Abstract
Objectives
Prescription Drug Monitoring Programs (PDMPs) can help inform patient management, coordinate care, and identify drug safety risks, abuse, or diversion. However, many clinicians are not registered to use these systems, and use may be suboptimal. We sought to describe outreach efforts in one state (Oregon); quantify uptake of system use; identify barriers; and identify potential system improvements.
Methods
Program reports of outreach efforts and operational metrics provided rates of registration and use. A statewide survey identified perceived barriers and potential improvements from users and non-users of the system.
Results
Even with extensive registration efforts, less than 25 percent of clinicians and pharmacists acquired PDMP accounts over 2 years of operation. Rapid increases in registration and use in 2013 corresponded to new requirements among large pharmacy chains that pharmacists register for and use the PDMP. Among surveyed PDMP non-users, nearly half were unaware they could register. Among users and non-users, over two-thirds indicated that time constraints were a major barrier and over half thought inability to delegate access was a major barrier. Desired improvements included linking state systems, faster entry of pharmacy data, and use of unique patient identifiers. Users also wanted better insurance coverage for mental health and addiction referrals.
Discussion
Increasing registration and use of PDMPs remains important. Clinician feedback indicates that program enhancements and healthcare system changes would facilitate using and responding to PDMP information. It appears premature to judge the efficacy of PDMPs until best practices for their use are identified and impacts are assessed.
Prescription Drug Monitoring Programs (PDMPs) have been implemented or authorized in 49 states. These statewide databases typically capture information from all pharmacies in the state for prescriptions that are filled for controlled substances. The programs are widely seen as important tools for curbing the epidemic of prescription drug abuse that has emerged in the U.S., and the accompanying high rate of overdose deaths.1 Clinicians use these programs to help inform patient assessments and treatment options, coordinate care, and identify possible drug safety risks, misuse, abuse, or diversion.
Although California launched the earliest PDMP in 1939, most other states delayed until internet technology in the 1990s made systems more feasible. By 2002, there were still only 17 programs, and most have been implemented since then, thanks in part to funding support from the Department of Justice.1 Thus, most programs are relatively new, and their design and use are rapidly evolving. Some of these programs were implemented primarily with law enforcement in mind, but there is increasing interest in their use as clinical and public health tools.
Clinicians make wide use of these programs, but there is no evidence that defines who should use PDMPs. Not all providers prescribe controlled substances, so who should utilize these systems remains unclear. In a 2008–2009 multistate survey, an average of 53% of physicians were registered to use PDMPs.2 Program use varies by state, by clinical specialty, and by design and administrative location of the programs.2–4 However, most surveys of PDMP users have been small, limited to single specialties or academic practices, and constrained by low response rates.2, 4–7 Few surveys have systematically queried non-users of the PDMP about barriers, and few have examined the pace of uptake and use of newly implemented PDMP systems.
Our goals were to describe outreach efforts employed to encourage use of Oregon’s relatively new PDMP; examine the pace of registration and utilization of the program; identify barriers to registration and use; and identify system improvements that might enhance the value of such programs.
METHODS
Institutional Review Boards at Oregon Health and Science University and at the Oregon Health Authority’s Public Health Division approved this study. This was a mixed-methods study, utilizing program narrative reports, PDMP data, and a provider survey.
Description of Outreach Efforts
Data were summarized from biannual reports on the PDMP prepared by the PDMP coordinator (TB), and his personal knowledge.
Trend data
Oregon’s PDMP went online on September 1, 2011. We used publicly available data from Oregon’s PDMP to examine trends in registration to use the PDMP and numbers of queries to the system from its initiation through December 2013. These data are tracked by credential (physician, pharmacist, dentist, nurse practitioner, physician assistant, naturopathic physician) on a monthly basis.8
Survey data
Data on barriers to use and clinician recommendations for improvement were obtained from a statewide survey of prescribers in April, 2013. The detailed survey methodology has been described elsewhere,9 and is briefly summarized here.
Because the survey was focused on prescribing decisions, we sampled all Oregon clinicians, but did not include pharmacists. We used professional board registration databases to identify active clinicians, regardless of whether they were registered to use the PDMP. Data were obtained from the Boards of Medicine, Nursing, Dentistry, Naturopathy, and Optometry. These were matched with DEA registration files to assure that we sampled only professionals who were eligible to register for the PDMP.
In collaboration with the state Public Health Division, we used the PDMP over a 3-month period (December 2012 through February 2013) to identify three strata for sampling: frequent users (more than 1 query per month); infrequent users (1 or fewer queries per month, but at least 1 query to the database); and non-registrants. This dividing point was chosen because at that time, only 955 prescribers had queried 5 or more times over the 3-month interval, and we wanted to be confident of having an adequate pool for our target of 650 “frequent” users. Within each of the user strata, a random sample generator function within the Statistical Package for the Social Sciences (SPSS) software was used to randomly select the study sample.
Surveys were sent by mail to the random sample of prescribers in each stratum, with an option to complete an identical online survey. There were approximately 1,300 frequent users, 4,300 infrequent users, and 16,300 non-registrants at the time of the sample. Our goal was to sample 650 users in each of the frequent and infrequent user groups, and 2,000 non-registrants, anticipating a lower response rate among non-registrants. Because of invalid addresses, recent retirees, and a sampling error that inadvertently included a small number of pharmacists (subsequently excluded), the final valid number of requests were to 612 frequent users, 503 infrequent users, and 1,789 non-registrants.
RESULTS
Oregon Registration Efforts (Figure 1)
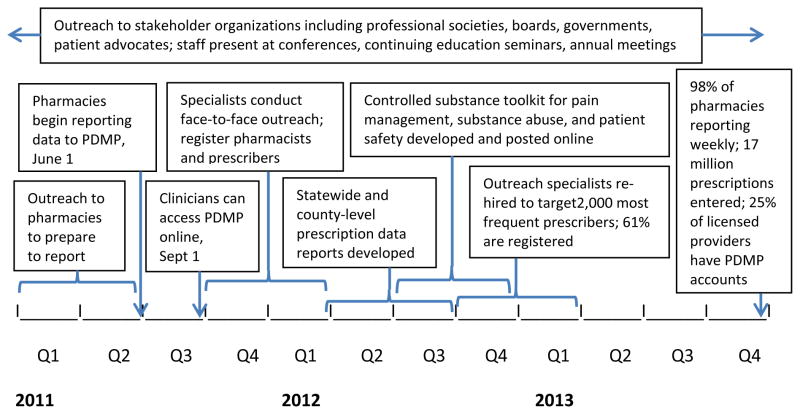
Figure 1.
Timeline of key events in implementing the Oregon Prescription Drug Monitoring Program
January-June, 2011
The Oregon Health Authority began outreach to pharmacies regarding reporting requirements. Administrative rules were adopted, and key stakeholders (pharmacies, professional boards, patient advocates, professional societies, and government) were engaged in planning implementation. Posters at pharmacies notified patients, and a website made information available to stakeholders and the public.
June 1, 2011
Pharmacies began reporting data to the Oregon PDMP. Outreach to prescribers began by stakeholders, including newsletters, websites, and listservs.
September 1, 2011
The PDMP went online, available to clinicians and pharmacists.
October–December 2011
Outreach specialists, hired full time but for limited 6-month intervals, worked with pharmacies to ensure compliance and conduct face-to-face meetings with prescribers and pharmacists to inform and to register system users. These specialists became notary publics to facilitate the notarization required for registration. By December, 90% of pharmacies were uploading data.
January –June 2012
New efficiencies were added to facilitate online registration. Face-to-face outreach by specialists concluded in March 2012, after more than 3,500 contacts with providers, pharmacists, and associated staff.
July–December 2012
By year’s end, over 98% of pharmacies had submitted data; 7 million prescriptions were entered in 2012. In September, three outreach workers were rehired, with a focus on enrolling the 2,000 most frequent prescribers of controlled substances, who wrote approximately 60 percent of prescriptions in the database. They also educated key clinic staff, who became champions of the PDMP and helped to register providers beyond the periods of targeted outreach. The program developed and posted a controlled substances “toolkit”, addressing substance abuse, mental health, pain management, and safety recommendations.10 Staff conducted targeted one-on-one outreach with providers and presented at conferences, seminars, and continuing education courses.
January–December, 2013
The three outreach specialists concluded their efforts, and 61 percent of the 2,000 most frequent prescribers were registered. By the end of December, almost 17 million prescription records had been uploaded into the system. Of the 830 Oregon-licensed pharmacies, 825 were in compliance with the statutory reporting requirement, and 98 percent were reporting weekly as required by law.
Trends in registration and use
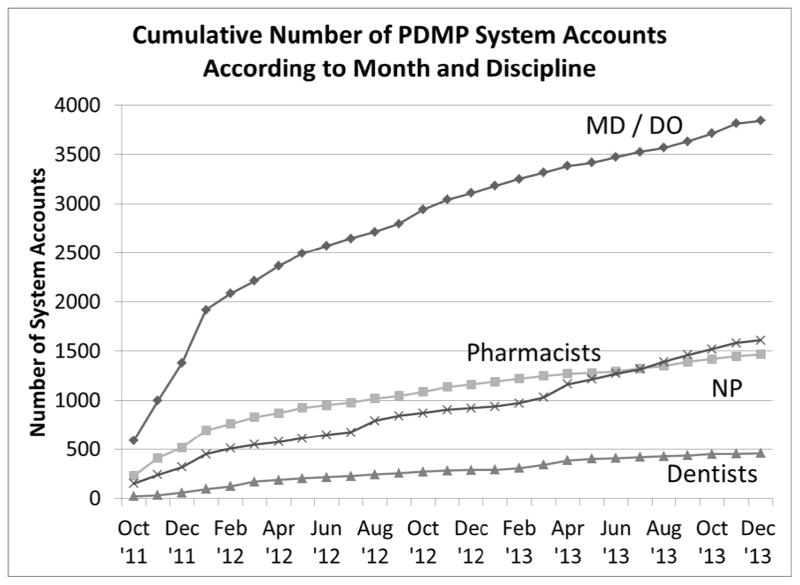
Registration of healthcare providers and pharmacists to use the PDMP increased rapidly during the first four months of operation (Figure 2). Physicians have been the largest group of registrants. By the end of 2012, PDMP staff had activated 5,547 system accounts; by the end of 2013, this number increased to 7,218 (25 percent of 29,000 licensed healthcare providers who can prescribe and licensed pharmacists who can dispense controlled substances).
Figure 2.
Cumulative Number of PDMP System Accounts According to Month and Discipline
Medical doctors comprised 45 percent of accounts, followed by pharmacists and nurses with 22 and 13 percent respectively. Of the 15,433 providers who prescribed at least one controlled substance in 2013, 5,582 (36%) had active PDMP accounts (Table 1). Doctors of osteopathy and prescribing nurses had the highest proportions registered, at 50%, followed by physician assistants and medical doctors (Table 1). Seventy-eight percent of the prescriptions listed in the database were written by a cohort of 4,000 prescribers. By the end of 2013, 59 percent of these prescribers had active system accounts, as opposed to 25% of all licensed prescribers.
Table 1.
Comparison of Oregon licensees who have PDMP accounts through 12/31/13 and who prescribed in 2013 by discipline
| Licensed Discipline | Number who prescribed at least one CS II-IV* in 2013 | Number with PDMP accounts by December, 2013 (% of those who prescribed any CS II-IV) | Estimated total number of licensees† |
|---|---|---|---|
| Nurse Practitioners | 1,887 | 945 (50.1) | 2,600 |
| Dentists | 2,409 | 506 (21.0) | 3,750 |
| Osteopathic physicians | 750 | 378 (50.4) | 875 |
| Medical Physicians (MD) | 8,822 | 3,201 (36.3) | 12,700 |
| Naturopathic physicians | 344 | 87 (25.3) | 850 |
| Physician Assistants | 1,136 | 457 (40.2) | 1,500 |
| Optometrists | 85 | 8 (9.4) | 750 |
| Totals | 15,433 | 5,582 (36.2) | 23,025 |
Controlled substance in FDA schedules II–IV
Estimates provided by individual professional licensing boards
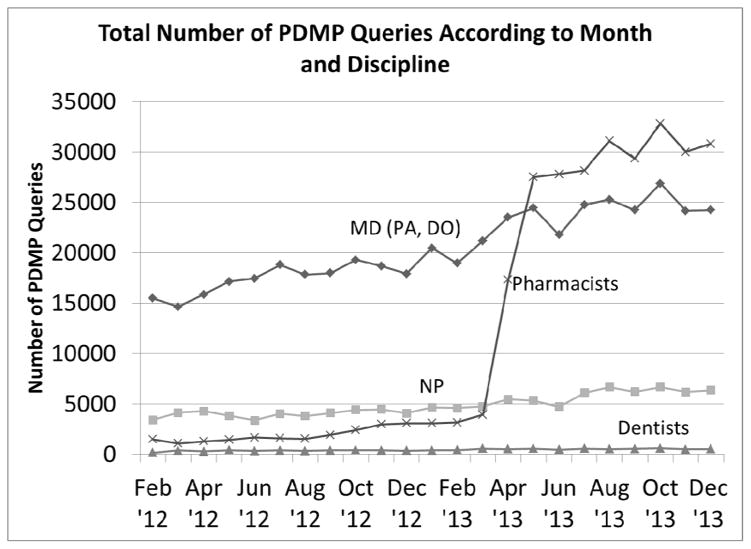
For 2013, health care providers and pharmacists conducted 621,570 system queries, more than double the number in 2012 (Figure 3). From 2012 to 2013, the average number of queries per system user (those with at least one query) increased from 14 to 16 per month. The increase in system queries in the second quarter of 2013 was driven by pharmacists’ use of the system. This followed a business policy change by two large pharmacy chains requiring their pharmacists to register and use the PDMP before dispensing specific controlled substances. Pharmacists from other large chains enrolled simultaneously as interest and knowledge about the system increased.
Figure 3.
Total Number of PDMP Queries According to Month and Discipline
The distribution of queries per user was highly skewed. For example, in calendar 2012, the mean number of queries (including registrants with no queries) was 81, but the median was just 7. In that year, just 74 prescribers accounted for 25% of all system queries, and 330 prescribers accounted for half of all queries.
Survey of barriers to use identified by clinicians
We received responses from 358 frequent users of the PDMP (59% response rate), from 261 infrequent users of the PDMP (52% response rate), and from 439 non-registrants (25% response rate). The age (overall 45% aged 50 or greater) and sex (51% male) of the survey respondents mirrored those of the matched professional board registry populations.
Medical and osteopathic physicians comprised the majority of survey respondents (590 respondents, 55.8% overall), followed by nurse practitioners (19.5%), dentists (12.4%), physician assistants (7.8%) and naturopathic physicians (1.0%). Optometrists and respondents with unreported credentials comprised the remainder. Among PDMP registrants, physicians were an even larger proportion (63.7%). Among PDMP users, considering both physicians and non-physicians, the most common specialties were primary care (family medicine and general internal medicine, 50.4%) and emergency medicine (15.3%).
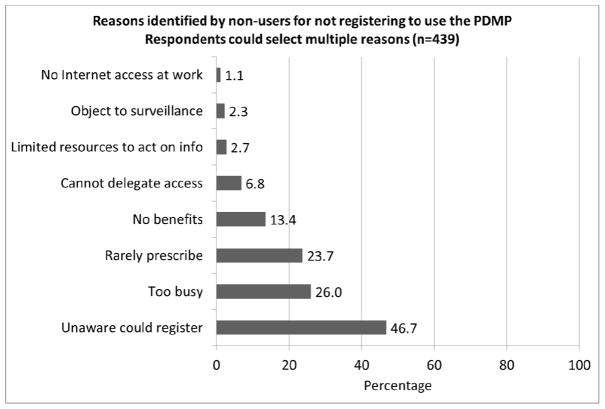
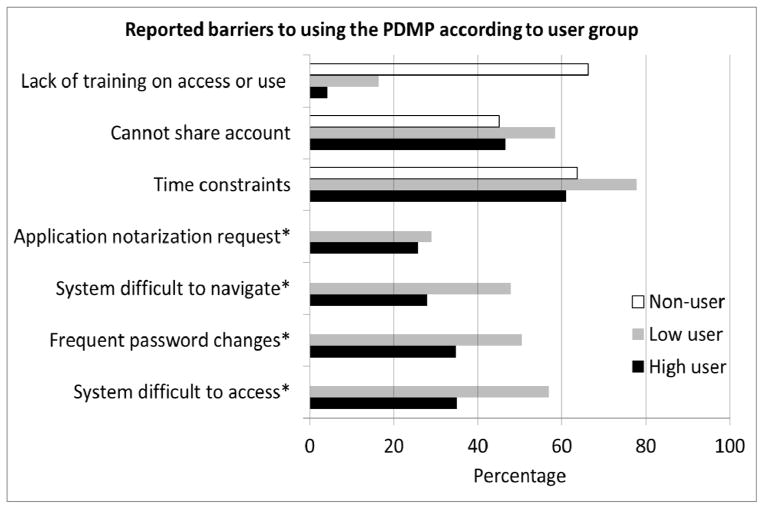
Clinicians who were not registered to use the PDMP were asked why they had not registered (Figure 4). The most common response (46.7%) was that they did not know they could register. Although 23.7% of non-registrants reported rarely prescribing (1 prescription per month), 63% prescribed controlled substances “occasionally” (1–5 prescriptions per week) or “frequently” (5 or more prescriptions per week). Prescribing of controlled substances was common among non-registrants who were unaware that they could register to use the PDMP. Among this group, 53.5% prescribed opioids at least weekly. Time constraints to accessing the PDMP during patient visits comprised the most frequently cited barrier to using the PDMP, endorsed by the majority of frequent users, infrequent users, and non-registrants (Figure 5). The clinician’s inability to delegate PDMP access to other medical staff was a barrier for roughly half of respondents (46.6% of frequent users, 58.4% of infrequent users, and 45.1% of non-registrants). The Oregon legislature has addressed this with a new law that went into effect January 1, 2014, allowing registered PDMP users to authorize staff members (e.g., nurse’s assistant) to check the PDMP on their behalf.
Figure 4.
Reasons identified by non-registrants for not registering to use the PDMP. Respondents could select multiple reasons (n=439)
Figure 5.
Reported barriers to using the PDMP according to user group.
Two-thirds of non-users cited a lack of training on accessing and using the PDMP as a barrier, but this was not a barrier for registered users. Nearly half (45.4%) of non-users cited a cumbersome registration process, and 8.6% cited discomfort using a computer or the Internet as a barrier to using the PDMP.
Among registered users, difficulty accessing the PDMP and frequent password changes were cited as barriers by more infrequent users than frequent users (56.9% vs. 35.1% and 50.4% vs. 34.8%, respectively). Difficult navigation was a barrier for 47.8% of infrequent users and 28.0% of frequent users. Relatively few respondents reported that scrutiny by law enforcement or licensing boards was a concern: less than 5% of frequent users, and about 10% of non-users. Oregon’s PDMP is not accessible to law enforcement without a court order based upon probable cause, and regulatory boards may only request information on a licensee as part of an active investigation.
Clinician recommendations for system improvements
All survey respondents were asked what would make the PDMP easier to use. Registered users most often cited proactive alerts: having the state send reports automatically when a prescription pattern suggests potential misuse or diversion (56% of frequent users; 66% of infrequent users).
Additionally, registered users were asked what would make the PDMP more useful in clinical practice. Linking multiple state PDMP systems was endorsed by 97.3% of registered users. Faster availability of prescription data was favored by 88.7% of users. This varied somewhat by specialty: 80% of internal medicine subspecialty physicians indicated it would be “somewhat” or “very” useful, versus 87% among primary care physicians, and 94% among emergency medicine or pain specialists. Currently, pharmacies are required to report filled prescriptions to the Oregon PDMP within 7 days. Eighty-six percent of users endorsed better insurance coverage for mental health or addiction referrals, suggesting a common obstacle to effectively responding to PDMP data. Almost 81% endorsed the development of a unique patient identifier to reduce mistaken identity or use of aliases.
DISCUSSION
Even with extensive efforts to facilitate registration and use of the PDMP, we found that some clinicians have been slow to register. On the other hand, rapid increases in registration can be attributed to early adopters and clinical use policies. Some clinicians are unaware of these systems, while a majority of others cite time constraints as a barrier to access and use PDMPs. Users recommended increased system functionality, especially in linking multiple state systems, faster entry of pharmacy data, and unique patient identifiers. These recommendations need further investigation and discussion; they should be assessed for clinical value and community impact.
The use of targeted outreach workers to enhance PDMP registration appears to have been worthwhile, given the higher PDMP registration rate among the targeted high prescribers than among others. We cannot know if this difference would have occurred without the outreach workers, but their efforts extended to training other PDMP champions, as well.
The impact of pharmacy chain policies on PDMP use was substantial, and suggests the power of administrative mandates. How this change affected prescribing clinicians is not yet clear, but other studies have described important communication between pharmacists and clinicians regarding PDMP findings.11 Some states have mandated use of the PDMP in certain circumstances or by certain prescribers (eg emergency physicians), and some have mandated registration by all prescribers.1 Though the impact of these mandates is not yet well-studied, our findings suggest they are likely to increase PDMP use.
In most states, PDMPs are relatively new, and did not exist when many clinicians completed their training. Thus, it may not be surprising that substantial numbers remain unaware of such programs or are unfamiliar with how to use them. Furthermore, these systems have not yet been integrated into the workflow of most clinicians, for example, into electronic medical record systems. Many technical issues need to be addressed before such integration can occur, particularly in maintaining data security and protecting the privacy of individuals’ personal health information.
Finally, our survey suggests that even if clinicians access PDMP data, barriers such as limited insurance coverage may impede constructive mental health and addiction screening, assessment, and referrals. Such factors suggest a need for comprehensive outreach, education and training for clinicians and a consideration of possible health system changes.
The data also point to the need for making PDMP systems easier to use. Primary care clinicians manage the largest fraction of patients with chronic pain,12 and they represented the largest specialty group among PDMP users in our survey. These clinicians often face 10 to 15 minute patient appointments, and 2 or 3 minutes spent accessing PDMP information is a substantial fraction of that time. Easier login and navigation of PDMP systems; integration into electronic health records; delegated access for medical staff; and systematic notification of prescribers when a patient exceeds a prescription threshold would help alleviate time constraints. Some of these issues can be addressed with simple system interface changes, but others require significant technological development, pose security and privacy issues, or involve statutory changes.
Better cross-state access to PDMP data was favored by an overwhelming majority of survey respondents. Oregon’s largest urban center, Portland, is located right on the Washington state border. By statute, Oregon is allowed to share PDMP data with other states only if the confidentiality, security and privacy standards are equivalent. To date, this has not allowed data sharing. However, as of 2014, Washington, Idaho, and California providers can apply for an Oregon PDMP account.
Our findings are consistent with reports from other surveys. A survey in Rhode Island and Connecticut found that many non-users were unaware of the PDMP system.5 A survey of physician members of the American College of Toxicology reported that time constraints were the most common reason for not checking the PDMP on every patient receiving a prescription for controlled substances.7 The latter survey also reported system access and navigation as barriers, and almost 50% of respondents called for simplified login procedures. Reducing the lag time in prescription data entry was also a high priority among respondents in that survey, 78% of whom practiced emergency medicine.
Our study has the advantages of drawing on complete statewide PDMP registration and query data, and a statewide survey that sampled all prescribers, regardless of credential or specialty. Our response rate among PDMP users was 52–59%, compared to 29.6% in an earlier survey,5 though our response among PDMP nonusers was lower. Response rates to large sample physician surveys in general have averaged 52–54%.13,14 The lower response rate among nonusers – despite the demographic similarity of respondents to the full board registries - creates the potential for bias if respondents and non-respondents differ in reasons for not registering or in perceived barriers.
There are some other important limitations. Our data are from a single state, and may not be typical of states that have substantially different PDMP system designs, operational standards and processes, and outcome objectives. As in all surveys, many factors, including social desirability, influence responses.
While our data indicate healthcare providers’ perceived utility of these systems, the efficacy of PDMPs has not been thoroughly evaluated.15,16 For the goal of improving patient health, we need to determine best practices related to the use of these systems. Who should use PDMPs? What clinical indicators should prompt their use? How can the information be used to inform patient assessments and treatment?
Beyond maximizing registration and use of these systems, more in-depth study should be done to determine their impact. What benefits may accrue to patients? What patient health outcomes and community health outcomes should be the focus of evaluating PDMPs’ efficacy? Are there unintended consequences related to clinical practice or patient outcomes? How does the use of PDMPs affect the health and safety of communities? It appears premature to judge the efficacy of PDMPs until best practices for their use are identified and impacts are assessed.
Acknowledgments
Supported by the National Institutes of Health, National Institute for Drug Abuse through Grant # 1 R01 DA031208-01A1 and by the National Center for Research Resources and the National Center for Advancing Translational Sciences, through grant UL1RR024140.
Footnotes
The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the participating institutions.
References
- 1.Deyo RA, Irvine J, Millet L, Beran T, O’Kane N, Wright D, McCarty D. Measures such as interstate cooperation would improve the efficacy of programs to track controlled drug prescriptions. Health Affairs. 2013 Mar;32(3):603–613. doi: 10.1377/hlthaff.2012.0945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fleming ML, Chandwani H, Barner JC, Weber SN, Okoro TT. Prescribers and pharmacists requests for prescription monitoring program (PMP) data: does PMP structure matter? J Pain Palliat Care Pharmacother. 2013;27:136–42. doi: 10.3109/15360288.2013.788598. [DOI] [PubMed] [Google Scholar]
- 3.Perrone J, Nelson LS. Medication reconciliation for controlled substances – an “ideal” prescription-drug monitoring program. N Engl J Me. 366(25):2341–2343. doi: 10.1056/NEJMp1204493. [DOI] [PubMed] [Google Scholar]
- 4.Feldman L, Williams KS, Coates J, Knox M. Awareness and utilization of a prescription monitoring program among physicians. J Pain Palliat Care Pharmacother. 2011;25:313–317. doi: 10.3109/15360288.2011.606292. [DOI] [PubMed] [Google Scholar]
- 5.Green TC, Mann MR, Bowman SE, et al. How does use of a prescription monitoring program change medical practice? Pain Med. 2012;13:1314–1323. doi: 10.1111/j.1526-4637.2012.01452.x. [DOI] [PubMed] [Google Scholar]
- 6.Feldman L, Williams KS, Knox, Coates J. Influencing controlled substance prescribing: attending and resident physician use of a state prescription monitoring program. Pain Med. 2012;13:908–914. doi: 10.1111/j.1526-4637.2012.01412.x. [DOI] [PubMed] [Google Scholar]
- 7.Perrone J, DeRoos FJ, Nelson LS. Prescribing practices, knowledge, and use of prescription drug monitoring programs (PDMP) by a national sample of medical toxicologists, 2012. J Med Toxicol. 2012;8:341–352. doi: 10.1007/s13181-012-0250-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. [accessed October 25, 2013];Oregon PDMP home, reports. http://www.orpdmp.com/monthly-reports.html.
- 9.Irvine JM, Hallvik SE, Hildebran C, Marino M, Beran T, Deyo RA. Who uses a prescription Drug Monitoring Program and how/Insights from a statewide survey of Oregon clinicians. J Pain. 2014;15:747–755. doi: 10.1016/j.jpain.2014.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. [accessed 10/25/13]; The toolkit and links to resources can be found at http://www.orpdmp.com/health-care-provider-resources.html.
- 11.Hildebran C, Cohen DJ, Irvine JM, Foley C, O’Kane N, Beran T, Deyo RA. How clinicians use prescription drug monitoring programs: a qualitative inquiry. Pain Med. 2014 May 16; doi: 10.1111/pme.12469. epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Breuer B, Cruciani R, Portenoy RK. Pain management by primary care physicians, pain physicians, chiropractors, and acupuncturists: a national survey. South Med J. 2010;103:738–747. doi: 10.1097/SMJ.0b013e3181e74ede. [DOI] [PubMed] [Google Scholar]
- 13.Asch DA, Jedrziewski MK, Christakis NA. Response rates to mail surveys published in medical journals. J Clin Epidemiol. 1997;50:1129–1136. doi: 10.1016/s0895-4356(97)00126-1. [DOI] [PubMed] [Google Scholar]
- 14.Cummings SM, Savitz LA, Konrad TR. Reported response rates to mailed physician questionnaires. Health Serv Res. 2001;35:1347–1355. [PMC free article] [PubMed] [Google Scholar]
- 15.Government Accountability Office. Prescription drugs: state monitoring programs provide useful tool to reduce diversion [Internet] Washington (DC): GAO; 2002. May, [cited 2013 Jan 17]. (Report No. GAO-02-634). Available from: http://www.gao.gov/new.items/d02634.pdf. [Google Scholar]
- 16.Paulozzi LJ, Kilbourne EM, Desai HA. Prescription drug monitoring programs and death rates from drug overdose. Pain Med. 2011;12:747–54. doi: 10.1111/j.1526-4637.2011.01062.x. [DOI] [PubMed] [Google Scholar]