Abstract
Prevalence of the metabolic syndrome has increased in tandem with obesity and is associated with structural and functional cerebral damage. A new study confirms the association between the metabolic syndrome and reduced brain volume in the absence of diabetes mellitus. Here, we highlight how vascular dysfunction potentially contributes to this brain damage.
The prevalence of obesity among US adults is currently an astonishing 35.9%, with 15.5% of the population having a BMI ≥35 kg/m2 and 6.3% having a BMI ≥40 kg/m2.1 Obesity is strongly linked to the metabolic syndrome, a cluster of disease risk factors that includes hypertension, abdominal obesity, elevated triglycerides, low HDL and hyperglycaemia (or marked insulin resistance).2 The prevalence of the metabolic syndrome increases with increasing weight and age, reaching nearly 40% in 40–60 year olds and more than 50% in those over 60 years of age.3 What is particularly worrisome, in addition to the increased rates of diabetes mellitus and cardiovascular disease that are associated with the metabolic syndrome, is the fact that the metabolic syndrome is also associated with significant brain impairments. Tiehuis and colleagues studied a large cohort of middle-aged and elderly patients with manifest arterial disease, including coronary artery disease (myocardial infarction and/or coronary bypass/angioplasty), cerebrovascular disease (transient ischaemic attack or stroke), peripheral arterial disease (claudication, at rest pain or angioplasty) and aortic aneurism (distal aortic diameter ≥3 cm).4 The researchers demonstrated that presence of the metabolic syndrome is associated with a more global brain atrophy, even in individuals without diabetes mellitus.4 Although this is an interesting finding, it is difficult to generalize from these data the effect on brain integrity in other individuals with the metabolic syndrome but who have milder forms of arterial disease.
Autopsy studies have shown that brain atrophy is part of the normal aging process5 and thus should be first placed in a more general context. These studies show that brain mass peaks at 20 year of age, after which time it declines at a rate of 0.1–0.2% per year, with the rate of brain tissue loss accelerating after about 65 years of age.5 Post-mortem analysis of the brains of participants in the Honolulu–Asia aging study provided early evidence of a direct relationship between high blood pressure and brain atrophy, in addition to increased neuropathic cerebrovascular lesions.6 MRI is now extensively used to noninvasively characterize brain volume ; MRI studies have established that brain atrophy is a feature of normal aging and have confirmed that atrophy rates increase with a large number of comorbidities.
Tiehuis and co-workers provide evidence that the metabolic syndrome is associated with reduced brain volume.4 Previous cross-sectional studies have reported associations between the metabolic syndrome and silent brain infarctions, white matter lesions, and among other things, elevated levels of myoinositol that are suggestive of neuroimflammation.7 Furthermore, the metabolic syndrome has been associated with significant cognitive dysfunction. Memory, attention and executive functions are the most commonly reported cognitive domains affected. However, most of these cognitive and structural brain findings, including those of the SMART–MR study reported by Tiehuis and colleagues,4 have been derived from studies of middle-aged or elderly individuals, and it is difficult to ascertain the effects of the metabolic syndrome on the brain independent of cardiovascular disease, which so often accompanies the metabolic syndrome in this age group.
Focusing on much younger patients might provide a clearer view of the effect of the metabolic syndrome on the brain. Although not completely free of incipient cardiovascular pathology, such as increased carotid stiffness and intima–media thickness, obese adolescents with the metabolic syndrome are devoid of significant occlusive vascular disease. Therefore, adolescents might be an effective population to ascertain how the metabolic syndrome, independent of manifest vascular disease, affects brain integrity.
Previously, we demonstrated in adolescents that the metabolic syndrome, and insulin resistance in particular, was associated with increased brain atrophy and reductions in hippocampal volumes; importantly, these associations remained significant even after adjusting for BMI.8 Furthermore, we demonstrated that obese adolescents with the metabolic syndrome also had cognitive deficits and reductions in white matter microstructural integrity, in contrast to adolescents matched by education, socioeconomic status and other demographic variables but without the metabolic syndrome.8
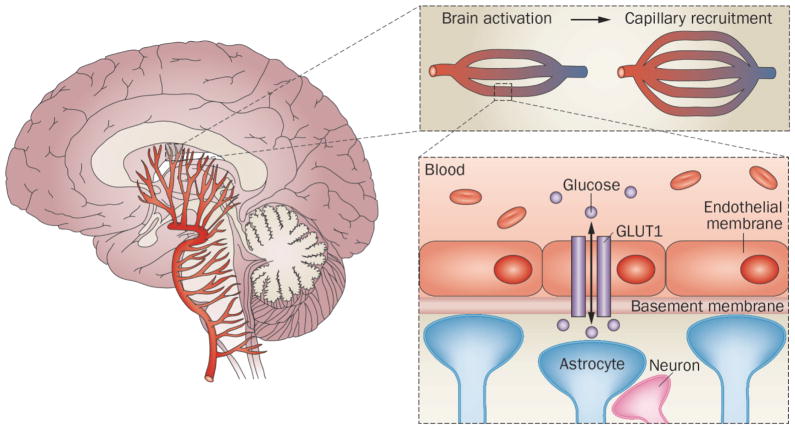
Insulin resistance is pivotal to the metabolic syndrome and is associated with endothelial dysfunction and abnormalities in peripheral vascular reactivity. The brain uses glucose as its main metabolic energy source and the glucose transporter type 1, GLUT1, at the blood–brain barrier (Figure 1) becomes saturated at normal physiological levels of blood glucose. When the brain becomes activated and utilizes increased amounts of metabolic substrate, the main way to shuttle extra glucose across the blood–brain barrier at these times of higher regional demand is to relax the regional capillary bed (capillary recruitment), thus exposing new glucose transporters to the blood. These additional glucose transporters help shuttle more glucose to the activated region of the brain. We have hypothesized that the diminished cerebral tissue perfusion and vascular reactivity associated with insulin resistance are at least partly responsible for the detrimental effects of insulin resistance and the metabolic syndrome on brain integrity. Brain perfusion and cerebral vascular reactivity are essential for maintaining energy-dependent processes (such as regional brain activation) by, in addition to generating sufficient metabolic substrate, also clearing the “waste products” produced by neuronal activity (for example, CO2, excess lactate, other metabolites and heat).9 Consequently, we have proposed that individuals with insulin resistance and/or the metabolic syndrome are unable to maintain an optimal neuronal environment, particularly during periods of high cerebral demand such as during regional brain activation. We contend that this dysfunction, when coupled with other detrimental factors that are associated with obesity-related metabolic syndrome (such as inflammation, dysregulation of the hypothalamic–pituitary axis, reduced protective neurotrophins and increased oxidative stress), will damage the brain.7,10
Figure 1.
Glucose metabolism in the brain. Glucose is transported from the blood to the brain via GLUT1. Regional activation of the brain leads to local reductions in interstitial glucose levels, which are compensated via capillary recruitment leading to increased capillary density.
Going forward, careful investigation of the role of endothelial function and cerebral vascular reactivity is warranted to understand the adverse effects of obesity-associated metabolic syndrome on brain integrity. Although the results presented by Tiehuis and colleagues are interesting, further prospective longitudinal studies of young high-risk individuals are required to help unravel the mechanisms involved in these processes.
Pullquotes.
“adolescents might be an effective population to ascertain how the metabolic syndrome … affects brain integrity”
“Insulin resistance is key to the metabolic syndrome and drives the ill effects of obesity on brain”
Acknowledgments
This work was in part supported by funding from the National Institutes of Health (DK083537).
Biographies
Henry Rusinek, PhD, is a professor in Radiology Department of New York University School of Medicine, NY, USA. He is experienced in biomedical modeling, instrumentation and imaging. He has developed algorithms for medical image analysis, physiological modeling, with emphasis on noninvasive estimates of tissue perfusion.
Antonio Convit, M.D., is the Deputy Director of the Nathan Kline Institute and a professor of Psychiatry, Medicine, and Radiology at the New York University School of Medicine, NY, USA. His work has focused on establishing the brain as a site of complications in metabolic disease and understanding possible mechanisms.
Footnotes
Competing interests: The authors declare no competing interests
References
- 1.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307:491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 2.National Cholesterol Education Program (NCEP) expert panel on detection evaluation treatment of high blood cholesterol in adults (Adult Treament Panel III). Third report of the National Cholesterol Education Program (NCEP) expert panel on detection evaluation treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- 3.Ervin RB. Prevalence of metabolic syndrome among adults 20 years of age and over, by sex, age, race and ethnicity, and body mass index: United States, 2003–2006. Natl Health Stat Report. 2009;5:1–7. [PubMed] [Google Scholar]
- 4.Tiehuis AM, et al. Metabolic syndrome, prediabetes, and brain abnormalities on MRI in patients with manifest arterial disease: the SMART-MR study. Diabetes Care. 2014 doi: 10.2337/dc14-0154. http://dx.doi.org/10.2337/dc14-0154. [DOI] [PubMed]
- 5.Dekaban AS. Changes in brain weights during the span of human life: relation of brain weights to body heights and body weights. Ann Neurol. 1978;4:345–356. doi: 10.1002/ana.410040410. [DOI] [PubMed] [Google Scholar]
- 6.Petrovitch H, et al. Midlife blood pressure and neuritic plaques, neurofibrillary tangles, and brain weight at death: the HAAS. Honolulu–Asia aging Study. Neurobiol Aging. 2000;21:57–62. doi: 10.1016/s0197-4580(00)00106-8. [DOI] [PubMed] [Google Scholar]
- 7.Yates KF, Sweat V, Yau PL, Turchiano MM, Convit A. Impact of metabolic syndrome on cognition and brain: a selected review of the literature. Arterioscler Thromb Vasc Biol. 2012;32:2060–2067. doi: 10.1161/ATVBAHA.112.252759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yau PL, Castro MG, Tagani A, Tsui WH, Convit A. Obesity and metabolic syndrome and functional and structural brain impairments in adolescence. Pediatrics. 2012;130:e856–864. doi: 10.1542/peds.2012-0324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Drake CT, Iadecola C. The role of neuronal signaling in controlling cerebral blood flow. Brain Lang. 2007;102:141–152. doi: 10.1016/j.bandl.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 10.Convit A. Links between cognitive impairment in insulin resistance: An explanatory model. Neurobiol Aging. 2005;26(Suppl 1):31–35. doi: 10.1016/j.neurobiolaging.2005.09.018. [DOI] [PubMed] [Google Scholar]