Key Points
Ex vivo fucosylation of cord blood cells improves their homing capacities, leading to faster neutrophil and platelet engraftments.
This method is quick, safe, and does not require a GMP laboratory; therefore, it can be used widely.
Abstract
Delayed engraftment is a major limitation of cord blood transplantation (CBT), due in part to a defect in the cord blood (CB) cells’ ability to home to the bone marrow. Because this defect appears related to low levels of fucosylation of cell surface molecules that are responsible for binding to P- and E-selectins constitutively expressed by the marrow microvasculature, and thus for marrow homing, we conducted a first-in-humans clinical trial to correct this deficiency. Patients with high-risk hematologic malignancies received myeloablative therapy followed by transplantation with 2 CB units, one of which was treated ex vivo for 30 minutes with the enzyme fucosyltransferase-VI and guanosine diphosphate fucose to enhance the interaction of CD34+ stem and early progenitor cells with microvessels. The results of enforced fucosylation for 22 patients enrolled in the trial were then compared with those for 31 historical controls who had undergone double unmanipulated CBT. The median time to neutrophil engraftment was 17 days (range, 12-34 days) compared with 26 days (range, 11-48 days) for controls (P = .0023). Platelet engraftment was also improved: median was 35 days (range, 18-100 days) compared with 45 days (range, 27-120 days) for controls (P = .0520). These findings support ex vivo fucosylation of multipotent CD34+ CB cells as a clinically feasible means to improve engraftment efficiency in the double CBT setting. The trial is registered to www.clinicaltrials.gov as #NCT01471067.
Introduction
Cord blood transplantation (CBT) is an effective alternative for patients lacking a fully HLA-matched donor.1,2 Indeed, significantly lower doses and a more naïve repertoire of T cells in cord blood (CB) grafts permit a higher degree of HLA mismatch. This unique advantage and the availability of large numbers of CB units in the global inventory allow identification of a suitable unit for almost every patient without an acceptable HLA-matched donor.1,3 However, by comparison with transplantation from matched unrelated donors,2,4-7 CBT has certain limitations, such as delayed engraftment and poor immune reconstitution due to limited numbers of hematopoietic stem and progenitor cells (HSPCs) in the CB graft, which typically result in higher morbidity and mortality rates.8 Transplantation with 2 CB units has increased the number of adults who can be transplanted, but the median time to neutrophil or platelet engraftment remains inferior to engraftment with bone marrow or peripheral HSPCs.9-13 Currently, a number of strategies are being investigated to compensate for the limitations of CB as a source of cells for allogeneic transplantation. One promising approach is ex vivo expansion of CB cells,14-17 but this manipulation does not address a persistent problem intrinsic to CBT: the relatively weak affinity of a large subset of CD34+ cells for the bone marrow microvasculature, leading to defective homing of infused HSPCs to their respective marrow niches.
To overcome this obstacle, our group has taken advantage of the requirement for specific adhesion molecules in the migration of HSPCs to the bone marrow. Briefly, the first step in this process—the capture, rolling, and arrest of leukocytes on bone marrow endothelium—is mediated largely by the interactions of E- and P-selectins on endothelial cells with ligands on HSPCs.18-20 E- and P-selectins are membrane-bound C-type lectins, and their physiologically relevant ligands must be α1,3-fucosylated to form terminal glycan determinants, such as sialylated Lewis x or sLex (NeuAα2-3Galβ1-4[Fucα1-3]GlcNAcβ1-R).18,21,22 Of the surface glycoproteins recognized by these lectins, P-selectin glycoprotein ligand-1 (PSGL-1) is the best characterized.23 In vivo, P-selectin binds to a small N-terminal region of PSGL-1 that must be first modified by sulfation of tyrosines and addition of sLex to a core 2 O-glycan. E-selectin binds to 1 or more different sites on PSGL-1 and to other α2,3-sialylated and α1,3-fucosylated cell surface glycoconjugates as well. The homing of HSPCs to the bone marrow is impaired in immunodeficient mice that lack P- and E-selectins, whereas injection of wild-type mice with blocking antibodies to P-selectin or PSGL-1 diminishes the rolling of CB-derived HSPCs on bone marrow microvessels.24,25
The above studies and others25-27 support a critical role for the selectins and their ligands in HSPC homing to bone marrow, yet they indicate a clear deficit in this property for CB cells, apparently due to reduced levels of fucosylation of E- and/or P-selectin ligands on CB cells compared with those on marrow or peripheral blood-derived HSPCs. Thus, the treatment of CB-derived HSPCs ex vivo with guanosine diphosphate (GDP) fucose and the enzyme fucosyltransferase (FT)-VI has been shown to improve cell surface fucosylation and alleviate this adhesion defect in immunodeficient mice.25-28 We therefore hypothesized that increasing the level of CD34+ cell surface fucosylation ex vivo may improve HSPC homing to bone marrow in CBT patients, leading to enhanced neutrophil and platelet engraftment. In the first-in-humans clinical trial reported here, we demonstrate the safety and logistical feasibility of this strategy in the double CBT setting and provide evidence for fucosylation-dependent improvement in time to neutrophil and platelet engraftment.
Methods
Optimization of conditions for clinical use of α1,3-FT-VI
The preclinical laboratory conditions for use of FT-VI, as recommended by the manufacturer (Targazyme, formerly America Stem Cell, Carlsbad, CA), included incubation of the CB cells at 37°C for 30 minutes in Hanks balanced salt solution containing 1% human serum albumin, 160 mU/mL FT-VI, 1 mM GDP β-fucose, and 1 mM MnCl2. For the optimization experiments, we performed flow cytometry with the HECA-452 antibody (BD Pharmingen, San Diego, CA) to sLex/cutaneous lymphocyte antigen (CLA),29 the fucosylated selectin ligand, to measure the levels of cell surface fucosylation. The end points evaluated included the concentration of the FT-VI enzyme, the optimal duration and temperature for CB-FT(VI)-GDP-fucose incubation, the requirement for manganese (MnCl2), and the stability of the CB product following fucosylation.
Study design
This trial was designed to assess the safety, feasibility, and clinical activity of enforced CB cell surface fucosylation of a single CB unit in the context of double CBT for patients with advanced cancer. The primary end point was the time to neutrophil and platelet engraftment, relative to results for a comparable cohort of patients who had undergone double unmanipulated CBT at this center.
Eligibility
Patients with high-risk hematologic malignancies who lacked a suitable HLA-matched related or unrelated donor were eligible if they had 2 CB units matched at ≥4 HLA loci by intermediate-resolution typing for HLA class I alleles (A and B) or by high-resolution typing for the HLA class II DRB1 allele, and had ≥1.5 × 107 total nucleated cells (TNCs) per kilogram of body weight per CB unit. Adequate organ system function was also required, as indicated by a left ventricular ejection fraction of ≥40%, a pulmonary diffusion capacity of ≥50% of the predicted value, a serum creatinine value <1.6 mg/dL, and an alanine aminotransferase/bilirubin ≤2.0 times normal. This study (http://clinicaltrials.gov study number NCT01471067) was approved by the MD Anderson Institutional Review Board (Protocol 2010-0658) and the Food and Drug Administration (IND 14897).
Preparative regimen and supportive care
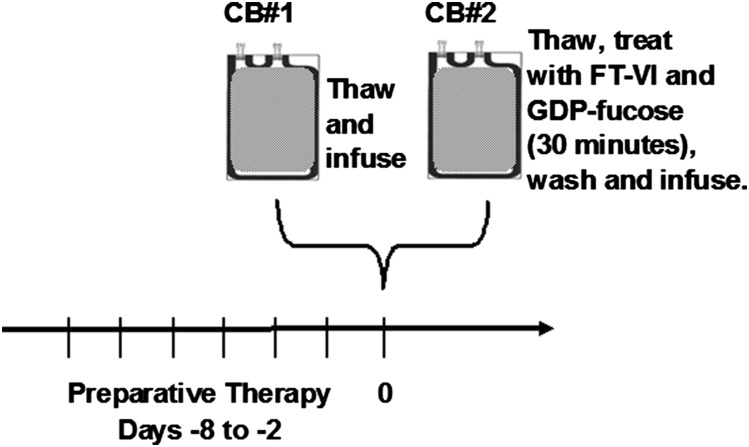
The study schema is shown in Figure 1. The myeloablative regimen consisted of fludarabine, 10 mg/m2 per day (days −7 through −4); clofarabine, 30 mg/m2 per day (days −7 through −4); busulfan at a dose calculated to deliver a daily area under the curve of 4000 µmol/min for 4 days (days −7 through −4) based on an outpatient test dose of 32 mg/m2; and 2 Gy of total body irradiation on day −3. The reduced intensity conditioning regimen for patients >60 years or those with comorbidities consisted of fludarabine (40 mg/m2 per day, days −5 through −2) and melphalan (140 mg/m2, day −2). Prophylaxis against graft-versus-host disease (GVHD) consisted of rabbit antithymocyte globulin for a total of 3 mg/kg infused over 2 days on days −4 and −3, tacrolimus on days −2 through 180, and mycophenolate mofetil at a dose of 15 mg/kg (maximum dose of 1 g orally twice daily) on days −2 through 100. Filgrastim was administered starting on day 0 until neutrophil engraftment. Antimicrobial prophylaxis and blood product support were given according to institutional guidelines.
Figure 1.
Transplantation of unmanipulated and fucosylated CB cells. Patients were admitted on day −8 for intravenous hydration, and the preparative regimen was given from days −7 to −2. On day 0, the CB unit with the highest TNC dose was thawed, washed, and infused without further manipulation. The unit with the smaller TNC dose was then thawed, washed, and treated with 100 mU/mL FT-VI and 1 mM GDP β-fucose (Targazyme) for 30 minutes at room temperature. The fucosylated cells were then washed and infused.
Fucosylation and transplantation procedures
All CB units used in this study were red blood cell (RBC) depleted prior to cryopreservation and shipment to our center (we do not use RBC-replete units). On day 0, the CB unit with the highest TNC dose was thawed, washed on the Sepax device using the CordWash protocol (Biosafe SA), and infused without further manipulation (Figure 1). The second unit with the smaller TNC dose was then thawed and washed on the Sepax device. The 50-mL output volume (106 cells/mL) was treated with FT-VI (100 mU/mL) and GDP β-fucose (1 mM) for 30 minutes at room temperature. The fucosylated cells were then washed a second time on the Sepax device, with the final 100-mL output volume collected and infused. An aliquot of the cells was evaluated by flow cytometry using the Becton-Dickinson FACSCanto II instrument (BD Biosciences, San Jose, CA) before and, for the fucosylated units, after the fucosylation procedure to detect CD45+, CD34+, and CD34+ subsets, as well as megakaryocytes (CD34+CD61+), natural killer (NK) cells (CD56+), T cells (CD3+), monocytes (CD3−CD4+), and B cells (CD19+) as previously described.30 The HECA-452 antibody against the CLA antigen was used to measure fucosylation before and for the treated units, after addition of the FT-VI enzyme and GDP fucose, as previously described.27
Engraftment
The time to neutrophil engraftment was defined as the first of 3 consecutive days with an absolute neutrophil count (ANC) of ≥0.5 × 109/L, and the time to platelet engraftment as the first of 7 consecutive days with a platelet count of ≥20 × 109/L without platelet transfusion. Chimerism in the peripheral blood was documented on days 30 and 60 and every 3 months after CB infusion, using polymerase chain reaction with primer sets flanking microsatellite repeats.
Statistical analysis
Engraftment results in the study cohort (n = 22) were compared with those for historical controls (n = 31) who had undergone double unmanipulated CBT at our institution and whose baseline clinical characteristics, including preparative regimens, were matched as closely as possible to those of the study group (Table 1). Cumulative incidence curves with death as a competing event were constructed by the methods of Gooley et al31 and used to analyze times to platelet and neutrophil engraftment after infusion. A Cox proportional hazards model was used to assess predictors of time to engraftment. Although confirmed by biopsy when feasible, the diagnosis of GVHD was ultimately determined by clinical presentation. Acute GVHD was clinically graded as 0 to IV based on standard criteria32; chronic GVHD was classified as none, limited, or extensive.33 The risk for induction of GVHD within 100 days was estimated by the generation of cumulative incidence curves, with death considered to be the competing risk. No adjustments were made for multiple testing. The 95% confidence intervals (CIs) for the hazard ratios (HR) in the Cox multivariate model were approximated by use of the profile likelihood test.34 The Wilcoxon rank-sum test was used to compare continuous variables, whereas the χ2 or Fisher’s exact test was applied in comparisons of dichotomous variables among groups of patients, using a 2-sided α of 0.05. All statistical analyses were performed with SAS 9.3 for Windows, SAS Institute Inc. (2014).
Table 1.
Patient summary
| Characteristic | Study cohort (n = 22) | Historical controls (n = 31) | P value |
|---|---|---|---|
| Age | |||
| Median (range), years | 42 (20-68) | 49 (15-65) | .464 |
| Sex | |||
| Male | 13 (59%) | 13 (42%) | .218 |
| Female | 9 (41%) | 18 (58%) | |
| Race | |||
| White | 13 (59.1%) | 17 (54.8%) | .915 |
| Hispanic | 6 (27.3%) | 9 (29%) | |
| Black | 2 (9.1%) | 2 (6.5%) | |
| Asian | 1 (4.5%) | 3 (9.7%) | |
| Weight | |||
| Median (range), kg | 79 (52-94) | 75 (43-144) | .454 |
| Body surface area | |||
| Median (range), m2 | 1.92 (1.54-2.19) | 1.9 (1.36-2.38) | .657 |
| Diagnosis | |||
| ALL | 3 (14%) | 4 (13%) | .4327 |
| AML/MDS | 12 (55%) | 20 (65%) | |
| CLL | 0 (0%) | 1 (3%) | |
| CML/MPD | 1 (5%) | 2 (6%) | |
| Hodgkin lymphoma | 3 (14%) | 0 (0%) | |
| Lymphoma | 3 (14%) | 4 (13%) | |
| Disease risk index | |||
| Intermediate | 13 (59%) | 11 (35.5%) | .233 |
| High | 7 (32%) | 15 (48.4%) | |
| Very high | 2 (9%) | 5 (16.1%) | |
| Conditioning regimen | |||
| Flu/Mel/ATG | 15 (68%) | 17 (55%) | .3997 |
| Flu/ Bu/+/− Clo/ATG/TBI 200 cGy | 7 (32%) | 14 (45%) | |
| Cryopreserved TNC dose (×107/kg), median (range) | |||
| Unmanipulated cord | 3.124 (2.23-5.9) | — | |
| Fucosylated cord | 2.38 (1.82-3.33) | — | |
| Total | 5.51 (4.3-8.1) | 4.78 (1.96-8.94) | .005 |
| Cryopreserved CD34 dose (×105/kg), median (range) | |||
| Unmanipulated cord | 1.15 (0.43-3.27) | — | |
| Fucosylated cord | 0.92 (0.28-2.09) | — | |
| Total | 2.38 (0.78-4.48) | 1.82 (0.39-9.92) | .154 |
| Infused TNC dose (×107/kg), median (range) | |||
| Unmanipulated cord | 2.59 (1.54-4.75) | — | |
| Fucosylated cord | 1.75 (0.64-2.5) | — | |
| Total | 4.26 (2.73-6.3) | 3.72 (1.5-7.0) | .220 |
| Donor HLA matchUnmanipulated CB unit | |||
| 4/6 | 11 (50%) | — | |
| 5/6 | 11 (50%) | — | |
| Fucosylated CB unit | |||
| 6/6 | 1 (5%) | — | |
| 5/6 | 10 (45%) | — | |
| 4/6 | 11 (50%) | — | |
| Combined CB units | |||
| 6/6 and 5/6 | 1 (4.5%) | 0 (0%) | .584 |
| 5/6 and 5/6 | 8 (36.3%) | 9 (29%) | |
| 5/6 and 4/6 | 4 (18.2%) | 6 (19.4%) | |
| 4/6 and 4/6 | 9 (40.9%) | 16 (51.6%) |
ALL, acute lymphoblastic leukemia; AML, acute myeloid leukemia; ATG, anti-thymocyte globulin; Bu, busulfan; CLL, chronic lymphoblastic leukemia; Clo, clofarabine; CML, chronic myeloid leukemia; Flu, fludarabine; MDS, myelodysplastic syndromes; Mel, melphalan; MPD, myeloproliferative disease; TBI, total body irradiation; —, data were not available or not applicable to historical controls.
Results
Development of FT-VI treatment of clinical use
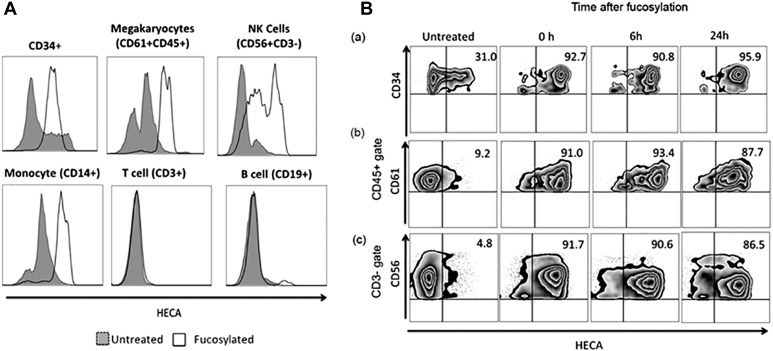
Optimal conditions for fucosylation of the CB-derived mononuclear cells consisted of a 30-minute incubation at room temperature with FT-VI (100 mU/mL) in Hanks balanced salt solution containing 1% HSA and 1 mM GDP β-fucose. The addition of manganese, which was originally recommended by the manufacturer, did not add to the already maximal fucosylation achieved by FT-VI treatment alone27 and was deleted from the procedure. Maximal fucosylation of CD34+ cells was achieved over a range of HSPC concentrations in the CB preparation (8-64 × 106 cells/mL) without a loss of enzyme efficiency, an advantage allowing considerable flexibility in the procedure independent of cell number. Indeed, the median expression of fucosylated CD34+ cells in the study cohort’s CB units was only 36.5% (95% CI, 31.5-41.5%) before FTVI treatment, but increased to 98.9% (95% CI, 98.2-99.6%) after treatment (Figure 2A, top left). FTVI treatment also led to substantial fucosylation of CD61+ megakaryocytes, CD14+ monocytes, and CD56+CD3− NK cells, whereas CD3+ T cells and CD19+ B cells were not fucosylated at all following this treatment (Figure 2A, all remaining panels). The CD34+, CD56+, and CD61+ subsets remained stably fucosylated for up to 24 hours after treatment as assessed by HECA-452 staining (Figure 2Ba-Bc).
Figure 2.
Extent and durability of fucosylation of CB cells. (A) Mean fluorescence intensity of fucosylated (white) and untreated (gray) CB cells. The degree of fucosylation (measured with the HECA antibody) on CB-CD34+ cells, megakaryocytes (CD61+CD45+), NK cells (CD3−CD56+), and monocytes (CD14+) was increased compared with that of the corresponding untreated cells (gray), whereas neither T cells (CD3+) nor B cells (CD19+) showed increased fucosylation. (B) Stable HECA expression (fucosylation) on (a) CD34+ cells, (b) megakaryocytes (CD45+CD61+), and (c) NK cells (CD3−CD56+) for up to 24 hours after the fucosylation procedure.
Patients
Between August 2012 and January 2014, 22 patients with a median age of 42 years (range, 20-68 years) were enrolled and treated in this study (Table 1). Their presenting characteristics, underlying diagnoses, donor HLA compatibility, and conditioning regimens did not differ significantly from findings in 31 historical controls who had undergone double unmanipulated CBT at this center. By standard risk index criteria,35 59% of the study cohort had intermediate-risk disease, 32% high-risk disease, and 9% very-high-risk disease, and 64.5% of the control group had high or very high risk. One half of the study patients had a comorbidity score36 of 3 or higher, whereas 22% had a score of 1 or 2. Table 1 also summarizes cryopreserved TNCs and CD34 doses in both the groups. The study group received a median of 2.38 × 107 TNCs/kg (range, 1.82-3.33 TNCs/kg) in the fucosylated unit and 3.12 × 107 TNCs/kg (range, 2.23-5.90 TNCs/kg) in the unmanipulated unit. Although the total dose of TNCs (5.5 × 107 TNCs/kg; range, 4.29-8.05 TNCs/kg) was statistically higher in the study population compared with the controls (4.8 × 107 TNCs/kg; range, 1.96-8.94 TNCs/kg), the differences were clinically insignificant. Further, there were no differences in the CD34 doses among the groups. The study patients received a median of 0.92 × 105 CD34+ cells/kg (range, 0.28-2.09 cells/kg) in the fucosylated unit and 1.15 × 105 CD34+ cells/kg (range, 0.43-3.27 cells/kg) in the unmanipulated unit, for a total dose of 2.37 × 105 CD34+ cells/kg (range, 0.78-4.5 cells/kg), which was similar to total CD34 cell dose in the controls (1.82 × 105 CD34+ cells/kg; (range, 0.39-9.92 cells/kg).
Neutrophil and platelet engraftment
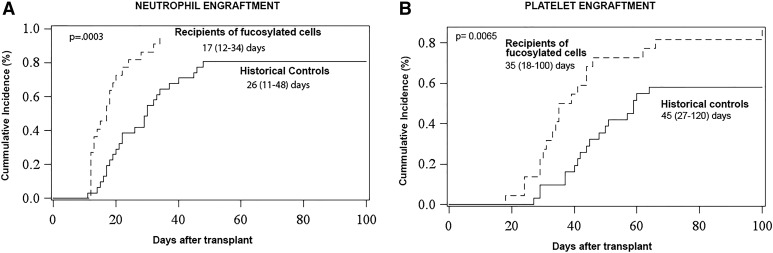
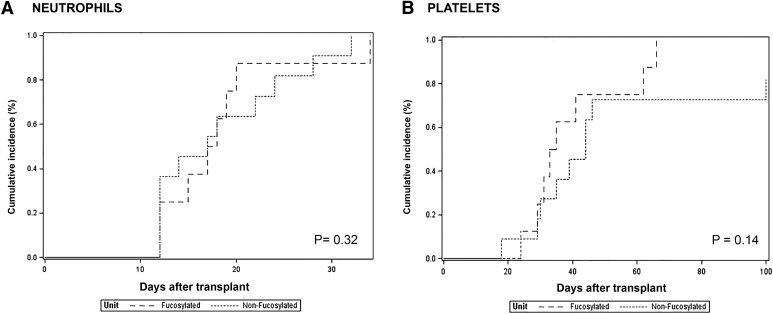
One patient died of bacterial sepsis on day 23 without engrafting neutrophils or platelets, and one developed secondary graft failure on the day after initial engraftment (day 14 after transplantation) and was rescued with previously stored autologous peripheral blood progenitor cells. Among the 20 remaining patients, the median time to neutrophil recovery was 17 days (range, 12-34 days), which was significantly shorter than the 26 days (range, 11-48 days) for our historical control group (P = .0023). The median time to platelet engraftment in the study cohort was 35 days (range, 18-100 days) compared with 45 days (range, 27-120 days) for the historical controls (P = .0520). At 30 days after transplantation, the cumulative incidence of neutrophil engraftment in the study cohort (Figure 3A) was 95.5% (95% CI, 40.8-99.8%) vs 81.7% (95% CI, 60.6-91.2%) in controls (P = .0003) for overall comparison. The cumulative incidence of platelet engraftment at 65 days (Figure 3B) was likewise increased over the control group: 86.4% (95% CI, 54.54-96.52%) vs 58.1% (95% CI, 38.4-73.4%; P = .0065). Within the limits of the small sample sizes, there was no difference in the time to or cumulative incidence of engraftment when the analysis was based on the conditioning regimens that were used (data not shown).
Figure 3.
Accelerated engraftment after CB cell fucosylation. (A) Cumulative incidence of neutrophil engraftment at 30 days after transplant was 95.5% (95% CI, 40.8-99.8%) in the study group compared with 81.65% (95% CI, 60.56-91.19%) in controls (P = .0003). (B) Cumulative incidence of platelet engraftment at 65 days was 86.36% (95% CI, 54.54-96.52%) in the study group compared with 58.07% (95% CI, 38.41-73.43%) in controls (P = .0065).
We also asked whether the time to neutrophil or platelet engraftment correlated with key properties of the 2 CB units received by each patient, including the infused doses (per kilogram) of TNCs, CD34+ cells, CD34+CLA+ cells, and CD45+CLA+ cells. The results were analyzed with a Cox proportional hazards model, first by individual CB unit and then by the combined results for both units. The parameters evaluated included the per kilogram doses of TNCs, CD34+ cells, CD34+CLA+ cells, CD45+ cells, CD45+CLA+ cells, and CD3+ cells. The only significant predictors of a faster time to neutrophil engraftment were the sums in the 2 units of (1) CD34+ cell doses (HR, 2.602; 95% CI, 1.106-6.12%; P = .0285), (2) CD34+CLA+ cell doses (HR, 3.7503; 95% CI, 1.21-1.67%; P = .0225), and (3) CD45+CLA+ cell doses (HR, 5.82; 95% CI, 1.8-18.8%; P = .0033). The sole significant predictor of a faster time to platelet engraftment was the sum of the CD34+ cell doses (HR, 2.65; 95% CI, 1.19-5.86%; P = .0162).
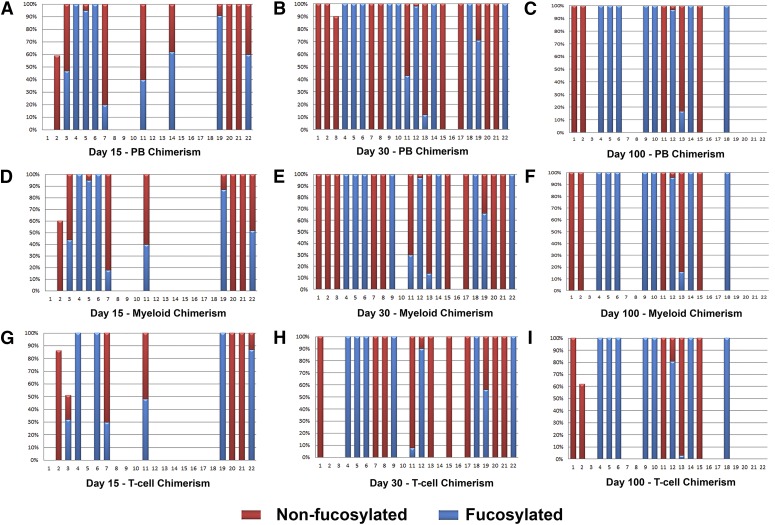
Chimerism and the dominating CB unit
Twenty evaluable patients had complete (100%) donor engraftment with one or both CB units in the leukocyte, T-cell, and myeloid cell compartments of peripheral blood at day 30 after transplantation (Figure 4). Eight of these patients (40%) had evidence of hematopoiesis solely from the unmanipulated CB unit, whereas in 8 others (40%), it stemmed solely from the fucosylated CB unit. Four patients (20%) had hematopoiesis derived from both units at day 30, with 2 of the 4 having a single predominant CB unit predominate at later time points (1 fucosylated and 1 unmanipulated). There was no difference between the cumulative incidence curves for neutrophil or platelet engraftment, whether patients engrafted from the unmanipulated or the fucosylated CB unit (Figure 5A-B).
Figure 4.
Contributions of fucosylated (blue) and unfucosylated (red) CB units to chimerism on days 15, 30, and 100, analyzed with polymerase chain reaction primer sets that flanked microsatellite repeats. Numbers beneath the graph represent individual patients. (A-C, D-F, and G-I) Results for the peripheral blood (PB), myeloid, and T-cell compartments, respectively.
Figure 5.
Times to engraftment by dominant CB unit. Cumulative incidence curves for either (A) neutrophils or (B) platelets did not differ, whether the dominant unit was fucosylated (n = 8) or not (n = 12). See also Figure 4.
Toxicity and survival
All CB cell infusions were well tolerated. The 100-day cumulative incidence of grade II to IV acute GVHD was 40.9% (95% CI, 20.18-60.71%) in the study population compared with 38.71% (95% CI, 21.67-55.49%) in controls (P = .86), whereas that of grade III or IV GVHD was 9.1% (95% CI, 1.5-25.6%) vs 12.9% (95% CI, 3.97-27.26%) in controls (P = .66). The overall cumulative incidence of chronic GVHD in the study group was 5% (95% CI, 0.3-19.55%) vs 22.51% (95% CI, 8.48-40.61%) in controls (P = .17). There were no other serious adverse events that appeared related to the CB cell infusions. At a median follow-up of 8 months (range, 3-20 months) for surviving patients, 10 of these 22 high-risk patients remained alive (Table 2). The causes of death included infections (5), chemotherapy-related organ toxicities (3), relapse (3), and GVHD (1).
Table 2.
Survival and GVHD analyses
| Study group (n = 22) | Controls (n = 31) | P value | |
|---|---|---|---|
| No. alive | 10 | 5 | |
| No. alive, progression free | 7 | 5 | |
| Median (range) days of follow-up, days | 55 (103-593) | 210 (42-1055) | .53 |
| GVHD, cumulative incidence (95% CI) | |||
| Acute grade II-IV GVHD at 100 days | 40.91% (20.18-60.71%) | 38.71% (21.67-55.49%). | .86 |
| Acute grade III-IV GVHD at 100 days | 9.1% (1.5-25.6%) | 12.90% (3.97-27.26%). | .66 |
| Chronic GVHD overall | 5% (0.30-19.55%) | 22.51% (8.48-40.61%). | .17 |
Discussion
In this trial we sought to test the safety and feasibility of infusions of fucosylated CB hematopoietic progenitors as a means to improve neutrophil and platelet engraftment in patients undergoing CBT for advanced cancer. We first demonstrate the efficiency and efficacy of ex vivo incubation of CB cells with the enzyme FT-VI and its substrate, GDP-fucose, for 30 minutes at room temperature for increasing the surface fucosylation of CD34+ cells. When combined with a second, unmanipulated CB unit, the fucosylated unit was associated with rapid engraftment of neutrophils (median, 17 days) and platelets (median, 35 days) following myeloablative therapy. Indeed, this outcome was clearly improved over that in our historical control group (26 days for neutrophils and 45 days for platelets) and over results reported by others for double unmanipulated CBT.9-11,37 Neutrophil and platelet engraftment times similar to ours were attained by Delaney et al,14 Horwitz et al17 and Wagner et al,38 who expanded 1 of 2 CB units ex vivo using systems that require 14 to 21 days of culture with cytokines prior to infusion. Our findings agree well with the predictions of preclinical studies,25,27 with the exception of a report by Hidalgo and Frenette.26 Although demonstrating marked enhancement of FTVI-treated CD34+ cells in their interaction with the bone marrow microvasculature, these authors were unable to show improved homing into the marrow. The basis for this discrepancy is unclear, but may reflect the type of homing assays used or the relatively low numbers of transplanted CD34+ cells.
We attribute the accelerated engraftment of neutrophils and platelets in our study to several factors. First, surface fucosylation of essentially all CB-derived CD34+ HSPCs (Figure 2) likely increased the proportion of infused cells able to interact with E- and P-selectins expressed on vascular endothelial cells and therefore to be recruited to bone marrow microenvironmental niches. Second, the substantial degree of fucosylation of NK cells may have boosted engraftment through an effect that was initially described by a “hybrid resistance” model and was shown to be mediated through the classical “missing self-recognition” phenomenon.39,40 Third, the activity of other accessory cells, such as CD14+ monocytes, which were highly fucosylated after treatment with FT-VI, may have facilitated the generation of neutrophils and platelets from HSPCs.41
A surprising outcome in this trial was that the unfucosylated CB unit dominated in half of the patients studied, yet the times to engraftment of neutrophils and platelets were essentially the same in both groups (Figure 4). This observation contrasts with that of Cutler et al,42 who reported a contribution to engraftment from prostaglandin E2-treated CB cells in 83% (10 of 12) of their patients. One explanation is that we evaluated the patients for chimerism too late and missed an early wave of engraftment, when the effects of the fucosylated unit might have been readily detected. We are now evaluating chimerism as soon as the patients engraft, so that in the future we should be able to determine whether the engraftment of CB occurs early and is then replaced by the unmanipulated unit, as we have seen with ex vivo expanded CB.15 Another possibility is that even though the fucosylated unit was not detected, it may have facilitated the engraftment of the unmanipulated CB preparation. In this alternative, specific accessory cell populations could be activated through passive mechanisms of increased cell flow, resulting in a streaming effect whereby the unfucosylated cells traffic with the fucosylated cells into the hematopoietic niche and then preferentially home to the marrow.41 Higher doses of CD45+CLA+ cells were indeed a predictor of faster engraftment, suggesting that the fucosylation of accessory cells not expressing CD34 may be important. It is also conceivable that increased homing of the fucosylated cells to the marrow results in increased expression of integrins and other adhesion molecules in the microenvironment, thus further promoting engraftment of the unmanipulated unit.
In addition to improving neutrophil and platelet engraftment, we demonstrate that CB fucosylation in the context of double CBT is safe, with no serious infusion-related toxicity seen over the extended follow-up period. In particular, there was no increase in the incidence of acute or chronic GVHD in the study population. Similarly, within the limitations of a phase 1 trial, enforced fucosylation of HSPCs was not associated with an increased mortality rate. Poor survival noted in the control group is a reflection of their underlying high risk disease, as about two-thirds of the patients had high- to very-high-risk disease.
In summary, we showed that ex vivo fucosylation of CB cells is a rapid, logistically straightforward, and safe procedure that appears to improve times to neutrophil and platelet engraftment in high-risk patients with hematologic malignancies who have undergone double CBT. We recognize that the use of historical controls and a relatively small sample size hindered our ability to identify factors that may predispose patients to engraft predominantly with fucosylated or nonfucosylated unit. With ongoing recruitment of patients, we should be able to understand and overcome this restriction. Finally, because CB cell expansion by mesenchymal stromal cell coculture also results in shorter times to neutrophil and platelet engraftment,15 we suggest that fucosylation of ex vivo-expanded CB cells may further accelerate engraftment of these cells, a possibility warranting both clinical and mechanistic investigation.
Acknowledgments
This work was supported in part by National Institutes of Health National Cancer Institute grants RO1 CA061508-19 and PO1 CA148600-02, Cancer Prevention Research Institute of Texas grant RO1 RP100469, and Anderson Cancer Center core grant CA016672.
Footnotes
There is an Inside Blood Commentary on this article in this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Authorship
Contribution: U.P. contributed to experimental design and wrote the manuscript; R.S.M. contributed to data analysis and figures and wrote the manuscript; K.R. contributed to experimental design, enrolled patients in the study, and wrote the manuscript; P.F. analyzed data and wrote the statistical section of the manuscript; K.K. performed and provided data for the ex vivo experiments; D.M., I.M., M.A., I.K., E.Y., L.J.N.C., and C.B. analyzed data and wrote the manuscript; B.O., C.H., A.O, S.P., N.S., P.K., M.d.L., P.T., R.E.C., Y.N., B.S.A., A.A., R.B.J., M.H.Q., Q.B., S.C., S.A., P.A., and J.J.M. enrolled patients in the study and monitored clinical responses; D.B. provided patient-related data and wrote the manuscript; J.C. provided clinical data; M.T. supervised the ex vivo fucosylation of cells; L.M. and S.W. contributed new vital reagents; P.S. and S.R. performed preclinical ex vivo experiments; P.A.Z.-M. contributed to experimental design; and E.J.S. conceptualized and supervised the research, ensured compliance with regulatory requirements for the clinical trial, and wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Elizabeth J. Shpall, The University of Texas MD Anderson Cancer Center, Stem Cell and Transplantation & Cellular Therapy, 1515 Holcombe Blvd, Unit Number 423, Houston, TX 77030; e-mail: eshpall@mdanderson.org.
References
- 1.Ballen KK, Koreth J, Chen YB, Dey BR, Spitzer TR. Selection of optimal alternative graft source: mismatched unrelated donor, umbilical cord blood, or haploidentical transplant. Blood. 2012;119(9):1972–1980. doi: 10.1182/blood-2011-11-354563. [DOI] [PubMed] [Google Scholar]
- 2.Copelan EA. Hematopoietic stem-cell transplantation. N Engl J Med. 2006;354(17):1813–1826. doi: 10.1056/NEJMra052638. [DOI] [PubMed] [Google Scholar]
- 3.Gragert L, Eapen M, Williams E, et al. HLA match likelihoods for hematopoietic stem-cell grafts in the U.S. registry. N Engl J Med. 2014;371(4):339–348. doi: 10.1056/NEJMsa1311707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Laughlin MJ, Barker J, Bambach B, et al. Hematopoietic engraftment and survival in adult recipients of umbilical-cord blood from unrelated donors. N Engl J Med. 2001;344(24):1815–1822. doi: 10.1056/NEJM200106143442402. [DOI] [PubMed] [Google Scholar]
- 5.Rubinstein P, Carrier C, Scaradavou A, et al. Outcomes among 562 recipients of placental-blood transplants from unrelated donors. N Engl J Med. 1998;339(22):1565–1577. doi: 10.1056/NEJM199811263392201. [DOI] [PubMed] [Google Scholar]
- 6.Ballen KK, Spitzer TR. The great debate: haploidentical or cord blood transplant. Bone Marrow Transplant. 2011;46(3):323–329. doi: 10.1038/bmt.2010.260. [DOI] [PubMed] [Google Scholar]
- 7.Rocha V, Labopin M, Sanz G, et al. Acute Leukemia Working Party of European Blood and Marrow Transplant Group; Eurocord-Netcord Registry. Transplants of umbilical-cord blood or bone marrow from unrelated donors in adults with acute leukemia. N Engl J Med. 2004;351(22):2276–2285. doi: 10.1056/NEJMoa041469. [DOI] [PubMed] [Google Scholar]
- 8.Komanduri KV, St John LS, de Lima M, et al. Delayed immune reconstitution after cord blood transplantation is characterized by impaired thymopoiesis and late memory T-cell skewing. Blood. 2007;110(13):4543–4551. doi: 10.1182/blood-2007-05-092130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barker JN, Fei M, Karanes C, et al. Results of a prospective multicentre myeloablative double-unit cord blood transplantation trial in adult patients with acute leukaemia and myelodysplasia. Br J Haematol. 2014;168(3):405–412. doi: 10.1111/bjh.13136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barker JN, Weisdorf DJ, DeFor TE, et al. Transplantation of 2 partially HLA-matched umbilical cord blood units to enhance engraftment in adults with hematologic malignancy. Blood. 2005;105(3):1343–1347. doi: 10.1182/blood-2004-07-2717. [DOI] [PubMed] [Google Scholar]
- 11.Scaradavou A, Brunstein CG, Eapen M, et al. Double unit grafts successfully extend the application of umbilical cord blood transplantation in adults with acute leukemia. Blood. 2013;121(5):752–758. doi: 10.1182/blood-2012-08-449108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schmitz N, Beksac M, Hasenclever D, et al. European Group for Blood and Marrow Transplantation. Transplantation of mobilized peripheral blood cells to HLA-identical siblings with standard-risk leukemia. Blood. 2002;100(3):761–767. doi: 10.1182/blood-2001-12-0304. [DOI] [PubMed] [Google Scholar]
- 13.Horowitz MM, Rowlings PA, Passweg JR. Allogeneic bone marrow transplantation for CML: a report from the International Bone Marrow Transplant Registry. Bone Marrow Transplant. 1996;17(Suppl 3):S5–S6. [PubMed] [Google Scholar]
- 14.Delaney C, Heimfeld S, Brashem-Stein C, Voorhies H, Manger RL, Bernstein ID. Notch-mediated expansion of human cord blood progenitor cells capable of rapid myeloid reconstitution. Nat Med. 2010;16(2):232–236. doi: 10.1038/nm.2080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.de Lima M, McNiece I, Robinson SN, et al. Cord-blood engraftment with ex vivo mesenchymal-cell coculture. N Engl J Med. 2012;367(24):2305–2315. doi: 10.1056/NEJMoa1207285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fares I, Chagraoui J, Gareau Y, et al. Cord blood expansion. Pyrimidoindole derivatives are agonists of human hematopoietic stem cell self-renewal. Science. 2014;345(6203):1509–1512. doi: 10.1126/science.1256337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Horwitz ME, Chao NJ, Rizzieri DA, et al. Umbilical cord blood expansion with nicotinamide provides long-term multilineage engraftment. J Clin Invest. 2014;124(7):3121–3128. doi: 10.1172/JCI74556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Katayama Y, Hidalgo A, Furie BC, Vestweber D, Furie B, Frenette PS. PSGL-1 participates in E-selectin-mediated progenitor homing to bone marrow: evidence for cooperation between E-selectin ligands and alpha4 integrin. Blood. 2003;102(6):2060–2067. doi: 10.1182/blood-2003-04-1212. [DOI] [PubMed] [Google Scholar]
- 19.Sackstein R. Engineering cellular trafficking via glycosyltransferase-programmed stereosubstitution. Ann N Y Acad Sci. 2012;1253:193–200. doi: 10.1111/j.1749-6632.2011.06421.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ley K, Laudanna C, Cybulsky MI, Nourshargh S. Getting to the site of inflammation: the leukocyte adhesion cascade updated. Nat Rev Immunol. 2007;7(9):678–689. doi: 10.1038/nri2156. [DOI] [PubMed] [Google Scholar]
- 21.Frenette PS, Subbarao S, Mazo IB, von Andrian UH, Wagner DD. Endothelial selectins and vascular cell adhesion molecule-1 promote hematopoietic progenitor homing to bone marrow. Proc Natl Acad Sci USA. 1998;95(24):14423–14428. doi: 10.1073/pnas.95.24.14423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mazo IB, Gutierrez-Ramos JC, Frenette PS, Hynes RO, Wagner DD, von Andrian UH. Hematopoietic progenitor cell rolling in bone marrow microvessels: parallel contributions by endothelial selectins and vascular cell adhesion molecule 1. J Exp Med. 1998;188(3):465–474. doi: 10.1084/jem.188.3.465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Carlow DA, Gossens K, Naus S, Veerman KM, Seo W, Ziltener HJ. PSGL-1 function in immunity and steady state homeostasis. Immunol Rev. 2009;230(1):75–96. doi: 10.1111/j.1600-065X.2009.00797.x. [DOI] [PubMed] [Google Scholar]
- 24.Hidalgo A, Weiss LA, Frenette PS. Functional selectin ligands mediating human CD34(+) cell interactions with bone marrow endothelium are enhanced postnatally. J Clin Invest. 2002;110(4):559–569. doi: 10.1172/JCI14047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Xia L, McDaniel JM, Yago T, Doeden A, McEver RP. Surface fucosylation of human cord blood cells augments binding to P-selectin and E-selectin and enhances engraftment in bone marrow. Blood. 2004;104(10):3091–3096. doi: 10.1182/blood-2004-02-0650. [DOI] [PubMed] [Google Scholar]
- 26.Hidalgo A, Frenette PS. Enforced fucosylation of neonatal CD34+ cells generates selectin ligands that enhance the initial interactions with microvessels but not homing to bone marrow. Blood. 2005;105(2):567–575. doi: 10.1182/blood-2004-03-1026. [DOI] [PubMed] [Google Scholar]
- 27.Robinson SN, Simmons PJ, Thomas MW, et al. Ex vivo fucosylation improves human cord blood engraftment in NOD-SCID IL-2Rγ(null) mice. Exp Hematol. 2012;40(6):445–456. doi: 10.1016/j.exphem.2012.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zarbock A, Ley K, McEver RP, Hidalgo A. Leukocyte ligands for endothelial selectins: specialized glycoconjugates that mediate rolling and signaling under flow. Blood. 2011;118(26):6743–6751. doi: 10.1182/blood-2011-07-343566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ohmori K, Fukui F, Kiso M, et al. Identification of cutaneous lymphocyte-associated antigen as sialyl 6-sulfo Lewis X, a selectin ligand expressed on a subset of skin-homing helper memory T cells. Blood. 2006;107(8):3197–3204. doi: 10.1182/blood-2005-05-2185. [DOI] [PubMed] [Google Scholar]
- 30.Sutherland DR, Anderson L, Keeney M, Nayar R, Chin-Yee I International Society of Hematotherapy and Graft Engineering. The ISHAGE guidelines for CD34+ cell determination by flow cytometry. J Hematother. 1996;5(3):213–226. doi: 10.1089/scd.1.1996.5.213. [DOI] [PubMed] [Google Scholar]
- 31.Gooley TA, Leisenring W, Crowley J, Storer BE. Estimation of failure probabilities in the presence of competing risks: new representations of old estimators. Stat Med. 1999;18(6):695–706. doi: 10.1002/(sici)1097-0258(19990330)18:6<695::aid-sim60>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 32.Przepiorka D, Weisdorf D, Martin P, et al. 1994 Consensus Conference on Acute GVHD Grading. Bone Marrow Transplant. 1995;15(6):825–828. [PubMed] [Google Scholar]
- 33.Filipovich AH, Weisdorf D, Pavletic S, et al. National Institutes of Health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. Diagnosis and staging working group report. Biol Blood Marrow Transplant. 2005;11(12):945–956. doi: 10.1016/j.bbmt.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 34.Fine JGR. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94(446):496–509. [Google Scholar]
- 35.Armand P, Gibson CJ, Cutler C, et al. A disease risk index for patients undergoing allogeneic stem cell transplantation. Blood. 2012;120(4):905–913. doi: 10.1182/blood-2012-03-418202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sorror ML. How I assess comorbidities before hematopoietic cell transplantation. Blood. 2013;121(15):2854–2863. doi: 10.1182/blood-2012-09-455063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chen YB, Aldridge J, Kim HT, et al. Reduced-intensity conditioning stem cell transplantation: comparison of double umbilical cord blood and unrelated donor grafts. Biol Blood Marrow Transplant. 2012;18(5):805–812. doi: 10.1016/j.bbmt.2011.10.016. [DOI] [PubMed] [Google Scholar]
- 38.Wagner JE, Brunstein CG, McKenna D, et al. Safety and exploratory efficacy of ex vivo expanded umbilical cord blood (UCB) hematopoietic stem and progenitor cells (HSPC) using cytokines and stem-regenin 1 (SR1): interim results of a phase 1/2 dose escalation clinical study Blood. 2014;124(21). Abstract 698. [Google Scholar]
- 39.Barao I, Murphy WJ. The immunobiology of natural killer cells and bone marrow allograft rejection. Biol Blood Marrow Transplant. 2003;9(12):727–741. doi: 10.1016/j.bbmt.2003.09.002. [DOI] [PubMed] [Google Scholar]
- 40.Ruggeri L, Capanni M, Urbani E, et al. Effectiveness of donor natural killer cell alloreactivity in mismatched hematopoietic transplants. Science. 2002;295(5562):2097–2100. doi: 10.1126/science.1068440. [DOI] [PubMed] [Google Scholar]
- 41.Fugier-Vivier IJ, Rezzoug F, Huang Y, et al. Plasmacytoid precursor dendritic cells facilitate allogeneic hematopoietic stem cell engraftment. J Exp Med. 2005;201(3):373–383. doi: 10.1084/jem.20041399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cutler C, Multani P, Robbins D, et al. Prostaglandin-modulated umbilical cord blood hematopoietic stem cell transplantation. Blood. 2013;122(17):3074–3081. doi: 10.1182/blood-2013-05-503177. [DOI] [PMC free article] [PubMed] [Google Scholar]