Abstract
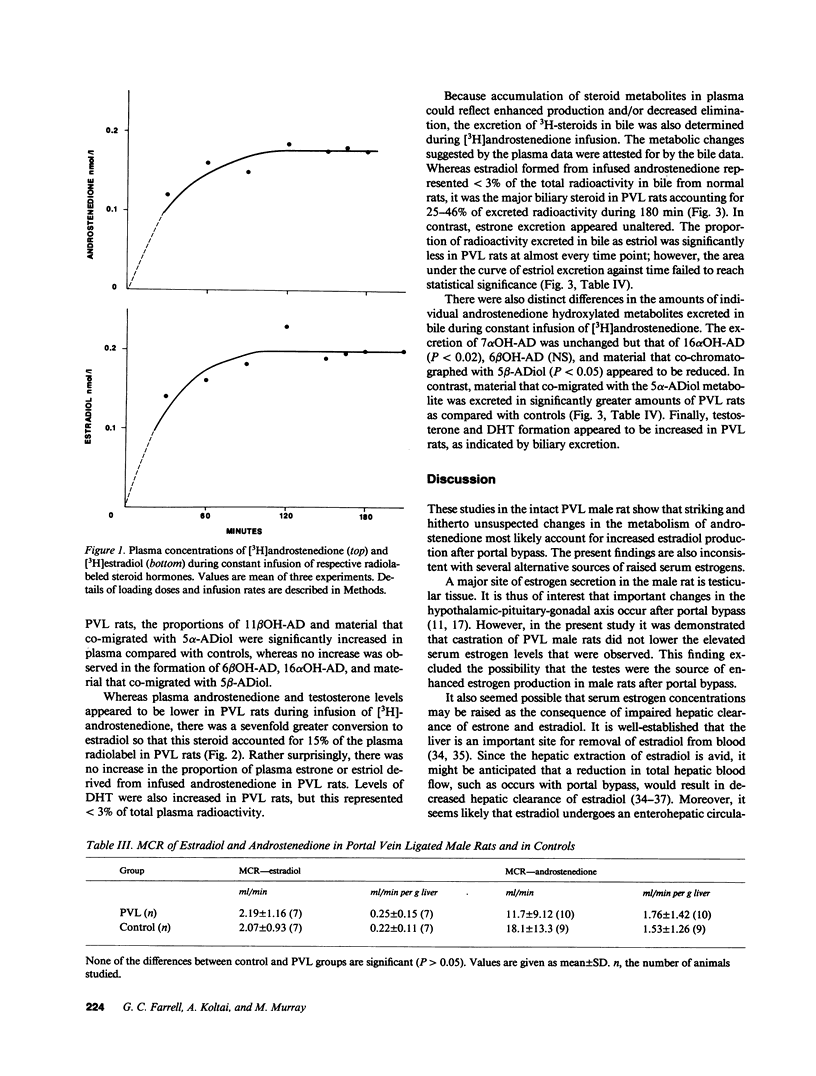
We sought to establish the mechanism for the raised serum estrogen levels that occur in male rats with portal hypertension and resultant portal bypass. Using the portal vein ligated (PVL) rat model, we evaluated plasma steroid hormone concentrations, metabolic clearance rate (MCR) of estradiol, and hepatic metabolism of androstenedione to estrogens and other products. In contrast to serum testosterone levels that were reduced, serum androstenedione levels were normal in the PVL rat. Estradiol MCR was measured by a constant intravenous infusion technique and was found to be similar in PVL and control animals. Androstenedione MCR was determined during constant intravenous infusion of [3H]androstenedione, and the resultant radiolabeled steroids present in plasma were separated by thin layer chromatography. The MCR of androstenedione was not diminished in PVL rats compared with controls. However, there was a sevenfold increase in the plasma estradiol derived from [3H]androstenedione in rats with portal bypass. Examination of radiolabel excreted in bile during infusion of [3H]androstenedione showed that 25-46% of this steroid was converted to estradiol in PVL rats compared with less than 3% in control male rats (P less than 0.001). Moreover, there was a selective reduction in the excretion of 16 alpha-hydroxyandrostenedione, a finding which suggested that the metabolism of androstenedione via this pathway was decreased. Androstenedione 16 alpha-hydroxylation is known to be catalyzed by a male-specific cytochrome P-450 isoform, P-450UT-A. We conclude that raised plasma estradiol levels after portal bypass in male rats are due to increased production rates, resulting in turn from enhanced aromatization of androstenedione to estradiol. On the basis of the observed specific changes in androstenedione hydroxylation pathways, it is proposed that alterations in levels of sex-specific forms of cytochrome P-450 occur in male rats with portal bypass and could account for the enhanced formation of estradiol.
Full text
PDF






Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Adlercreutz H. Oestrogen metabolism in liver disease. J Endocrinol. 1970 Jan;46(1):129–163. doi: 10.1677/joe.0.0460129. [DOI] [PubMed] [Google Scholar]
- Back D. J., Breckenridge A. M., Crawford F. E., Giles M., Orme M. L., Rowe P. H. The pharmacokinetics of oestrone sulphate in the rat. J Steroid Biochem. 1981 Oct;14(10):1045–1047. doi: 10.1016/0022-4731(81)90214-4. [DOI] [PubMed] [Google Scholar]
- Cheng K. C., Schenkman J. B. Testosterone metabolism by cytochrome P-450 isozymes RLM3 and RLM5 and by microsomes. Metabolite identification. J Biol Chem. 1983 Oct 10;258(19):11738–11744. [PubMed] [Google Scholar]
- Farrell G. C., Gollan J. L., Schmid R. Efflux of bilirubin into plasma following hepatic degradation of exogenous heme. Proc Soc Exp Biol Med. 1980 Apr;163(4):504–509. doi: 10.3181/00379727-163-40805. [DOI] [PubMed] [Google Scholar]
- Farrell G. C., Koltai A., Zaluzny L., Murray M. Effects of portal vein ligation on sex hormone metabolism in male rats: relationship to lowered hepatic cytochrome P450 levels. Gastroenterology. 1986 Feb;90(2):299–305. doi: 10.1016/0016-5085(86)90924-8. [DOI] [PubMed] [Google Scholar]
- Farrell G. C., Zaluzny L. Portal vein ligation selectively lowers hepatic cytochrome P450 levels in rats. Gastroenterology. 1983 Aug;85(2):275–282. [PubMed] [Google Scholar]
- Gordon G. G., Olivo J., Rafil F., Southren A. L. Conversion of androgens to estrogens in cirrhosis of the liver. J Clin Endocrinol Metab. 1975 Jun;40(6):1018–1026. doi: 10.1210/jcem-40-6-1018. [DOI] [PubMed] [Google Scholar]
- Green G. R. Mechanism of hypogonadism in cirrhotic males. Gut. 1977 Oct;18(10):843–853. doi: 10.1136/gut.18.10.843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross G., Perrier C. V. Letter: Intrahepatic portasystemic shunting in cirrhotic patients. N Engl J Med. 1975 Nov 13;293(20):1046–1047. doi: 10.1056/NEJM197511132932017. [DOI] [PubMed] [Google Scholar]
- Gustafsson J. A., Mode A., Norstedt G., Skett P. Sex steroid induced changes in hepatic enzymes. Annu Rev Physiol. 1983;45:51–60. doi: 10.1146/annurev.ph.45.030183.000411. [DOI] [PubMed] [Google Scholar]
- Hirokata Y., Tong S., Siddik Z. H., Trush M. A., Mimnaugh E. G., Gram T. E. Sex-dependent differences in the effects of portacaval anastomosis on hepatic monooxygenases in rats. Biochem Pharmacol. 1982 Feb 15;31(4):499–502. doi: 10.1016/0006-2952(82)90150-2. [DOI] [PubMed] [Google Scholar]
- Horton R., Tait J. F. Androstenedione production and interconversion rates measured in peripheral blood and studies on the possible site of its conversion to testosterone. J Clin Invest. 1966 Mar;45(3):301–313. doi: 10.1172/JCI105344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kato R. Sex-related differences in drug metabolism. Drug Metab Rev. 1974;3(1):1–32. doi: 10.3109/03602537408993737. [DOI] [PubMed] [Google Scholar]
- Longcope C., Billiar R. B., Takaoka Y., Reddy P. S., Richardson D., Little B. Tissue sites of aromatization in the female rhesus monkey. Endocrinology. 1983 Nov;113(5):1679–1682. doi: 10.1210/endo-113-5-1679. [DOI] [PubMed] [Google Scholar]
- Longcope C., Kato T., Horton R. Conversion of blood androgens to estrogens in normal adult men and women. J Clin Invest. 1969 Dec;48(12):2191–2201. doi: 10.1172/JCI106185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacGeoch C., Morgan E. T., Gustafsson J. A. Hypothalamo-pituitary regulation of cytochrome P-450(15) beta apoprotein levels in rat liver. Endocrinology. 1985 Nov;117(5):2085–2092. doi: 10.1210/endo-117-5-2085. [DOI] [PubMed] [Google Scholar]
- Miyairi S., Fishman J. Radiometric analysis of oxidative reactions in aromatization by placental microsomes. Presence of differential isotope effects. J Biol Chem. 1985 Jan 10;260(1):320–325. [PubMed] [Google Scholar]
- Mode A., Gustafsson J. A., Jansson J. O., Edén S., Isaksson O. Association between plasma level of growth hormone and sex differentiation of hepatic steroid metabolism in the rat. Endocrinology. 1982 Nov;111(5):1692–1697. doi: 10.1210/endo-111-5-1692. [DOI] [PubMed] [Google Scholar]
- Morgan E. T., MacGeoch C., Gustafsson J. A. Hormonal and developmental regulation of expression of the hepatic microsomal steroid 16 alpha-hydroxylase cytochrome P-450 apoprotein in the rat. J Biol Chem. 1985 Oct 5;260(22):11895–11898. [PubMed] [Google Scholar]
- Morgan E. T., MacGeoch C., Gustafsson J. A. Sexual differentiation of cytochrome P-450 in rat liver. Evidence for a constitutive isozyme as the male-specific 16 alpha-hydroxylase. Mol Pharmacol. 1985 Apr;27(4):471–479. [PubMed] [Google Scholar]
- Murray M., Zaluzny L., Dannan G. A., Guengerich F. P., Farrell G. C. Altered regulation of cytochrome P-450 enzymes in choline-deficient cirrhotic male rat liver: impaired regulation and activity of the male-specific androst-4-ene-3,17-dione 16 alpha-hydroxylase, cytochrome P-450UT-A, in hepatic cirrhosis. Mol Pharmacol. 1987 Jan;31(1):117–121. [PubMed] [Google Scholar]
- Nimrod A., Ryan K. J. Aromatization of androgens by human abdominal and breast fat tissue. J Clin Endocrinol Metab. 1975 Mar;40(3):367–372. doi: 10.1210/jcem-40-3-367. [DOI] [PubMed] [Google Scholar]
- Olivo J., Gordon G. G., Rafii F., Southren A. L. Estrogen metabolism in hyperthyroidism and in cirrhosis of the liver. Steroids. 1975 Jul;26(1):47–56. doi: 10.1016/0039-128x(75)90005-7. [DOI] [PubMed] [Google Scholar]
- Ossenberg F. W., Pointard L., Benhamou J. P. Effect of portacaval shunt on hepatic cytochrome P-450 in rats. Rev Eur Etud Clin Biol. 1972 Oct;17(8):791–793. [PubMed] [Google Scholar]
- POPPER H., ELIAS H., PETTY D. E. Vascular pattern of the cirrhotic liver. Am J Clin Pathol. 1952 Aug;22(8):717–729. doi: 10.1093/ajcp/22.8.717. [DOI] [PubMed] [Google Scholar]
- Pector J. C., Ossenberg F. W., Peignoux M., Benhamou J. P. The effect of portacaval transposition on hepatic cytochrome P-450 in the rat. Biomedicine. 1975 Jun 10;23(5):160–162. [PubMed] [Google Scholar]
- Pector J. C., Winand J., Dehaye J. P., Christophe J. Effects of portacaval shunt and transposition on fatty acid and cholesterol biosynthesis in rat liver. Am J Physiol. 1980 Aug;239(2):G83–G89. doi: 10.1152/ajpgi.1980.239.2.G83. [DOI] [PubMed] [Google Scholar]
- Ruh T. S. Simultaneous separation of estrogens and androgens using thin-layer chromatography. J Chromatogr. 1976 Jun 9;121(1):82–84. doi: 10.1016/s0021-9673(00)82302-x. [DOI] [PubMed] [Google Scholar]
- Ryan D. E., Iida S., Wood A. W., Thomas P. E., Lieber C. S., Levin W. Characterization of three highly purified cytochromes P-450 from hepatic microsomes of adult male rats. J Biol Chem. 1984 Jan 25;259(2):1239–1250. [PubMed] [Google Scholar]
- Schindler A. E. Steroid metabolism of fetal tissues. II. Conversion of androstenedione to estrone. Am J Obstet Gynecol. 1975 Oct 1;123(3):265–268. doi: 10.1016/0002-9378(75)90196-9. [DOI] [PubMed] [Google Scholar]
- Smuk M., Schwers J. Aromatization of androstenedione by human adult liver in vitro. J Clin Endocrinol Metab. 1977 Nov;45(5):1009–1012. doi: 10.1210/jcem-45-5-1009. [DOI] [PubMed] [Google Scholar]
- Thompson E. A., Jr, Siiteri P. K. Utilization of oxygen and reduced nicotinamide adenine dinucleotide phosphate by human placental microsomes during aromatization of androstenedione. J Biol Chem. 1974 Sep 10;249(17):5364–5372. [PubMed] [Google Scholar]
- Thorneycroft I. H., Ribeiro W. O., Stone S. C., Tillson S. A. A radioimmunoassay of androstenedione. Steroids. 1973 Jan;21(1):111–122. doi: 10.1016/0039-128x(73)90024-x. [DOI] [PubMed] [Google Scholar]
- Van Thiel D. H., Gavaler J. S., Cobb C. F., McClain C. J. An evaluation of the respective roles of portosystemic shunting and portal hypertension in rats upon the production of gonadal dysfunction in cirrhosis. Gastroenterology. 1983 Jul;85(1):154–159. [PubMed] [Google Scholar]
- Van Thiel D. H., Gavaler J. S., Schade R. R. Liver disease and the hypothalamic pituitary gonadal axis. Semin Liver Dis. 1985 Feb;5(1):35–45. doi: 10.1055/s-2008-1041756. [DOI] [PubMed] [Google Scholar]
- Van Thiel D. H., Gavaler J. S., Wight C., Smith W. I., Jr, Abuid J. Thyrotropin-releasing hormone (TRH)-induced growth hormone (hGH) responses in cirrhotic men. Gastroenterology. 1978 Jul;75(1):66–70. [PubMed] [Google Scholar]
- Waxman D. J., Dannan G. A., Guengerich F. P. Regulation of rat hepatic cytochrome P-450: age-dependent expression, hormonal imprinting, and xenobiotic inducibility of sex-specific isoenzymes. Biochemistry. 1985 Jul 30;24(16):4409–4417. doi: 10.1021/bi00337a023. [DOI] [PubMed] [Google Scholar]
- Waxman D. J., Ko A., Walsh C. Regioselectivity and stereoselectivity of androgen hydroxylations catalyzed by cytochrome P-450 isozymes purified from phenobarbital-induced rat liver. J Biol Chem. 1983 Oct 10;258(19):11937–11947. [PubMed] [Google Scholar]
- Waxman D. J. Rat hepatic cytochrome P-450 isoenzyme 2c. Identification as a male-specific, developmentally induced steroid 16 alpha-hydroxylase and comparison to a female-specific cytochrome P-450 isoenzyme. J Biol Chem. 1984 Dec 25;259(24):15481–15490. [PubMed] [Google Scholar]
- Wood A. W., Ryan D. E., Thomas P. E., Levin W. Regio- and stereoselective metabolism of two C19 steroids by five highly purified and reconstituted rat hepatic cytochrome P-450 isozymes. J Biol Chem. 1983 Jul 25;258(14):8839–8847. [PubMed] [Google Scholar]
- Wu C. H., Lundy L. E. Radioimmunoassay of plasma estrogens. Steroids. 1971 Jul;18(1):91–111. doi: 10.1016/s0039-128x(71)80174-5. [DOI] [PubMed] [Google Scholar]



