Abstract
Recently, the Vaccines to Vaccinate (v2V) initiative was reconfigured into the Partnership for Dengue Control (PDC), a multi-sponsored and independent initiative. This redirection is consistent with the growing consensus among the dengue-prevention community that no single intervention will be sufficient to control dengue disease. The PDC's expectation is that when an effective dengue virus (DENV) vaccine is commercially available, the public health community will continue to rely on vector control because the two strategies complement and enhance one another. Although the concept of integrated intervention for dengue prevention is gaining increasingly broader acceptance, to date, no consensus has been reached regarding the details of how and what combination of approaches can be most effectively implemented to manage disease. To fill that gap, the PDC proposed a three step process: (1) a critical assessment of current vector control tools and those under development, (2) outlining a research agenda for determining, in a definitive way, what existing tools work best, and (3) determining how to combine the best vector control options, which have systematically been defined in this process, with DENV vaccines. To address the first step, the PDC convened a meeting of international experts during November 2013 in Washington, DC, to critically assess existing vector control interventions and tools under development. This report summarizes those deliberations.
Introduction
Dengue virus (DENV) causes more human morbidity and mortality than any other arboviral disease. Recent estimates are that approximately 390 million people are infected each year and 96 million manifest with clinically apparent disease [1]. The World Health Organization (WHO) called for an increased focus on dengue prevention in its 2013 report on neglected tropical diseases. Dengue’s explosive epidemic potential and the worldwide increase in dengue cases was noted. Specifically, dengue has experienced a 30-fold increase in incidence over the past 50 years that shows no sign of slowing down. The report calls for evaluation and integration of current intervention strategies to achieve a 50% reduction in dengue mortality and 25% reduction in dengue morbidity by 2020 [2].
DENV is transmitted from one person to another by Aedes mosquitoes, principally Aedes aegypti [3]. Human infections can result in a spectrum of diseases ranging from mild, self-limiting febrile illness to classic dengue fever to shock syndrome and death [4], but it has been recognized that the majority of infections are mild or show no clinical manifestations. Presently, there are no commercially available antivirals or dengue vaccines, though progress on their development is encouraging [5–11]. Dengue prevention, therefore, is currently limited to mosquito control. A few well-documented successes indicate that rigorously applied vector control can reduce DENV transmission and disease. During the 1950s and 1960s a regional program across much of the Caribbean and Central and South America dramatically reduced Ae. aegypti populations, resulting in striking reductions in human yellow fever and DENV infections and purported elimination of Ae. aegypti from most of the region by the early 1970s [12,13]. Vector control programs for dengue control in Singapore during the 1970s and 1980s [14] and in Cuba during the 1980s and 1990s [15–17] are similarly recognized as public health successes, but they, too, were unfortunately not sustainable. The inability of these countries to sustain their gains is considered, at least in part, to be the consequence of diminished herd immunity [18]. This is worth emphasizing, particularly in the context of envisaged vaccination programmes, which may help overcome the problem of vector control sustainability by elevating herd immunity [19]. Less dramatic results, for example during 2000–2010 in Peru, were seen by the successful use of emergency vector control to reduce the force of DENV infection [20], i.e., per capita risk of human infection [19]. There is, however, considerable frustration because vector control has failed to prevent epidemics and DENV’s expanding geographic distribution [21]. Although the concept of vector control is reasonable, control must be early in an outbreak or strategically applied during inter-epidemic periods to prevent escalation in transmission and successful broad scale application has been difficult to achieve (Box 1).
Box 1. Key Learning Points from Vector Control for Dengue Prevention
Success in reducing the public health burden of dengue will require a multi-pronged approach that includes developing the underlying theory of effective dengue control, continuing to review and assess existing interventions and strategies, and gathering new empirical data that tests fundamental concepts and strategies. This is best achieved through:
Controlled experimental studies are urgently needed to assess the health impact of dengue vector control based on epidemiological and entomological metrics. Interventions under development are required to address this issue. The gap is greatest for existing tools and strategies, which were developed in an era when epidemiologic assessments were not carried out.
Although greater emphasis should be placed on proactive strategies that aim to prevent, diminish, or eliminate transmission, dengue outbreaks occur and response requires attention to development of tools and strategies that can be rapidly deployed and have swift impact.
Dengue is a growing problem in modern mega-urban centers that span across countries and regions. Scaling up from successful small-scale experimental trials to broad-scale public health application is among the biggest challenges for improving mosquito control for dengue prevention.
There is a growing consensus that eliminating dengue as a public health burden can only be achieved by integrating vector control with vaccines. Prioritizing the vector interventions based on their potential to prevent disease will facilitate determining how to combine the best options with DENV vaccines.
Mission of the Partnership for Dengue Control
The initiative Vaccines to Vaccination (v2V) was established in 2009 to facilitate delivery of DENV vaccines following regulatory approval. After publication of results from a phase 2b clinical dengue vaccine trial in Thailand indicating varying levels of vaccine efficacy [9], the program was reconfigured into the Partnership for Dengue Control (PDC), a multi-sponsored and independent initiative. Redirection of the program was consistent with the growing consensus among the dengue prevention community that no single intervention will be sufficient to control dengue disease. This is due to heterogeneities in mosquito vector, viral pathogen, and human host factors that drive the complexity of transmission. It was decided, therefore, that, for the greatest likelihood of sustained dengue prevention, the PDC mission should be to promote development and implementation of multiple innovative, integrated, and synergistic interventions.
The PDC’s expectation is that when an effective DENV vaccine is commercially available, the public health community will continue to rely on vector control because the two strategies complement and enhance one another [19]. A dengue vaccine can be used to artificially elevate herd immunity and vector control to lower the force of infection. Theory and results from field studies with other vector-borne pathogens support the power of simultaneously targeting the vector and pathogen. The global malaria burden has been reduced using anti-Plasmodium drugs in conjunction with insecticide-treated bed nets [22–25]. Lymphatic filariasis (LF) is more rapidly and efficiently managed when anti-parasite drugs are combined with vector control than when drugs alone are used [26–32]. As has been the case for malaria and lymphatic filariasis, guidance for how to best integrate interventions against a complicated, multi-strain pathogen with complex transmission dynamics, like DENV, will benefit from preliminary, theoretical assessment with mathematical and simulation models [33,34].
The use of multiple strategies for vector-borne disease prevention is the basis of WHO’s Integrated Vector Management (IVM) program for control of mosquito vectors, including those that transmit DENV [35]. An element of IVM is decision-making guided by operational research and entomological and epidemiological surveillance and evaluation. The expectation is that as field data becomes available for dengue vector interventions, so, too, will the ability to refine guiding principles for implementation and maximizing impact. This evidence will serve as the basis for assessment, challenging traditional paradigms and changes in the standards for delivery of vector control and/or vaccines.
As a first step, the PDC initiated a study to assess state-of-the-art vector control for dengue. Goals were to critically review different tools and strategies, identify those approaches with the greatest potential for positive public health impact, identify key missing information required for guiding successful vector management, and propose productive ways for filling knowledge gaps and advancing dengue prevention. This report summarizes those deliberations.
Assessment Process
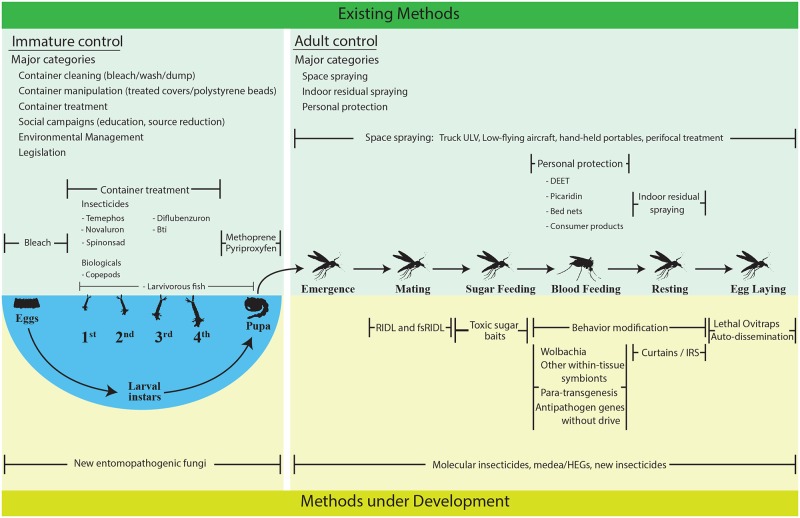
Although the concept of integrated intervention for dengue prevention is gaining increasingly broader acceptance, to date, no consensus has been reached regarding the details of how and what combination of approaches can be most effectively implemented to manage disease. To fill that gap, the PDC proposed a three step process: (1) a critical assessment of current tools and those under development, (2) outlining a research agenda for determining, in a definitive way, what existing tools work best, and (3) determining how to combine the best vector control options, which have systematically been defined in this process, with DENV vaccines. The PDC convened a meeting of international experts during November 2013 in Washington, DC, to address the first step, i.e., critically review existing interventions and tools under development (Box 2 and Fig 1).
Box 2. Key Papers from Vector Control for Dengue Prevention
Egger JR, Ooi EE, Kelly DW, Woolhouse ME, Davies CR, Coleman PG. Reconstructing historical changes in the force of infection of dengue fever in Singapore: Implications for surveillance and control. Bulletin of the World Health Organization. 2008; 86(3): 187–196. doi:10.2471/blt.07.040170.
Erlanger TE, Keiser J, Utzinger J. Effect of dengue vector control interventions on entomological parameters in developing countries: A systematic review and meta-analysis. Med Vet Entomol. 2008; 22(3): 203–221. doi:10.1111/j.1365-2915.2008.00740.x.
Scott TW, Morrison AC. Vector dynamics and transmission of dengue virus: Implications for dengue surveillance and prevention strategies: vector dynamics and dengue prevention. In: Rothman AL, editor. Dengue virus. Berlin: Springer-Verlag Berlin; 2010.pp. 115–128. doi:10.1007/978-3-642-02215-9_9.
Gubler D. Dengue, urbanization and globalization: The unholy trinity of the 21st century. Int J Infect Dis. 2012; 16E2-E2. doi:10.1016/j.ijid.2012.05.009.
World Health Organization. Sustaining the drive to overcome the global impact of neglected tropical diseases: Second WHO report on neglected diseases. Geneva: World Health Organization; 2013.
Fig 1. Existing and developing control methods.
Existing methods (upper green region) and methods under development (lower yellow region) are enumerated and separated by those that affect larval mosquito stages (left) and those that affect adult mosquito stages (right). Methods that target a particular sub-stage within a mosquito’s life cycle are oriented vertically with those sub-stages.
Deliberations fell into three broad categories: (1) current state-of-the-art (existing) interventions, (2) new tools and strategies (methods under development), and (3) mosquito ecology and modeling. For existing interventions, assessment included which life stage was targeted and evidence establishing the degree to which the intervention impacts mosquito populations and DENV transmission (S1 Table). Expectations of impact were based on available data from small-scale experiments, large-scale field trials, and model results. For interventions under development, assessment included progress within a product developmental pipeline (S2 Table). Best circumstances were outlined for successful deployment of all interventions and challenges faced in contexts where an intervention has already been introduced or is being considered was outlined (S3 Table). Although rigorous economic assessment of each intervention was outside the scope of this workshop, general issues related to ways that development, delivery, and cost could be improved for each intervention were explored (S4 Table). Cost-effectiveness will be fundamentally important in the future for selection and implementation of any vector control intervention.
Existing Tools and Strategies
A list of currently recommended vector control interventions was generated from WHO guidelines for dengue control (S1 Table) [4]. Topical repellents and legislation (regulation) were added to the list. To streamline discussion, interventions were categorized by tools that: (1) offer best sustained control, (2) offer best epidemic mitigation, or (3) are politically driven, but may not provide substantial benefit to reduced disease. The primary assessment criterion of a single existing strategy was expert opinion regarding evidence of adult vector population reduction. The discipline of vector control has been strongly influenced by the theory developed by Ronald Ross and George Macdonald (i.e., the Ross-Macdonald model), which asserts that the potential for mosquito-borne pathogen transmission is largely dependent on adult vector mosquito abundance, survival through the pathogen incubation period, and human-biting rate [36]. Interventions that reduce adult mosquito population density, daily probability of survival, and mosquito contact with humans are, therefore, expected to have the biggest impact on decreasing virus transmission. It should be noted, however, that the Ross-Macdonald model was not formulated to specifically explore larval mosquito control. Recent quantitative assessments indicate that under certain circumstances larval control may result in larger than previously expected reductions in pathogen transmission [37].
Sustained Management
Tools and strategies recommended by panel participants for sustained dengue mitigation included indoor spraying (preferably with residual insecticides) and perifocal spraying with residual insecticides to kill adult mosquitoes [38]. This is supported by results from the perifocal residual insecticide treatment of receptacles for the control of larvae and resting adult mosquitoes in two successful Ae. aegypti eradication programs in the Northern Territory of Australia from 2004 to 2006 (Tennant Creek) and from 2006 to 2008 (Groote Eylandt) [39]. Perifocal spraying, complimented with source reduction, was the mainstay of the eradication campaign in the Americas. In the Cayman Islands, perifocal spraying was successfully combined with larviciding, as well as intra- and extra-domiciliary spraying [40]. Although perifocal spraying of containers that are potential larval development sites with residual insecticide is frequently promoted in literature on dengue prevention [41], indoor residual insecticide application has only been carried out on a few occasions as part of a top-down approach for dengue vector control [42]. Studies of indoor residual spraying (IRS) in Cairns, however, indicate that the strategy, when used appropriately, (1) reduces adult female density [43] and (2) significantly reduces DENV transmission risk [44].
Comprehensive container larvicide treatment (with insecticides or biologicals) and container removal are recommended for sustained management of immatures, and, thus, indirectly adult Aedes, based on demonstration of small-scale successes using combinations of interventions [45]. Social mobilization campaigns (education, public relations) [46,47], environmental management [48], and legislation (enforcement and incentives) were considered effective as components of sustained mitigation programs [14]. Failure of dengue vector control strategies has often been associated with the absence of active local community involvement [49].
Conversely, two highly visible interventions (aerial and truck mounted ultra-low volume [ULV] space-spraying) were not recommended due to lack of impact on mosquito population reduction and lack of cost-effectiveness for routine delivery [50].
Improving sustained mitigation will require a “career structure” that maintains trained staff through inter-epidemic and epidemic periods. Lack of personnel with appropriate technical expertise plagues many dengue prevention programs [51]. This could be addressed by generating permanent positions that, through financial or promotional gains, ensure continuity in operational implementation. Establishing staff work schedules that fit community lifestyles would facilitate visits to homes and other structures when residents/owners are most likely to be present and allow access.
Epidemic Mitigation
Epidemic response tools and strategies can reduce dengue cases. When applied early in the transmission season (i.e., during the increase of epidemic cases), indoor ULV insecticide applications were associated with a reduction in the number of dengue cases in Iquitos, Peru [20]. Similarly, dengue epidemics in Brazil and Hawaii were controlled using indoor spraying with residual insecticide [52]. The challenge for this approach is early recognition of increased risk followed quickly by comprehensive broad scale intra-domicile insecticide application. This is difficult, if not impossible, to accomplish in complex mega-cities. Improved surveillance efforts that guide more logistically feasible spatial and temporal implementation of vector control are needed to improve the speed of response and to elevate the public health impact of targeted epidemic suppression strategies [19]. In most circumstances, as for sustained management, spraying with low-flying aircraft was not considered a viable approach for epidemic mitigation of dengue.
Under certain specific circumstances, in conjunction with indoor residual spray, personal repellents (e.g., DEET) and insecticide treated material inside homes (e.g., bed nets and/or treated lining) where Ae. aegypti rest and bite humans were recognized as a potential component of epidemic mitigation. Laboratory studies have shown that Ae. aegypti and Ae. albopictus infected with the four DENV serotypes respond similarly to uninfected mosquitoes indicating that repellents containing DEET may be effective against infective mosquitoes in the field [53].
Field studies in Mexico demonstrated reduction in vector populations using pyrethroid treated curtains and water jar covers [54]. Data, however, are lacking to assess to what extent these interventions reduce dengue cases during an epidemic.
At the local level, emergency legislation for immediate access to vacant lots, households, schools, and/or offices may be required, where not currently enacted, to allow comprehensive attention to key virus transmission sites.
Perhaps the most important point derived from panel discussions is that the primary reason for the inability to recommend a specific existing intervention for either sustained management or epidemic mitigation is the absence of data providing clear evidence of a direct, positive health impact, i.e., reduced human dengue cases. For example, no panelist was aware of any controlled study carried out to evaluate the protective efficacy of ULV spraying against human DENV infection despite the fact that ULV spraying continues to be a frequently used intervention for dengue. The group recognized that selection and impact of existing, or any, vector control strategy to mitigate vector populations and/or the overall impact on dengue will be site-specific based on underlying human, virus, and/or vector dynamics, which is consistent with the requirement for an integrated approach [54]. Political pressures, however, typically drive implementation of highly visible activities, such as aerial, truck-mounted, and space-spraying, without a solid empirical basis for using these approaches to reduce human infection and/or disease.
Interventions Currently under Development
Because, as currently used, existing tools for suppressing dengue vector populations are often judged ineffective, there has been increasing interest in developing new tools. Some are being developed by technological improvement of existing approaches. Others involve conceptually novel approaches that have emerged from breakthroughs in biotechnologies.
Meeting participants developed a list of tools and strategies in development for dengue suppression (S2 Table) that are designed to (1) reduce the overall mosquito population, (2) change the age structure of the female mosquito population, (3) manipulate female mosquito behavior, (4) replace wild-type mosquitoes with strains/genotypes that do not transmit DENV, or (5) some combination of the above. Each tool was evaluated based on criteria related to the (1) current stage of development, (2) predicted efficacy, (3) expected limitations, and (4) potential for integration with other tools.
Population Reduction
Synthetic insecticides have long been used to suppress mosquito populations, but negative environmental and health impacts, lack of intrinsic efficacy, and evolution of insecticide-resistant mosquitoes are challenging current insecticide-reliant strategies [55–59]. Two major paths for alleviating these problems come from investment in new chemical classes of insecticides [60] and “molecular insecticides” that use specially engineered nanoparticles to target insecticides at specific insect tissues and protect the active ingredient from environmental degradation [61]. There have been major investments in developing and testing new insecticides within existing chemical classes (and in new classes) with low off-target effects and long residual efficacy. Some of the first products from these efforts are expected to be field tested in the near future, and completely novel compounds should soon follow. The goal is to have a tool(s) that is as effective at suppressing DENV transmission as DDT was (high kill and/or repellent with effectiveness for six months or more), but without associated health or environmental impacts. Early indications are encouraging, but it is too soon to draw firm conclusions about the potential for reaching that goal. As with any intervention that poses a potential selection pressure on mosquito populations, behavioral or physiological, monitoring for change in efficacy over time will be a vital part of the strategy.
There are a number of tools in the pipeline that involve using insect genetic engineering for population reduction. The one furthest in development is an Ae. aegypti strain engineered by the start-up company, Oxitec, that has conditional lethality (RIDLR) [62]. The genetically engineered strain can be reared to high numbers in captivity simply by adding tetracycline to the larval diet. When transgenic males are released into wild-type mosquito populations in the field and mate with normal females, almost 100% of the offspring are expected to die during late larval development stages. Data from small-scale trials indicate that wild populations can be suppressed, but suppression takes a number of months and requires continual release of the transgenic strain. This approach is expected to work best when the initial population is at low density and the treatment area is relatively small. Thus, this approach could be used with other tools that decrease vector population size before RIDLR mosquitoes are released. Promising results were obtained from field trials in Malaysia and the Cayman Islands [63,64] and small Brazilian communities [65,66]. As for any transgenic mosquito strain, public acceptance and regulatory approval will be required.
A public/private partnership (Gates/Oxitec) developed a different transgenic Ae. aegypti strain (OX36404C) in which only the females die (fsRIDL) when tetracycline is removed from their larval diet [67]. Such a strain could be more effective than one in which both sexes die. Although indoor large-cage trials were successful [68], results from an outdoor field-cage trial in Mexico were disappointing [69]. Lowered mating competitiveness of transgenic males was one cause of the failure of that trial. It is possible that new strains with this female-killing transgenic construct may have better performance. Detailed population dynamics models indicate that mosquito suppression with this female-killing technique may be problematic in heterogeneous city settings and that attention must be paid to developing effective male release methods [70]. Some researchers also question the feasibility of RIDL for large cities or large geographic areas due to logistic challenges of delivery and concerns about cost. The developers, however, argue that these obstacles can be overcome [71].
A conceptually similar, but methodologically different, biotechnology approach for population reduction would entail multiple releases of male Ae. aegypti artificially infected with a strain of a microbe, Wolbachia, that renders them 100% reproductively incompatible with wild-type females [72]. If incompatibility was less than 100%, releases could presumably result in resurgence of a mosquito population carrying the Wolbachia (see below).
Another transgenic method based on sex ratio distortion exploits the specificity of the homing endonuclease I-Ppol, and is in early stages of development in Anopheles mosquitoes [73]. Using this approach, a mosquito strain was developed that produces >95% male offspring and has been shown to suppress caged wild-type mosquitoes following multiple releases. This approach of sex ratio distortion may provide the foundation for self-perpetuating control of Anopheles if the DNA sequence causing sex distortion can be inserted on the Y-chromosome. In the future, it may be possible to develop similar methods for Ae. aegypti that could suppress wild Ae. aegypti populations based on a single release of a transgenic strain. This is a more daunting challenge with Ae. aegypti because it lacks a distinct sex chromosome.
In the past few years, a new tool for insect transgenesis and genome editing has emerged. This tool, based on CRISPR/Cas9 DNA double-strand breaks and repair, has the potential to substantially propel the field of genetic pest management forward [74,75]. Unlike homing endonucleases, in which changing the DNA target site requires major protein engineering, the CRISPR/Cas9 system enables targeting based simply on changing the nucleotide sequences coding for guide RNAs. This transforms the whole process of gene manipulation into one that is much more efficient and less costly. The CRISPR/Cas9 approach could be used for building self-perpetuating, sex-biasing Aedes strains or strains that drive a genetic load into an Aedes population strong enough to cause substantial decline in density, or local elimination.
Attracting and then killing female mosquitoes as they lay eggs, via lethal ovitraps or sticky gravid traps, is a targeted, alterative strategy for vector population reduction first recognized in the 1970s [76]. Early attempts in Brazil [77] and Thailand [78] demonstrated reduction in Ae. aegypti adult and larval populations, but did not meet expectations required for elimination. More efficient trap designs are currently being developed and evaluated [79]. This includes a new lethal ovitrap design that was coupled with a bacteria formulation that produces volatile compounds that are attractive to ovipositing female Ae. aegypti [80–82]. A recent field trial in Peru generated encouraging preliminary results [83]. Lethal killing stations utilizing adhesives have also been shown to reduce gravid Ae. aegypti by ~80% in Puerto Rico [79]. Larger, more comprehensive trials with epidemiologic outcomes are planned.
Other population reduction approaches in early development include mosquitocidal fungus [84,85]. Mathematical models are being used to assist in optimizing vector population reduction tools and strategies [86,87]. Early tests of curtains impregnated with insecticide to reduce mosquito populations in Guatemala were encouraging [54], but a subsequent trial in Thailand was not successful [88]. Differences in results may have been due to differences in the structure of houses at the two study locations.
Altered Age Distribution
One strategy, involving insertion of the wMelPop strain of Wolbachia into Ae. aegypti, aims at shifting the vector population age-structure by reducing the number of females that live long enough to become infectious and transmit DENV [89]. Output from mathematical models indicates that such a Wolbachia strain could reduce dengue transmission [90]. Field tests in Australia and Vietnam were, however, disappointing because high fitness costs of the wMelPop strain to infected Ae. aegypti prevented its establishment [91,92]. New life-shorting strains are in development, but are not as encouraging as Wolbachia-transfected virus refractory strains discussed below. Transgenic gene-drive constructs tightly linked with effector genes that shorten life span have been discussed as a control strategy, but none are currently in development.
Behavior Modification
The use of behavior-modifying chemicals and products, such as spatial repellents, that deter blood-seeking mosquitoes from humans, and, thus, reduce or prevent pathogen transmission, is receiving increased research attention [93]. Unlike the traditional use of chemicals that are designed to kill following contact of vectors with a treated surface, these active ingredients are volatile and are released into a space, such as inside a home, to prevent mosquito entry and/or disrupt sensory perception required to detect and locate a human host [93,94]. These same products may also interfere with indoor resting behavior, thereby further enhancing the effect on adult vector populations due to mosquitoes being forced to search and rest under suboptimal environmental conditions required for survival. In Australian houses, metofluthrin has been shown to rapidly reduce biting and, in some cases, kill adult Ae. aegypti without expelling them through open windows [95,96]. Field studies in Vietnam have shown densities of adult Ae. aegypti inside homes treated with metofluthrin plastic latticework strips to be significantly lower than those in untreated houses for six weeks [97]. Randomized, cluster-controlled trials using mosquito coils containing either transfluthrin or metofluthrin in China and Indonesia, respectively, have demonstrated protective efficacy against new malaria infections with an associated reduction in vector densities and biting rates at sentinel homes, respectively [98,99]. A similar, small-scale field trial combining both entomological and epidemiological metrics will begin soon to evaluate the impact of a similar spatial repellent product to interfere with mosquito-human contact in a DENV transmission setting.
Refractory Strains/Genotypes
The most promising near-term approach for rendering mosquito populations incapable of DENV transmission involves artificial infection with a strain of Wolbachia that does not significantly impact mosquito life span and, thus, has high fitness, allowing for rapid field establishment [69]. Field trials in Australia and Vietnam are underway, and the strain is well established in several Australian locations [91,100–106]. Potential for the spread of this strain is being evaluated and new strains are in development [91]. Field trials to assess the epidemiologic impact of Wolbachia-transfected Ae. aegypti on DENV transmission began recently.
An alternative approach is engineering a DNA sequence into the mosquito’s genome that, when transcribed, produces an RNA molecule that blocks DENV replication. An RNAi transmission-blocking strain for DENV-2 was developed and evaluated in the laboratory [107,108]. No field tests have been conducted. Mathematical models indicate that spreading this transgene into wild populations would require far fewer lab-reared mosquitoes than the conditional lethal RIDLR approaches, but would likely require continuous releases lasting about one year [109,110]. These would need to be followed by intermittent releases if there was a small fitness cost associated with the gene for refractoriness [111]. The current strain only inhibits one of the four DENV serotypes. Efforts are underway to develop a transgenic strain that does not transmit any of the DENV serotypes.
Instead of spreading anti-dengue genes into populations through repeated releases, transgenic approaches could potentially link an anti-dengue gene with a gene-drive mechanism that pushes the anti-dengue gene into the mosquito population based on super-Mendelian inheritance. One long-term effort involves a gene drive mechanism, Medea, in which all offspring from a female die if they do not inherit the gene-drive sequence and the linked anti-dengue gene [112]. Although this and other gene-drive mechanisms have worked in fruit flies, to date, they have not been successful in Ae. aegypti. The recent emergence of the CRISPR/Cas9 methodology [74,75], discussed above, has the potential to reinvigorate research aimed at driving anti-dengue genes into Aedes populations.
Considerations regarding Entomological Endpoints of Health Impact
Panel members recognized that critical to the evaluation of new vector control strategies currently under development, as well as a limitation of previous efficacy trials, has been the methodological challenges of documenting changes in vector densities or other entomological endpoints. Surveillance for Aedes vectors of dengue has historically concentrated on immature stages, such as larvae and pupae [113]. This has ranged from container-based indices, such as the Breteau Index and House index, to pupal demographic surveys. With the exception of pupal surveys, immature container indices have generally failed to correlate well with adult populations, let yet alone dengue risk [114–116]. Often container and pupal surveys are compromised by unknown cryptic or inaccessible containers, such as subterranean pits/tanks [117,118] and roof gutters [119], that can serve as major Aedes producers. Recent emphasis has shifted to the measure of adult populations, especially female Ae. aegypti. The advent of adult sampling methods such as aspirators [120,121], Biogents Sentinel traps [122], and gravid traps [123–125] allow for relatively simple and inexpensive means to measure actual adult populations. Measurement of adult female populations provides a much more direct assessment of the impact of interventions on risk of human DENV infection than do immature mosquito surveys [113,114]. Furthermore, adult females that are captured can be assayed for virus and biocontrol agents, such as Wolbachia [125]. The highly variable and clumped distribution of Ae. aegypti indicates, however, that trials need to be sufficiently powered with stratified designs to capture account for this variability. When considering design, the techniques described above fall into two major categories: house-to-house surveys and fixed trap methods. Survey methods, although more susceptible to operator variation, can often cover more houses per unit time (often better spatial coverage) than fixed trap methods, which better capture short-term temporal variation.
Summary and Future Directives
Vector control for dengue can be effective, but, in order for that to happen, implementation must be done thoroughly, comprehensively, and be sustained. Deliberations at this workshop were the first in a three-step process that will develop a framework to guide decision-making on the effective application and integration of dengue vector control interventions. Updating the assessment of vector control options is desirable given the breadth of currently available vector control tools; the increasing number of new interventions under development; expectations that a dengue vaccine will be commercially available in the near future; and the seemingly unabated, expanding burden of dengue illness.
Decreasing dengue will require increased capacity for informed preventive, versus the current reliance on reactive, vector control efforts that use existing and/or novel interventions with improved, more efficient delivery systems. It is time to stop using interventions simply because they have been used in the past or because they are politically popular. Many of the current Ae. aegypti control methods continue to be deployed simply for community visibility without evidence that they prevent disease. The public health cost—benefit of existing tools and strategies needs to be more clearly defined to reduce dengue at regional and global scales. Limited resources in endemic countries must be more efficiently targeted to only those essential activities that will have an epidemiologic impact on specific virus transmission scenarios, even if this requires policy changes and results in implementation challenges. For example, given that the vector control strategies for dengue and chikungunya viruses are broadly similar, the recent and rapid geographic expansion and intensified transmission of chikungunya virus has cost—benefit implications for integration of vector and disease management. In many areas, it may be possible to simultaneously tackle both diseases with the same or similar tools and strategies.
Many of the Ae. aegypti control strategies in development will have time-lagged impacts on adult populations, i.e., Wolbachia and transgenics. Those kinds of interventions will be best applied in sustained, proactive implementation and will likely be inadequate for rapid control of a developing epidemic. In addition to such proactive strategies, dengue prevention will benefit from enhanced capacity for outbreak response, before epidemics have peaked and begun to decline on their own. In this regard, spatial repellents, molecular insecticides, and indoor insecticide application may be particularly amenable to swift deployment with high public health impact.
To reach their full potential for all interventions, proactive and reactive, will require additional thinking about the conceptual basis for strategic innovation, updated guidelines for rigorous assessment of intervention options, and an expanded prevention toolbox that is supported by solid empirical data. Funding agencies that are requiring systematic testing and assessment of novel interventions through the product development pipeline are facilitating these changes. Conversely, most existing interventions were developed in an era when epidemiologic outcomes were not emphasized. Understanding when and how existing tools (i.e., indoor application of existing insecticides) can be best applied will require a shift in attention toward these issues and, interestingly, can benefit from lessons learned from the newer interventions currently in development.
Predicting the effectiveness of existing tools is not currently possible because almost nothing is known about how well they prevent disease. There is a vital need for robust, rigorously designed field trials with epidemiological and entomological outcomes to improve understanding of how well existing tools can reduce DENV transmission and their optimal implementation. Only then can strategy-specific programs be realistically developed and evaluated. Mathematical models indicate that spatially or temporally targeting existing vector control interventions may be more effective than applying them evenly across different locations and times [86,126,127]. Likewise, targeting control on mosquito life stages other than adults (larvae and pupae) may be more effective than previously thought based on the Ross-Macdonald theory [37]. These theoretical advances are helpful, but they are not a replacement for results from field studies and, therefore, new theories require empirical validation.
Among the greatest challenges in dengue vector control is scaling-up local, small-scale successes. Ideally, the aim will be to implement an effective intervention, or combination of interventions, across modern mega-cities as well as large geographic areas that encompass entire countries and transcend national boundaries. The current inability to effectively scale-up and predict the public health impact over large geographic areas explains much of the failure of current dengue prevention programs, despite their potential to be effective at small scales. This roadblock must be overcome. Unless effective control can be scaled-up for mega-cities and regional control, the dengue burden will continue to grow.
There is a growing consensus among dengue experts that eliminating dengue as a public health burden can only be achieved by integrating vector control with vaccines. Integrated strategies will pose new challenges, such as (1) designing vector control strategies that account for variation in spatial and temporal patterns in vaccine rollout and the subsequent alterations that the vaccine may cause in virus transmission dynamics, (2) effective integration of entomologic measures in vaccine trials to guide site characterization and measures of trial impact on disease, (3) integrating epidemiological indexes to measure the capacity of vector control interventions to prevent disease, and (4) designing surveillance systems that can distinguish the epidemiologic impact of vaccines versus vector control. Addressing these issues will be a central part of developing a research agenda for assessing the epidemiological impact of the top vector control candidates, alone and in combination with a DENV vaccine.
Supporting Information
Abbreviations: *Dengue: guidelines for diagnosis, treatment, prevention and control, World Health Organization 2009; ** RCT, randomized cluster trial; SS, small scale field evaluations (<1,000 houses in both intervention and control arms; short duration); LS, large scale field evaluation (>1,000 houses in both intervention and control arms; long duration); RE, relative effectiveness (from Erlanger et al. 2008) 1-relative reduction of density index (BI, CI, HI in all cases cited), 0 indicates elimination whereas 1 indicates no difference between intervention and control; ***unpublished data.
(DOCX)
Green cells indicate that an assessment has been completed successfully, whereas yellow cells indicate that an assessment is currently in progress.
(DOCX)
Abbreviations: E, existing intervention; D, intervention under development; NA, not applicable as intervention testing is currently underway or has yet to be tested under controlled field study designs and/or implemented in public health program.
(DOCX)
Abbreviations: E, existing intervention; D, intervention under development.
(DOCX)
Acknowledgments
We wish to acknowledge the following individuals who contributed significantly to the development of this document through expert panel discussion: Louise Gresham, CEO, Foundation Merieux USA, Inc., Washington DC, United States of America; Georges Thiry, Acting Director, Dengue Vaccine Initiative (DVI), International Vaccine Institute, Seoul, South Korea; Joachim Hombach, Initiative for Vaccine Research (IVR), WHO, Geneva, Switzerland; Charles Wondji, Liverpool School of Tropical Medicine, Liverpool, United Kingdom; Barry Beaty, Colorado State University, Fort Collins, Colorado, USA; Scott O’Neill, Monash University, Clayton, Australia; Hadyn Parry, CEO, Oxitec Ltd., UK; Dawn Wesson, Tulane University, New Orleans, Louisiana, USA; Eva Harris, University of California Berkeley, USA; Roberto Barrera, Centers for Disease Control, Puerto Rico; Deric Cummings, Johns Hopkins University, Baltimore, Maryland, USA; Donald Sheppard, Brandeis University, Waltham, Massachusetts, USA; Gregor Devine, Australian Infectious Diseases Research Centre, Queensland, Australia; and Karen Campbell, San Diego State University, San Diego, California, USA. We also thank Natalie Meyers, E-Research & VecNet Digital Librarian, University of Notre Dame, Indiana, USA, for her assistance in manuscript formatting and reference development.
Funding Statement
This review was supported by the Partnership for Dengue Control (PDC). NLA, RCR, ACM, and TWS acknowledge support from the Bill & Melinda Gates Foundation award OPP1081737. TAP, RCR, and TWS received support from the Research and Policy for Infectious Disease Dynamics program of the Science and Technology Directory, Department of Homeland Security, and Fogarty International Center, National Institutes of Health. FG, ACM, and TWS received support from National Institutes of Health (NIH) grant R01AI091980-01A1. The PDC had no role in study design, data collection and analysis. RT participated in the decision to publish and preparation of the manuscript.
References
- 1. Bhatt S, Gething PW, Brady OJ, Messina JP, Farlow AW, Moyes CL, et al. The global distribution and burden of dengue. Nature. 2013; 496(7446): 504–507. 10.1038/nature12060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. World Health Organization. Sustaining the drive to overcome the global impact of neglected tropical diseases: Second WHO report on neglected diseases. Geneva: World Health Organization;2013. http://www.who.int/iris/handle/10665/77950. [Google Scholar]
- 3. Lambrechts L, Scott TW, Gubler DJ. Consequences of the expanding global distribution of Aedes albopictus for dengue virus transmission. PLoS Negl Trop Dis. 2010; 4(5): 9 10.1371/journal.pntd.0000646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. World Health Organization; Dengue guidelines for diagnosis, treatment, prevention and control. Geneva: World Health Organization;2009. http://www.who.int/iris/handle/10665/44188. [PubMed] [Google Scholar]
- 5. Gunther VJ, Putnak R, Eckels KH, Mammen MP, Scherer JM, Lyons A, et al. A human challenge model for dengue infection reveals a possible protective role for sustained interferon gamma levels during the acute phase of illness. Vaccine. 2011; 29(22): 3895–3904. 10.1016/j.vaccine.2011.03.038 [DOI] [PubMed] [Google Scholar]
- 6. Guy B, Saville M, Lang J. Development of Sanofi Pasteur tetravalent dengue vaccine. Hum Vaccines. 2010; 6(9): 696–705. 10.4161/hv.6.9.12739 [DOI] [PubMed] [Google Scholar]
- 7. Lyons AG. The human dengue challenge experience at the Walter Reed Army Institute of Research. J Infect Dis. 2014; 209549–555. 10.1093/infdis/jiu174 [DOI] [PubMed] [Google Scholar]
- 8. Poo J, Galan F, Forrat R, Zambrano B, Lang J, Dayan GH. Live-attenuated tetravalent dengue vaccine in dengue-naive children, adolescents, and adults in Mexico City randomized controlled Phase 1 trial of safety and immunogenicity. Pediatr Infect Dis J. 2011; 30(1): E9–E17. 10.1097/INF.0b013e3181fe05af [DOI] [PubMed] [Google Scholar]
- 9. Sabchareon A, Wallace D, Sirivichayakul C, Limkittikul K, Chanthavanich P, Suvannadabba S, et al. Protective efficacy of the recombinant, live-attenuated, cyd tetravalent dengue vaccine in thai schoolchildren: A randomised, controlled Phase 2b trial. Lancet. 2012; 380(9853): 1559–1567. 10.1016/s0140-6736(12)61428-7 [DOI] [PubMed] [Google Scholar]
- 10. Sun W, Eckels KH, Putnak JR, Lyons AG, Thomas SJ, Vaughn DW, et al. Experimental dengue virus challenge of human subjects previously vaccinated with live attenuated tetravalent dengue vaccines. J Infect Dis. 2013; 207(5): 700–708. 10.1093/infdis/jis744 [DOI] [PubMed] [Google Scholar]
- 11. Capeding MR, Tran NH, Hadinegoro SRS, Ismail HIHJM, Chotpitayasunondh T, Chua MN, et al. Clinical efficacy and safety of a novel tetravalent dengue vaccine in healthy children in Asia: A Phase 3, randomised, observer-masked, placebo-controlled trial. The Lancet. 2014; 384(9951): 1358–1365. 10.1016/S0140-6736(14)61060-6 [DOI] [PubMed] [Google Scholar]
- 12. Monath TP. Yellow fever and dengue—the interactions of virus, vector and host in the reemergence of epidemic disease. Semin Virol. 1994; 5(2): 133–145. 10.1006/smvy.1994.1014 [DOI] [Google Scholar]
- 13. Monath TP. Dengue: The risk to developed and developing countries. Proc Natl Acad Sci U S A. 1994; 91(7): 2395–2400. 10.1073/pnas.91.7.2395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ooi EE, Goh KT, Gubler DJ. Dengue prevention and 35 years of vector control in Singapore. Emerg Infect Dis. 2006; 12(6): 887–893. 10.3201/10.3201/eid1206.051210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Arias J. El dengue en Cuba. Revista Panamericana de Salud Pública. 2002; 11221–222. 10.1590/S1020-49892002000400002 [DOI] [PubMed] [Google Scholar]
- 16. Gessa JAA, Gonzalez RF. Application of environmental management principles in the program for eradication of Aedes (Stegomyia) aegypti (Linneus, 1762) in the republic of Cuba, 1984. Bull Pan Am Health Organ. 1986; 20(2): 186–193. [PubMed] [Google Scholar]
- 17. Kouri G, Guzman MG, Valdes L, Carbonel I, del Rosario D, Vazquez S, et al. Reemergence of dengue in Cuba: A 1997 epidemic in Santiago de Cuba. Emerg Infect Dis. 1998; 4(1): 89–92. 10.3201/eid0401.980111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Egger JR, Ooi EE, Kelly DW, Woolhouse ME, Davies CR, Coleman PG. Reconstructing historical changes in the force of infection of dengue fever in Singapore: Implications for surveillance and control. Bulletin of the World Health Organization. 2008; 86(3): 187–196. 10.2471/blt.07.040170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Scott TW, Morrison AC. Vector dynamics and transmission of dengue virus: Implications for dengue surveillance and prevention strategies: vector dynamics and dengue prevention In: Rothman AL, editor. Dengue virus. Berlin: Springer-Verlag Berlin; 2010. pp. 115–128. 10.1007/978-3-642-02215-9_9 [DOI] [PubMed] [Google Scholar]
- 20. Stoddard ST, Wearing HJ, Reiner RC Jr., Morrison AC, Astete H, Vilcarromero S, et al. Long-term and seasonal dynamics of dengue in Iquitos, Peru. PLoS Negl Trop Dis. 2014; 8(7): e3003 10.1371/journal.pntd.0003003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gubler D. Dengue, urbanization and globalization: The unholy trinity of the 21st century. Int J Infect Dis. 2012; 16E2–E2. 10.1016/j.ijid.2012.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bhattarai A, Ali AS, Kachur SP, Martensson A, Abbas AK, Khatib R, et al. Impact of artemisinin-based combination therapy and insecticide-treated nets on malaria burden in Zanzibar. PLoS Med. 2007; 4(11): 1784–1790. 10.1371/journal.pmed.0040309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Griffin JT, Hollingsworth TD, Okell LC, Churcher TS, White M, Hinsley W, et al. Reducing plasmodium falciparum malaria transmission in Africa: A model-based evaluation of intervention strategies. PLoS Med. 2010; 7(8): 17 10.1371/journal.pmed.1000324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Mayor S. Who report shows progress in efforts to reduce malaria incidence. BMJ. 2008; 337 10.1136/bmj.a1678 [DOI] [PubMed] [Google Scholar]
- 25. World Health Organization; World malaria report 2008. Geneva, Switzerland: World Health Organization;2008. http://www.who.int/iris/handle/10665/43939 [Google Scholar]
- 26. Bockarie MJ, Pedersen EM, White GB, Michael E. Role of vector control in the global program to eliminate lymphatic filariasis. Annual review of entomology. Palo Alto: Annual Reviews; 2009. pp. 469–487. 10.1146/annurev.ento.54.110807.090626 [DOI] [PubMed] [Google Scholar]
- 27. Burkot TR, Taleo G, Toeaso V, Ichimori K. Progress towards, and challenges for, the elimination of filariasis from Pacific-Island communities. Ann Trop Med Parasitol. 2002; 96S61–S69. 10.1179/000349802125002419 [DOI] [PubMed] [Google Scholar]
- 28. Eigege A, Kal A, Miri E, Sallau A, Umaru J, Mafuyai H, et al. Long-lasting insecticidal nets are synergistic with mass drug administration for interruption of lymphatic filariasis transmission in Nigeria. PLoS Negl Trop Dis. 2013; 7(10): 4 10.1371/journal.pntd.0002508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Maxwell CA, Mohammed K, Kisumku U, Curtis CF. Can vector control play a useful supplementary role against bancroftian filariasis? Bulletin of the World Health Organization. 1999; 77(2): 138–143. http://www.who.int/iris/handle/10665/56253 [PMC free article] [PubMed] [Google Scholar]
- 30. Reimer LJ, Thomsen EK, Tisch DJ, Henry-Halldin CN, Zimmerman PA, Baea ME, et al. Insecticidal bed nets and filariasis transmission in Papua New Guinea. N Engl J Med. 2013; 369(8): 745–753. 10.1056/NEJMoa1207594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Sunish IP, Rajendran R, Mani TR, Munirathinam A, Dash AP, Tyagi BK. Vector control complements mass drug administration against bancroftian filariasis in Tirukoilur, India. Bulletin of the World Health Organization. 2007; 85(2): 138–145. 10.2471/blt.06.029389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. van den Berg H, Velayudhan R, Ebol A, Catbagan BH Jr., Turingan R, Tuso M, et al. Operational efficiency and sustainability of vector control of malaria and dengue: Descriptive case studies from the Philippines. Malar J. 2012; 11269 10.1186/1475-2875-11-269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Johansson MA, Hombach J, Cummings DAT. Models of the impact of dengue vaccines: A review of current research and potential approaches. Vaccine. 2011; 29(35): 5860–5868. 10.1016/j.vaccine.2011.06.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Smith DL, Perkins TA, Reiner RC, Barker CM, Niu TC, Chaves LF, et al. Recasting the theory of mosquito-borne pathogen transmission dynamics and control. Trans Roy Soc Trop Med Hyg. 2014; 108(4): 185–197. 10.1093/trstmh/tru026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. World Health Organization; Handbook for integrated vector management. Geneva, Switzerland: World Health Organization;2012. http://www.who.int/iris/handle/10665/44768 [Google Scholar]
- 36. Smith DL, Battle KE, Hay SI, Barker CM, Scott TW, McKenzie FE. Ross, Macdonald, and a theory for the dynamics and control of mosquito-transmitted pathogens. PLoS Pathog. 2012; 8(4): 13 10.1371/journal.ppat.1002588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Smith DL, Perkins TA, Tusting LS, Scott TW, Lindsay SW. Mosquito population regulation and larval source management in heterogeneous environments. PLoS One. 2013; 8(8): e71247 10.1371/journal.pone.0071247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Pettit WJ, Whelan PI, McDonnell J, Jacups SP. Efficacy of alpha-cypermethrin and lambda-cyhalothrin applications to prevent Aedes breeding in tires. J Am Mosq Control Assoc. 2010; 26(4): 387–397. 10.2987/09-5962.1 [DOI] [PubMed] [Google Scholar]
- 39. Nguyen HT, Whelan PI, Shortus MS, Jacups SP. Evaluation of bifenthrin applications in tires to prevent Aedes mosquito breeding. J Am Mosq Control Assoc. 2009; 25(1): 74–82. 10.2987/08-5752.1 [DOI] [PubMed] [Google Scholar]
- 40. Nathan MB, Giglioli ME. Eradication of Aedes aegypti on Cayman Brac and Little Cayman, West Indies, with Abate (temephos) in 1970–1971. Bull Pan Am Health Organ. 1982; 16(1): 28–39. [PubMed] [Google Scholar]
- 41. Lloyd LS. Strategic report 7: Best practices for dengue prevention and control in the Americas. Washington, DC: Environmental health project USAID Bureau for Latin America and Caribbean; 2003. [Google Scholar]
- 42. Gubler DJ. Aedes aegypti and Aedes aegypti-borne disease control in the 1990s—top down or bottom up. Am J Trop Med Hyg. 1989; 40(6): 571–578. [DOI] [PubMed] [Google Scholar]
- 43. Ritchie SA, Long S, Smith G, Pyke A, Knox TB. Entomological investigations in a focus of dengue transmission in Cairns, Queensland, Australia, by using the sticky ovitraps. J Med Entomol. 2004; 41(1): 1–4. 10.1603/0022-2585-41.1.1 [DOI] [PubMed] [Google Scholar]
- 44. Vazquez-Prokopec GM, Kitron U, Montgomery B, Horne P, Ritchie SA. Quantifying the spatial dimension of dengue virus epidemic spread within a tropical urban environment. PLoS Negl Trop Dis. 2010; 4(12). 10.1371/journal.pntd.0000920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Tun-Lin W, Lenhart A, Nam VS, Rebollar-Tellez E, Morrison AC, Barbazan P, et al. Reducing costs and operational constraints of dengue vector control by targeting productive breeding places: A multi-country non-inferiority cluster randomized trial. Trop Med Int Health. 2009; 14(9): 1143–1153. 10.1111/j.1365-3156.2009.02341.x [DOI] [PubMed] [Google Scholar]
- 46. Arunachalam N, Tyagi BK, Samuel M, Krishnamoorthi R, Manavalan R, Tewari SC, et al. Community-based control of Aedes aegypti by adoption of eco-health methods in Chennai City, India. Pathog Glob Health. 2012; 106(8): 488–496. 10.1179/2047773212y.0000000056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Caceres-Manrique FdM, Angulo-Silva ML, Vesga-Gomez C. Efficacy of the social mobilization and the social participation in dengue control measures. Biomedica: revista del Instituto Nacional de Salud. 2010; 30(4): 539–550. 10.7705/biomedica.v30i4.292 [DOI] [PubMed] [Google Scholar]
- 48. Vanlerberghe V, Toledo ME, Rodriguez M, Gomez D, Baly A, Benitez JR, et al. Community involvement in dengue vector control: Cluster randomised trial. BMJ. 2009; 338 10.1136/bmj.b1959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Scientific Working Group on Dengue. Report of the scientific working group meeting on dengue, Geneva, 1–5 october 2006;2006. http://www.who.int/iris/handle/10665/69787
- 50. Reiter P, Nathan MB. Guidelines for assessing the efficacy of insecticidal space sprays for control of the dengue vector Aedes aegypti. Geneva: World Health Organization; 2001. [Google Scholar]
- 51. Horstick O, Runge-Ranzinger S, Nathan MB, Kroeger A. Dengue vector control services: How do they work? A systematic literature review and country case studies. Trans Roy Soc Trop Med Hyg. 2010; 104(6): 379–386. 10.1016/j.trstmh.2009.07.027 [DOI] [PubMed] [Google Scholar]
- 52. Roberts D, Tren R, Bate R, Zambone J. The excellent powder: DDT's political and scientific history. Indianapolis, IN: Dog Ear Pub; 2010. [Google Scholar]
- 53. Frances SP, Sithiprasasna R, Linthicum KJ. Laboratory evaluation of the response of Aedes aegypti and Aedes albopictus uninfected and infected with dengue virus to Deet. J Med Entomol. 2011; 48(2): 334–336. 10.1603/me10120 [DOI] [PubMed] [Google Scholar]
- 54. Kroeger A, Lenhart A, Ochoa M, Villegas E, Levy M, Alexander N, et al. Effective control of dengue vectors with curtains and water container covers treated with insecticide in Mexico and Venezuela: Cluster randomised trials. BMJ. 2006; 332(7552): 1247–1250A. 10.1136/bmj.332.7552.1247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Erlanger TE, Keiser J, Utzinger J. Effect of dengue vector control interventions on entomological parameters in developing countries: A systematic review and meta-analysis. Med Vet Entomol. 2008; 22(3): 203–221. 10.1111/j.1365-2915.2008.00740.x [DOI] [PubMed] [Google Scholar]
- 56. Garcia GP, Flores AE, Fernandez-Salas I, Saavedra-Rodriguez K, Reyes-Solis G, Lozano-Fuentes S, et al. Recent rapid rise of a permethrin knock down resistance allele in Aedes aegypti in Mexico. PLoS Negl Trop Dis. 2009; 3(10): 10 10.1371/journal.pntd.0000531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Marcombe S, Darriet F, Tolosa M, Agnew P, Duchon S, Etienne M, et al. Pyrethroid resistance reduces the efficacy of space sprays for dengue control on the island of Martinique (caribbean). PLoS Negl Trop Dis. 2011; 5(6): e1202 10.1371/journal.pntd.0001202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Marcombe S, Darriet F, Tolosa M, Agnew P, Etienne M, Yp-Tcha MM, et al. Resistance of Aedes aegypti to insecticides in Martinique and implications for dengue vector control. Trop Med Int Health. 2011; 16(s1): 284–284. 10.1111/j.1365-3156.2011.02861.x [DOI] [Google Scholar]
- 59. Ranson H, N'Guessan R, Lines J, Moiroux N, Nkuni Z, Corbel V. Pyrethroid resistance in African anopheline mosquitoes: What are the implications for malaria control? Trends Parasitol. 2011; 27(2): 91–98. 10.1016/j.pt.2010.08.004 [DOI] [PubMed] [Google Scholar]
- 60. Hemingway J. The role of vector control in stopping the transmission of malaria: Threats and opportunities. Philos Trans R Soc B-Biol Sci. 2014; 369(1645): 5 10.1098/rstb.2013.0431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.DeSimone JM. Molecular mosquitocides. http://desimone-group.chem.unc.edu/?p=1855. Accessed: 8/14/2014.
- 62. Phuc HK, Andreasen MH, Burton RS, Vass C, Epton MJ, Pape G, et al. Late-acting dominant lethal genetic systems and mosquito control. BMC Biol. 2007; 511 10.1186/1741-7007-5-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Harris AF, McKemey AR, Nimmo D, Curtis Z, Black I, Morgan SA, et al. Successful suppression of a field mosquito population by sustained release of engineered male mosquitoes. Nat Biotechnol. 2012; 30(9): 828–830. 10.1038/nbt.2350 [DOI] [PubMed] [Google Scholar]
- 64. Lacroix R, McKemey AR, Raduan N, Wee LK, Ming WH, Ney TG, et al. Open field release of genetically engineered sterile male Aedes aegypti in Malaysia. Plos One. 2012; 7(8). 10.1371/journal.pone.0042771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Oxitec Ltd. Mandacaru field trial report—press summary: Oxitec report 96% suppression of the dengue mosquito in Brazilian trials. Oxitec Ltd. 2013; http://www.oxitec.com/press-release-oxitec-report-96-suppression-of-the-dengue-mosquito-in-brazilian-trials/. Accessed: 8/14/2014.
- 66.Biofábrica Moscamed Brasil. Projeto aedes transgênico. http://www.moscamed.org.br/2012/projeto-aedes/1. Accessed: 08/19/2014.
- 67.Oxitec. Aedes aegypti ox3604c. Oxitec Ltd. http://www.oxitec.com/health/our-products/aedes-agypti-ox3604c Accessed: 8/20/2014.
- 68. Wise de Valdez MR, Nimmo D, Betz J, Gong H-F, James AA, Alphey L, et al. Genetic elimination of dengue vector mosquitoes. Proc Natl Acad Sci U S A. 2011; 108(12): 4772–4775. 10.1073/pnas.1019295108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Facchinelli L, Valerio L, Ramsey JM, Gould F, Walsh RK, Bond G, et al. Field cage studies and progressive evaluation of genetically-engineered mosquitoes. PLoS Negl Trop Dis. 2013; 7(1): 12 10.1371/journal.pntd.0002001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Legros M, Xu C, Morrison A, Scott TW, Lloyd AL, Gould F. Modeling the dynamics of a non-limited and a self-limited gene drive system in structured Aedes aegypti populations. PLoS One. 2013; 8(12): e83354 10.1371/journal.pone.0083354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Alphey L, Benedict M, Bellini R, Clark GG, Dame DA, Service MW, et al. Sterile-insect methods for control of mosquito-borne diseases: An analysis. Vector-Borne Zoonotic Dis. 2010; 10(3): 295–311. 10.1089/vbz.2009.0014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. McGraw EA, O'Neill SL. Beyond insecticides: New thinking on an ancient problem. Nature reviews Microbiology. 2013; 11(3): 181–193. 10.1038/nrmicro2968 [DOI] [PubMed] [Google Scholar]
- 73. Galizi R, Doyle LA, Menichelli M, Bernardini F, Deredec A, Burt A, et al. A synthetic sex ratio distortion system for the control of the human malaria mosquito. Nature communications. 2014; 53977 10.1038/ncomms4977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Esvelt KM, Smidler AL, Catteruccia F, Church GM. Concerning RNA-guided gene drives for the alteration of wild populations. eLife. 2014; e03401 10.7554/eLife.03401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Oye KA, Esvelt K, Appleton E, Catteruccia F, Church G, Kuiken T, et al. Biotechnology. Regulating gene drives. Science (New York, NY). 2014; 345(6197): 626–628. 10.1126/science.1254287 [DOI] [PubMed] [Google Scholar]
- 76. Lok CK, Kiat NS, Koh TK. An autocidal ovitrap for the control and possible eradication of Aedes aegypti . Southeast Asian J Trop Med Public Health. 1977; 8(1): 56 [PubMed] [Google Scholar]
- 77. Perich MJ, Kardec A, Braga IA, Portal IF, Burge R, Zeichner BC, et al. Field evaluation of a lethal ovitrap against dengue vectors in Brazil. Med Vet Entomol. 2003; 17(2): 205–210. 10.1046/j.1365-2915.2003.00427.x [DOI] [PubMed] [Google Scholar]
- 78. Sithiprasasna R, Mahapibul P, Noigamol C, Perich MJ, Zeichner BC, Burge B, et al. Field evaluation of a lethal ovitrap for the control of Aedes aegypti (Diptera: Culicidae) in Thailand. J Med Entomol. 2003; 40(4): 455–462. 10.1603/0022-2585-40.4.455 [DOI] [PubMed] [Google Scholar]
- 79. Barrera R, Amador M, Acevedo V, Caban B, Felix G, Mackay AJ. Use of the CDC autocidal gravid ovitrap to control and prevent outbreaks of Aedes aegypti (Diptera: Culicidae). J Med Entomol. 2014; 51(1): 145–154. 10.1603/me13096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Brannon K. Toxic traps prey on mosquito’s motherly instincts. Tulane University. 2010; Available: http://tulane.edu/news/newwave/111910_mosquitoes.cfm.
- 81.Brannon K. Trap tricks pregnant mosquitoes with enticingly lethal maternity ward. Tulane University. 2010; Available: http://tulane.edu/news/newwave/111910_mosquitoes.cfm. Accessed: 8/19/2014.
- 82.Wesson D. Personal communication.
- 83.Wesson D. Unpublished data.
- 84. Luz C, Tai MHH, Santos AH, Rocha LFN, Albernaz DAS, Silva HHG. Ovicidal activity of entomopathogenic hyphomycetes on Aedes aegypti (Diptera: Culicidae) under laboratory conditions. J Med Entomol. 2007; 44(5): 799–804. 10.1603/0022-2585(2007)44[799:oaoeho]2.0.co;2 [DOI] [PubMed] [Google Scholar]
- 85. Scholte E-J, Takken W, Knols BGJ. Infection of adult Aedes aegypti and Ae. albopictus mosquitoes with the entomopathogenic fungus metarhizium anisopliae. Acta Trop. 2007; 102(3): 151–158. 10.1016/j.actatropica.2007.04.011 [DOI] [PubMed] [Google Scholar]
- 86. Campbell KM, Lin CD, Iamsirithawom S, Scott TW. The complex relationship between weather and dengue virus transmission in Thailand. Am J Trop Med Hyg. 2013; 89(6): 1066–1080. 10.4269/ajtmh.13-0321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Negreiros M, Xavier AE, Xavier AFS, Maculan N, Michelon P, Lima JWO, et al. Optimization models, statistical and dss tools for prevention and combat of dengue disease In: Jao C, editor. Optimization Models, Statistical and DSS Tools for Prevention and Combat of Dengue Disease, Efficient Decision Support Systems—Practice and Challenges in Biomedical Related Domain: InTech;2011. 10.5772/1685 [DOI] [Google Scholar]
- 88. Lenhart A, Trongtokit Y, Alexander N, Apiwathnasorn C, Satimai W, Vanlerberghe V, et al. A cluster-randomized trial of insecticide-treated curtains for dengue vector control in Thailand. Am J Trop Med Hyg. 2013; 88(2): 254–259. 10.4269/ajtmh.2012.12-0423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. McMeniman CJ, Lane RV, Cass BN, Fong AW, Sidhu M, Wang YF, et al. Stable introduction of a life-shortening Wolbachia infection into the mosquito Aedes aegypti . Science (New York, NY). 2009; 323(5910): 141–144. 10.1126/science.1165326 [DOI] [PubMed] [Google Scholar]
- 90. Hughes H, Britton NF. Modelling the use of Wolbachia to control dengue fever transmission. Bull Math Biol. 2013; 75(5): 796–818. 10.1007/s11538-013-9835-4 [DOI] [PubMed] [Google Scholar]
- 91.O'Neill SL. Personal communication.
- 92. Yeap HL, Axford JK, Popovici J, Endersby NM, Iturbe-Ormaetxe I, Ritchie SA, et al. Assessing quality of life-shortening Wolbachia-infected Aedes aegypti mosquitoes in the field based on capture rates and morphometric assessments. Parasites & Vectors. 2014; 7 10.1186/1756-305-7-58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Achee NL, Bangs MJ, Farlow R, Killeen GF, Lindsay S, Logan JG, et al. Spatial repellents: From discovery and development to evidence-based validation. Malar J. 2012; 11(164): 9 10.1186/1475-2875-11-164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. World Health Organization, WHO Pesticide Evaluation Scheme. Guidelines for Efficacy Testing of Spatial Repellents. Geneva: World Health Organization;2013. uri:http://www.who.int/iris/handle/10665/78142 [Google Scholar]
- 95. Rapley LP, Russell RC, Montgomery BL, Ritchie SA. The effects of sustained release metofluthrin on the biting, movement, and mortality of Aedes aegypti in a domestic setting. Am J Trop Med Hyg. 2009; 81(1): 94–99. [PubMed] [Google Scholar]
- 96. Ritchie S, Devine G. Confusion, knock-down and kill of Aedes aegypti using metofluthrin in domestic settings: A powerful tool to prevent dengue transmission? Parasites & Vectors. 2013; 6(262). 10.1186/1756-3305-6-262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Kawada H, Maekawa Y, Takagi M. Field trial on the spatial repellency of metofluthrin-impregnated plastic strips for mosquitoes in shelters without walls (beruga) in Lombok, Indonesia. J Vector Ecol. 2005; 30(2): 181–185. [PubMed] [Google Scholar]
- 98. Hill N, Zhou H, Wang P, Guo X, Carneiro I, Moore S. A household randomized, controlled trial of the efficacy of 0.03% transfluthrin coils alone and in combination with long-lasting insecticidal nets on the incidence of Plasmodium falciparum and Plasmodium vivax malaria in Western Yunnan Province, China. Malar J. 2014; 13(1): 208 uri:http://www.malariajournal.com/content/13/1/208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Syafruddin D, Bangs MJ, Sidik D, Elyazar I, Asih PB, Chan K, et al. Impact of spatial repellents on malaria incidence in two villages in Sumba, Indonesia. Am J Trop Med Hyg. 2014; 91(6): 1079–87. 10.4269/ajtmh.13-0735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Frentiu FD, Zakir T, Walker T, Popovici J, Pyke AT, van den Hurk A, et al. Limited dengue virus replication in field-collected Aedes aegypti mosquitoes infected with Wolbachia . PLoS Negl Trop Dis. 2014; 8(2): e2688 10.1371/journal.pntd.0002688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Hoffmann AA, Montgomery BL, Popovici J, Iturbe-Ormaetxe I, Johnson PH, Muzzi F, et al. Successful establishment of Wolbachia in Aedes populations to suppress dengue transmission. Nature. 2011; 476(7361): 454–457. 10.1038/nature10356 [DOI] [PubMed] [Google Scholar]
- 102. McNaughton D, Duong TT. Designing a community engagement framework for a new dengue control method: A case study from central Vietnam. PLoS Negl Trop Dis. 2014; 8(5): e2794 10.1371/journal.pntd.0002794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Cairns field trial update: March 2014. Eliminate Dengue Australia. 2014; Available: http://www.eliminatedengue.com/australia/progress/article/262/year/2014/month/3/pg/1. Accessed: 8/19/2014.
- 104.Cairns field trial update: September 2013. Eliminate Dengue Australia. 2013; Available: http://www.eliminatedengue.com/australia/progress/article/236/year/2013/month/9/pg/1. Accessed: 8/19/2014.
- 105.Tri Nguyen Island field trial update—September 2013 Eliminate Denge Vietnam. 2013; Available: http://www.eliminatedengue.com/library/publication/document/field_trial_update/tni_trial_update/2013.09.03_tni_trial_update_english_final.pdf http://www.eliminatedengue.com/library/publication/document/field_trial_update/tni_trial_update/2013.09.03_tni_trial_update_vietnamese_final.pdf. Accessed: 8/19/2014.
- 106.Second Wolbachia field trial begins in vietnam. Eliminate Dengue Program. 2014; Available: http://www.eliminatedengue.com/vietnam/progress/article/286/year/2014/month/5/pg/1. Accessed: 8/19/2014.
- 107. Franz AW, Sanchez-Vargas I, Adelman ZN, Blair CD, Beaty BJ, James AA, et al. Engineering RNA interference-based resistance to dengue virus type 2 in genetically modified Aedes aegypti . Proc Natl Acad Sci U S A. 2006; 103(11): 4198–4203. 10.1073/pnas.0600479103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Sanchez-Vargas I, Travanty EA, Keene KM, Franz AW, Beaty BJ, Blair CD, et al. RNA interference, arthropod-borne viruses, and mosquitoes. Virus research. 2004; 102(1): 65–74. 10.1016/j.virusres.2004.01.017 [DOI] [PubMed] [Google Scholar]
- 109. Okamoto KW, Robert MA, Gould F, Lloyd AL. Feasible introgression of an anti-pathogen transgene into an urban mosquito population without using gene-drive. PLoS Negl Trop Dis. 2014; 8(7): e2827 10.1371/journal.pntd.0002827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Okamoto KW, Robert MA, Lloyd AL, Gould F. A reduce and replace strategy for suppressing vector-borne diseases: Insights from a stochastic, spatial model. PLoS ONE. 2013; 8(12): e81860 10.1371/journal.pone.0081860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Franz AW, Sanchez-Vargas I, Raban RR, Black WCt, James AA, Olson KE. Fitness impact and stability of a transgene conferring resistance to dengue-2 virus following introgression into a genetically diverse Aedes aegypti strain. PLoS Negl Trop Dis. 2014; 8(5): e2833 10.1371/journal.pntd.0002833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Akbari OS, Chen C-H, Marshall JM, Huang H, Antoshechkin I, Hay BA. Novel synthetic medea selfish genetic elements drive population replacement in Drosophila; a theoretical exploration of medea-dependent population suppression. ACS Synth Biol. 2012; 3(12): 915–928. 10.1021/sb300079h [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Morrison AC, Zielinski-Gutierrez E, Scott TW, Rosenberg R. Defining challenges and proposing solutions for control of the virus vector Aedes aegypti . PLos Med. 2008; 5(3): 362–366. 10.1371/journal.pmed.0050068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Bowman LR, Runge-Ranzinger S, McCall PJ. Assessing the relationship between vector indices and dengue transmission: A systematic review of the evidence. PLoS Negl Trop Dis. 2014; 8(5). 10.1371/journal.pntd.0002848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Focks DA, Brenner RJ, Hayes J, Daniels E. Transmission thresholds for dengue in terms of Aedes aegypti pupae per person with discussion of their utility in source reduction efforts. Am J Trop Med Hyg. 2000; 62(1): 11–18. [PubMed] [Google Scholar]
- 116. Focks DA, Chadee DD. Pupal survey: An epidemiologically significant surveillance method for Aedes aegypti: An example using data from Trinidad. Am J Trop Med Hyg. 1997; 56(2): 159–167. [DOI] [PubMed] [Google Scholar]
- 117. Burke R, Barrera R, Lewis M, Kluchinsky T, Claborn D. Septic tanks as larval habitats for the mosquitoes Aedes aegypti and Culex quinquefasciatus in Playa-Playita, Puerto Rico. Med Vet Entomol. 2010; 24(2): 117–123. 10.1111/j.1365-2915.2010.00864.x [DOI] [PubMed] [Google Scholar]
- 118. Montgomery BL, Ritchie SA, Hart AJ, Long SA, Walsh ID. Subsoil drain sumps are a key container for Aedes aegypti in Cairns, Australia. J Am Mosq Control Assoc. 2004; 20(4): 365–369. [PubMed] [Google Scholar]
- 119. Montgomery BL, Ritchie SA. Roof gutters: A key container for Aedes aegypti and Ochlerotatus notoscriptus (Diptera: Culicidae) in Australia. Am J Trop Med Hyg. 2002; 67(3): 244–246. [DOI] [PubMed] [Google Scholar]
- 120. Clark GG, Seda H, Gubler DJ. Use of the "CDC backpack aspirator" for surveillance of Aedes aegypti in San Juan, Puerto Rico. J Am Mosq Control Assoc. 1994; 10(1): 119–124. [PubMed] [Google Scholar]
- 121. Vazquez-Prokopec GM, Galvin WA, Kelly R, Kitron U. A new, cost-effective, battery-powered aspirator for adult mosquito collections. J Med Entomol. 2009; 46(6): 1256–1259. 10.1603/033.046.0602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Krockel U, Rose A, Eiras AE, Geier M. New tools for surveillance of adult yellow fever mosquitoes: Comparison of trap catches with human landing rates in an urban environment. J Am Mosq Control Assoc. 2006; 22(2): 229–238. 10.2987/8756-971X(2006)22[229:NTFSOA]2.0.CO;2 [DOI] [PubMed] [Google Scholar]
- 123. Chadee DD, Ritchie SA. Efficacy of sticky and standard ovitraps for Aedes aegypti in Trinidad, West Indies. Journal of Vector Ecology. 2010; 35(2): 395–400. 10.1111/j.1948-7134.2010.00098.x [DOI] [PubMed] [Google Scholar]
- 124. Mackay AJ, Amador M, Barrera R. An improved autocidal gravid ovitrap for the control and surveillance of Aedes aegypti . Parasites & Vectors. 2013; 6 10.1186/1756-3305-6-225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Ritchie SA, Buhagiar TS, Townsend M, Hoffmann A, van den Hurk AF, McMahon JL, et al. Field validation of the gravid Aedes trap (gat) for collection of Aedes aegypti (Diptera: Culicidae). J Med Entomol. 2014; 51(1): 210–219. 10.1603/me13105 [DOI] [PubMed] [Google Scholar]
- 126. Lloyd-Smith JO, Schreiber SJ, Kopp PE, Getz WM. Superspreading and the effect of individual variation on disease emergence. Nature. 2005; 438(7066): 355–359. 10.1038/nature04153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Woolhouse ME, Dye C, Etard JF, Smith T, Charlwood JD, Garnett GP, et al. Heterogeneities in the transmission of infectious agents: Implications for the design of control programs. In: Proc Natl Acad Sci U S A. January 7 1997. pp. 338–342. uri:http://www.ncbi.nlm.nih.gov/pmc/articles/PMC19338/pdf/pq000338.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Abbreviations: *Dengue: guidelines for diagnosis, treatment, prevention and control, World Health Organization 2009; ** RCT, randomized cluster trial; SS, small scale field evaluations (<1,000 houses in both intervention and control arms; short duration); LS, large scale field evaluation (>1,000 houses in both intervention and control arms; long duration); RE, relative effectiveness (from Erlanger et al. 2008) 1-relative reduction of density index (BI, CI, HI in all cases cited), 0 indicates elimination whereas 1 indicates no difference between intervention and control; ***unpublished data.
(DOCX)
Green cells indicate that an assessment has been completed successfully, whereas yellow cells indicate that an assessment is currently in progress.
(DOCX)
Abbreviations: E, existing intervention; D, intervention under development; NA, not applicable as intervention testing is currently underway or has yet to be tested under controlled field study designs and/or implemented in public health program.
(DOCX)
Abbreviations: E, existing intervention; D, intervention under development.
(DOCX)