Abstract
Study Design
Review paper
Introduction
Hand dexterity is multifaceted and essential to the performance of daily tasks. Timed performance and precision demands are the most common features of quantitative dexterity testing. Measurement concepts such as rate of completion, in-hand manipulation and dynamic force control of instabilities are being integrated into assessment tools for the pediatric population.
Purpose
To review measurement concepts inherent in pediatric dexterity testing and introduce concepts that are infrequently measured or novel as exemplified with two assessment tools.
Methods
Measurement concepts included in common assessment tools are introduced first. We then describe seldom measured and novel concepts embedded in two instruments; the Functional Dexterity Test (FDT) and the Strength-Dexterity (SD) Test.
Discussion
The inclusion of measurement concepts and tools that are infrequently measured or novel in our repertoire of assessments potentially aids our understanding of atypical dexterity contributing to the design of targeted therapy programs.
Keywords: brachial plexus injury, infant, child, assessment, muscle, weakness, international classification of functioning, disability, health
Introduction
Clinicians examine dexterity to gauge skill level and change in performance after hand surgery or rehabilitation. Differences in proficiency based on age, development, hand dominance, cognition and clinical conditions are verified through assessment. The purpose of this paper is to review measurement concepts integral to pediatric dexterity testing and introduce concepts that are seldom measured or novel as exemplified with two assessment tools.
The terms “dexterity” and “manipulation” have many definitions and connotations. In children dexterity and manipulation skills change with development which also presents a challenge to their assessment. Therefore it is critical that the clinician select and use a tool that can quantify, and is sensitive to changes in, the components of dexterity of clinical interest in the developing child. Our objective is not to advocate for a specific dexterity assessment tool — as this depends on the scientific and clinical purpose of measurement. Instead, we review features of dexterity and measurement concepts that are integral to common tools validated in pediatrics and introduce innovative concepts embedded within the design of a few sample instruments.
Dexterity Measurement
Dexterity can be measured through observation of task performance, recording from a checklist or the use of a standardized assessment tool. Common features of standardized tools are timed performance and precision. The time for task completion is often measured in seconds or minutes using a timer.1-2 Precision is illustrated by the expectation to place small rings on thin pegs in the Purdue Pegboard Test.3 Table 1 outlines features of dexterity testing measured with common dexterity tests with normative values for children. Normative reference values are useful with pediatric populations, where it is important to distinguish between expected developmental changes and the effects of intervention.
Table 1. Features of Common Pediatric Dexterity Tests with Normative data.
| DEXTERITY TEST | Pediatric Norms | Timed Test | Precision | In Hand Manipulation | Time to Administer |
|---|---|---|---|---|---|
| Box and Block4-6 | 6-19 years | Yes | Yes | No | < 5 min* |
| Grooved Pegboard Test 1,7 | 3-20 years | Yes | Yes | Yes – rotation of peg | > 5 min* |
| Jebsen Taylor Hand Function Test 6,8 | 6-19 years | Yes | Yes – stack checkers | Yes – rotation of spoon | > 5 min |
| Nine Hole Peg Test 1-2 | 3 to 20 years | Yes | Yes | Yes - rotation & translation of peg assessed – not validated9-10 | < 5 min |
| Purdue Pegboard1,3,6, 11-12 | 2.6 to 5.11 years, 5-15 years, 14-19 years | Yes | Yes | No | < 5 min |
< 5 = less than 5; > 5 = more than 5; min = minutes
Features of dexterity that are not often measured or are more difficult to measure include: 1) rate of completion; 2) in-hand manipulation; and 3) dynamic force control. For example, in-hand manipulation has been explored but not fully integrated into dexterity testing (see Table 1). To better understand the value of including innovative measurement concepts in our assessments we will review the concepts and describe a few dexterity tests that incorporate them.
Rate of Completion and In-Hand Manipulation
In addition to measuring the time to task completion, performance can be expressed as a rate of task completion (i.e., speed).13 This scoring strategy allows for statistically valid numerical comparisons against other quantitative functional variables and graphing of rate of completion along a continuous age scale. Although useful this scoring strategy is rarely used in dexterity testing.
In-hand manipulation (IHM) is defined as movement or reconfiguration of an object as it is held with one hand.13 Although there are other taxonomies for IHM,15-17 the classification scheme by Exner18-19 is described here by three main features: shift (movement across finger pads), translation (finger-to-palm and palm-to-finger), and rotation (simple and complex). The three components of IHM are assessed with the task of picking up a coin and placing it in a vertical slot. In this example, shift is displayed when we move the coin across the finger pads; while palm-to-finger translation is demonstrated when we move the coin from the palm to the finger pads. Complex rotation is illustrated when we turn the coin on its axis with the fingers, before placement in a slot. IHM develops between 18 months and 7 years of age.14, 18 By 3 years of age, IHM has developed to the point that standardized testing can be reliably performed.9-10,19 IHM is required to complete the Functional Dexterity Test (FDT).13,20
Functional Dexterity Test (FDT)
The Functional Dexterity Test (North Coast Medical, Gilroy, CA) is a timed pegboard instrument.20 The FDT is not new but employs the unique concepts of rate of completion and in-hand manipulation that are not commonly measured. When validated in adults, the FDT had excellent test-retest (ICC=0.95) and intra-rater (ICC=0.91) reliability.20 When compared against performance tests that assess activity and participation, it had the highest ratings for clinimetric quality.21 Adult FDT normative reference values are published20 and were recently updated22. Pediatric normative values are also available.13
The FDT consists of 16 cylindrical pegs (4 cm × 2.2 cm) arranged in four rows of four pegs each (Figure 1). It requires a tripod pinch and two aspects of IHM; rotation and shift. Participants turn over all pegs (rotation) in a specified order by manipulating each peg with the finger pads (shift). Participants complete one practice trial and the second trial is timed. Results are recorded as the number of pegs completed divided by time elapsed (pegs/time). This calculation of a test score provides a measure of speed.23 The original FDT scoring involved assessing penalties and adding their point values to the test completion time to arrive at a final score.20 Even though the penalties were subsequently modified for children24 they proved inadequate. As grasp and movement patterns develop a true assessment of pediatric penalties would require a menu of changing, age-specific items, which hampers the ease of test administration. Inefficient movements are reflected in decreased speed, thus do not require the additional adjustment for penalties.13 The FDT is sensitive enough to detect functional inefficiencies of IHM, and thus penalties have been eliminated from pediatric FDT scoring.
Fig. 1.
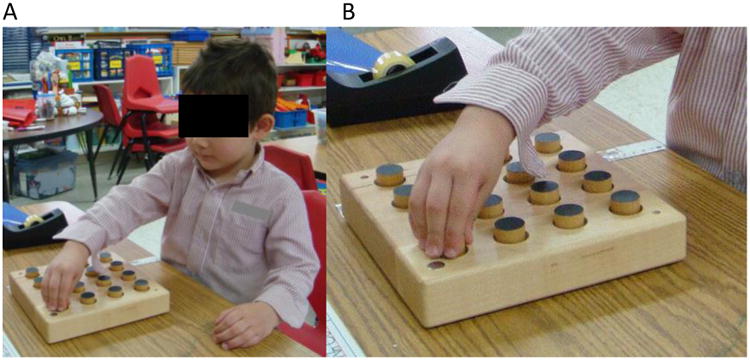
A: The FDT can be easily administered to very young children, allowing for longitudinal evaluation into adulthood. B: A unimanual 3-jaw chuck prehension pattern is required.
Normative FDT speed (pegs/sec) for the dominant and non-dominant hands among typically-developing children increases linearly with age at a constant rate of 0.037pegs/sec/year between 3 to 17 years of age (Figure 2).13 There are no gender differences through 17 years of age. Dominant hands are faster than non-dominant hands at all ages and the difference between the two remains constant.
Fig. 2.
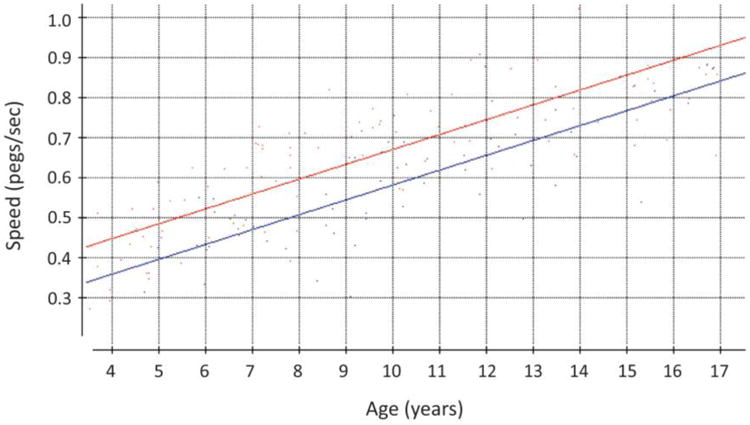
Normative FDT scatterplot showing speed (pegs/second) versus age. The continuous “growth chart” style (versus arbitrary age groupings) allows for more precise comparison to typically developing children 4 to 17 years old. Dominant hands are shown in red, non-dominant hands in blue.13 Permission to reprint from Gogola et al13 was received.
Presenting normative values as a “growth chart” of FDT speed versus age facilitates easy visualization of expected speed for any given age using a continuous age scale. The use of regression on fractional age provides a more precise estimate of performance than would be possible by presenting the data in a table grouped by arbitrary age ranges. Clinicians who treat children are accustomed to this “growth chart” format for tracking height and weight. It has also been successfully used to report pediatric hand strength.25-26 Based on linear regression analysis, age and hand dominance can predict speed. The available norms allow clinicians to compare both speed and rate of change over time of pediatric clients against the norms for typically-developing children.
The FDT has been used in children to assess dexterity after pollicization27 (surgically replace an absent thumb with a functional finger)28-30 and performance in children with congenital conditions. We used the FDT to assess the unaffected hands of children ages 4 to 17 years of age with unilateral congenital differences and found that the unaffected hands were slower than the age-matched norms (unpublished). The results revealed that dexterity in the unaffected hands of unilaterally affected children does not develop at the same rate as typically-developing peers; strengthening the notion that contralateral hands should be included in therapeutic programming. Current work includes instrumenting the individual FDT pegs with wireless inertial sensors equipped with an accelerometer and gyroscope in order to acquire movement data (smoothness, jerk, and accuracy) in addition to speed.
The FDT is an example of a tool that requires IHM and measures the unique feature of rate of completion. It is easy to administer and accommodates a child's short attention span and clinical time constraints. It reliably measures the performance of young children with and without congenital hand differences. Finally, it can detect subtle deficits missed with visual observations or simpler grasp and release dexterity instruments.
Dynamic Force Control
Hand-held dynamometers and pinch meters have been used extensively to quantify normative and clinical levels of static grip and pinch strength.31 Unfortunately, these measures of force magnitude are not informative of the dexterous capabilities of the person as they include the potential confounds of motivation, pain avoidance, etc. Interestingly, Lee-Valkov and colleagues24 found that in typically developing children pinch strength correlated poorly with dexterity based on the FDT. In addition, the prehensile forces necessary to engage in activities of daily living (ADL) are surprisingly low.32 Therefore; although clinically useful for other reasons, maximal static force magnitude may not be an essential component of dexterity measurement.
Skilled grasp and manipulation of objects requires grading of fingertip forces to prevent slips and breakage.33 We grade grip (squeeze) and load (lift) force in advance of object contact (anticipatory control) and modify these forces based on somatosensory feedback during manipulation.34 Fingertip force magnitude and the rate of onset are usually low when we grasp a potato chip and increase when we lift a full glass of water. In adults, grip and load force increase in a parallel, synergistic manner whereas in young children fingertip forces increase sequentially35 with long durations exhibited for each task phase (i.e., time to increase grip force); suggesting dominance of a feedback strategy early on.35 After two years of age both feedback and anticipatory control strategies are evident by the more frequent display of single peaked force rate profiles and shorter phase durations during grip-lift tasks of static objects.35
Dynamic manipulation (as opposed to grip-lift tasks) requires that the direction and magnitude of fingertip force vectors be continuously modified to maintain object stability during task performance. 36-38 As dexterity develops, the quality of manipulation is influenced by the task goal and our ability to maintain stability of the grasped object by aptly responding to perturbations or task dynamics.39-41 Improvement in dynamic manipulation progresses into late adolescence; influenced by the development of the neuromuscular system, experience and improvement in sensorimotor control.37,40,42-43
The method used to capture the capacity to grade fingertip forces is based on the information desired. Indirect assessment can be done through task performance such as stacking checkers during the Jebsen Test of Hand Function8. Objective measurement of performance on static grip-lift tasks usually involves laboratory-based instruments equipped with single or multi-axial force transducers.43 Dynamic manipulation must be assessed by the ability to regulate fingertip force vectors to control unstable objects.36-38 While a measure of dynamic force control would be useful, the challenge is how to quantitatively measure it in the clinic.
Strength-Dexterity Test
To quantify the dynamic regulation of magnitude and direction of fingertip forces Valero-Cuevas et al.36 developed the Strength-Dexterity (S-D) paradigm. This paradigm has been used to assess hand dexterity in typical and atypical adults36,38,41,44 and children.37,40,45-46 The SD test is not yet commercially available yet details of the SD device are described in previous publications.36-38,41,44-51 In the SD Test individuals use the fingertips to compress a slender and compliant spring that is prone to buckling (Figure 3).52 Buckling is a form of instability, which becomes exacerbated as the spring is compressed further—noting that the force magnitudes needed to compress the spring the limit of instability are very low, on the order of < 3N. Retaining control of the spring requires dynamic regulation of the magnitude and direction of the finger movements and fingertip force vectors. To obtain quantitative data, the compression spring can be fit with two miniature compression load cells (ELB4-10, Measurement Specialties, Hampton, VA) to record dynamic compression forces, as depicted in Figure 3. The maximal level of compression (units of force) is indicative of the maximal level of instability that the neuromusculoskeletal system is able to control.37-38 This metric serves as an informative measure of neuromotor control for dexterous manipulation.
Fig. 3.
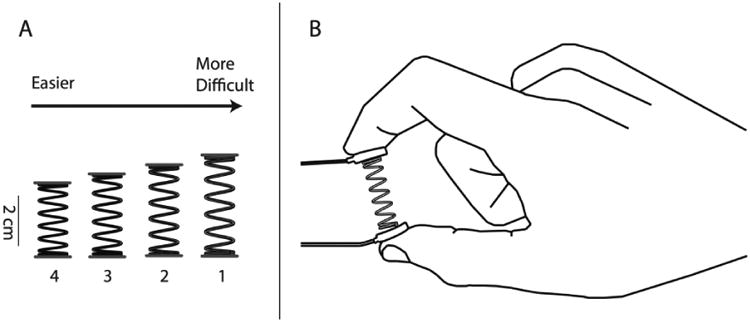
Four springs used for a pediatric version of the Strength-Dexterity Test.35 Note the SD Test shown is a particular instance of the SD paradigm (Figure 4). In this SD Test, miniature load cells mounted on either end of the spring over plastic end caps. The compression requires force magnitudes < 3 N. The task requires a two-finger palmar pinch or a lateral pinch to compress and hold the spring at the maximal compression force without buckling. Permission to reprint from Dayanidhi et al.37 was received.
In the SD paradigm, the mechanical design of the spring determines the force magnitudes needed to compress it to the limit of instability.36 The current SD Test which expanded upon work in pediatric populations,45 is designed to require very low force magnitudes c. 2-3 N.37-38,52 The SD paradigm was developed to explicitly separate the dexterity and strength requirements of the task as described in Valero-Cuevas et al36, 50 and shown in Figure 4 from Dayanidhi et al.37
Fig. 4.
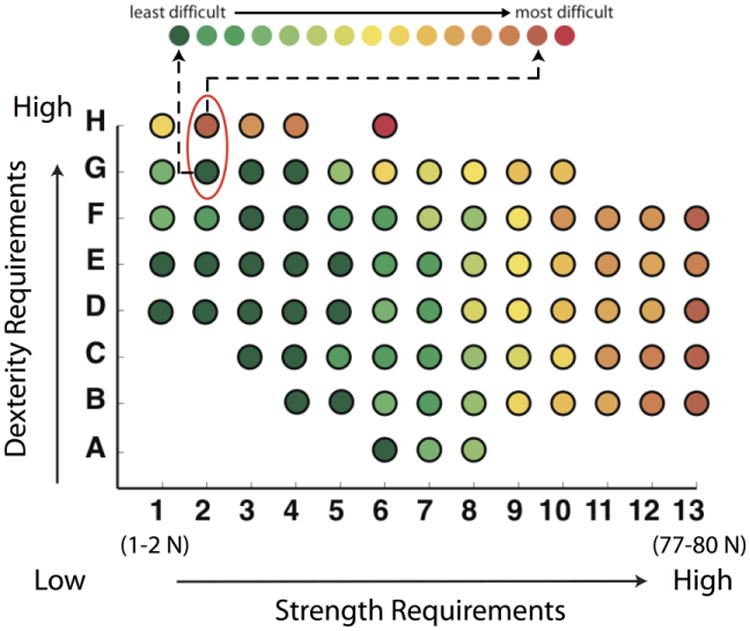
The Strength-Dexterity paradigm uses a two-dimensional plane34 to explicitly distinguish the contribution of strength from dexterity requirements. The material properties and geometry of the springs can be adjusted to be more or less prone to buckling (unstable), or more or less stiff. Stiffer springs increase the strength requirement (x axis). More slender springs increase the dexterity requirement (y axis). As shown in Vollmer et al.,45 springs in the lower range of the strength requirement (< 3 N) can be appropriate for pediatric and clinical use. They allow the quantification dexterity (i.e., the neuromuscular ability to stabilize an unstable object prone to buckling with the fingertips) while requiring little strength. Figure adapted from Valero-Cuevas et al,36 Vollmer et al.,45 and Talati et al.50 Permission to reprint from Dayanidhi et al.37 was received.
Obtaining a dexterity score using the SD Test requires individuals compress the spring in a controlled, self-paced manner to the point of maximal compression without slippage or uncontrolled buckling.37 Participants familiarize themselves with this task (∼10 repetitions) until they exhibit compression for ≥ five seconds (Figure 5).37,46 After familiarization, individuals complete a minimum of 10 trials/hand while sustained compression force is recorded. The mean sustained grip force for three maximal trials is used to calculate the dexterity score in grams of force (gmf).37
Fig. 5.
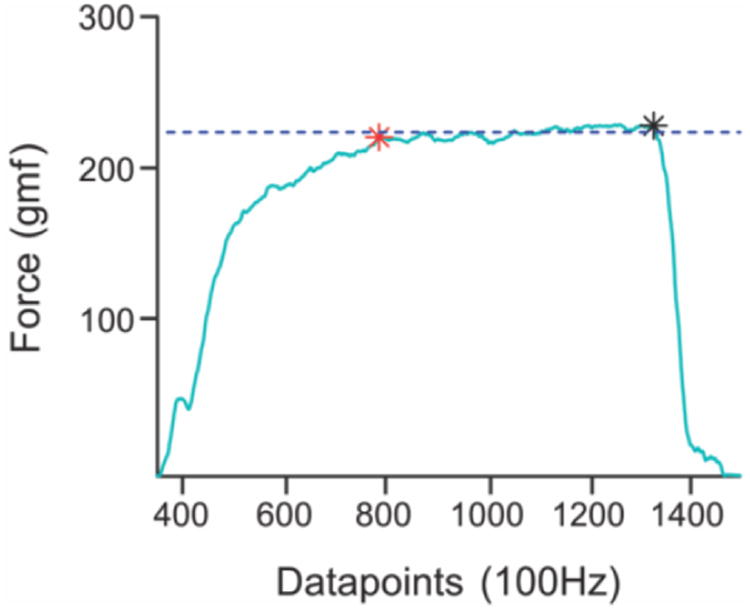
Representative sample of fingertip forces during steady state compression for a single hold using the SD test.35 The red star represents the start and the black star the end of steady state at maximal compression during the 5s hold. Permission to reprint from Dayanidhi et al.37 was received.
The quantification of sensorimotor skill needed to stabilize objects using the dexterity score exemplifies the features of dynamic force control and precision.37, 46 Results from this research have been used to better understand the local and distributed neural mechanisms associated with maturation, muscle contractile speeds, functional neural connectivity and neural networks across gender, age and clinical populations.37,44-51 Results from a pediatric population are shown in Figure 6. Work is in progress to bring the SD paradigm into clinical practice.
Fig. 6.
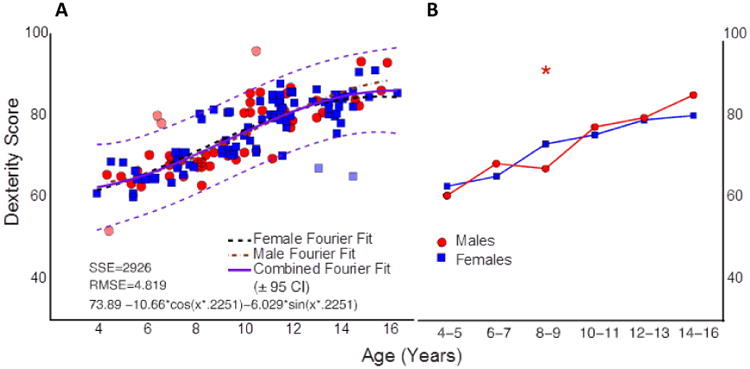
Dexterity score from children 4-16 years of age on the SD test shown to depict the significant change in performance across age. A. The regression line (CI – 95%) on a Fourier robust fit is shown in green/magenta, respectively. Data in A and B are colored by gender (blue, girls; red, boys), with individual regression lines for each. Significant increase in dexterity score by adjacent age groups were found across childhood and into late adolescence as indicated by asterisks (P = < 0.05), SSE=sum of squared residuals; RMSE=root mean squared error; CI=confidence interval. Permission to reprint from Dayanidhi et al.37 was received.
Dexterity Assessment and ADL Function
Measures of dexterity should relate to activities of daily living (ADL) and quality of life. Dexterity tests fall within the Body, Functioning, Structure and Activity Domains of the International Classification of Function for Children and Youth (ICF-CY, Organization)53 depending on the specific features and scoring strategy used. A limited number of studies in adults have been conducted to examine the relationship of findings on dexterity testing to ADL in the Activity Domain of the ICF framework. Poole and colleagues54 report a reduction in dexterity as measured by the Nine-Hole Peg Test and Grooved Peg Test associated with perceived difficulty with ADL and a need for greater assistance as measured by the Functional Status Index55. Aaron and Stenick-Jensen20 report that the FDT scores correlated with ADL tasks that require a 3-jaw chuck (3-fingered pinch) such as buttoning or tying a knot in adults with hand injuries. Improved individual performance of a specific functional task employing a 3-jaw chuck predicted a lower performance time on the FDT. The relationship between performance on ADL tasks and the Nine-Hole Peg Test, the FDT or other tools has not been examined in children.
The SD paradigm measures a dimension of sensorimotor capability different from strength, whole-arm motion, and reach-to-grasp behavior.45 Thus, the SD test's assessment of a child's ability to stabilize objects is unique and informative. Studies are needed that relate performance on the SD test for children to select ADLs requiring dexterity and manipulation.
Summary
The evaluation of dexterity in a pediatric population requires consideration of the developmental level of the child and the clinical condition being evaluated. These factors influence the skill level and dexterity we should expect, thus directing us to the appropriate assessment tool. Although the number of tests available continues to grow, it is important to closely examine the features of dexterity that the tool measures and the measurement concepts involved in scoring. Innovative scoring strategies are characteristic of tools such as the FDT and SD test. The FDT is commercially available with pediatric normative data13 while, the SD test is being examined for clinical utility. As the data becomes available the SD test could provide the pediatric clinician with a unique outcome measure of dynamic force control.
Obtaining a comprehensive view of dexterity requires administration of a combination of assessments. For instance, the combined use of the FDT and SD test could provide measures of rate of completion, in-hand manipulation, and dynamic force control. Validation of common and novel assessments employing unique scoring strategies will add to our understanding of the underlying mechanisms of atypical dexterity and provide pediatric clinical practitioners and researchers with information useful in the design of targeted interventions.
Highlights.
Review of common and seldom used measurement concepts in dexterity testing
Description of innovative scoring strategies and dexterity assessment tools
Acknowledgments
This publication was supported by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development under award number T32HD064578. Research reported was supported by NIAMS of the National Institutes of Health under award numbers R01AR050520 and R01AR052345 to FVC. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Susan V. Duff, Email: susan.duff@jefferson.edu.
Dorit H. Aaron, Email: Dorit@awhand.com.
Gloria R. Gogola, Email: ggogola@shrinenet.org.
Francisco J. Valero-Cuevas, Email: Valero@usc.edu.
References
- 1.Wang YC, Magasi SR, Bohannon RW, et al. Assessing dexterity function: A comparison of two alternatives for the NIH toolbox. J Hand Ther. 2011;24(4):313–321. doi: 10.1016/j.jht.2011.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Poole JL, Burtner PA, Torres TA, McMullen CK, Markham A, Marcum ML, Anderson JB, Qualls C. Measuring Dexterity in Children Using the Nine-hole Peg Test. J Hand Ther. 2005;18:348–351. doi: 10.1197/j.jht.2005.04.003. [DOI] [PubMed] [Google Scholar]
- 3.Wilson BC, Iacoviello JM, Wilson JJ, Risucci D. Purdue Pegboard Performance of Normal Preschool Children. J Clin Neuropsychol. 1982;4:19–26. doi: 10.1080/01688638208401113. [DOI] [PubMed] [Google Scholar]
- 4.Fess EE. Functional tests. In: Skirven TM, et al., editors. Rehabilitation of the Hand and Upper Extremity. 6th. Philadelphia PA: Mosby; 2011. p. 159. [Google Scholar]
- 5.Jongbloed-Pereboom M, Nijhuis-Van Der Sanden MWG, Steenbergen B. Norm scores of the box and block test for children ages 3-10 years. Am J Occup Ther. 2013;67(3):312–318. doi: 10.5014/ajot.2013.006643. [DOI] [PubMed] [Google Scholar]
- 6.Yancosek KE, Howell DA. Narrative review of dexterity assessments. J Hand Ther. 2009;22(3):258–69. doi: 10.1016/j.jht.2008.11.004. [DOI] [PubMed] [Google Scholar]
- 7.Bryden PJ, Roy EA. A new method of administering the Grooved Pegboard Test: Performance as a function of handedness and sex. Brain Cog. 2005;58(3):258–268. doi: 10.1016/j.bandc.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 8.Taylor N, Sand PL, Jebsen RH. Evaluation of hand function in children. Arch Phys Med Rehabil. 1973;54(3):129–135. [PubMed] [Google Scholar]
- 9.Pehoski C, Henderson A, Tickle-Degnen L. In-hand manipulation in young children: rotation movements. Am J Occup Ther. 1997a;51(7):744–52. doi: 10.5014/ajot.51.7.544. [DOI] [PubMed] [Google Scholar]
- 10.Pehoski C, Henderson A, Tickle-Degnen L. In-hand manipulation in young children: translation movements. Am J Occup Ther. 1997b;51(9):719–728. doi: 10.5014/ajot.51.9.719. [DOI] [PubMed] [Google Scholar]
- 11.Gardner RA, Broman M. The Purdue Pegboard: Normative Data on 1334 School Children. J Clin Child Psychol. 1979;1:156–162. [Google Scholar]
- 12.Mathiowetz V, Rogers SL, Dowe-Keval M, Donahoe L, Rennells C. The Purdue Pegboard: Norms for 14- to 19 Year-Olds. Am J Occup Ther. 1986;40:174–179. doi: 10.5014/ajot.40.3.174. Wilson BC, Iacoviello JM. [DOI] [PubMed] [Google Scholar]
- 13.Gogola GR, Velleman PF, Zu S, Morse AM, Lacy B, Aaron D. Hand Dexterity in children: administration and normative values of the functional dexterity test. J Hand Surg Am. 2013;38(12):2426–31. doi: 10.1016/j.jhsa.2013.08.123. [DOI] [PubMed] [Google Scholar]
- 14.Exner CE. Development of hand functions. In: Pratt PN, Allen AS, editors. Occupational Therapy for children. 2nd. St. Louis: Mosby; 1989. [Google Scholar]
- 15.Bullock IM, Dollar AM. Classifying Human Manipulation Behavior. IEEE International Conference on Rehabilitation Robotics. 2011:5975408. doi: 10.1109/ICORR.2011.5975408. [DOI] [PubMed] [Google Scholar]
- 16.MacKenzie CL, Iberall T. The grasping hand. Amsterdam; New York: North-Holland: 1994. [Google Scholar]
- 17.Pont K, Wallen M, Bundy A. Conceptualising a modified system for classification of in-hand manipulation. Aust Occup Ther J. 2009;56(1):2–15. doi: 10.1111/j.1440-1630.2008.00774.x. [DOI] [PubMed] [Google Scholar]
- 18.Exner CE. In-hand manipulation skills. In: Case-Smith J, Pehoski C, editors. Development of Hand Skills in the Child. AOTA; Rockville MD: 1992. [Google Scholar]
- 19.Exner CE. In-hand manipulation skills. In: Case-Smith J, editor. Occupational Therapy for Children. St Louis: Mosby; 2001. [Google Scholar]
- 20.Aaron DH, Stegink Jansen CW. Development of the Functional Dexterity Test (FDT): construction, validity, reliability, and normative data. J Hand Ther. 2003;16:12–21. doi: 10.1016/s0894-1130(03)80019-4. [DOI] [PubMed] [Google Scholar]
- 21.Schoneveld K, Wittink H, Takken T. Clinimetric evaluation of measurement tools used in hand therapy to assess activity and participation. J Hand Ther. 2009;22(3):221–36. doi: 10.1016/j.jht.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 22.Satorio F, Bravini E, Vercelli S, Ferriero G, Plebani G, Foti C, Franchignoni F. The Functional Dexterity Test: test-retest reliability analysis and up-to date reference norms. J Hand Ther. 2013;26(1):62–7. doi: 10.1016/j.jht.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 23.Velleman PF, Hoaglin DC. Exploratory Data Analysis. APA Handbook of Research Methods in Psychology. 2012;3 [Google Scholar]
- 24.Lee-Valkov PM, Aaron DH, Eladoumikdachi F, Thornby J, Netscher DT. Measuring normal hand dexterity values in normal 3-,4-, and 5-year old children and their relationship with grip and pinch strength. J Hand Ther. 2003;16:22–28. doi: 10.1016/s0894-1130(03)80020-0. [DOI] [PubMed] [Google Scholar]
- 25.Molenaar HM, Selles RW, Zuidam JM, Willemsen SP, Stam HJ, Hovius SER. Growth Diagrams for Grip Strength in Children. Clin Orthop Relat Res. 2010;468:217–38. doi: 10.1007/s11999-009-0881-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Xu S, Morse AM, Lacy B, Baggett S, Gogola GR. Peg Restrained Intrinsic Muscle Evaluator (PRIME): Development, Reliability and Normative Values of a Device to Quantify Intrinsic Hand Muscle Strength in Children. J Hand Surg. 2011;36A:894–903. doi: 10.1016/j.jhsa.2011.01.006. [DOI] [PubMed] [Google Scholar]
- 27.Lightdale-Miric N, Mueske NM, Lawrence EL, Loiselle J, Berggren J, Dayanidhi S, Stevanovic M, Valero-Cuevas FJ, Wren TA. Long Term Functional Outcomes After Early Childhood Pollicization. J Hand Ther. 2015 doi: 10.1016/j.jht.2014.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Aliu O, Netscher DT, Staines KG, Thornby J, Armenta A. A 5-Year Interval Evaluation of Function after Pollicization for Congenital Thumb Aplasia Using Multiple Outcome Measures. Plast Reconstr Surg. 2008;122:198–205. doi: 10.1097/PRS.0b013e318177427d. [DOI] [PubMed] [Google Scholar]
- 29.Kozin SH. Pollicization: the concept, technical details, and outcome. Clin Orthop Surg. 2012;4(1):18–35. doi: 10.4055/cios.2012.4.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Staines KG, Majzoub R, Thornby J, Netscher DT. Functional Outcome for Children with Thumb Aplasia Undergoing Pollicization. Plast Reconstr Surg. 2005;116:1314–1324. doi: 10.1097/01.prs.0000181820.36306.a0. [DOI] [PubMed] [Google Scholar]
- 31.Mathiowetz V, Wiemer DM, Federman SM. Grip and pinch strength: norms for 6- to 19 year olds. Am J Occup Ther. 1986;40(10):705–11. doi: 10.5014/ajot.40.10.705. [DOI] [PubMed] [Google Scholar]
- 32.Smaby N, Johanson ME, Baker B, Kenney DE, Murray WM, Hentz VR. Identificaiton of key pinch forces required to complete functional tasks. J Rehabil Res Dev. 2004;41(2):215–24. doi: 10.1682/jrrd.2004.02.0215. [DOI] [PubMed] [Google Scholar]
- 33.Westling G, Johansson R. Roles of glabrous skin receptors and sensorimotor memory in automatic control of precision grip when lifting rougher or more slippery objects. Exp Brain Res. 1984;56:550–564. doi: 10.1007/BF00237997. [DOI] [PubMed] [Google Scholar]
- 34.Johansson R, Cole KJ. Sensory-motor coordination during grasping and manipulative actions. Curr Opin Neurobiol. 1992;2:815–23. doi: 10.1016/0959-4388(92)90139-c. [DOI] [PubMed] [Google Scholar]
- 35.Forssberg H, Eliasson AC, Kinoshita H, Johansson RS, Westling G. Development of human precision grip I: basic coordination of force. Exp Brain Res. 1991;85:451–57. doi: 10.1007/BF00229422. [DOI] [PubMed] [Google Scholar]
- 36.Valero-Cuevas FJ, Smaby N, Venkadesan M, Peterson M, Wright T. The strength-dexterity test as a measure of dynamic pinch performance. J Biomech. 2003;36(2):265–70. doi: 10.1016/s0021-9290(02)00340-8. [DOI] [PubMed] [Google Scholar]
- 37.Dayanidhi S, Hedberg Å, Valero-Cuevas FJ, Forssberg H. Developmental improvements in dynamic control of fingertip forces last throughout childhood and into adolescence. J Neurophysiol. 2013a;110:1583–92. doi: 10.1152/jn.00320.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lawrence EL, Fassola I, Werner I, Leclercq C, Valero-Cuevas FJ. Quantification of dexterity as the dynamical regulation of instabilities: comparisons across gender, age, and disease. Front Neurol. 2014;5(53):1–13. doi: 10.3389/fneur.2014.00053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Contaldo A, Cola E, Minichilli F, et al. Object use affects motor planning in infant prehension. Hum Mov Science. 32(3):498–510. doi: 10.1016/j.humov.2013.02.005. [DOI] [PubMed] [Google Scholar]
- 40.Dayanidhi S, Kutch JJ, Valero-Cuevas FJ. Decrease in muscle contraction time complements neural maturation in the development of dynamic manipulation. J Neurosci. 2013b;33(38):15050–55. doi: 10.1523/JNEUROSCI.1968-13.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Racz K, Valero-Cuevas FJ. Spatio-temporal analysis reveals active control of both task-relevant and task-irrelevant variables. Front Comput Neurosci. 2013;7:155. doi: 10.3389/fncom.2013.00155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Eyre JA. Corticospinal tract development and its plasticity after perinatal injury. Neurosci Biobehav Rev. 2007;31(8):1136–49. doi: 10.1016/j.neubiorev.2007.05.011. [DOI] [PubMed] [Google Scholar]
- 43.Duff SV, Gordon AM. Learning of grasp control in children with cerebral palsy. Dev Med Child Neurol. 2003;45(11):746–57. doi: 10.1017/s0012162203001397. [DOI] [PubMed] [Google Scholar]
- 44.Dayanidhi S, Valero-Cuevas FJ. Dexterous manipulation is poorer at older ages and is dissociated from decline of hand strength. J Geron Series B: Biol Sci Med Sci. 2014;69(9):1139. doi: 10.1093/gerona/glu025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vollmer B, Holmstrom L, Forsman L, Krumlinde-Sundholm L, Valero-Cuevas F, Forssberg H, et al. Evidence of validity of a new method for measurement of dexterity in children and adolescents. Dev Med Child Neurol. 2010;52:948–54. doi: 10.1111/j.1469-8749.2010.03697.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dayanidhi S. PhD dissertation. Los Angeles, CA: University of Southern California; 2012. Behavioral, Muscular and Dynamical Changes in Low Force Dexterous Manipulation during Development and Aging. [Google Scholar]
- 47.Fassola I, Lawrence E, Dayanidhi S, Ko N, Leclercq C, Valero-Cuevas F. Proceedings of the 1st International Thumb Osteoarthritis Workshop. Vol. 13. Newport, RI: 2013. Is osteoarthritis of the thumb strictly a orthopedic condition? p. 12. [Google Scholar]
- 48.Holmström L, Lennartsson F, Eliasson AC, Flodmark O, Clark C, Tedroff K, Forssberg H, Vollmer B. Diffusion MRI in corticofugal fibers correlates with hand function in unilateral cerebral palsy. Neurology. 2011;77:775–783. doi: 10.1212/WNL.0b013e31822b0040. [DOI] [PubMed] [Google Scholar]
- 49.Mosier KM, Lau C, Wang Y, Venkadesan M, Valero-Cuevas FJ. Controlling instabilities in manipulation requires specific cortical-striatal-cerebellar networks. J Neurophysiol. 2011;105:1295–1305. doi: 10.1152/jn.00757.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Talati A, Valero-Cuevas FJ, Hirsch J. Visual and tactile guidance of dexterous manipulation tasks: an fMRI study. Percept Mot Skills. 2005;101:317–34. doi: 10.2466/pms.101.1.317-334. [DOI] [PubMed] [Google Scholar]
- 51.Venkadesan M, Guckenheimer J, Valero-Cuevas FJ. Manipulating the edge of instability. J Biomech. 2007;40:1653–1661. doi: 10.1016/j.jbiomech.2007.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.US patent 6,537.075
- 53.World Health Organization. [cited 2014 Nov 08];International Classification of Functioning, Disability and Health for Children and Youth (ICF-CY) 2014 Available from: http://www.who.int/classifications/icf/en/
- 54.Poole JL, Nakamoto T, McNullty T, Montoya JR, Weill D, Dieruf K, Skipper B. Dexterity, visual perception, and activities of daily living in persons with multiple sclerosis. Occup Ther Health Care. 2010;24(2):159–70. doi: 10.3109/07380571003681202. [DOI] [PubMed] [Google Scholar]
- 55.Jette A. Functional Status Index: Reliability of a chronic disease evaluation instrument. Arch Phys Med Rehabil. 1980;61:395–401. 1980. [PubMed] [Google Scholar]


