Abstract
Purpose
To examine behavioral patterns and sociodemographic predictors of diet, inactivity and tobacco use among a diverse sample of residents from low-income housing developments.
Design
Cross-sectional survey study. Households and residents were randomly selected using multi-stage cluster sampling.
Setting
Twenty low-income housing developments in the Boston metropolitan area.
Participants
828 residents completed the survey (response rate=49.3%). Forty-one percent of participants were Hispanic and 38% were non-Hispanic Black.
Measures
Outcomes measured were diet, inactivity, and tobacco use. Predictors measured were age, race/ethnicity, gender, education, country born, language spoken, and financial hardship.
Analysis
Logistic regression analyses were conducted to examine the association of three health behaviors with sociodemographic factors.
Results
Age, gender, language spoken, and financial hardship showed significant relationships with all three behaviors. For example, those who reported less financial hardship (OR=1.75) were more likely to eat healthier. Residents who spoke no English, or at least one language in addition to English, were significantly more likely to report healthier eating (OR=2.78 and 3.30 respectively) than those who spoke English only. Men were significantly more likely to report less healthy eating (OR=0.65) than women. Similar trends emerged for inactivity and tobacco use.
Conclusion
Effective health promotion interventions in low-income housing developments that leverage protective factors while addressing risk factors have the potential to reduce income-related health disparities in these concentrated resource-deprived neighborhoods.
Keywords: health promotion, health behavior, low-income population, African Americans, immigrants, public housing
PURPOSE
Persistent disparities in health behaviors and their attendant health outcomes by socio-economic status (SES) remain a central public health problem. There is robust evidence suggesting that various indicators of SES (e.g., education, income, financial hardship) are associated with disparities in participation in health behaviors,1-3 morbidity,4 and mortality.5 There are similar disparities in participation in health behaviors among people from racial/ethnic minority groups, though race/ethnicity and SES indicators are highly correlated. However, the direction of the association between membership in a certain racial/ethnic group and level of health behavior participation appears to vary by specific behaviors. For example, Centers for Disease Control and Prevention surveillance data show that Hispanics report lower smoking rates than both non-Hispanic Whites and non-Hispanic Blacks, but also report doing less physical activity and eating fewer vegetables.1,6
Understanding patterns of multiple health behaviors by SES, race/ethnicity, and relevant sociodemographic characteristics, such as gender and age, has important implications for planning policy and community intervention approaches. Evidence is accumulating that interventions addressing more than one health behavior are efficacious,7,8 cost-effective,9 and health promoting.10 With an improved understanding of the potential patterns and predictors of multiple health behaviors, it may be possible to maximize intervention effectiveness and disease prevention by strategically grouping targeted behaviors and tailoring messages and modalities to best suit the audience. There is a particular need for interventions that are responsive to the multiple health behavior patterns of persons with low income, less education, or who are immigrants.
This paper reports results from a study of residents of low-income housing developments. Intentionally segregated by lower SES, low-income housing developments represent a probable setting to address chronic disease prevention among a potentially high-risk population and have garnered increased attention in the health promotion field.11,12 About 1.2 million households in the U.S. live in public housing developments.13 These developments not only offer a geographically defined setting, they often also have community spaces, communication modalities, and infrastructures (e.g., resident liaisons and tenant councils) that could support health promotion efforts.
Prior research has shown that residents of low-income housing developments report low participation in health behaviors, including low levels of physical activity14-16 and fruit and vegetable consumption,17-19 high levels of meat and sweets consumption,19 and high rates of obesity17,20,21 and smoking.17 Low-income housing developments are also characterized by high proportions of immigrant residents who, interestingly, report varying participation in health behaviors. This variation, sometimes attributed to level of acculturation,22,23 challenges public health professionals to design contextually relevant interventions for racially/ethnically diverse settings.
The purpose of this paper is to examine the occurrence and co-occurrence of dietary patterns, sedentary behavior and tobacco use among a diverse sample of residents from low-income housing developments. We also examine the association of selected sociodemographic characteristics (gender, age, education, race/ethnicity, country of origin, language spoken, and financial hardship) with these health behaviors. This paper provides a nuanced examination of behavioral patterns and key predictors within a low-income group that will inform program development in a structured community setting.
METHODS
Design
The Health in Common study was an observational study conducted between 2005 and 2009 to investigate personal, social and environmental determinants of health behaviors among residents of low-income housing developments. Participants were recruited from the adult population of 15 publicly- and 5 privately-managed low-income housing developments across three cities in the Boston metropolitan area. In order to be eligible, a housing development had to be considered low-income housing (based on Department of Housing and Urban Development (HUD) guidelines); have mostly family units; have a minimum of 40 households within the development (largest site had 268 households); and have indicated that the primary language in the majority of households was either English, Spanish, or Haitian Creole.
Sample
Households and residents were randomly selected from 20 participating developments using multi-stage cluster sampling where the clusters were the housing developments, the listing units were households within the developments, and the elementary units were the adults within households. Project staff recruited participants via door-to-door contact. Residents of single adult households were designated as the participant. In a multi-adult household, the project staff randomly selected a resident within the household using a systematic selection methodology attributed to Kish.24 Residents were eligible for participation if they were: (1) a resident of the housing development; (2) over 18 years of age; and (3) spoke English, Spanish, or Haitian Creole.
Measures
The Resident Survey was interviewer-administered by project staff who were bilingual (English/Spanish or English/Haitian Creole). A trained project staff member conducted the 45-60 minute Resident Survey in each participant's home at a convenient time for the participant. The Resident Survey included standard items used on existing national and state surveys, items from our prior research, and items from the research literature. Where possible, we used measures with tested validity and reliability. To ensure item comprehension, linguistic appropriateness, and face validity, we conducted cognitive walk-throughs25 of survey questions in all three languages prior to their use in data collection. The measures from the Resident Survey used in our analyses were all items obtained from existing national and state surveys.
Health Behaviors
Dietary Behavior
We assessed dietary patterns using the 14-item PrimeScreen questionnaire.26 In comparison with a 131-item semi-quantitative food frequency questionnaire (SFFQ), the PrimeScreen had a mean correlation coefficient of 0.70 for reproducibility and 0.61 for comparability with the SFFQ for foods and food groups.26 Participants were asked to recall their consumption during the past seven days. All dietary factors were calculated as servings per day except red meat, which was calculated as servings per week. Daily servings of fruits and vegetables was created by summing servings of: 100% orange or grapefruit juice; other 100% fruit juices; fruit, not counting juices; green salad; baked, boiled or mashed potatoes; and vegetables. Weekly servings of red meat was developed by combining consumption of beef, pork or lamb and processed meats. Daily servings of sugary snacks was created by combining servings of ice cream or sherbet with sugary snacks such as Pop Tarts, Twinkies, cake, and donuts. We used one item capturing daily servings of drinks with added sugar. Fast food intake was assessed using one item (servings of fast food meals from restaurants such as McDonald's, Wendy's, and Taco Bell).
In order to capture eating behavior across dietary indicators, we created a summary healthy eating index using a method previously published by Prochaska and colleagues27 and used in another study recently published examining multiple behavioral indicators.28 To create the healthy eating index we first calculated the standardized scores (Z-scores) for three diet measures: daily servings of fruits and vegetables; red meat; and junk food (sum of sugary drinks, snacks, and fast food).27 The Z-score for each diet measure was created by subtracting the daily servings from the mean and dividing the result by the standard deviation. Then the Z-scores of red meat and junk food were subtracted from the fruit and vegetable Z-score. This method resulted in a healthy eating index score, with a positive value indicating healthier eating. To facilitate interpretation of the healthy eating index, we categorized scores into three groups: Low, Medium and High, with higher scores indicating healthier eating. The Low score group was the lower 25th percentile, the Medium score group was the 25th -75th percentile and the High score group was the upper 75th percentile.
Sedentary Behavior
We asked two questions to capture total daily sitting at work and at home, both adapted from the International Physical Activity Questionnaire (IPAQ) long form.29 In a 12-country study of the reliability and validity of the IPAQ, the test-retest reliability for total sitting ranged between 0.74 – 0.89 (Spearman correlation) for the long form, ‘past 7-days’ format.28 Criterion validity for total sitting, as tested against an accelerometer, ranged from 0.25-0.51 (Spearman correlation) for the long form, ‘past 7-days’ format.29 Cut points to define High, Medium, and Low sedentary behavior were determined using percentiles. High sedentary behavior was defined as ≥ 7 hours of sitting per day (upper 75th percentile), while Medium was defined as 2-7 hours (25th- 75th percentile) and Low defined as 0-2 hours (lower 25th percentile).
Tobacco Use
Tobacco use was measured using questions from the NCI Tobacco Screener used in the Health Information National Trends Survey, 2005.30 While reliability and validity data were not reported specifically for the tobacco questions, the survey underwent significant testing prior to use.31 We calculated a two-category measure: current users and non-users/former users. Current users smoked at least 100 cigarettes in their lifetime and responded to being a current smoker of cigarettes, cigars, or pipes. Former users have smoked at least 100 cigarettes in their lifetime and are not current smokers of cigarettes, cigars, or pipes. Non-users have not smoked 100 cigarettes in their lifetime and are not current users of cigarettes, cigars, or pipes.
Sociodemographic Factors
Age, race/ethnicity, gender and education were measured using HINTS 2005 demographic questionnaire.30,31 Country born and language spoken were assessed using questions from the New Immigrant Survey.32 We defined language spoken using three categories: No English, English only, and English plus, the latter indicating that the participant spoke English plus at least one other language. We measured financial hardship with one question from the Women's Health and Aging Study asking, “In general, how do you find your household's finances usually work out at the end of the month?” Response options were: not enough to make ends meet, just enough to make ends meet, and some money left over.33
Analysis
While the amount of missing data on the Resident Survey were quite small, we used complete cases analysis because this method makes the fewest assumptions about the mechanisms of missing data except to assume that the data are missing at random. Logistic regression analyses were conducted to examine the association of healthy eating, sedentary behavior, and tobacco use with the sociodemographic factors. For tobacco use, a dichotomous outcome, we used logistic regression with a logit link function to model binary outcomes. For total sitting and the healthy eating index, both outcomes with three categories, we used a cumulative logit model to account for the ordinal nature of each measure. The proportional odds assumption was tested and satisfied in the ordinal logistic regression models. The ordinal outcomes were coded such that the regression modeled the probability of increased sedentary behavior (more hours spent sitting) and more healthy eating (higher score on healthy eating index). The clustering of participants within sites was controlled for as a fixed effect in all models.
In all multivariable models we examined the relationships between the behavioral outcomes and the following predictors: education, age, race/ethnicity, gender, country born, language spoken, and financial hardship. We selected this list of predictors based on two factors. First, we wanted to control for known sociodemographic factors (education, age, race/ethnicity, and gender) associated with our behavioral outcomes. Second, we wanted to examine the relationship of key sociodemographic factors (country born, language spoken, and financial hardship) relevant to our diverse sample. We did not include household income as a predictor in the models because the sample was inherently low-income with little variation in reported income.
For this type of examination of associations, the power of a test to detect an odds ratio as statistically significant depends on the level of the association, the prevalence of the outcome measure in the reference group, and the within development concordance of the measures (intra-cluster correlation, ICC). For a range of prevalence values, ICC's and subgroup sizes, this study had 80% power to detect as statistically significant odds ratios that were as low as 1.6.
RESULTS
A sample of 1937 households was selected from across the 20 sites, of which 1679 were eligible. Of these 1679, 828 residents (49.3%) completed the survey. The number of completed surveys ranged across sites from 18-64. Most participants had completed high school or beyond (62%); were less than 50 years of age (65%); and identified themselves as either Hispanic (41%) or non-Hispanic Black (38%) (Table 1). Most were female (80%) and foreign-born (68%). A majority reported some level of financial hardship, with more than one-third not being able to make ends meet each month. An examination of these sociodemographic factors by housing development shows that the sites varied (p<0.05) on all of these variables.
Table 1.
Sociodemographic characteristics of Health in Common study participants (n=828), 2007-2010
| Characteristic | n (%) |
|---|---|
| Education – | |
| Grade school or below (<8 yrs) | 152 (21%) |
| Some HS (9-11.5 yrs) | 123 (17%) |
| High School (12 yrs) | 200 (27%) |
| More than high school (13+ yrs) | 261 (35%) |
| Age – | |
| 18-29 | 153 (19%) |
| 30-39 | 218 (26%) |
| 40-49 | 169 (20%) |
| 50-59 | 145 (18%) |
| 60+ | 140 (17%) |
| Race/ethnicity – | |
| Hispanic | 341 (41%) |
| Non-Hispanic White | 93 (11%) |
| Non-Hispanic Black | 316 (38%) |
| Other | 74 (9%) |
| Gender – | |
| Male | 169 (20%) |
| Female | 659 (80%) |
| Country born – | |
| U.S. | 261 (32%) |
| Non-U.S. | 565 (68%) |
| Language spoken – | |
| No English | 249 (30%) |
| English only | 196 (24%) |
| English plus | 382 (46%) |
| Financial hardship – | |
| Not enough to make ends meet | 318 (39%) |
| Just enough | 360 (44%) |
| Some money left over | 136 (17%) |
| Dietary Factors – | |
| ≥ 5 daily servings fruits & vegetables | 63 (7.6%) |
| ≥ 5 weekly servings red meat | 153 (18.5%) |
| ≥ 5 weekly servings sugary drinks | 392 (47.5%) |
| ≥ 5 weekly servings sugary snacks | 171 (20.6%) |
| ≥ 5 weekly servings fast food | 24 (2.8%) |
Individual Health Behaviors
As a starting point for understanding the dietary factors (fruits and vegetables, red meat, sugary snacks and drinks, and fast food), we examined their prevalence (Table 1). About 92% of the sample was consuming less than five servings of fruits and vegetables per day and about 18% consumed five or more servings of red meat per week. While there is no set threshold for the appropriate number of weekly servings of sugary drinks and snacks or fast food, we found that about 48% of our sample consumed five or more servings of sugary drinks weekly, 20.6% consumed five or more servings of sugary snacks weekly, and about 3% consumed five or more servings of fast food weekly.
Our healthy eating index combined all of these dietary variables into one score, which was categorized into Low, Medium and High score groups. To facilitate interpretation of our healthy eating index, we also reported the mean daily servings of fruits and vegetables, red meat, and total junk food in the index across the Low, Medium, and High groups (Table 2). All means were shown to be significantly different from one another (p≤ 0.05). Higher scoring groups consumed more servings of fruits and vegetables and fewer servings of red meat and junk food than lower scoring groups.
Table 2.
Mean daily servings of each food group in the healthy eating index categories
| Healthy Eating Index Food Groups | Low Score ≤25th percentile (n=207) Mean daily servings (SE) | Medium Score 25th-75th percentile (n=414) Mean daily servings (SE) | High Score ≥75th percentile (n=207) Mean daily servings (SE) |
|---|---|---|---|
| Fruits and vegetables | 1.95 (0.09) servings | 2.30 (0.07) servings | 3.95 (0.09) servings |
| Red meat | 0.86 (0.03) servings | 0.33 (0.02) servings | 0.14 (0.03) servings |
| Total junk food (sugary drinks + sugary snacks + fast food) | 2.23 (0.05) servings | 1.17 (0.04) servings | 0.56 (0.05) servings |
We found that residents, on average, spent 4.8 hours sitting during the day (standard deviation=3.7; range 0-17 hours). We also examined the distribution of mean hours of sitting in each of the three sitting groups: Low, Medium and High. In the Low scoring group (≤ 25th percentile), mean daily sitting was 1.30 hours ± 0.7. In the Medium scoring group, mean daily sitting was 4.21 hours ± 1.2. In the High scoring group (≥ 75th percentile), mean daily sitting 10.0 hours ± 2.5. Approximately 21% of the participants were current tobacco users.
Multiple Health Behaviors
About half the sample (50.6%) reported behaviors that fell into one or more of the following risk categories: 1) the lowest category for healthy eating, 2) the highest category for total sitting, or 3) current tobacco use. Within this 50.6% of the sample, most (64.9%) reported only one of these risk categories, 28.6% reported two of the risk categories and 6.4% reported all three risk categories.
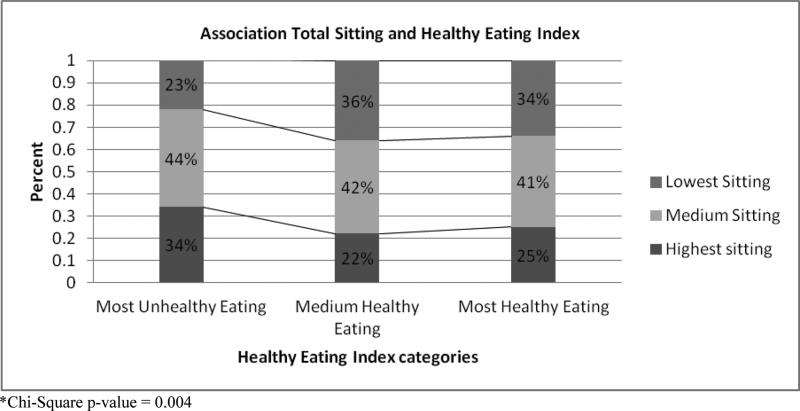
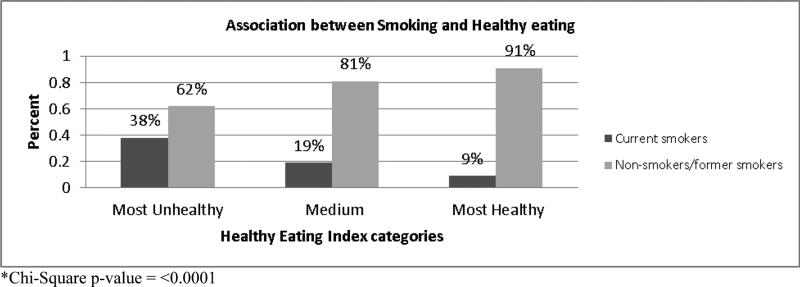
In terms of associations between health behaviors, current tobacco use was significantly associated with more hours of sitting (p=0.01). Current tobacco use was also significantly associated with the healthy eating index (p<0.0001), such that current smokers were more likely to report less healthy eating compared to non-smokers. Healthy eating and total sitting were also significantly associated (p=0.004), such that residents in the least healthy eating group reported higher amounts of sitting. Figures 1a-c present these relationships graphically.
Figure 1a.
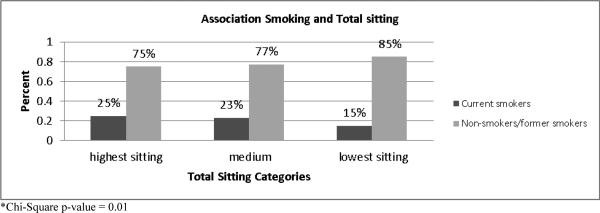
Associations between health behaviors-- total sitting and current tobacco use
Figure 1c.
Associations between health behaviors-- total sitting and healthy eating
Bivariate Relationships
Three of the sociodemographic factors (race, country born and language spoken) were significantly associated with all three health behaviors in the bivariate analyses (data not shown). Hispanic and Black residents were significantly more likely to report higher healthy eating scores, less sitting and were less likely to report current tobacco use. These relationships held for the “Other” race category for healthy eating and tobacco use. Across all three health behaviors, residents that were born in the U.S. reported significantly more risk than those born elsewhere (e.g., lower healthy eating scores, more sitting, and more likely to be a current tobacco user). Similarly, residents who reported speaking no English or English plus another language reported significantly less risk across all three behaviors (e.g., higher healthy eating scores, less sitting, and less likely to be a current tobacco user).
Multivariable Models
Significant Predictors across Health Behaviors
Based on the multivariable models, four sociodemographic variables (age, gender, language spoken, and financial hardship) showed significant relationships with all three health behaviors (Table 3). Age had a mixed relationship with the health behaviors. Generally younger people were less likely to report healthful eating than those aged 60-70+ years, with only those aged 18-29 years reaching significance (OR=0.34; 95% CI 0.20-0.61). For total sitting, younger people generally were likely to have reported less sitting than those aged 60-70+ years, with residents aged 40-49 and 50-59 years reaching significance (OR=0.44; 95% CI 0.26-0.75 and OR=0.51; 95% CI 0.30-0.86 respectively). For current tobacco use, younger residents were generally more likely to be current tobacco users than the 60-70+ year olds, with those aged 50-59 years reaching significance (OR=3.29; 95% CI 1.50-7.23).
Table 3.
Multivariate associations between sociodemographic factors and health behaviors, 2007-20101
| Healthy Eating Index1 | Total Sitting1 | Tobacco Use2 | ||||
|---|---|---|---|---|---|---|
| Predictors | OR (95%CI) | p | OR (95%CI) | p | OR (95%CI) | p |
| Education: | ||||||
| Grade school | 0.80(0.49-1.3) | 0.6600 | 0.66(0.40-1.07) | 0.007 | 0.88(0.40-1.91) | 0.41 |
| Some HS | 1.10(0.69-1.74) | 0.46(0.29-0.72) | 1.27(0.67-2.39) | |||
| HS | 0.93(0.63-1.37) | 0.66(0.45-0.96) | 0.74(0.43-1.29) | |||
| (ref: >HS) | 1.00 | 1.00 | 1.00 | |||
| Age : | ||||||
| 18-29 | 0.34(0.20-0.61) | <.0001 | 0.61(0.35-1.08) | 0.03 | 1.50(0.65-3.43) | 0.01 |
| 30-39 | 0.64(0.38-1.08) | 0.62(0.37-1.05) | 1.20(0.51-2.79) | |||
| 40-49 | 0.74(0.44-1.24) | 0.44(0.26-0.75) | 2.16(0.99-4.71) | |||
| 50-59 | 1.21(0.72-2.04) | 0.51(0.30-0.86) | 3.29(1.50-7.23) | |||
| (ref: 60-70+) | 1.00 | 1.00 | 1.00 | |||
| Race: | ||||||
| Hispanic | 1.10(0.58-2.11) | 0.3963 | 0.91(0.48-1.72) | 0.92 | 1.03(0.45-2.36) | 0.19 |
| Black | 1.51(0.83-2.77) | 1.06(0.58-1.92) | 0.53(0.26-1.11) | |||
| Other | 1.27(0.63-2.58) | 1.06(0.53-2.11) | 0.82(0.34-1.96) | |||
| (ref: White) | 1.00 | 1.00 | 1.00 | |||
| Gender: | ||||||
| Male | 0.65(0.44-0.94) | 0.0235 | 1.47(1.02-2.11) | 0.04 | 2.03(1.20-3.43) | 0.009 |
| (ref: Female) | 1.00 | 1.00 | 1.00 | |||
| Country Born: | ||||||
| U.S. | 0.79(0.50-1.27) | 0.3377 | 0.83(0.52-1.33) | 0.44 | 7.17(3.76-13.67) | <.0001 |
| (ref: Non-US) | 1.00 | 1.00 | 1.00 | |||
| Language Spoken : | ||||||
| English plus | 3.30(1.90-5.74) | 0.0001 | 0.40 (0.23-0.70) | 0.0002 | 0.60 (0.30-1.21) | 0.03 |
| No English | 2.78(1.44-5.38) | 0.24 (0.12-0.47) | 0.26 (0.10-0.70) | |||
| (ref: English Only) | 1.00 | 1.00 | 1.00 | |||
| Financial Hardship: | ||||||
| Some money left over | 1.75(1.11-2.75) | 1.79(1.15-2.77) | 0.29(0.15-0.55) | |||
| Just enough ends meet | 1.54(1.10-2.17) | 0.0154 | 1.39(0.99-1.95) | 0.03 | 0.40(0.24-0.65) | 0.0001 |
| (ref: Not enough) | 1.00 | 1.00 | 1.00 | |||
| Site3 | 0.0008 | 0.07 | 0.07 | |||
Logistic regression with site as a fixed effect and a cumulative logit for ordinal outcomes.
Logistic regression with site as a fixed effect and a logit link for binary outcomes.
Estimates to all sites are not shown.
Financial hardship exhibited a more consistent relationship with the health behaviors than age did. Those with some money left over at the end of the month were significantly more likely to report healthier eating (OR=1.75; 95% CI 1.11-2.75), more total sitting (OR=1.79; 95% CI 1.15-2.77) and no current tobacco use (OR=0.29; 95% CI 0.15-0.55) than those with not enough money to make ends meet. Those with just enough money to make ends meet were also significantly more likely to report healthier eating (OR=1.54; 95% CI 1.10-2.17) and no current tobacco use (OR=0.40; 95% CI 0.24-0.65) than those with not enough money to make ends meet, however, the relationship with more total sitting was not significant.
Gender and language spoken exhibited the most consistent relationships with the health behaviors. Men were significantly more likely to report less healthy eating (OR=0.65; 95% CI 0.44-0.94), more total sitting (OR=1.47; 95% CI 01.02-2.11), and were twice as likely to report current tobacco use (OR=2.03; 95% CI 1.20-3.43) as women. Speaking no English or at least one language in addition to English had a largely protective effect, with those residents significantly more likely to report healthier eating (p=0.0001), less sitting (p=0.0002), and lower odds of being a current smoker (p=0.03) than residents who spoke English only. Some of the effect estimates for language spoken were notable. For example, residents who spoke no English were almost three times more likely to have higher healthy eating scores (OR=2.78; 95% CI 1.44-5.38). They were also four times less likely to report higher levels of sitting (OR=0.24; 95% CI 0.12-0.47) and current tobacco use (OR=0.26; 95% CI 0.10-0.70).
Race was the only variable to exhibit a consistently non-significant relationship across the three health behaviors, despite its significant relationships in the bivariate analyses. In addition, housing site was significant for the healthy eating index (p=0.0008) and marginally significant for total sitting and tobacco use (p=0.07 for both).
DISCUSSION
We examined the relationship between selected sociodemographic factors and three health behaviors (diet, sedentary behavior, and tobacco use) in a diverse, low-income sample. While all study participants were low-income, they reported varying levels of financial hardship, which was a significant predictor across the health behaviors. People who had some money left over at the end of the month reported healthier lifestyles than those who did not have enough to make ends meet. Those who spoke no English, or at least one language in addition to English, also reported healthier lifestyles. Men reported significantly less healthy lifestyles than women. In contrast to our expectations and previous studies,7,34 the majority of participants reporting risk factors only reported one risk factor rather than a cluster of risk factors.
Compared to the general U.S. population, our sample consumed fewer fruits and vegetables,35 was less sedentary,36 and smoked at similar rates.1 For example, 7.6% of our sample met recommendations for fruit and vegetable consumption, while Blanck and colleagues report that 20.3% of men and 29.6% of women met recommendations for consuming five servings of fruits and vegetables per day.35 These findings emphasize the importance of developing effective strategies promoting healthy eating in low income communities that are relevant and achievable for families living with financial hardship. Our data also indicated that housing site was significantly associated with healthy eating. This suggests that variation in eating patterns was related, in part, to place. Therefore, the broader neighborhood context of food and transportation availability may be important considerations for intervention efforts.
Gender has not been fully integrated into health promotion frameworks, limiting our understanding of how gender influences health promotion and ultimately health.37 In our analyses, men were significantly less likely to participate in healthy behaviors than women. Further complicating our understanding of the relationship between gender and health promotion is the co-occurrence of financial hardship, which the majority of our participants experienced and our data shows also impacts participation in healthy behaviors. While gender differences in health behavior participation have been established previously,38,39 the consistent relationship across behaviors and sizeable effect-estimates from this data point to how critical men's health promotion efforts are in low-income communities.40
Increasingly, financial hardship is being used to explore the association between socioeconomic conditions, health behaviors and health.41-44 Financial hardship is believed to be a better measure of socioeconomic circumstances than the traditional measures of socioeconomic status (e.g., income and education). Different demands on economic resources, as well as disparate rates in the accumulation of assets across households, can result in variations in financial hardship.
Traditional measures, such as income, may not capture this heterogeneity.45-47 The significant relationship between financial hardship and all of the health behaviors in the present study illustrates the remarkably heterogeneous experience of an entirely low-income sample. By examining how monthly finances worked out, we found that within a low-income sample those with some money left at the end of the month or just enough to make ends meet were more likely to report healthier behaviors than those with not enough to make ends meet. While numerous studies have shown an income gradient related to health behavior participation,1-3 this study taps into a dimension of socioeconomic circumstances not captured by traditional measures of socioeconomic status. This finding supports the critical need for health-related services and programming for those struggling to make ends meet each month and emphasizes that “...economic policy is public health policy (p 818).48”
Language spoken had a protective effect across the health behaviors for those residents who reported speaking no English or English plus another language. This finding confirms previous work with native Spanish speakers.23,49 Thinking of language spoken as one of many potential factors related to acculturation, this finding illustrates that communities of immigrants may retain elements of a healthier lifestyle compared with their English-only speaking counterparts. In terms of programming implications, intervention program goals should aim to be contextually relevant to the immigration history of the target communities. For example, relevant program goals might be preventing deterioration of health behavior participation such as maintaining low fast food consumption or not adopting tobacco use. An asset-based approach might be particularly relevant in housing developments with substantial proportions of immigrant residents.
Limitations
While these data contribute useful findings about the nuances of health behavior patterns and predictors within a low-income sample, certain limitations should be considered. It is noteworthy that race/ethnicity was not associated with any of the health behaviors in the multivariable analyses. One hypothesis regarding this finding is that income and financial hardship were the driving factors related to health behaviors in this sample. In terms of race/ethnicity, this sample was comprised of heterogeneous African-origin and Latino groups. For example, our sample included both African Americans and Haitian immigrants, both of whom were categorized in our data as non-Hispanic Black in terms of race. The sample also included Latinos from multiple countries of origin, all of whom who were categorized as Hispanic. It is possible that the daily lived experience within these heterogeneous groups is qualitatively different and that grouping them together into non-Hispanic Black and Hispanic dilutes the information contained in that variable.
Though we acknowledge that our response rate leaves open the possibility of selection bias, there is substantial value in engaging an understudied, hard-to-reach population at risk for income-related health disparities in a comprehensive examination of patterns and predictors of health behaviors. Our survey data relies on self-report, which may be subject to social desirability and recall biases in varying degrees. Because our survey did not cover sensitive topics, was administered by trained project staff, and utilized valid and reliable outcome measures, the self-reported nature of the data collection was not likely to significantly decrease the quality of the data. While each of our survey tools had been used previously in large surveillance studies, not all of them had published reliability and validity data. Additionally, our sample was over-represented by female participants, which may be a function of women being home more often during data collection hours and/or a predominance of female-headed households. Finally, more comprehensive dietary measurement would have allowed for calculation of relative contributions of the different dietary factors to overall caloric consumption. This added information would have been useful in comparing findings across previous studies and compiling a more nuanced description of participants’ diets, however, such dietary data collection was not feasible in a study of this scale. Our study endeavored to advance the science of health promotion by collecting a broad spectrum of multi-level data from a racially and ethnically diverse sample of more than 800 participants residing in low-income housing developments.
Conclusions
With the persistence of poverty rates in the U.S., low-income housing developments—with their tenant leadership, communication modalities, and community spaces—represent both a safety net and an important intervention setting. Our data showed that both protective factors and risk factors exist among the diverse residents of low income housing developments. A critical next step is developing effective health promotion interventions in low-income housing developments that leverage protective factors while considering those factors that put residents at higher risk. For example, future intervention research could explore strategies that help residents achieve desired domains of acculturation (e.g., English language skills) while retaining potentially protective cultural practices (e.g., eating habits, culinary skills), perhaps by convening multi-cultural groups of residents who could learn from one another. Another area for future study would be to examine the infrastructure (e.g., geographically defined community, available community spaces) and administrative strengths and constraints of public housing to learn effective methods of delivering interventions in this setting. Specific issues to examine include options for ownership of program administration, feasibility of involving tenant leadership in project design and implementation, and potential for housing authority- and housing development-level policy changes. Finally, it would be important to explore food buying practices and their relationship to diet quality with the purpose of developing intervention strategies specific to food access in a neighborhood and the related availability of public transportation. Delivering successful interventions to the 1.2 million households living in low-income housing developments has the potential to reduce income-related health disparities and prevent disease in these concentrated resource-deprived neighborhoods.
SO WHAT?
What is already known on this topic?
Although research shows income-related disparities in health behavior participation, there is insufficient examination of patterns and predictors of health behavior participation among residents of low-income housing developments.
What does this article add?
This study contributes to the literature by examining a large, diverse sample of residents of low-income housing developments across three health behaviors critical to chronic disease prevention: diet, inactivity, and tobacco use. Contrary to literature showing clustering of health behaviors, most residents reported a level of risk for only one health behavior. Financial hardship (more nuanced than income) and speaking a language other than English were predictive of participating in healthier behaviors.
What are the implications for health promotion practice or research?
Effective health promotion interventions in low-income housing developments that leverage protective factors while addressing risk factors have the potential to reduce income-related health disparities in these concentrated resource-deprived neighborhoods.
Figure 1b.
Associations between health behaviors—healthy eating and current tobacco use
Acknowledgments
This research was supported by the National Cancer Institute (R01 CA111310-01A1) and the NIH/NCI Harvard Education Program in Cancer Prevention and Control (R25 CA057713 to Glorian Sorensen, PhD). The authors would like to thank the 20 low-income housing sites that participated in this research, as well as the Cambridge, Somerville, and Chelsea Public Housing Authorities for their assistance. The authors also thank the administrative and field staff at the Harvard School of Public Health and Dana-Farber Cancer Institute and the study participants for their contributions to this project.
Footnotes
Indexing Key Words:
Manuscript format: research
Research purpose: modeling/relationship testing
Study design: non-experimental
Outcome measure: behavioral
Setting: local community
Health focus: fitness/physical activity, nutrition, and smoking control
Strategy: N/A
Target population age: adults
Target population circumstances: education/income level, geographic location, and race/ ethnicity
Contributor Information
Amy E. Harley, Joseph J. Zilber School of Public Health, University of Wisconsin-Milwaukee..
May Yang, New England Research Institutes, Inc., Watertown, MA.
Anne M. Stoddard, New England Research Institutes, Inc., Watertown, MA.
Gary Adamkiewicz, Harvard School of Public Health, Boston, MA.
Renee Walker, Joseph J. Zilber School of Public Health, University of Wisconsin-Milwaukee..
Reginald D. Tucker-Seeley, Harvard School of Public Health and the Dana-Farber Cancer Institute, Boston, MA.
Jennifer D. Allen, Dana-Farber Cancer Institute.
Glorian Sorensen, Harvard School of Public Health and the Dana-Farber Cancer Institute, Boston, MA.
References
- 1.Centers for Disease Control and Prevention (CDC) [September 28, 2012];Adult Cigarette Smoking in the United States: Current Estimate. 2012 Available at: http://www.cdc.gov/tobacco/data_statistics/fact_sheets/adult_data/cig_smoking/index.htm.
- 2.Reeves RJ, Rafferty AP. Healthy lifestyle characteristics among adults in the United States, 2000. Arch Intern Med. 2005;165:854–857. doi: 10.1001/archinte.165.8.854. [DOI] [PubMed] [Google Scholar]
- 3.Siahpush M, Borland R, Scollo M. Smoking and financial stress. Tob Control. 2003;12(1):60–66. doi: 10.1136/tc.12.1.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marmot M, Shipley M, Brunner E, Hemingway H. Relative contribution of early life and adult socioeconomic factors to adult morbidity in the Whitehall II study. J Epidemiol Community Health. 2001;55:301–307. doi: 10.1136/jech.55.5.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wong MD, Shapiro MF, Boscardin WJ, Ettner SL. Contribution of major diseases to disparities in mortality. N Engl J Med. 2002;347:585–1592. doi: 10.1056/NEJMsa012979. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention (CDC) Prevalence of Fruit and Vegetable Consumption and Physical Activity by Race/Ethnicity --- United States, 2005. MMWR Morb Mortal Wkly Rep. 2007;56(13):301–304. [PubMed] [Google Scholar]
- 7.Vandelanotte C, Reeves MM, Brug J, De Bourdeaudhuij I. A randomized trial of sequential and simultaneous multiple behavior change interventions for physical activity and fat intake. Prev Med. 2008;46:232–237. doi: 10.1016/j.ypmed.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 8.Harley A, Devine C, Beard B, Stoddard A, Sorensen G, Hunt M. Multiple health behavior change in a cancer prevention intervention for construction laborers. Prev Chronic Dis. 2010;7(3) [PMC free article] [PubMed] [Google Scholar]
- 9.de Vries H, van't Reit J, Spigt M, et al. Clusters of lifestyle behaviors: Results from the Dutch SMILE study. Prev Med. 2008;46:203–208. doi: 10.1016/j.ypmed.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 10.Morabia A, Constanza MC. Piling up healthy behaviors. Prev Med. 2012;55:161–162. doi: 10.1016/j.ypmed.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 11.Wiggers J, Radvan D, Clover K, Hazell T, Alexander J, Considine R. Public housing, public health: Health needs of public housing tenants. Aust N Z J Public Health. 2001;25:111–4. doi: 10.1111/j.1753-6405.2001.tb01830.x. [DOI] [PubMed] [Google Scholar]
- 12.Ahluwalia JS, Hollen N, Kaur H, James AS, Mayo MS, Resinicow K. Pathways to Health: Cluster-randomized trial to increase fruit and vegetable consumption among smokers in public housing. Health Psychol. 2007;26(2):214–221. doi: 10.1037/0278-6133.26.2.214. [DOI] [PubMed] [Google Scholar]
- 13.U.S. Department of Housing and Urban Development (HUD) [October 15, 2012];HUD's Public Housing Program. 2012 Available at: http://portal.hud.gov/hudportal/HUD?src=/topics/rental_assistance/phprog.
- 14.Shelton RC, McNeill LH, Puleo E, Wolin KY, Emmons KM. The association between social factors and physical activity among low-income adults living in public housing. Am J Public Health. 2011;101:2102–2110. doi: 10.2105/AJPH.2010.196030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heinrich KM, Lee RE, Suminski RR, et al. Associations between the built environment and physical activity in public housing residents. Int J Behav Nutr Phys Act. 2007;4:56. doi: 10.1186/1479-5868-4-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bennett GG, Wolin KY, Puleo E, Emmons KM. Pedometer-determined physical activity among multiethnic low-income housing residents. Med Sci Sports Exerc. 2006;38(4):768–773. doi: 10.1249/01.mss.0000210200.87328.3f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shankar S, Klassen AC, Garrett-Mayer E, et al. Evaluation of a nutrition education intervention for women residents of Washington, DC, public housing communities. Health Educ Res. 2007;22(3):425–437. doi: 10.1093/her/cyl092. [DOI] [PubMed] [Google Scholar]
- 18.Klassen AC, Smith KC, Black MM, Caulfield LE. Mixed method approaches to understanding cancer-related dietary risk reduction among public housing residents. J Urban Health. 2009;86(4):624–640. doi: 10.1007/s11524-009-9352-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Crump SR, Taylor BD, Sung JFC, et al. Dietary intake to reduce cancer risk among African American women in public housing: Do sociodemographic factors make a difference? Ethn Dis. 2006;16:963–970. [PubMed] [Google Scholar]
- 20.Eugeni ML, Baxter M, Scherezade KM, et al. Disconnections of African American public housing residents: Connections to physical activity, dietary habits and obesity. Am J Community Psychol. 2011;47(3-4):264–76. doi: 10.1007/s10464-010-9402-1. [DOI] [PubMed] [Google Scholar]
- 21.Heinrich KM, Lee RE, Regan GR, et al. How does the built environment relate to body mass index and obesity prevalence among public housing residents? Am J Health Promot. 2008;22(3):187–194. doi: 10.4278/ajhp.22.3.187. [DOI] [PubMed] [Google Scholar]
- 22.Berrigan D, Dodd K, Troiano RP, Reeve BB, Ballard-Barbash R. Physical activity and acculturation among adult Hispanics in the United States. Res Q Exerc Sport. 2006;77(2):147–57. doi: 10.1080/02701367.2006.10599349. [DOI] [PubMed] [Google Scholar]
- 23.Neuhouser ML, Thompson B, Coronado G, Solomon CC. Higher fat intakes and lower fruit and vegetables intakes are associated with greater acculturation among Mexicans living in Washington State. J Am Diet Assoc. 2004;104:51–57. doi: 10.1016/j.jada.2003.10.015. [DOI] [PubMed] [Google Scholar]
- 24.Kish J. Survey Sampling. Wiley & Sons, Inc; New York: 1965. [Google Scholar]
- 25.Carbone ET, Campbell MK, Honess-Morreale L. Use of cognitive interview techniques in the development of nutrition surveys and interactive nutrition messages for low-income populations. J Am Diet Assoc. 2002;102(5):690–696. doi: 10.1016/s0002-8223(02)90156-2. [DOI] [PubMed] [Google Scholar]
- 26.Rifas-Shiman SL, Willett WC, Lobb R, Kotch J, Dart C, Gillman MW. PrimeScreen, a brief dietary screening tool: reproducibility and comparability with both a longer food frequency questionnaire and biomarkers. Public Health Nutr. 2001;4(2):249–54. doi: 10.1079/phn200061. [DOI] [PubMed] [Google Scholar]
- 27.Prochaska JJ, Velicer WF, Nigg CR, Prochaska JO. Methods of quantifying change in multiple risk factor interventions. Prev Med. 2008;46:260–265. doi: 10.1016/j.ypmed.2007.07.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Drake BF, Quintiliani LM, Sapp A, Li Y, Harley AE, Emmons KM, Sorensen G. A comparison of strategies for assessing multiple health behavior change outcomes in behavioral intervention studies. Behav Med Pract Policy Res. 2013;3(1):114–121. doi: 10.1007/s13142-013-0195-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, Pratt M, Ekelund U, Yngve A, Sallis JF, Oja P. International Physical Activity Questionnaire: 12-Country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 30.National Cancer Institute (NCI) [October 15, 2012];Health Information National Trends Survey (HINTS) 2005 Available at: http://hints.cancer.gov/docs/HINTS_2005_main_study_instrument_eng.pdf.
- 31.Cantor D, Covell J, Davis T, Park I, Rizzo L. Health Information National Trends Survey 2005 (HINTS 2005) Final Report. Weststat; Rockville, MD.: [October 15, 2012]. Available at: http://hints.cancer.gov/docs/HINTS_2005_Final_Report.pdf. [Google Scholar]
- 32.Jasso G, Massey DS, Rosenzweig MR, Smith JP. Migration Information Source. Migration Policy Institute; Washington, DC: [October 15, 2012]. The New Immigrant Survey in the US: The experience over time, 2003. Available at: http://www.migrationinformation.org/Feature/display.cfm?ID=81. [Google Scholar]
- 33.Guralnik JM, Fried LP, Simonsick EM, Kasper JD, Lafferty ME. The Women's Health and Aging Study. DHHS Publication; Washington, DC: 1995. NIH 95-4009. [Google Scholar]
- 34.Schuit AJ, Van Loon AJM, Tijhuis M, Ocke MC. Clustering of lifestyle risk factors in a general adult population. Prev Med. 2002;35(3):219–224. doi: 10.1006/pmed.2002.1064. [DOI] [PubMed] [Google Scholar]
- 35.Blanck HM, Gillespie C, Kimmons JE, Seymour JD, Serdula MK. Trends in fruit and vegetable consumption among U.S. men and women, 1994–2005. Prev Chronic Dis. 2008;5(2) [PMC free article] [PubMed] [Google Scholar]
- 36.Healy GN, Matthews CE, Dunstan DW, Winkler EAH, Owen N. Sedentary time and cardio-metabolic biomarkers in US adults: NHANES 2003–06. Eur Heart J. 2011;32(5):590–597. doi: 10.1093/eurheartj/ehq451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gelb K, Pederson A, Greaves L. How have health promotion frameworks considered gender? Health Promot Int. 2011;27(4):445–452. doi: 10.1093/heapro/dar087. [DOI] [PubMed] [Google Scholar]
- 38.Liang W, Shediac-Rizkallah MC, Celentano DD, Rohde C. A population-based study of age and gender differences in patterns of health-related behaviors. Am J Prev Med. 1999;17(1):8–17. doi: 10.1016/s0749-3797(99)00040-9. [DOI] [PubMed] [Google Scholar]
- 39.Hasson H, Brown C, Hasson D. Factors associated with high use of a workplace web-based stress management program in a randomized controlled intervention study. Health Educ Res. 2010;25(4):596–607. doi: 10.1093/her/cyq005. [DOI] [PubMed] [Google Scholar]
- 40.Jeanfreau SG. Is anyone promoting the health of men? Am J Mens Health. 2011;5(4):285. doi: 10.1177/1557988311408586. [DOI] [PubMed] [Google Scholar]
- 41.Tucker-Seeley RD, Li Y, Subramanian SV, Sorensen G. Financial hardship and mortality among older adults using the 1996-2004 Health and Retirement Study. Ann Epidemiol. 2009;19:850–857. doi: 10.1016/j.annepidem.2009.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ahnquist J, Fredlund P, Wamala SP. Is cumulative exposure to economic hardships more hazardous to women's health than men's? A 16-year follow-up study of the Swedish Survey of Living Conditions. J Epidemiol Community Health. 2007;61(4):331–336. doi: 10.1136/jech.2006.049395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kahn JR, Pearlin LI. Financial strain over the life course and health among older adults. J Health Soc Behav. 2006;47(1):17–31. doi: 10.1177/002214650604700102. [DOI] [PubMed] [Google Scholar]
- 44.Siahpush M, Spittal M, Singh GK. Smoking cessation and financial stress. J Public Health. 2007;29(4):338–342. doi: 10.1093/pubmed/fdm070. [DOI] [PubMed] [Google Scholar]
- 45.Perry B. The mismatch between income measures and direct outcome measures of poverty. Social Policy Journal of New Zealand. 2002;19:101–127. [Google Scholar]
- 46.Beverly SG. Measures of material hardship: Rationale and recommendations. J Poverty. 2001;5(1):23–41. [Google Scholar]
- 47.Lynch J, Kaplan G. Socioeconomic Position. In: Berkman LF, Kawachi I, editors. Social Epidemiology. England Oxford University Press; Oxford: 2000. pp. 13–35. [Google Scholar]
- 48.Lynch J, Kaplan GA, Salonen JT. Why do poor people behave poorly? Variation in adult health behaviors and psychosocial characteristics by stages of the socioeconomic lifecourse. Soc Sci Med. 1997;44(6):809–819. doi: 10.1016/s0277-9536(96)00191-8. [DOI] [PubMed] [Google Scholar]
- 49.Montez JK, Eschbach K. Country of birth and language are uniquely associated with intakes of fat, fiber, and fruits and vegetables among Mexican-American women in the United States. J Am Diet Assoc. 2008;108:473–480. doi: 10.1016/j.jada.2007.12.008. [DOI] [PubMed] [Google Scholar]