Abstract
Purpose:
To determine the sensitivity and specificity of anterior and posterior corneal elevation parameters as determined by Orbscan II (Bausch and Lomb, Rochester, NY, USA) in discriminating between (sub) clinical keratoconus (KCN) and normal corneas.
Methods:
This prospective case-control study included 28 eyes with subclinical KCN, 65 with clinical KCN and 141 normal corneas. Anterior and posterior corneal elevation was measured and compared in the central 5-mm corneal zone using Orbscan II.
Results:
Receiver operating curves (ROC) curve analyses for posterior corneal elevation showed predictive accuracy in both KCN and subclinical KCN with an area under the curve (AUC) of 0.97 and 0.69, respectively while optimal cutoff points were 51 μm for KCN and 35 μm for subclinical KCN. These values were associated with sensitivity and specificity of 89.23% and 98.58%, respectively, for KCN; and 50.00% and 88.65% for subclinical KCN. ROC curve analyses for anterior corneal elevation showed predictive accuracy in both KCN and subclinical KCN with AUC of 0.97 and 0.69, respectively while optimal cutoff points were 19 μm for KCN and 16 μm for subclinical KCN. These values were associated with sensitivity and specificity of 93.85% and 97.16%, respectively, for KCN; and 60.71% and 87.94% for subclinical KCN.
Conclusion:
Anterior and posterior corneal elevation data obtained by Orbscan II can well discriminate between KCN and normal corneas, however the reliability of their indices is lower in differentiating subclinical KCN from normal cases.
Keywords: Corneal Elevation, Keratoconus, Orbscan, Receiver Operating Curve, Sensitivity, Specificity
INTRODUCTION
Keratoconus (KCN) is a bilateral, non-inflammatory and usually progressive ectatic corneal disorder characterized by thinning and protrusion of the central cornea, leading to decreased vision as a result of myopia and irregular astigmatism.[1,2,3,4] Biomicroscopic examination and placido disk–based corneal topography are widely used methods for the diagnosis of KCN. Placido disk–based corneal topography is a highly sensitive and specific diagnostic tool, however; it only evaluates the anterior surface of the cornea. With the advent of scanning slit topography and rotating Scheimpflug imaging, anterior and posterior corneal surface elevation measurements and curvature map detection became possible.
Height data can directly assess protrusion; they differ from curvature map assessments of relative distortion of the cornea, and can provide useful diagnostic information in KCN. Current diagnostic concern in the management of KCN is detection of subclinical KCN which is critical prior to keratorefractive procedures considering the high prevalence of KCN among corneal refractive surgery candidates and the fact that the condition is the main cause of keratectasia after refractive surgeries.[4,5,6]
This study was designed to evaluate the sensitivity and specificity of anterior and posterior corneal elevation data obtained by Orbscan IIz (Bausch and Lomb, Rochester, NY, USA) in differentiating subclinical and clinical KCN from normal corneas.
METHODS
This prospective, case-control study was comprised of 118 refractive surgery candidates (a total of 234 eyes) aged 19-48 years with subclinical KCN, clinical KCN and normal corneas. The study subjects were consecutive patients examined at the Cornea and Refractive Surgery Service at Labbafinejad Medical Center, Tehran, Iran between January 2010 and December 2010. The study was performed in accordance with ethical standards of the Declaration of Helsinki.
All subjects underwent slit-lamp biomicroscopy, funduscopy, retinoscopy, keratometry and Placido disk–based videokeratography, and were subsequently divided into three groups including subclinical KCN, clinical KCN and normal according to slit lamp examination (conical protrusion, stromal thinning, Fleischer ring, and Vogt's striae) and placido disk–based topography (TMS-4, TOMEY Co., Nagoya, Japan) findings.
Slit lamp and placido disk–based videokeratography features were categorized into major and minor criteria. Major criteria were the presence of Vogt's striae and Fleischer ring of at least 2 mm detected by slit lamp, skewed radial axis (SRAX) index exceeding 20°, keratoconus prediction index (KPI) >0.3, keratoconus severity index (KSI) >30%, and keratoconus index (KCI) reported as an abnormal topographic pattern. Minor criteria included asymmetric bow-tie pattern without SRAX, inferior steepening, KSI of 15% to 30%, and KPI of 23% to 30%. KCN was defined by the presence of two major, or one major and two minor criteria. Subclinical KCN was described in the presence of one major topographic or two minor criteria. Subjects without any major or minor criteria were considered as normal.
Height data in terms of anterior and posterior corneal elevation maps were obtained for both eye of each patient in the central 3- and 5-mm zone using the Orbscan IIz slit beam topography system (Bausch and Lomb, Rochester, NY, USA). Anterior and posterior corneal elevation values in subclinical and clinical KCN were compared to that of normal corneas in separate analyses. In order to distinguish clinical and subclinical KCN from normal eyes, receiver operating characteristic (ROC) curves were generated and areas under the curves (AUC) were calculated for anterior and posterior corneal elevations. Optimal anterior and posterior elevation cutoff points, positive likelihood ratio [sensitivity/(1-specificity)], and negative likelihood ratio [(1-sensitivity)/specificity] for these cutoff points were also calculated.
We also compared the anterior and posterior corneal elevation data between the three groups using one-way analysis of variance (ANOVA) and post Hoc multiple comparison of Dunnett's T3. Box plot figures were employed to compare the distribution of anterior and posterior elevation in normal corneas, and eyes with subclinical or clinical keratoconus.
Statistical analysis was performed using STATA software (version 11, StataCorp, College Station, TX, USA) and SPSS software (version 17, SPSS Inc., Chicago, IL, USA). P values less than 0.05 were considered as statistically significant.
RESULTS
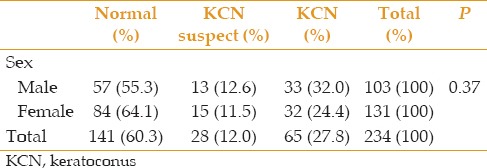
A total of 234 eyes of 118 patients were evaluated. The normal group (controls) consisted of 141 (60.30%) eyes, and the subclinical and clinical KCN (cases) included 28 (12%) and 65 (27.80%) eyes, respectively. Mean patient age was 29.22 ± 5.27 (range, 19-48) years overall, 29.32 ± 5.37 (range, 21-40) years in the subclinical KCN group, 29.46 ± 5.56 (range, 19-40) years in the KCN group and 29.21 ± 5.05 (range, 20-48) years in the normal group. One-way ANOVA yielded no significant difference between the three groups in terms of age (P = 0.95). Table 1 demonstrates the sex distribution of the study groups.
Table 1.
Sex distribution of KCN in the study groups
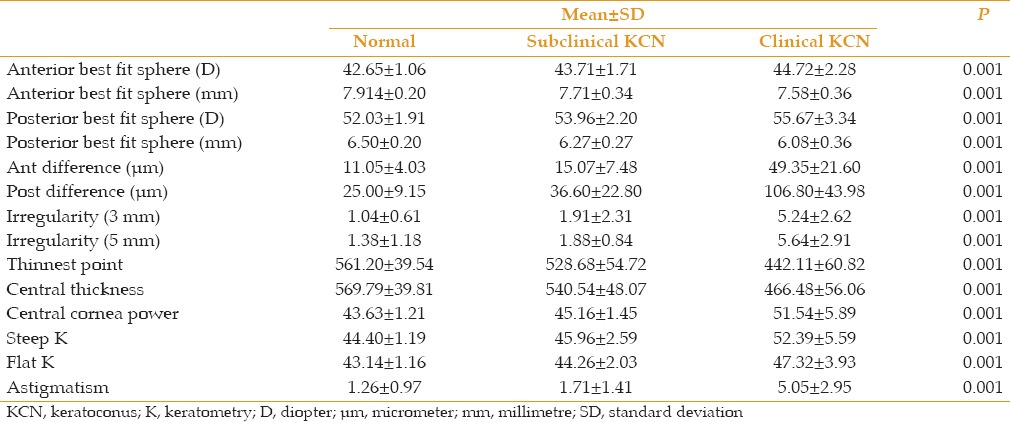
Mean anterior corneal elevations in both KCN (49.35 ± 21.60 μm; P = 0.001) and subclinical KCN (15.07 ± 7.48 μm; P = 0.028) groups were significantly higher as compared to the normal group (11.05 ± 4.03 μm). Mean posterior corneal elevations in both KCN (106.80 ± 43.72 μm; P = 0.001), and subclinical KCN (36.60 ± 22.80 μm; P = 0.038) groups were also significantly higher as compared to the normal group (25.00 ± 9.15 μm). The distribution of anterior and posterior corneal elevation in the three study groups is summarized in Figure 1.
Figure 1.

Distribution of anterior and posterior corneal elevation (microns) in normal corneas and eyes with subclinical and clinical keratoconus. KCN, keratoconus; Post, posterior elevation; Ant, anterior elevation.
Mean anterior and posterior corneal elevation data in the central 3- and 5-mm zone for subclinical KCN, clinical KCN and normal corneas are detailed in Table 2. One-way ANOVA revealed a significant difference between mean values of anterior and posterior corneal elevation (P-vale = 0.001).
Table 2.
Mean anterior and posterior corneal data measurements in the study groups
Figures 2 and 3 compare ROC curve analysis of anterior and posterior corneal elevation in subclinical and clinical KCN versus normal corneas. The ROC graphs showed that anterior and posterior corneal elevation could perfectly discriminate between KCN and normal corneas. AUC of posterior corneal elevation was 0.98 (95% confidence interval [CI], 0.94-0.99) for KCN and 0.698 (95% CI, 0.62-0.76) for subclinical KCN. AUC of anterior corneal elevation was 0.97 (95% CI, 0.937-0.987) for KCN and 0.69 (95% CI, 0.62-0.76) for subclinical KCN.
Figure 2.
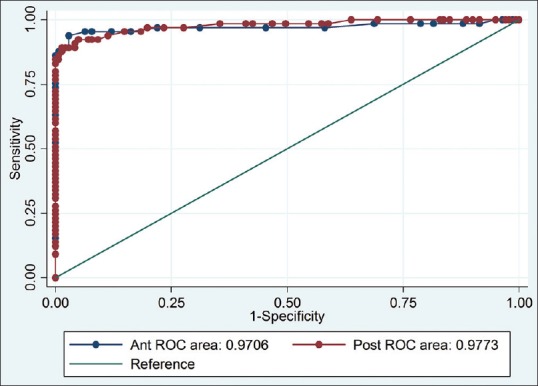
Receiver operator characteristic (ROC) curves of anterior and posterior corneal elevation for prediction of clinical keratoconus versus normal corneas.
Figure 3.
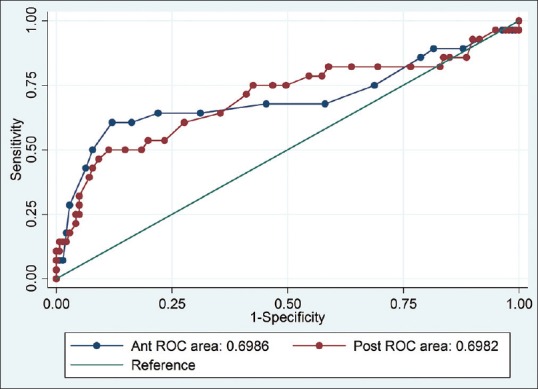
Receiver operator characteristic (ROC) curves of anterior and posterior corneal elevation for prediction of subclinical keratoconus versus normal corneas.
Tables 3 and 4 summarize the sensitivity, specificity, and positive and negative likelihood ratios (LRs) identified by cutoff points for anterior and posterior corneal elevation selected a priori in discriminating between eyes with clinical or subclinical KCN versus normal corneas. Based on Youden index, the optimal cutoff points measured in posterior elevation were 51 μm for KCN and 35 μm for subclinical KCN. These values were associated with sensitivity and specificity of 89.2% and 98.5%, respectively for KCN, and 50.0% and 88.6% for subclinical KCN. ROC curve analysis showed high overall predictive accuracy for anterior elevation in KCN as compared to subclinical KCN. The optimal cutoff points based on Youden index, were estimated to be 19 μm for KCN and 16 μm for subclinical KCN. These values were associated with sensitivity and specificity of 93.85% and 97.16%, respectively, for KCN, and 60.71% and 87.94% for subclinical KCN.
Table 3.
Sensitivity, specificity, positive and negative likelihood ratios and cutoff points for anterior corneal elevation in eyes with KCN or subclinical KCN versus normal corneas

Table 4.
Sensitivity, specificity, positive and negative likelihood ratios and cutoff points for posterior corneal elevation in eyes with KCN or subclinical KCN versus normal corneas

DISCUSSION
Diagnosis of subclinical KCN based on retinoscopic, biomicroscopic or keratometric features is more challenging as compared to KCN. The term subclinical KCN is applied to an early preclinical stage of the condition when the characteristic retinoscopic, biomicroscopic, or keratometric signs are absent but subtle topographic features similar to clinical KCN are evident on plasido-disk or elevation-based topography.[2,7,8,9]
The purpose of the current study was to determine the sensitivity and specificity of anterior and posterior corneal elevation data in discriminating subclinical or clinical KCN from normal corneas employing the Orbscan IIz scanning slit topographer. Mean age of our study participants was younger than those enrolled in the study by de Sanctis et al[2] There was no statistically significant difference between our three study groups in terms of gender; in other words, sex may not have a significant effect on detecting normal subjects from subclinical and clinical KCN.
We found mean posterior corneal elevation to be 106.80 ± 43.98 μm in KCN, 36.60 ± 22.80 μm in subclinical KCN, and 25.00 ± 9.15 μm in normal eyes. These values were significantly higher in both clinical and subclinical KCN than normal corneas, therefore posterior corneal elevation is a useful index for discriminating between these conditions. Mean posterior corneal elevation in normal corneas using Orbscan II has been reported to range from 28 to 30.47 μm by other authors.[9,10,11] Schlegel et al,[8] showed maximum central posterior elevation values to be 28.8 μm in keratoconus-suspect eyes and 20.6 μm in normal eyes while corresponding figures were 26 μm in normal eyes and 46 μm in keratoconus-suspect eyes in another study by Lim et al[12] Quisling et al reported that mean posterior corneal elevation was 48.50 μm in 36 eyes with clinical KCN employing the Orbscan II.[13] These discrepancies may be due to differences in patient characteristics.
In a study by de Sanctis et al,[2] mean posterior corneal elevation measured by pentacam was 100.7 ± 49.2 μm in KCN, 39.9 ± 15.0 μm in subclinical KCN, and 19.8 ± 6.37 μm in normal eyes. This discrepancy could be explained by different diagnostic tools in each study; scanning slit topography in the present study and rotating Scheimpflug imaging in de Sanctis study. Other probable explanation could be different age, sex and ethnicity in these two studies.
Measuring the anterior corneal elevation in our case groups (clinical and subclinical KCN) and comparing the results with that of in our controls (normal cornea) is noteworthy in the present study. In addition, we investigated the ability of these measures to distinguish clinical and subclinical KCN from normal individuals using the area under the ROC curve.
The current study also evaluated optimal cutoff points for anterior and posterior corneal elevations to discriminate clinical/subclinical KCN from normal eyes. A cutoff point of ≥ 51 μm was highly sensitive (89.23%) and specific (98.58%) for posterior corneal elevation and a cutoff point of ≥ 19 μm was highly sensitive (93.85%) and specific (97.16%) for anterior corneal elevation to differentiate clinical KCN from normal subjects. The optimal cutoff points for posterior elevation on Orbscan II topography used to differentiate clinical KCN and KCN suspect from normal corneas was 40 μm in studies by Rao et al[14] and Fam and Lim[10] A cutoff point of ≥ 42 μm in our study showed sensitivity of 92.31% and specificity of 95.04%. In de Sanctis et al[2] study employing Pentacam, the cutoff point of posterior elevation for detecting clinical KCN from normal subjects with high sensitivity (97.3%) and specificity (96.9%) was 35 μm. Therefore, the cutoff point of posterior elevation using Orbscan II topography seems to be higher than Pentacam rotating Scheimpflug camera.
Posterior elevation data was less powerful in discriminating subclinical KCN from normal eyes as compared to the discrimination between KCN and normal subjects; in the current study a cutoff point of ≥ 35 μm for subclinical KCN yielded sensitivity of 50.00% and specificity of 88.65%. Although it has been suggested that an increase in posterior elevation may be the earliest sign of subclinical KCN, placido disk–based videokeratography indices may be more sensitive in detecting subclinical KCN.[13] The present study revealed that the best anterior elevation cutoff point for discriminating subclinical KCN from normal eyes was ≥ 16 microns (μm) with sensitivity of 60.71% and specificity of 87.94%. These figures relatively less powerful for distinguishing normal from subclinical KCN subjects. Nevertheless, in eyes with subclinical KCN, the scanning slit topography (Orbscan II) may add further information to placido disk–based videokeratography data.
In conclusion, although anterior and posterior corneal elevation data measured by Orbscan II are very effective for discriminating clinical KCN from normal corneas, the performance of these measurements is lower for differentiating subclinical KCN from normal corneas. Thus, anterior and posterior elevation results should be combined with other data for evaluation of patients suspected of KCN.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Gharaibeh AM, Muhsen SM, AbuKhader IB, Ababneh OH, Abu-Ameerh MA, Albdour MD. KeraRing intrastromal corneal ring segments for correction of keratoconus. Cornea. 2012;31:115–120. doi: 10.1097/ICO.0b013e3182215a15. [DOI] [PubMed] [Google Scholar]
- 2.de Sanctis U, Loiacono C, Richiardi L, Turco D, Mutani B, Grignolo FM. Sensitivity and specificity of posterior corneal elevation measured by Pentacam in discriminating keratoconus/subclinical keratoconus. Ophthalmology. 2008;115:1534–1539. doi: 10.1016/j.ophtha.2008.02.020. [DOI] [PubMed] [Google Scholar]
- 3.Shetty R, Shetty R, Mahendradas P, Shetty BK. Are the surgeons safe during UV-A radiation exposure in collagen cross-linking procedure? Cornea. 2012;31:167–171. doi: 10.1097/ICO.0b013e31821e6597. [DOI] [PubMed] [Google Scholar]
- 4.Ishii R, Kamiya K, Igarashi A, Shimizu K, Utsumi Y, Kumanomido T. Correlation of corneal elevation with severity of keratoconus by means of anterior and posterior topographic analysis. Cornea. 2012;31:253–258. doi: 10.1097/ICO.0B013E31823D1EE0. [DOI] [PubMed] [Google Scholar]
- 5.Wilson SE, Klyce SD. Screening for corneal topographic abnormalities before refractive surgery. Ophthalmology. 1994;101:147–152. doi: 10.1016/s0161-6420(94)31372-8. [DOI] [PubMed] [Google Scholar]
- 6.Varssano D, Kaiserman I, Hazarbassanov R. Topographic patterns in refractive surgery candidates. Cornea. 2004;23:602–607. doi: 10.1097/01.ico.0000121699.74077.f0. [DOI] [PubMed] [Google Scholar]
- 7.Bühren J, Kook D, Yoon G, Kohnen T. Detection of subclinical keratoconus by using corneal anterior and posterior surface aberrations and thickness spatial profiles. Invest Ophthalmol Vis Sci. 2010;51:3424–3432. doi: 10.1167/iovs.09-4960. [DOI] [PubMed] [Google Scholar]
- 8.Schlegel Z, Hoang-Xuan T, Gatinel D. Comparison of and correlation between anterior and posterior corneal elevation maps in normal eyes and keratoconus-suspect eyes. J Cataract Refract Surg. 2008;34:789–795. doi: 10.1016/j.jcrs.2007.12.036. [DOI] [PubMed] [Google Scholar]
- 9.Sonmez B, Doan MP, Hamilton DR. Identification of scanning slit-beam topographic parameters important in distinguishing normal from keratoconic corneal morphologic features. Am J Ophthalmol. 2007;143:401–408. doi: 10.1016/j.ajo.2006.11.044. [DOI] [PubMed] [Google Scholar]
- 10.Fam HB, Lim KL. Corneal elevation indices in normal and keratoconic eyes. J Cataract Refract Surg. 2006;32:1281–1287. doi: 10.1016/j.jcrs.2006.02.060. [DOI] [PubMed] [Google Scholar]
- 11.Wei RH, Lim L, Chan WK, Tan DT. Evaluation of Orbscan II corneal topography in individuals with myopia. Ophthalmology. 2006;113:177–183. doi: 10.1016/j.ophtha.2005.11.004. [DOI] [PubMed] [Google Scholar]
- 12.Lim L, Wei RH, Chan WK, Tan DT. Evaluation of keratoconus in Asians: Role of Orbscan II and Tomey TMS-2 corneal topography. Am J Ophthalmol. 2007;143:390–400. doi: 10.1016/j.ajo.2006.11.030. [DOI] [PubMed] [Google Scholar]
- 13.Quisling S, Sjoberg S, Zimmerman B, Goins K, Sutphin J. Comparison of Pentacam and Orbscan IIz on posterior curvature topography measurements in keratoconus eyes. Ophthalmology. 2006;113:1629–1632. doi: 10.1016/j.ophtha.2006.03.046. [DOI] [PubMed] [Google Scholar]
- 14.Rao SN, Raviv T, Majmudar PA, Epstein RJ. Role of Orbscan II in screening keratoconus suspects before refractive corneal surgery. Ophthalmology. 2002;109:1642–1646. doi: 10.1016/s0161-6420(02)01121-1. [DOI] [PubMed] [Google Scholar]


