Abstract
Childhood dystonia is a movement disorder characterized by involuntary sustained or intermittent muscle contractions causing twisting and repetitive movements, abnormal postures, or both (Sanger et al. 2003). Dystonia is a devastating neurological condition that prevents the acquisition of normal motor skills during critical periods of development in children. Moreover, it is particularly debilitating in children when dystonia affects the upper extremities such that learning and consolidation of common daily motor actions are impeded. Thus, the treatment and rehabilitation of dystonia is a challenge that continuously requires exploration of novel interventions. This review will initially describe the underlying neurophysiological mechanisms of the motor impairments found in childhood dystonia followed by the clinical measurement tools that are available to document the presence and severity of symptoms. Finally, we will discuss the state-of-the-art of therapeutic options for childhood dystonia, with particular emphasis on emergent and innovative strategies.
Introduction
Childhood dystonia can lead to lifelong disability, thus it represents a significant healthcare and rehabilitation challenge. Currently, dyskinetic cerebral palsy (CP), a type of CP primarily associated with damage to the basal ganglia,1 is the most common cause of dystonia in children. It accounts for approximately 10–15% of cases of cerebral palsy.2,3 It has a total incidence of 0.15–0.25 per 1,000 in Western countries with an expected prevalence in the US of 50,000–75,000.4 Dystonia in children manifests differently than in adults, partly because childhood dystonia is a dynamic disorder that prevents the acquisition of typical motor skills during critical periods of learning and skill development.5,6 This is particularly trying when dystonia affects the upper extremities, as when common motor actions associated with self-care and play are profoundly limited and when there are harmful consequences for school participation and social interaction.
It is important that the outcome measures chosen for this population clearly assess the symptoms of dystonia and the associated function. Sensitive outcome measures not only support the benefit of medical and rehabilitation intervention, but they allow for the comparison of different treatment options. Given the influence of dystonia on everyday life and the ongoing search for effective treatments, the use of targeted outcome measures is crucial.
Current intervention options, including physical and occupational therapies, pharmacological approaches, and deep brain stimulation, are often not successful or only partially successful in controlling symptoms.7–9 As a result, there is a need to investigate new noninvasive options for treating dystonia in children.
The purpose of this paper is to describe the pathophysiology of childhood dystonia, review the clinical measures used to assess severity and motor impairments, and describe the state-of-the-art for therapeutic interventions.
Definition
A National Institutes of Health taskforce on childhood motor disorders established the following consensus-based definition of dystonia: “A movement disorder in which involuntary sustained or intermittent muscle contractions cause twisting and repetitive movements, abnormal postures, or both”.5 The etymology of dystonia originates from Greek that means abnormal (dys) tone (tonia), although tone is not always abnormal in dystonia. “Dystonia can be classified by the affected body region(s) as focal if it affects a single body part, segmental if it affects one or more contiguous body parts, multifocal if it affects two or more noncontiguous body parts, generalized if it affects one leg and the trunk plus one other body part, or both legs plus one other body part, and hemidystonia if it affects only one half of the body” (p. 624).10 Dystonia is often classified by etiology as primary when it is the most salient feature of an identified genetic disorder or the origin is unknown, and secondary when it is a symptom of another known underlying disease, such as brain injury, encephalitis, vascular diseases, autoimmune disorders, cerebral malformations, metabolic disease, and neurodegenerative disease.6,10–12 In children, dystonia is more commonly secondary and thus usually represents a symptom caused by an underlying brain disorder. Certain dystonia syndromes such as occupational hand cramps or blepharospasm are rare in children, but torticollis and opisthotonus occur more frequently.10,11
Pathophysiology
Dystonia has been associated with injury to the basal ganglia.13–15 According to one model, dystonia arises from a net decrease in firing of inhibitory neurons projecting from the internal segment of globus pallidus to the ventral thalamus, causing an increase in the activity of excitatory thalamocortical projections to motor and premotor regions of the frontal cortex.16 In some cases, however, no basal ganglia injury can be identified and recent evidence from both humans and animal models suggests that other brain areas including cerebellum,17–20 brainstem,21 or sensory cortex22–23 can be causes of dystonia.
The presence of abnormal postures that are superimposed upon or substitute for voluntary movements is a characteristic feature of dystonia. Dystonic postures are repeated and include particular patterns or postures and are characteristic of each child at a given point in time. There are certain common postures that may occur in many different children. Postures can be sustained or brief. Dystonic postures are often triggered by attempts at voluntary movement or voluntary posture. The severity and quality of dystonic postures may vary with body position, specific tasks, emotional state, or level of consciousness.5,6
Dystonia can be a cause of hypertonia, although there are other causes of hypertonia1. Hypertonia is defined as abnormally increased resistance to externally imposed movement about a joint5. Hypertonia associated with dystonia was previously thought to be the result of tonically co-contracting muscles that contribute to passive joint stiffness,5 but more recent studies suggest that reflexes may play a more important role in hypertonic dystonia24 (see further discussion below). Hypertonic dystonia differs from hypertonia caused by spasticity, which is a velocity-dependent resistance of a muscle to stretch, often associated with a threshold speed or joint angle for activation.5
It is difficult to determine the relative contribution of dystonia and chorea to hyperkinetic movements, and it is possible that hyperkinetic movements primarily occur due to superimposed chorea. Chorea is defined as “an ongoing random-appearing sequence of one or more discrete involuntary movements or movement fragments” (pag. 1542).6 Yet it is also possible that dystonia is a cause of hyperkinetic movements by inserting dystonic postures that result in movements of a part of the body away from the intended movements. If multiple brief dystonic postures are inserted in voluntary movements, this could result in variable, jerky, and tremulous movements. If sustained dystonic postures are inserted in voluntary movements, this could result in the impediment of movement, substitution of an unwanted posture for an intended posture, or slow movement in an attempt to overcome the inserted dystonic posture. It has been shown that hyperkinetic and unwanted movements in upper extremities in children with dyskinetic CP are characterized by increased signal-dependent noise (SDN) of the motor system.25–27 The SDN theory states that noise in motor commands (e.g. spatial variability) tends to increase with the motor command’s magnitude (e.g. force, velocity) .28–30 This means that children with dystonia require significantly slower movements to contain the increased motor variability if they want to achieve comparable precision to typically developing children.25,27 The relationship between basal ganglia injury and increased signal dependent noise is not known. Nevertheless, based on the theory that the basal ganglia are responsible for the selective reinforcement of desired muscle patterns and inhibition of undesired muscle patterns,31,32 basal ganglia disease might lead to decreased inhibition or perhaps even excitation of unwanted patterns, resulting in increased motor variability.5,26,33
Although co-contraction is normally identified as a feature of dystonia,34,35 co-contraction is not necessary for the maintenance of stable postures, either for voluntary postures or for dystonic postures. Co-contraction may not be as frequently present in children with dystonia as originally thought,36 and in some cases co-contraction could represent voluntary compensation. For example, if the elbow flexion muscles are activated as part of a dystonic posture, the child may activate the extensor muscles voluntarily in an attempt to overcome the involuntary flexion. It would be difficult to distinguish this situation from involuntary dystonic co-activation of the flexors and extensors.6
Although co-contraction may contribute to hypertonia in some patients with dystonia, the role of reflex activation has been investigated as another possible contributor.24 van Doornik and colleagues24 reported an involuntary or reflex muscle activation in response to stretch, suggesting that this involuntary activation might be a significant contributor to increased tone in hypertonic dystonia. They proposed that this activation might be more important than co-contraction for determining the resistance to passive movement. The important role of reflex stabilization seems more likely in view of the observation that dystonic postures often maintain joints at a mid-range of joint angle, which, in the absence of reflexes, would require improbably precise matching of flexor and extensor torque.
Another disabling feature characteristic of dystonia is overflow: the close temporal association of unwanted muscle contractions with an intended movement. In many circumstances it is the apparent spread of motor activation to surrounding or distant muscles different from those typically appropriate for the goal-directed action. Overflow may also trigger a dystonic posture during voluntary movement. The mechanism of overflow in dystonia is not well understood but theoretical and neurophysiological studies suggest overflow could be due to poor awareness of muscle activation, such that during actions related but unwanted muscles or motor programs are not suppressed adequately.5,31,37,38
New insights suggest that dystonia could originate from a lack of reliable sensory feedback regarding motor actions.39 In particular, dystonia could stem from distorted and excessive afferent inputs linked via reflexes to create abnormal motor ouputs.40,41
Evaluation
Clinical Measures
Discriminating dystonia in children is complex and requires careful observation and knowledge of the disorders commonly concurrent with dystonia, such as spasticity, weakness and bradykinesia.5 Therefore, sensitive clinical measures become essential to distinguish dystonia from other pediatric movement disorders and to plan for optimal care. A thorough neurological examination in combination with valid and reliable scales assist the clinician in objectively quantifying dystonia. In this paper we briefly review some of the common clinical scales used to diagnose and quantify the severity of dystonia (for an extensive review see 42).
The Hypertonia Assessment Tool (HAT) for children was developed to differentiate the clinical features of childhood hypertonia: dystonia, spasticity and rigidity.5,43 The HAT consists of 7 items to assess the presence or absence of hypertonic components. The HAT has been shown to be useful both clinically and for research purposes to assist in identifying the presence or absence of dystonia, spasticity and rigidity.43
The Burke-Fahn-Marsden Movement Scale (BFM) was developed to assess primary dystonia.44 This scale is designed with two components: a movement scale and a disability scale. The movement scale assesses 9 different body regions. Two factors are examined in each region: a severity factor and a provoking factor (circumstance in which the dystonia appears). The disability scale is based on the individual’s assessment of how the dystonia affects activities of daily living.
The Barry-Albright Dystonia Scale (BAD) was developed to address limitations using the BFM in children and adults who are unable to cooperate with the examination, particularly children with secondary dystonia.45 The BFM is mainly based on function and was designed to evaluate primary dystonia. Individuals with secondary dystonia may have cognitive deficits, may be unable to follow instructions, and often have difficulty with daily motor activities. The BAD scale is a 5-point ordinal scale for each of 8 body regions: eyes, mouth, neck, trunk, left and right upper extremity and left and right lower extremity and since it is based on observation it does not require cooperation from the subject.
The Unified Dystonia Rating Scale (UDRS) was developed by the Dystonia Study Group to permit detailed evaluation, as well as to address concerns about limitations of the BFM scale.46 UDRS evaluates severity and duration of excess movements in dystonia in 14 different body regions. UDRS includes more body regions and is more specific in defining the region than the BFM scale. The UDRS quantifies involuntary excess movement and does not reflect hypertonia or fixed postures. The Global Dystonia Rating Scale (GDS) is a more detailed version of UDRS with a larger ordinal scale range (from 0 to 10 instead of from 0 to 4 points) for the 14 body regions.46
Kinematic Measures
Kinematic (spatial-temporal) measures are used for upper extremities to quantify the features and severity of dystonia. One study compared children with dyskinetic CP (all had dystonia) to children in a control group in terms of arm trajectory (hand path) during a finger-to-nose reaching task.26 Children with dystonia were found to have increased variability and lacked a straight-line trajectory (hand path) compared to children in the control group. In another study, children with dystonia demonstrated decreased speed and greater variability during an upper extremity reaching task.36 An examination of temporal-spatial parameters during a reach-and-grasp cycle in children with hemiplegic CP compared to children in a control group supported that children with dyskinetic CP have slower arm movements.47 Results from these studies are consistent with the hypotheses that children with dystonia have an inability to remove unwanted components of movement resulting in reduced velocity to compensate for greater spatial variability and muscle overflow (see signal-dependent noise described previously). 5,25–27,31,37,38
Another study demonstrated that spasticity and dystonia in children with CP could be differentiated using kinematic measures.48 Children with dystonia made lower velocity, curved hand paths during reaching, whereas children with spasticity tended to demonstrate higher peak velocities during reaches with less curved paths. Children with dystonia displayed greater overflow in the non-moving arm during active movement of the contralateral arm/hand. Measurements taken in this study43 were highly correlated with the clinical measures on the BAD and Modified Ashworth scale (a clinical scale to quantify the severity of spasticity).49
Target size during reaching also influences the speed of movement for children with dystonia. In studies of reach to targets of various sizes and distances, children with dystonia scaled movement speed with the target size but moved slower than children in the control group for targets of identical size.25–27,50 These results support that children with dystonia require larger targets to achieve speed comparable to controls, suggesting that they compensate for the underlying motor variability by reducing speed. Functional implications of the speed-accuracy trade-off for human movements have been demonstrated to be particularly useful for the design of touch-screen communication devices used by children with CP.51,52 Moreover, the sensory-motor ability to trade-off between speed and accuracy in a pointing task using the upper extremities provides evidence for the usefulness and validity of speed-accuracy quantification as a diagnostic tool for dystonia in children.27
The clinical scales discussed above are characterized by ease of use and prompt qualitative outcome measure of severity of dystonia. However, they are ordinal scales with a component of subjective interpretation, particularly for severity, and they lack sensitivity to fine details of movement that might not be detected or differentiated with the human eye. Hence, adding a quantitative and objective kinematic measure is a very important adjunct for the sensory-motor assessment of childhood dystonia (Table 1).
Table 1.
Clinical and kinematic masures to evalute the severity in childhood dystonia
| Clinical measures | |||
|---|---|---|---|
| Scale | Study | Features | Outcomes |
| The Hypertonia Assessment Tool (HAT) | Jethwa et al., 201043 | Developed to differentiate the clinical features of childhood hypertonia: dystonia, spasticity and rigidity | The score is 7 items tool to assess the presence or absence of hypertonic components whereby an evaluator moves a child’s arm or leg in a series of purposeful stretches and movements |
|
| |||
| The Burke-Fahn-Marsden Movement Scale (BFM) | Burke et al., 198544 | Developed to assess primary dystonia | Divided in 2 components. 1) movement scale: to assess 9 different body regions. 2) disability scale: based on the individual’s assessment of how the dystonia affects activities of daily living |
|
| |||
| Barry-Albright Dystonia Scale (BAD) | Barry et al., 199945 | Developed to particularly evaluate children with secondary dystonia | The scale is a 5-point ordinal scale for each of 8 body regions: eyes, mouth, neck, trunk, left and right upper extremity and left and right lower extremity |
|
| |||
| Unified Dystonia Rating Scale (UDRS) | Comella et al., 200346 | The scale includes more body regions and is more specific in defining the region than BFM scale | The scale evaluates severity and duration of excess movements in dystonia in 14 different body regions. |
|
| |||
| Global Dystonia Rating Scale (GDS) | Comella et al., 200346 | A more detailed version of UDRS | Larger points ordinal scale on the 14 body regions than UDRS (from 0 to 10 instead of from 0 to 4 points) |
| Kinematic measures | ||
|---|---|---|
| Study | Features | Outcomes |
| Sanger, 200626 | Kinematic analysis of the trajectory in a finger-to-nose reaching task | Children with dystonia were found to have increased spatial variability and a lack of straight-line trajectory (hand path) compared to typically developing children |
|
| ||
| Malfait & Sanger, 200636 | Kinematic analysis of the trajectory in a finger-to-nose reaching task | Children diagnosed with arm dystonia due to cerebral palsy or primary dystonia showed decreased speed and greater spatial variability |
|
| ||
| Butler et al., 201047 | Kinematic analysis of the trajectory during a reach-and-grasp cycle | Children with dystonia due to cerebral palsy had slower arm movements |
|
| ||
| Gordon et al., 200648 | Kinematic analysis of reaching and tapping tasks to differentiate dystonia and spasticity in children with cerebral palsy | Children with dystonia made curved hand paths during reaching, whereas children with spasticity tended to demonstrate higher peak velocities. Children with dystonia also were found to display greater overflow during tapping of the contralateral arm/hand. |
|
| ||
| Sanger et al,. 200525 | Measured the speed of arm movement while children attempted to contact targets of different sizes | Children with dystonia moved significantly more slowly at all button sizes, and their movement speed was more sensitive to changes in target size |
|
| ||
| Bertucco & Sanger, 201327 | Measured the speed-accuracy trade-off during pointing movement using the iPad® with different distances and targets size (Fitts' law50) | Both children with dystonia and typically developing children scaled the movement speed with distance and target size. Children with dystonia had slower movement and were more sensitive to changes in target size and distance |
Intervention
Dystonia almost always results in limitations in function. Children are expected to improve function if dystonia can be reduced. In most cases, dystonia cannot be completely eliminated, and therefore treatment goals are aimed at ameliorating selected symptoms and improving function. Physical and occupational therapy might reduce the progression of dystonia with focused rehabilitative interventions, although commonly practiced therapy methods are often ineffective.7 Treatment of childhood dystonia differs from that of adult dystonia because: (1) childhood dystonia is more often secondary rather than primary; (2) mixed motor disorders are frequent, (3) in children, the course of dystonia may be influenced by ongoing brain maturation and plasticity; (4) dystonia interferes with the typical motor development and consolidation of daily-life motor skills; (5) drug tolerability and effectiveness can be different in children; and (6) cognitive and social skills must be taken into account.
Constraint-Induced Movement Therapy and Bimanual Training
Most clinicians consider physical and occupational therapy a potential adjunct to medical therapy for dystonia. They are designed to improve posture and to prevent contractures by recognizing compensatory movements and habits that may have developed as a result of dystonia. Physical therapy may be a useful tool in the treatment of cervical dystonia.8,53,54 Although well-fitted braces may provide benefits in focal dystonia, they are poorly tolerated in children with dystonia.8 Constraint-induced movement therapy (CIMT) and bimanual training (BIM) have shown to be efficacious interventions in neurorehabilitation of stroke55–57 and spastic hemiplegic cerebral palsy without dystonia. However their effectiveness in children with dystonia is less clear.57–59 CIMT is a rehabilitation strategy that combines restraint of the unaffected limb and intensive shaping activities with the affected limb.55 CIMT has been successfully used for treatment of focal hand dystonia,60,61 It has been reported that casting, for example, can decrease hand dystonia in patients with early onset, mild dystonia (Pesenti et al., 2004; Priori et al.,2001).62,63 However, the constraint must be used with caution since dystonia can worsen in a casted limb, and high forces against the cast or brace may lead to skin breakdown. BIM is focused on equal use of both hands in bimanual shaping tasks and was developed to address bimanual co-ordination while maintaining the positive aspects of intensive training of the impaired limb.57
Despite an improvement in the child’s perceptions about their function as well as participation and physical health, CIMT and BIM did not show significant improvements in sensorimotor function or quality of upper limb movement in children with dystonia due to CP.64,65 It is worthwhile to note that the children in these studies presented a mixture of symptoms including spasticity and dystonia. Therefore, it remains unclear to what extent these interventions specifically contribute to amelioration of dystonic symptoms.
Common Intervention Strategies
It is unclear whether stretching and strengthening improves dystonic symptoms in children.7 In certain types of adult focal dystonia, it is possible that sensory retraining can be helpful.66,67 The role that this strategy may play in childhood dystonia requires research. The use of an adaptive environment, including special purpose equipment or tools that may enhance a child’s motor abilities may improve independence in activities of daily living. These alternative interventions require more study.
Biofeedback and Childhood Dystonia
It is generally accepted that augmented feedback enhances motor learning and it is effectively used in rehabilitation.68 Augmented feedback is defined as information that cannot be elaborated without an external source.69,71 It is provided by technical displays, such as visual, hearing, haptic and tactile modalities. By bringing an individual’s attention to covert physiological activity, the individual can learn to develop conscious awareness, and eventually control, over that activity.68,71 This approach has been shown to help individuals with a variety of neuromuscular disorders to increase or decrease the level of muscle activity.72 For example, several studies have reported positive effects of biofeedback of muscle activity in reducing muscle activation in individuals with dyskinetic CP,73–75 focal hand dystonia,76 and generalized dystonia.77 Two recent studies investigated the effectiveness of visual biofeedback of hand muscle activity in children with dystonia.37,78 Children with dystonia significantly reduced their co-contraction, as well as their overflow of the non-task muscle activity when visual feedback was provided. These results indicate that children with dystonia are at least partially able to control co-contraction and reduce overflow.
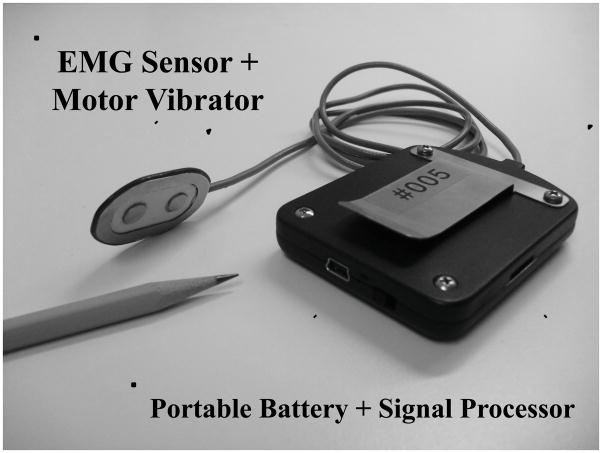
Experimental work suggests a role of sensory deficits in the genesis of dystonia.79–81 A recent computational model has provided an explanation for the link between sensory deficits and the development of motor disorders.82 For this reason, we have designed and built battery-powered wearable electromyographic (EMG) feedback devices. The person wearing the device is alerted to muscle activity by smooth changes in the speed of a silent vibration motor (Figure 1). Proportional tactile sensory feedback is achieved by driving the motor with a signal proportional to the estimated EMG power, and the vibration is provided at the site of the active muscle. A recently published study with 10 children with dystonia reported significant improvement in arm function after using the EMG biofeedback 5 hours per day for 1 month.83 A further open-label pilot study, testing a new version of the biofeedback device in 9 children and adults ages 2–20 has shown benefits during 1 month of device use compared with 1 month without the device (manuscript in preparation). We predict that the mechanism of motor improvement using EMG biofeedback could be related to increased attention and enhanced sensation of muscle contraction mimicking proprioception. Another possible mechanism for improvement is the induction of Hebbian plasticity84 associated with increased correlation between a motor action and its sensory result. By increasing the sensation associated with muscle contraction, biofeedback can further enhance cortical or subcortical representations of movement.83–85 Further investigations are needed to clarify whether the increased attention and enhanced sensation leads to reduced activity of abnormal muscle activation or enhances activity of antagonist or synergistic muscles.
Figure 1.
EMG-based biofeedback device with vibration motor embedded. The device alerts the person of his/her muscle activity with smooth changes in the speed of a silent vibration motor. Proportional tactile feedback is achieved by driving the motor with a signal proportional to the estimated EMG power, and the vibration is provided at the site of the active muscle.
Multijoint reaching movements have been studied by applying robot-generated forces.86 This non-invasive tool allows accurate observation and quantification of the motor response to an external dynamic interaction, including possible short-term adaptation strategies. Robot-generated forces during multijoint reaching movements have been applied to investigate motor control as well as to tune neuromotor adaptation. For example, Masia and colleagues evaluated adaptation of children with CP to a robot-generated force field in order to evaluate whether their motor learning capability was impaired.87 In this framework, a recent study evaluated whether the application of force to limbs could improve motor learning in children affected by primary dystonia.88 Typically developing children and children with dystonia were asked to perform upper limb movements, triangle-reaching (three directions) and circle-writing, using a haptic robot interacting with ad-hoc developed task-specific visual interfaces. A constant disturbing force (intensity = 1.3 N) was applied to the pencil during the task performances by the haptic robot. It was found that in the dystonic population the altered dynamic environment induces improvement in the form of a beneficial after-effect. The authors speculated that the short-time error-enhancing training in dystonia represented an effective approach for motor performance improvement, since the exposure to controlled dynamic alterations induced a refinement of the existing but strongly imprecise motor scheme and sensorimotor patterns.88
These results strongly suggest that methods of augmented biofeedback focusing on inappropriate muscle activation and force adaptation might provide a clinical benefit for treatment of children with dystonia. However, further research is warranted to determine the effectiveness of multiple simultaneous feedback modalities, such as tactile, visual, haptic and auditory, and to determine which particular motor deficits and types of dystonia are most influenced by these interventions.
Non-invasive neurostimulation techniques to treat childhood dystonia
Transcranial direct current stimulation (tDCS) and transcranial magnetic stimulation (TMS) are non-invasive techniques that have been studied for over 15 years to understand their clinical benefits in adults and children with movement disorders. tDCS uses constant direct current delivered through two surface electrodes on the scalp. When these electrodes are placed in the region of interest, the electrodes induce intracerebral current flow altering neuronal excitability and leading to alteration of brain function.89 Over the past decade, the effects of tDCS have been investigated in basic neurophysiology and motor learning, as well as in clinical applications, such as stroke,90 Parkinson’s disease,91 writer’s cramp,92 and musician’s dystonia.93–95 Cathodal tDCS (negative stimulation) of the motor cortex has been shown to decrease cortical excitability96 with the effect lasting for minutes to hours post-stimulation, depending on stimulation parameters.97 Research supports that cortical inhibition is impaired in dystonia98–100 and that methods to restore inhibition can help alleviate dystonic symptoms. Hence, studies have tested the hypothesis that cathodal tDCS over the primary motor cortex could reduce the symptoms of dystonia in children, improving voluntary muscle control and reducing overflow activity in nearby muscles during a tracking task using EMG of hand muscles.101–103 The results showed that cathodal tDCS of the motor cortex improved active control of muscle activity or reduced involuntary overflow only in a subset of children with primary or secondary dystonia either with a single-day session101,102 or multiday sessions.103 Heterogeneous effects of stimulation might be due to the variety of etiologies and levels of impairment of the patients recruited in the studies. The lack of improvement in the majority of participants supports the results of several recent studies of cathodal tDCS in musician’s dystonia and writer’s cramp.93–95
Anodal tDCS (positive stimulation) increases the neuronal excitability of the area being stimulated, and enhances motor skill acquisition.104–105 However, recent findings of a multiday experimental design in children with dystonia suggest that anodal stimulation is not helpful and in fact may make symptoms worse.103 Despite the absence of meaningful clinical benefits of tDCS in childhood dystonia, further research will need to explore the effects with higher stimulation currents, multiday stimulation lasting weeks or months, alternative types of stimulation (e.g. transcranial alternating current stimulation), and its effect on specific dystonic etiologies or motor impairments.
Transcranical magnetic stimulation (TMS) is a noninvasive method to depolarize or hyperpolarize neurons. It uses a strong brief electromagnetic pulse to induce weak electric currents.106 A variant of TMS, repetitive transcranial magnetic stimulation (rTMS), can modify the excitability of the cortical area in which the stimulation is applied, and it can be used as a therapeutic tool.106 Several studies confirmed that low-frequency rTMS can improve motor symptoms107,108 or reduce pain109 associated with dystonia. To date, there are no experimental data using rTMS to reduce symptoms in childhood dystonia. We have recently conducted a pilot study in our lab (unpublished data) using continuous theta-burst stimulation (cTBS), a high-frequency variant of rTMS, to induce suppression of excitatory circuits in the motor cortex in children with dystonia.110 Testing was limited by technical difficulties applying this technology to children, including difficulty identifying the motor threshold, very high motor thresholds, unusual location of motor areas, and some children complaining of scalp discomfort. Thus, further studies will need to test the feasibility and clinical benefits of TMS with more homogeneous groups of participants and may need to recruit older patients who might better tolerate the discomfort of TMS pulses.
Deep Brain Stimulation
Deep Brain Stimulation (DBS) is a very important emerging invasive therapy for treatment of dystonia in children.9 It consists of surgical implantation of electrodes that send high-frequency electrical impulses to specific parts of the brain. DBS of the globus pallidus internus (GPi) is an effective site for treatment for childhood primary and secondary dystonia.111–113 Despite an incomplete understanding of the DBS mechanism of action, it is plausible that GPi DBS modulates the basal ganglia and thalamocortical network resulting in improved processing of sensorimotor information and reduction of disease symptoms.114 DBS has been most effective in patients with primary generalized dystonia, and patients with a DYT1 mutation are reported to have the best response.115,116 Patients with secondary dystonia have also experienced improvement with DBS.117,118
The complexity, expense, and the risks of this procedure have meant that most children have waited until all other options for treatment have been exhausted. Although this is currently considered a method of last resort, for some children the dramatic improvements have raised the possibility that this procedure could have wider applicability in the future. Clinical trials are needed in order to determine the optimal DBS parameters (e.g. voltage, frequency, pulse width, and location of stimulation). DBS may strengthen the benefits of physical and occupational therapy, neurorehabilitation and other techniques.
Botulinum toxin and pharmacologic treatments
The use of botulinum toxin has resulted in a significant improvement in the treatment of hypertonia in children with dystonia. The ability to relax specific muscles without systemic side effects is tremendously important. Although botulinum toxin has been used in generalized and focal dystonias, its therapeutic application has been most studied in cervical dystonia.8 Treatment can improve function in children in whom a few muscles are the major cause of the disability. However, although botulinum toxin reduces hypertonia, it does not improve strength and does not directly improve function. It must be used carefully and in combination with an active program of other rehabilitation techniques. The therapeutic benefit of botulinum toxin is mainly due to its primary mechanism of action of blocking the release of acetylcholine into the neuromuscular junction causing local temporary chemodenervation and muscle paralysis.8 By blocking the neuromuscular junction, botulinum toxin only has the ability to decrease tone that is related to ongoing neural activation of muscle. Whether botulinum toxin's benefit is primarily due to weakness from inhibition of force-generating extrafusal fibers or reduced reflexes due to inhibition of stretch-sensitive intrafusal fibers is not known. We favor the latter explanation because botulinum toxin is often effective for reducing dystonia even in the absence of overt weakness. Botulinum toxin in some cases can delay or prevent the need for invasive surgical treatments including DBS and orthopedic procedures. Although the duration of action of botulinum toxin is between 3 and 6 months, it is possible that more prolonged benefit can be obtained if an ongoing stretching and strengthening exercise program is used.7 Stretching exercise is usually indicated to increase flexibility and to preserve joint integrity in case of muscle shortening due to a protracted dystonic syndrome. Strengthening is recommended to build up underused muscles and improve the range of motion of joints particularly for daily motor tasks such as reaching and pointing movements.
Dystonia is resistant to pharmacologic treatment in many cases. Trihexyphenidyl has been the mainstay of treatment in adults and children.119 The use of trihexyphenidyl in children is more recent, with a retrospective study120 documenting its probable effectiveness.121 Trihexyphenidyl is a centrally acting anticholinergic medicine that reduces dystonia in some children. The prevalence of cholinergic synapses in the basal ganglia makes this a possible site of action, but the mechanism of its effect on dystonia is unknown. Tetrabenazine has been helpful in the treatment of tardive dystonia, but its effectiveness in childhood primary or secondary dystonia has been disappointing.122–127 Benzodiazepines are useful for the treatment of dystonia and spasticity. However, their side effects often limit their utility. Benzodiazepines are primarily active at the GABA receptor. \The presence of GABA receptors in the basal ganglia and spinal cord \ could explain the effect on dystonia.7 The discovery of dopa-responsive dystonia (Segawa’s disease128) has led to many children receiving trials of dopaminergic medication prior to the initiation of other therapy. One consequence of this has been the observation that many children with cerebral palsy or other motor disorders have responded to dopaminergic medication, perhaps because of a mild deficiency due to partial injury to the substantia nigra. Dyskinesia may respond to carbamazepine or amantadine, and oral or intrathecal baclofen is sometimes useful perhaps due to its effect on concomitant spasticity, but perhaps with a direct effect on central GABAb receptors.
Conclusion
Dystonia management in childhood is a challenge for clinicians. The sensorimotor impairments in childhood dystonia often hamper the acquisition and consolidation of the gross and fine motor skills that are crucial for cognitive and social development. Therefore, adequate and timely interventions have extreme importance for the care of children with dystonia. The advent of new technologies has provided encouraging results in reducing dystonic symptoms, particularly the use of EMG-based biofeedback. This may refocus the current therapeutic paradigms on treating motor deficits in childhood dystonia, as well as effectively assist therapists during training sessions. Further studies will need to determine whether the combination of new therapeutic approaches with traditional ones may strengthen the results of treatment. Finally, better understanding of the pathophysiology of childhood dystonia will open new avenues for the development of therapeutic protocols and devices to support and augment the work of physical and occupational therapists.
Highlights.
Description of the pathophysiology of childhood dystonia.
Clinical measures used to assess severity and motor impairments in childhood dystonia.
State-of-the-art of therapeutic options for childhood dystonia with emphasis on emergent and innovative strategies.
Acknowledgments
We would like to thank Diana Ferman for useful comments and suggestions during the preparation of the manuscript. Support for this project was provided the Don and Linda Carter Foundation, the Crowley-Carter Foundation, the National Institutes of Health (NS064046), and the University of Southern California Department of Biomedical Engineering.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Kyllerman M, Bager B, Bensch J, Bille B, Olow I, Voss H. Dyskinetic cerebral palsy. I. Clinical categories, associated neurological abnormalities and incidences. Acta Pediatr Scand. 1982;71:543–550. doi: 10.1111/j.1651-2227.1982.tb09472.x. [DOI] [PubMed] [Google Scholar]
- 2.Hagberg G, Olow I. The changing panorama of cerebral palsy in Sweden 1954–1970. II. Analysis of the various syndromes. Acta Paediatr Scand. 1975;64(2):193–200. doi: 10.1111/j.1651-2227.1975.tb03821.x. [DOI] [PubMed] [Google Scholar]
- 3.Kyllerman M. Reduced optimality in pre- and perinatal conditions in dyskinetic cerebral palsy-distribution and comparison to controls. Neuropediatrics. 1983;14(1):29–36. doi: 10.1055/s-2008-1059549. [DOI] [PubMed] [Google Scholar]
- 4.Hensleigh PA, Fainstat T, Spencer R. Perinatal events and cerebral palsy. Am J Obstet Gynecol. 1986;154(5):978–981. doi: 10.1016/0002-9378(86)90732-5. [DOI] [PubMed] [Google Scholar]
- 5.Sanger TD, Delgado MR, Gaebler-Spira D, Hallett M, Mink JW. Classification and Definition of Disorders Causing Hypertonia in Childhood. Pediatrics. 2003;111(1):e89–e97. doi: 10.1542/peds.111.1.e89. [DOI] [PubMed] [Google Scholar]
- 6.Sanger TD, Chen D, Fehlings DL, Hallett M, Lang AE, Mink JW, et al. Definition and classification of hyperkinetic movements in childhood. Mov Disord. 2010;25(11):1538–1549. doi: 10.1002/mds.23088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sanger TD. Hypertonia in children: how and when to treat. Curr Treat Options Neurol. 2005;7(6):427–439. doi: 10.1007/s11940-005-0043-x. [DOI] [PubMed] [Google Scholar]
- 8.Jankovic J. Treatment of dystonia. Lancet Neurol. 2006;5(10):864–872. doi: 10.1016/S1474-4422(06)70574-9. [DOI] [PubMed] [Google Scholar]
- 9.Krauss JK, Yianni J, Loher TJ, Aziz TZ. Deep brain stimulation for dystonia. J Clin Neurophysiol. 2004;21(1):18–30. doi: 10.1097/00004691-200401000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Sanger TD. Toward a definition of childhood dystonia. Curr Opin Pediatr. 2004;16:623–627. doi: 10.1097/01.mop.0000142487.90041.a2. [DOI] [PubMed] [Google Scholar]
- 11.Albanese A. The clinical expression of primary dystonia. J Neurol. 2003;250:1145–1151. doi: 10.1007/s00415-003-0236-8. [DOI] [PubMed] [Google Scholar]
- 12.Fahn S, Bressman SB, Marsden CD. Classification of dystonia. Adv Neurol. 1998;78:1–10. [PubMed] [Google Scholar]
- 13.Marsden CD, Obeso JA, Zarranz JJ, Lang AE. The anatomical basis of symptomatic hemidystonia. Brain. 1985;108:463–483. doi: 10.1093/brain/108.2.463. [DOI] [PubMed] [Google Scholar]
- 14.Bhatia KP, Marsden CD. The behavioral and motor consequences of focal lesions of the basal ganglia in man. Brain. 1994;117:859–876. doi: 10.1093/brain/117.4.859. [DOI] [PubMed] [Google Scholar]
- 15.Berardelli A, Rothwell JC, Hallett M, Thompson PD, Manfredi M, Marsden CD. The pathophysiology of primary dystonia. Brain. 1998;121:1195–1212. doi: 10.1093/brain/121.7.1195. [DOI] [PubMed] [Google Scholar]
- 16.Vitek JL. Pathophysiology of dystonia: a neuronal model. Mov Disord. 2002;17 (Suppl 3):S49–62. doi: 10.1002/mds.10142. [DOI] [PubMed] [Google Scholar]
- 17.Le Ber I, Clot F, Vercueil L, et al. Predominant dystonia with marked cerebellar atrophy: a rare phenotype in familial dystonia. Neurology. 2006;67:1769–1773. doi: 10.1212/01.wnl.0000244484.60489.50. [DOI] [PubMed] [Google Scholar]
- 18.Jinnah HA, Hess EJ. A new twist on the anatomy of dystonia: the basal ganglia and the cerebellum? Neurology. 2006;67:1740–1741. doi: 10.1212/01.wnl.0000246112.19504.61. [DOI] [PubMed] [Google Scholar]
- 19.Pizoli CE, Jinnah HA, Billingsley ML, Hess EJ. Abnormal cerebellar signaling induces dystonia in mice. J Neurosci. 2002;22:7825–7833. doi: 10.1523/JNEUROSCI.22-17-07825.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.LeDoux MS, Lorden JF. Abnormal spontaneous and harmaline-stimulated Purkinje cell activity in the awake genetically dystonic rat. Exp Brain Res. 2002;145:457–467. doi: 10.1007/s00221-002-1127-4. [DOI] [PubMed] [Google Scholar]
- 21.Loher TJ, Krauss JK. Dystonia Associated with pontomesencephalic lesions. Mov Disord. 2008;24:157–167. doi: 10.1002/mds.22196. [DOI] [PubMed] [Google Scholar]
- 22.Blake DT, Byl NN, Cheung S, Bedenbaugh P, Nagarajan S, Lamb M, Merzenich M. Sensory representation abnormalities that parallel focal hand dystonia in a primate model. Somatosens Mot Res. 2002;19:347–357. doi: 10.1080/0899022021000037827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sanger TD, Merzenich MM. Computational model of the role of sensory disorganization in focal task-specific dystonia. J Neurophysiol. 2000;84:2458–2464. doi: 10.1152/jn.2000.84.5.2458. [DOI] [PubMed] [Google Scholar]
- 24.van Doornik J, Kukke S, Sanger TD. Hypertonia in childhood secondary dystonia due to cerebral palsy is associated with reflex muscle activation. Mov Disord. 2009;24(7):965–971. doi: 10.1002/mds.22282. [DOI] [PubMed] [Google Scholar]
- 25.Sanger TD, Kaiser J, Placek B. Reaching Movements in Childhood Dystonia Contain Signal-Dependent Noise. J Child Neurol. 2005;20(6):489–496. doi: 10.1177/088307380502000604. [DOI] [PubMed] [Google Scholar]
- 26.Sanger TD. Arm Trajectories in Dyskinetic Cerebral Palsy Have Increased Random Variability. J Child Neurol. 2006;21(7):551–557. doi: 10.1177/08830738060210070201. [DOI] [PubMed] [Google Scholar]
- 27.Bertucco M, Sanger TD. Speed-Accuracy Testing on the Apple iPad® Provides a Quantitative Test of Upper Extremity Motor Performance in Children with Dystonia. J Child Neurol. 2013 Aug 21; doi: 10.1177/0883073813494265. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Harris CM, Wolpert DM. Signal-dependent noise determines motor planning. Nature. 1998;394(6695):780–784. doi: 10.1038/29528. [DOI] [PubMed] [Google Scholar]
- 29.Slifkin AB, Newell KM. Noise, information transmission, and force variability. J Exp Psychol Hum Percept Perform. 1999;25(3):837–51. doi: 10.1037//0096-1523.25.3.837. [DOI] [PubMed] [Google Scholar]
- 30.Jones KE, Hamilton AF, Wolpert DM. Sources of signal-dependent noise during isometric force production. J Neurophysiol. 2002;88(3):1533–1544. doi: 10.1152/jn.2002.88.3.1533. [DOI] [PubMed] [Google Scholar]
- 31.Mink JW. The basal ganglia: focused selection and inhibition of competing motor programs. Prog Neurobiol. 1996;50:381–425. doi: 10.1016/s0301-0082(96)00042-1. [DOI] [PubMed] [Google Scholar]
- 32.Mink JW. Basal ganglia motor function in relation to Hallervorden-Spatz syndrome. Pediatr Neurol. 2001;25(2):112–117. doi: 10.1016/s0887-8994(01)00270-3. [DOI] [PubMed] [Google Scholar]
- 33.Mink JW. The Basal Ganglia and involuntary movements: impaired inhibition of competing motor patterns. Arch Neurol. 2003;60(10):1365–1368. doi: 10.1001/archneur.60.10.1365. [DOI] [PubMed] [Google Scholar]
- 34.Sitburana O, Jankovic J. Focal hand dystonia, mirror dystonia and motor overflow. J Neurol Sci. 2008;266:31–33. doi: 10.1016/j.jns.2007.08.024. [DOI] [PubMed] [Google Scholar]
- 35.Liu X, Tailor J, Wang S, Yianni J, Gregory R, Stein J, Aziz T. Reversal of hypertonic co-contraction after bilateral pallidal stimulation in generalized dystonia: a clinical and electromyogram case study. Mov Disord. 2004;19:336–340. doi: 10.1002/mds.10655. [DOI] [PubMed] [Google Scholar]
- 36.Malfait N, Sanger TD. Does dystonia always include co-contraction? A study of unconstrained reaching in children with primary and secondary dystonia. Exp Brain Res. 2007;176:206–216. doi: 10.1007/s00221-006-0606-4. [DOI] [PubMed] [Google Scholar]
- 37.Young SJ, van Doornik J, Sanger TD. Finger muscle control in children with dystonia. Mov Disord. 2011;26(7):1290–1296. doi: 10.1002/mds.23534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lunardini F, Maggioni S, Casellato C, Bertucco M, Pedrocchi A, Terence DS. Increased task-irrelevant components of muscle activity in childhood dystonia. doi: 10.1186/s12984-015-0045-1. Under Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ostry DJ, Darainy M, Mattar AA, Wong J, Gribble PL. Somatosensory plasticity and motor learning. J Neurosci. 2010;30:5384–5393. doi: 10.1523/JNEUROSCI.4571-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tinazzi M, Priori A, Bertolasi L, Frasson E, Mauguière F, Fiaschi A. Abnormal central integration of a dual somatosensory input in dystonia. Evidence for sensory overflow. Brain. 2000;123:42–50. doi: 10.1093/brain/123.1.42. [DOI] [PubMed] [Google Scholar]
- 41.Sanger TD, Tarsy D, Pascual-Leone A. Abnormalities of spatial and temporal sensory discrimination in writer's cramp. Mov Disord. 2001;16:94–99. doi: 10.1002/1531-8257(200101)16:1<94::aid-mds1020>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 42.Pavone L, Burton J, Gaebler-Spira D. Dystonia in childhood: clinical and objective measures and functional implications. J Child Neurol. 2013;28(3):340–350. doi: 10.1177/0883073812444312. [DOI] [PubMed] [Google Scholar]
- 43.Jethwa A, Mink J, Macarthur C, Knights S, Fehlings T, Fehlings D. Development of the Hypertonia Assessment Tool (HAT): a discriminative tool for hypertonia in children. Dev Med Child Neurol. 2010;52(5):e83–7. doi: 10.1111/j.1469-8749.2009.03483.x. [DOI] [PubMed] [Google Scholar]
- 44.Burke RE, Fahn S, Marsden CD, Bressman SB, Moskowitz C, Friedman J. Validity and reliability of a rating scale for the primary torsion dystonias. Neurology. 1985;35:73–77. doi: 10.1212/wnl.35.1.73. [DOI] [PubMed] [Google Scholar]
- 45.Barry MJ, Van Swearingen JM, Albright AL. Reliability and responsiveness of the Barry-Albright Dystonia Scale. Dev Med Child Neurol. 1999;41:404–411. doi: 10.1017/s0012162299000870. [DOI] [PubMed] [Google Scholar]
- 46.Comella CL, Leurgans S, Wuu J, Stebbins GT, Chmura T Dystonia Study Group. Rating scales for dystonia: a multicenter assessment. Mov Disord. 2003;18(3):303–312. doi: 10.1002/mds.10377. [DOI] [PubMed] [Google Scholar]
- 47.Butler E, Ladd A, LaMont L, Rose J. Temporal-spatial parameters of the upper limb during a reach & grasp cycle for children. Gait Posture. 2010;32:301–306. doi: 10.1016/j.gaitpost.2010.05.013. [DOI] [PubMed] [Google Scholar]
- 48.Gordon L, Keller J, Stashinko E, Hoon AH, Bastian AJ. Can Spasticity and dystonia be independently measured in cerebral palsy? Pediatr Neurol. 2006;35:375–381. doi: 10.1016/j.pediatrneurol.2006.06.015. [DOI] [PubMed] [Google Scholar]
- 49.Bohannon RW, Smith MB. Interrater reliability of a modified Ashworth scale of muscle spasticity. Phys Ther. 1987;67(2):206–207. doi: 10.1093/ptj/67.2.206. [DOI] [PubMed] [Google Scholar]
- 50.Fitts PM. The information capacity of the human motor system in controlling the amplitude of movement. J Exp Psychol. 1954;47:381–391. [PubMed] [Google Scholar]
- 51.Plamondon R, Alimi AM. Speed/accuracy trade-offs in target-directed movements. Behav Brain Sci. 1997;20:279–349. doi: 10.1017/s0140525x97001441. [DOI] [PubMed] [Google Scholar]
- 52.Sanger TD, Henderson J. Optimizing Assisted Communication Devices for Children With Motor Impairments Using a Model of Information Rate and Channel Capacity. IEEE Trans Neural Syst Rehabil Eng. 2007;15(3):458–68. doi: 10.1109/TNSRE.2007.903969. [DOI] [PubMed] [Google Scholar]
- 53.Smania N, Corato E, Tinazzi M, Montagnana B, Fiaschi A, Aglioti SM. The effect of two different rehabilitation treatments in cervical dystonia: preliminary results in four patients. Funct Neurol. 2003;18(4):219–225. [PubMed] [Google Scholar]
- 54.Tassorelli C, Mancini F, Balloni L, Pacchetti C, Sandrini G, Nappi G, Martignoni E. Botulinum toxin and neuromotor rehabilitation: An integrated approach to idiopathic cervical dystonia. Mov Disord. 2006;21(12):2240–2243. doi: 10.1002/mds.21145. [DOI] [PubMed] [Google Scholar]
- 55.Taub E, Morris DM. Constraint-induced movement therapy to enhance recovery after stroke. Curr Atheroscler Rep. 2001;3(4):279–286. doi: 10.1007/s11883-001-0020-0. [DOI] [PubMed] [Google Scholar]
- 56.Uswatte G, Taub E. Constraint-induced movement therapy: a method for harnessing neuroplasticity to treat motor disorders. Prog Brain Res. 2013;207:379–401. doi: 10.1016/B978-0-444-63327-9.00015-1. [DOI] [PubMed] [Google Scholar]
- 57.Charles J, Gordon AM. Development of hand-arm bimanual intensive training (HABIT) for improving bimanual coordination in children with hemiplegic cerebral palsy. Dev Med Child Neurol. 2006;48:931–936. doi: 10.1017/S0012162206002039. [DOI] [PubMed] [Google Scholar]
- 58.Huang HH, Fetters L, Hale J, McBride A. Bound for success: a systematic review of constraint-induced movement therapy in children with cerebral palsy supports improved arm and hand use. Phys Ther. 2009;89:1126–1141. doi: 10.2522/ptj.20080111. [DOI] [PubMed] [Google Scholar]
- 59.Charles J, Gordon AM. A critical review of constraint-induced movement therapy and forced use in children with hemiplegia. Neural Plast. 2005;12:245–261. doi: 10.1155/NP.2005.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Candia V, Elbert T, Altenmuller E, Rau H, Schafer T, Taub E. Constraint-Induced Movement therapy for focal hand dystonia in musicians. Lancet. 1999;353:42. doi: 10.1016/S0140-6736(05)74865-0. [DOI] [PubMed] [Google Scholar]
- 61.Candia V, Schafer T, Taub E, Rau H, Altenmuller E, Rockstroh B, Elbert T. Sensory motor retuning: a behavioral treatment for focal hand dystonia of pianists and guitarists. Arch Phys Med Rehabil. 2002;83:1342–1348. doi: 10.1053/apmr.2002.35094. [DOI] [PubMed] [Google Scholar]
- 62.Pesenti A, Barbieri S, Priori A. Limb immobilization for occupational dystonia: a possible alternative treatment for selected patients. Adv Neurol. 2004;94:247–254. [PubMed] [Google Scholar]
- 63.Priori A, Pesenti A, Cappellari A, Scarlato G, Barbieri S. Limb immobilization for the treatment of focal occupational dystonia. Neurology. 2001;57:405–409. doi: 10.1212/wnl.57.3.405. [DOI] [PubMed] [Google Scholar]
- 64.Gordon AM, Schneider JA, Chinnan A, Charles JR. Efficacy of a hand-arm bimanual intensive therapy (HABIT) in children with hemiplegic cerebral palsy: a randomized control trial. Dev Med Child Neurol. 2007;49(11):830–838. doi: 10.1111/j.1469-8749.2007.00830.x. [DOI] [PubMed] [Google Scholar]
- 65.Sakzewski L, Carlon S, Shields N, Ziviani J, Ware RS, Boyd RN. Impact of intensive upper limb rehabilitation on quality of life: a randomized trial in children with unilateral cerebral palsy. Dev Med Child Neurol. 2012;54(5):415–423. doi: 10.1111/j.1469-8749.2012.04272.x. [DOI] [PubMed] [Google Scholar]
- 66.Byl NN, Nagajaran S, McKenzie AL. Effect of sensory discrimination training on structure and function in patients with focal hand dystonia: a case series. Arch Phys Med Rehabil. 2003;84(10):1505–1514. doi: 10.1016/s0003-9993(03)00276-4. [DOI] [PubMed] [Google Scholar]
- 67.Zeuner KE, Hallett M. Sensory training as treatment for focal hand dystonia: a 1-year follow-up. Mov Disord. 2003;18(9):1044–1047. doi: 10.1002/mds.10490. [DOI] [PubMed] [Google Scholar]
- 68.Sigrist R, Rauter G, Riener R, Wolf P. Augmented visual, auditory, haptic, and multimodal feedback in motor learning: A review. Psychon Bull Rev. 2013;20(1):21–53. doi: 10.3758/s13423-012-0333-8. [DOI] [PubMed] [Google Scholar]
- 69.Schmidt R, Wrisberg C. Motor learning and performance: A situation-based learning approach. Illinois: Human Kinetics Publishers Inc; 2008. [Google Scholar]
- 70.Utley A, Astill S. Bios Instant Notes. Taylor & Francis Group; 2008. Motor control, learning and development. [Google Scholar]
- 71.Basmajian JV. Research foundations of EMG biofeedback in rehabilitation. Biofeedback Self Regul. 1988;13:275–298. doi: 10.1007/BF00999085. [DOI] [PubMed] [Google Scholar]
- 72.Huang H, Wolf SL, He J. Recent developments in biofeedback for neuromotor rehabilitation. J Neuroeng Rehabil. 2006;3:11. doi: 10.1186/1743-0003-3-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Cataldo MF, Bird BL, Cunningham CE. Experimental analysis of EMG feedback in treating cerebral palsy. J Behav Med. 1978;1:311–322. doi: 10.1007/BF00846682. [DOI] [PubMed] [Google Scholar]
- 74.Finley WW, Niman C, Standley J, Ender P. Frontal EMG- biofeedback training of athetoid cerebral palsy patients: a report of six cases. Biofeedback Self Regul. 1976;1:169–182. doi: 10.1007/BF00998584. [DOI] [PubMed] [Google Scholar]
- 75.Neilson PD, McCaughey J. Self-regulation of spasm and spasticity in cerebral palsy. J Neurol Neurosurg Psychiatry. 1982;45:320–330. doi: 10.1136/jnnp.45.4.320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Deepak KK, Behari M. Specific muscle EMG biofeedback for hand dystonia. Appl Psychophysiol Biofeedback. 1999;24(4):267–280. doi: 10.1023/a:1022239014808. [DOI] [PubMed] [Google Scholar]
- 77.Bird BL, Cataldo MF. Experimental analysis of EMG feedback in treating dystonia. Ann Neurol. 1978;3:310–315. doi: 10.1002/ana.410030406. [DOI] [PubMed] [Google Scholar]
- 78.Young SJ, van Doornik J, Sanger TD. Visual feedback reduces co-contraction in children with dystonia. J Child Neurol. 2011;26(1):37–43. doi: 10.1177/0883073810371828. [DOI] [PubMed] [Google Scholar]
- 79.Harris FA. Inapproprioception: a possible sensory basis for athetoid movements. Phys Ther. 1971;51(7):761–770. doi: 10.1093/ptj/51.7.761. [DOI] [PubMed] [Google Scholar]
- 80.Hallett M. Is dystonia a sensory disorder? Ann Neurol. 1995;38(2):139–140. doi: 10.1002/ana.410380203. [DOI] [PubMed] [Google Scholar]
- 81.Molloy FM, Carr TD, Zeuner KE, Dambrosia JM, Hallett M. Abnormalities of spatial discrimination in focal and generalized dystonia. Brain. 2003;126:2175–2182. doi: 10.1093/brain/awg219. [DOI] [PubMed] [Google Scholar]
- 82.Sanger TD. Failure of motor learning for large initial errors. Neural Comput. 2004;16(9):1873–1886. doi: 10.1162/0899766041336431. [DOI] [PubMed] [Google Scholar]
- 83.Bloom R, Przekop A, Sanger TD. Prolonged electromyogram biofeedback improves upper extremity function in children with cerebral palsy. J Child Neurol. 2010;25(12):1480–1484. doi: 10.1177/0883073810369704. [DOI] [PubMed] [Google Scholar]
- 84.Hebb DO. The Organization of Behavior: A Neuropsychological Theory. New York: Wiley and Sons; 1949. [Google Scholar]
- 85.Casellato C, Maggioni S, Lunardini F, Bertucco M, Pedrocchi A, Sanger TD. Dystonia: Altered Sensorimotor Control and Vibro-tactile EMG-Based Biofeedback Effects. XIII Mediterranean Conference on Medical and Biological Engineering and Computing 2013 IFMBE Proceedings; pp. 1742–1746. [Google Scholar]
- 86.Shadmehr R, Mussa-Ivaldi FA. Adaptive representation of dynamics during learning of a motor task. J Neurosci. 1994;14:3208–3224. doi: 10.1523/JNEUROSCI.14-05-03208.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Masia L, Frascarelli F, Morasso P, Di Rosa G, Petrarca M, Castelli E, Cappa P. Reduced short term adaptation to robot generated dynamic environment in children affected by Cerebral Palsy. J Neuroeng Rehabil. 2011;8:28. doi: 10.1186/1743-0003-8-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Casellato C, Pedrocchi A, Zorzi G, Rizzi G, Ferrigno G, Nardocci N. Error-enhancing robot therapy to induce motor control improvement in childhood onset primary dystonia. J Neuroeng Rehabil. 2012;9:46. doi: 10.1186/1743-0003-9-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Nitsche MA, Cohen LG, Wassermann EM, Priori A, Lang N, Antal A, et al. Transcranial direct current stimulation: State of the art 2008. Brain Stimulation. 2008;1(3):206–223. doi: 10.1016/j.brs.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 90.Boggio PS, Nunes A, Rigonatti SP, Nitsche MA, Pascual-Leone A, Fregni F. Repeated sessions of noninvasive brain DC stimulation is associated with motor function improvement in stroke patients. Restor Neurol Neurosci. 2007;25:123–129. [PubMed] [Google Scholar]
- 91.Wu AD, Fregni F, Simon DK, Deblieck C, Pascual-Leone A. Noninvasive brain stimulation for Parkinson’s disease and dystonia. Neurotherapeutics. 2008;5:345–361. doi: 10.1016/j.nurt.2008.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Benninger DH, Lomarev M, Lopez G, Pal N, Luckenbaugh DA, Hallett M. Transcranial direct current stimulation for the treatment of focal hand dystonia. Mov Disord. 2011;26:1698–1702. doi: 10.1002/mds.23691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Buttkus F, Weidenmüller M, Schneider S, Jabusch HC, Nitsche MA, Paulus W, Altenmüller E. Failure of cathodal direct current stimulation to improve fine motor control in musician’s dystonia. Mov Disord. 2010;25:389–394. doi: 10.1002/mds.22938. [DOI] [PubMed] [Google Scholar]
- 94.Buttkus F, Baur V, Jabusch HC, Paulus W, Nitsche MA, Altenmüller E. Retraining and transcranial direct current stimulation in musician’s dystonia - a case report. Mov Disord. 2010;25:1758–1760. doi: 10.1002/mds.23259. [DOI] [PubMed] [Google Scholar]
- 95.Buttkus F, Baur V, Jabusch HC, de la Cruz Gomez-Pellin M, Paulus W, Nitsche MA, Altenmüller E. Single-session tDCS- supported retraining does not improve fine motor control in musician’s dystonia. Restor Neurol Neurosci. 2011;29:85–90. doi: 10.3233/RNN-2011-0582. [DOI] [PubMed] [Google Scholar]
- 96.Nitsche MA, Paulus W. Excitability changes induced in the human motor cortex by weak transcranial direct current stimulation. J Physiol (Lond) 2000;527:633–639. doi: 10.1111/j.1469-7793.2000.t01-1-00633.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Monte-Silva K, Kuo MF, Liebetanz D, Paulus W, Nitsche MA. Shaping the optimal repetition interval for cathodal transcranial direct current stimulation (tDCS) J Neurophysiol. 2010;103:1735–1740. doi: 10.1152/jn.00924.2009. [DOI] [PubMed] [Google Scholar]
- 98.Ridding MC, Sheean G, Rothwell JC, Inzelberg R, Kujirai T. Changes in the balance between motor cortical excitation and inhibition in focal, task specific dystonia. J Neurol Neurosurg Psychiatry. 1995;59:493–498. doi: 10.1136/jnnp.59.5.493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Beck S, Richardson SP, Shamim EA, Dang N, Schubert M, Hallett M. Short intracortical and surround inhibition are selectively reduced during movement initiation in focal hand dystonia. J Neurosci. 2008;28:10363–10369. doi: 10.1523/JNEUROSCI.3564-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Hallett M. Neurophysiology of dystonia: the role of inhibition. Neurobiol Dis. 2011;42:177–184. doi: 10.1016/j.nbd.2010.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Young SJ, Bertucco M, Sheehan-Stross R, Sanger TD. Cathodal transcranial direct current stimulation in children with dystonia: a pilot open-label trial. J Child Neurol. 2013;28(10):1238–1244. doi: 10.1177/0883073812460092. [DOI] [PubMed] [Google Scholar]
- 102.Young SJ, Bertucco M, Sanger TD. Cathodal transcranial direct current stimulation in children with dystonia: a sham-controlled study. J Child Neurol. 2014;29(2):232–239. doi: 10.1177/0883073813492385. [DOI] [PubMed] [Google Scholar]
- 103.Bhanpuri NH, Bertucco M, Young SJ, Lee A, Sanger TD. Multiday Transcranial Direct Current Stimulation can Induce Mild Changes in Childhood Dystonia. doi: 10.1177/0883073815575369. Under review. [DOI] [PubMed] [Google Scholar]
- 104.Reis J, Schambra HM, Cohen LG, Buch ER, Fritsch B, Zarahn E, Celnik PA, Krakauer JW. Noninvasive cortical stimulation enhances motor skill acquisition over multiple days through an effect on consolidation. Proc Natl Acad Sci USA. 2009;106(5):1590–1595. doi: 10.1073/pnas.0805413106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Galea JM, Vazquez A, Pasricha N, de Xivry JJ, Celnik P. Dissociating the roles of the cerebellum and motor cortex during adaptive learning: the motor cortex retains what the cerebellum learns. Cereb Cortex. 2011;21(8):1761–1770. doi: 10.1093/cercor/bhq246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Pascual-Leone A, Davey N, Rothwell J, Wassermann EM, Puri BK. Handbook of Transcranial Magnetic Stimulation. London: Edward Arnold; 2002. [Google Scholar]
- 107.Siebner HR, Tormos JM, Ceballos-Baumann AO, Auer C, Catala MD, Conrad B, Pascual-Leone A. Low-frequency repetitive transcranial magnetic stimulation of the motor cortex in writer's cramp. Neurology. 1999;52(3):529–537. doi: 10.1212/wnl.52.3.529. [DOI] [PubMed] [Google Scholar]
- 108.Murase N, Rothwell JC, Kaji R, Urushihara R, Nakamura K, Murayama N, Igasaki T, Sakata-Igasaki M, Mima T, Ikeda A, Shibasaki H. Subthreshold low-frequency repetitive transcranial magnetic stimulation over the premotor cortex modulates writer's cramp. Brain. 2005;128:104–115. doi: 10.1093/brain/awh315. [DOI] [PubMed] [Google Scholar]
- 109.Lefaucheur JP, Fénelon G, Ménard-Lefaucheur I, Wendling S, Nguyen JP. Low-frequency repetitive TMS of premotor cortex can reduce painful axial spasms in generalized secondary dystonia: a pilot study of three patients. Neurophysiol Clin. 2004;34:141–145. doi: 10.1016/j.neucli.2004.07.003. [DOI] [PubMed] [Google Scholar]
- 110.Di Lazzaro V, Pilato F, Saturno E, Oliviero A, Dileone M, Mazzone P, Insola A, Tonali PA, Ranieri F, Huang YZ, Rothwell JC. Theta-burst repetitive transcranial magnetic stimulation suppresses specific excitatory circuits in the human motor cortex. J Physiol. 2005;565:945–950. doi: 10.1113/jphysiol.2005.087288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Air EL, Ostrem JL, Sanger TD, Starr PA. Deep brain stimulation in children: experience and technical pearls. Clinical article. J Neurosurg Pediatr. 2011;8:566–574. doi: 10.3171/2011.8.PEDS11153. [DOI] [PubMed] [Google Scholar]
- 112.Bronte-Stewart H, Taira T, Valldeoriola F, Merello M, Marks WJ, Jr, Albanese A, Bressman S, Moro E. Inclusion and exclusion criteria for DBS in dystonia. Mov Disord. 2011;26 (Suppl 1):S5–S16. doi: 10.1002/mds.23482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Coubes P, Cif L, El Fertit H, Hemm S, Vayssiere N, Serrat S, Picot MC, Tuffery S, Claustres M, Echenne B, Frerebeau P. Electrical stimulation of the globus pallidus internus in patients with primary generalized dystonia: long-term results. J Neurosurg. 2004;101:189–194. doi: 10.3171/jns.2004.101.2.0189. [DOI] [PubMed] [Google Scholar]
- 114.Miocinovic S, Somayajula S, Chitnis S, Vitek JL. History, applications, and mechanisms of deep brain stimulation. JAMA Neurol. 2013;70(2):163–171. doi: 10.1001/2013.jamaneurol.45. [DOI] [PubMed] [Google Scholar]
- 115.Alterman RL, Tagliati M. Deep brain stimulation for torsion dystonia in children. Childs Nerv Syst. 2007;23:1033–1040. doi: 10.1007/s00381-007-0382-x. [DOI] [PubMed] [Google Scholar]
- 116.Panov F, Gologorsky Y, Connors G, Tagliati M, Miravite J, Alterman RL. Deep brain stimulation in DYT1 dystonia: a 10-year experience. Neurosurgery. 2013;73:86–93. doi: 10.1227/01.neu.0000429841.84083.c8. [DOI] [PubMed] [Google Scholar]
- 117.Koy A, Hellmich M, Pauls KA, Marks W, Lin JP, Fricke O, Timmermann L. Effects of deep brain stimulation in dyskinetic cerebral palsy: a meta-analysis. Mov Disord. 2013;28:647–654. doi: 10.1002/mds.25339. [DOI] [PubMed] [Google Scholar]
- 118.Olaya JE, Christian E, Ferman D, Luc Q, Krieger MD, Sanger TD, Liker MA. Deep brain stimulation in children and young adults with secondary dystonia: the Children's Hospital Los Angeles experience. Neurosurg Focus. 2013;35(5):E7. doi: 10.3171/2013.8.FOCUS13300. [DOI] [PubMed] [Google Scholar]
- 119.Marsden CD, Marion MH, Quinn N. The treatment of severe dystonia in children and adults. J Neurol Neurosurg Psychiatry. 1984;47:1166–1173. doi: 10.1136/jnnp.47.11.1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Hoon AH, Jr, Freese PO, Reinhardt EM, Wilson MA, Lawrie WT, Jr, Harryman SE, Pidcock FS, Johnston MV. Age-dependent effects of trihexyphenidyl in extrapyramidal cerebral palsy. Pediatr Neurol. 2001;25:55–58. doi: 10.1016/s0887-8994(01)00287-9. [DOI] [PubMed] [Google Scholar]
- 121.Sanger TD, Bastian A, Brunstrom J, Damiano D, Delgado M, Dure L, Gaebler-Spira D, Hoon A, Mink JW, Sherman-Levine S, Welty LJ Child Motor Study Group. Prospective open-label clinical trial of trihexyphenidyl in children with secondary dystonia due to cerebral palsy. J Child Neurol. 2007;22:530–537. doi: 10.1177/0883073807302601. [DOI] [PubMed] [Google Scholar]
- 122.Jankovic J, Beach J. Long-term effects of tetrabenazine in hyperkinetic movement disorders. Neurology. 1997;48:358–362. doi: 10.1212/wnl.48.2.358. [DOI] [PubMed] [Google Scholar]
- 123.Jankovic J, Orman J. Tetrabenazine therapy of dystonia, chorea, tics, and other dyskinesias. Neurology. 1988;38:391–394. doi: 10.1212/wnl.38.3.391. [DOI] [PubMed] [Google Scholar]
- 124.Heggarty H, Wright T. Tetrabenazine in athetoid cerebral palsy. Dev Med Child Neurol. 1974;16:137–142. doi: 10.1111/j.1469-8749.1974.tb02733.x. [DOI] [PubMed] [Google Scholar]
- 125.Jankovic J. Treatment of hyperkinetic movement disorders with tetrabenazine: a double-blind crossover study. Ann Neurol. 1982;11:41–47. doi: 10.1002/ana.410110108. [DOI] [PubMed] [Google Scholar]
- 126.Asher SW, Aminoff MJ. Tetrabenazine and movement disorders. Neurology. 1981;31:1051–1054. doi: 10.1212/wnl.31.8.1051. [DOI] [PubMed] [Google Scholar]
- 127.Swash M, Roberts AH, Zakko H, Heathfield KW. Treatment of involuntary movement disorders with tetrabenazine. J Neurol Neurosurg Psychiatry. 1972;35:186–191. doi: 10.1136/jnnp.35.2.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Segawa M, Nishiyama N, Nomura Y. DOPA-responsive dystonic parkinsonism: pathophysiologic considerations. Adv Neurol. 1999;80:389–400. [PubMed] [Google Scholar]