Abstract
Purpose:
To compare ultrasound pachymetry and Orbscan II for measurement of central corneal thickness (CCT) in normal eyes.
Methods:
The current study was performed at Labbafinejad Medical Center (LMC), Tehran, Iran. Three hundred eyes from 150 healthy individuals referred for keratorefractive surgery were assessed first by Orbscan II and then by ultrasound pachymetry, and CCT values were recorded and compared.
Results:
Overall, Orbscan II overestimated CCT as compared to ultrasound pachymetry by about 2.4% (mean values 547.6 ± 34.7 versus 534.8 ± 34.7, respectively, P < 0.001). The difference was more significant when CCT was less than 500 microns (mean values 493.2 ± 16.9 versus 479.9 ± 15.6, mean overestimation: 2.6%, P < 0.001). There was good linear correlation between the two methods (Pearson's correlation r = 0.968, P < 0.0001).
Conclusion:
Orbscan II has good correlation with ultrasound pachymetry for measurement of CCT in normal eyes; however Orbscan II should not be used to evaluate corneal thickness before keratorefractive surgeries, as it tends to overestimate corneal thickness and may result in undesirable, low residual stromal thickness.
Keywords: Central Corneal Thickness, Orbscan II, Ultrasound Pachymetry
INTRODUCTION
Central corneal thickness (CCT) is an important parameter in ophthalmology and optometry.[1] It has a critical role in determining flap and residual stromal thickness and also optical zone in keratorefractive procedures.[2] This matter is of particular importance since the extensive popularity of keratorefractive procedures has resulted in cases of post keratorefractive surgery ectasia.[3,4]
CCT is also a valuable parameter in patients with glaucoma. Measurement of intraocular pressure (IOP), especially with applanation tonometry, may be affected by CCT.[5] Moreover, CCT is an independent risk factor for developing glaucomatous optic nerve damage.[6]
Corneal thickness can be measured by several methods, although ultrasound pachymetry is still the gold standard. Disadvantages of ultrasonic pachymetry include direct placement of the probe on the cornea, the risk infection and corneal epithelial damage, the necessity for topical anesthesia (which may influence CCT measurements),[7] and dependence on examiner experience for reliable measurements.
Newer technologies are being used by many clinicians, such as scanning slit topography, confocal microscopy, specular microscopy and spectral oscillation interferometry, all of which employ optical methods. The reliability and repeatability of these methods have been studied by many researchers yielding different results.[8,9]
Orbscan is a corneal topographer which employs scanning slit topography and videokeratography to obtain corneal curvature and thickness maps. Many ophthalmologists routinely use Orbscan to evaluate corneas before refractive surgeries. Since the mucus layer of the tear film increases corneal thickness measured by Orbscan, the acoustic factor (AF) determined by the manufacturer, is used to modify the measured values. However, there is no consensus about the reliability of CCT measurements by Orbscan II as compared to ultrasound as the gold standard.[10,11,12]
Regarding the controversial results of previous studies and the need to adjust measurements taken by Orbscan II, this study was performed to compare corneal pachymetry obtained by the ultrasound method and by Orbscan II and to search for the optimal AF in the studied population.
METHODS
This cross-sectional comparative study includes 300 eyes of 150 consecutive patients referred for refractive surgery to the eye clinic at Labbafinejad Medical Center (LMC). Sample size was calculated according to the formula: N = 2(SD)2 (Z1-α/2 + Z1-β)2/d2, where SD = 34, α = 0.05, 1-β = 0.95 and d = 10 microns. Inclusion criteria were age between 18-35 years, keratometry between 44-48 diopters, normal corneal topographic pattern, myopia with or without regular astigmatism, and stable refraction for at least 6 months. Exclusion criteria consisted of previous refractive surgery, corneal lesions (e.g. scar), keratoconus, history of cataract or glaucoma surgery, recent use of contact lenses and use of topical medications.
A questionnaire regarding age, sex, past medical and surgical history was completed for each subject and a comprehensive ophthalmic examination was performed. The study was performed according to conditions set by the Ethics Committee of the Ophthalmic Research Center, Shahid Beheshti University of Medical Sciences.
Orbscan II (Bausch and Lomb, Rochester, NY, USA) imaging was performed for all eyes, and CCT was adjusted by an AF of 0.92 as suggested by the manufacturer.[13] Other AF values were also used to alter the results. This measurement was followed by ultrasound pachymetry (Tomey SP-3000, Tomey Ltd, Japan). Ultrasonic pachymetry was performed by one experienced operator on all patients under topical anesthesia with tetracaine 1%. Measurements were obtained 5 times from the center of the cornea with an SD < 2.0 and the average reading was recorded for each patient.
All data was recorded in SPSS v. 20 software and analyzed by paired t and Chi square tests. The correlation between the measurements was assessed by Pearson's correlation analysis. P values less than 0.05 were considered as significant. 95% limits of agreement (LoA) between readings by the two instruments were calculated using Bland-Altman analysis.
RESULTS
CCT values of 300 eyes from 150 otherwise healthy people including 94 (63%) women and 56 (37%) men were measured by ultrasound pachymetry and Orbscan II. Mean patient age was 25.4 ± 7.2 (range 18-32) years.
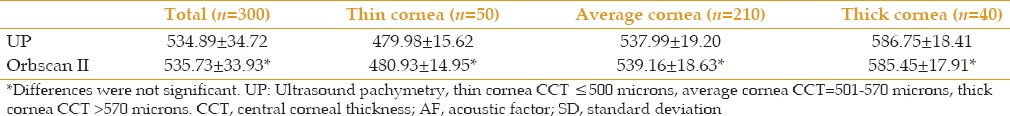
Mean CCT values measured by ultrasound pachymetry and Orbscan II were 534.89 ± 34.72 and 547.64 ± 34.77, respectively, the difference between which was statistically significant [Table 1]. Differences between the measurements and LoAs are detailed in Table 2. Pearson's correlation analysis revealed a good linear correlation (r = 0.963, P < 0.0001) between the two instruments as depicted in Figure 1a.
Table 1.
Central corneal thickness (mean±SD) measured by Orbscan II (AF=0.92) and UP
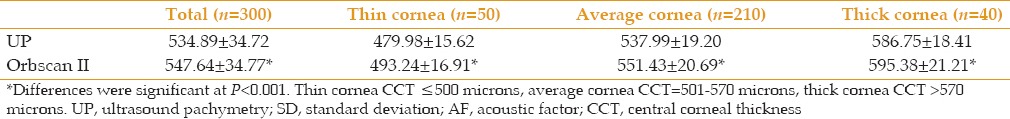
Table 2.
Agreement between UP and Orbscan II for central corneal thickness measurements
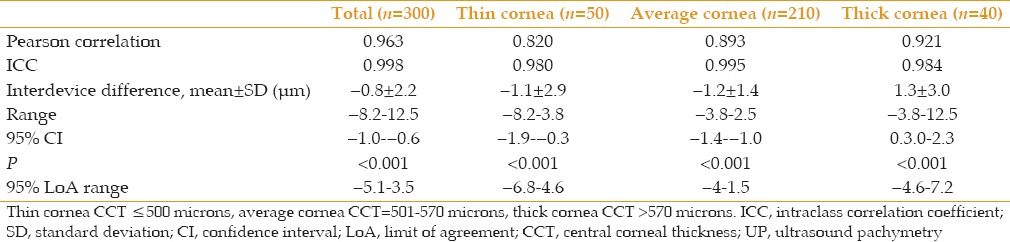
Figure 1.
Scatter diagram showing the regression line for central corneal thickness (μm) measured by Orbscan II and ultrasound pachymetry in all cases (a), thin corneas (b), average corneas (c), and thick corneas (d).
Eyes were divided into 3 groups according to ultrasonic central corneal thickness values: Thin corneas (CCT ≤ 500 microns), average corneas (CCT 501-570 microns) and thick corneas (CCT > 570 microns). Although CCT was significantly overestimated by Orbscan II in all thickness groups, the least difference was seen with thick corneas and the greatest was observed in the thin cornea group [Table 1]. Logistic regression plots of the subgroups are shown in Figure 1b–d.
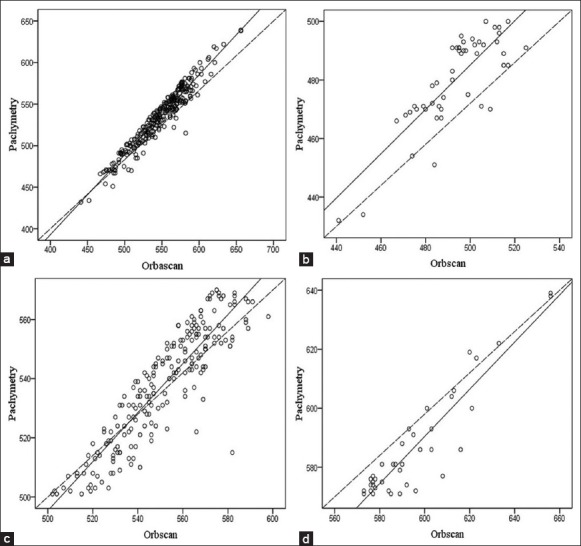
The two devices showed a remarkable intraclass correlation coefficient (ICC), as shown in Table 2. Differences between mean measurements and LoA are detailed in Table 2 and LoA plots are shown in Figure 2a–d. When the measurements of Orbscan II were adjusted with an AF of 0.90, the results were closest to ultrasonic pachymetry (UP) measurements in all thickness groups [Table 3].
Figure 2.
Interdevice agreements shown by Bland-Altman plots for ultrasound pachymetry (UP) against Orbscan II (ORB II) in all cases (a) and different corneal thickness groups (b-d).
Table 3.
CCT measured by Orbscan II (AF=0.90) and UP (mean±SD)
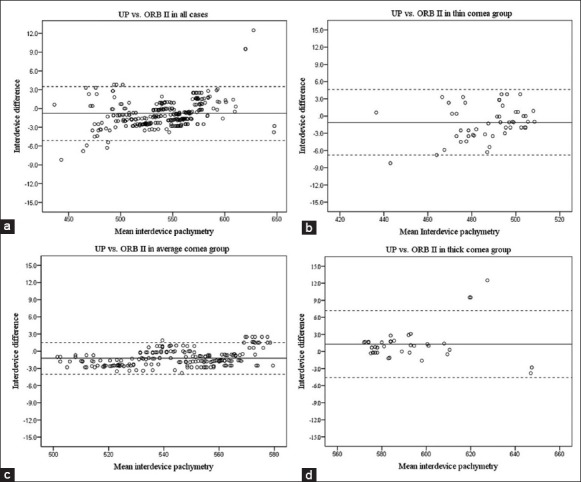
Mean CCT by UP and Orbscan II were, 535.6 and 547.4 in male, versus 534.5 and 547.8 in female subjects, respectively with no significant difference between the genders. Measurements by UP (535.4 versus 534.4) and Orbscan II (547.9 versus 547.5) were comparable between the right and left eyes, respectively. Furthermore, there was no correlation between age and interdevice differences as shown in Figure 3. Linear regression analysis showed no significant effect from sex, laterality, or age on differences between measurements of the two instruments.
Figure 3.
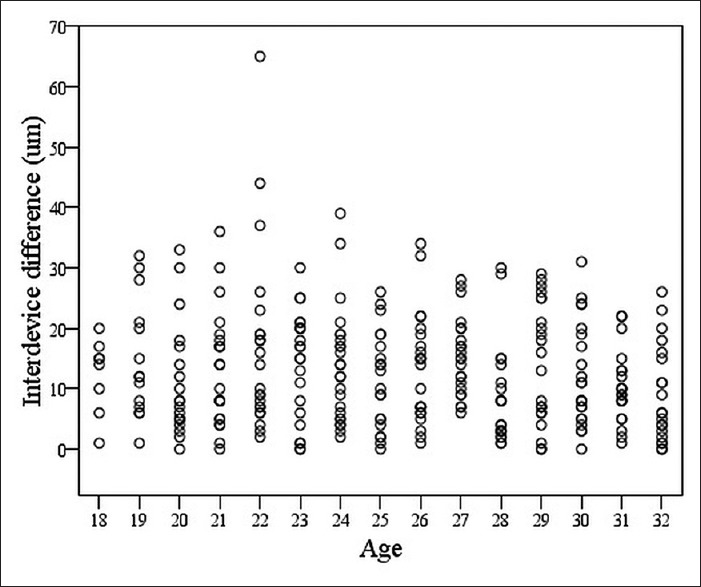
Scatter diagram showing CCT differences measured by UP versus Orbscan II plotted against patient age.
DISCUSSION
Corneal thickness is a critical factor in patient selection for keratorefractive surgery. Ultrasound pachymetry remains the gold standard for measuring corneal thickness; however, several non-contact methods are being used for this purpose by many clinicians. Orbscan II provides topographic information of the cornea as well as a corneal pachymetric map by using the scanning slit method. Orbscan is widely used in the preoperative evaluation of keratorefractive surgery candidates.
In this study, CCT of 300 eyes from 150 patients referred for keratorefractive surgery were measured by ultrasound pachymetry and Orbscan II, and the results were compared. The results showed that, although a good linear correlation existed between the two methods, Orbscan II overestimated CCT as compared to ultrasound pachymetry, even after adjustment with the acoustic factor (AF) [Table 1]. The difference was higher in thinner corneas. When the acoustic factor was set to 0.90, measurements by Orbscan II were much closer to UP [Table 3].
Discrepancies between ultrasound and Orbscan II in corneal thickness measurements have been reported in several studies. Without correcting using an AF, there has been significant overestimation of CCT by Orbscan II.[14,15,16,17] Proposed to preclude tear film interference with measurement of CCT, the acoustic factor is recommended by the manufacturer and is usually set at 0.92.
After making adjustments with the usual recommended acoustic factor (0.92), Radford et al reported overestimation by Orbscan II,[18] as also observed in the current study. Similarly, Ou et al found that after correcting with an AF of 0.935, Orbscan yielded significantly higher corneal thickness values as compared to ultrasound pachymetry.[19] In most studies however, Orbscan II measured CCT lower than or equal to UP after the AF was applied.[20,21,22,23,24]
Nissen et al proposed that ultrasound pachymetry may underestimate the thickness of the corneal epithelium by displacement of the tear film.[25] Suzuki et al proposed that the different mechanisms of the two instruments for diagnosing the posterior corneal surface may be the origin of differences in CCT measurements between Orbscan II and ultrasound.[22]
Lu et al believed that the acoustic factor is a variable, not a constant. In their study, there was a strong, significant correlation between corneal thickness (i.e. corneal swelling induced by overnight RGP use) and the percentage of change by the adjusted AF. They suggested that the usage of a single AF for all corneal thicknesses may be untenable.[26]
In the current study, Orbscan II overestimated CCT in all thickness ranges, especially in thin corneas (i.e. CCT less than or equal to 500 microns) for which the overestimation was greater [Table 1]. This finding is in agreement with the results of Radford et al using AF of 0.92 and Ou et al employing an AF of 0.935.[18,19] In contrast, many studies that used the adjusted AF of 0.92 reported significant underestimation by Orbscan II, especially in the lower range of CCT.[20,21,23,27] Also, in some studies, there was no significant difference between Orbscan II and ultrasound after adjustment by an AF of 0.92.[11,22] The current study found that after adjusting Orbscan II results with an AF of 0.90, measurements were closest to the gold standard (UP) method [Table 3].
Recently, Elbaz et al used several methods on a large study sample to approximate the results of the Orbscan II to ultrasonic measurements. Although linear correction methods (multiplication and subtraction) were associated with good interdevice correlation, only nonlinear correction methods (i.e. polynomial, logarithmic, and power fit methods) narrowed the 95% LoA intervals.[28] In the current study, however, the application of an AF of 0.92 was associated with narrow LoA intervals, and measurements by both instruments were comparable in all groups. The relatively narrow LoA intervals observed in the present study might be due to technical differences in ultrasonic measurements and determination of the corneal center by the technician. Ocular surface conditions (i.e. tear film) can also affect measurements by Orbscan II. The application of an AF of 0.90 was associated with more accurate results, but this value might be specific to the center at which the current study was performed and/or to the studied population but might not be applicable to other subjects.
In conclusion, although Orbscan II has excellent correlation with ultrasound pachymetry for measurement of CCT in normal eyes, it may be misleading, especially in extremes of corneal thickness. It may be used safely for preoperative evaluations before surface ablation methods; however, it should not replace ultrasound measurement before laser in situ keratomileusis (LASIK) as it has shown out-of-range results in most studies. Studies that use multiple adjustment methods with larger sample size that also include abnormal corneas may find the best adjustment method for Orbscan II results.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Patwardhan AA, Khan M, Mollan SP, Haigh P. The importance of central corneal thickness measurements and decision making in general ophthalmology clinics: A masked observational study. BMC Ophthalmol. 2008;8:1. doi: 10.1186/1471-2415-8-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Argento C, Cosentino MJ, Tytiun A, Rapetti G, Zarate J. Corneal ectasia after laser in situ keratomileusis. J Cataract Refract Surg. 2001;27:1440–1448. doi: 10.1016/s0886-3350(01)00799-4. [DOI] [PubMed] [Google Scholar]
- 3.Pallikaris IG, Kymionis GD, Astyrakakis NI. Corneal ectasia induced by laser in situ keratomileusis. J Cataract Refract Surg. 2001;27:1796–802. doi: 10.1016/s0886-3350(01)01090-2. [DOI] [PubMed] [Google Scholar]
- 4.Malecaze F, Coullet J, Calvas P, Fournié P, Arné JL, Brodaty C. Corneal ectasia after photorefractive keratectomy for low myopia. Ophthalmology. 2006;113:742–746. doi: 10.1016/j.ophtha.2005.11.023. [DOI] [PubMed] [Google Scholar]
- 5.Doughty MJ, Zaman ML. Human corneal thickness and its impact on intraocular pressure measures: A review and meta-analysis approach. Surv Ophthalmol. 2000;44:367–408. doi: 10.1016/s0039-6257(00)00110-7. [DOI] [PubMed] [Google Scholar]
- 6.Mokbel TH, Ghanem AA. Correlation of central corneal thickness and optic nerve head topography in patients with primary open-angle glaucoma. Oman J Ophthalmol. 2010;3:75–80. doi: 10.4103/0974-620X.64231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sanchis-Gimeno JA, Palanca-Sanfrancisco JM, García-Lázaro S, Madrid-Costa D, Cerviño A. The effect of anesthetic eye drop instillation on the distribution of corneal thickness. Cornea. 2013;32:e102–e105. doi: 10.1097/ICO.0b013e318275e7a6. [DOI] [PubMed] [Google Scholar]
- 8.González-Pérez J, González-Méijome JM, Rodríguez Ares MT, Parafita MA. Central corneal thickness measured with three optical devices and ultrasound pachometry. Eye Contact Lens. 2011;37:66–70. doi: 10.1097/ICL.0b013e31820c6ffc. [DOI] [PubMed] [Google Scholar]
- 9.Dutta D, Rao HL, Addepalli UK, Vaddavalli PK. Corneal thickness in keratoconus: Comparing optical, ultrasound, and optical coherence tomography pachymetry. Ophthalmology. 2013;120:457–63. doi: 10.1016/j.ophtha.2012.08.036. [DOI] [PubMed] [Google Scholar]
- 10.Kawana K, Miyata K, Tokunaga T, Kiuchi T, Hiraoka T, Oshika T. Central corneal thickness measurements using Orbscan II scanning slit topography, noncontact specular microscopy, and ultrasonic pachymetry in eyes with keratoconus. Cornea. 2005;24:967–971. doi: 10.1097/01.ico.0000159733.37554.ba. [DOI] [PubMed] [Google Scholar]
- 11.Faramarzi A, Ziai H. Central Corneal Thickness Measurement by Ultrasound versus Orbscan II. J Ophthalmic Vis Res. 2008;3:83–86. [PMC free article] [PubMed] [Google Scholar]
- 12.Hashemi H, Roshani M, Mehravaran S, Parsafar H, Yazdani K. Effect of corneal thickness on the agreement between ultrasound and Orbscan II pachymetry. J Cataract Refract Surg. 2007;33:1694–700. doi: 10.1016/j.jcrs.2007.05.036. [DOI] [PubMed] [Google Scholar]
- 13.González-Méijome JM, Cerviño A, Yebra-Pimentel E, Parafita MA. Central and peripheral corneal thickness measurement with Orbscan II and topographical ultrasound pachymetry. J Cataract Refract Surg. 2003;29:125–132. doi: 10.1016/s0886-3350(02)01815-1. [DOI] [PubMed] [Google Scholar]
- 14.Doughty MJ, Jonuscheit S. An assessment of regional differences in corneal thickness in normal human eyes, using the Orbscan II or ultrasound pachymetry. Optometry. 2007;78:181–190. doi: 10.1016/j.optm.2006.08.018. [DOI] [PubMed] [Google Scholar]
- 15.Hashemi H, Mehravaran S. Central corneal thickness measurement with Pentacam, Orbscan II, and ultrasound devices before and after laser refractive surgery for myopia. J Cataract Refract Surg. 2007;33:1701–1707. doi: 10.1016/j.jcrs.2007.05.040. [DOI] [PubMed] [Google Scholar]
- 16.Fishman GR, Pons ME, Seedor JA, Liebmann JM, Ritch R. Assessment of central corneal thickness using optical coherence tomography. J Cataract Refract Surg. 2005;31:707–711. doi: 10.1016/j.jcrs.2004.09.021. [DOI] [PubMed] [Google Scholar]
- 17.Yaylali V, Kaufman SC, Thompson HW. Corneal thickness measurements with the Orbscan Topography System and ultrasonic pachymetry. J Cataract Refract Surg. 1997;23:1345–1350. doi: 10.1016/s0886-3350(97)80113-7. [DOI] [PubMed] [Google Scholar]
- 18.Radford SW, Lim R, Salmon JF. Comparison of Orbscan and ultrasound pachymetry in the measurement of central corneal thickness. Eye (Lond) 2004;18:434–436. doi: 10.1038/sj.eye.6700669. [DOI] [PubMed] [Google Scholar]
- 19.Ou TH, Lai IC, Teng MC. Comparison of central corneal thickness measurements by ultrasonic pachymetry, Orbscan II, and SP3000P in eyes with glaucoma or glaucoma suspect. Chang Gung Med J. 2012;35:255–262. doi: 10.4103/2319-4170.106146. [DOI] [PubMed] [Google Scholar]
- 20.Basmak H, Sahin A, Yildirim N. The reliability of central corneal thickness measurements by ultrasound and by Orbscan system in schoolchildren. Curr Eye Res. 2006;31:569–575. doi: 10.1080/02713680600801115. [DOI] [PubMed] [Google Scholar]
- 21.Lackner B, Schmidinger G, Pieh S, Funovics MA, Skorpik C. Repeatability and reproducibility of central corneal thickness measurement with Pentacam, Orbscan, and ultrasound. Optom Vis Sci. 2005;82:892–899. doi: 10.1097/01.opx.0000180817.46312.0a. [DOI] [PubMed] [Google Scholar]
- 22.Suzuki S, Oshika T, Oki K, Sakabe I, Iwase A, Amano S, et al. Corneal thickness measurements: Scanning-slit corneal topography and noncontact specular microscopy versus ultrasonic pachymetry. J Cataract Refract Surg. 2003;29:1313–1318. doi: 10.1016/s0886-3350(03)00123-8. [DOI] [PubMed] [Google Scholar]
- 23.McLaren JW, Nau CB, Erie JC, Bourne WM. Corneal thickness measurement by confocal microscopy, ultrasound, and scanning slit methods. Am J Ophthalmol. 2004;137:1011–1020. doi: 10.1016/j.ajo.2004.01.049. [DOI] [PubMed] [Google Scholar]
- 24.Chakrabarti HS, Craig JP, Brahma A, Malik TY, McGhee CN. Comparison of corneal thickness measurements using ultrasound and Orbscan slit-scanning topography in normal and post-LASIK eyes. J Cataract Refract Surg. 2001;27:1823–1828. doi: 10.1016/s0886-3350(01)01089-6. [DOI] [PubMed] [Google Scholar]
- 25.Nissen J, Hjortdal JO, Ehlers N, Frost-Larsen K, Sørensen T. A clinical comparison of optical and ultrasonic pachometry. Acta Ophthalmol (Copenh) 1991;69:659–663. doi: 10.1111/j.1755-3768.1991.tb04857.x. [DOI] [PubMed] [Google Scholar]
- 26.Lu F, Simpson T, Fonn D, Sorbara L, Jones L. Validity of pachymetric measurements by manipulating the acoustic factor of Orbscan II. Eye Contact Lens. 2006;32:78–83. doi: 10.1097/01.icl.0000174760.95482.9c. [DOI] [PubMed] [Google Scholar]
- 27.Crawford AZ, Patel DV, McGhee CN. Comparison and repeatability of keratometric and corneal power measurements obtained by Orbscan II, Pentacam, and Galilei corneal tomography systems. Am J Ophthalmol. 2013;156:53–60. doi: 10.1016/j.ajo.2013.01.029. [DOI] [PubMed] [Google Scholar]
- 28.Elbaz U, Zadok D, Frenkel S, Pokroy R, Orucoglu Orucov F, Caspi Z, et al. Mathematical approximation of Orbscan II central corneal thickness to contact ultrasound. Cornea. 2013;32:772–778. doi: 10.1097/ICO.0b013e318274a6b1. [DOI] [PubMed] [Google Scholar]


