymal changes, possibly ischemic | NA | ND / ND | Normal | 1.02 / 57 | 16 | Cataract | Hypertension; osteoporosis; colon cancer. |
| (III:3) | F / 60 | ND / ND | + / + | WT | Frontoparietal subcortical WML | No | 9 / 6 | SVT | 0.8 / 80 | 2.8 | Normal | Hypohidrosis. Weakness. Palpitations. Fibromyalgia. |
| (III:4) | F / 51 | 33 / ND | + / + | WT | Normal | No | 9 / 7 | WAP | 0.6 / 106 | 5.6 | Normal | Paraesthesias. Palpitations. Hyperthyroidism. |
| (IV:1) | M / 36 | 83 / ND | + | WT | Normal | No | 9 / ND | SVPB | 0.9 / 109 | 2.2 | Normal | Angiokeratoma. |
P: proband. Gender: male (M) / female (F). Age in years (Y). α-galactosidase A (α-Gal) enzyme activity, as measured in dried blood spots (DBS) or in plasma, is expressed as percentage (%) of the normal control mean. The molecular data reported for the α-galactosidase A gene (GLA) in each case is the presence of the p.(Arg118Cys)(R118C) variant, either in hemizygosity (+), heterozygosity (+ / −) or homozygosity (+ / +), as well as the presence of any of the 5’-untranslated region (5’UTR) polymorphisms that may affect enzyme expression (−30G>A/−12G>A/10C>T); WT: wild-type 5’UTR sequence.CNS: central nervous system. MRI: magnetic resonance imaging. WML: white matter lesions. LVH: left ventricular hypertrophy, clinical diagnosis. The interventricular septal thickness (IVS) is expressed in mm, as measured by echocardiography (Echo) / cardiac MRI. Holter monitoring (24-hour)— SVPB: supraventricular premature beats; SVT: supraventricular tachycardia; AV: atrioventricular; WAP: wandering atrial pacemaker. sCr: serum creatinine level, expressed as mg/dl; eGFR: glomerular filtration rate estimated by the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation [http://www.kidney.org/professionals/kdoqi/gfr_calculator.cfm], expressed in ml/min/1.73m2. UACR: urine albumin-to-creatinine ratio, expressed as mg of albumin per g of creatinine; uPr: urine protein concentration. Eye: ocular phenotype as described on slit-lamp ophthalmological examination.CAD: coronary artery disease. New York Heart Association (NYHA) functional classification of heart failure. ND: not done/determined; NA: not assessed.
3.5. Microsatellite haplotyping studies in Portuguese individuals
The microsatellite haplotypes segregating with the GLA p.(Arg118Cys) allele were determined in 5 males and three females from apparently unrelated Portuguese families. Five different Cys118 haplotypes were identified in the 8 chromosomes, suggesting that the C>T transition underlying the emergence of p.(Arg118Cys) is a relatively frequent mutational event, in accordance with its location at a CpG dinucleotide [39].
4. Discussion
Our data suggest that the GLA p.(Arg118Cys) variant does not segregate with FD manifestations at least in a highly-penetrant Mendelian fashion. Hemizygous males and homozygous or compound heterozygous females may live at least up to the 8th decade of life, and heterozygous females up to the 9th decade, without developing major organ complications typical of FD, even in presence of other significant cardiovascular risk factors. These data may explain the absence of FD history in the Italian family identified by newborn screening [28]. Surprisingly, carriers of the Cys118 allele may present only with a typical eruption of angiokeratomas, which is usually considered a manifestation of classic FD.
The allelic frequency of GLA Cys118 in the Portuguese population is similar to that reported in North Americans: it can be estimated from those epidemiological data that in a gender-even cohort of 10.000 individuals, ≈5 males and ≈10 females will carry the Cys118 allele, which is a threefold higher prevalence than the European definition of “rare disorder” [http://ec.europa.eu/health/ph_threats/non_com/docs/rare_com_en.pdf]. Furthermore, in a neonatal screening carried out in the northwest of Spain, 50% of the newborns with low plasma α-Gal activity in whom missense GLA variants were subsequently identified were hemizygous for the GLA Cys118 allele [40].
In the PORTYSTROKE cohort, the GLA p.(Arg.118Cys) and p.(Asp313Tyr) variants were significantly more prevalent than in the general population; on the other hand, the Cys118 and the Tyr313 hemizygous males had comparable residual plasma α-Gal activities, at ≈40% the normal mean, while their average leukocyte α-Gal activities were respectively ≈35% and ≈50% of the normal [29]. These similarities suggest that subnormal α-Gal enzyme activity might be a quantitative, metabolic modulator of the multifactorial risk of cerebrovascular disease by as yet unknown mechanisms. Recent observations in non-FD patients have offered some clues as to possible additional links between human disease and GLA gene expression, α-Gal activity and Gb3 metabolism: (i) slightly decreased GLA gene expression, leading to an average reduction of leukocyte α-Gal activity of no more than ≈16.5%, may be a risk factor for sporadic Parkinson disease, possibly due to dysfunction of the autophagic-lysosomal system [41, 42]; (ii) increased urinary Gb3 excretion is independently associated with the risk of short-term death of patients with common forms of heart disease [43], perhaps signaling a systemic disturbance of sphingolipid metabolism in patients with end-stage heart failure, leading to increased incorporation of Gb3 in cell membranes.
Moreover, co-segregation of GLA variants associated with high residual enzyme activity and the 5’UTR g.1170C>T SNP may have additive effects, possibly further decreasing the residual enzyme activity even into the range usually seen in patients with later-onset phenotypic variants of FD. Therefore, screening for the presence of the g.1170C>T SNP may be helpful for the interpretation of genotype-to-phenotype correlations in patients with such GLA variants. These hypotheses will have to be confirmed in larger, properly designed studies.
The GLA p.(Arg118Cys) variant was also identified in the SIFAP cohort [32], the largest ever FD case-finding study among stroke patients (Table 2). As in the Portuguese study, the screening method was by genotyping, but SIFAP predominantly enrolled patients from northern and central European countries. Although the Cys118 allele was regarded as a pathogenic mutation and its presence was a criterion for definite diagnosis of FD, the investigators did not provide any convincing evidence to support their assumption. In contrast to the SIFAP results, GLA p.(Arg118Cys) was not identified in the Belgian Fabry Study (BeFaS) [44], which screened a total of 993 adult patients (545 males, 54.9%) presenting with cerebrovascular disease before the age of 61 years.
One female heterozygous for the GLA Cys118 allele was identified in the European Anderson-Fabry Disease Survey [31] (Table 2), a FD screening study of patients with unexplained HCM. As that woman also manifested angiokeratoma(s?) and albuminuria, GLA p.(Arg118Cys) was considered pathogenic, but the investigators did not provide histopathological evidence of FD cardiomyopathy or nephropathy, and the clinical observation of angiokeratoma(s) is inconclusive, since the presence of isolated or a few scattered angiokeratomas is not uncommon in otherwise healthy individuals [45]. In contrast to these results, the GLA p.(Arg118Cys) variant was not identified in any of 279 male patients with HCM screened for FD in a French case-finding study [38], neither in any of 508 non-selected patients (328 males, 64.6%) with HCM screened for FD in a Spanish case-finding study [46], using plasma α-Gal activity as the screening method; however, it is of note that three unrelated men in this cohort were hemizygous for the GLA Tyr313 allele.
The GLA p.(Arg118Cys) variant was identified in two unrelated males and two sisters, enrolled in a Spanish case-finding study of FD among patients with end-stage renal failure (ESRF) on chronic hemodialysis [30], that used a DBS α-Gal assay as the first-tier screening method. Although the investigators concluded that GLA p.(Arg118Cys) was a pathogenic mutation, they did not provided enough evidence to support that claim. The very old age of the two men precludes the interpretation that their renal, cardiac and cerebrovascular complications were caused by FD and, for the reason discussed above, even the presence of angiokeratoma(s?) is not convincing. In addition to not being clear why the two sisters were enrolled for GLA genotyping since their α-Gal activities on the DBS assays were, respectively, 123% and 94% of the female control mean, they both had human immunodeficiency virus (HIV) infection that may also cause kidney disease. Furthermore, a kidney biopsy from the younger sister reportedly showed glomerulosclerosis and hyalinosis, but did not show the most typical LM feature of Fabry nephropathy (e.g. vacuolation). While glomerulosclerosis and hyalinosis are possible manifestations of HIV-associated nephropathy, in Caucasians immune-complex-mediated kidney injury is much more common due to the absence of the ApoL1 polymorphisms associated with HIV nephropathy. Of note, the investigators classified the GLA p.(Asp313Tyr) SNP, that was found in an 80-year-old female and a 74-year-old male, as a sequence variant of controversial pathogenicity. Apparently in line with these observations, one Cys118 hemizygous male enrolled in the Fabry Registry [47] started dialysis at age 45 years.
In contrast to those Spanish data, neither the p.(Arg118Cys) nor the p.(Asp313Tyr) GLA variants were identified in the 2688 men enrolled in the Portuguese screening of FD among non-selected dialysis patients [48]. Although the Portuguese investigators also used a DBS α-Gal assay for case finding, the <30% cut-off level of residual enzyme activity to proceed with further diagnostic tests (unpublished data) was more stringent than in the Spanish study, and patients showing high residual enzyme activities, in the range observed in hemizygous males for GLA p.(Arg118Cys) or p.(Asp313Tyr), would not be selected for genotyping.
Overall, those studies demonstrate that the identification of GLA variants associated with residual α-Gal activity on large cohorts will critically depend on the screening method used and, when based on enzyme assays, on the predefined cut-off level of residual enzyme activity to select cases for genotyping.
It should be noted, however, that the correlations between the in vitro α-Gal residual activity, substrate accumulation and the FD clinical phenotype are complex and still incompletely understood, and that other factors, besides the residual level of enzyme activity, play a crucial role in the pathogenesis of the disease [49]. It might also be possible that the in vitro α-Gal assays do not reflect the biological enzyme activity in vivo, thereby confounding the interpretation of genotype-phenotype correlations.
Because of the non-specific features of the late-onset cerebrovascular, cardiac and renal complications of FD, and the much higher prevalence of other causes of stroke, LVH/HCM and ESRF in adult populations, FD case-finding studies among high-risk patients are intrinsically biased. Accordingly, reports of patients identified in such studies, carrying either novel GLA sequence variants or VUS, particularly when associated with high residual α-Gal activity, should provide enough clinical, biochemical and histopathological details to support the diagnosis of FD, and exclude the relevant differential diagnoses, on a case-by-case basis. This same approach has been recently recommended by Dutch experts on FD [50]. Furthermore, proper assessment of the medical relevance of newly identified GLA sequence variants or VUS should also take into consideration the genetic makeup of the source populations, but the relevant allelic frequencies will have to be estimated in studies large enough to identify low-frequency (MAF between 0.05–0.005) and rare variants (MAF <0.005), which vastly outnumber the common variants in the human genome and show substantial geographic differentiation [51, 52]. Although the country of origin of the patient(s) carrying the p.(Arg118Cys) allele identified in the SIFAP and EAFDS studies was not reported, it appears from the published data that the allelic frequency of p.(Arg118Cys) is significantly lower in northern and central European countries than in the Iberian populations.
The assumption that GLA p.(Arg118Cys) is a pathogenic mutation causing a later-onset FD phenotype [28] was based on theoretical considerations about the similarities of the structural changes it induces in the α-Gal monomer and of its in vitro overexpression levels, with those of well-known missense GLA mutations associated with later-onset clinical phenotypes, as well as on the reasoning that its sulfhydryl-binding potential might interfere with the normal disulfide bonds of the α-Gal monomers. In our opinion, which is instead based upon detailed and unbiased clinical, biochemical, histopathological and family data, the mild/moderate deficiency of α-Gal activity associated with p.(Arg118Cys) is not of enough magnitude to cause major complications of FD and, therefore, carriers of the Cys118 allele currently have no straightforward indication for enzyme replacement or enhancement (chaperone) therapy. Despite involving a cysteine residue, GLA p.(Arg118Cys) most likely is a non-pathogenic or of low-pathogenicity exonic variant, like p.(Asp313Tyr) and a few others [50]. A notable example of another GLA variant whose alleged pathogenic role has recently been questioned [53] is the guanine to adenine transition (G>A) in codon 143 (c.427G>A), resulting in the replacement of alanine (Ala) by threonine (Thr) in the α-Gal monomers – i.e., p.(Ala143Thr). Although hemizygous males for the GLA Thr143 allele may variably show undetectable to moderately reduced α-Gal activity in vitro, the previously reported association of this variant with renal failure, stroke, and LVH could be the result of selection bias. Indeed, most of those cases were detected in screenings of high-risk patients, in whom histopathological or ultrastructural evidence of Gb3 accumulation in affected tissues was not specifically investigated [53].
Finally, the observation that the estimated prevalence of individuals carrying the GLA Cys118 allele in the Portuguese population is higher than current definitions of “rare diseases”, should have regulatory implications for the inclusion of such individuals in therapeutic drug trials for FD. Nevertheless, further studies are needed to clarify a potential disease-modifying role, especially in cerebrovascular disease.
Acknowledgements
Carmen Valbuena, MD, PhD, for selecting and providing the photomicrographs and electron micrographs included in this manuscript.
Christiane Auray-Blais, LL.M, PhD, Département de Pédiatrie, Service de Génétique, Centre de Recherche Clinique Étienne-Le Bel, Centre Hospitalier Universitaire de Sherbrooke, Quebec, Canada, for Gb3 and lyso-Gb3 assays in plasma and urine.
Jan-Eric Månsson, PhD, Laboratory of Neurochemistry, Department of Psychiatry and Neurochemistry, Institute of Neuroscience and Physiology, Sahlgrenska Academy, University of Gothenburg, Sweden, for Gb3 assays in plasma and Gb3/sphingomyelin assay in the urinary sediment.
Maria Clara Sá Miranda, PhD, Instituto de Genética Médica “Jacinto de Magalhães”, Porto, Portugal, for plasma Gb3 assay.
Karelle Benistan, MD, Division of Medical Genetics, Centre Hospitalier Universitaire Raymond Poincaré, Garches, France, for GLA genotyping.
Alberto Ortiz, MD, PhD, is supported by the grants FIS-PI13/00047, ISCIII-RETIC REDinREN, RD 12/0021, Comunidad de Madrid S2010/BMD-2378, CYTED IBERERC, Programa de Intensificación de la Actividad Investigadora, Instituto de Salud Carlos III (ISCIII).
This article is part of Susana Ferreira’s PhD Thesis research plan supervised by João Paulo Oliveira MD, PhD.
Conflict of Interest Declaration
J. P. Oliveira is member of the European Advisory Board of the Fabry Registry, a global observational registry of patients with Fabry disease sponsored by Genzyme Corporation. He has received unrestricted research grants and funding for research projects from Genzyme Corporation; consulting honoraria and speaker’s fees from Genzyme Corporation; conference registration fees and travel grants from Genzyme Corporation, Shire Human Genetic Therapies and Amicus Therapeutics.
S. Ferreira has received unrestricted research grants and funding for research projects from Genzyme Corporation; conference registration fees and travel grants from Genzyme Corporation and Shire Human Genetic Therapies.
A. Ortiz is member of the European Advisory Board of the Fabry Registry, a global observational registry of patients with Fabry disease sponsored by Genzyme Corporation. He has received consulting honoraria and speaker’s fees from Genzyme Corporation; speaker’s fees from Shire Human Genetic Therapies and conference registration fees and travel grants from Genzyme Corporation and Shire Human Genetic Therapies.
D. P. Germain is member of the European Advisory Board of the Fabry Registry, a global observational registry of patients with Fabry disease sponsored by Genzyme Corporation. He has received consulting honoraria, speaker’s fees and travel grants from Genzyme Corporation, Shire Human Genetic Therapies and Amicus Therapeutics.
M. Viana-Baptista is member of the Global Neurological Fabry Board supported by Genzyme Corporation. He has received consultant honoraria and speaking fees from Genzyme Corporation and Genzyme Portugal. He has received unrestricted research grants and funding for research projects from Genzyme Portugal.
Footnotes
Parts of these data have been presented at the 3rd Update on Fabry Nephropathy – Biomarkers, Progression and Treatment Opportunities, Hong Kong, June 4–5, 2013.
Contributor Information
Susana Ferreira, Email: susanadg@med.up.pt.
Alberto Ortiz, Email: aortiz@fjd.es.
Dominique P. Germain, Email: dominique.germain@uvsq.fr.
Miguel Viana-Baptista, Email: mvianabaptista@fcm.unl.pt.
António Caldeira Gomes, Email: viladoconde@diaverum.com.
Maria Fenollar-Cortés, Email: mariadelmar.fenollar@salud.madrid.org.
Ángel Gallegos-Villalobos, Email: angelgallegos.nefro@gmail.com.
Jesús Egido, Email: jegido@fjd.es.
Sebastián Mas, Email: smas@fjd.es.
Helena Alves, Email: helena.d.alves@gmail.com.
Scott C. Garman, Email: garman@biochem.umass.edu.
João Paulo Oliveira, Email: jpo@med.up.pt, dr.jpoliveira@sapo.pt.
References
- 1.Desnick RJ, Ioannou YA, Eng CM. α-Galactosidase A deficiency: Fabry disease. In: Scriver CR, Beaudet AL, Sly WS, Valle D, editors. The metabolic and molecular bases of inherited disease. New York: McGraw-Hill; 2001. pp. 3733–3774. [Google Scholar]
- 2.Garman SC, Garboczi DN. The molecular defect leading to Fabry disease: structure of human alpha-galactosidase. Journal of molecular biology. 2004;337:319–335. doi: 10.1016/j.jmb.2004.01.035. [DOI] [PubMed] [Google Scholar]
- 3.Germain DP. Fabry disease. Orphanet journal of rare diseases. 2010;5:30. doi: 10.1186/1750-1172-5-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wilcox WR, Oliveira JP, Hopkin RJ, Ortiz A, Banikazemi M, Feldt-Rasmussen U, Sims K, Waldek S, Pastores GM, Lee P, Eng CM, Marodi L, Stanford KE, Breunig F, Wanner C, Warnock DG, Lemay RM, Germain DP. Females with Fabry disease frequently have major organ involvement: lessons from the Fabry Registry. Mol Genet Metab. 2008;93:112–128. doi: 10.1016/j.ymgme.2007.09.013. [DOI] [PubMed] [Google Scholar]
- 5.Gal A. Molecular Genetics of Fabry Disease and Genotype–Phenotype Correlation. In: Elstein D, Altarescu G, Beck M, editors. Fabry Disease. Dordrecht: Springer; 2010. pp. 3–19. [Google Scholar]
- 6.Eng CM, Resnick-Silverman LA, Niehaus DJ, Astrin KH, Desnick RJ. Nature and frequency of mutations in the alpha-galactosidase A gene that cause Fabry disease. American journal of human genetics. 1993;53:1186–1197. [PMC free article] [PubMed] [Google Scholar]
- 7.Eng CM, Niehaus DJ, Enriquez AL, Burgert TS, Ludman MD, Desnick RJ. Fabry disease: twenty-three mutations including sense and antisense CpG alterations and identification of a deletional hot-spot in the alpha-galactosidase. A gene Hum Mol Genet. 1994;3:1795–1799. doi: 10.1093/hmg/3.10.1795. [DOI] [PubMed] [Google Scholar]
- 8.Ploos van Amstel JK, Jansen RP, de Jong JG, Hamel BC, Wevers RA. Six novel mutations in the alpha-galactosidase A gene in families with Fabry disease. Hum Mol Genet. 1994;3:503–505. doi: 10.1093/hmg/3.3.503. [DOI] [PubMed] [Google Scholar]
- 9.Okumiya T, Ishii S, Kase R, Kamei S, Sakuraba H, Suzuki Y. Alpha-galactosidase gene mutations in Fabry disease: heterogeneous expressions of mutant enzyme proteins. Hum Genet. 1995;95:557–561. doi: 10.1007/BF00223869. [DOI] [PubMed] [Google Scholar]
- 10.Blanch LC, Meaney C, Morris CP. A sensitive mutation screening strategy for Fabry disease: detection of nine mutations in the alpha-galactosidase A gene. Hum Mutat. 1996;8:38–43. doi: 10.1002/(SICI)1098-1004(1996)8:1<38::AID-HUMU5>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 11.Davies JP, Eng CM, Hill JA, Malcolm S, MacDermot K, Winchester B, Desnick RJ. Fabry disease: fourteen alpha-galactosidase A mutations in unrelated families from the United Kingdom and other European countries. Eur J Hum Genet. 1996;4:219–224. doi: 10.1159/000472202. [DOI] [PubMed] [Google Scholar]
- 12.Eng CM, Ashley GA, Burgert TS, Enriquez AL, D'Souza M, Desnick RJ. Fabry disease: thirty-five mutations in the alpha-galactosidase A gene in patients with classic and variant phenotypes. Mol Med. 1997;3:174–182. [PMC free article] [PubMed] [Google Scholar]
- 13.Germain DP, Poenaru L. Fabry disease: identification of novel alpha-galactosidase A mutations and molecular carrier detection by use of fluorescent chemical cleavage of mismatches. Biochem Biophys Res Commun. 1999;257:708–713. doi: 10.1006/bbrc.1999.0310. [DOI] [PubMed] [Google Scholar]
- 14.Topaloglu AK, Ashley GA, Tong B, Shabbeer J, Astrin KH, Eng CM, Desnick RJ. Twenty novel mutations in the alpha-galactosidase A gene causing Fabry disease. Mol Med. 1999;5:806–811. [PMC free article] [PubMed] [Google Scholar]
- 15.Ashton-Prolla P, Tong B, Shabbeer J, Astrin KH, Eng CM, Desnick RJ. Fabry disease: twenty-two novel mutations in the alpha-galactosidase A gene and genotype/phenotype correlations in severely and mildly affected hemizygotes and heterozygotes. J Investig Med. 2000;48:227–235. [PubMed] [Google Scholar]
- 16.Ashley GA, Shabbeer J, Yasuda M, Eng CM, Desnick RJ. Fabry disease: twenty novel alpha-galactosidase A mutations causing the classical phenotype. J Hum Genet. 2001;46:192–196. doi: 10.1007/s100380170088. [DOI] [PubMed] [Google Scholar]
- 17.Blaydon D, Hill J, Winchester B. Fabry disease: 20 novel GLA mutations in 35 families. Hum Mutat. 2001;18:459. doi: 10.1002/humu.1219. [DOI] [PubMed] [Google Scholar]
- 18.Galanos J, Nicholls K, Grigg L, Kiers L, Crawford A, Becker G. Clinical features of Fabry's disease in Australian patients. Intern Med J. 2002;32:575–584. doi: 10.1046/j.1445-5994.2002.00291.x. [DOI] [PubMed] [Google Scholar]
- 19.Shabbeer J, Yasuda M, Luca E, Desnick RJ. Fabry disease: 45 novel mutations in the alpha-galactosidase A gene causing the classical phenotype. Mol Genet Metab. 2002;76:23–30. doi: 10.1016/s1096-7192(02)00012-4. [DOI] [PubMed] [Google Scholar]
- 20.Rodriguez-Mari A, Coll MJ, Chabas A. Molecular analysis in Fabry disease in Spain: fifteen novel GLA mutations and identification of a homozygous female. Hum Mutat. 2003;22:258. doi: 10.1002/humu.9172. [DOI] [PubMed] [Google Scholar]
- 21.Yasuda M, Shabbeer J, Benson SD, Maire I, Burnett RM, Desnick RJ. Fabry disease: characterization of alpha-galactosidase A double mutations and the D313Y plasma enzyme pseudodeficiency allele. Hum Mutat. 2003;22:486–492. doi: 10.1002/humu.10275. [DOI] [PubMed] [Google Scholar]
- 22.Schafer E, Baron K, Widmer U, Deegan P, Neumann HP, Sunder-Plassmann G, Johansson JO, Whybra C, Ries M, Pastores GM, Mehta A, Beck M, Gal A. Thirty-four novel mutations of the GLA gene in 121 patients with Fabry disease. Hum Mutat. 2005;25:412. doi: 10.1002/humu.9327. [DOI] [PubMed] [Google Scholar]
- 23.Shabbeer J, Robinson M, Desnick RJ. Detection of alpha-galactosidase a mutations causing Fabry disease by denaturing high performance liquid chromatography. Hum Mutat. 2005;25:299–305. doi: 10.1002/humu.20144. [DOI] [PubMed] [Google Scholar]
- 24.Filoni C, Caciotti A, Carraresi L, Cavicchi C, Parini R, Antuzzi D, Zampetti A, Feriozzi S, Poisetti P, Garman SC, Guerrini R, Zammarchi E, Donati MA, Morrone A. Functional studies of new GLA gene mutations leading to conformational Fabry disease. Biochim Biophys Acta. 2010;1802:247–252. doi: 10.1016/j.bbadis.2009.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Meng Y, Zhang WM, Shi HP, Wei M, Huang SZ. [Clinical manifestations and mutation study in 16 Chinese patients with Fabry disease] Zhonghua Yi Xue Za Zhi. 2010;90:551–554. [PubMed] [Google Scholar]
- 26.Mukdsi JH GS, Belén Barrón B, Novoa P, Fernández S, De Diller AB, Torres AI, A OM, Formica RN., Jr Renal Variant of Fabry Disease: A case with a novel Gal A hemizygote mutation. J Nephropathology. 2012;1:194–197. doi: 10.5812/nephropathol.8123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sánchez-Niño MD OA. Is it or is it not a pathogenic mutation? Is it or is it not the podocyte? J Nephropathology. 2012;1:152–154. doi: 10.5812/nephropathol.8110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Spada M, Pagliardini S, Yasuda M, Tukel T, Thiagarajan G, Sakuraba H, Ponzone A, Desnick RJ. High incidence of later-onset fabry disease revealed by newborn screening. American journal of human genetics. 2006;79:31–40. doi: 10.1086/504601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Baptista MV, Ferreira S, Pinho-E-Melo T, Carvalho M, Cruz VT, Carmona C, Silva FA, Tuna A, Rodrigues M, Ferreira C, Pinto AAN, Leitao A, Gabriel JP, Calado S, Oliveira JP, Ferro JM, P.O.Y.S. Investigators. Falcao F, Pinho e Melo T, Canhao P, Massano J, Azevedo E, da Feira SM, Cruz VT, Oliveira A, Milheiro M, Pita F, Silva F, Goncalves F, Rodrigues M, Fontes JR, Lopes G, Correia M, Guerreiro RM, Goncalves G, Pinto AN, Inacio N, Simoes R, Brito V, Silva MR, Palma I, Viana-Baptista M. Mutations of the GLA gene in young patients with stroke: the PORTYSTROKE study--screening genetic conditions in Portuguese young stroke patients. Stroke. 2010;41:431–436. doi: 10.1161/STROKEAHA.109.570499. [DOI] [PubMed] [Google Scholar]
- 30.Gaspar P, Herrera J, Rodrigues D, Cerezo S, Delgado R, Andrade CF, Forascepi R, Macias J, del Pino MD, Prados MD, de Alegria PR, Torres G, Vidau P, Sa-Miranda MC. Frequency of Fabry disease in male and female haemodialysis patients in Spain. BMC medical genetics. 2010;11:19. doi: 10.1186/1471-2350-11-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Elliott P, Baker R, Pasquale F, Quarta G, Ebrahim H, Mehta AB, Hughes DA. Prevalence of Anderson-Fabry disease in patients with hypertrophic cardiomyopathy: the European Anderson-Fabry Disease survey. Heart (British Cardiac Society) 2011;97:1957–1960. doi: 10.1136/heartjnl-2011-300364. [DOI] [PubMed] [Google Scholar]
- 32.Rolfs A, Fazekas F, Grittner U, Dichgans M, Martus P, Holzhausen M, Bottcher T, Heuschmann PU, Tatlisumak T, Tanislav C, Jungehulsing GJ, Giese AK, Putaala J, Huber R, Bodechtel U, Lichy C, Enzinger C, Schmidt R, Hennerici MG, Kaps M, Kessler C, Lackner K, Paschke E, Meyer W, Mascher H, Riess O, Kolodny E, Norrving B. Acute cerebrovascular disease in the young: the Stroke in Young Fabry Patients study. Stroke. 2013;44:340–349. doi: 10.1161/STROKEAHA.112.663708. [DOI] [PubMed] [Google Scholar]
- 33.Turaca LT, Pessoa JG, Motta FL, Munoz Rojas MV, Muller KB, Lourenco CM, Junior Marques W, D'Almeida V, Martins AM, Pesquero JB. New mutations in the GLA gene in Brazilian families with Fabry disease. J Hum Genet. 2012;57:347–351. doi: 10.1038/jhg.2012.32. [DOI] [PubMed] [Google Scholar]
- 34.Morais P, Santos AL, Baudrier T, Mota AV, Oliveira JP, Azevedo F. Angiokeratomas of Fabry successfully treated with intense pulsed light. Journal of Cosmetic and Laser Therapy. 2008;10:218–222. doi: 10.1080/14764170802275832. [DOI] [PubMed] [Google Scholar]
- 35.Valbuena C, Leitao D, Carneiro F, Oliveira JP. Immunohistochemical diagnosis of Fabry nephropathy and localisation of globotriaosylceramide deposits in paraffin-embedded kidney tissue sections. Virchows Arch. 2012;460:211–221. doi: 10.1007/s00428-011-1182-y. [DOI] [PubMed] [Google Scholar]
- 36.Oliveira JP, Ferreira S, Barcelo J, Gaspar P, Carvalho F, Sa Miranda MC, Mansson JE. Effect of single-nucleotide polymorphisms of the 5' untranslated region of the human alpha-galactosidase gene on enzyme activity, and their frequencies in Portuguese caucasians. J Inherit Metab Dis. 2008;31(Suppl 2):S247–S253. doi: 10.1007/s10545-008-0818-9. [DOI] [PubMed] [Google Scholar]
- 37.Oliveira JP, Ferreira S, Reguenga C, Carvalho F, Mansson JE. The g.1170C>T polymorphism of the 5' untranslated region of the human alpha-galactosidase gene is associated with decreased enzyme expression--evidence from a family study. J Inherit Metab Dis. 2008;31(Suppl 2):S405–S413. doi: 10.1007/s10545-008-0972-0. [DOI] [PubMed] [Google Scholar]
- 38.Hagege AA, Caudron E, Damy T, Roudaut R, Millaire A, Etchecopar-Chevreuil C, Tran TC, Jabbour F, Boucly C, Prognon P, Charron P, Germain DP. Screening patients with hypertrophic cardiomyopathy for Fabry disease using a filter-paper test: the FOCUS study. Heart (British Cardiac Society) 2011;97:131–136. doi: 10.1136/hrt.2010.200188. [DOI] [PubMed] [Google Scholar]
- 39.Cooper DN, Youssoufian H. The CpG dinucleotide and human genetic disease. Hum Genet. 1988;78:151–155. doi: 10.1007/BF00278187. [DOI] [PubMed] [Google Scholar]
- 40.Rana-Diez P, Colon C, Alonso-Fernandez J, Fraga J, Gonzalez-Bouzon R, Carracedo A, Barros F. High incidence of Fabry disease-causing mutations in Galicia. North-west Spain (Abstract) European Journal of Human Genetics. 2009;17(Supplement 2):350. [Google Scholar]
- 41.Wu G, Huang J, Feng X, Zhang A, Li J, Pang S, Gu K, Dong H, Zhang J, Gao H, Yan B. Decreased expression of lysosomal alpha-galactosiase A gene in sporadic Parkinson's disease. Neurochem Res. 2011;36:1939–1944. doi: 10.1007/s11064-011-0516-0. [DOI] [PubMed] [Google Scholar]
- 42.Wu G, Yan B, Wang X, Feng X, Zhang A, Xu X, Dong H. Decreased activities of lysosomal acid alpha-D-galactosidase A in the leukocytes of sporadic Parkinson's disease. J Neurol Sci. 2008;271:168–173. doi: 10.1016/j.jns.2008.04.011. [DOI] [PubMed] [Google Scholar]
- 43.Schiffmann R, Forni S, Swift C, Brignol N, Wu X, Lockhart DJ, Blankenship D, Wang X, Grayburn PA, Taylor MR, Lowes BD, Fuller M, Benjamin ER, Sweetman L. Risk of death in heart disease is associated with elevated urinary globotriaosylceramide. J Am Heart Assoc. 2014;3:e000394. doi: 10.1161/JAHA.113.000394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Brouns R, Thijs V, Eyskens F, Van den Broeck M, Belachew S, Van Broeckhoven C, Redondo P, Hemelsoet D, Fumal A, Jeangette S, Verslegers W, Baker R, Hughes D, De Deyn PP. Belgian Fabry study: prevalence of Fabry disease in a cohort of 1000 young patients with cerebrovascular disease. Stroke. 2010;41:863–868. doi: 10.1161/STROKEAHA.110.579409. [DOI] [PubMed] [Google Scholar]
- 45.Zampetti A, Orteu CH, Antuzzi D, Bongiorno MR, Manco S, Gnarra M, Morrone A, Cardinali G, Kovacs D, Aspite N, Linder D, Parini R, Feliciani C. Angiokeratoma: decision-making aid for the diagnosis of Fabry disease. Br J Dermatol. 2012;166:712–720. doi: 10.1111/j.1365-2133.2012.10742.x. [DOI] [PubMed] [Google Scholar]
- 46.Monserrat L, Gimeno-Blanes JR, Marin F, Hermida-Prieto M, Garcia-Honrubia A, Perez I, Fernandez X, de Nicolas R, de la Morena G, Paya E, Yague J, Egido J. Prevalence of fabry disease in a cohort of 508 unrelated patients with hypertrophic cardiomyopathy. J Am Coll Cardiol. 2007;50:2399–2403. doi: 10.1016/j.jacc.2007.06.062. [DOI] [PubMed] [Google Scholar]
- 47.Ortiz A, Cianciaruso B, Cizmarik M, Germain DP, Mignani R, Oliveira JP, Villalobos J, Vujkovac B, Waldek S, Wanner C, Warnock DG. End-stage renal disease in patients with Fabry disease: natural history data from the Fabry Registry. Nephrol Dial Transplant. 2010;25:769–775. doi: 10.1093/ndt/gfp554. [DOI] [PubMed] [Google Scholar]
- 48.Mignani R, Feriozzi S, Schaefer RM, Breunig F, Oliveira JP, Ruggenenti P, Sunder-Plassmann G. Dialysis and transplantation in Fabry disease: indications for enzyme replacement therapy. Clin J Am Soc Nephrol. 2010;5:379–385. doi: 10.2215/CJN.05570809. [DOI] [PubMed] [Google Scholar]
- 49.Weidemann F, Sanchez-Nino MD, Politei J, Oliveira JP, Wanner C, Warnock DG, Ortiz A. Fibrosis: a key feature of Fabry disease with potential therapeutic implications. Orphanet journal of rare diseases. 2013;8:116. doi: 10.1186/1750-1172-8-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.van der Tol L, Smid BE, Poorthuis BJ, Biegstraaten M, Deprez RH, Linthorst GE, Hollak CE. A systematic review on screening for Fabry disease: prevalence of individuals with genetic variants of unknown significance. J Med Genet. 2014;51:1–9. doi: 10.1136/jmedgenet-2013-101857. [DOI] [PubMed] [Google Scholar]
- 51.Abecasis GR, Altshuler D, Auton A, Brooks LD, Durbin RM, Gibbs RA, Hurles ME, McVean GA. A map of human genome variation from population-scale sequencing. Nature. 2010;467:1061–1073. doi: 10.1038/nature09534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Abecasis GR, Auton A, Brooks LD, DePristo MA, Durbin RM, Handsaker RE, Kang HM, Marth GT, McVean GA. An integrated map of genetic variation from 1,092 human genomes. Nature. 2012;491:56–65. doi: 10.1038/nature11632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Terryn W, Vanholder R, Hemelsoet D, Leroy BP, Van Biesen W, De Schoenmakere G, Wuyts B, Claes K, De Backer J, De Paepe G, Fogo A, Praet M, Poppe B. Questioning the Pathogenic Role of the GLA p.Ala143Thr"Mutation" in Fabry Disease: Implications for Screening Studies and ERT. JIMD Rep. 2013;8:101–108. doi: 10.1007/8904_2012_167. [DOI] [PMC free article] [PubMed] [Google Scholar]