Abstract
Mucosal tissues contain large numbers of memory CD4+ T cells that, through T-cell receptor-dependent interactions with antigen-presenting cells, are believed to have a key role in barrier defense and maintenance of tissue integrity. Here we identify a major subset of memory CD4+ T cells at barrier surfaces that coexpress interleukin-18 receptor alpha (IL-18Rα) and death receptor-3 (DR3), and display innate lymphocyte functionality. The cytokines IL-15 or the DR3 ligand tumor necrosis factor (TNF)-like cytokine 1A (TL1a) induced memory IL-18Rα+DR3+CD4+ T cells to produce interferon-γ, TNF-α, IL-6, IL-5, IL-13, granulocyte–macrophage colony-stimulating factor (GM-CSF), and IL-22 in the presence of IL-12/IL-18. TL1a synergized with IL-15 to enhance this response, while suppressing IL-15-induced IL-10 production. TL1a- and IL-15-mediated cytokine induction required the presence of IL-18, whereas induction of IL-5, IL-13, GM-CSF, and IL-22 was IL-12 independent. IL-18Rα+DR3+CD4+ T cells with similar functionality were present in human skin, nasal polyps, and, in particular, the intestine, where in chronic inflammation they localized with IL-18-producing cells in lymphoid aggregates. Collectively, these results suggest that human memory IL-18Rα+DR3+ CD4+ T cells may contribute to antigen-independent innate responses at barrier surfaces.
Introduction
Body surfaces including mucosal tissues and the skin are continually exposed to challenges from the external environment, including resident commensal microorganisms as well as a multitude of bacterial and viral pathogens that use these tissues as portals of entry and infection.1, 2, 3 Maintenance of barrier tissue homeostasis is critically dependent on the immune system's ability to respond appropriately to such challenges, a breakdown in which can lead to chronic inflammatory diseases including inflammatory bowel disease, asthma, and allergy.4, 5, 6
Barrier tissues contain numerous subsets of innate and adaptive immune cells that together contribute to maintain tissue homeostasis, and also, when poorly controlled, to detrimental inflammatory reactions. Adaptive immune responses at barrier surfaces take several days to weeks to develop as naive CD4+ T-cell scan antigen-presenting cells (APCs) in tissue draining lymph nodes in search of their cognate antigen, clonally expand, and subsequently migrate as effector CD4+ T cells to lymphoid follicles, providing help to B cells, or via the circulation into peripheral tissues. Having entered barrier tissues, activated CD4+ T cells can persist for long periods of time as tissue-resident memory populations,7 where they, through the production of proinflammatory and regulatory cytokines, have key roles in regulating local immunity. The activity of tissue-resident memory CD4+ T cell is primarily believed to be regulated through T-cell receptor (TCR)-dependent recognition of cognate antigen-major histocompatibility complex (MHC)-II on local APCs,8, 9 however memory CD4+ T cells can produce cytokines independently of TCR activation. For example, IL-12 and IL-18 have been shown to induce TCR-independent interferon-γ (IFN-γ) production in CD4+ T cells10, 11 and addition of either IL-1510 or the tumor necrosis factor (TNF) family member, TNF-like cytokine 1A (TL1a)/TNF super family member 15, can enhance this response.11, 12, 13 Whether IL-15 and TL1a can synergize to induce cytokine production by CD4+ T cells, the identity of such cytokine-responsive CD4+ T cells, and their potential presence at human barrier tissues remains however unclear.
Here we identify interleukin-18 receptor alpha-positive (IL-18Rα+) death receptor-3 (DR3)+CD4+ T cells as a major population of human memory CD4+ T cells with innate lymphocyte functionality. Among memory CD4+ T cells, IL-18Rα+DR3+CD4+ T cells alone produced a wide range of cytokines in response to IL-12/IL-18/IL-15 or IL-12/IL-18/TL1a, and this response was significantly enhanced after the addition of both TL1a and IL-15. We further demonstrate that IL-18Rα+DR3+CD4+ T cells with similar functionality are present in large numbers in barrier tissues, in particular in the intestinal mucosa, where they represented the majority of tissue-resident CD4+ T cells. Taken together, our results highlight a hitherto underappreciated innate activity of memory CD4+ T cells in barrier tissues.
Results
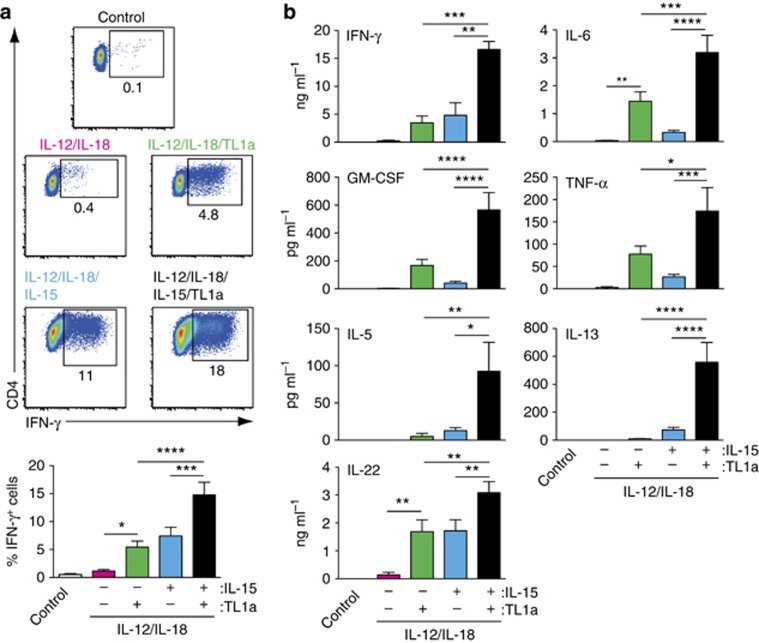
TL1a and IL-15 synergize to induce proinflammatory cytokine production in peripheral blood CD45RO+CD4+ T cells
To assess the impact of TL1a and IL-15 in regulating proinflammatory cytokine production in memory CD4+ T cells, CD45RO+CD4+ T cells were purified from peripheral blood (PB) of healthy donors and cultured with IL-12/IL-18 together with IL-15, TL1a, or IL-15 and TL1a (Figure 1). Consistent with previous results,10, 11 TL1a or IL-15 induced IFN-γ production in CD45RO+CD4+ T cells in the presence of IL-12/IL-18 (Figure 1a, b and Supplementary Figure S1A online). To determine whether TL1a and IL-15 synergize to promote IFN-γ responses, CD45RO+CD4+ T cells were incubated with optimal concentrations of TL1a (100 ng ml−1) together with IL-15 (25 ng ml−1) in the presence of IL-12/IL-18 (Figure 1a, b). Addition of both TL1a and IL-15 induced a twofold increase in the percentage of IFN-γ+ cells and a threefold increase in IFN-γ secretion compared with either cytokine alone (Figure 1a, b). TL1a induces the production of several proinflammatory cytokines in IL-12/IL-18-stimulated CD4+ T cells including GM-CSF, TNF-α, IL-6, and IL-13.13 We thus assessed whether IL-15 enhanced production of cytokines other than IFN-γ in the presence of IL-12/IL-18 and whether TL1a and IL-15 synergized to promote expression of these cytokines (Figure 1b). In IL-12/IL-18 cultures, both TL1a and IL-15 dose dependently induced IL-6, TNF-α, GM-CSF, IL-5, IL-13, and IL-22 expression in CD45RO+CD4+ T cells (Supplementary Figure S1B) and addition of IL-15 (25 ng ml−1) together with optimal concentrations of TL1a (100 ng ml−1) induced a marked increase in all cytokines (Figure 1b). To confirm that cytokine production by CD45RO+CD4+ T cells occurred independently of cognate TCR–MHC-II interactions, similar experiments were performed in the presence of neutralizing MHC-II antibody (Supplementary Figure S2). Addition of neutralizing MHC-II antibody had no effect on cytokine induced cytokine production by CD45RO+CD4+ T cells (Supplementary Figure S2A), despite its ability to inhibit cell proliferation in a mixed lymphocyte reaction (Supplementary Figure S2B). Previous studies have shown that IL-12/IL-1814, 15 and IL-12/IL-18/IL-15, but not anti-CD3-mediated induction of IFN-γ is p38 mitogen-activated protein kinase dependent,10, 14, 15 and we found that TL1a- and IL-15-induced proinflammatory cytokine production was p38 mitogen-activated protein kinase and phosphoinositide 3-kinase dependent (Supplementary Figure S2C). Collectively, these results indicate a marked synergy between TL1a and IL-15 in promoting proinflammatory cytokine production in CD45RO+CD4+ T cells in the presence of IL-12/IL-18.
Figure 1.
Tumor necrosis factor-like cytokine 1A (TL1a) and interleukin-15 (IL-15) synergize to induce proinflammatory cytokine production in peripheral blood CD45RO+CD4+ T cells. Peripheral blood CD45RO+CD4+ T cells (1 × 106 cells ml−1, 200 μl per well) were cultured in medium alone (control) or with IL-12 (2 ng ml−1), IL-18 (50 ng ml−1), IL-15 (25 ng ml−1), and TL1a (100 ng ml−1) as indicated. (a) Representative intracellular staining (top) and percent (bottom row) of CD4+ T cells expressing interferon-γ (IFN-γ) 4 days after incubation with indicated cytokines or medium alone (control). Results are the mean (s.e.m.) of 10 biological replicates. Cells were pregated on live single cells. (b) Cytokine levels in culture supernatants were assessed after 1 day (IFN-γ) and 4 days (other cytokines). Results are the mean (s.e.m.) of 4 (IFN-γ), 6 (IL-22), or 13 (other cytokines) biological replicates.
TL1a modulates cytokine expression through DR3
To determine whether the TL1a-mediated induction of proinflammatory cytokines in CD4+ T cells was dependent on DR3, CD45RO+CD4+ T cells were stimulated with IL-12/IL-18/IL-15 in the presence/absence of TL1a together with a neutralizing DR3 Fab′ or control Fab′ fragment (Supplementary Figure S3). Addition of neutralizing DR3 Fab′, but not control Fab′, inhibited TL1a-mediated upregulation of all proinflammatory cytokines, indicating that the proinflammatory effects of TL1a on CD45RO+CD4+ T cells are mediated through DR3.
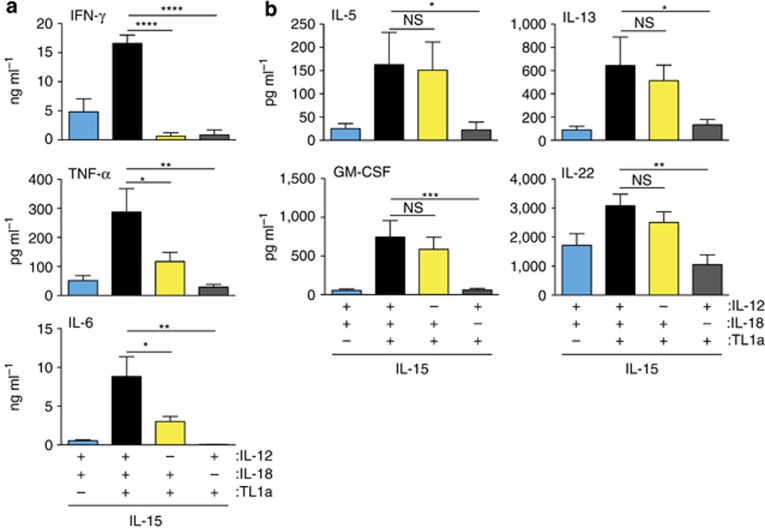
IL-15 and TL1a induction of proinflammatory cytokines requires synergy with IL-18
To assess the role of IL-12 and IL-18 in TL1a/IL-15-induced proinflammatory cytokine production, CD45RO+CD4+ T cells were stimulated with IL-15 and TL1a in the presence/absence of IL-12 or IL-18 (Figure 2). Removal of IL-12 from the cytokine cocktail prevented IL-15/TL1a-induced IFN-γ production and reduced IL-15/TL1a-induced TNF-α and IL-6 production (Figure 2a). However, IL-12 was not required for TL1a/IL-15-mediated induction of IL-5, IL-13, IL-22, and GM-CSF (Figure 2b). In contrast, the ability of TL1a/IL-15 to induce all cytokines was markedly reduced in the absence of IL-18 (Figure 2b). Collectively, these results suggest that IL-18 is required for TL1a/IL-15-driven proinflammatory cytokine production in CD45RO+CD4+ T cells.
Figure 2.
Interleukin-15 (IL-15) and tumor necrosis factor-like cytokine 1A (TL1a) induction of proinflammatory cytokines in CD45RO+CD4+ T cells requires synergy with IL-18. Peripheral blood CD45RO+CD4+ T cells (1 × 106 cells per ml, 200 μl per well) were cultured with IL-12 (2 ng ml−1), IL-18 (50 ng ml−1), IL-15 (25 ng ml−1), and TL1a (100 ng ml−1) as indicated, and cytokine levels were determined in culture supernatants at day 1 (interferon-γ (IFN-γ)) or day 4 (other cytokines). (a) TL1a and IL-15 synergy in inducing IFN-γ, IL-6, and TNF-α requires both IL-12 and IL-18. Results are the mean (s.e.m.) of 4 (IFN-γ) and 9 (IL-6 and TNF-α) biological replicates. (b) TL1a and IL-15 synergy in inducing GM-CSF, IL-5, IL-13, and IL-22 is IL-12 independent and IL-18 dependent. Results are the mean (s.e.m.) of 6 (IL-22) or 9 (other cytokines) biological replicates.
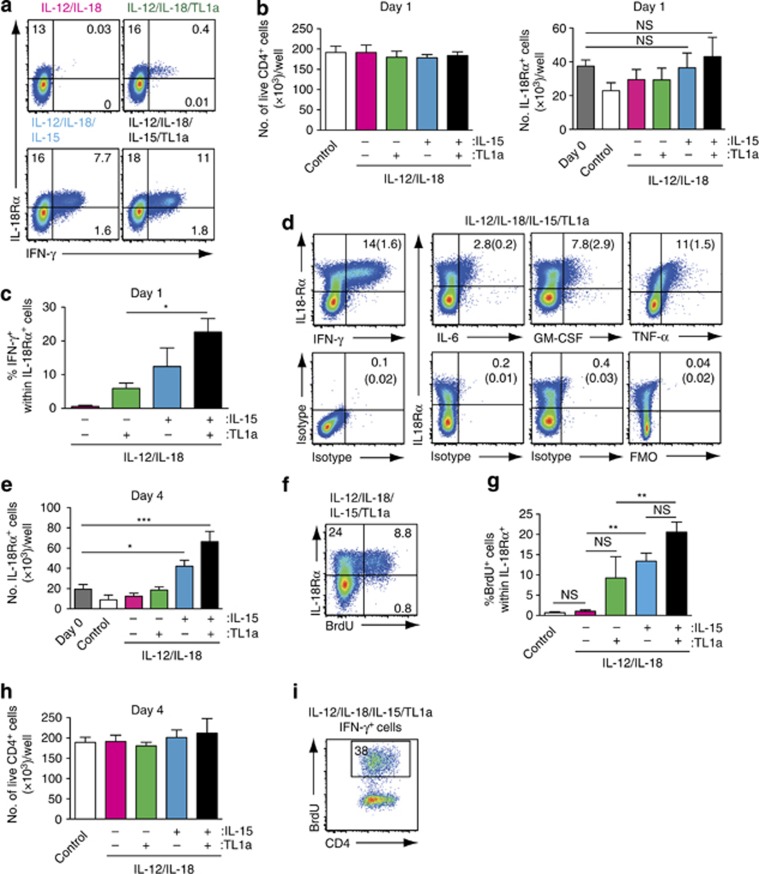
IL-15 and TL1a synergize to induce IFN-γ production in IL-18Rα+ CD45RO+CD4+ T cells
A subset of T cells expressing the C-type lectin membrane glycoprotein and natural killer cell-associated marker CD161 were recently suggested to be the major TL1a-responsive CD4+ T-cell subset in PB.12, 13 Conversely, a subset of memory CD4+ T cells expressing IL-18Rα was shown to be the primary IFN-γ-secreting population after stimulation with IL-15.10 We thus assessed the phenotype of cytokine-producing CD45RO+CD4+ T cells after culture with the different cytokine cocktails (Figure 3). In one day cultures containing IL-12 and IL-18, IL-15 and TL1a alone or in combination induced IFN-γ production in a minor subset of PB CD45RO+CD4+ T cells that coexpressed IL-18Rα (Figure 3a), consistent with the IL-18 dependency of this response (Figure 2a). While the total number of CD4+ T cells and IL-18Rα+ CD4+ T cells in the wells did not change at this time point (Figure 3b), addition of both IL-15 and TL1a to IL-12/IL-18 cultures enhanced the proportion of IFN-γ-producing IL-18Rα+CD4+ T cells compared with either cytokine alone (Figure 3a, c). Taken together, these results indicate that TL1a and IL-15 in the presence of IL-12/IL-18 rapidly induce IFN-γ production in IL-18Rα+CD45RO+CD4+ T cells and that both cytokines synergize to promote this response.
Figure 3.
Tumor necrosis factor (TNF)-like cytokine 1A (TL1a) and interleukin-15 (IL-15) synergize to induce proliferation of IL-18Rα+ CD4+ T cells in IL-12/IL-18 cultures. Peripheral blood CD45RO+CD4+ T cells (1 × 106 cells ml−1, 200 μl per well) were cultured in medium alone (control) or with IL-12 (2 ng ml−1), IL-18 (50 ng ml−1), IL-15 (25 ng ml−1), and TL1a (100 ng ml−1) as indicated. Representative flow cytometry plots depicting interferon-γ (IFN-γ) expression by IL-18Rα+CD4+ T cells (a), total number of live CD4+ cells (left) and total number of live CD4+IL-18Rα+ cells (right) (b) and percent of IFN-γ+ cells within the IL-18Rα+CD4+ T cell population (c) after one day of culture. Results are mean (s.e.m.) from 4 biological replicates. (d) Representative flow cytometry plots showing IFN-γ-, TNF-α-, IL-6-, and granulocyte–macrophage colony-stimulating factor (GM-CSF)-expressing CD4+ T cells (top row) and isotype controls (IFN-γ, IL-6, and GM-CSF) and fluorescence minus one (FMO) (TNF-α) (lower row) as assessed by intracellular cytokine staining after 4 days of culture with the indicated cytokine cocktail. Brefeldin A was added to the cultures 4 h before analysis of TNF-α, IL-6, and GM-CSF, whereas cultures for IFN-γ analysis were left untreated. Numbers in quadrants represent the mean (s.e.m.) from 3 biological replicates. (e) Number of IL-18Rα+CD4+ T cells at day 0 and after 4 days of culture with the indicated cytokines. Results are mean (s.e.m.) of 6 biological replicates. (f and g) IL-15 and TL1a induce selective proliferation of IL-18Rα+ cells. 5-Bromodeoxyuridine (BrdU) was added at the start of the culture and incorporation assessed 4 days later by flow cytometry. (f) Representative flow cytometry plot and (g) percent BrdU+ cells within the IL-18Rα+ CD4+ population after incubation with the indicated cytokine cocktails or medium alone (control). Results are the mean (s.e.m.) of 6 biological replicates. (h) Total number of live memory CD4+ T cells after 4 days of culture. Results are mean (s.e.m.) of 5 biological replicates. (i) Representative flow cytometry plot assessing BrdU incorporation in IFN-γ+CD4+ T cells after 4 days of culture with the indicated cytokine cocktail. Results are representative of 3 biological replicates.
TL1a and IL-15 synergize to induce proliferation of IL-18Rα+ CD4+ T cells
IL-18Rα+ T cells were also the major proinflammatory cytokine producers in 4 day cultures (Figure 3d). However, in contrast to 1 day cultures, by 4 days the total number of IL-18Rα+ T cells in IL-12/IL-18 cultures containing IL-15 or TL1a had increased, and the numbers were further enhanced in IL-12/IL-18 cultures containing both TL1a and IL-15 (Figure 3e). To assess whether the increased number of IL-18Rα+ cells in 4 day cultures could in part be explained by selective proliferation of these cells, 5-bromodeoxyuridine (BrdU) was added at the start of the culture and the percentage and phenotype of BrdU+ cells were assessed after 4 days by flow cytometry (Figure 3f, g). Only IL-18Rα+CD4+ T cells incorporated BrdU under all cytokine conditions (Figure 3f, data not shown); however, the total percentage of CD4+ T cells that incorporated BrdU was low, consistent with the observation that total CD4+ T-cell counts did not differ significantly between the culture conditions (Figure 3h). The proportion of IL-18Rα+CD4+ T cells that were BrdU+ increased after the addition of TL1a or IL-15 to IL-12/IL-18 cultures, although the former did not reach statistical significance (Figure 3g), and this was further increased after the addition of both TL1a and IL-15 (Figure 3g). Proliferation was not, however, required for cytokine-induced IFN-γ production (Figure 3i).
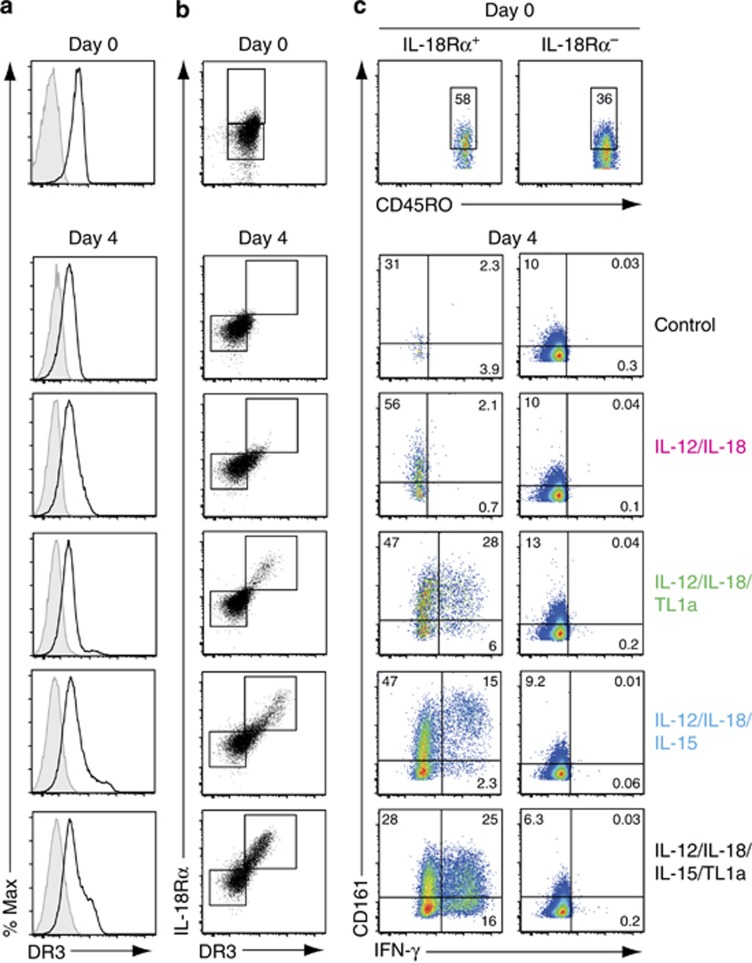
IL-18Rα+CD45RO+CD4+ T cells express high level of the TL1a receptor DR3 in cytokine cultures
Having identified IL-18Rα-expressing cells as the major cytokine-responsive CD45RO+CD4+ T-cell subset, we next assessed the expression of DR3 and CD161 on these cells (Figure 4). DR3 expression was assessed by staining cells with either a fluorescently labeled anti-DR3 Fab′ or a polyclonal DR3 antibody (Supplementary Figure S4), and gave similar results. The expression of IL-18Rα correlated with high expression of DR3 under all cytokine culture conditions (Figure 4a, b). While a large proportion of IL-18Rα+DR3hiCD4+ memory T cells also expressed CD161, both CD161+ and CD161−IL-18Rα+DR3hi cells produced IFN-γ (Figure 4c). Moreover, a subset of IL-18Rα−DR3lo cells expressed low levels of CD161 and these cells failed to produce IFN-γ (Figure 4b). Overall, these data suggest that CD161 expression is not a reliable marker for TL1a-responsive CD4+ T cells, but that this property is restricted to a subset of CD45RO+ IL-18Rα+CD4+ T cells that express high levels of DR3.
Figure 4.
The tumor necrosis factor-like cytokine 1A (TL1a) receptor death receptor 3 (DR3) is expressed at high levels on interleukin-18 receptor alpha (IL-18Rα)+CD45RO+CD4+ T cells in cytokine cultures. (a–c) DR3, IL-18Rα, CD161, and interferon-γ (IFN-γ) expression was assessed on peripheral blood CD45RO+CD4+ T cells by flow cytometry at day 0 or day 4 after culture (1 × 106 cells ml−1, 200 μl per well) with interleukin-12 (IL-12) (2 ng ml−1), IL-18 (50 ng ml−1), IL-15 (25 ng ml−1), and TL1a (100 ng ml−1) or medium alone (control). (a) Representative plots showing DR3 expression (black line, unfilled histogram) or fluorescence minus one (FMO) control (shaded histogram) on CD45RO+CD4+ T cells. (b) DR3 and IL-18Rα expression on CD45RO+CD4+ T cells. Boxes within plots are gates defining IL-18Rα+ or IL-18Rα− (day 0) and IL-18Rα+DR3hi or IL-18Rα−DR3lo (day 4) CD4+ T cells. (c) IFN-γ and CD161 expression on IL-18Rα+DR3hi or IL-18Rα−DR3lo CD4+ T cells as defined in b. Quadrants are set based on isotype control (IFN-γ) and FMO control (CD161) staining of IL-18Rα+DR3hi and IL-18Rα−DR3lo CD4+ T cells under each of the cytokine culture conditions. Results are representative of 3 (day 0) or 7 (day 4) biological replicates.
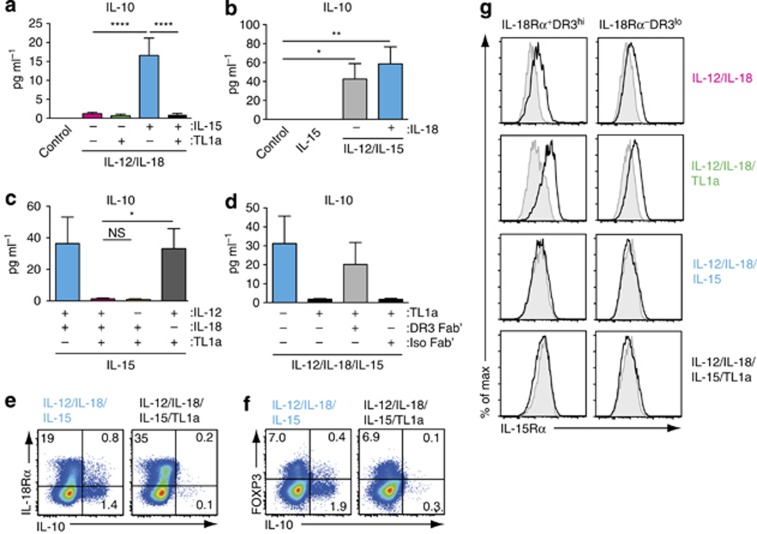
TL1a inhibits IL-15-mediated induction of IL-10 in CD45RO+CD4+ T cells
In addition to proinflammatory cytokines, we measured IL-10 levels in the CD45RO+CD4+ T-cell cultures (Figure 5). In marked contrast to proinflammatory cytokine induction, IL-15, but not TL1a, dose dependently induced IL-10 production in IL-12/IL-18 cultures (Supplementary Figure S5 and Figure 5a). IL-15 induction of IL-10 was dependent on the presence of IL-12 but not IL-18 in the cultures (Figure 5a, b). Further, rather than synergize with IL-15, addition of TL1a to IL-12/IL-18/IL-15 cultures inhibited IL-15-induced IL-10 production (Figure 5a). The ability of TL1a to inhibit IL-15-mediated induction of IL-10 was dependent on IL-18 and DR3 (Figure 5c, d). Staining for IL-10 demonstrated that IL-15-induced IL-10 production in both IL-18Rα+ and IL-18Rα−CD4+ T cells (Figure 5e), and that IL-10-producing cells were primarily FoxP3− T cells (Figure 5f). Further TL1a inhibited IL-10 production in both IL-18Rα+ and IL-18Rα−CD4+ T cells (Figure 5e). Prior studies have suggested that functional IL-15Rα is expressed by both IL-18Rα+ and IL-18Rα− memory CD4+ T cells.10 We thus assessed IL-15Rα expression on IL-18Rα+ and IL-18Rα−CD4+ T cells under the various culture conditions (Figure 5g). IL-15Rα was expressed by IL-18Rα+ and IL-18Rα−CD4+ cells in both IL-12/IL-18 and IL-12/IL-18/TL1a cultures. In contrast, IL-15Rα was not detected on either population of cells in cultures containing IL-15, presumably as a result of ligand-mediated receptor internalization,16 providing further evidence that both IL-18Rα+ and IL-18Rα−CD4+ cells are responsive to IL-15. Collectively, these results indicate that TL1a functions through IL-18Rα+DR3+CD4+ T cells to suppress IL-15-mediated induction of IL-10 in IL-18Rα+ and IL-18Rα−CD45RO+CD4+ T cells.
Figure 5.
The ability of tumor necrosis factor-like cytokine 1A (TL1a) to inhibit interleukin-15 (IL-15)-mediated IL-10 production is IL-18 dependent. (a–d) Peripheral blood CD45RO+CD4+ T cells (1 × 106 cells ml−1, 200 μl per well) were cultured in medium alone (control) or with IL-12 (2 ng ml−1), IL-18 (50 ng ml−1), IL-15 (25 ng ml−1), and TL1a (100 ng ml−1) as indicated, and IL-10 levels were determined in culture supernatants at day 4. (a) IL-15 induces IL-10 production in CD45RO+CD4+ T cells that is inhibited by TL1a. Results are mean (s.e.m.) of 13 biological replicates. (b) IL-15-mediated induction of IL-10 requires IL-12 but not IL-18. Results are mean (s.e.m.) of 5 biological replicates. (c) TL1a-mediated inhibition of IL-10 is IL-18 dependent. Results are mean (s.e.m.) of 9 biological replicates. (d) TL1a-mediated inhibition of IL-10 is DR3 dependent. CD45RO+CD4+T cells were cultured with the indicated cytokines in the presence of DR3 Fab′ or isotype control Fab′ (5 μg ml−1). Results are the mean (s.e.m.) of 14 biological replicates. IL-15 induces IL-10 production in (e) IL-18Rα+ and IL-18Rα−CD45RO+CD4+ T cells and (f) FoxP3+ and FoxP3−CD45RO+CD4+ T cells. CD45RO+CD4+ T cells were cultured as indicated for 4 days, stimulated 4 h with phorbol 12-myristate 13-acetate (PMA) and ionomycin, and stained for IL-10. Results are representative of 3 biological replicates. (g) IL-15Rα expression on IL-18Rα+ and IL-18Rα−CD4+ T cells 4 days after culture with the indicated cytokine cocktails (black line, unfilled histogram). Results are representative plots from 3 biological replicates. Isotype, shaded histogram.
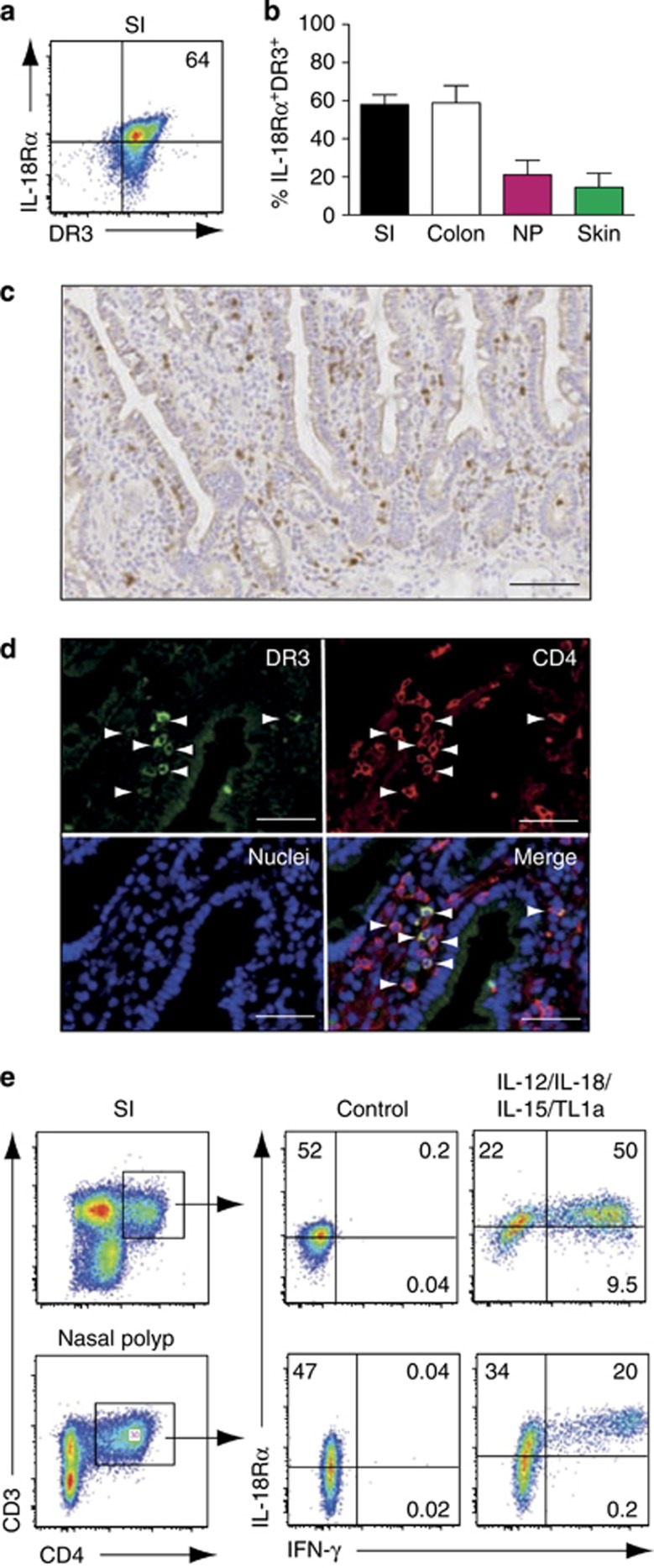
IL-18Rα+DR3+ CD4+ T cells are present at barrier surfaces and display innate lymphocyte functionality
Most memory CD4+ T cells in the body are located at barrier surfaces, where they are believed to have important roles in maintaining tissue homeostasis and in protection against invading pathogens.17 To determine whether tissue-resident CD4+ T cells contained IL-18Rα+DR3+CD4+ T cells, we assessed IL-18Rα and DR3 expression on freshly isolated CD4+ T cells isolated from human small intestine, colon, nasal polyps, and skin (Figure 6a, b). CD4+ T cells isolated from healthy small intestine expressed low levels of DR3 (Supplementary Figure S6); however, expression levels increased after 2 days of culture in medium alone (Figure 6a and Supplementary Figure S6), indicating that the enzyme cocktail used to isolate these cells to some extent cleaved DR3. Consistent with this possibility, the enzyme cocktail reduced DR3 expression on PB mononuclear cells (data not shown) and CD4+ T cells that migrated out of undigested finely cut intestinal tissues expressed DR3 at similar levels to those found after 2 days of culture in the medium (Supplementary Figure S6). In contrast to DR3, IL-18Rα expression was not affected by the digestion procedure (data not shown). IL-18Rα+DR3+CD4+ T cells were present in all tissues, in particular within the small intestine and colon, where they represented the majority of CD4+ T cells (Figure 6b). Immunohistochemical analysis demonstrated that DR3+ cells were scattered throughout the small intestinal lamina propria (LP) (Figure 6c), and that most of these cells coexpressed CD4 (Figure 6d). To determine which tissue-derived CD4+ T cells could be induced to express IFN-γ following cytokine stimulation, cell suspensions from the small intestine and nasal polyps (tissue samples that contained the greatest number of cells) were cultured in medium alone or with IL-12/IL-18/IL-15/TL1a and IFN-γ expression by CD4+ T cells assessed after 2 days by intracellular staining (Figure 6e). Consistent with results obtained with circulating CD45RO+CD4+ T cells, the cytokine cocktail selectively induced IFN-γ production in nasal polyp or small intestinal-derived IL-18Rα+DR3+CD4+ T cells (Figure 6e). Collectively, these results indicate that cytokine-responsive IL-18Rα+DR3+CD4+ T cells are present in barrier tissues.
Figure 6.
Interleukin-18 receptor alpha (IL-18Rα)+death receptor 3 (DR3)+CD4+ T cells are present at barrier surfaces. (a) Representative flow cytometry plot and (b) percentage of IL-18Rα+DR3+ cells in the indicated organs. IL-18Rα and DR3 expression on CD4+ T cells was assessed after incubation in culture medium for 2 days to allow re-expression of DR3. Gating is on live, CD3+CD4+ cells. (b) Results are mean (s.e.m.) of 7 (small intestine, SI), 3 (nasal polyp, NP), 5 (colon), and 3 (skin) stainings performed. (c and d) DR3+CD4+ cells are diffusely distributed throughout the healthy human small intestine. (c) Small intestinal sections were stained with DR3 antibody. (d) Sections were stained with DR3 and CD4 antibody together with 4',6-diamidino-2-phenylindole (DAPI) to identify cell nuclei and analyzed by confocal microscopy. Arrowheads depict DR3+CD4+ cells. Bars=(c) 0.1 mm and (d) 50 μm. Images are from one representative tissue of at least (c) 20 and (d) 3 analyzed. (e) Cytokines induce tissue-resident IL-18Rα+CD4+ T cells to produce interferon-γ (IFN-γ). SI and NP cell suspensions were cultured in medium alone (control) or with interleukin (IL)-12 (2 ng ml−1), IL-18 (50 ng ml−1), IL-15 (25 ng ml−1) and tumor necrosis factor-like cytokine 1A (TL1a) (100 ng ml−1) for 2 days before analysis. Cells were gated on live CD3+CD4+ cells (left panels). Results are representative of 5 (small intestine) and 3 (NP) biologic replicates.
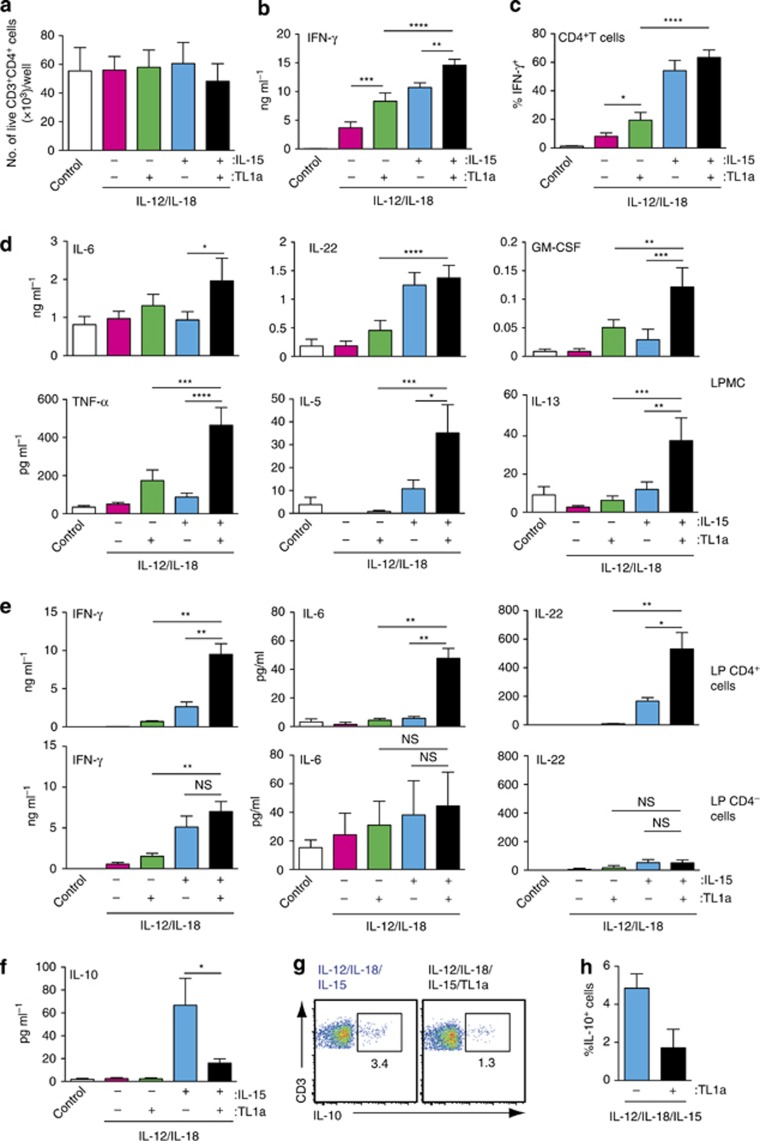
TL1a and IL-15 synergize to promote proinflammatory cytokines in tissue-resident IL-18Rα+DR3+CD4+ T cells
To assess whether TL1a and IL-15 synergize to promote cytokine production in tissue-resident IL-18Rα+DR3+ CD4+ T cells, we focused on small intestinal surgical samples, which gave the numerically greatest yield of cells. LP mononuclear cells (LPMCs) prepared from healthy human small intestine were cultured with the various cytokine cocktails for 2 days. Addition of cytokines did not have a significant impact on CD4+ T-cell numbers during this time period (Figure 7a). TL1a and IL-15 induced IFN-γ production in LPMC cultures containing IL-12/IL-18 and this was further enhanced after the addition of both cytokines (Figure 7b). Similarly, TL1a and IL-15 enhanced the proportion of IFN-γ-expressing LP CD4+ T cells in these cultures (Figure 7c). Addition of neutralizing MHC-II antibody to the cultures had no impact on IFN-γ levels, indicating that cytokine-induced IFN-γ production was independent on cognate TCR–MHC-II interactions (Supplementary Figure S7A). TL1a and IL-15 similarly synergized to promote TNF-α, IL-6, GM-CSF, IL-5, and IL-13 production in LPMC cultures in the presence of IL-12/IL-18 (Figure 7d). Intracellular cytokine staining confirmed that, among LP CD4+ T cells, production of IFN-γ (Figure 7e), IL-6, GM-CSF, and TNF-α was restricted to IL-18Rα+DR3+ cells (Supplementary Figure S7B). However, as expected, other cells including CD8+ T cells as well as CD3− cells produced these cytokines in LPMC cultures (Supplementary Figure S7C) and likely contributed to the overall cytokine levels detected in LPMC culture supernatants. We were unable to detect IL-5, IL-22, or IL-13 in any of these population by intracellular flow cytometry. To determine directly whether TL1a and IL-15 synergized to enhance cytokine production in LP CD4+ T cells, CD4+ T cells were purified from LPMC digestions by positive magnetic-activated cell sorting (purity 95%) and CD4+ and CD4− LPMC fractions were cultured for 2 days with the indicated cytokines (Figure 7e). The levels of cytokines in the CD4+ and CD4- LPMC fractions were notably lower compared with total LPMC (compare Figure 7d and e), indicating that this purification procedure impacted on cellular functionality, and we were unable to detect IL-13, IL-5, or GM-CSF in either CD4+ or CD4− LPMC fractions (data not shown). Nevertheless, TL1a and IL-15 displayed a significant synergy, in the presence of IL-12/IL-18, in inducing IL-6, IFN-γ, and IL-22 in LP CD4+ T cells (Figure 7e). Collectively, these results indicate that IL-15 and TL1a synergize to induce proinflammatory cytokine production in tissue-resident IL-18Rα+DR3+CD4+ T cells. Finally, as observed with PB CD45RO+CD4+ T cells, addition of IL-15 to LPMC cultures in the presence of IL-12/IL-18 induced IL-10 production in LPMCs and this was inhibited by coincubation with TL1a (Figure 7f). Further TL1a inhibited IL-15-induced IL-10 production in LP-derived CD4+ T cells as assessed by flow cytometry analysis (Figure 7g, h).
Figure 7.
Interleukin-15 (IL-15) and tumor necrosis factor-like cytokine 1A (TL1a) synergize to induce cytokine production in tissue-resident IL-18Rα+DR3+CD4+ T cells. Small intestinal lamina propria mononuclear cells (a–d, f–h) or purified CD4+ and CD4− lamina propria cell fractions (e) were incubated (1 × 106 cells per ml, 200 μl per well) with the indicated cytokines or medium alone (control). (a) Number of live CD3+CD4+ cells after 2 days of culture. The cytokine levels in (b, d, e, and f) cell culture supernatants, (c) intracellular cytokine staining, or (g and h) IL-10 secretion assay staining assessed after 2 days. (c, g, and h) Gating is on live CD3+CD4+ T cells. Results are mean (s.e.m.) of (a) 3, (b, d, and f) 9, (c) 5, (e) 3 and (g and h) 3 small intestinal preparations.
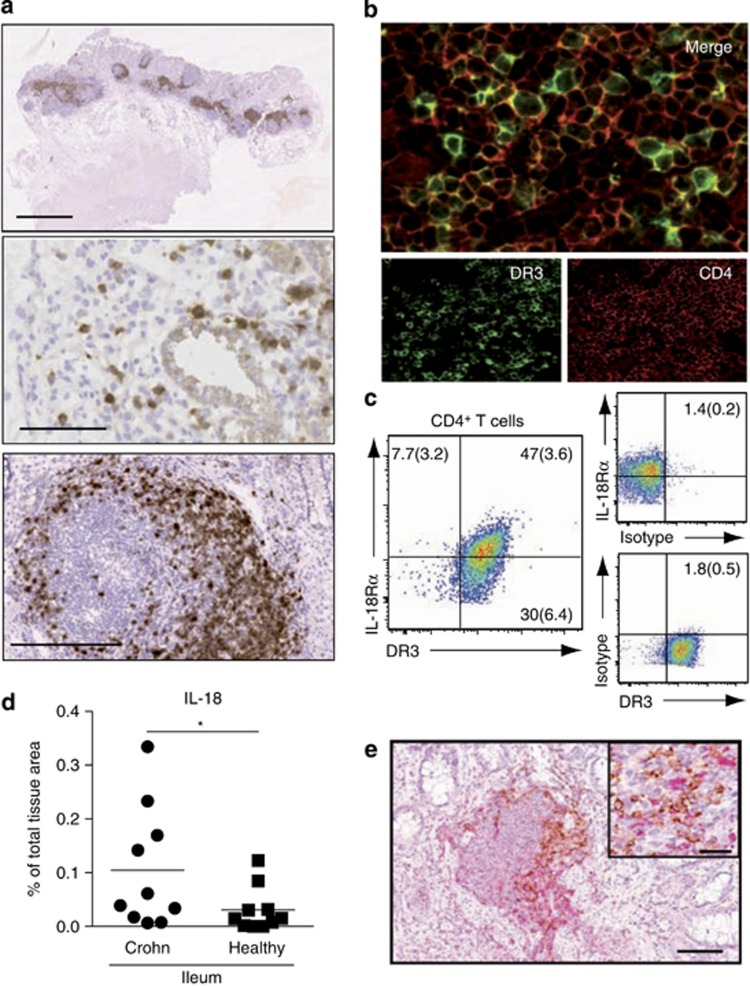
IL-18Rα+DR3+ T cells co-localize with IL-18 expressing cells in the intestine of Crohn's disease patients
IL-18, IL-15, IL-12, and TL1a expression is increased in a wide array of autoimmune and chronic inflammatory diseases including Crohn's disease (CD)18, 19, 20, 21, 22, 23, 24, 25 and have been implicated in disease pathogenesis (for reviews see refs 26,27,28). We thus assessed whether cytokine-responsive IL-18Rα+DR3+CD4+ T cells were present in the inflamed intestine of CD patients. DR3+ cells were distributed diffusely throughout the small intestine of CD patients and accumulated in large numbers within lymphoid aggregates, many of which were B-cell-containing lymphoid follicles (Figure 8a, data not shown). Costaining confirmed that DR3+ cells within these aggregates were CD4+ T cells and not B cells (Figure 8b, data not shown). Consistent with this finding, many CD4+ T cells isolated from the inflamed small intestine coexpressed DR3 and IL-18Rα (Figure 8c). Given the requirement for IL-18 in cytokine-induced CD4+ T-cell responses, we finally assessed IL-18 expression in the inflamed small intestine of CD patients and determined whether IL-18 immune reactivity colocalized with IL-18Rα+DR3+CD4+ T cells (Figure 8d, e). IL-18 immune reactivity was greater in the inflamed small intestine of CD patients compared with healthy controls (Figure 8d). Further in CD small intestine IL-18-expressing cells were primarily localized within lymphoid aggregates in immediate proximity to IL-18Rα+DR3+CD4+ T cells (Figure 8e). Taken together, these results suggest that lymphoid aggregates and lymphoid follicles may serve as sites of cytokine-induced T-cell activation in CD.
Figure 8.
Interleukin-Il-18R alpha (IL-18Rα)+death receptor 3 (DR3)+CD4+ T cells colocalize with interleukin-18 (IL-18)-expressing cells in inflamed small intestine. (a) DR3+ cells (brown) are diffusely distributed throughout the inflamed human small intestine and predominantly located within lymphoid aggregates and follicles. Six micrometer sections of inflamed small intestine biopsies from Crohn's disease (CD) patients were stained with DR3 antibody as described in Methods section. Results are from one representative patient of 15 analyzed. Bars=2 mm (top), 0.1 mm (middle), and 0.25 mm (bottom). (b) DR3+ cells within aggregates are CD4+ T cells. Sections were stained with DR3 and CD4 antibody as described in Methods section and analyzed by confocal microscopy. Results are from one representative patient of 5 analyzed. (c) Most DR3+CD4+ T cells from inflamed small intestine coexpress IL-18Rα. Lamina propria mononuclear cells were prepared from inflamed small intestine and maintained in culture medium for 2 days before analysis. Gating is on live CD3+CD4+ cells. Results are mean (s.e.m.) of five biological replicates (two from surgical resection tissue and three from biopsies of untreated, newly diagnosed CD patients). (d) IL-18 expression increases in the inflamed small intestine of CD patients. Tissue sections were stained by immunohistochemistry for IL-18 and the numbers of pixels displaying IL-18-positive staining were quantified using computerized image analysis, as described in Methods section. Data are expressed as mean percentage of the total tissue area occupied by IL-18-positive immunoreactivity (circles denote individual patients) (e) IL-18-producing cells colocalize with CD4+ cells in lymphoid aggregates in CD small intestine. Sections were stained with CD4 antibody (brown) and IL-18 antibody (red). Results are a representative staining from 1 of 10 patients examined. Bar=0.1 mm. Insert bar=40 μm.
Discussion
In the current study, we demonstrate potent synergy between IL-15 and TL1a in inducing TCR-independent proinflammatory cytokine production by human CD45RO+CD4+ T cells. IL-15- and TL1a-induced proinflammatory cytokine production was restricted to a subset of memory CD4+ T cells that coexpressed IL-18Rα and DR3 and required the presence of IL-18. IL-18Rα+DR3+CD4+ T cells with similar functionality were present in a range of barrier tissues, most notably in the intestine where they represented the majority of CD4+ T cells. Thus, in addition to their well-recognized adaptive immune functions, our results suggest that many tissue-resident memory CD4+ T cells are capable of innate-like functionality independent of cognate antigen recognition. Finally, IL-18Rα+DR3+CD4+ T cells localized together with IL-18-expressing cells in lymphoid aggregates and lymphoid follicles in the inflamed small intestine of CD patients, suggesting that these structures may serve as potential sites of cytokine-induced CD4+ T-cell activation in CD.
IL-12 and IL-18 induce limited IFN-γ production in human CD4+ T helper cells; however, the addition of either IL-15 or TL1a enhances this response.10, 11 Furthermore, TL1a was recently found in the presence of IL-12 and IL-18 to induce production of multiple proinflammatory cytokines in PB CD4+ T cells.13 Here we confirm and extend these findings, demonstrating that both TL1a and IL-15 induce expression of a wide range of cytokines, including IFN-γ, IL-6, GM-CSF, IL-5, IL-13, TNF-α, and IL-22 in CD45RO+CD4+ T cells and show for the first time, as far as we are aware, a significant synergy between TL1a and IL-15 in enhancing this response. While IL-18 was critically required for TL1a- and IL-15-mediated induction of all inflammatory cytokines, IL-12 was required for TL1a- and IL-15-mediated induction of IFN-γ, IL-6, and TNF-α, but not for TL1a- and IL-15-mediated induction of IL-22- or the Th2-associated cytokines IL-13 and IL-5 and GM-CSF. These results suggest that local levels of IL-12 may determine whether TL1a and IL-15 skews innate memory CD4+ T-cell responses toward a Th1- or Th2-dominated response. Of note, transgenic expression of TL1a in murine dendritic cells/macrophages or T cells leads to elevated levels of IL-13 but not IFN-γ, and development of IL-13-mediated inflammation in the small intestine.29, 30 While RAG−/− mice transgenic for TL1a display enhanced levels of IL-13 derived from TL1a-responsive ILC2s,31, 32 our results suggest that in a T-cell-competent setting, intestinal memory CD4+ T cells may also contribute to this response.
Information on the phenotype of cytokine-responsive CD4+ T cells is sparse. Sattler et al10 identified a subset of circulating IL-18Rα+ CD4+ T cells as the primary IFN-γ-producing cells after stimulation with IL-15/IL-12/IL-18, whereas TL1a/IL-12/IL-18 has been shown to induce IFN-γ expression in a subset of memory CD4+ cells expressing CD161.12, 13 Our findings that TL1a and IL-15 induced proinflammatory cytokine production was IL-18 dependent suggested that both cytokines functioned primarily in IL-18Rα+CD4+ T cells. Consistent with this possibility, we found that IL-15 and TL1a alone or in combination selectively induce proinflammatory cytokine expression in IL-18Rα+CD4+ cells. We found that PB IL-18Rα+ but not IL-18Rα− memory CD4+ T cells in cytokine cultures expressed high levels of the TL1a receptor, DR3. Further, while CD161 was coexpressed on a large proportion of these cells, IL-18Rα+DR3hi memory T cells lacking expression of CD161 produced IFN-γ after cytokine stimulation, demonstrating that CD161 is not a selective marker for IL-15- or TL1a-responsive memory CD4+ T cells.
After 1 day of culture, IL-15 and TL1a synergized to induce IFN-γ production in IL-18Rα+DR3+CD4+ T cells without impacting on IL-18Rα+ T-cell numbers. In contrast, increased numbers of IL-18Rα+CD4+ T cells were observed in 4 days of culture, and BrdU incorporation studies demonstrated that TL1a or IL-15 induced a selective proliferation of IL-18Rα+CD4+ T cells that was further enhanced after the addition of both cytokines. Thus, in addition to directly inducing cytokine production in IL-18Rα+CD4+ T cells, IL-15 and TL1a synergize to promote IL-18Rα+CD4+ T-cell proliferation. Proliferation was not required for cytokine-induced IFN-γ production in IL-18Rα+CD4+ T cells; however, enhanced numbers of cytokine-responsive IL-18Rα+CD4+ T cells in cultures containing IL-15 and TL1a likely contributed to the enhanced levels of proinflammatory cytokines observed in these cultures.
In contrast to the IL-18-dependent proinflammatory cytokine induction by IL-15, we found that IL-18 was not required for IL-15-mediated induction of IL-10 in CD45RO+CD4+ T cells, similar to previous findings in human natural killer cells.33 Consistent with these results, we found that both IL-18Rα+ and IL-18Rα−CD45RO+CD4+ T cells expressed IL-15Rα and that IL-15 induced IL-10 production in both these populations. Further, in direct contrast to the synergistic activity of TL1a and IL-15 in driving proinflammatory cytokine production, TL1a inhibited IL-15-mediated induction of IL-10 in both IL-18Rα+ and IL-18Rα−CD45RO+CD4+ T cells. While the underlying mechanism of TL1a-mediated inhibition of IL-10 remains unclear, it was IL-18 and DR3 dependent, demonstrating that inhibition requires signaling through IL-18Rα+DR3+CD4+ T cells, and indicating indirect inhibition via cell-bound and/or soluble factors generated by IL-18Rα+ T cells. Thus, TL1a and IL-15 display marked opposing effects in regulating IL-10 production in CD45RO+CD4+ T cells. The ability of TL1a to inhibit IL-10 production in CD45RO+CD4+ T cells represents a novel proinflammatory function for this cytokine.
Barrier tissues contain the largest population of memory CD4+ T cells in the body, where they are believed to have key roles in TCR-dependent immune surveillance after recognition of foreign and self-antigen presented on local antigen-presenting cells. Here we find that a large proportion of tissue-resident memory CD4+ T cells, characterized by coexpression of IL-18Rα and DR3, can be induced to express inflammatory cytokines independently of cognate antigen recognition. We further show that intestinal IL-18Rα+DR3+ memory CD4+ T cells are diffusely dispersed throughout the normal healthy intestinal LP and are thus in immediate proximity to intestinal macrophages and dendritic cells,34, 35 which can serve as important sources of IL-15, IL-18, IL-12, and TL1a,36, 37, 38, 39 in particular after microbial and inflammatory insult.39, 40, 41, 42 Collectively, these findings suggest that IL-18Rα+DR3+CD4+ T cells may contribute to early innate non-cognate responses within these tissues. Consistent with this possibility, non-cognate IL-18-dependent cytokine production by CD4+ T cells was recently suggested to contribute to the resolution of Salmonella infection in mice.43
There is now considerable evidence that the TL1a/DR3 axis has a central proinflammatory role in inflammatory bowel disease.44 TL1a levels are elevated in the inflamed mucosa of both CD and ulcerative colitis patients20, 21 and single-nucleotide polymorphisms in the TL1a gene are associated with increased risk of inflammatory bowel disease.45, 46 Further, in animal models of colitis, neutralization of TL1a/DR3 activity attenuates inflammation,29, 47 whereas overexpression of TL1a in the T-cell or myeloid compartment of mice leads to spontaneous small intestinal inflammation.29, 48 Our findings that TL1a synergizes with IL-15 to enhance proinflammatory cytokine production in PB and tissue-resident memory IL-18Rα+DR3+CD4+ T cells, combined with our observations that IL-18Rα+DR3+CD4+ T cells are present in large numbers in the inflamed intestine of CD patients, suggest that these cells are a potential TL1a target population in the inflamed mucosa. Further studies will however be required to determine the role of IL-18Rα+DR3+CD4+ T cells, as well as TL1a-dependent cytokine responses by these cells in inflammatory bowel disease pathogenesis.
Methods
Patient material. This study was carried out in accordance with the Declaration of Helsinki. Healthy donor blood was obtained from Rigshospitalet, Copenhagen, Denmark after informed consent. All human tissue material was obtained through Skåne University Hospital, Sweden except the intestinal cryosections in Figure 6c, d, and Figure 8a, b that were obtained from Cambridge Bioscience (Cambridge, UK). Healthy small intestinal tissue was obtained from patients undergoing cystectomy with bladder reconstruction. Inflamed small intestinal tissue was obtained from CD patients at surgery or from biopsies at colonoscopy; healthy colon biopsies were obtained from patients referred to colonoscopy because of bowel discomfort, loose stool, or anemia that showed no endoscopic or histologic signs of inflammation. Only CD patients and controls without clinical signs of infection and not on immunosuppressive medication were included in the study. Healthy skin samples were obtained from patients undergoing surgery with full-thickness skin grafting because of tumor excisions in the face. Patients were not taking immunosuppressive medication and did not suffer from inflammatory skin disease, such as atopic dermatitis or psoriasis. Finally, inflamed nasal tissue was obtained from patients with nasal polyposis undergoing routine polypectomy. All materials were obtained with informed patient consent and in accordance with local ethical approval from the Regional Ethics committee.
Cell isolation Isolation of PB memory CD4+ T cells. CD4+ T cells were isolated from whole blood by negative selection using “Rosette sep CD4+ T cell enrichment cocktail” (StemCell Technologies, Vancouver, BC, Canada) and memory CD4+ T cells were purified from the CD4+ T cells by negative selection using the “Memory CD4+ T Cell Isolation Kit” (Miltenyi Biotec, Bergisch Gladbach, Germany) and an autoMACS pro separator (Miltenyi Biotec). CD45RO+CD4+ T-cell purity was 95–99%.
Isolation of intestinal LPMCs. Intestinal LPMCs were isolated from surgical samples essentially as previously described.34, 35 However, after removal of epithelial cells, tissue was incubated in R-10 medium (RPMI-1640, fetal calf serum (10%), HEPES (10 mM), sodium pyruvate (1 mM), b-mercaptoethanol (50 μM), penicillin (100 U ml−1), and gentamycin (50 μg ml−1)) supplemented with 0.2 μm-filtered collagenase 1a (1 mg ml−1) and DNase I (10 U ml−1) with magnetic stirring at 37 °C for 60 min. The cell suspension was then passed through a 100 μm cell strainer, cells were washed, and then used for experiments. For isolation of LP CD4+ cells, LPMCs were centrifuged through a 40%/70% percoll gradient followed by positive selection by magnetic-activated cell sorting using CD4 microbeads (Miltenyi Biotec). For removal of epithelial cells from intestinal biopsies, tissue fragments were first incubated in 20 ml Hank's balanced salt solution containing EDTA (2 mM), fetal calf serum (5%), HEPES (10 mM), and penicillin (100 U ml−1) with magnetic stirring at 37 °C for 45 min. After incubation, the epithelial cells in suspension were removed by aspiration and the remaining tissue was washed in R-10, and digested as above.
Isolation of dermal cells. Skin samples were cut into 1 cm2 pieces and placed into 25 cm2 tissue culture flasks (Sarstedt, Nürnbrecht, Germany) with 20 ml Hank's balanced salt solution containing EDTA (2 mM), fetal calf serum (5%), HEPES (10 mM), and penicillin (100 U ml−1) for 20 min with continuously shaking at 37 °C. The epidermal layer was then cut from the tissue, and the remaining dermis was cut into small pieces using surgical blades and put in R-10 medium supplemented with 0.2 μm-filtered collagenase 1a (1 mg ml−1) and DNase I (10 U ml−1) with magnetic stirring at 37 °C for 60 min. After digestion, the cell suspension was passed through a 100 μm cell strainer, and the collected cell pellet washed and used in experiments.
Isolation of cells from nasal polyps. Isolation of cells from nasal polyps was performed essentially as previously described.49 However, the tissue was first incubated in 15 ml Hank's balanced salt solution containing EDTA (2 mM), fetal calf serum (5%), HEPES (10 mM), penicillin (100 U ml−1), and DL-dithiothreitol (0.15 mg ml−1) with magnetic stirring at 37 °C for 30 min. After epithelial cell removal, the remaining tissue was finely cut with surgical blades and incubated in 10 ml PBS containing collagenase D (0.5 mg ml−1), DNase I (0.5 mg ml−1), and dispase II (3 mg ml−1) with magnetic stirring at 37 °C for 60 min. The resulting cell suspension was passed through a 100 μm cell strainer, cells were washed, and used for experiments.
Cell culture. Cells (1 × 106 cells ml−1) were incubated in culture medium (RPMI-1640, penicillin (100 U ml−1), and human serum (10%)) with the indicated cytokines in 96-well plates at 37 °C in 5% CO2 for 1–4 days (PB CD45RO+CD4+ T cells) or 2 days (cells derived from intestine, skin, or nasal polyps). Cytokine levels in culture supernatants were assessed by Bio-Plex Pro Human Cytokine 17-plex Assay or Bio-Plex Pro Human Th17 Cytokine IFN-γ Set/Bio-Plex Pro Human Th17 Cytokine IL-10 Set (Bio-Rad, Hercules, CA) according to the manufacturer's instructions using the Bio-Plex 200 System (Bio-Rad). For mixed lymphocyte reactions, peripheral blood mononucleated cells from two donors were isolated using Ficoll gradients and cultured (2 × 105 cells per donor, total volume 200 μl) in 96-well plates. Wells containing 4 × 105 cells from the same donor were used as negative controls. [3H]thymidine (Perkin-Elmer, Waltham, MA) was added to the cultures on day 3 at 1 μCi per well, and 18 h later, the cells were harvested using a filtermate harvester (Perkin-Elmer) and analyzed using a Topcounter NXT (Perkin-Elmer).
Generation of anti-DR3 Fab′. For the generation of antagonistic anti-DR3 Fab′, mice were immunized with DR3 protein containing extracellular domains only. Generated antibodies were screened for their capacity to prevent TL1a binding to DR3-transfected cells (HEK293 and CHO cells). The anti-DR3-Fab′ fragment was generated by papain digestion. Anti-TNP IgG4 Fab′ was generated in house in a similar manner and used as a control.
Generation of hDR3-transfected cells. The HEK293-EBNA expression system described by Durocher et al.50 was used for transient expression. Briefly, HEK293-6E cells were transiently transfected with the suitable pTT5 vector, containing hDR3 with a truncated intracellular death domain. An empty pTT5 vector was used as mock control. Cells were transfected with 293Fectin (Invitrogen, Carlsbad, CA) and standard 30 μg DNA/30 ml culture (containing 106 cells per ml).
Flow cytometry analysis. Flow cytometry analysis was performed essentially as previously described.35 Before staining with relevant antibodies, cells were incubated for 15 min with 10% human serum. For detection of DR3, cells were either (1) incubated with biotinylated polyclonal DR3 antibody followed by incubation with biotinylated anti-goat IgG and streptavidin-PE or (2) incubated with APC-DR3 Fab′. For detection of IL-10, T cells were stained with the APC-IL-10 secretion assay according to the manufacturer's instructions (Miltenyi Biotec), with an extended secretion period (1 h). Intracellular cytokine and FoxP3 staining was performed using the BD Cytofix/Cytoperm Kit (BD Biosciences, San Jose, CA) or Inside Stain Kit (Miltenyi Biotec) according to the manufacturer's instructions. Foxp3/Transcription Factor Staining Buffer Set was used for FoxP3 staining according to the manufacturer's instruction (eBioscience, San Diego CA). For detection of intracellular IL-6, TNFα, and GM-CSF (Figure 3c and Supplementary Figure S7B), brefedin A (10 μg ml−1) was added to the cell cultures 4 h before analysis. BrdU incorporation was assessed using the APC BrdU Flow Kit assay (Invitrogen) according to the manufacturer's instructions. Flow cytometry was performed on an LSR II flow cytometer (BD Biosciences) and data were analyzed with FlowJo software (Tree Star, Ashland, OR).
Immunohistochemistry. For DR3 staining, 6 μm cryostat sections were dried and fixed in ice-cold acetone. Nonspecific binding sites were blocked with donkey serum (7%), human serum (3%), and non-fat dry milk (3%). Sections were incubated with an in house-generated mouse monoclonal antibody recognizing an epitope within the cysteine-rich domain 3 in the DR3 extracellular domain, followed by a biotinylated donkey anti-mouse secondary antibody (Jackson ImmunoResearch, West Grove, PA). Antibody binding was detected using peroxidase-conjugated avidin–biotin complex (VectorStain; Vector Laboratories, Burlingame, CA) and indirect biotin-conjugated tyramide signal amplification system (NEL700 from Perkin-Elmer) visualized by diaminobenzidine (D5905; Sigma-Aldrich, St. Louise, MO). All slides were scanned in a Nanozoomer digital slide scanner (Hamamatsu, Hamamatsu City, Japan). Double immunofluorescence staining for DR3 and CD4 were performed using the same DR3 antibody as above and a rabbit monoclonal anti-CD4 antibody (clone SP35; Nordic BioSite, Stockholm, Sweden). Antibody binding was visualized using tyramide signal amplification-Alexa 488 (DR3) and goat anti-rabbit Alexa 594 (CD4) (Invitrogen). Slides were analyzed by confocal microscopy using an FV10i confocal microscope (Olympus, Tokyo, Japan). For IL-18 staining, 4 μm paraffin sections were stained with polyclonal rabbit anti-IL-18 (Sigma; HPA 003980; dilution 1:100) and mouse monoclonal anti-CD4 (Thermo Scientific, Waltham, MA; 4B12, 1:100) as primary antibodies using the EnVision Doublestain System Kit (K5361; Dako, Glostrup, Denmark). For assessment of immunoreactivity, slides were digitalized in an automated slide scanner (ScanScope; Aperio Technologies, Vista, CA) and VisiomorphDP image software (Visiopharm, Hoersholm, Denmark) was used to quantify marker-specific chromogen, as described previously.51
Statistical analysis. All single column comparisons were performed using the paired Student's t-test and all multiple column analyses were performed using “repeated-measures ANOVA” followed by “Bonferroni's multiple comparison test” (*P<0.05, **P<0.01, and ***P<0.001). Statistical analysis was performed using GraphPad Prism software (GraphPad, La Jolla, CA).
Acknowledgments
We thank A. Mowat (Glasgow University, Glasgow) for constructive comments on the manuscript before submission. This work was supported by NordForsk Nordic PPP PhD program, grants from Novo Nordisk A/S, the Swedish Medical Research Council, the IngaBritt and Arne Lundbergs Foundation, and a clinical grant from the Swedish National Health Service.
P.H., K.R., L.H., and K.H. are or have been employees at Novo Nordisk A/S and own stocks in Novo Nordisk A/S, which partly supported this project.
Footnotes
SUPPLEMENTARY MATERIAL is linked to the online version of the paper at http://www.nature.com/mi
Supplementary Material
References
- Harder J., Schroder J.M., Glaser R. The skin surface as antimicrobial barrier: present concepts and future outlooks. Exp. Dermatol. 2013;22:1–5. doi: 10.1111/exd.12046. [DOI] [PubMed] [Google Scholar]
- Bosch A.A., Biesbroek G., Trzcinski K., Sanders E.A., Bogaert D. Viral and bacterial interactions in the upper respiratory tract. PLoS Pathogen. 2013;9:e1003057. doi: 10.1371/journal.ppat.1003057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamada N., Seo S.U., Chen G.Y., Nunez G. Role of the gut microbiota in immunity and inflammatory disease. Nat.Rev.Immunol. 2013;13:321–335. doi: 10.1038/nri3430. [DOI] [PubMed] [Google Scholar]
- Maloy K.J., Powrie F. Intestinal homeostasis and its breakdown in inflammatory bowel disease. Nature. 2011;474:298–306. doi: 10.1038/nature10208. [DOI] [PubMed] [Google Scholar]
- Martinez F.D., Vercelli D. Asthma. Lancet. 2013;382:1360–1372. doi: 10.1016/S0140-6736(13)61536-6. [DOI] [PubMed] [Google Scholar]
- Berin M.C., Sampson H.A. Mucosal immunology of food allergy. Curr. Biol. 2013;23:R389–R400. doi: 10.1016/j.cub.2013.02.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheridan B.S., Lefrancois L. Regional and mucosal memory T cells. Nat. Immunol. 2011;12:485–491. doi: 10.1038/ni.2029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodland D.L., Kohlmeier J.E. Migration, maintenance and recall of memory T cells in peripheral tissues. Nat. Rev. Immunol. 2009;9:153–161. doi: 10.1038/nri2496. [DOI] [PubMed] [Google Scholar]
- McLachlan J.B., Catron D.M., Moon J.J., Jenkins M.K. Dendritic cell antigen presentation drives simultaneous cytokine production by effector and regulatory T cells in inflamed skin. Immunity. 2009;30:277–288. doi: 10.1016/j.immuni.2008.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sattler A., et al. Cytokine-induced human IFN-gamma-secreting effector-memory Th cells in chronic autoimmune inflammation. Blood. 2009;113:1948–1956. doi: 10.1182/blood-2008-02-139147. [DOI] [PubMed] [Google Scholar]
- Papadakis K.A., et al. TL1A synergizes with IL-12 and IL-18 to enhance IFN-gamma production in human T cells and NK cells. J. Immunol. 2004;172:7002–7007. doi: 10.4049/jimmunol.172.11.7002. [DOI] [PubMed] [Google Scholar]
- Cohavy O., Shih D.Q., Doherty T.M., Ware C.F., Targan S.R. Cd161 defines effector T cells that express light and respond to Tl1a-Dr3 signaling. Eur. J. Microbiol. Immunol. (Bp) 2011;1:70–79. doi: 10.1556/EuJMI.1.2011.1.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin S., et al. TL1A/TNFSF15 directly induces proinflammatory cytokines, including TNFalpha, from CD3+CD161+ T cells to exacerbate gut inflammation. Mucosal Immunol. 2013;6:886–899. doi: 10.1038/mi.2012.124. [DOI] [PubMed] [Google Scholar]
- Yang J., Zhu H., Murphy T.L., Ouyang W., Murphy K.M. IL-18-stimulated GADD45 beta required in cytokine-induced, but not TCR-induced, IFN-gamma production. Nat. Immunol. 2001;2:157–164. doi: 10.1038/84264. [DOI] [PubMed] [Google Scholar]
- Berenson L.S., Yang J., Sleckman B.P., Murphy T.L., Murphy K.M. Selective requirement of p38alpha MAPK in cytokine-dependent, but not antigen receptor-dependent, Th1 responses. J. Immunol. 2006;176:4616–4621. doi: 10.4049/jimmunol.176.8.4616. [DOI] [PubMed] [Google Scholar]
- Kumaki S., Armitage R., Ahdieh M., Park L., Cosman D. Interleukin-15 up-regulates interleukin-2 receptor alpha chain but down-regulates its own high-affinity binding sites on human T and B cells. Eur. J. Immunol. 1996;26:1235–1239. doi: 10.1002/eji.1830260608. [DOI] [PubMed] [Google Scholar]
- Swain S.L., McKinstry K.K., Strutt T.M. Expanding roles for CD4(+) T cells in immunity to viruses. Nat. Rev. Immunol. 2012;12:136–148. doi: 10.1038/nri3152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pizarro T.T., et al. IL-18, a novel immunoregulatory cytokine, is up-regulated in Crohn's disease: expression and localization in intestinal mucosal cells. J. Immunol. 1999;162:6829–6835. [PubMed] [Google Scholar]
- Monteleone G., et al. Bioactive IL-18 expression is up-regulated in Crohn's disease. J. Immunol. 1999;163:143–147. [PubMed] [Google Scholar]
- Bamias G., et al. Expression, localization, and functional activity of TL1A, a novel Th1-polarizing cytokine in inflammatory bowel disease. J. Immunol. 2003;171:4868–4874. doi: 10.4049/jimmunol.171.9.4868. [DOI] [PubMed] [Google Scholar]
- Prehn J.L., et al. Potential role for TL1A, the new TNF-family member and potent costimulator of IFN-gamma, in mucosal inflammation. Clin. Immunol. 2004;112:66–77. doi: 10.1016/j.clim.2004.02.007. [DOI] [PubMed] [Google Scholar]
- Sakai T., et al. Interleukin 15 activity in the rectal mucosa of inflammatory bowel disease. Gastroenterology. 1998;114:1237–1243. doi: 10.1016/s0016-5085(98)70430-5. [DOI] [PubMed] [Google Scholar]
- Liu Z., Geboes K., Colpaert S., D'Haens G.R., Rutgeerts P., Ceuppens J.L. IL-15 is highly expressed in inflammatory bowel disease and regulates local T cell-dependent cytokine production. J. Immunol. 2000;164:3608–3615. doi: 10.4049/jimmunol.164.7.3608. [DOI] [PubMed] [Google Scholar]
- Parronchi P., et al. Type 1 T-helper cell predominance and interleukin-12 expression in the gut of patients with Crohn's disease. Am. J. Pathol. 1997;150:823–832. [PMC free article] [PubMed] [Google Scholar]
- Monteleone G., et al. Interleukin 12 is expressed and actively released by Crohn's disease intestinal lamina propria mononuclear cells. Gastroenterology. 1997;112:1169–1178. doi: 10.1016/s0016-5085(97)70128-8. [DOI] [PubMed] [Google Scholar]
- Monteleone G., Fina D., Caruso R., Pallone F. New mediators of immunity and inflammation in inflammatory bowel disease. Curr. Opin. Gastroenterol. 2006;22:361–364. doi: 10.1097/01.mog.0000231808.10773.8e. [DOI] [PubMed] [Google Scholar]
- Meylan F., Richard A.C., Siegel R.M. TL1A and DR3, a TNF family ligand-receptor pair that promotes lymphocyte costimulation, mucosal hyperplasia, and autoimmune inflammation. Immunol. Rev. 2011;244:188–196. doi: 10.1111/j.1600-065X.2011.01068.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Heel D.A. Interleukin 15: its role in intestinal inflammation. Gut. 2006;55:444–445. doi: 10.1136/gut.2005.079335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meylan F., et al. The TNF-family cytokine TL1A drives IL-13-dependent small intestinal inflammation. Mucosal Immunol. 2011;4:172–185. doi: 10.1038/mi.2010.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taraban V.Y., et al. Sustained TL1A expression modulates effector and regulatory T-cell responses and drives intestinal goblet cell hyperplasia. Mucosal Immunol. 2011;4:186–196. doi: 10.1038/mi.2010.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu X., et al. TNF superfamily member TL1A elicits type 2 innate lymphoid cells at mucosal barriers. Mucosal Immunol. 2013;7:730–740. doi: 10.1038/mi.2013.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meylan F., et al. The TNF-family cytokine TL1A promotes allergic immunopathology through group 2 innate lymphoid cells. Mucosal Immunol. 2013;7:958–968. doi: 10.1038/mi.2013.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fehniger T.A., et al. Differential cytokine and chemokine gene expression by human NK cells following activation with IL-18 or IL-15 in combination with IL-12: implications for the innate immune response. J. Immunol. 1999;162:4511–4520. [PubMed] [Google Scholar]
- Bain C.C., et al. Resident and pro-inflammatory macrophages in the colon represent alternative context-dependent fates of the same Ly6Chi monocyte precursors. Mucosal Immunol. 2013;6:498–510. doi: 10.1038/mi.2012.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Persson E.K., et al. IRF4 transcription-factor-dependent CD103(+)CD11b(+) dendritic cells drive mucosal T helper 17 cell differentiation. Immunity. 2013;38:958–969. doi: 10.1016/j.immuni.2013.03.009. [DOI] [PubMed] [Google Scholar]
- Vignali D.A., Kuchroo V.K. IL-12 family cytokines: immunological playmakers. Nat. Immunol. 2012;13:722–728. doi: 10.1038/ni.2366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fehniger T.A., Caligiuri M.A. Interleukin 15: biology and relevance to human disease. Blood. 2001;97:14–32. doi: 10.1182/blood.v97.1.14. [DOI] [PubMed] [Google Scholar]
- Kamada N., et al. TL1A produced by lamina propria macrophages induces Th1 and Th17 immune responses in cooperation with IL-23 in patients with Crohn's disease. Inflamm. Bowel Dis. 2010;16:568–575. doi: 10.1002/ibd.21124. [DOI] [PubMed] [Google Scholar]
- Dinarello C.A., Novick D., Kim S., Kaplanski G. Interleukin-18 and IL-18 binding protein. Front. Immunol. 2013;4:289. doi: 10.3389/fimmu.2013.00289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prehn J.L., Thomas L.S., Landers C.J., Yu Q.T., Michelsen K.S., Targan S.R. The T cell costimulator TL1A is induced by FcgammaR signaling in human monocytes and dendritic cells. J. Immunol. 2007;178:4033–4038. doi: 10.4049/jimmunol.178.7.4033. [DOI] [PubMed] [Google Scholar]
- Perera P.Y., Lichy J.H., Waldmann T.A., Perera L.P. The role of interleukin-15 in inflammation and immune responses to infection: implications for its therapeutic use. Microbes Infect. 2012;14:247–261. doi: 10.1016/j.micinf.2011.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchan S.L., Taraban V.Y., Slebioda T.J., James S., Cunningham A.F., Al-Shamkhani A. Death receptor 3 is essential for generating optimal protective CD4(+) T-cell immunity against Salmonella. Eur. J. Immunol. 2011;42:580–588. doi: 10.1002/eji.201041950. [DOI] [PubMed] [Google Scholar]
- O'Donnell H., et al. Toll-like receptor and inflammasome signals converge to amplify the innate bactericidal capacity of T helper 1 cells. Immunity. 2014;40:213–224. doi: 10.1016/j.immuni.2013.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shih D.Q., et al. Insights into TL1A and IBD pathogenesis. Adv. Exp. Med. Biol. 2011;691:279–288. doi: 10.1007/978-1-4419-6612-4_29. [DOI] [PubMed] [Google Scholar]
- Yamazaki K., et al. Single nucleotide polymorphisms in TNFSF15 confer susceptibility to Crohn's disease. Hum. Mol. Genet. 2005;14:3499–3506. doi: 10.1093/hmg/ddi379. [DOI] [PubMed] [Google Scholar]
- Wang K., et al. Comparative genetic analysis of inflammatory bowel disease and type 1 diabetes implicates multiple loci with opposite effects. Hum. Mol. Genet. 2010;19:2059–2067. doi: 10.1093/hmg/ddq078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takedatsu H., et al. TL1A (TNFSF15) regulates the development of chronic colitis by modulating both T-helper 1 and T-helper 17 activation. Gastroenterology. 2008;135:552–567. doi: 10.1053/j.gastro.2008.04.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shih D.Q., et al. Constitutive TL1A (TNFSF15) expression on lymphoid or myeloid cells leads to mild intestinal inflammation and fibrosis. PLoS One. 2011;6:e16090. doi: 10.1371/journal.pone.0016090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu T., et al. Forkhead box P3+ T cells express interleukin-17 in nasal mucosa of patients with both allergic rhinitis and polyposis. Clin. Exp. Immunol. 2011;163:59–64. doi: 10.1111/j.1365-2249.2010.04278.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durocher Y., Perret S., Kamen A. High-level and high-throughput recombinant protein production by transient transfection of suspension-growing human 293-EBNA1 cells. Nucleic Acids Res. 2002;30:E9. doi: 10.1093/nar/30.2.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mori M., et al. Appearance of remodelled and dendritic cell-rich alveolar-lymphoid interfaces provides a structural basis for increased alveolar antigen uptake in chronic obstructive pulmonary disease. Thorax. 2013;68:521–531. doi: 10.1136/thoraxjnl-2012-202879. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.