Abstract
The inclusion of nutrition economics in dietary guidance would help ensure that the Dietary Guidelines for Americans benefit equally all segments of the US population. The present review outlines some novel metrics of food affordability that assess nutrient density of foods and beverages in relation to cost. Socioeconomic disparities in diet quality in the United States are readily apparent. In general, groups of lower socioeconomic status consume cheaper, lower-quality diets and suffer from higher rates of noncommunicable diseases. Nutrient profiling models, initially developed to assess the nutrient density of foods, can be turned into econometric models that assess both calories and nutrients per reference amount and per unit cost. These novel metrics have been used to identify individual foods that were affordable, palatable, culturally acceptable, and nutrient rich. Not all nutrient-rich foods were expensive. In dietary surveys, both local and national, some high-quality diets were associated with relatively low cost. Those population subgroups that successfully adopted dietary guidelines at an unexpectedly low monetary cost were identified as “positive deviants.” Constructing a healthy diet based on dietary guidelines can be done, provided that nutrient density of foods, their affordability, as well as taste and social norms are all taken into account.
Keywords: dietary guidelines, nutrient profiling, nutrient density, food prices, affordability, positive deviance
Introduction
The Dietary Guidelines for Americans (DGAs)3 encourage consumption of a healthful diet, one that contains more nutrients than calories (1). Because of inadequate intake of nutrients of concern, prominently featured advice is to consume more vegetables and fruit, low-fat dairy products, whole grains, and lean meats and fish. By contrast, refined grains, sodium, and empty calories from solid fats, added sugars, and alcohol are to be consumed only in moderation (1). The DGAs are the basis of federal nutrition policies and the starting point for many nutrition education programs (1). Their goal is to guide consumer food choices in order to help reduce the risk of obesity and noncommunicable diseases (NCDs) and to promote better health for all.
The aim of federal food and nutrition policies should be to promote better adherence to the guidelines across all socioeconomic groups. However, it is well established that diet quality in the United States follows a socioeconomic gradient (2). The observed impact of socioeconomic status (SES) variables on diet quality appears to be mediated, moreover, by food prices and by diet costs (3, 4). That income inequalities may pose a barrier to the adoption of healthier diets by lower-SES groups (5) remains a challenge needing to be addressed.
There is ample evidence that the DGAs are not followed evenly across all socioeconomic strata (2, 6, 7). Recent analyses of US diet quality in relation to diet cost have shown that empty calories cost less, whereas more nutrient-rich foods and higher-quality diets generally cost more (2). Higher values of the Healthy Eating Index 2005, a federal measure of compliance with the DGAs, were associated with higher per-calorie diet costs, the latter assessed by using a national food prices database (2). In general, more costly and higher-quality diets were bought and eaten by groups of higher SES (8, 9). Conversely, cheaper and lower-quality diets were bought and eaten by lower-SES groups (7). It is well established (7) that lower-SES groups suffer from higher rates of NCDs and are more likely to be overweight and obese.
Whether lower-income Americans can afford to buy healthier foods on a regular basis remains a controversial issue (10, 11). Several studies have recognized that the recommended healthier foods tend to cost more per calorie than do refined grains, added sugars, and fats (7, 12). A recent systematic review and meta-analysis of 27 studies from 10 countries confirmed that healthier foods and higher-quality diet patterns did cost more than did the less-healthy options (13). The price differential was estimated at ∼$500 per person per year or $2000 for a family of 4 (13). By contrast, studies by the Economic Research Service (ERS) of the USDA have repeatedly claimed that the low cost of energy-dense fats and sweets was merely a mathematical artifact and that there was no evidence for a price disparity between empty calories and the recommended healthier options (14). In particular, the ERS found no evidence that cheaper energy-dense foods were preferentially selected by lower-income groups largely because of their low cost (14). In that view, many lower-SES Americans simply chose to eat badly (11, 15, 16).
Constructing a healthy diet based on the DGAs is subject to a number of constraints. Identifying those nutrient-rich foods and food groups that reduce NCD risk is the first task. The formal charge to the Dietary Guidelines Advisory Committee (DGAC) is to review and summarize the published research on diets and health and to determine the ideal dietary intake for all persons, regardless of their SES. The DGAC reports, issued every 5 y, represent the best evidence-based advice that is grounded in a massive review of the global literature on diets and health (1). Taking affordability into account, the 2010 DGAC report stressed that low-income Americans would need greater financial incentives to purchase, prepare, and consume more nutrient-rich foods (17).
Identifying foods that are affordable, accessible, and nutrient-rich would greatly help to implement the DGAs across all socioeconomic strata. However, the congressional mandate to the DGAC is to focus only on the nutrient and food recommendations that are based on sound nutrition science. The 2010 DGAs, issued 1 y after the DGAC report, have steered clear of any mention of food cost. Yet, food cost, along with taste and convenience, is one of the key drivers of purchases and food choice (18, 19). Furthermore, even though food patterns were made more prominent than previously, much of dietary advice was still focused on promoting or avoiding specific foods, individual nutrients, or single dietary ingredients (1).
Reducing complex dietary patterns to single nutrients is not without controversy; recent research has pointed to the importance of food patterns and the total diet (20). Indeed, studies in nutritional epidemiology, the main evidence base for the DGAs, find it difficult to disentangle dietary patterns from social class variables and from economic constraints (8). Because individuals and their food habits are closely intertwined, it can be difficult to isolate the impact of a single nutrient or food ingredient on body weight or health.
Linking dietary sugars and fats with the obesity epidemic is one example. Multiple studies found temporal or statistical links between the consumption of energy-dense foods and obesity risk (21–23). Because such data relied on ecologic comparisons, time trends, and cross-sectional surveys, tracking health outcomes to a single nutrient was a persistent problem. Perhaps as a result, the blame for the obesity epidemic has regularly shifted from sugar to fat and then back again. Throughout the 1990s, the avoidance of fat was the mainstream dietary advice in obesity prevention and control. The avoidance of sugar was further down the list. Sugar trailed fat narrowly in the 2005 DGAs but moved ahead of fat in the 2010 DGAs, becoming the principal nutrient of public health concern. As the popular press put it: fat was once the devil (24), but it was sugar that was finally exposed as the deadly villain in the obesity epidemic (25).
Current Status of Knowledge
The observed SES gradient in diet quality can be explained in part by the low cost of empty calories (13, 26, 27). First, energy-dense foods, including many sweets and fats, are inexpensive, good-tasting, and convenient (2). Second, many such foods provide ample calories but can have minimal nutritional value (28). Third, low-cost, energy-dense diets tend to be consumed by lower-SES groups that also suffer from higher rates of obesity and NCDs (29). In other words, low per-calorie diet cost, often associated with low diet quality, may be the key economic risk factor for subsequent ill health (2, 26, 27, 30). Yet, relatively few studies have examined the financial cost of following the DGAs (25–28) or have explored the links between diet quality, household economic resources, and later health outcomes (3, 4, 9).
Constructing a healthy diet based on the DGAs poses an economic as well as a behavioral challenge. Here, novel nutrient profiling models can help consumers identify those foods that are affordable, accessible, and nutrient rich (31, 32).
Initially, nutrient profiling models were developed to assess the overall nutrient content of foods relative to calories. In the United States, nutrient profiling systems were developed primarily for use in supermarkets, to steer consumers toward healthier products. However, many such systems are proprietary, confidential, and not in the public domain. Their impact on improving diet quality remains to be seen (33, 34). In the European Union, nutrient profiling was initially developed to qualify (or disqualify) foods from making a health or a nutrition claim. Here, the impact of nutrient profiling was moot, because most submitted claims were rejected by the European Food Safety Authority. The food industry has been using multiple nutrient profiling systems to review and improve the quality of their product portfolio. Some of these profiling systems have been published (35, 36), but some have not.
The family of Nutrient Rich Foods (NRF) indexes is unique in many respects. First, all of the algorithms have been published in peer-reviewed journals (31, 32). Second, the Nutrient Rich profiling model is one of the few to have been compared with energy density of foods and with per-calorie food cost (37). Only one other publicly available score, the French individual nutrient adequacy score (SAIN), nutrients to limit (LIM), has gone through the same rigorous rounds of testing and validation (38). Third, the Nutrient Rich principles were used to develop new value metrics for foods, based on nutrients per calorie and nutrients per unit cost (6, 20, 39–41). Such value metrics showed, for example, that potatoes and beans supplied the most nutrients per penny.
How food choices are made.
Food choices are made on the basis of taste, cost, convenience, health, and variety (32). Taste refers to the sensory appeal of foods, with the principal components of palatability, aroma, and texture. Taste and energy density, the latter expressed as dietary energy per unit weight (kcal/100 g), are closely linked. The most palatable foods tend to be energy dense and vice versa. Grains, sweets, and fats are more energy dense than is fresh produce and tend to be liked better, especially by young children. Cost refers to food prices per unit weight, whereas energy cost refers to food cost per unit of energy ($/1000 kcal). Convenience refers to the time spent on buying, preparing, and cooking food. Health refers to concerns with body weight and nutritional status, whereas variety refers to the innate drive to secure a diverse diet composed of multiple food groups. Energy-adjusted diet costs refer to cost per 1000 kcal.
Constructing a healthy diet based on dietary recommendations and guidelines also needs to take the existing food preferences and eating habits into account. Long-term adherence to dietary guidelines requires the adoption of food patterns that are nutritionally adequate, affordable, available, and culturally appropriate (42). In particular, the guidelines need to feature those foods and food groups that are already a part of the eating repertoire (42). One approach, adopted in France, is that never-before-eaten foods have no part in dietary guidance (42).
For that reason, data on population-specific social norms are critical to constructing healthier food patterns (42). Although energy requirements and most nutrient needs can be met cheaply, the resulting food patterns may lack variety or cultural or sensory appeal. Researchers have puzzled over the fact that some low-cost yet highly nutritious foods are rejected by the low-income consumer (42). One hypothesis is that such foods may deviate from the accepted social norms and are socially or culturally inappropriate. Rather than consume nutrient-rich powdered milk, canned fish, lentils, and seeds, many US families would prefer to consume meat, milk, potatoes, carrots, and cabbage, which offer high nutrient density at a relatively low cost and are more culturally and socially acceptable (43).
Metrics of nutrients per calorie and nutrients per unit cost.
The concept of nutrient density is the cornerstone of dietary guidelines, including the DGAs, MyPyramid, and MyPlate (1, 2). Americans are advised to get the most nutrition out of their calories and to make smart, nutrient-dense choices from every food group. The main challenge to implementing dietary guidelines is how to maximize nutrient density of the diet without exceeding daily energy requirements.
The family of NRF indexes (32, 33) was developed to provide a single score reflecting each food’s overall nutritional value. Nutrient density was defined in terms of nutrients per calorie or per serving. The NRF9.3 variant of the NRF family of scores was based on the sum of the percentage of daily values (%DVs) for 9 nutrients to encourage minus the sum of the percentage of maximum recommended values for 3 nutrients to limit, with all DVs calculated per 100 kcal and capped at 100% (32). In this terminology, nutrients to encourage were (for the most part) shortfall nutrients of public health concern. By contrast, nutrients to limit were those to be consumed only in moderation.
Nutrients to encourage in the NRF 9.3 model were protein, fiber, calcium, iron, potassium, magnesium, and vitamins A, C, and E (32). Their selection was based on the US FDA definition of “healthy foods” and on shortfall nutrients in the United States, as identified by the DGAs. Nutrients to limit in the NRF9.3 model were saturated fat, added sugar, and sodium. Foods are disqualified from nutrition and health claims in the United States if they contain above-specified amounts of fat, saturated fat, trans fat, cholesterol, and sodium. In the French SAIN, LIM nutrient profiling system, saturated fat and added sugar and sodium were the nutrients to limit (38, 44). Alternative versions of the NRF algorithm were based on a variable number of nutrients to encourage (from 5 to 23) and the same 3 nutrients to limit (45).
Nutrient-profiling models can be useful insofar as they help consumers identify better foods and create healthier diets. Ideally, the highest-scoring foods ought to be nutrient dense, as well as affordable and appealing. Merging the Food and Nutrient Database for Dietary Studies (FNDDS) nutrient composition database with the USDA Center for Nutrition Policy and Promotion national food prices data has allowed us to study the nutrient density of US foods in relation to their cost (2, 28).
In published work (28), such analyses were based on 1387 foods from the USDA FNDDS 1.0. That database includes foods from the 9 major food groups: 1) milk and milk products; 2) meat, poultry, and fish; 3) eggs; 4) dry beans, legumes, nuts, and seeds; 5) grain products; 6) fruit; 7) vegetables; 8) fats, oils, and salad dressings; and 9) sugars, sweets, and beverages. The FNDDS nutrient composition data were merged with the Center for Nutrition Policy and Promotion national food prices and with the added-sugars data obtained from the USDA Pyramid Servings Database. Portion sizes were obtained from the FDA (46). For calculations of nutrients per unit cost, positive NRF scores were divided by food prices per reference amount (per serving or 100 kcal). The Affordable Nutrition Index was then calculated in terms of the relative amount of nutrients per dollar.
The research goal was to identify those food sources of specific nutrients that provided the nutrients at the lowest cost. Analyses showed that eggs, meat, milk and milk products, and dry beans and legumes were the lowest-cost sources of protein. Dry beans, nuts, and seeds were the lowest-cost sources of fiber, in some cases lower than grains. Eggs and milk were the lowest-cost sources of vitamin A, whereas vegetables and fruit were the lowest-cost sources of vitamin C. Milk products were the lowest-cost source of dietary calcium, followed by eggs and egg mixtures. Grains, dry beans, and eggs were the lowest-cost sources of iron. Vegetables, including white potatoes, and dry beans were the lowest-cost sources of potassium.
One limitation of this nutrient-driven approach is that different food groups differ in protein quality and in the bioavailability of different nutrients. Calcium and iron from animal products, in particular, are more bioavailable than from plant foods (31). New profiling models that take bioavailability into account are under development.
Within each food group, there was a wide diversity of food prices. For example, the milk and milk products group included lower-cost fluid milk as well as the higher-cost creams, cheeses, and milk desserts. The vegetables group included a wide range of lower-cost white potatoes, sweet potatoes, and carrots and a variety of canned vegetables, as well as more costly fresh produce and salad greens. The fruit group included canned fruit, dried fruit, and 100% fruit juices as well as berries and more exotic fruit. The research goal was to identify those foods within each food group, whether processed or fresh, that offered the most nutrients per penny.
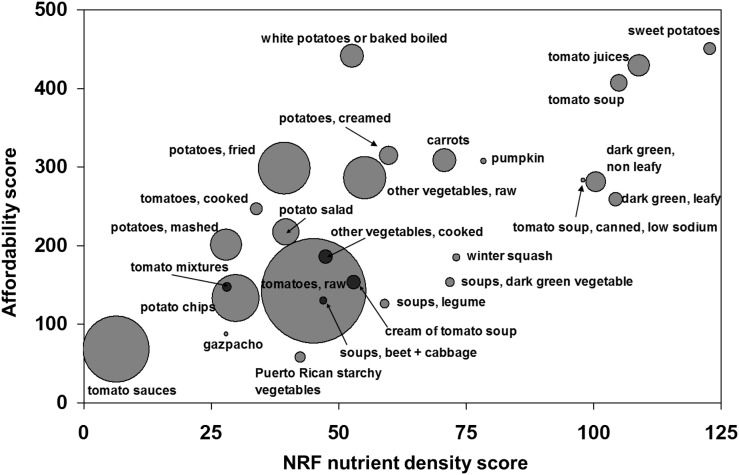
Analyses of NRF scores alone showed that citrus juices, milk, fish and shellfish, beef steak, cooked and ready-to-eat cereals, beans and nuts, vegetables, and chicken were more nutrient-rich than were cakes and cookies, sweet snacks, or desserts. Similar results were obtained whether the NRF algorithm was based on serving size or on 100 kcal of food.
Different results were obtained when positive NRF scores were divided by the food cost per serving. Here, foods that had the highest NRF nutrient density scores were not always the most economical choices. For example, the high nutrient content of green vegetables was more than offset by their higher cost, such that it was white potatoes that provided better nutritional value for the money. In terms of nutrients per unit cost, as identified by the NRF, the highest values were obtained for citrus juices, milk, fortified ready-to-eat cereals, white potatoes, and legumes and beans. As indicated in Figure 1, many of these foods offered high nutrient density as well as optimal nutrient value.
FIGURE 1.
Scatterplot of the Affordable Nutrition Index for selected food groups plotted against energy density. NRF, Nutrient Rich Foods index. Data adapted from reference 37 with permission.
New metrics of affordable nutrition.
The econometric approach to nutrient profiling, based on value metrics, can help identify affordable nutrient-rich foods within and across food groups. Studies on the nutritive value of foods as related to cost are a direct legacy of Wilbur Atwater (28). Widely credited with the development of agricultural and human nutrition research in the United States, Atwater aimed to assist people in making more nutritious food choices on a budget. In his view, knowledge of population food habits combined with data on food prices and nutrient composition tables were the basis for advising the public on how to purchase the most economical diets (28).
In Atwater’s view, the most economical foods were not only inexpensive but also best adapted to the needs, wants, and resources of the population. Combining nutrient profiling, food prices, and the knowledge of people’s food habits is one approach to integrated dietary guidance. One limitation of that approach was that vitamins and other dietary components had not yet been discovered (13). Following these principles, and based on recent nutrition science, food patterns that are consistent with the DGAs need to take into account the food’s nutritional value as well as taste, cost, convenience, and social norms (28).
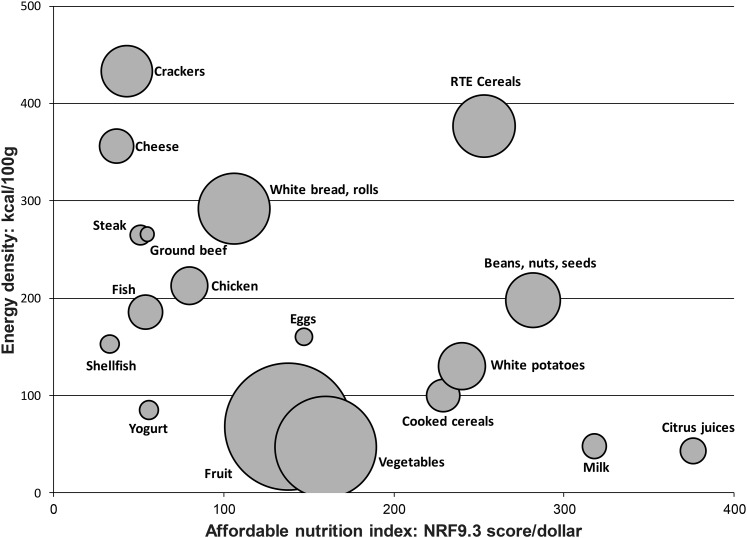
New value metrics have explored the relation between the nutrient density of foods and their cost (43, 47–49). Focusing on vegetables, one study asked which vegetables, including canned vegetables, juices, and soups, provided the most nutrients per unit cost (48). Nutrient density was measured by using the NRF9.3 index. Food cost in dollars was calculated per 100 g, per 100 kcal, per serving, and per nutrient content (48).
As shown in Figure 2, tomato juices and tomato soups, dark-green leafy and nonleafy vegetables, and deep-yellow vegetables, including sweet potatoes, had the highest nutrient density scores overall (48). However, the highest NRF scores per penny were obtained for sweet potatoes, white potatoes, tomato juices and soups, carrots, and broccoli. Based on nutrients per penny scores, these vegetables were accordingly identified as being both affordable and nutrient rich.
FIGURE 2.
The NRF index plotted against the Affordable Nutrition Index affordability score for vegetable subgroups and selected individual vegetables. Data are means for selected subcategories within the USDA vegetable food group. The size of the circle denotes combined 2-d frequency of consumption in the NHANES 2003–2004 data. The Affordable Nutrition Index score is obtained by dividing nutrient density per serving by price per serving. NRF, nutrient rich foods; RTE, ready-to-eat. Reproduced from reference 48 with permission.
High-scoring vegetables were not limited to fresh or raw produce but included vegetables cooked from frozen and canned sources. Processed tomato juices and some tomato soups also had high NRF and affordability scores. However, the reported frequency of consumption, a crude measure of consumer acceptance, was not driven by the nutrient density or the affordability of vegetables. Indeed, the reported consumption of nutrient-dense dark-green and nonleafy vegetables in the NHANES was negligible. By contrast, the lower-scoring tomato sauces, raw tomatoes, and potato chips were among the most frequently eaten vegetables, reflecting higher consumer acceptance.
Only white potatoes (boiled and baked) and carrots managed to combine nutrient density, affordability, and consumer acceptance. Additional and more detailed studies are clearly needed to determine which affordable, nutrient-rich vegetables—whether fresh, frozen, canned, or processed—are best accepted by children or adults. For example, there may be standouts among the dark-green and deep-yellow vegetables that combine high nutrient density and excellent nutrient value.
The cost of following dietary guidelines.
The 2010 DGAs concluded that food patterns built around vegetables, fruit, whole grains, and low-fat dairy products promoted good health. However, the concern was that these nutrient-dense foods were not consumed in sufficient amounts. The typical US diet contains inadequate quantities of vitamin D, calcium, potassium, and dietary fiber, along with excessive amounts of refined grains, added sugars, and fats.
Our studies suggest that such dietary imbalances may have an economic dimension. First, some nutrient-rich foods tend to cost more than do energy-dense foods of minimal nutritional value. Second, retail prices of nutrient-rich foods have increased more rapidly over time than the prices for sweets and fats. The consumers’ ability to follow the DGAs may be compromised to some degree by limited food budgets (6).
In past studies, we found that diets higher in fruit and vegetables in France were associated with higher per-calorie diet costs (39, 40, 42). Conversely, higher consumption of fats and sweets was associated with lower diet costs. For persons in the lowest 20% of energy intakes, each additional 100 g of fats and sweets was associated with 0.40€/d less in diet costs. The relation between consumption and cost flattened at higher energy intakes, but even for persons in the highest quintile of energy intakes, each additional 100 g of fats and sweets was associated with 0.13€/d less in diet costs. In other words, diets built around sweets and fats cost less, whereas low-energy-dense vegetables and fruit cost more (39, 40).
Very similar results were obtained among 2000 adults living in Seattle’s King County (4). Sociodemographic data for a stratified random sample of adult study participants were obtained through a telephone survey. Dietary intakes were obtained from an FFQ (n = 1266). Following standard procedures, nutrient intakes were adjusted for energy by using the residual method and were converted into quintiles. The estimated diet cost for each study respondent was based on Seattle supermarket retail prices for 384 FFQ component foods.
Higher intakes of dietary fiber; vitamins A, C, D, E, and B-12; and β-carotene, folate, iron, calcium, potassium, and magnesium were each associated with higher energy-adjusted diet costs (4). The cost gradient was most marked for potassium, vitamin C, β-carotene, and magnesium. Potassium, also identified as a nutrient of concern by the DGAC (1), was the most costly nutrient. As expected, higher intakes of saturated fats, trans fats, and added sugars were associated with lower energy-adjusted diet costs. This relation between diet quality measures and diet cost was found to be more pronounced for women than for men (6).
Nutrients commonly associated with a lower risk of chronic disease were associated with higher diet costs (4). In observational studies based on nationally representative NHANES data, higher-quality diets were characterized by higher intakes of vitamin C, potassium, and fiber and also cost more per calorie (2). Based on cost estimates, increasing the consumption of potassium would add an estimated $380/y to the average consumer’s food budget (6). It was not altogether surprising that cheaper and lower-quality diets were also more likely to be consumed by lower-SES groups (4).
Nutrients associated with higher NCD risk were also associated with lower diet costs. Each time study subjects obtained an additional 10% of their daily calories from saturated fat and added sugar, their diet costs were lower. Even though some researchers have dismissed it as implausible (14), the cost variable may help explain why lower-income groups fail to comply with dietary guidelines and have the highest rates of diet-related NCDs (7).
Food prices drive dietary behaviors, not only for lower-income groups. People select foods on the basis of taste, cost, convenience, and nutritional value (18). Low-income consumers faced with budgetary constraints may opt for lower-cost foods of high energy density but potentially lower nutritional value. These findings suggest that improving the American diet will require additional guidance, especially for households with little budget flexibility, as well as new policies to increase the availability and reduce the cost of healthful foods.
Vegetable cost metrics.
Vegetables are important sources of dietary fiber, vitamins, and minerals in the diets of children and adults. The cost of school meals has come under scrutiny with the USDA National School Lunch Program’s new requirements for weekly servings of vegetables, beans, and peas. We estimated the cost impact of meeting the USDA regulations using 2008 national prices for 98 vegetables in fresh, frozen, and canned form (49). Food costs were calculated per 100 g, per 100 kcal, and per edible cup. Our measure of nutrient density was based on 6 nutrients: dietary fiber, potassium, magnesium, and vitamins A, C, and K. The cost-per-nutrient value metric was based on the estimated cost of meeting 10% of the DV for each nutrient per reference amount.
Creating healthy food patterns needs to take nutrient density, cost, as well as children’s food preferences into account. One finding of interest was that most of the vegetables listed by the USDA (52 of 98) were never actually consumed by children or adolescents in the 2003–2004 NHANES database. Clearly, taste, acceptability, and social norms need to enter into the creation of healthy food patterns. For those vegetables that were consumed (46 of 98), the lowest-cost items were beans (pinto beans and lentils), white potatoes, sweet potatoes, French-fried potatoes, and carrots. Of these, beans were least expensive but also provided the most calories per gram (49). In general, beans and starchy vegetables, including white potatoes, were cheaper per 100 kcal than were dark-green and deep-yellow vegetables.
The median cost per 10% DV for potassium and fiber was lowest for potatoes ($0.14 for potassium and $0.19 for fiber) and for beans ($0.10 and $0.05, respectively). For vitamin C, potatoes ($0.10) and dark-green vegetables ($0.12) had the lowest cost per 10% DV. For vitamins A and K, dark-green vegetables had the lowest cost per 10% DV.
Overall, the best nutritional value was provided by beans, white potatoes, sweet potatoes, and carrots. The combined affordability metric, based on 6 nutrients, showed that beans scored best (257.5), followed by potatoes (177.9). It is also worth noting that not all of the top-ranked products were fresh; frozen and canned produce was very affordable, specifically canned beans, green beans, and collard greens. Fresh, frozen, and canned vegetables had similar nutrient profiles and similar nutritional value. Among the most affordable vegetables, white potatoes (fried and nonfried) and carrots were best liked and had the highest frequency of use.
These new metrics of affordable nutrition can help food service and health professionals identify those vegetable subgroups in the school lunch that are liked and provide the best nutritional value per penny (49, 50).
Preparation and time.
One criticism of the USDA Thrifty Food Plan, an optimized nutrient-rich diet at low cost, was that many of the low-cost foods required both time and skills to prepare (51, 52). Time poverty, often associated with material poverty, was not always taken into account in assessing the true diet cost (51). Research on the time spent on cooking and preparing food in relation to diet quality has been limited. A recent report examined the time spent in food preparation, as reported by 1317 adults in a population-based survey (53). Dividing the population sample into 3 groups by time spent (<1, 1–2, and >2 h) showed that working adults who placed a high priority on convenience spent the least time in the kitchen. Those adults also spent more money on foods away from home and were more likely to visit fast-food restaurants. Interestingly, more time spent in food preparation was associated with more frequent consumption of vegetables, salads, fruit, and fruit juices. The time spent cooking and preparing food may be another, not fully recognized, predictor of healthier diets (53) and may deserve a separate mention in dietary guidance.
Conclusions
The present hypothesis is that the observed social gradient in NCDs may be related in part to food prices and diet costs. Faced with lower food budgets and diminished purchasing power, most people are unwilling to go hungry or to abandon their usual eating habits. The most viable economic option is to select lower-cost, energy-dense diets, even though such diets are likely to be nutrient poor. Indeed, diets of lower-income households provide cheap, concentrated energy but can be deficient in essential nutrients. Compliance with the DGAs, as measured by the Healthy Eating Index 2005, was associated with higher incomes, more education, lower rates of obesity and overweight, and with higher per-calorie diet cost (2).
Diet optimization modeling, based on linear programming (54, 55), has provided an alternative econometric approach to modeling human behavior. In modeling studies, a sharp reduction in food budgets uniformly led to energy-dense diets that were similar in composition to those consumed by the poor (27). Recently, an inadvertent confirmation of the French modeling studies was provided by economic analyses from the United Kingdom (56). The open letter to Prime Minister David Cameron (5) stressed that low-wage groups in the United Kingdom were not earning enough money to meet their most basic nutritional needs to maintain a healthy diet. In the wake of the economic recession of 2008, more British consumers have turned to cheaper energy-dense foods, higher in sugars and fats (56), and with lower per-calorie diet cost. According to the letter, the economic recession has translated into families cutting back on fresh produce and buying cheap, sweet, fatty, salty, or processed foods that need little cooking (5). The ERS/USDA research has repeatedly declared such behavior to be impossible (14).
However, not all low-cost foods are necessarily nutrient poor. Based on nutrient profiling and the affordability metrics described above, white potatoes, beans, legumes, pulses, carrots, milk, and eggs were among the most affordable yet nutrient-rich foods (57). Similarly, not all low-cost diets need to be nutrient poor. For any level of diet cost, a wide variation in diet quality was observed. Conversely, a given level of diet quality could be associated with a range of estimated per-calorie diet costs.
In every population, there were subgroups who achieved high-quality diets at an unexpectedly low cost. In published analyses of NHANES data, these more resilient groups included older adults, women, and Mexican Americans/other Hispanics (57). At this time, given the cross-sectional databases, nutrition resilience has not yet been linked with improved health outcomes. Clearly, more research on this topic is needed.
In the behavioral literature, the ability to find better solutions to a problem despite similar constraints has been called positive deviance. People who achieve high diet quality at low cost may already have the solution. The research challenge is to identify who they are, what they think, how they shop, and what foods they buy. Further examination of their diets may help inform future DGAs. Promoting food patterns that are both healthful and affordable should be the goal of food and nutrition policy.
Acknowledgments
The sole author had responsibility for all parts of the manuscript.
Footnotes
Abbreviations used: DGAC, Dietary Guidelines Advisory Committee; DGAs, Dietary Guidelines for Americans; DV, daily value; ERS, Economic Research Service; FNDDS, Food and Nutrient Database for Dietary Studies; NCD, noncommunicable disease; NRF, Nutrient Rich Foods; SES, socioeconomic status.
References
- 1.USDA; US Department of Health and Human Services. Dietary guidelines for Americans, 2010. 7th ed. Washington (DC): US Government Printing Office; 2010. [DOI] [PMC free article] [PubMed]
- 2.Rehm CD, Monsivais P, Drewnowski A. The quality and monetary value of diets consumed by adults in the United States. Am J Clin Nutr 2011;94:1333–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Monsivais P, Aggarwal A, Drewnowski A. Are socio-economic disparities in diet quality explained by diet cost? J Epidemiol Community Health 2012;66:530–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aggarwal A, Monsivais P, Drewnowski A. Nutrient intakes linked to better health outcomes are associated with higher diet costs in the US. PLoS ONE 2012;7:e37533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ashton JR, Middleton J, Lang T. Open letter to Prime Minister David Cameron on food poverty in the UK. Lancet 2014;383:1631. [DOI] [PubMed] [Google Scholar]
- 6.Monsivais P, Aggarwal A, Drewnowski A. Following federal guidelines to increase nutrient consumption may lead to higher food costs for consumers. Health Aff (Millwood) 2011;30:1471–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr 2004;79:6–16. [DOI] [PubMed] [Google Scholar]
- 8.Darmon N, Drewnowski A. Does social class predict diet quality? Am J Clin Nutr 2008;87:1107–17. [DOI] [PubMed] [Google Scholar]
- 9.Monsivais P, Drewnowski A. Lower-energy-density diets are associated with higher monetary costs per kilocalorie and are consumed by women of higher socioeconomic status. J Am Diet Assoc 2009;109:814–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Drewnowski A, Barratt-Fornell A. Do healthier diets cost more? Nutr Today 2004;39:161–8. [Google Scholar]
- 11.Golan E, Stewart H, Kuchler F, Dong D. Can low-income Americans afford a healthy diet? USDA, Economic Research Service. [cited 2014 Jul 6]. Available from: http://www.ers.usda.gov/amber-waves/2008-november/can-low-income-americans-afford-a-healthy-diet.aspx#.VO5ElC59hLM.
- 12.Cassady D, Jetter KM, Culp J. Is price a barrier to eating more fruits and vegetables for low-income families? J Am Diet Assoc 2007;107:1909–15. [DOI] [PubMed] [Google Scholar]
- 13.Rao M, Afshin A, Singh G, Mozaffarian D. Do healthier foods and diet patterns cost more than less healthy options? A systematic review and meta-analysis. BMJ Open 2013;3:e004277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Davis GC, Carlson A. The inverse relationship between food price and energy density: is it spurious? Public Health Nutr 2014;1–7 (Epub ahead of print). [DOI] [PMC free article] [PubMed]
- 15.Carlson A, Frazão E. Are healthy foods really more expensive? It depends on how you measure the price. Economic Research Service USDA Economic Information Bulletin [cited 2014 Jul 3]. Available from: http://www.ers.usda.gov/publications/eib-economic-information-bulletin/eib96.aspx#.U_JCdmPCcZx.
- 16.Stewart H, Hyman J, Buzby JC, Frazão E, Carlson A. How much do fruits and vegetables cost? USDA Economic Information Bulletin [cited 2014 Jul 5]. Available from: http://www.ers.usda.gov/publications/eib-economic-information-bulletin/eib71.aspx#.U_JDFGPCcZx.
- 17.Monsivais P, Rehm CD. Potential nutritional and economic effects of replacing juice with fruit in the diets of children in the United States. Arch Pediatr Adolesc Med 2012;166:459–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Glanz K, Basil M, Maibach E, Goldberg J, Snyder D. Why Americans eat what they do: taste, nutrition, cost, convenience, and weight control concerns as influences on food consumption. J Am Diet Assoc 1998;98:1118–26. [DOI] [PubMed] [Google Scholar]
- 19.Kant AK. Consumption of energy-dense, nutrient-poor foods by adult Americans: nutritional and health implications. The Third National Health and Nutrition Examination Survey, 1988–1994. Am J Clin Nutr 2000;72:929–36. [DOI] [PubMed] [Google Scholar]
- 20.Slawson DL, Fitzgerald N, Morgan KT. Position of the Academy of Nutrition and Dietetics: the role of nutrition in health promotion and chronic disease prevention. J Acad Nutr Diet 2013;113:972–9. [DOI] [PubMed] [Google Scholar]
- 21.Prentice AM, Jebb SA. Fast foods, energy density and obesity: a possible mechanistic link. Obes Rev 2003;4:187–94. [DOI] [PubMed] [Google Scholar]
- 22.Bray GA, Nielsen SJ, Popkin BM. Consumption of high-fructose corn syrup in beverages may play a role in the epidemic of obesity. Am J Clin Nutr 2004;79:537–43. [DOI] [PubMed] [Google Scholar]
- 23.Bray GA, Popkin BM. Dietary fat intake does affect obesity! Am J Clin Nutr 1998;68:1157–73. [DOI] [PubMed] [Google Scholar]
- 24.Jameson M. A reversal on carbs. Los Angeles Times. 2010 Dec 20 [cited 2014 Jul 1]. Available from: http://articles.latimes.com/2010/dec/20/health/la-he-carbs-20101220.
- 25.Chronic Disease Prevention. Sugar—the real villain [cited 2014 Jul 2]. Available from: http://chronicdiseaseprevention29.blogspot.com/2012/11/sugar-real-villain.html.
- 26.James WP, Nelson M, Ralph A, Leather S. Socioeconomic determinants of health: the contribution of nutrition to inequalities in health. BMJ 1997;314:1545–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Darmon N, Ferguson E, Briend A. Do economic constraints encourage the selection of energy dense diets? Appetite 2003;41:315–22. [DOI] [PubMed] [Google Scholar]
- 28.Drewnowski A. The cost of US foods as related to their nutritive value. Am J Clin Nutr 2010;92:1181–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mendoza JA, Drewnowski A, Christakis DA. Dietary energy density is associated with obesity and the metabolic syndrome in U.S. adults. Diabetes Care 2007;30:974–9. [DOI] [PubMed] [Google Scholar]
- 30.Schröder H, Marrugat J, Covas MI. High monetary costs of dietary patterns associated with lower body mass index: a population-based study. Int J Obes (Lond) 2006;30:1574–9. [DOI] [PubMed] [Google Scholar]
- 31.Drewnowski A, Fulgoni V III. Nutrient profiling of foods: creating a nutrient-rich food index. Nutr Rev 2008;66:23–39. [DOI] [PubMed] [Google Scholar]
- 32.Fulgoni, 3rd VL, Keast DR, Drewnowski A. Development and validation of the nutrient-rich foods index: a tool to measure nutritional quality of foods. J Nutr 2009;139:1549–54. [DOI] [PubMed] [Google Scholar]
- 33.Hawley KL, Roberto CA, Bragg MA, Liu PJ, Schwartz MB, Brownell KD. The science on front-of-package food labels. Public Health Nutr 2013;16:430–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Savoie N, Barlow Gale K, Harvey KL, Binnie MA, Pasut L. Consumer perceptions of front-of-package labelling systems and healthiness of foods. Can J Public Health 2013;104:e359–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nestlé. Nestle Nutritional Profiling System: supporting the optimization of products [cited 2014 Jul 2]. Available from: http://www.research.nestle.com/nutritionhealth/nutritionalprofiling.
- 36.Unilever. The Choices Programme [cited 2014 Jul]. Available from: http://www.unilever.com/aboutus/Nutritionandhealth/Thechoicesprogramme.
- 37.Drewnowski A. The Nutrient Rich Foods Index helps to identify healthy, affordable foods. Am J Clin Nutr 2010;91(Suppl):1095S–101S. [DOI] [PubMed] [Google Scholar]
- 38.Maillot M, Darmon N, Darmon M, Lafay L, Drewnowski A. Nutrient-dense food groups have high energy costs: an econometric approach to nutrient profiling. J Nutr 2007;137:1815–20. [DOI] [PubMed] [Google Scholar]
- 39.Darmon N, Briend A, Drewnowski A. Energy-dense diets are associated with lower diet costs: a community study of French adults. Public Health Nutr 2004;7:21–7. [DOI] [PubMed] [Google Scholar]
- 40.Drewnowski A, Darmon N, Briend A. Replacing fats and sweets with vegetables and fruits—a question of cost. Am J Public Health 2004;94:1555–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Darmon N, Ferguson EL, Briend A. A cost constraint alone has adverse effects on food selection and nutrient density: an analysis of human diets by linear programming. J Nutr 2002;132:3764–71. [DOI] [PubMed] [Google Scholar]
- 42.Maillot M, Darmon N, Drewnowski A. Are the lowest-cost healthful food plans culturally and socially acceptable? Public Health Nutr 2010;13:1178–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Drewnowski A. The contribution of milk and milk products to micronutrient density and affordability of the U.S. diet. J Am Coll Nutr 2011;30:422S–8S. [DOI] [PubMed] [Google Scholar]
- 44.Drewnowski A, Maillot M, Darmon N. Testing nutrient profile models in relation to energy density and energy cost. Eur J Clin Nutr 2009;63:674–83. [DOI] [PubMed] [Google Scholar]
- 45.Drewnowski A, Maillot M, Darmon N. Should nutrient profiles be based on 100 g, 100 kcal or serving size? Eur J Clin Nutr 2009;63:898–904. [DOI] [PubMed] [Google Scholar]
- 46.US Food and Drug Administration. Food labeling, C.F.R. title 21, vol. 2, part 101. Reference amounts customarily consumed per eating occasion. [cited Jul 6]. Available from: http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/cfrsearch.cfm?fr=101.12.
- 47.Darmon N, Darmon M, Maillot M, Drewnowski A. A nutrient density standard for vegetables and fruits: nutrients per calorie and nutrients per unit cost. J Am Diet Assoc 2005;105:1881–7. [DOI] [PubMed] [Google Scholar]
- 48.Drewnowski A. New metrics of affordable nutrition: which vegetables provide most nutrients for least cost? J Acad Nutr Diet 2013;113:1182–7. [DOI] [PubMed] [Google Scholar]
- 49.Drewnowski A, Rehm CD. Vegetable cost metrics show that potatoes and beans provide most nutrients per penny. PLoS ONE 2013;8:e63277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shanklin CW, Wie S. Nutrient contribution per 100 kcal and per penny for the 5 meal components in school lunch: entree, milk, vegetable/fruit, bread/grain, and miscellaneous. J Am Diet Assoc 2001;101:1358–61. [DOI] [PubMed] [Google Scholar]
- 51.Rose D. Food stamps, the Thrifty Food Plan, and meal preparation: the importance of the time dimension for US nutrition policy. J Nutr Educ Behav 2007;39:226–32. [DOI] [PubMed] [Google Scholar]
- 52.Wilde PE, Llobrera J. Using the Thrifty Food Plan to assess the cost of a nutritious diet. J Consum Aff 2009;43:274–304. [Google Scholar]
- 53.Monsivais P, Aggarwal A, Drewnowski A. Time spent on home food preparation and indicators of healthy eating. Am J Prev Med 2014;47:796–802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Darmon N, Vieux F, Maillot M, Volatier JL, Martin A. Nutrient profiles discriminate between foods according to their contribution to nutritionally adequate diets: a validation study using linear programming and the SAIN,LIM system. Am J Clin Nutr 2009;89:1227–36. [DOI] [PubMed] [Google Scholar]
- 55.Maillot M, Ferguson EL, Drewnowski A, Darmon N. Nutrient profiling can help identify foods of good nutritional quality for their price: a validation study with linear programming. J Nutr 2008;138:1107–13. [DOI] [PubMed] [Google Scholar]
- 56.Butler P. Britain in nutrition recession as food prices rise and incomes shrink. The Guardian. 2012 Nov 18 [cited 2014 Jul 5]. Available from: http://www.theguardian.com/society/2012/nov/18/breadline-britain-nutritional-recession-austerity.
- 57.Monsivais P, Rehm CD, Drewnowski A. The DASH diet and diet costs among ethnic and racial groups in the United States. JAMA Intern Med 2013;173:1922–4. [DOI] [PMC free article] [PubMed] [Google Scholar]