Abstract
Objective:
We examined attempted and completed suicides after stroke to determine whether they were associated with socioeconomic status, other patient characteristics, or time after stroke.
Methods:
This nationwide cohort study included stroke patients from Riksstroke (the Swedish Stroke Register) from 2001 to 2012. We used personal identification numbers to link the Riksstroke data with other national registers. Suicide attempts were identified by a record of hospital admission for intentional self-harm (ICD-10: X60-X84), and completed suicides were identified in the national Cause of Death Register. We used multiple Cox regression to analyze time from stroke onset to first suicide attempt.
Results:
We observed 220,336 stroke patients with a total follow-up time of 860,713 person-years. During follow-up, there were 1,217 suicide attempts, of which 260 were fatal. This was approximately double the rate of the general Swedish population. Patients with lower education or income (hazard ratio [HR] 1.37, 95% confidence interval [CI] 1.11–1.68) for primary vs university and patients living alone (HR 1.73, 95% CI 1.52–1.97) had an increased risk of attempted suicide, and patients born outside of Europe had a lower risk compared to patients of European origin. Male sex, young age, severe stroke, and poststroke depression were other factors associated with an increased risk of attempted suicide after stroke. The risk was highest during the first 2 years after stroke.
Conclusions:
Both clinical and socioeconomic factors increase the risk of poststroke suicide attempts. This suggests a need for psychosocial support and suicide preventive interventions in high-risk groups of stroke patients.
Stroke patients with previous mood disorders and who have poststroke depression are at particular risk for suicidal thoughts.1 Having had a stroke increases not only the risk of suicidal thoughts1–3 but also the risk of suicide.4–6 The suicide risk is particularly high in patients who are relatively young.4,5
In the general population, suicide rates vary with socioeconomic factors such as civil status, education, and income.7 After a stroke, existential distress might be prominent8 and add to the direct biological effects of brain injury to cause depression.9 A Portuguese study of 177 stroke patients found that suicidal thoughts were more common among patients with a low level of education,3 but there are no previous studies on how suicide attempts or completed suicides relate to socioeconomic factors in stroke patients.
We aimed to study how major socioeconomic factors (education, income, civil status, and country of birth) are associated with suicide attempts and completed suicides in patients who have had a stroke. We also explored other factors associated with suicide attempts, including the time after stroke at which suicide risk was the greatest and what methods were used in the suicide attempts.
METHODS
The Swedish stroke register (Riksstroke) was established in 1994 to monitor, support, and improve the quality of stroke care in Sweden.10 All hospitals admitting acute stroke patients in Sweden participate (72 hospitals in 2012). Swedish acute care hospitals are all publicly financed. Some rehabilitation services have private ownership but are commissioned and financed by country councils and local communities. The most common form of entirely private financing is rehabilitation stays in Mediterranean countries, estimated to constitute far less than 1% of all rehabilitation services. A review of the Swedish health care system has been published by the European Observatory on Health Systems and Policies.11 The Riksstroke register has an estimated coverage of 94% of all acute stroke patients treated in Swedish hospitals12 and takes into account that acute stroke is overdiagnosed in routine administrative registers.13 Riksstroke includes information on living conditions and comorbidities prior to stroke and on the acute treatment that was provided immediately after the stroke. A Riksstroke follow-up 3 months after stroke onset includes information on patient-reported outcome, depression, use of antidepressant medication, rehabilitation, and support. Details on what information is collected are available at the Riksstroke Web site (http://www.riksstroke.org/eng/).
This study included patients with intracerebral hemorrhage, ischemic stroke, and unspecified stroke (ICD-10 codes I61, I63, and I64) who were discharged alive from the hospital. The patients were followed from their first registration in Riksstroke from January 1, 2001, until death or the study end date on December 31, 2012.
We used level of consciousness on admission to the hospital as a proxy for stroke severity. It was registered using 3 levels based on the Reaction Level Scale (RLS).14 Alert corresponded to RLS 1, drowsy to RLS 2–3, and unconscious to RLS 4–8. Independence in activities of daily living (ADL) was defined as the patient being able to manage dressing, using the toilet, and walking unassisted.
The 3-month follow-up includes the question “Do you feel depressed?” with responses of never or almost never, sometimes, often, constantly, or do not know. Patients who answered “often” or “constantly” were considered to have self-reported depression. Another question concerned treatment of depression with responses of yes, no, or do not know. General health was assessed by the question “How would you assess your general health?” with responses of very good, quite good, quite poor, very poor, or do not know.
Riksstroke was linked with the Swedish National Inpatient Register15 and the Cause of Death Register,16 which are managed by the National Board of Health and Welfare, using personal identification numbers. A suicide attempt was identified by a record of hospital admission for or an underlying or contributing cause of death by intentional self-harm (ICD-10: X60–X84). The attempts were grouped by means, including self-poisoning (X60–X69); hanging, drowning, firearm discharge, explosive material, smoke, fire and flames, steam, and hot objects (X70–X77); sharp or blunt object (X78–X79); jumping or crashing of a vehicle (X80–X82); or other specified (caustic substances, crashing of aircraft, or electrocution) or unspecified means (X83–X84). Registrations within 28 days with the same grouped means of suicide attempt were excluded.
Information on patient education and income for the year preceding stroke and country of birth were retrieved using personal identification numbers through linkage with the Longitudinal Integration Database for Health Insurance and Labor Market Studies (LISA by its Swedish acronym),17 which is managed by Statistics Sweden. Highest achieved education was grouped into primary school, secondary school, or university education. To measure income, we used the individual's part of the family disposable income grouped into tertiles (low, middle, or high income). Country of birth was grouped into Sweden, other Nordic countries (Finland, Norway, Denmark, and Iceland), other European countries, and outside Europe.
Annual age- and sex-specific suicide incidence for the general population was retrieved from the National Board of Health and Welfare's Statistical Database of Cause of Deaths as of July 31, 2014.18
Standard protocol approvals, registrations, and patient consents.
Patients are informed that participation in Riksstroke is voluntary and patients can deny participation in Riksstroke at any time. This particular study was approved by the Ethical Review Board in Umeå (reference no. 2014/130-31).
Statistical methods.
Time from stroke onset to first attempted suicide was analyzed by Cox regression. Patients were censored at time of death, emigration, or end of study. We used both a simple Cox regression model and a model adjusting for sex and age by including them as independent factors. We performed a sensitivity analysis in patients with 3-month follow-up data from Riksstroke where we added ADL function 3 months after stroke to the model. We examined Kaplan-Meier survival curves to identify major deviations from the proportional hazard assumption. The χ2 test was used to analyze the association of patient-reported outcome at 3 months and attempted suicide within 1 year after stroke. In addition, we used multiple logistic regression to adjust for sex and age. We also analyzed the time from 3 months to attempted suicide during the total follow-up using Cox regression. Outcome from Cox regression was presented by the hazard ratio (HR) and outcome from logistic regression by the odds ratio (OR) with corresponding 95% confidence interval (CI). Education level was missing for 8,578 (3.8%) of the patients, so unknown education was included as a separate category. No other variable exceeded 1.5% missing data, and patients with other missing information were dropped from the relevant analyses. We used IBM (Armonk, NY, USA) SPSS version 22 for statistical analysis.
RESULTS
The study included 220,336 stroke survivors who were followed for up to 12 years (a total of 860,713 person-years). During follow-up, we observed 1,217 suicide attempts in 985 patients, of whom 852 attempted suicide once, 90 attempted suicide twice, and 43 attempted suicide 3 times or more. A total of 147 patients attempted suicide within 3 months from stroke, 44 of whom attempted suicide while still in hospital. We observed 260 completed suicides (fatal), 233 of which were first attempt suicides.
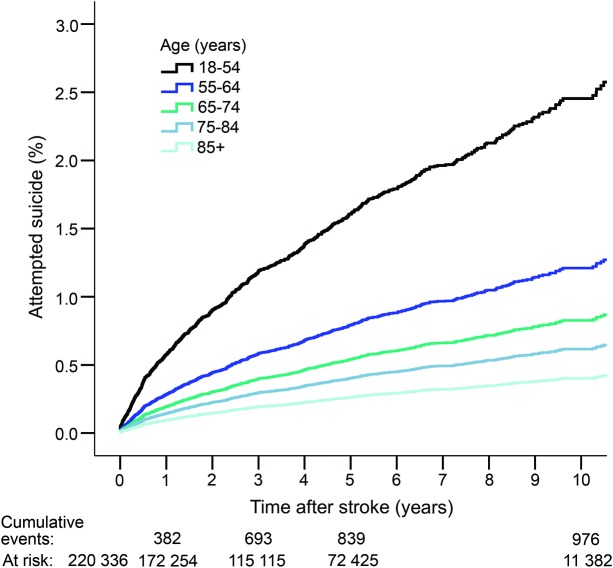
Young age was strongly associated with an increased risk of attempted suicide (table 1; figure 1) and the youngest patients (18–54 years) had 6 times higher risk compared to patients over 85 years. Men had an increased risk compared to women (HR 1.39), which was partially explained by men's younger age at stroke onset (HR 1:19 after adjustment for age) (table 1).
Table 1.
Sex, age, and socioeconomic factors
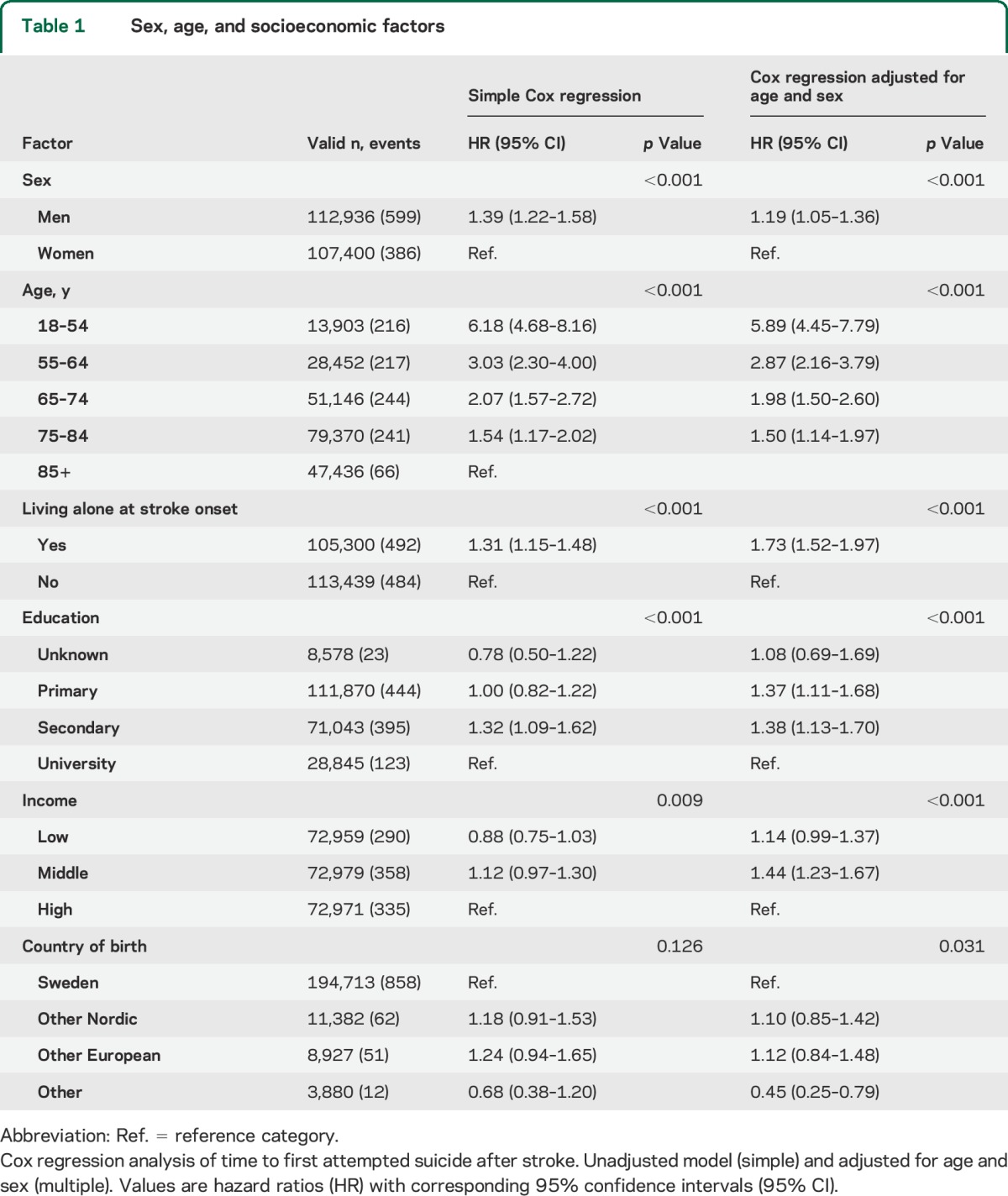
Figure 1. Proportion of patients attempting suicide after stroke.
Estimated proportion of stroke patients attempting suicide (Cox survival regression). Cumulative number of events and number of patients at risk at 0, 1, 3, 5, and 10 years after stroke in different age groups.
After adjustments for sex and age, patients living alone at stroke onset had an increased risk of attempted suicide compared to married or cohabiting patients. Moreover, patients with primary or secondary school education and patients with low and middle income also had an increased risk compared with university-educated and high-income patients (table 1). Patients born outside Europe had a markedly lower risk of attempted suicide (HR 0.45).
We performed a sensitivity analysis in patients with 3-month follow-up data from Riksstroke. ADL function 3 months after stroke was added to the model (in addition to age and sex), showing similar results.
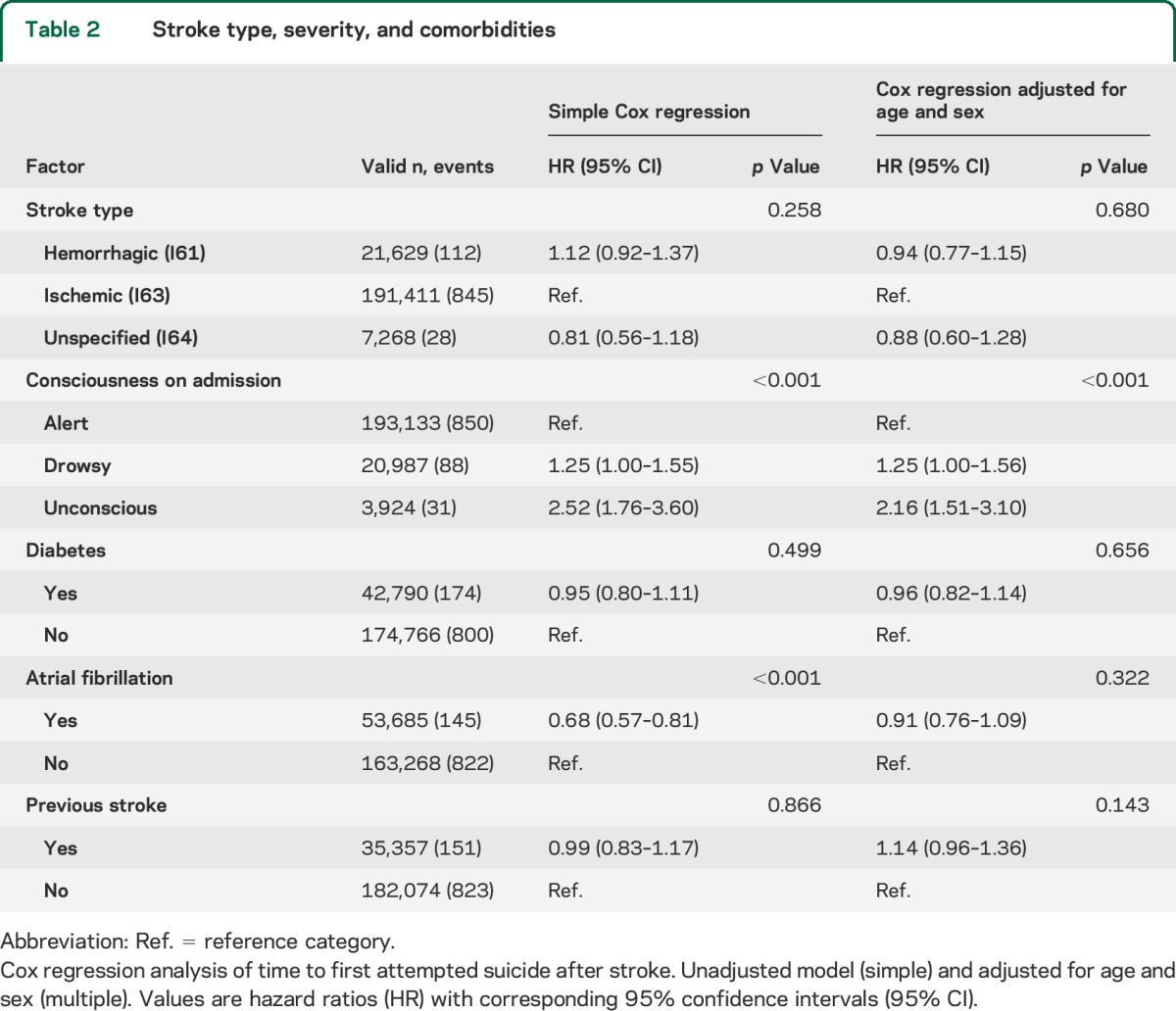
Stroke severity (being drowsy or unconscious on hospital admission) was another factor related with risk of attempted suicide. Stroke type and comorbidities (diabetes, atrial fibrillation, and previous stroke) were not significantly associated with attempted suicide (table 2).
Table 2.
Stroke type, severity, and comorbidities
Of the 1,217 attempts, 889 (73.0%) were by means of self-poisoning, 199 (16.4%) by hanging, drowning, or firearm discharge, 68 (5.6%) by sharp or blunt object, 44 (3.6%) by jumping or by crashing of a vehicle, and 17 (1.2%) by other means. The incidence rate of a first attempted suicide was highest in the first year after stroke at 2.2 suicide attempts per 1,000 person-years. This rate decreased to 1.3 attempts the second year and 1.1 attempts the third year, and it stabilized at 0.8 attempts in subsequent years after the stroke (figure 1).
Self-reported outcome 3 months after stroke.
A total of 179,495 (81.5%) of the patients were still alive 3 months after their stroke and completed the Riksstroke follow-up. Of those, 284 patients had attempted suicide within 1 year after their stroke. A higher proportion of patients who attempted suicide compared to those who did not perceived their health as poor or very poor (42.7% vs 20.5%, χ2 test p < 0.001, OR adjusted for age and sex 3.20, 95% CI 2.48–4.13), reported that they often or always felt depressed (41.1% vs 13.0%, p < 0.001, OR 4.65, 95% CI 3.62–5.97), and were using antidepressant medication (51.4% vs 18.8%, p < 0.001, OR 4.98, 95% CI 3.89–6.38) at 3 months after their stroke. The proportion of patients who were dependent in ADL did not differ significantly between the 2 groups (21.0% vs 24.9%, p = 0.133, OR 1.10, 95% CI 0.81–1.49).
A Cox regression analysis of time from 3-month follow-up to first suicide attempt showed similar results concerning the association between self-reported outcome and risk of attempted suicide (data not shown).
Incidence of complete suicides after stroke compared to the general Swedish population.
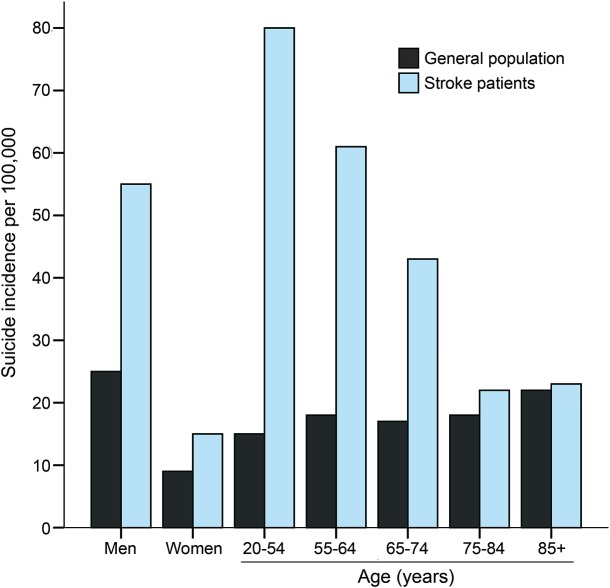
We observed 260 complete suicides for an incidence rate of 30 suicides per 100,000 person-years, and this was higher than the general adult Swedish population with the same age distribution that has an incidence rate of 16 suicides per 100,000 person-years.
The first-year sex-specific incidence of suicide in stroke patients compared to the general population was 15 vs 9 in women and 55 vs 25 in men per 100,000 person-years (figure 2). The incidence was highest in younger stroke patients at 80 suicides per 100,000 person-years in 20- to 54-year-old patients compared with 15 suicides per 100,000 person-years in the same age group in the general Swedish population. In older patients, the incidence decreased to a similar rate as in the general population (figure 2).
Figure 2. Suicide incidence 1 year after stroke compared to the general Swedish population.
Incidence of complete suicides 1 year after stroke per 100,000 person-years in men and women and different age groups compared to the general Swedish population, 2001–2011.
DISCUSSION
Specific socioeconomic groups of stroke patients, namely those with a low level of education, low income, or who are single, are at particularly high risk of poststroke suicide attempts. On the other hand, the risk is markedly lower in stroke patients born outside Europe compared to patients born in Sweden or other European countries. The risk of suicide is particularly high within the first 2 years after the stroke.
Our results demonstrate that poststroke suicides have about the same socioeconomic profile as suicides in the general population.7 A previous Swedish study of the general population has, like ours, shown the risk of suicide to be markedly lower in people born outside Europe compared to those born in Sweden.19 This was driven by a particularly low risk among people born in the Middle East and a possible explanation may be protective religious and cultural factors.19
In addition to the results on socioeconomic factors associated with suicide, our results confirm some previous observations on stroke patients committing suicide. A marked risk increase in younger age groups has previously been reported.1 There seems to be a breaking point around 75 years, and in stroke patients above this age there is no apparent excess risk of suicide. This is notable because the risk of depression, including poststroke depression,20 increases with age. However, most elderly people do not expect to live a life without disease, and they tend to accept physical illness and functional impairments more than younger people do.21 It might also be that elderly stroke patients are less apt to take drastic initiatives or that they have reduced capacity to take their own lives. The latter may also explain why dependency in ADL appeared not to associate with poststroke suicide even if stroke severity did.
There is no previous information on how the risk of suicide relates to stroke severity. However, in a Finnish stroke population suicidal ideation was more common in patients with severe impairment after stroke.22 Our finding that the excess risk levels off a few years after the stroke agrees with previous findings.5,23
We found that self-reported poor health and low mood at 3 months after stroke were strong predictors of suicide attempts. The suicidal thoughts that often emerge after stroke3,9,24 have mostly been regarded as a psychological reaction to the stroke and its consequences with suicide being regarded as a solution to a perceived intolerable life situation.25 Thus stroke would be similar to other severe neurologic disorders in which suicidal thoughts are common.25 Suicidal thoughts early after stroke more related to biological effects of the stroke have in previous studies been distinguished from delayed suicidal thoughts, which seem to be associated with the psychological impact of dealing with cognitive and physical impairments, hopelessness, and other negative feelings.9,24
The association between poststroke depression and suicide ideation has repeatedly been observed.1 We now report that actual suicide attempts are, not unexpectedly, associated with depressed mood after stroke. It is notable that more than half of the patients attempting suicide had been treated with antidepressant drugs. Our study was not designed to explore any eventual effect of antidepressants on the risk of suicide after stroke, but our findings suggest that—in a majority of patients with suicide attempts—clinical depression had been diagnosed and treated without any preventive effects on suicide attempts.
The incidence of completed suicide after stroke was low, with only one in 3,000 stroke patients committing suicide during the first year after stroke. This is considerably lower than what was reported from Denmark in a study performed in the 1980s and early 1990s,5 which is still the only previous population-based study providing incidence or mortality data. Part of the difference between that study and ours might be that the Danish stroke population was, on average, 9 years younger than in our study. Also, completed suicides have declined by more than 50% in Sweden (as in most other Western European countries) since the 1980s.26 The relatively low incidence of completed suicide after stroke is notable in light of the fact that suicidal ideation occurs in as many as 10%–15% of all stroke patients.2,3,22
A strength of this study is that it has nationwide coverage, with all hospitals in the country admitting acute stroke patients participating in the Riksstroke register. The coverage is high and is estimated at 94% of all stroke patients in the country.12 Because all hospitals are publicly financed, there is minimal risk of active patient selection by ability to pay. Using personal identification numbers, linkage to both the Patient Administrative Register and the Cause of Death Register was possible. This permitted us to analyze both attempted suicides resulting in hospital admission and completed suicides. The Riksstroke database has permitted more detailed analyses than in studies based solely on routine administrative data.
Our findings might be limited by the use of administrative registers to study outcome because suicide diagnoses have not been systematically validated in the Swedish Inpatient Register and the Cause of Death Register. However, positive predictive values for various inpatient register diagnoses are high at 85%–95%.15 The stroke diagnoses in Swedish hospitals have a positive predictive value of 88%.13 The imprecision in diagnoses might affect absolute levels (incidence), but because attempted and completed suicides were ascertained in the same way in different patient subgroups, it is less likely that relative differences between patient groups (HRs) were affected. We did not include self-inflicted injuries with unclear intention (ICD-10 diagnosis codes Y10–Y34). Therefore, the estimates of poststroke suicides might be conservative.
Registration in Riksstroke has been kept simple in order to maximize coverage and the lack of detailed medical information is a limitation. Level of consciousness was used as a proxy for stroke severity, and outcome measures like depression and ADL were self-reported by the patient rather than assessed clinically. Riksstroke's question of depression has been validated against The Primary Care Evaluation of Mental Disorders showing a high specificity but a low sensitivity20 and Riksstroke's assessment of ADL dependency has shown high sensitivity and specificity against the Barthel Index.27
Despite more than 200,000 stroke patients being observed for at least 1 year, only 985 patients attempting suicide were observed. Although this makes our study the largest ever performed on poststroke suicide, we cannot rule out that nonsignificant associations (e.g., concerning comorbidities) were due to lack of power to detect weaker associations. The limited number of events did not permit extensive subgroup analyses. It would, for instance, have been of value to explore in more detail which non-European cultures are associated with a particularly low risk of poststroke suicide. Rates and means of suicide vary between countries28 and our results may only be generalized to other modern welfare states.
A major implication of this study is that although suicide attempts and completed suicides are relatively uncommon after stroke, subgroups of stroke patients at clearly elevated risk can be identified. Indicators of enhanced risk for suicide include not only clinical but also socioeconomic factors. In high-risk groups, there is reason to explore suicidal thoughts and behaviors and to specifically consider psychosocial support and suicide preventive interventions (e.g., improve recognition and management of depression, reduction of social isolation, easy access to care, and suicide means restriction).29,30
Supplementary Material
ACKNOWLEDGMENT
The authors thank the members of the Riksstroke Collaboration (http://www.Riksstroke.org).
GLOSSARY
- ADL
activities of daily living
- CI
confidence interval
- HR
hazard ratio
- ICD-10
International Classification of Diseases–10
- OR
odds ratio
- RLS
Reaction Level Scale
Footnotes
Editorial, page 1724
AUTHOR CONTRIBUTIONS
All authors participated in the planning of the study. M.E. performed the statistical analysis and drafted and revised the manuscript. E.-L.G. and B.N. revised the manuscript. K.A. drafted and revised the manuscript.
STUDY FUNDING
Supported by grants from the Swedish Research Council for Health, Working Life and Welfare (grant No. 2011-0657) and the Swedish Research Council (2011–2395).
DISCLOSURE
M. Eriksson and E. Glader report no disclosures relevant to the manuscript. B. Norrving serves on the data safety monitoring board for Astra Zeneca; has received speaker honoraria from Bayer HealthCare Pharmaceuticals and Daiichi Sankyo; serves as senior consulting editor for Stroke, on the editorial board for International Journal of Stroke, and as associate editor for Neuroepidemiology; has received royalties for Hjärnan, Karolinska Institutet University Press, and Oxford Textbook on Stroke and Cerebrovascular Disease, Oxford University Press 2014; and has received research grants from European Union, European Stroke Implementation Score (EIS) project. K. Asplund reports no disclosures relevant to the manuscript. Go to Neurology.org for full disclosures.
REFERENCES
- 1.Pompili M, Venturini P, Campi S, et al. Do stroke patients have an increased risk of developing suicidal ideation or dying by suicide? An overview of the current literature. CNS Neurosci Ther 2012;18:711–721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fuller-Thomson E, Tulipano MJ, Song M. The association between depression, suicidal ideation, and stroke in a population-based sample. Int J Stroke 2012;7:188–194. [DOI] [PubMed] [Google Scholar]
- 3.Santos CO, Caeiro L, Ferro JM, Figueira ML. A study of suicidal thoughts in acute stroke patients. J Stroke Cerebrovasc Dis 2012;21:749–754. [DOI] [PubMed] [Google Scholar]
- 4.Stenager EN, Madsen C, Stenager E, Boldsen J. Suicide in patients with stroke: epidemiological study. BMJ 1998;316:1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Teasdale TW, Engberg AW. Suicide after a stroke: a population study. J Epidemiol Community Health 2001;55:863–866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yamauchi T, Inagaki M, Yonemoto N, et al. Death by suicide and other externally caused injuries after stroke in Japan (1990-2010): the Japan public health center-based prospective study. Psychosom Med 2014;76:452–459. [DOI] [PubMed] [Google Scholar]
- 7.Mortensen PB, Agerbo E, Erikson T, Qin P, Westergaard-Nielsen N. Psychiatric illness and risk factors for suicide in Denmark. Lancet 2000;355:9–12. [DOI] [PubMed] [Google Scholar]
- 8.Nilsson I, Jansson L, Norberg A. Crisis phenomena after stroke reflected in an existential perspective. Int J Aging Hum Dev 1999;49:259–277. [DOI] [PubMed] [Google Scholar]
- 9.Kishi Y, Kosier JT, Robinson RG. Suicidal plans in patients with acute stroke. J Nerv Ment Dis 1996;184:274–280. [DOI] [PubMed] [Google Scholar]
- 10.Asplund K, Hulter Asberg K, Appelros P, et al. The Riks-Stroke story: building a sustainable national register for quality assessment of stroke care. Int J Stroke 2011;6:99–108. [DOI] [PubMed] [Google Scholar]
- 11.Anell A, Glenngard AH, Merkur S. Sweden health system review. Health Syst Transit 2012;14:1–159. [PubMed] [Google Scholar]
- 12.Riksstroke. Riksstroke Årsrapport 2012 [Annual Report 2012]. Available at: http://www.riksstroke.org/wp-content/uploads/2014/02/Riks-Strokes_Arsrapport-2012.pdf. Accessed August 1, 2014. [Google Scholar]
- 13.Koster M, Asplund K, Johansson A, Stegmayr B. Refinement of Swedish administrative registers to monitor stroke events on the national level. Neuroepidemiology 2013;40:240–246. [DOI] [PubMed] [Google Scholar]
- 14.Starmark JE, Stalhammar D, Holmgren E. The reaction level scale (RLS85): manual and guidelines. Acta Neurochir 1988;91:12–20. [DOI] [PubMed] [Google Scholar]
- 15.Ludvigsson JF, Andersson E, Ekbom A, et al. External review and validation of the Swedish national inpatient register. BMC Public Health 2011;11:450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.National Board of Health and Welfare. Dödsorsaksregistret [Cause of Death Registry]. Available at: http://www.socialstyrelsen.se/register/dodsorsaksregistret. Accessed July 31, 2014. [Google Scholar]
- 17.Statistics Sweden. Longitudinell Integrationsdatabas För Hälsoförsäkrings- Och Arbetsmarknadsstudier (LISA) [Longitudinal Integration Database for Health Insurance and Labour Market Studies]. Available at: http://www.scb.se/lisa. Accessed July 31, 2014. [Google Scholar]
- 18.National Board of Health and Welfare. Statistikdatabasen [Statistical Database]. Available at: http://www.socialstyrelsen.se/statistik/statistikdatabas/dodsorsaker. Accessed July 31, 2014. [Google Scholar]
- 19.Westman J, Sundquist J, Johansson LM, Johansson SE, Sundquist K. Country of birth and suicide: a follow-up study of a national cohort in Sweden. Arch Suicide Res 2006;10:239–248. [DOI] [PubMed] [Google Scholar]
- 20.Eriksson M, Asplund K, Glader EL, et al. Self-reported depression and use of antidepressants after stroke: a national survey. Stroke 2004;35:936–941. [DOI] [PubMed] [Google Scholar]
- 21.Sarkisian CA, Hays RD, Mangione CM. Do older adults expect to age successfully? The association between expectations regarding aging and beliefs regarding healthcare seeking among older adults. J Am Geriatr Soc 2002;50:1837–1843. [DOI] [PubMed] [Google Scholar]
- 22.Pohjasvaara T, Vataja R, Leppavuori A, Kaste M, Erkinjuntti T. Suicidal ideas in stroke patients 3 and 15 months after stroke. Cerebrovasc Dis 2001;12:21–26. [DOI] [PubMed] [Google Scholar]
- 23.Forsstrom E, Hakko H, Nordstrom T, Rasanen P, Mainio A. Suicide in patients with stroke: a population-based study of suicide victims during the years 1988-2007 in northern Finland. J Neuropsychiatry Clin Neurosci 2010;22:182–187. [DOI] [PubMed] [Google Scholar]
- 24.Kishi Y, Robinson RG, Kosier JT. Suicidal plans in patients with stroke: comparison between acute-onset and delayed-onset suicidal plans. Int Psychogeriatr 1996;8:623–634. [DOI] [PubMed] [Google Scholar]
- 25.Arciniegas DB, Anderson CA. Suicide in Neurologic illness. Curr Treat Options Neurol 2002;4:457–468. [DOI] [PubMed] [Google Scholar]
- 26.World Health Organization Regional Office for Europe. European Health for All Database (HFA-DB). Available at: http://data.euro.who.int/hfadb/. Accessed August 12, 2014. [Google Scholar]
- 27.Glader EL. Stroke Care in Sweden: Hospital Care and Patient Follow-up Based on Riks-stroke, the National Quality Register for Stroke Care [Doctoral Thesis]. Umeå: Umeå University; 2003. [Google Scholar]
- 28.Hawton K, van Heeringen K. Suicide. Lancet 2009;373:1372–1381. [DOI] [PubMed] [Google Scholar]
- 29.Lapierre S, Erlangsen A, Waern M, et al. A systematic review of elderly suicide prevention programs. Crisis 2011;32:88–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mann JJ, Apter A, Bertolote J, et al. Suicide prevention strategies: a systematic review. JAMA 2005;294:2064–2074. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.