Abstract
Diabetes mellitus affects almost 350 million individuals throughout the globe resulting in significant morbidity and mortality. Of further concern is the growing population of individuals that remain undiagnosed but are susceptible to the detrimental outcomes of this disorder. Diabetes mellitus leads to multiple complications in the central and peripheral nervous systems that include cognitive impairment, retinal disease, neuropsychiatric disease, cerebral ischemia, and peripheral nerve degeneration. Although multiple strategies are being considered, novel targeting of trophic factors, Wnt signaling, Wnt1 inducible signaling pathway protein 1, and stem cell tissue regeneration are considered to be exciting prospects to overcome the cellular mechanisms that lead to neuronal injury in diabetes mellitus involving oxidative stress, apoptosis, and autophagy. Pathways that involve insulin-like growth factor-1, fibroblast growth factor, epidermal growth factor, and erythropoietin can govern glucose homeostasis and are intimately tied to Wnt signaling that involves Wnt1 and Wnt1 inducible signaling pathway protein 1 (CCN4) to foster control over stem cell proliferation, wound repair, cognitive decline, β-cell proliferation, vascular regeneration, and programmed cell death. Ultimately, cellular metabolism through Wnt signaling is driven by primary metabolic pathways of the mechanistic target of rapamycin and AMP activated protein kinase. These pathways offer precise biological control of cellular metabolism, but are exquisitely sensitive to the different components of Wnt signaling. As a result, unexpected clinical outcomes can ensue and therefore demand careful translation of the mechanisms that govern neural repair and regeneration in diabetes mellitus.
Keywords: Alzheimer's disease, AMPK, apoptosis, autophagy, central nervous system, CCN4, EGF, diabetes mellitus, erythropoietin, EPO, FGF, IGF-1, mTOR, neuron, neuropathy, oxidative stress, psychiatric, stem cells, WISP1, Wnt
The Impact of Diabetes Mellitus on the Nervous System
The incidence of diabetes mellitus (DM) is increasing in accordance with the growth of obesity in the world's population (Maiese et al., 2011a, 2013c; Rutter et al., 2012; Jia et al., 2014; Xu et al., 2014a). Obesity can lead to DM (Lim et al., 2014) as well as independently result in metabolic dysfunction. Excess body fat can precipitate pancreatic β cell injury (Shao et al., 2013), cellular inflammation (Essser et al., 2014), impaired growth factor release (Maiese et al., 2005b, 2012a; White, 2014; Zhang et al., 2014c), changes in protein tyrosine phosphatase signaling (Chong and Maiese, 2007; Xu et al., 2014a), oxidative stress (Maiese et al., 2013c; Liu et al., 2014), and insulin resistance (Maiese et al., 2007a; Caron et al., 2014; Essser et al., 2014). With the significant increases in DM and obesity, the World Health Organization estimates that DM will be the seventh leading cause of death in the year 2030 (World Health Organization, 2011). Worldwide, approximately 347 million individuals suffer form DM. In the United States (US) alone, 21 million individuals are diagnosed with DM. Yet, of equal concern is that an estimated additional 8 million individuals presently remain undiagnosed with DM but remain susceptible to the ill effects of this disease (Centers for Disease Control and Prevention, 2014). It is believed that DM costs US employers $69 billion in reduced productivity and another $176 billion for direct medical costs. This represents a significant cost for the country especially with the Centers for Medicare and Medicaid Services reporting that the US spends 2.8 trillion on healthcare that equals $8,915 per person and 17.2 percent of the Gross Domestic Product.
Although some overlap exists, DM can be divided into either non-insulin dependent (Type 1) DM or insulin dependent (Type 2) DM (Maiese et al., 2010a, 2013b). In approximately 90% of individuals with DM, Type 2 DM is present and usually occurs in individuals over the age of 40. It presents with a progressive deterioration of glucose tolerance with early β-cell compensation (Maiese et al., 2007b, 2013c). Loss of insulin secretion can result from impaired β-cell function, prolonged exposure to free fatty acids and hyperglycemia, and the absence of inhibitory feedback through plasma glucagon levels. Type 1 DM occurs in the remaining 10% of patients with DM and it is considered to be the result of an autoimmune disorder associated with the alleles of the human leukocyte antigen class II genes within the major histocompatibility complex (Maiese et al., 2007b). Loss of insulin production and homeostasis occurs as a result of the destruction of pancreatic β-cells with inflammatory infiltration of the islets of Langerhans. Approximately 90% of patients with Type 1 DM have increased titers of autoantibodies (Type 1A DM), but the remaining 10% of Type 1 DM individuals do not have serum autoantibodies. These individuals have maturity-onset diabetes of the young (MODY) that can be the result of β-cell dysfunction with autosomal-dominant inheritance (Type IB DM). Type 1 and Type 2 DM are not completely independent entities since almost 10% of individuals with Type 2 DM may have elevated serum autoantibodies similar to Type 1 DM. In addition, insulin resistance also may be a component of Type 1 DM in some patients.
DM affects all components of the central and peripheral nervous systems. For example, DM can foster retinal disease (Tang et al., 2011; Fu et al., 2012; Busch et al., 2014), injury to the neuroglialvascular unit (Busch et al., 2014), angiogenesis impairment (Chen et al., 2012), endothelial cell demise (Chong et al., 2007; Hou et al., 2010a; Chong et al., 2011b; Schaffer et al., 2012; Liu et al., 2013c; Wang et al., 2014; Zhang et al., 2014c), endothelial cell senescence (Arunachalam et al., 2014), dysfunctional maintenance and mobilization of endothelial progenitor cells (Barthelmes et al., 2014; Kim et al., 2014), and peripheral nerve disorders (Schmeichel et al., 2003; Gomes and Negrato, 2014). Although it is estimated that 60–70% of individuals with DM can develop some degree of peripheral neuropathy, the incidence of disorders such as peripheral neuropathy can be difficult to assess since the course of the disease may occur over several years, initial progression of the disease may be sub-clinical, and improved control of DM may lead to correction of prior clinical deficits. DM also can result in memory loss (Zhao et al., 2013; Mao et al., 2014; Du et al., 2015), neuropsychiatric disorders (Aksu et al., 2012; Reagan, 2012), stroke (Jiang et al., 2014), and impairment of neuronal longevity (White, 2014). Furthermore, complications of DM such as insulin resistance and dementia has been reported in patients with Alzheimer's disease (Maiese et al., 2007b; Sonnen et al., 2009), indicating that some neurodegenerative disorders may be the result of impaired cellular metabolism similar to that which occurs during DM (Kapogiannis et al., 2014).
Diabetes Mellitus, Oxidative Stress, and Programmed Cell Death
The generation of reactive oxygen species (ROS) leading to the induction of oxidative stress can be a critical determinant of neuronal and vascular cell injury during DM (Yang et al., 2011b; Bagul and Banerjee, 2013; Liu et al., 2013b; Maiese et al., 2013b, c; Peng et al., 2013; Weinberg et al., 2014; Xu et al., 2014b). ROS can alter cellular metabolic pathways (Maiese et al., 2010a, 2011a; Fu et al., 2012; Gomes and Negrato, 2014; Xu et al., 2014b) and influence epigenetic pathways (Maiese et al., 2008b; Fraineau et al., 2014; Jenwitheesuk et al., 2014; Xin et al., 2015) with subsequent nervous system deficits that lead to cognitive loss (Chong et al., 2005a; Kim et al., 2015; Wright and Harding, 2015), post-traumatic injury (Harish et al., 2015), and stroke (Chong et al., 2005b; Peng et al., 2015). ROS include superoxide free radicals, nitric oxide, hydrogen peroxide, and singlet oxygen that result in mitochondrial dysfunction, DNA destruction, cell injury, and protein misfolding (Chong et al., 2005b; Maiese et al., 2013b; Asaithambi et al., 2014; Chen et al., 2014a; Palma et al., 2014; Zeldich et al., 2014). Protective pathways within the body and nervous system can serve to limit the deleterious effects of ROS and oxidative stress. These include vitamins such as B, C, D, and K (Maiese et al., 2009; Bowes Rickman et al., 2013; Miret and Munne-Bosch, 2014; Xu et al., 2014b; Yousef and Mohamed, 2015) as well as catalase, glutathione peroxidase, and superoxide dismutase (Li et al., 2012; Muley et al., 2012; Maiese et al., 2013b; Vishwas et al., 2013; Akasaki et al., 2014; Gezginci-Oktayoglu et al., 2014; Mao et al., 2014; Moghaddasi et al., 2014; Palma et al., 2014; Srivastava and Shivanandappa, 2014; Zhou et al., 2014b).
Patients with Type 2 DM have serum markers of oxidative stress with ischemia-modified albumin (Kurban et al., 2011). Interestingly, brief periods as well as chronic exposure of hyperglycemia that can occur during DM can lead to ROS (Yano et al., 2004; Monnier et al., 2006). Formation of ROS and activation of caspases (Weinberg et al., 2014) can occur through advanced glycation end products (AGEs), entities that lead to complications in DM (Maiese, 2008; Chong and Maiese, 2012). In addition, glucolipotoxicity caused by elevated plasma glucose and high lipid levels promotes oxidative stress with cytochrome c release, caspase activation, and apoptosis in pancreatic β-cells (Liu et al., 2012b). High fat diets (Ribeiro et al., 2009) and free fatty acids also have been shown to result in ROS generation, lead to mitochondrial DNA damage, and result in pancreatic β-cell dysfunction (Rachek et al., 2006). During oxidative stress with DM, opening of the mitochondrial membrane permeability transition pore occurs to promote cytochrome c release and caspase activity (Hou et al., 2010a, b; Chong et al., 2011b; Tang et al., 2011; Cardoso et al., 2012; Du et al., 2015; Mao et al., 2014). Alterations in uncoupling proteins (UCPs) also occur that influence cell survival during DM (Maiese et al., 2007a; Liu et al., 2013b; Zhang et al., 2014b). Uncoupling of respiration by UCPs can alter ATP synthesis, fatty acid release, and glucose oxidation. Ultimately, mitochondrial dysfunction and UCP activity can then be followed by programmed cell death with apoptosis and autophagy (Fu et al., 2012).
Apoptosis (Maiese et al., 2010b; Damasceno et al., 2013; Gomes and Negrato, 2014; Wang et al., 2014; Xu et al., 2014b) and autophagy (Maiese et al., 2012b, 2013b; Yamada and Singh, 2012; Jia et al., 2014) are pathways of programmed cell death that play significant roles in controlling cell survival during DM and oxidative stress. With apoptosis, there exists an early phase that consists of the loss of plasma membrane lipid phosphatidylserine asymmetry that can identify cells for disposal by microglia in the nervous system (Schutters and Reutelingsperger, 2010; Wei et al., 2013; Williams and Dexter, 2014). A later phase in apoptosis results in cell death with DNA degradation (Chong et al., 2005b, 2006; Favaloro et al., 2012; Folch et al., 2012; Shao et al., 2013; Nguyen et al., 2014). During DM, apoptosis results in the death of neurons (Das et al., 2011; Aksu et al., 2012; Kimura et al., 2013; Mao et al., 2014), pancreatic β-cell loss (Deng et al., 2009; Choi et al., 2010; Miao et al., 2013), and endothelial cell destruction (Chong et al., 2007; Hou et al., 2010b; Hamed et al., 2011; Chen et al., 2012; Arunachalam et al., 2014).
Autophagy has three categories that permit cells to recycle cytoplasmic components and eliminate dysfunctional organelles for tissue remodeling (Maiese et al., 2012b; Cai and Yan, 2013; Chen et al., 2014b, c; Nakka et al., 2014). Of the three categories for autophagy, microautophagy employs the invagination of the lysosomal membrane for the sequestration and digestion of cytoplasmic components (Maiese et al., 2012b). In chaperone-mediated autophagy, cytosolic chaperones transport cytoplasmic components across lysosomal membranes. The most prevalent category of autophagy is macroautophagy that consists of the sequestration of cytoplasmic proteins and organelles into autophagosomes. These autophagosomes then combine with lysosomes for degradation and are subsequently recycled for future cellular processes. Autophagy has both a beneficial and detrimental side during DM (Chong et al., 2012c; Maiese et al., 2013c; Chen et al., 2014b; Min et al., 2014; Nakka et al., 2014). Exercise in mice has been shown to initiate autophagy and regulate glucose homeostasis (He et al., 2012). In addition, autophagy can improve insulin sensitivity during high fat diets in mice (Liu et al., 2014). Without autophagy, obesity may progression to DM, since experimental studies illustrate that autophagy haploinsufficiency in murine animal models of obesity can lead to increased insulin resistance with elevated lipids and inflammation (Lim et al., 2014). Autophagy also may be necessary to eliminate misfolded proteins and non-functioning mitochondria to prevent β-cell dysfunction and the onset of DM (Liu et al., 2013d). Yet, as noted, autophagy can play a detrimental role in DM. Although apoptosis may be a greater contributor to neuronal death than autophagy (Wang et al., 2012b), autophagy can impair endothelial progenitor cells, lead to mitochondrial oxidative stress, and prevent the formation of new blood vessels during elevated glucose exposure (Kim et al., 2014). AGEs also result in the induction of autophagy and vascular smooth muscle proliferation that can lead to atherosclerosis (Hu et al., 2012) and cardiomyopathy (Lee et al., 2012b). Furthermore, increased activation of autophagy can lead to loss of cardiac and liver tissue in diabetic rats during attempts to achieve glycemic control through diet modification (Lee et al., 2014).
Targeting Trophic Factors for DM in the Nervous System
For the nervous system, a number of avenues are being pursued to treat the complications of DM and oxidative stress. These include the modulation of sirtuins (Hou et al., 2010b; Maiese et al., 2011b; Chong et al., 2012a; Halperin-Sheinfeld et al., 2012; Shao et al., 2013; Arunachalam et al., 2014; Moroz et al., 2014), metabotropic receptors (Lin and Maiese, 2001; Maiese et al., 2007b, 2008c; Domin et al., 2014; Jantas et al., 2014; Domin et al., 2015), nicotinamide adenine dinucleotide (NAD+) precursors (Maiese et al., 2009, 2011a; Zhou et al., 2009; John et al., 2012; Carneiro et al., 2013; Ghasemi et al., 2014), protein tyrosine phosphatases (Chong and Maiese, 2007; Chen et al., 2012; Xu et al., 2014a; Geldman and Pallen, 2015), anti-oxidant therapies (Schaffer et al., 2012; Bagul and Banerjee, 2013; Gomes and Negrato, 2014; Xu et al., 2014b; Yousef and Mohamed, 2015), and trophic factors (Maiese et al., 2005b, 2008d, 2012a; Barthelmes et al., 2014; Hamed et al., 2014; Wang et al., 2014; White, 2014; Zhang et al., 2014c).
Growth factors are of particular interest since complications of DM and oxidative stress may be exacerbated during the loss of trophic factors (Figure 1). In experimental animal models of DM, oxidative stress may lead to reduced expression of insulin-like growth factor-1 (IGF-1), increased apoptosis of prefrontal cortex neurons, and subsequent anxiety (Aksu et al., 2012). In addition, insulin producing cells derived from stem cells may require the specific presence of fibroblast growth factor (FGF) and epidermal growth factor (EGF) (Czubak et al., 2014), growth factors that have been demonstrated to block neuronal injury during oxidative stress (Maiese et al., 1993). EGF also promotes the neuroprotective effects of glucagon-like peptide-1 against neuronal cell apoptosis in cell culture models of DM (Kimura et al., 2013) and FGF may block vascular disease during DM (Zhang et al., 2013). Erythropoietin (EPO) is another trophic factor of interest for DM since it can prevent retinal and photoreceptor injury from insults such as excessive light (Colella et al., 2011), oxidative stress (Shen et al., 2014) and DM (Busch et al., 2014). EPO can have multiple beneficial effects and lead to reduced blood glucose levels in animal models of DM and obesity (Katz et al., 2010), attenuate oxidative stress and apoptosis in Schwann cells mediated by AGEs (Yu et al., 2015), and protect endothelial cells during experimental models of DM (Chong et al., 2007, 2011b). Furthermore, EPO can limit high glucose-induced oxidative stress in renal tubular cells (Dang et al., 2010), control the detrimental effects of obesity in animal models (Zhang et al., 2014c), promote wound healing during DM (Hamed et al., 2014), and foster cellular mitochondrial function and energy metabolism (Wang et al., 2014). Through improvement of vascular perfusion by EPO (Kang et al., 2014), EPO may ultimately lead to cognitive repair (Hralova et al., 2013), reduce seizure occurrence (Castaneda-Arellano et al., 2014), and block peripheral nerve injury during DM (Yu et al., 2014).
Figure 1.
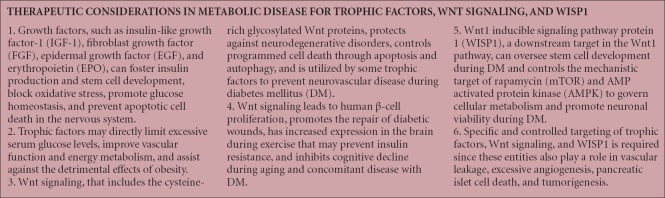
Therapeutic strategies in metabolic disease with trophic factors, wnt signaling, and WISP1.
Cellular Pathways of Wingless, the CCN Family, and Stem Cells
However, growth factors such as EPO rely upon multiple cellular pathways to exert cellular protection (Chong et al., 2002, 2003, 2012b; Maiese et al., 2008a; Chamorro et al., 2013; Kwon et al., 2014; Ma et al., 2014; Parvin et al., 2014; Schafer et al., 2014; Zhang et al., 2015). In regards to DM and oxidative stress, EPO relies upon the wingless pathway of Wnt proteins (Figure 1). Wnt proteins are cysteine-rich glycosylated proteins that control multiple processes involving neuronal development, angiogenesis, immunity, tumorigenesis, fibrosis, and stem cell proliferation (Li et al., 2006; Maiese et al., 2008e; Wexler et al., 2011; Zeljko et al., 2011; Heo et al., 2013; Berwick and Harvey, 2014; Thorfve et al., 2014). In the nervous system, Wnt signaling may be instrumental in the pathogenesis of disorders such as Parkinson's disease (Marchetti et al., 2013; Berwick and Harvey, 2014), protect against neuronal mitochondrial injury and cerebral ischemia (Chong et al., 2010; Xing et al., 2012, 2014), limit spinal cord injury (Gonzalez-Fernandez et al., 2013), maintain microglial and macrophage integrity and function (Shang et al., 2010; Wang et al., 2015), and serve as an anti-depressant (Pilar-Cuellar et al., 2013). Through pathways that involve the Wnt1 protein, EPO blocks cerebral endothelial cell injury in models of experimental diabetes (Chong et al., 2007). EPO prevents the loss of Wnt1 expression that would occur in the absence of EPO during elevated glucose. In studies that block Wnt1 with a Wnt1 antibody, EPO protection is neutralized, indicating that Wnt1 is vital for the protection of EPO during elevated glucose exposure such as DM (Chong et al., 2007). EPO also may require Wnt signaling for the preservation of mesenchymal stem cells (Danielyan et al., 2009), to control “pro-apoptotic” forkhead transcription factors in DM (Chong et al., 2011b), foster the maintenance of immune cells of the nervous system during oxidative stress (Shang et al., 2011), and block β-amyloid (Aβ) toxicity in microglia of the brain (Shang et al., 2012b).
Independent of EPO, Wnt1 and Wnt signaling can block autophagy (Wang et al., 2012b; Fu et al., 2014; Geng et al., 2014; Ortiz-Masia et al., 2014) and apoptotic endothelial cell injury during elevated glucose exposure (Chong et al., 2007) (Figure 1). Wnt signaling also promotes human β-cell proliferation (Aly et al., 2013), fosters the repair of diabetic wounds (Sun et al., 2014), impacts the vasculature of the brain (Guo et al., 2012), and prevents cognitive decline during aging and potential concomitant disease such as during DM (Bayod et al., 2014a). Components of the Wnt pathway also have increased expression in the brain during periods of exercise (Bayod et al., 2014b) that may assist against insulin resistance. Given the complexities of the Wnt signaling pathway and the ability of Wnt to promote angiogenesis (Chong et al., 2011a; Cui et al., 2012; Lee et al., 2012a; Maiese, 2014d), it should be noted that Wnt signaling in some cases can potentiate injury such as vascular leakage and inflammation during DM retinopathy (Lee et al., 2012a), promote retinal oxidative stress (Zhou et al., 2011; Liu et al., 2013c), and lead to keratoconus cornea (Iqbal et al., 2013). Furthermore, Wnt1 and Wnt signaling pathways are proliferative in nature and can result in tumorigenesis. In the nervous system Wnt signaling may lead to malignant glioma development (Liu et al., 2012a; Tu et al., 2013), malignant melanoma (Uzdensky et al., 2013), and metastatic disease (James et al., 2012; Kafka et al., 2014; Klinke, 2014; Knoblich et al., 2014). In addition, growth factors such as EPO with prolonged exposure can have non-beneficial effects such as the proliferation of cancer (Maiese et al., 2005a; Hedley et al., 2011; Zhang et al., 2014a), increased risk during cardiac conditions and hypertension (Palazzuoli et al., 2014), inflammation, and blood-brain barrier injury (Ogunshola et al., 2013).
A downstream target in the Wnt1 pathway is Wnt1 inducible signaling pathway protein 1 (WISP1), a protein that is present in the brain, epithelium, heart, kidney, lung, pancreas, placenta, ovaries, small intestine, and spleen (Maiese, 2014d). WISP1, also known as CCN4, is a member of the six secreted extracellular matrix associated CCN family of proteins that are mediators of skeletal system development, vascular repair, cellular survival, and extracellular matrix growth. The CCN term is defined by the first three members of the family that include Cysteine-rich protein 61, Connective tissue growth factor, and Nephroblastoma over-expressed gene.
Initial studies demonstrated that WISP1 stops p53 mediated DNA damage and apoptosis (Su et al., 2002). Subsequent work with WISP1 further illustrated the ability to prevent apoptosis (Price et al., 2004; Venkatesan et al., 2010; Wang et al., 2013), control caspase activation (Venkatesan et al., 2010; Wang et al., 2012a, 2013), and oversee autophagy (Maiese et al., 2012b; Wang et al., 2012b). For regeneration and/or repair of injury in the nervous system, WISP1 may have a critical role. The expression of WISP1 is increased during oxidative stress in neurons and the presence of WISP1 is necessary for neuronal protection by reducing the expression of the Bim/Bax complex, increasing the expression of Bclx(L)/Bax complex, and blocking cytochrome c release with caspase 3 activation (Wang et al., 2012a). WISP1 also autoregulates its own expression by maintaining the activity of β-catenin and limiting the induction of autophagy (Wang et al., 2012b). In addition, WISP1 can protect neurons by controlling the forkhead transcription factor FoxO3a, a modulator of cellular metabolism and cell survival (Maiese et al., 2008b; Chong et al., 2011b; Uranga et al., 2013; Fong et al., 2014; Safarian et al., 2014; Zeldich et al., 2014). Furthermore, WISP1 promotes the nuclear trafficking and increased activity of the silent mating type information regulation 2 homolog 1 (S. cerevisiae) (SIRT1) which can lead to neuronal protection (Wang et al., 2013) and block apoptotic injury (Hou et al., 2010b; Tanno et al., 2010; Hou et al., 2011).
In regards to DM and the control of cellular metabolism, WISP1 is one of several genes that are over-expressed during pancreatic regeneration, suggesting that WISP1 may oversee stem cell development during DM (Lim et al., 2002) (Figure 1). WISP1 can regulate induced pluripotent stem cell reprogramming (Yang et al., 2011a; Jung et al., 2014) and stem cell migration (Lough et al., 2013). Expression of WISP1 also is increased during human adipocyte differentiation (Murahovschi et al., 2014) and may support vascular regeneration during saphenous vein crush injury (Price et al., 2004). WISP1 fosters vascular smooth muscle proliferation that can assist with tissue repair during injury (Reddy et al., 2011; Liu et al., 2013a), but modulates cellular senescence (Du et al., 2014) and does not promote excessive cellular proliferation in aging vascular cells (Marchand et al., 2011), a component of atherosclerosis. WISP1 expression also is affected by weight change in humans and increases during insulin resistance in glucose-tolerant individuals (Murahovschi et al., 2014), indicating that WISP1 may represent an important reparative process in individuals with DM.
In relation to cellular mechanisms that impact DM, WISP1 employs metabolic pathways that involve the mechanistic target of rapamycin (mTOR) to prevent the injury to the central nervous system (Chong et al., 2012c; Maiese, 2014c). WISP1 through mTOR downstream pathways that modulate the proline rich Akt substrate 40 kDa (PRAS40) (Shang et al., 2012a) and tuberin (tuberous sclerosis 2) TSC2 (Shang et al., 2013) can increases cell survival for microglial cells against oxidative stress and Aβ toxicity. mTOR is closely tied to cellular metabolism (Maiese et al., 2013a, 2014a; Johnson et al., 2015) and independently can prevent apoptotic injury in pancreatic β-cells (Zhou et al., 2014a), lead to pancreatic β-cell proliferation (Miao et al., 2013), inhibit neuronal cell apoptosis during DM through the EGF receptor (Kimura et al., 2013), and limit vascular disease with atherosclerosis (Peng et al., 2014). WISP1 also controls the post-translational phosphorylation of AMP activated protein kinase (AMPK) that is involved in glucose homeostasis (Chong and Maiese, 2012; Maiese et al., 2013c; Kopp et al., 2014; Martinez de Morentin et al., 2014). AMPK regulates the activity of the hamartin (tuberous sclerosis 1)/tuberin (tuberous sclerosis 2) (TSC1/TSC2) complex that is an inhibitor of mTOR Complex 1 (mTORC1) (Maiese, 2014b). The ability of WISP1 to oversee AMPK activity is vital to control cellular metabolism during DM (Martinez de Morentin et al., 2014). WISP1 modulates AMPK activation by differentially decreasing phosphorylation of TSC2 at Ser1387, a target of AMPK, and increasing phosphorylation of TSC2 at Thr1462, a target of protein kinase B (Akt) (Shang et al., 2013). This enables WISP1 to provide a minimal level of TSC2 and AMPK activity to control both cell survival and cell metabolism (Shang et al., 2013). Under some scenarios, increased AMPK activity can reduce insulin resistance and diminished oxidative stress mediated through the activation of autophagy (Liu et al., 2014). AMPK activation also can result in correcting metabolic parameters of cells (Jessen et al., 2010) and prevent adipocyte differentiation, lipid accumulation, and obesity (Lai et al., 2012). Yet, the degree of AMPK activity remains an important consideration, since in some experimental models of Type 2 DM, AMPK activation promotes apoptotic cell death in pancreatic islet cells (Guan et al., 2014).
However, similar to the pathways of Wnt1, WISP1 is a proliferative agent and may have a role in tumor cell development and proliferation (Maiese, 2014d) (Figure 1). Under some circumstances, WISP1 independently may result in cancer growth (Klinke, 2014) and increased combined expression of Wnt1, WISP1, survivin, and cyclin-D1 may be suggestive that these pathways work synergistically to lead to tumorigenesis with the inhibition of apoptosis (Khor et al., 2006). During chronic ethanol consumption, WISP1 is associated with hepatic cell proliferation that may be not only reparative, but also associated with liver cancer (Mercer et al., 2014). WISP1 expression in the nervous system also is increased in neurofibromatosis type 1 tumorigenesis (Pasmant et al., 2010). Variants of WISP1 have been described to be extremely aggressive in promoting cell growth (Tanaka et al., 2003), but non-variant WISP1 expression may block tumor cell invasion, motility, and metastases (Soon et al., 2003). Differential expression of CCN family members in breast cancer also has suggested that WISP1 may function to limit breast cancer growth (Davies et al., 2007) and Notch1 activation that leads to increased WISP1 expression can suppress melanoma growth (Shao et al., 2011). Yet, WISP1 may be able to limit metastatic disease only under certain cellular conditions, since some studies also suggest that WISP1 may promote distant metastatic disease (Ono et al., 2013).
Future Considerations for Promoting Neuronal Protection in DM
DM can lead to significant complications in the central as well as the peripheral nervous systems. Complications can include loss of vision due to retinal disease, impaired cognition with dementia that my involve Alzheimer's disease, destruction of the blood brain barrier that results in ischemic cerebral disease, and peripheral nerve dysfunction. At the cellular level, neuronal cell injury during DM can occur through oxidative stress and the generation of ROS that ultimately lead to apoptosis and autophagy. Although apoptosis usually results in cell death, autophagy under some circumstances can be protective during DM and may control insulin resistance and prevent β-cell dysfunction.
Given the complex cellular processes that can result in neuronal cell injury during metabolic disease, novel targeting with trophic factors, Wnt, WISP1, and the oversight of stem cell proliferation may offer new strategies to prevent the complications of DM in the nervous system. Growth factors such as IGF-1, FGF, EGF, and EPO can modulate glucose homeostasis and prevent neuronal injury during oxidative stress and DM. EPO also employs pathways of Wnt signaling to protect against cerebral endothelial cell injury, block “pro-apoptotic” pathways, and maintain the integrity of immune cells of the nervous system. Independently, Wnt signaling that involves Wnt1 and WISP1 (CCN4) is becoming recognized as a vital neuroprotective component during DM to modulate stem cell proliferation, repair diabetic wounds, reverse cognitive decline, increase human β-cell proliferation, promote vascular regeneration, and control programmed cell death through apoptosis and autophagy. Cellular mechanisms of Wnt and WISP1 govern primary metabolic pathways of mTOR and AMPK. However, it appears that the degree of activation of these biological systems is an important consideration in developing therapies for DM, since Wnt signaling as well as growth factors can affect vascular leakage in sensitive regions such as the retina as well as promote tumor development in the nervous system. WISP1, also a proliferative protein, can similarly lead to tumor growth while promoting reparative regeneration of tissues. Downstream, AMPK under some scenarios may result in the death of pancreatic islet cells. Yet, WISP1 also has been reported not only to be neuroprotective especially during DM, but also potentially block the spread of metastatic disease. Future development of novel strategies for metabolic disease in the nervous system must continue to elucidate the potential varied clinical outcomes of the Wnt and WISP1 pathways and precisely target mechanisms that drive outcomes for neuronal repair and regeneration.
Footnotes
Funding: This research was supported by the following grants to KM: American Diabetes Association, American Heart Association, NIH NIEHS, NIH NIA, NIH NINDS, and NIH ARRA.
References
- Akasaki Y, Alvarez-Garcia O, Saito M, Carames B, Iwamoto Y, Lotz MK. FOXO transcription factors support oxidative stress resistance in human chondrocytes. Arthritis Rheumatol. 2014;66:3349–3358. doi: 10.1002/art.38868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aksu I, Ates M, Baykara B, Kiray M, Sisman AR, Buyuk E, Baykara B, Cetinkaya C, Gumus H, Uysal N. Anxiety correlates to decreased blood and prefrontal cortex IGF-1 levels in streptozotocin induced diabetes. Neurosci Lett. 2012;531:176–181. doi: 10.1016/j.neulet.2012.10.045. [DOI] [PubMed] [Google Scholar]
- Aly H, Rohatgi N, Marshall CA, Grossenheider TC, Miyoshi H, Stappenbeck TS, Matkovich SJ, McDaniel ML. A novel strategy to increase the proliferative potential of adult human beta-cells while maintaining their differentiated phenotype. PLoS One. 2013;8:e66131. doi: 10.1371/journal.pone.0066131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arunachalam G, Samuel SM, Marei I, Ding H, Triggle CR. Metformin modulates hyperglycaemia-induced endothelial senescence and apoptosis through SIRT1. Br J Pharmacol. 2014;171:523–535. doi: 10.1111/bph.12496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asaithambi A, Ay M, Jin H, Gosh A, Anantharam V, Kanthasamy A, Kanthasamy AG. Protein kinase D1 (PKD1) phosphorylation promotes dopaminergic neuronal survival during 6-OHDA-induced oxidative stress. PLoS One. 2014;9:e96947. doi: 10.1371/journal.pone.0096947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagul PK, Banerjee SK. Insulin resistance, oxidative stress and cardiovascular complications: role of sirtuins. Curr Pharm Des. 2013;19:5663–5677. doi: 10.2174/13816128113199990372. [DOI] [PubMed] [Google Scholar]
- Barthelmes D, Zhu L, Shen W, Gillies MC, Irhimeh MR. Differential gene expression in Lin-/VEGF-R2+ bone marrow-derived endothelial progenitor cells isolated from diabetic mice. Cardiovasc Diabetol. 2014;13:42. doi: 10.1186/1475-2840-13-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bayod S, Felice P, Andres P, Rosa P, Camins A, Pallas M, Canudas AM. Downregulation of canonical Wnt signaling in hippocampus of SAMP8 mice. Neurobiol Aging. 2014a;36:720–729. doi: 10.1016/j.neurobiolaging.2014.09.017. [DOI] [PubMed] [Google Scholar]
- Bayod S, Menella I, Sanchez-Roige S, Lalanza JF, Escorihuela RM, Camins A, Pallas M, Canudas AM. Wnt pathway regulation by long-term moderate exercise in rat hippocampus. Brain Res. 2014b;1543:38–48. doi: 10.1016/j.brainres.2013.10.048. [DOI] [PubMed] [Google Scholar]
- Berwick DC, Harvey K. The regulation and deregulation of Wnt signaling by PARK genes in health and disease. J Mol Cell Biol. 2014;6:3–12. doi: 10.1093/jmcb/mjt037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowes Rickman C, Farsiu S, Toth CA, Klingeborn M. Dry age-related macular degeneration: mechanisms, therapeutic targets, and imaging. Invest Ophthalmol Vis Sci. 2013;54:ORSF68–80. doi: 10.1167/iovs.13-12757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Busch S, Kannt A, Kolibabka M, Schlotterer A, Wang Q, Lin J, Feng Y, Hoffmann S, Gretz N, Hammes HP. Systemic treatment with erythropoietin protects the neurovascular unit in a rat model of retinal neurodegeneration. PLoS One. 2014;9:e102013. doi: 10.1371/journal.pone.0102013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai Z, Yan LJ. Rapamycin, autophagy, and Alzheimer's disease. J Biochem Pharmacol Res. 2013;1:84–90. [PMC free article] [PubMed] [Google Scholar]
- Cardoso S, Santos RX, Correia SC, Carvalho C, Santos MS, Baldeiras I, Oliveira CR, Moreira PI. Insulin-induced recurrent hypoglycemia exacerbates diabetic brain mitochondrial dysfunction and oxidative imbalance. Neurobiol Dis. 2012;49C:1–12. doi: 10.1016/j.nbd.2012.08.008. [DOI] [PubMed] [Google Scholar]
- Carneiro J, Duarte-Pereira S, Azevedo L, Castro LF, Aguiar P, Moreira IS, Amorim A, Silva RM. The evolutionary portrait of metazoan NAD salvage. PLoS One. 2013;8:e64674. doi: 10.1371/journal.pone.0064674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caron AZ, He X, Mottawea W, Seifert EL, Jardine K, Dewar-Darch D, Cron GO, Harper ME, Stintzi A, McBurney MW. The SIRT1 deacetylase protects mice against the symptoms of metabolic syndrome. FASEB J. 2014;28:1306–1316. doi: 10.1096/fj.13-243568. [DOI] [PubMed] [Google Scholar]
- Castaneda-Arellano R, Beas-Zarate C, Feria-Velasco AI, Bitar-Alatorre EW, Rivera-Cervantes MC. From neurogenesis to neuroprotection in the epilepsy: signalling by erythropoietin. Front Biosci (Landmark Ed) 2014;19:1445–1455. doi: 10.2741/4295. [DOI] [PubMed] [Google Scholar]
- Atlanta, GA: US Department of Health and Human Services; Centers for Disease Control and Prevention (2014) National Diabetes Statistics Report: Estimates of Diabetes and Its Burden in the United States. [Google Scholar]
- Chamorro ME, Wenker SD, Vota DM, Vittori DC, Nesse AB. Signaling pathways of cell proliferation are involved in the differential effect of erythropoietin and its carbamylated derivative. Biochim Biophys Acta. 2013;1833:1960–1968. doi: 10.1016/j.bbamcr.2013.04.006. [DOI] [PubMed] [Google Scholar]
- Chen JX, Tuo Q, Liao DF, Zeng H. (2012) Inhibition of protein tyrosine phosphatase improves angiogenesis via enhancing Ang-1/Tie-2 signaling in diabetes. Exp Diabetes Res. 2012 doi: 10.1155/2012/836759. 836759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Q, Yu W, Shi J, Shen J, Gao T, Zhang J, Xi F, Li J, Li N. Insulin alleviates the inflammatory response and oxidative stress injury in cerebral tissues in septic rats. J Inflamm (Lond) 2014a;11:18. doi: 10.1186/1476-9255-11-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen W, Sun Y, Liu K, Sun X. Autophagy: a double-edged sword for neuronal survival after cerebral ischemia. Neural Regen Res. 2014b;9:1210–1216. doi: 10.4103/1673-5374.135329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y, Liu XR, Yin YQ, Lee CJ, Wang FT, Liu HQ, Wu XT, Liu J. Unravelling the multifaceted roles of Atg proteins to improve cancer therapy. Cell Prolif. 2014c;47:105–112. doi: 10.1111/cpr.12095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi D, Schroer SA, Lu SY, Wang L, Wu X, Liu Y, Zhang Y, Gaisano HY, Wagner KU, Wu H, Retnakaran R, Woo M. Erythropoietin protects against diabetes through direct effects on pancreatic beta cells. J Exp Med. 2010;207:2831–2842. doi: 10.1084/jem.20100665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chong ZZ, Maiese K. The Src homology 2 domain tyrosine phosphatases SHP-1 and SHP-2: diversified control of cell growth, inflammation, and injury. Histol Histopathol. 2007;22:1251–1267. doi: 10.14670/hh-22.1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chong ZZ, Maiese K. Mammalian target of rapamycin signaling in diabetic cardiovascular disease. Cardiovasc Diabetol. 2012;11:45. doi: 10.1186/1475-2840-11-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chong ZZ, Kang JQ, Maiese K. Erythropoietin is a novel vascular protectant through activation of Akt1 and mitochondrial modulation of cysteine proteases. Circulation. 2002;106:2973–2979. doi: 10.1161/01.cir.0000039103.58920.1f. [DOI] [PubMed] [Google Scholar]
- Chong ZZ, Kang JQ, Maiese K. Apaf-1, Bcl-xL, cytochrome c, and caspase-9 form the critical elements for cerebral vascular protection by erythropoietin. J Cereb Blood Flow Metab. 2003;23:320–330. doi: 10.1097/01.WCB.0000050061.57184.AE. [DOI] [PubMed] [Google Scholar]
- Chong ZZ, Li F, Maiese K. Stress in the brain: novel cellular mechanisms of injury linked to Alzheimer's disease. Brain Res Brain Res Rev. 2005a;49:1–21. doi: 10.1016/j.brainresrev.2004.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chong ZZ, Li F, Maiese K. Oxidative stress in the brain: Novel cellular targets that govern survival during neurodegenerative disease. Prog Neurobiol. 2005b;75:207–246. doi: 10.1016/j.pneurobio.2005.02.004. [DOI] [PubMed] [Google Scholar]
- Chong ZZ, Li F, Maiese K. Attempted cell cycle induction in post-mitotic neurons occurs in early and late apoptotic programs through Rb, E2F1, and caspase 3. Curr Neurovasc Res. 2006;3:25–39. doi: 10.2174/156720206775541741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chong ZZ, Shang YC, Maiese K. Vascular injury during elevated glucose can be mitigated by erythropoietin and Wnt signaling. Curr Neurovasc Res. 2007;4:194–204. doi: 10.2174/156720207781387150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chong ZZ, Shang YC, Maiese K. Cardiovascular disease and mTOR signaling. Trends Cardiovasc Med. 2011a;21:151–155. doi: 10.1016/j.tcm.2012.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chong ZZ, Shang YC, Hou J, Maiese K. Wnt1 neuroprotection translates into improved neurological function during oxidant stress and cerebral ischemia through AKT1 and mitochondrial apoptotic pathways. Oxid Med Cell Longev. 2010;3:153–165. doi: 10.4161/oxim.3.2.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chong ZZ, Shang YC, Wang S, Maiese K. SIRT1: New avenues of discovery for disorders of oxidative stress. Expert opinion on therapeutic targets. 2012a;16:167–178. doi: 10.1517/14728222.2012.648926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chong ZZ, Shang YC, Wang S, Maiese K. PRAS40 is an integral regulatory component of erythropoietin mTOR signaling and cytoprotection. PLoS One. 2012b;7:e45456. doi: 10.1371/journal.pone.0045456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chong ZZ, Shang YC, Wang S, Maiese K. Shedding new light on neurodegenerative diseases through the mammalian target of rapamycin. Prog Neurobiol. 2012c;99:128–148. doi: 10.1016/j.pneurobio.2012.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chong ZZ, Hou J, Shang YC, Wang S, Maiese K. EPO relies upon novel signaling of Wnt1 that requires Akt1, FoxO3a, GSK-3β, and β-catenin to foster vascular integrity during experimental diabetes. Curr Neurovasc Res. 2011b;8:103–120. doi: 10.2174/156720211795495402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colella P, Iodice C, Di Vicino U, Annunziata I, Surace EM, Auricchio A. Non-erythropoietic erythropoietin derivatives protect from light-induced and genetic photoreceptor degeneration. Hum Mol Genet. 2011;20:2251–2262. doi: 10.1093/hmg/ddr115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui J, Jiang W, Wang S, Wang L, Xie K. Role of Wnt/beta-catenin signaling in drug resistance of pancreatic cancer. Curr Pharm Des. 2012;18:2464–2471. doi: 10.2174/13816128112092464. [DOI] [PubMed] [Google Scholar]
- Czubak P, Bojarska-Junak A, Tabarkiewicz J, Putowski L. (2014) A modified method of insulin producing cells’ generation from bone marrow-derived mesenchymal stem cells. J Diabetes Res. 2014 doi: 10.1155/2014/628591. 628591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damasceno DC, Sinzato YK, Bueno A, Netto AO, Dallaqua B, Gallego FQ, Iessi IL, Corvino SB, Serrano RG, Marini G, Piculo F, Calderon IM, Rudge MV. (2013) Mild diabetes models and their maternal-fetal repercussions. J Diabetes Res. 2013 doi: 10.1155/2013/473575. 473575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dang J, Jia R, Tu Y, Xiao S, Ding G. Erythropoietin prevents reactive oxygen species generation and renal tubular cell apoptosis at high glucose level. Biomed Pharmacother. 2010;64:681–685. doi: 10.1016/j.biopha.2010.06.011. [DOI] [PubMed] [Google Scholar]
- Danielyan L, Schafer R, Schulz A, Ladewig T, Lourhmati A, Buadze M, Schmitt AL, Verleysdonk S, Kabisch D, Koeppen K, Siegel G, Proksch B, Kluba T, Eckert A, Kohle C, Schoneberg T, Northoff H, Schwab M, Gleiter CH. Survival, neuron-like differentiation and functionality of mesenchymal stem cells in neurotoxic environment: the critical role of erythropoietin. Cell Death Differ. 2009;16:1599–1614. doi: 10.1038/cdd.2009.95. [DOI] [PubMed] [Google Scholar]
- Das F, Dey N, Venkatesan B, Kasinath BS, Ghosh-Choudhury N, Choudhury GG. High glucose upregulation of early-onset Parkinson's disease protein DJ-1 integrates the PRAS40/TORC1 axis to mesangial cell hypertrophy. Cell Signal. 2011;23:1311–1319. doi: 10.1016/j.cellsig.2011.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies SR, Watkins G, Mansel RE, Jiang WG. Differential expression and prognostic implications of the CCN family members WISP-1, WISP-2, and WISP-3 in human breast cancer. Ann Surg Oncol. 2007;14:1909–1918. doi: 10.1245/s10434-007-9376-x. [DOI] [PubMed] [Google Scholar]
- Deng X, Cheng J, Zhang Y, Li N, Chen L. Effects of caloric restriction on SIRT1 expression and apoptosis of islet beta cells in type 2 diabetic rats. Acta Diabetol 47 Suppl. 2009;1:177–185. doi: 10.1007/s00592-009-0159-7. [DOI] [PubMed] [Google Scholar]
- Domin H, Jantas D, Smialowska M. Neuroprotective effects of the allosteric agonist of metabotropic glutamate receptor 7 AMN082 on oxygen-glucose deprivation- and kainate-induced neuronal cell death. Neurochem Int. 2015 doi: 10.1016/j.neuint.2014.12.010. doi: 10.1016/j.neuint.2014.12.010. [DOI] [PubMed] [Google Scholar]
- Domin H, Golembiowska K, Jantas D, Kaminska K, Zieba B, Smialowska M. Group III mGlu receptor agonist, ACPT-I, exerts potential neuroprotective effects in vitro and in vivo. Neurotox Res. 2014;26:99–113. doi: 10.1007/s12640-013-9455-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du J, Klein JD, Hassounah F, Zhang J, Zhang C, Wang XH. Aging increases CCN1 expression leading to muscle senescence. Am J Physiol Cell Physiol. 2014;306:C28–36. doi: 10.1152/ajpcell.00066.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du LL, Chai DM, Zhao LN, Li XH, Zhang FC, Zhang HB, Liu LB, Wu K, Liu R, Wang JZ, Zhou XW. AMPK activation ameliorates Alzheimer's disease-like pathology and spatial memory impairment in a streptozotocin-induced Alzheimer's disease model in rats. J Alzheimers Dis. 2015;43:775–784. doi: 10.3233/JAD-140564. [DOI] [PubMed] [Google Scholar]
- Essser N, Paquot N, Scheen AJ. Anti-inflammatory agents to treat or prevent type 2 diabetes, metabolic syndrome and cardiovascular disease. Expert Opin Investig Drugs. 2014;24:1–25. doi: 10.1517/13543784.2015.974804. [DOI] [PubMed] [Google Scholar]
- Favaloro B, Allocati N, Graziano V, Di Ilio C, De Laurenzi V. Role of apoptosis in disease. Aging (Albany NY) 2012;4:330–349. doi: 10.18632/aging.100459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folch J, Junyent F, Verdaguer E, Auladell C, Pizarro JG, Beas-Zarate C, Pallas M, Camins A. Role of cell cycle re-entry in neurons: a common apoptotic mechanism of neuronal cell death. Neurotox Res. 2012;22:195–207. doi: 10.1007/s12640-011-9277-4. [DOI] [PubMed] [Google Scholar]
- Fong Y, Lin YC, Wu CY, Wang HM, Lin LL, Chou HL, Teng YN, Yuan SS, Chiu CC. (2014) The antiproliferative and apoptotic effects of sirtinol, a sirtuin inhibitor on human lung cancer cells by modulating Akt/beta-catenin-Foxo3a axis. ScientificWorldJournal. 2014 doi: 10.1155/2014/937051. 937051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fraineau S, Pal CG, 2nd, Allan DS, Brand M. Epigenetic regulation of endothelial-cell-mediated vascular repair. FEBS J. 2014 doi: 10.1111/febs.13183. doi: 10.1111/febs.13183. [DOI] [PubMed] [Google Scholar]
- Fu D, Wu M, Zhang J, Du M, Yang S, Hammad SM, Wilson K, Chen J, Lyons TJ. Mechanisms of modified LDL-induced pericyte loss and retinal injury in diabetic retinopathy. Diabetologia. 2012;55:3128–3140. doi: 10.1007/s00125-012-2692-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu Y, Chang H, Peng X, Bai Q, Yi L, Zhou Y, Zhu J, Mi M. Resveratrol inhibits breast cancer stem-like cells and induces autophagy via suppressing Wnt/beta-catenin signaling pathway. PLoS One. 2014;9:e102535. doi: 10.1371/journal.pone.0102535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geldman A, Pallen CJ. Protein tyrosine phosphatases in mast cell signaling. Methods Mol Biol. 2015;1220:269–286. doi: 10.1007/978-1-4939-1568-2_17. [DOI] [PubMed] [Google Scholar]
- Geng Y, Ju Y, Ren F, Qiu Y, Tomita Y, Tomoeda M, Kishida M, Wang Y, Jin L, Su F, Wei C, Jia B, Li Y, Chang Z. Insulin receptor substrate 1/2 (IRS1/2) regulates Wnt/beta-catenin signaling through blocking autophagic degradation of dishevelled2. J Biol Chem. 2014;289:11230–11241. doi: 10.1074/jbc.M113.544999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gezginci-Oktayoglu S, Sacan O, Bolkent S, Ipci Y, Kabasakal L, Sener G, Yanardag R. Chard (Beta vulgaris L. var. cicla) extract ameliorates hyperglycemia by increasing GLUT2 through Akt2 and antioxidant defense in the liver of rats. Acta histochemica. 2014;116:32–39. doi: 10.1016/j.acthis.2013.04.016. [DOI] [PubMed] [Google Scholar]
- Ghasemi A, Khalifi S, Jedi S. Streptozotocin-nicotinamide-induced rat model of type 2 diabetes. Acta Physiol Hung. 2014;101:408–420. doi: 10.1556/APhysiol.101.2014.4.2. [DOI] [PubMed] [Google Scholar]
- Gomes MB, Negrato CA. Alpha-lipoic acid as a pleiotropic compound with potential therapeutic use in diabetes and other chronic diseases. Diabetol Metab Syndr. 2014;6:80. doi: 10.1186/1758-5996-6-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez-Fernandez C, Fernandez-Martos CM, Shields S, Arenas E, Rodriguez FJ. Wnts are expressed in the spinal cord of adult mice and are differentially induced after injury. J Neurotrauma. 2013;31:565–581. doi: 10.1089/neu.2013.3067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan FY, Gu J, Li W, Zhang M, Ji Y, Li J, Chen L, Hatch GM. Compound K protects pancreatic islet cells against apoptosis through inhibition of the AMPK/JNK pathway in type 2 diabetic mice and in MIN6 beta-cells. Life Sci. 2014;107:42–49. doi: 10.1016/j.lfs.2014.04.034. [DOI] [PubMed] [Google Scholar]
- Guo S, Zhou Y, Xing C, Lok J, Som AT, Ning M, Ji X, Lo EH. The vasculome of the mouse brain. PLoS One. 2012;7:e52665. doi: 10.1371/journal.pone.0052665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halperin-Sheinfeld M, Gertler A, Okun E, Sredni B, Cohen HY. The Tellurium compound, AS101, increases SIRT1 level and activity and prevents type 2 diabetes. Aging (Albany NY) 2012;4:436–447. doi: 10.18632/aging.100468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamed S, Bennett CL, Demiot C, Ullmann Y, Teot L, Desmouliere A. Erythropoietin, a novel repurposed drug: an innovative treatment for wound healing in patients with diabetes mellitus. Wound Repair Regen. 2014;22:23–33. doi: 10.1111/wrr.12135. [DOI] [PubMed] [Google Scholar]
- Hamed S, Ullmann Y, Egozi D, Daod E, Hellou E, Ashkar M, Gilhar A, Teot L. Fibronectin potentiates topical erythropoietin-induced wound repair in diabetic mice. J Invest Dermatol. 2011;131:1365–1374. doi: 10.1038/jid.2011.15. [DOI] [PubMed] [Google Scholar]
- Harish G, Mahadevan A, Pruthi N, Sreenivasamurthy SK, Puttamallesh VN, Keshava Prasad TS, Shankar SK, M MS. Characterization of traumatic brain injury in human brains reveals distinct cellular and molecular changes in contusion and pericontusion. J Neurochem. 2015 doi: 10.1111/jnc.13082. doi: 10.1111/jnc.13082. [DOI] [PubMed] [Google Scholar]
- He C, Bassik MC, Moresi V, Sun K, Wei Y, Zou Z, An Z, Loh J, Fisher J, Sun Q, Korsmeyer S, Packer M, May HI, Hill JA, Virgin HW, Gilpin C, Xiao G, Bassel-Duby R, Scherer PE, Levine B. Exercise-induced BCL2-regulated autophagy is required for muscle glucose homeostasis. Nature. 2012;481:511–515. doi: 10.1038/nature10758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedley BD, Allan AL, Xenocostas A. The role of erythropoietin and erythropoiesis-stimulating agents in tumor progression. Clin Cancer Res. 2011;17:6373–6380. doi: 10.1158/1078-0432.CCR-10-2577. [DOI] [PubMed] [Google Scholar]
- Heo J, Ahn EK, Jeong HG, Kim YH, Leem SH, Lee SJ, Park EK, Yang M. Transcriptional characterization of Wnt pathway during sequential hepatic differentiation of human embryonic stem cells and adipose tissue-derived stem cells. Biochem Biophys Res Commun. 2013;434:235–240. doi: 10.1016/j.bbrc.2013.02.109. [DOI] [PubMed] [Google Scholar]
- Hou J, Chong ZZ, Shang YC, Maiese K. FoxO3a governs early and late apoptotic endothelial programs during elevated glucose through mitochondrial and caspase signaling. Mol Cell Endocrinol. 2010a;321:194–206. doi: 10.1016/j.mce.2010.02.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hou J, Chong ZZ, Shang YC, Maiese K. Early apoptotic vascular signaling is determined by Sirt1 through nuclear shuttling, forkhead trafficking, bad, and mitochondrial caspase activation. Curr Neurovasc Res. 2010b;7:95–112. doi: 10.2174/156720210791184899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hou J, Wang S, Shang YC, Chong ZZ, Maiese K. Erythropoietin employs cell longevity pathways of SIRT1 to foster endothelial vascular integrity during oxidant stress. Curr Neurovasc Res. 2011;8:220–235. doi: 10.2174/156720211796558069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hralova M, Angerova Y, Gueye T, Bortelova J, Svestkova O, Zima T, Lippertova-Grunerova M. Long-term results of enriched environment and erythropoietin after hypobaric hypoxia in rats. Physiol Res. 2013;62:463–470. doi: 10.33549/physiolres.932354. [DOI] [PubMed] [Google Scholar]
- Hu P, Lai D, Lu P, Gao J, He H. ERK and Akt signaling pathways are involved in advanced glycation end product-induced autophagy in rat vascular smooth muscle cells. Int J Mol Med. 2012;29:613–618. doi: 10.3892/ijmm.2012.891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iqbal O, Fisher G, Vira S, Syed D, Sadeghi N, Freeman D, Campbell E, Sugar J, Feder R, Fareed J, Bouchard C. Increased expression of secreted frizzled-related protein-1 and microtubule-associated protein light chain 3 in keratoconus. Cornea. 2013;32:702–707. doi: 10.1097/ICO.0b013e318282987a. [DOI] [PubMed] [Google Scholar]
- James RG, Davidson KC, Bosch KA, Biechele TL, Robin NC, Taylor RJ, Major MB, Camp ND, Fowler K, Martins TJ, Moon RT. WIKI4, a novel inhibitor of tankyrase and Wnt/ss-catenin signaling. PLoS One. 2012;7:e50457. doi: 10.1371/journal.pone.0050457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jantas D, Greda A, Golda S, Korostynski M, Grygier B, Roman A, Pilc A, Lason W. Neuroprotective effects of metabotropic glutamate receptor group II and III activators against MPP(+)-induced cell death in human neuroblastoma SH-SY5Y cells: the impact of cell differentiation state. Neuropharmacology. 2014;83:36–53. doi: 10.1016/j.neuropharm.2014.03.019. [DOI] [PubMed] [Google Scholar]
- Jenwitheesuk A, Nopparat C, Mukda S, Wongchitrat P, Govitrapong P. Melatonin regulates aging and neurodegeneration through energy metabolism, epigenetics, autophagy and circadian rhythm pathways. Int J Mol Sci. 2014;15:16848–16884. doi: 10.3390/ijms150916848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jessen N, Koh HJ, Folmes CD, Wagg C, Fujii N, Lofgren B, Wolf CM, Berul CI, Hirshman MF, Lopaschuk GD, Goodyear LJ. Ablation of LKB1 in the heart leads to energy deprivation and impaired cardiac function. Biochim Biophys Acta. 2010;1802:593–600. doi: 10.1016/j.bbadis.2010.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jia G, Aroor AR, Martinez-Lemus LA, Sowers JR. Over-nutrition mTOR signaling and cardiovascular diseases. Am J Physiol Regul Integr Comp Physiol. 2014;307:R1198–1206. doi: 10.1152/ajpregu.00262.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang T, Yu JT, Zhu XC, Wang HF, Tan MS, Cao L, Zhang QQ, Gao L, Shi JQ, Zhang YD, Tan L. Acute metformin preconditioning confers neuroprotection against focal cerebral ischaemia by pre-activation of AMPK-dependent autophagy. Br J Pharmacol. 2014;171:3146–3157. doi: 10.1111/bph.12655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- John CM, Ramasamy R, Al Naqeeb G, Dhiab Al-Nuaimi AH, Adam A. Enhanced CD4 + CD25 + regulatory T cells with splenic proliferation and protection against oxidative stress by nicotinamide in gestational diabetes. Curr Med Chem. 2012 Epub ahead of print. [PubMed] [Google Scholar]
- Johnson SC, Sangesland M, Kaeberlein M, Rabinovitch PS. Modulating mTOR in aging and health. Interdiscip Top Gerontol. 2015;40:107–127. doi: 10.1159/000364974. [DOI] [PubMed] [Google Scholar]
- Jung DW, Kim WH, Williams DR. Reprogram or reboot: small molecule approaches for the production of induced pluripotent stem cells and direct cell reprogramming. ACS Chem Biol. 2014;9:80–95. doi: 10.1021/cb400754f. [DOI] [PubMed] [Google Scholar]
- Kafka A, Basic-Kinda S, Pecina-Slaus N. The cellular story of dishevelleds. Croat Med J. 2014;55:459–467. doi: 10.3325/cmj.2014.55.459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang J, Yun JY, Hur J, Kang JA, Choi JI, Ko SB, Lee J, Kim JY, Hwang IC, Park YB, Kim HS. Erythropoietin priming improves the vasculogenic potential of G-CSF mobilized human peripheral blood mononuclear cells. Cardiovasc Res. 2014;104:171–182. doi: 10.1093/cvr/cvu180. [DOI] [PubMed] [Google Scholar]
- Kapogiannis D, Boxer A, Schwartz JB, Abner EL, Biragyn A, Masharani U, Frassetto L, Petersen RC, Miller BL, Goetzl EJ. Dysfunctionally phosphorylated type 1 insulin receptor substrate in neural-derived blood exosomes of preclinical Alzheimer's disease. FASEB J. 2014;29:589–596. doi: 10.1096/fj.14-262048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz O, Stuible M, Golishevski N, Lifshitz L, Tremblay ML, Gassmann M, Mittelman M, Neumann D. Erythropoietin treatment leads to reduced blood glucose levels and body mass: insights from murine models. J Endocrinol. 2010;205:87–95. doi: 10.1677/JOE-09-0425. [DOI] [PubMed] [Google Scholar]
- Khor TO, Gul YA, Ithnin H, Seow HF. A comparative study of the expression of Wnt-1, WISP-1, survivin and cyclin-D1 in colorectal carcinoma. Int J Colorectal Dis. 2006;21:291–300. doi: 10.1007/s00384-005-0002-8. [DOI] [PubMed] [Google Scholar]
- Kim KA, Shin YJ, Akram M, Kim ES, Choi KW, Suh H, Lee CH, Bae ON. High glucose condition induces autophagy in endothelial progenitor cells contributing to angiogenic impairment. Biol Pharm Bull. 2014;37:1248–1252. doi: 10.1248/bpb.b14-00172. [DOI] [PubMed] [Google Scholar]
- Kim S, Kang IH, Nam JB, Cho Y, Chung DY, Kim SH, Kim JS, Cho YD, Hong EK, Sohn NW, Shin JW. Ameliorating the effect of astragaloside IV on learning and memory deficit after chronic cerebral hypoperfusion in rats. Molecules. 2015;20:1904–1921. doi: 10.3390/molecules20021904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimura R, Okouchi M, Kato T, Imaeda K, Okayama N, Asai K, Joh T. Epidermal growth factor receptor transactivation is necessary for glucagon-like peptide-1 to protect PC12 cells from apoptosis. Neuroendocrinology. 2013;97:300–308. doi: 10.1159/000345529. [DOI] [PubMed] [Google Scholar]
- Klinke DJ., 2nd Induction of Wnt-inducible signaling protein-1 correlates with invasive breast cancer oncogenesis and reduced type 1 cell-mediated cytotoxic immunity: a retrospective study. PLoS Comput Biol. 2014;10:e1003409. doi: 10.1371/journal.pcbi.1003409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knoblich K, Wang HX, Sharma C, Fletcher AL, Turley SJ, Hemler ME. Tetraspanin TSPAN12 regulates tumor growth and metastasis and inhibits beta-catenin degradation. Cell Mol Life Sci. 2014;71:1305–1314. doi: 10.1007/s00018-013-1444-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kopp C, Hosseini A, Singh SP, Regenhard P, Khalilvandi-Behroozyar H, Sauerwein H, Mielenz M. Nicotinic acid increases adiponectin secretion from differentiated bovine preadipocytes through G-protein coupled receptor signaling. Int J Mol Sci. 2014;15:21401–21418. doi: 10.3390/ijms151121401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurban S, Mehmetoglu I, Yerlikaya HF, Gonen S, Erdem S. Effect of chronic regular exercise on serum ischemia-modified albumin levels and oxidative stress in type 2 diabetes mellitus. Endocr Res. 2011;36:116–123. doi: 10.3109/07435800.2011.566236. [DOI] [PubMed] [Google Scholar]
- Kwon MS, Kim MH, Kim SH, Park KD, Yoo SH, Oh IU, Pak S, Seo YJ. Erythropoietin exerts cell protective effect by activating PI3K/Akt and MAPK pathways in C6 Cells. Neurol Res. 2014;36:215–223. doi: 10.1179/1743132813Y.0000000284. [DOI] [PubMed] [Google Scholar]
- Lai CS, Tsai ML, Badmaev V, Jimenez M, Ho CT, Pan MH. Xanthigen suppresses preadipocyte differentiation and adipogenesis through down-regulation of PPARgamma and C/EBPs and modulation of SIRT-1, AMPK, and FoxO pathways. J Agric Food Chem. 2012;60:1094–1101. doi: 10.1021/jf204862d. [DOI] [PubMed] [Google Scholar]
- Lee JH, Lee JH, Jin M, Han SD, Chon GR, Kim IH, Kim S, Kim SY, Choi SB, Noh YH. Diet control to achieve euglycemia induces significant loss of heart and liver weight via increased autophagy compared with ad libitum diet in diabetic rats. Exp Mol Med. 2014;46:e111. doi: 10.1038/emm.2014.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee K, Hu Y, Ding L, Chen Y, Takahashi Y, Mott R, Ma JX. Therapeutic potential of a monoclonal antibody blocking the Wnt pathway in diabetic retinopathy. Diabetes. 2012a;61:2948–2957. doi: 10.2337/db11-0300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee Y, Hong Y, Lee SR, Chang KT. Autophagy contributes to retardation of cardiac growth in diabetic rats. Lab Anim Res. 2012b;28:99–107. doi: 10.5625/lar.2012.28.2.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li F, Chong ZZ, Maiese K. Winding through the WNT pathway during cellular development and demise. Histol Histopathol. 2006;21:103–124. doi: 10.14670/hh-21.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li RP, Wang ZZ, Sun MX, Hou XL, Sun Y, Deng ZF, Xiao K. Polydatin protects learning and memory impairments in a rat model of vascular dementia. Phytomedicine. 2012;19:677–681. doi: 10.1016/j.phymed.2012.03.002. [DOI] [PubMed] [Google Scholar]
- Lim HW, Lee JE, Shin SJ, Lee YE, Oh SH, Park JY, Seong JK, Park JS. Identification of differentially expressed mRNA during pancreas regeneration of rat by mRNA differential display. Biochem Biophys Res Commun. 2002;299:806–812. doi: 10.1016/s0006-291x(02)02741-9. [DOI] [PubMed] [Google Scholar]
- Lim YM, Lim H, Hur KY, Quan W, Lee HY, Cheon H, Ryu D, Koo SH, Kim HL, Kim J, Komatsu M, Lee MS. Systemic autophagy insufficiency compromises adaptation to metabolic stress and facilitates progression from obesity to diabetes. Nat Commun. 2014;5:4934. doi: 10.1038/ncomms5934. [DOI] [PubMed] [Google Scholar]
- Lin SH, Maiese K. The metabotropic glutamate receptor system protects against ischemic free radical programmed cell death in rat brain endothelial cells. J Cereb Blood Flow Metab. 2001;21:262–275. doi: 10.1097/00004647-200103000-00010. [DOI] [PubMed] [Google Scholar]
- Liu H, Dong W, Lin Z, Lu J, Wan H, Zhou Z, Liu Z. CCN4 regulates vascular smooth muscle cell migration and proliferation. Mol Cells. 2013a;36:112–118. doi: 10.1007/s10059-013-0012-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J, Li J, Li WJ, Wang CM. (2013b) The role of uncoupling proteins in diabetes mellitus. J Diabetes Res. 2013 doi: 10.1155/2013/585897. 585897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Q, Li J, Cheng R, Chen Y, Lee K, Hu Y, Yi J, Liu Z, Ma JX. Nitrosative stress plays an important role in wnt pathway activation in diabetic retinopathy. Antioxid Redox Signal. 2013c;18:1141–1153. doi: 10.1089/ars.2012.4583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y, Palanivel R, Rai E, Park M, Gabor TV, Scheid MP, Xu A, Sweeney G. Adiponectin stimulates autophagy and reduces oxidative stress to enhance insulin sensitivity during high fat diet feeding in mice. Diabetes. 2014;64:36–48. doi: 10.2337/db14-0267. [DOI] [PubMed] [Google Scholar]
- Liu Y, Yan W, Zhang W, Chen L, You G, Bao Z, Wang Y, Wang H, Kang C, Jiang T. MiR-218 reverses high invasiveness of glioblastoma cells by targeting the oncogenic transcription factor LEF1. Oncol Rep. 2012a;28:1013–1021. doi: 10.3892/or.2012.1902. [DOI] [PubMed] [Google Scholar]
- Liu Y, Shi S, Gu Z, Du Y, Liu M, Yan S, Gao J, Li J, Shao Y, Zhong W, Chen X, Li C. Impaired autophagic function in rat islets with aging. Age (Dordr) 2013d;35:1531–1544. doi: 10.1007/s11357-012-9456-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Z, Stanojevic V, Brindamour LJ, Habener JF. GLP1-derived nonapeptide GLP1(28-36)amide protects pancreatic beta-cells from glucolipotoxicity. J Endocrinol. 2012b;213:143–154. doi: 10.1530/JOE-11-0328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lough D, Dai H, Yang M, Reichensperger J, Cox L, Harrison C, Neumeister MW. Stimulation of the follicular bulge LGR5+ and LGR6+ stem cells with the gut-derived human alpha defensin 5 results in decreased bacterial presence, enhanced wound healing, and hair growth from tissues devoid of adnexal structures. Plast Reconstr Surg. 2013;132:1159–1171. doi: 10.1097/PRS.0b013e3182a48af6. [DOI] [PubMed] [Google Scholar]
- Ma R, Huang C, Hu J, Wang M, Xiang J, Li G. JAK2/STAT5/Bcl-xL signaling is essential for erythropoietin-mediated protection against PC12 cells apoptosis induced by Abeta. Br J Pharmacol. 2014;171:3234–3245. doi: 10.1111/bph.12672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maiese K. Triple play: Promoting neurovascular longevity with nicotinamide, WNT, and erythropoietin in diabetes mellitus. Biomed Pharmacother. 2008;62:218–232. doi: 10.1016/j.biopha.2008.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maiese K. Driving neural regeneration through the mammalian target of rapamycin. Neural Regen Res. 2014a;9:1413–1417. doi: 10.4103/1673-5374.139453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maiese K. Taking aim at Alzheimer's disease through the mammalian target of rapamycin. Ann Med. 2014b;46:587–596. doi: 10.3109/07853890.2014.941921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maiese K. Cutting through the complexities of mTOR for the treatment of stroke. Curr Neurovasc Res. 2014c;11:177–186. doi: 10.2174/1567202611666140408104831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maiese K. WISP1: Clinical insights for a proliferative and restorative member of the CCN family. Curr Neurovasc Res. 2014d;11:378–389. doi: 10.2174/1567202611666140912115107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maiese K, Li F, Chong ZZ. Erythropoietin and cancer. JAMA. 2005a;293:1858–1859. doi: 10.1001/jama.293.1.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maiese K, Li F, Chong ZZ. New avenues of exploration for erythropoietin. Jama. 2005b;293:90–95. doi: 10.1001/jama.293.1.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maiese K, Morhan SD, Chong ZZ. Oxidative stress biology and cell injury during type 1 and type 2 diabetes mellitus. Curr Neurovasc Res. 2007a;4:63–71. doi: 10.2174/156720207779940653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maiese K, Chong ZZ, Shang YC. Mechanistic insights into diabetes mellitus and oxidative stress. Curr Med Chem. 2007b;14:1729–1738. doi: 10.2174/092986707781058968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maiese K, Chong ZZ, Shang YC. Raves and risks for erythropoietin. Cytokine Growth Factor Rev. 2008a;19:145–155. doi: 10.1016/j.cytogfr.2008.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maiese K, Chong ZZ, Shang YC. OutFOXOing disease and disability: the therapeutic potential of targeting FoxO proteins. Trends Mol Med. 2008b;14:219–227. doi: 10.1016/j.molmed.2008.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maiese K, Boniece I, DeMeo D, Wagner JA. Peptide growth factors protect against ischemia in culture by preventing nitric oxide toxicity. J Neurosci. 1993;13:3034–3040. doi: 10.1523/JNEUROSCI.13-07-03034.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maiese K, Chong ZZ, Shang YC, Hou J. Therapeutic promise and principles: Metabotropic glutamate receptors. Oxid Med Cell Longev. 2008c;1:1–14. doi: 10.4161/oxim.1.1.6842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maiese K, Chong ZZ, Li F, Shang YC. Erythropoietin: elucidating new cellular targets that broaden therapeutic strategies. Prog Neurobiol. 2008d;85:194–213. doi: 10.1016/j.pneurobio.2008.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maiese K, Li F, Chong ZZ, Shang YC. The Wnt signaling pathway: Aging gracefully as a protectionist? Pharmacol Ther. 2008e;118:58–81. doi: 10.1016/j.pharmthera.2008.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maiese K, Chong ZZ, Hou J, Shang YC. The vitamin nicotinamide: translating nutrition into clinical care. Molecules. 2009;14:3446–3485. doi: 10.3390/molecules14093446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maiese K, Shang YC, Chong ZZ, Hou J. Diabetes mellitus: channeling care through cellular discovery. Curr Neurovasc Res. 2010a;7:59–64. doi: 10.2174/156720210790820217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maiese K, Chong ZZ, Hou J, Shang YC. Oxidative stress: Biomarkers and novel therapeutic pathways. Exp Gerontol. 2010b;45:217–234. doi: 10.1016/j.exger.2010.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maiese K, Chong ZZ, Shang YC, Hou J. Novel avenues of drug discovery and biomarkers for diabetes mellitus. J Clin Pharmacol. 2011a;51:128–152. doi: 10.1177/0091270010362904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maiese K, Chong ZZ, Shang YC, Wang S. Translating cell survival and cell longevity into treatment strategies with SIRT1. Rom J Morphol Embryol. 2011b;52:1173–1185. [PMC free article] [PubMed] [Google Scholar]
- Maiese K, Chong ZZ, Shang YC, Wang S. Erythropoietin: new directions for the nervous system. Int J Mol Sci. 2012a;13:11102–11129. doi: 10.3390/ijms130911102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maiese K, Chong ZZ, Shang YC, Wang S. Targeting disease through novel pathways of apoptosis and autophagy. Expert Opin Ther Targets. 2012b;16:1203–1214. doi: 10.1517/14728222.2012.719499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maiese K, Chong ZZ, Shang YC, Wang S. mTOR: on target for novel therapeutic strategies in the nervous system. Trends Mol Med. 2013a;19:51–60. doi: 10.1016/j.molmed.2012.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maiese K, Chong ZZ, Wang S, Shang YC. Oxidant stress and signal transduction in the nervous system with the PI 3-K, Akt, and mTOR cascade. Int J Mol Sci. 2013b;13:13830–13866. doi: 10.3390/ijms131113830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maiese K, Chong ZZ, Shang YC, Wang S. Novel directions for diabetes mellitus drug discovery. Expert Opin Drug Discov. 2013c;8:35–48. doi: 10.1517/17460441.2013.736485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mao XY, Cao DF, Li X, Yin JY, Wang ZB, Zhang Y, Mao CX, Zhou HH, Liu ZQ. Huperzine A ameliorates cognitive deficits in streptozotocin-induced diabetic rats. Int J Mol Sci. 2014;15:7667–7683. doi: 10.3390/ijms15057667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marchand A, Atassi F, Gaaya A, Leprince P, Le Feuvre C, Soubrier F, Lompre AM, Nadaud S. The Wnt/beta-catenin pathway is activated during advanced arterial aging in humans. Aging Cell. 2011;10:220–232. doi: 10.1111/j.1474-9726.2010.00661.x. [DOI] [PubMed] [Google Scholar]
- Marchetti B, L’Episcopo F, Morale MC, Tirolo C, Testa N, Caniglia S, Serapide MF, Pluchino S. Uncovering novel actors in astrocyte-neuron crosstalk in Parkinson's disease: the Wnt/beta-catenin signaling cascade as the common final pathway for neuroprotection and self-repair. Eur J Neurosci. 2013;37:1550–1563. doi: 10.1111/ejn.12166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez de Morentin PB, Martinez-Sanchez N, Roa J, Ferno J, Nogueiras R, Tena-Sempere M, Dieguez C, Lopez M. Hypothalamic mTOR: the rookie energy sensor. Curr Mol Med. 2014;14:3–21. doi: 10.2174/1566524013666131118103706. [DOI] [PubMed] [Google Scholar]
- Mercer KE, Hennings L, Sharma N, Lai K, Cleves MA, Wynne RA, Badger TM, Ronis MJ. Alcohol consumption promotes diethylnitrosamine-induced hepatocarcinogenesis in male mice through activation of the Wnt/beta-catenin signaling pathway. Cancer Prev Res (Phila) 2014;7:675–685. doi: 10.1158/1940-6207.CAPR-13-0444-T. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miao XY, Gu ZY, Liu P, Hu Y, Li L, Gong YP, Shu H, Liu Y, Li CL. The human glucagon-like peptide-1 analogue liraglutide regulates pancreatic beta-cell proliferation and apoptosis via an AMPK/mTOR/P70S6K signaling pathway. Peptides. 2013;39:71–79. doi: 10.1016/j.peptides.2012.10.006. [DOI] [PubMed] [Google Scholar]
- Min JJ, Huo XL, Xiang LY, Qin YQ, Chai KQ, Wu B, Jin L, Wang XT. Protective effect of Dl-3n-butylphthalide on learning and memory impairment induced by chronic intermittent hypoxia-hypercapnia exposure. Sci Rep. 2014;4:5555. doi: 10.1038/srep05555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miret JA, Munne-Bosch S. Plant amino acid-derived vitamins: biosynthesis and function. Amino Acids. 2014;46:809–824. doi: 10.1007/s00726-013-1653-3. [DOI] [PubMed] [Google Scholar]
- Moghaddasi M, Javanmard SH, Reisi P, Tajadini M, Taati M. The effect of regular exercise on antioxidant enzyme activities and lipid peroxidation levels in both hippocampi after occluding one carotid in rat. J Physiol Sci. 2014;64:325–332. doi: 10.1007/s12576-014-0322-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monnier L, Mas E, Ginet C, Michel F, Villon L, Cristol JP, Colette C. Activation of oxidative stress by acute glucose fluctuations compared with sustained chronic hyperglycemia in patients with type 2 diabetes. JAMA. 2006;295:1681–1687. doi: 10.1001/jama.295.14.1681. [DOI] [PubMed] [Google Scholar]
- Moroz N, Carmona JJ, Anderson E, Hart AC, Sinclair DA, Blackwell TK. Dietary restriction involves NAD+-dependent mechanisms and a shift toward oxidative metabolism. Aging Cell. 2014;13:1075–1085. doi: 10.1111/acel.12273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muley MM, Thakare VN, Patil RR, Kshirsagar AD, Naik SR. Silymarin improves the behavioural, biochemical and histoarchitecture alterations in focal ischemic rats: a comparative evaluation with piracetam and protocatachuic acid. Pharmacol Biochem Behav. 2012;102:286–293. doi: 10.1016/j.pbb.2012.05.004. [DOI] [PubMed] [Google Scholar]
- Murahovschi V, Pivovarova O, Ilkavets I, Dmitrieva RM, Döcke S, Keyhani-Nejad F, Gögebakan Ö, Osterhoff M, Kemper M, Hornemann S, Markova M, Klöting N, Stockmann M, Weickert MO, Lamounier-Zepter V, Neuhaus P, Konradi A, Dooley S, von Loeffelholz C, Blüher M, Pfeiffer AF, et al. WISP1 is a novel adipokine linked to inflammation in obesity. Diabetes. 2014;64:856–866. doi: 10.2337/db14-0444. [DOI] [PubMed] [Google Scholar]
- Nakka VP, Prakash-Babu P, Vemuganti R. Crosstalk between endoplasmic reticulum stress, oxidative stress, and autophagy: potential therapeutic targets for acute CNS injuries. Mol Neurobiol. 2014 doi: 10.1007/s12035-014-9029-6. doi: 10.1007/s12035-014-9029-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen AQ, Cherry BH, Scott GF, Ryou MG, Mallet RT. Erythropoietin: Powerful protection of ischemic and post-ischemic brain. Exp Biol Med (Maywood) 2014;239:1461–1475. doi: 10.1177/1535370214523703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogunshola OO, Moransard M, Gassmann M. Constitutive excessive erythrocytosis causes inflammation and increased vascular permeability in aged mouse brain. Brain Res. 2013;1531:48–57. doi: 10.1016/j.brainres.2013.07.033. [DOI] [PubMed] [Google Scholar]
- Ono M, Inkson CA, Sonn R, Kilts TM, de Castro LF, Maeda A, Fisher LW, Robey PG, Berendsen AD, Li L, McCartney-Francis N, Brown AC, Crawford NP, Molinolo A, Jain A, Fedarko NS, Young MF. WISP1/CCN4: a potential target for inhibiting prostate cancer growth and spread to bone. PLoS One. 2013;8:e71709. doi: 10.1371/journal.pone.0071709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortiz-Masia D, Cosin-Roger J, Calatayud S, Hernandez C, Alos R, Hinojosa J, Apostolova N, Alvarez A, Barrachina MD. Hypoxic macrophages impair autophagy in epithelial cells through Wnt1: relevance in IBD. Mucosal Immuno. 2014;7:929–938. doi: 10.1038/mi.2013.108. [DOI] [PubMed] [Google Scholar]
- Palazzuoli A, Ruocco G, Pellegrini M, De Gori C, Del Castillo G, Giordano N, Nuti R. The role of erythropoietin stimulating agents in anemic patients with heart failure: solved and unresolved questions. Ther Clin Risk Manag. 2014;10:641–650. doi: 10.2147/TCRM.S61551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palma HE, Wolkmer P, Gallio M, Correa MM, Schmatz R, Thome GR, Pereira LB, Castro VS, Pereira AB, Bueno A, de Oliveira LS, Rosolen D, Mann TR, de Cecco BS, Graca DL, Lopes ST, Mazzanti CM. Oxidative stress parameters in blood, liver, and kidney of diabetic rats treated with curcumin and/or insulin. Mol Cell Biochem. 2014;386:199–210. doi: 10.1007/s11010-013-1858-5. [DOI] [PubMed] [Google Scholar]
- Parvin A, Pranap R, Shalini U, Devendran A, Baker JE, Dhanasekaran A. Erythropoietin protects cardiomyocytes from cell death during hypoxia/reperfusion injury through activation of survival signaling pathways. PLoS One. 2014;9:e107453. doi: 10.1371/journal.pone.0107453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasmant E, Ortonne N, Rittie L, Laurendeau I, Levy P, Lazar V, Parfait B, Leroy K, Dessen P, Valeyrie-Allanore L, Perbal B, Wolkenstein P, Vidaud M, Vidaud D, Bieche I. Differential expression of CCN1/CYR61, CCN3/NOV, CCN4/WISP1, and CCN5/WISP2 in neurofibromatosis type 1 tumorigenesis. J Neuropathol Exp Neurol. 2010;69:60–69. doi: 10.1097/NEN.0b013e3181c79bff. [DOI] [PubMed] [Google Scholar]
- Peng N, Meng N, Wang S, Zhao F, Zhao J, Su L, Zhang S, Zhang Y, Zhao B, Miao J. An activator of mTOR inhibits oxLDL-induced autophagy and apoptosis in vascular endothelial cells and restricts atherosclerosis in apolipoprotein E(-/-) mice. Sci Rep. 2014;4:5519. doi: 10.1038/srep05519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng S, Zhao S, Yan F, Cheng J, Huang L, Chen H, Liu Q, Ji X, Yuan Z. HDAC2 selectively regulates FOXO3a-mediated gene transcription during oxidative stress-induced neuronal cell death. J Neurosci. 2015;35:1250–1259. doi: 10.1523/JNEUROSCI.2444-14.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng Y, Huang S, Cheng B, Nie X, Enhe J, Feng C, Fu X. Mesenchymal stem cells: a revolution in therapeutic strategies of age-related diseases. Ageing Res Rev. 2013;12:103–115. doi: 10.1016/j.arr.2012.04.005. [DOI] [PubMed] [Google Scholar]
- Pilar-Cuellar F, Vidal R, Diaz A, Castro E, dos Anjos S, Pascual-Brazo J, Linge R, Vargas V, Blanco H, Martinez-Villayandre B, Pazos A, Valdizan EM. (2013) Neural plasticity and proliferation in the generation of antidepressant effects: hippocampal implication. Neural Plast. 2013 doi: 10.1155/2013/537265. 537265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price RM, Tulsyan N, Dermody JJ, Schwalb M, Soteropoulos P, Castronuovo JJ., Jr Gene expression after crush injury of human saphenous vein: using microarrays to define the transcriptional profile. J Am Coll Surg. 2004;199:411–418. doi: 10.1016/j.jamcollsurg.2004.04.023. [DOI] [PubMed] [Google Scholar]
- Rachek LI, Thornley NP, Grishko VI, LeDoux SP, Wilson GL. Protection of INS-1 cells from free fatty acid-induced apoptosis by targeting hOGG1 to mitochondria. Diabetes. 2006;55:1022–1028. doi: 10.2337/diabetes.55.04.06.db05-0865. [DOI] [PubMed] [Google Scholar]
- Reagan LP. Diabetes as a chronic metabolic stressor: causes, consequences and clinical complications. Exp Neurol. 2012;233:68–78. doi: 10.1016/j.expneurol.2011.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reddy VS, Valente AJ, Delafontaine P, Chandrasekar B. Interleukin-18/WNT1-inducible signaling pathway protein-1 signaling mediates human saphenous vein smooth muscle cell proliferation. J Cell Physiol. 2011;226:3303–3315. doi: 10.1002/jcp.22676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ribeiro MC, Barbosa NB, de Almeida TM, Parcianello LM, Perottoni J, de Avila DS, Rocha JB. High-fat diet and hydrochlorothiazide increase oxidative stress in brain of rats. Cell Biochem Funct. 2009;27:473–478. doi: 10.1002/cbf.1599. [DOI] [PubMed] [Google Scholar]
- Rutter MK, Massaro JM, Hoffmann U, O’Donnell CJ, Fox CS. Fasting glucose, obesity, and coronary artery calcification in community-based people without diabetes. Diabetes Care. 2012;35:1944–1950. doi: 10.2337/dc11-1950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safarian F, Khallaghi B, Ahmadiani A, Dargahi L. Activation of S1P receptor regulates PI3K/Akt/FoxO3a pathway in response to oxidative stress in PC12 Cells. J Mol Neurosci. 2014 doi: 10.1007/s12031-014-0478-1. doi: 10.1007/s12031-014-0478-1. [DOI] [PubMed] [Google Scholar]
- Schafer R, Mueller L, Buecheler R, Proksch B, Schwab M, Gleiter CH, Danielyan L. Interplay between endothelin and erythropoietin in astroglia: the role in protection against hypoxia. Int J Mol Sci. 2014;15:2858–2875. doi: 10.3390/ijms15022858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaffer SW, Jong CJ, Mozaffari M. Role of oxidative stress in diabetes-mediated vascular dysfunction: unifying hypothesis of diabetes revisited. Vascul Pharmacol. 2012;57:139–149. doi: 10.1016/j.vph.2012.03.005. [DOI] [PubMed] [Google Scholar]
- Schmeichel AM, Schmelzer JD, Low PA. Oxidative injury and apoptosis of dorsal root ganglion neurons in chronic experimental diabetic neuropathy. Diabetes. 2003;52:165–171. doi: 10.2337/diabetes.52.1.165. [DOI] [PubMed] [Google Scholar]
- Schutters K, Reutelingsperger C. Phosphatidylserine targeting for diagnosis and treatment of human diseases. Apoptosis. 2010;15:1072–1082. doi: 10.1007/s10495-010-0503-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shang YC, Chong ZZ, Hou J, Maiese K. Wnt1, FoxO3a, and NF-kappaB oversee microglial integrity and activation during oxidant stress. Cell Signal. 2010;22:1317–1329. doi: 10.1016/j.cellsig.2010.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shang YC, Chong ZZ, Wang S, Maiese K. Erythropoietin and Wnt1 govern pathways of mTOR, Apaf-1, and XIAP in inflammatory microglia. Curr Neurovasc Res. 2011;8:270–285. doi: 10.2174/156720211798120990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shang YC, Chong ZZ, Wang S, Maiese K. WNT1 Inducible signaling pathway protein 1 (WISP1) Targets PRAS40 to govern beta-amyloid apoptotic injury of microglia. Curr Neurovasc Res. 2012a;9:239–249. doi: 10.2174/156720212803530618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shang YC, Chong ZZ, Wang S, Maiese K. Prevention of beta-amyloid degeneration of microglia by erythropoietin depends on Wnt1, the PI 3-K/mTOR pathway, Bad, and Bcl-xL. Aging (Albany NY) 2012b;4:187–201. doi: 10.18632/aging.100440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shang YC, Chong ZZ, Wang S, Maiese K. Tuberous sclerosis protein 2 (TSC2) modulates CCN4 cytoprotection during apoptotic amyloid toxicity in microglia. Curr Neurovasc Res. 2013;10:29–38. doi: 10.2174/156720213804806007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shao H, Cai L, Grichnik JM, Livingstone AS, Velazquez OC, Liu ZJ. Activation of Notch1 signaling in stromal fibroblasts inhibits melanoma growth by upregulating WISP-1. Oncogene. 2011;30:4316–4326. doi: 10.1038/onc.2011.142. [DOI] [PubMed] [Google Scholar]
- Shao S, Yang Y, Yuan G, Zhang M, Yu X. Signaling molecules involved in lipid-induced pancreatic Beta-cell dysfunction. Dna Cell Biol. 2013;32:41–49. doi: 10.1089/dna.2012.1874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen W, Chung SH, Irhimeh MR, Li S, Lee SR, Gillies MC. Systemic administration of erythropoietin inhibits retinopathy in RCS Rats. PLoS One. 2014;9:e104759. doi: 10.1371/journal.pone.0104759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonnen JA, Larson EB, Brickell K, Crane PK, Woltjer R, Montine TJ, Craft S. Different patterns of cerebral injury in dementia with or without diabetes. Arch Neurol. 2009;66:315–322. doi: 10.1001/archneurol.2008.579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soon LL, Yie TA, Shvarts A, Levine AJ, Su F, Tchou-Wong KM. Overexpression of WISP-1 down-regulated motility and invasion of lung cancer cells through inhibition of Rac activation. J Biol Chem. 2003;278:11465–11470. doi: 10.1074/jbc.M210945200. [DOI] [PubMed] [Google Scholar]
- Srivastava A, Shivanandappa T. Prevention of hexachlorocyclohexane-induced neuronal oxidative stress by natural antioxidants. Nutr Neurosci. 2014;17:164–171. doi: 10.1179/1476830513Y.0000000075. [DOI] [PubMed] [Google Scholar]
- Su F, Overholtzer M, Besser D, Levine AJ. WISP-1 attenuates p53-mediated apoptosis in response to DNA damage through activation of the Akt kinase. Genes Dev. 2002;16:46–57. doi: 10.1101/gad.942902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun TJ, Tao R, Han YQ, Xu G, Liu J, Han YF. Therapeutic potential of umbilical cord mesenchymal stem cells with Wnt/beta-catenin signaling pathway pre-activated for the treatment of diabetic wounds. Eur Rev Med Pharmacol Sci. 2014;18:2460–2464. [PubMed] [Google Scholar]
- Tanaka S, Sugimachi K, Kameyama T, Maehara S, Shirabe K, Shimada M, Wands JR, Maehara Y. Human WISP1v, a member of the CCN family, is associated with invasive cholangiocarcinoma. Hepatology. 2003;37:1122–1129. doi: 10.1053/jhep.2003.50187. [DOI] [PubMed] [Google Scholar]
- Tang L, Zhang Y, Jiang Y, Willard L, Ortiz E, Wark L, Medeiros D, Lin D. Dietary wolfberry ameliorates retinal structure abnormalities in db/db mice at the early stage of diabetes. Exp Biol Med (Maywood) 2011;236:1051–1063. doi: 10.1258/ebm.2011.010400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanno M, Kuno A, Yano T, Miura T, Hisahara S, Ishikawa S, Shimamoto K, Horio Y. Induction of manganese superoxide dismutase by nuclear translocation and activation of SIRT1 promotes cell survival in chronic heart failure. J Biol Chem. 2010;285:8375–8382. doi: 10.1074/jbc.M109.090266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorfve A, Lindahl C, Xia W, Igawa K, Lindahl A, Thomsen P, Palmquist A, Tengvall P. Hydroxyapatite coating affects the Wnt signaling pathway during peri-implant healing in vivo. Acta Biomater. 2014;10:1451–1462. doi: 10.1016/j.actbio.2013.12.012. [DOI] [PubMed] [Google Scholar]
- Tu Y, Gao X, Li G, Fu H, Cui D, Liu H, Jin W, Zhang Y. MicroRNA-218 inhibits glioma invasion, migration, proliferation, and cancer stem-like cell self-renewal by targeting the polycomb group gene Bmi1. Cancer Res. 2013;73:6046–6055. doi: 10.1158/0008-5472.CAN-13-0358. [DOI] [PubMed] [Google Scholar]
- Uranga RM, Katz S, Salvador GA. Enhanced phosphatidylinositol 3-kinase (PI3K)/Akt signaling has pleiotropic targets in hippocampal neurons exposed to iron-induced oxidative stress. J Biol Chem. 2013;288:19773–19784. doi: 10.1074/jbc.M113.457622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uzdensky AB, Demyanenko SV, Bibov MY. Signal transduction in human cutaneous melanoma and target drugs. Curr Cancer Drug Targets. 2013;13:843–866. doi: 10.2174/1568009611313080004. [DOI] [PubMed] [Google Scholar]
- Venkatesan B, Prabhu SD, Venkatachalam K, Mummidi S, Valente AJ, Clark RA, Delafontaine P, Chandrasekar B. WNT1-inducible signaling pathway protein-1 activates diverse cell survival pathways and blocks doxorubicin-induced cardiomyocyte death. Cell Signal. 2010;22:809–820. doi: 10.1016/j.cellsig.2010.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vishwas DK, Mukherjee A, Haldar C, Dash D, Nayak MK. Improvement of oxidative stress and immunity by melatonin: An age dependent study in golden hamster. Exp Gerontol. 2013;48:168–182. doi: 10.1016/j.exger.2012.11.012. [DOI] [PubMed] [Google Scholar]
- Wang L, Di L, Noguchi CT. Erythropoietin, a novel versatile player regulating energy metabolism beyond the erythroid system. Int J Biol Sci. 2014;10:921–939. doi: 10.7150/ijbs.9518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang S, Chong ZZ, Shang YC, Maiese K. Wnt1 inducible signaling pathway protein 1 (WISP1) blocks neurodegeneration through phosphoinositide 3 kinase/Akt1 and apoptotic mitochondrial signaling involving Bad, Bax, Bim, and Bcl-xL. Curr Neurovasc Res. 2012a;9:20–31. doi: 10.2174/156720212799297137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang S, Chong ZZ, Shang YC, Maiese K. WISP1 (CCN4) autoregulates its expression and nuclear trafficking of beta-catenin during oxidant stress with limited effects upon neuronal autophagy. Curr Neurovasc Res. 2012b;9:89–99. doi: 10.2174/156720212800410858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang S, Chong ZZ, Shang YC, Maiese K. WISP1 neuroprotection requires FoxO3a post-translational modulation with autoregulatory control of SIRT1. Curr Neurovasc Res. 2013;10:54–60. doi: 10.2174/156720213804805945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang S, Sun Z, Zhang X, Li Z, Wu M, Zhao W, Wang H, Chen T, Yan H, Zhu J. Wnt1 positively regulates CD36 expression via TCF4 and PPAR-gamma in macrophages. Cell Physiol Biochem. 2015;35:1289–1302. doi: 10.1159/000373951. [DOI] [PubMed] [Google Scholar]
- Wei L, Sun C, Lei M, Li G, Yi L, Luo F, Li Y, Ding L, Liu Z, Li S, Xu P. Activation of Wnt/beta-catenin pathway by exogenous Wnt1 protects SH-SY5Y cells against 6-hydroxydopamine toxicity. J Mol Neurosci. 2013;49:105–115. doi: 10.1007/s12031-012-9900-8. [DOI] [PubMed] [Google Scholar]
- Weinberg E, Maymon T, Weinreb M. AGEs induce caspase-mediated apoptosis of rat BMSCs via TNFalpha production and oxidative stress. J Mol Endocrinol. 2014;52:67–76. doi: 10.1530/JME-13-0229. [DOI] [PubMed] [Google Scholar]
- Wexler EM, Rosen E, Lu D, Osborn GE, Martin E, Raybould H, Geschwind DH. Genome-wide analysis of a Wnt1-regulated transcriptional network implicates neurodegenerative pathways. Sci Signal. 2011;4:ra65. doi: 10.1126/scisignal.2002282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White MF. IRS2 integrates insulin/IGF1 signalling with metabolism, neurodegeneration and longevity. Diabetes Obes Metab 16 Suppl. 2014;1:4–15. doi: 10.1111/dom.12347. [DOI] [PubMed] [Google Scholar]
- Williams CJ, Dexter DT. Neuroprotective and symptomatic effects of targeting group III mGlu receptors in neurodegenerative disease. J Neurochem. 2014;129:4–20. doi: 10.1111/jnc.12608. [DOI] [PubMed] [Google Scholar]
- Geneva: World Health Organization (2011) Global status report on noncommunicable diseases 2010. [Google Scholar]
- Wright JW, Harding JW. The brain hepatocyte growth factor/c-Met receptor system: a new target for the treatment of alzheimer's disease. J Alzheimers Dis. 2015 doi: 10.3233/JAD-142814. doi: 10.3233/JAD-142814. [DOI] [PubMed] [Google Scholar]
- Xin YJ, Yuan B, Yu B, Wang YQ, Wu JJ, Zhou WH, Qiu Z. Tet1-mediated DNA demethylation regulates neuronal cell death induced by oxidative stress. Sci Rep. 2015;5:7645. doi: 10.1038/srep07645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xing XS, Liu F, He ZY. Akt regulates beta-catenin in a rat model of focal cerebral ischemia-reperfusion injury. Mol Med Rep. 2014;11:3122–3128. doi: 10.3892/mmr.2014.3000. [DOI] [PubMed] [Google Scholar]
- Xing Y, Zhang X, Zhao K, Cui L, Wang L, Dong L, Li Y, Liu Z, Wang C, Zhang X, Zhu C, Qiao H, Ji Y, Cao X. Beneficial effects of sulindac in focal cerebral ischemia: a positive role in Wnt/beta-catenin pathway. Brain Res. 2012;1482:71–80. doi: 10.1016/j.brainres.2012.08.057. [DOI] [PubMed] [Google Scholar]
- Xu E, Schwab M, Marette A. Role of protein tyrosine phosphatases in the modulation of insulin signaling and their implication in the pathogenesis of obesity-linked insulin resistance. Rev Endocr Metab Disord. 2014a;15:79–97. doi: 10.1007/s11154-013-9282-4. [DOI] [PubMed] [Google Scholar]
- Xu YJ, Tappia PS, Neki NS, Dhalla NS. Prevention of diabetes-induced cardiovascular complications upon treatment with antioxidants. Heart Fail Rev. 2014b;19:113–121. doi: 10.1007/s10741-013-9379-6. [DOI] [PubMed] [Google Scholar]
- Yamada E, Singh R. Mapping autophagy on to your metabolic radar. Diabetes. 2012;61:272–280. doi: 10.2337/db11-1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang CS, Lopez CG, Rana TM. Discovery of nonsteroidal anti-inflammatory drug and anticancer drug enhancing reprogramming and induced pluripotent stem cell generation. Stem Cells. 2011a;29:1528–1536. doi: 10.1002/stem.717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang H, Jin X, Kei Lam CW, Yan SK. Oxidative stress and diabetes mellitus. Clin Chem Lab Med. 2011b;49:1773–1782. doi: 10.1515/CCLM.2011.250. [DOI] [PubMed] [Google Scholar]
- Yano M, Hasegawa G, Ishii M, Yamasaki M, Fukui M, Nakamura N, Yoshikawa T. Short-term exposure of high glucose concentration induces generation of reactive oxygen species in endothelial cells: implication for the oxidative stress associated with postprandial hyperglycemia. Redox Rep. 2004;9:111–116. doi: 10.1179/135100004225004779. [DOI] [PubMed] [Google Scholar]
- Yousef JM, Mohamed AM. Prophylactic role of B vitamins against bulk and zinc oxide nano-particles toxicity induced oxidative DNA damage and apoptosis in rat livers. Pak J Pharm Sci. 2015;28:175–184. [PubMed] [Google Scholar]
- Yu T, Li L, Bi Y, Liu Z, Liu H, Li Z. Erythropoietin attenuates oxidative stress and apoptosis in Schwann cells isolated from streptozotocin-induced diabetic rats. J Pharm Pharmacol. 2014;66:1150–1160. doi: 10.1111/jphp.12244. [DOI] [PubMed] [Google Scholar]
- Yu T, Li L, Chen T, Liu Z, Liu H, Li Z. Erythropoietin attenuates advanced glycation endproducts-induced toxicity of schwann cells in vitro. Neurochem Res. 2015 doi: 10.1007/s11064-015-1516-2. doi:10.1007/s11064-015-1516-2. [DOI] [PubMed] [Google Scholar]
- Zeldich E, Chen CD, Colvin TA, Bove-Fenderson EA, Liang J, Tucker Zhou TB, Harris DA, Abraham CR. The neuroprotective effect of Klotho is mediated via regulation of members of the redox system. J Biol Chem. 2014;289:24700–24715. doi: 10.1074/jbc.M114.567321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeljko M, Pecina-Slaus N, Martic TN, Kusec V, Beros V, Tomas D. Molecular alterations of E-cadherin and beta-catenin in brain metastases. Front Biosci (Elite Ed) 2011;3:616–624. doi: 10.2741/e274. [DOI] [PubMed] [Google Scholar]
- Zhang C, Li Z, Cao Q, Qin C, Cai H, Zhou H, Qian J, Tao L, Ju X, Yin C. Association of erythropoietin gene rs576236 polymorphism and risk of adrenal tumors in a Chinese population. J Biomed Res. 2014a;28:456–461. doi: 10.7555/JBR.28.20130126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang C, Zhang L, Chen S, Feng B, Lu X, Bai Y, Liang G, Tan Y, Shao M, Skibba M, Jin L, Li X, Chakrabarti S, Cai L. The prevention of diabetic cardiomyopathy by non-mitogenic acidic fibroblast growth factor is probably mediated by the suppression of oxidative stress and damage. PLoS One. 2013;8:e82287. doi: 10.1371/journal.pone.0082287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X, Dong S, Qin Y, Bian X. Protective effect of erythropoietin against myocardial injury in rats with sepsis and its underlying mechanisms. Mol Med Rep. 2015;11:3317–3329. doi: 10.3892/mmr.2015.3155. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Zhang Y, Meng N, Lv Z, Li H, Qu Y. The gene polymorphisms of UCP1 but not PPAR gamma and TCF7L2 are associated with diabetic retinopathy in Chinese type 2 diabetes mellitus cases. Acta Ophthalmol. 2014b doi: 10.1111/aos.12542. doi: 10.1111/aos.12542. [DOI] [PubMed] [Google Scholar]
- Zhang Y, Wang L, Dey S, Alnaeeli M, Suresh S, Rogers H, Teng R, Noguchi CT. Erythropoietin action in stress response, tissue maintenance and metabolism. Int J Mol Sci. 2014c;15:10296–10333. doi: 10.3390/ijms150610296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Z, Huang G, Wang B, Zhong Y. Inhibition of NF-kappaB activation by Pyrrolidine dithiocarbamate partially attenuates hippocampal MMP-9 activation and improves cognitive deficits in streptozotocin-induced diabetic rats. Behav Brain Res. 2013;238:44–47. doi: 10.1016/j.bbr.2012.10.018. [DOI] [PubMed] [Google Scholar]
- Zhou J, Wu J, Zheng F, Jin M, Li H. Glucagon-like peptide-1 analog-mediated protection against cholesterol-induced apoptosis via mammalian target of rapamycin activation in pancreatic betaTC-6 cells. J Diabetes. 2014a doi: 10.1111/1753-0407.12177. doi: 10.1111/1753-0407.12177. [DOI] [PubMed] [Google Scholar]
- Zhou Q, Liu C, Liu W, Zhang H, Zhang R, Liu J, Zhang J, Xu C, Liu L, Huang S, Chen L. Rotenone induction of hydrogen peroxide inhibits mTOR-mediated S6K and 4E-BP1/eIF4E pathways, leading to neuronal apoptosis. Toxicol Sci. 2014b;143:81–96. doi: 10.1093/toxsci/kfu211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou SS, Li D, Sun WP, Guo M, Lun YZ, Zhou YM, Xiao FC, Jing LX, Sun SX, Zhang LB, Luo N, Bian FN, Zou W, Dong LB, Zhao ZG, Li SF, Gong XJ, Yu ZG, Sun CB, Zheng CL, et al. Nicotinamide overload may play a role in the development of type 2 diabetes. World J Gastroenterol. 2009;15:5674–5684. doi: 10.3748/wjg.15.5674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou T, Zhou KK, Lee K, Gao G, Lyons TJ, Kowluru R, Ma JX. The role of lipid peroxidation products and oxidative stress in activation of the canonical wingless-type MMTV integration site (WNT) pathway in a rat model of diabetic retinopathy. Diabetologia. 2011;54:459–468. doi: 10.1007/s00125-010-1943-1. [DOI] [PMC free article] [PubMed] [Google Scholar]


