Abstract
Purpose
Although functional outcomes following reconstruction for congenital hand differences are frequently described, much less is known regarding children’s ability to cope with psychosocial effects of these conditions. We qualitatively explored stress and coping mechanisms among children following reconstructive surgery for congenital hand differences.
Methods
Forty patients and their parents participated in semi-structured interviews examining stress related to hand functioning and appearance, emotional responses to stress, and coping strategies. Interviews were audio-taped, transcribed, and analyzed thematically. A consensus taxonomy for classifying content evolved from comparisons of coding by two reviewers. Themes expressed by participants were studied for patterns of connection and grouped into broader categories.
Results
In this sample, 58% of children and 40% of parents reported stress related to congenital hand differences, attributed to functional deficits (61%), hand appearance (27%), social interactions (58%), and emotional reactions (46%). Among the 18 children who reported stress, 43% of parents were not aware of the presence of stress. Eight coping strategies emerged, including humor (12%), self-acceptance (21%), avoidance (27%), seeking external support (30%), concealment (30%), educating others (9%), support programs (21%) and religion (24%).
Conclusions
Although children with congenital hand differences often experience emotional stress related to functional limitations and aesthetic deformities, many apply positive coping mechanisms that enhance self-esteem and self-esteem. Clinicians caring for children with congenital hand differences should inform families about potential sources of stress in order to direct resources toward strengthening coping strategies and support systems.
Level of Evidence
Level IV-Case series
Keywords: Congenital Hand Differences, Hand Surgery, Coping, Psychosocial Outcomes, Qualitative Research
Introduction
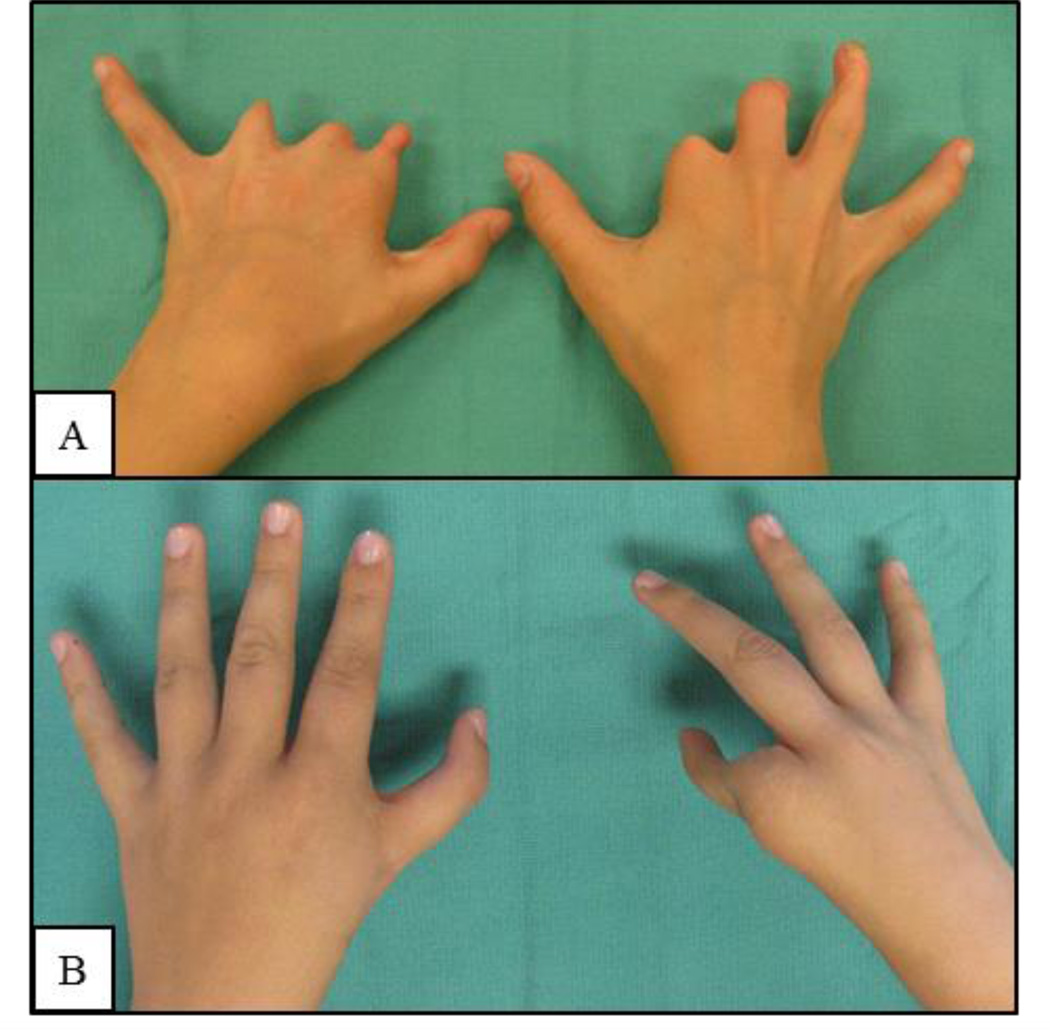
Over 2,000 children are born with congenital hand differences in the United States each year, which result in lifelong functional impairment and aesthetic deformities.1,2 Although reconstructive surgery is typically undertaken at an early age, many children experience lasting disability and aesthetic deformity (Figure 1).3 These aesthetic and functional differences can hinder children’s psychosocial functioning throughout life by causing social anxiety and depression.4,5 Hands are one of the most noticed parts of the body second only to the face, and are essential for daily tasks and interactions with other people and the environment, making them difficult to conceal.3,6 Although many studies have focused on functional outcomes following reconstruction, much less is known regarding the social and emotional outcomes of congenital hand differences.3,5,7
Figure 1.
Common Congenital Hand Differences. A) 10 year-old girl with bilateral amniotic band syndrome. B) 17 year-old girl with right hypoplastic thumb and left thumb clinodactyly.
For many congenital conditions, such as cleft lip and palate or craniofacial anomalies, visible deformities have been linked to anxiety, poor self-perceptions, and stigma as early as elementary school; these emotional responses can result in chronic stress that persists into adulthood. 5,7–9 Stress manifests when individuals perceive interactions with their environment as threatening to their well-being, and greater than they can manage using the resources at their disposal.10 Coping describes the process of managing stress both externally, from the relationship between individuals and their environment, as well as internally from the emotional responses they create.10 For example, young adults with cleft lip and palate experience stress from poor peer relationships and difficulty with social interactions. Receiving recognition from significant others can help these patients cope with stress and combat the resulting low self-esteem.9,11 Certain coping mechanisms and resources, such as social support from parents or peers, can mediate consequences of stress and improve children’s psychosocial adjustment and self-concept.3,12,13 Despite indications from related disciplines that visible differences resulting from congenital anomalies can cause social and emotional problems that are best managed with particular methods of coping, these aspects of congenital hand patient outcomes have not been systematically explored.
Understanding sources of stress and coping mechanisms among children with congenital hand differences can provide important insight for parents and clinicians caring for these patients. For example, identifying specific stressors can allow caregivers to target treatment plans and resources towards those issues that are most relevant to children with congenital hand differences, and potentially improve their social and emotional development throughout childhood. To examine this, we studied a cohort of patients ages six and older with congenital hand differences and their parents using a qualitative approach to determine sources of stress and common coping strategies employed by children and their families.
Materials and Methods
Study Design and Patient Sample
Qualitative methods can provide rich insight into complex social and emotional issues that support evidence-based medicine.14 Rather than relying on large statistical samples, qualitative research gains validity through the purposeful selection of individuals with characteristics of interest and in-depth analysis of their experiences.14–16 In this qualitative study, we performed semi-structured interviews with 33 patients with congenital hand differences, ages 6 to 17 years, and their parents (N=40). Patients were selected using purposive sampling to obtain a diverse group of individuals with characteristics that were germane to our study purpose.17 All patients had previously undergone reconstruction for a congenital hand difference at the University of Michigan. We excluded children with cognitive impairment that prevented them from participating in the interviews. Patient recruitment, interviewing, and data analysis were carried out simultaneously. Thematic saturation occurred after analysis of 25 transcripts. However, because this was part of a larger mixed-methods project we continued to recruit patients beyond the point of saturation, resulting in a sample of 33 patients and 40 parents. The University of Michigan Institutional Review Board approved all aspects of this study.
Qualitative Methods
Patient and parent interviews and subsequent transcript review followed grounded theory methodology, in which participants’ experiences, thoughts, and feelings were explored to generate relevant theories through iterative, inductive analysis of their transcribed responses. 14,18,19 Rather than testing a priori hypotheses, grounded theory seeks to explore, understand, and describe phenomena as they are perceived by participants without preconceived ideas from investigators.20 Therefore, we approached this study without assumptions and allowed themes and concepts to emerge from a multiphasic coding process.
Three investigators (LF, KN, JW) conducted in-person, audio-recorded interviews of each patient and his/her parent(s). The interviewers were previously unknown to the participants and were not involved in children’s clinical care. Interviews began in an open-ended fashion. The interviewers used targeted questions to explore specific psychosocial problems that caused stress and negative emotional responses to understand how children coped with these challenges. Interview topics included children’s hand function, daily activities at home and school, hand aesthetics, and social interactions.
Analysis
The audio-recorded interviews were transcribed verbatim before being analyzed. Three research staff (AC, LF, JW) completed the coding process independently to reduce biased interpretation.14 During the initial open coding phase, two coders reviewed each transcript to identify and label themes with codes. Codes either came directly from the text or were created by the readers to describe the concepts expressed by participants. 18,19 For example, the following excerpt from a patient’s interview, “when I'm in public I usually cover [my hand] up or hide it in my sleeve because I’m tired of questions,” was coded as “hiding hands.” Coding was compared between reviewers in order to resolve discrepancies and ensure accuracy. Axial coding, a process of relating codes and organizing them into a codebook, took place concurrently. 21 The readers created broad categories of similar codes and further subdivided codes into sub-codes as needed. The codebook was refined by review of the transcripts among investigators and tested on a subset of the data to determine inter-rater reliability. Inconsistencies in the application of the codes were brought to the principal investigator who modified the codebook as needed to increase the specificity of codes. This process was repeated until the coding agreement was greater than 80%. The two reviewers then completed selective coding using the finalized codebook to determine the prevalence of themes in the data, create and refine theories, and select quotations that reflect key concepts.
Results
In our sample of 33 patients, the average child age was 11.4 years, 39% were female, and 39% had bilateral hand involvement (Table 1). Additionally, 45% were school age (ages 6–10) and 55% were adolescents (ages 11–17). We included patients with the following types of congenital hand differences: syndactyly (24%), thumb duplication (24%), thumb hypoplasia (18%), amniotic band syndrome (15%), radial deficiency (9%), ulnar deficiency (3%), complex polydactyly (3%), and cleft hand (3%). Of the 40 parents participated, 63% were biological mothers, 18% were biological fathers, 15% were adoptive parents, and 5% were other family members. Overall, interviews averaged 46 minutes in duration (range, 19 to 71 minutes). From the analysis of these interviews using grounded theory methodology, 10 codes and 21 subcodes emerged within two broad categories: stress and coping mechanisms.
Table 1.
Characteristics of Participating Children (N=33)
| Age (mean ± SD) | 11.4±3.9 | |
|---|---|---|
| Children (ages 6–10) | 45% | |
| Adolescents (ages 11–17) | 55% | |
| Age in years at first hand surgery (mean ± SD) | 1.9±1.3 | |
| Sex | ||
| Boys | 60% | |
| Girls | 40% | |
| Affected side | ||
| Bilateral | 33% | |
| Unilateral: dominant hand | 15% | |
| Unilateral: non-dominant hand | 52% | |
| Primary Diagnosis | ||
| Duplicated thumb | 24% | |
| Hypoplastic or absent thumb | 18% | |
| Syndactyly: simple | 18% | |
| Amniotic band syndrome | 15% | |
| Radial deficiency | 9% | |
| Syndactyly: complex | 6% | |
| Polydactyly | 3% | |
| Ulnar hypoplasia | 3% | |
| Cleft hand | 3% | |
| Comorbidities and syndromes | ||
| Congenital difference of lower limb | 24% | |
| VACTERL association | 12% | |
| Congenital heart condition | 6% | |
| Hydrocephaly | 6% | |
| TAR syndrome | 3% | |
| Poland’s syndrome | 3% | |
| Duane’s syndrome | 3% | |
| Cleft palate | 3% | |
VACTERL = Vertebral abnormalities, Anal atresia, Cardiac anomalies, Tracheoesophageal fistula, Renal anomalies, Limb defects; TAR = Thrombocytopenia-absent radius
Stress
Stress has been defined by the American Psychological Association as emotional discomfort accompanied by behavioral changes due to the perception that their environmental demands exceed their adaptive capacity. 22 Using this definition, 19 children (58%) and 13 parents (39%) reported experiencing stress related to congenital hand differences. Overall, the agreement between children and parents regarding the occurrence of stress related to a congenital hand difference was 64%, (kappa statistic= 0.29, p<0.03). Disagreement occurred most frequently among 9 children who expressed feeling stressed, but their parent did not. (Table 2) Age and gender was not significantly correlated with reporting stress. (Table 3) However, parents of children with bilateral congenital hand differences were significantly more likely to report that their child experienced stress compared with parents of children with unilateral congenital hand differences (64% vs. 28%, p<0.04).
Table 2.
Agreement between parents and children with congenital hand differences regarding stress
| Parents | |||
|---|---|---|---|
| Stress | No stress | ||
| Children | Stress | 9 | 9 |
| No stress | 3 | 12 | |
Table 3.
Patient characteristics correlated with stress among children with congenital hand differences
| Child-reported | Parent-reported | ||||||
|---|---|---|---|---|---|---|---|
| Stress | No stress | p value | Stress | No stress | p value | ||
| Age | ≤ 10 years (school age) | 9 (60%) | 6 (40%) | 0.80 | 7 (47%) | 8 (53%) | 0.44 |
| > 10 years (adolescent | 10 (56%) | 8 (44%) | 6 (33%) | 12 (67%) | |||
| Gender | Male | 10 (50%) | 10 (50%) | 0.28 | 8 (40%) | 12 (60%) | 0.93 |
| Female | 9 (69%) | 4 (31%) | 5 (39%) | 8 (62%) | |||
| Affected hand | Bilateral | 7 (64%) | 4 (36%) | 0.62 | 7 (64%) | 4 (36%) | 0.04 |
| Unilateral | 12 (55%) | 10 (46%) | 6 (27%) | 16 (73%) | |||
Stress among children with congenital hand differences and their parents was driven by both internal (self-perception) and external (e.g. peer interactions) factors organized into the following code categories: (1) functional deficits, (2) aesthetic appearance, (3) social interactions, and (4) emotional reactions. Representative quotations from each category are detailed in Table 5.
Table 5.
Representative Quotations from Qualitative Interviews
| Stress | Functional limitations | “She has the hardest time opening packages of things…” - Mother of an 11 yo girl with congenital amputation and symbrachytactyly |
| “…She had difficulties buttoning and zipping and tying her shoelaces” - Mother of 17 yo female with thumb hypoplasia | ||
| Aesthetic Appearance | “I get these little baby hairs…on my hand. I don’t know why, but they bother me.” -16 yo female with complex syndactytly |
|
| Social | “The people looking [at my hand], they say ‘Ewww’ and then they're not gonna be by me or sometimes they tell other people.” –8-year-old boy with polydactyly |
|
| Emotional stress | “Because I’m not like the other kids…I’m self-conscious about my hand…[People ask me] why is my hand not like their hand, which is horrible.” – 16-year-old girl with thumb hypoplasia |
|
| “We were doing this game…where you have to reach out and grab someone’s hand…and the girl who I was holding her hand…took her hand off mine and said ‘Ew!’ and then…grabbed someone else’s [hand] so she didn’t have to hold mine. So I was really insulted.” – 16-year-old girl with complex syndactyly | ||
| Coping | Humor | “I joke around about it. People have said that I can swim faster because I have the little webbing there, I don’t really worry about it that much.” – 15-year-old boy with simple syndactyly |
| Self-acceptance | “It looks different, but I don’t care…I think I’m just fine.” – 10 year-old girl with thumb duplication |
|
| “I’ve lived with them so long it just a part of me…so no reason to change them now.” - 16 yo female with bilateral cleft hands | ||
| Avoidance | “I sometimes ignore them [when they say something mean] or just tell a teacher.” - 8 yo female with bilateral complex ulnar polydactyly |
|
| Seeking support | “Grandpa has four fingers on one hand and…[he] has always said that his hand is like Grandpa’s hand…He talks about his connection because him and Grandpa are alike…and look at all the things that Grandpa has been able to do.” - Parent of 7-year-old boy with radial deficiency |
|
| “Sometimes I get sad…what kind of boy would want a girlfriend with 7 fingers? …And then my mom says there’s that one person out there that’s meant for you and they’ll love everything about you. So then I think about that…if my family can love me with my 7 fingers then someone else will.” -16 yo girl with complex syndactyly | ||
| Hiding hands | “In public I usually cover it up or hide it in my sleeve because I’m tired of questions…Usually [my mom] tells me when kids are bothering you to not let it get to your head and stuff.” – 11-year-old girl with amniotic band syndrome |
|
| “I wear fingerless gloves though. I wear those all year.. so people don’t see it. It’s not like I hate it but it’s not like something I’m proud of.” - 16 yo girl with bilateral cleft hands | ||
| Educating others | “When I was younger…my mom used to come in and she would talk to my class about it…for me” -16 yo girl with complex syndactyly |
|
| Support programs | His attitude changed greatly after coming back from the summer camp]…he realized how lucky he was. Because there were…kids that had more severe disabilities and he was actually the helper. -Parent of 16 yo male with bilateral cleft hands |
|
| Religion | “I figure that [he] was made special for a reason…I think God has something pretty special intended for him because he wanted him to be noticed and he sure is.” -Parent of 16 yo male with bilateral cleft hands |
|
| “We used to say, “when you were born, God glued, you know you fingers were glued together.” -Parent of 17 yo male with simple syndactyly |
Functional Deficits
In our sample, 20 (61%) of families reported stress due to functional disability. The most common daily tasks cited as inciting stress included clothes (e.g. buttons, zippers) (58%), household chores (e.g. opening jars, door handles), writing (30%), and difficulty with sports (30%). Children with duplicated thumbs (n=5), hypoplastic thumbs (n=4), and radial deficiency (n=4) most commonly reported stress caused by functional difficulties compared to those with other diagnoses.
Aesthetic Differences
Hand appearance was a source of stress for 9 (27%) children, who were troubled by deviation of the finger (21%), scarring (19%), and abnormal hair growth (3%). Aesthetic differences resulted in feelings of self-consciousness and embarrassment in 50% of adolescents and 33% of younger children. However, younger children more frequently reported emotional stress due to external responses/reactions to visible differences of their hands rather than their own internal dislike of aesthetic irregularities compared with adolescents.
Social Interactions
Social interactions resulted in stress among 19 (58%) of children. Most commonly, teasing (39%), answering questions about hands (36%) and meeting new people (30%) caused stress. Feeling stigmatized (21%) and/or bullied (21%) was not uncommon among children who reported stress.
Emotional reactions
Emotional reactions exacerbated stress among 15 (45%) of children, most commonly due to feeling self-conscious regarding the appearance or function of their hands (33%), or frustrated with their inability to accomplish tasks with their hands (12%).
Coping Strategies
Children and their parents reported 8 categories of coping with congenital hand differences (Table 4). In this sample, 17 (52%) families endorsed using the following strategies: humor (12%), self-acceptance (21%), avoidance (27%), seeking external support (30%), concealment (30%), educating others (9%), support programs (21%) and religion (24%). Of these, several were focused toward reaffirming or improving children’s self-esteem: social/emotional support, self-acceptance, preparing a default answer about their hands, viewing hand differences positively, humor, and educating others. For example, children reported that accepting themselves helped them combat feelings of inadequacy (e.g. “When you get used to [having a congenital hand difference], it’s really cool, because you’re not like other people, you're different.”) However, participants also described three coping strategies that did not improve self-esteem: hiding hands, ignoring questions, and not disclosing their condition. Participants cited poorer self-esteem and greater insecurity due to congenital hand differences (e.g. “Sometimes I just slip my sleeves over it, like when you walked in…sometimes I don’t even like to look at it myself, so I just hide it a little bit.”)
Table 4.
Themes related to stress and coping: categories, codes, sub-codes, and frequencies
| Category | Code | Sub-codes | Frequency | ||
|---|---|---|---|---|---|
| N | % | ||||
| Stress | Functional limitations | Music | 9 | 27 | |
| Sports | 10 | 30 | |||
| Writing | 10 | 30 | |||
| Clothing and grooming | 19 | 58 | |||
| Typing | 7 | 21 | |||
| Utensils | 3 | 9 | |||
| Household chores | 12 | 36 | |||
| Total | 20 | 61 | |||
| Aesthetic appearance | Scarring | 6 | 19 | ||
| Deviation | 7 | 21 | |||
| Hair growth | 1 | 3 | |||
| Total | 9 | 27 | |||
| Social | Meeting new people | 10 | 30 | ||
| Disclosing differences | 12 | 36 | |||
| Stigmatization | 7 | 21 | |||
| Bullying | 7 | 21 | |||
| Alienation | 5 | 15 | |||
| Teasing | 13 | 39 | |||
| Total | 19 | 58 | |||
| Emotional reactions | Frustration | 4 | 12 | ||
| Anxiety | 2 | 6 | |||
| Embarrassment | 2 | 6 | |||
| Self-consciousness | 11 | 33 | |||
| Total | 15 | 46 | |||
| Coping | Humor | 4 | 12 | ||
| Self-acceptance | Viewing hands as “special/cool” | 7 | 21 | ||
| Avoidance | Avoiding social situations | 3 | 9 | ||
| Ignoring specific peers | 4 | 12 | |||
| Ignoring questions | 7 | 21 | |||
| Seeking emotional support | Seeking parent support | 6 | 18 | ||
| Seeking peer support | 5 | 15 | |||
| Seeking family/sibling support | 6 | 18 | |||
| Seeking authority figure support | 5 | 15 | |||
| Concealment | Hiding hands | 10 | 30 | ||
| Avoiding hand contact | 2 | 6 | |||
| Education | Educating peers or teachers | 3 | 9 | ||
| Support programs | 7 | 21 | |||
| Religion/spirituality | 8 | 24 | |||
| Total | 17 | 52 | |||
Children and parents reported 4 coping resources: parents, peers, teachers, and familiar social environments. For example, parents of children explained hand conditions using positive terminology that focused on their being special because of their differences (e.g. “I just told her that’s the way she was born and the way God made her, and that she was still capable of doing things and that she’s special.”) Being in a familiar social environment (e.g. living in a small town, staying at the same school) helped to minimize certain stressors; children received fewer questions about their hands, encountered new people less frequently, and could easily access social support (e.g. “We were such a small community that people were very supportive.”) Additionally, when children stayed at the same school, bullying subsided over time as their peers became familiar with them (e.g. “At first there were mean kids and stuff, but once they got to know him he seemed to do alright.”).
Discussion
Congenital hand differences have a profound, lifelong impact on a child’s social, emotional, and physical development. Using qualitative techniques, we explored the complex relationship between stress and coping among children with congenital hand differences. We identified several sources of stress among families of children with congenital hand differences: functional deficits, aesthetic deformities, social interactions, and emotional reactions. However, children and parents cite several important coping mechanisms and resources that serve to improve self-esteem (e.g. seeking social/emotional support). Nonetheless, other coping strategies, such as hiding hands and avoiding situations that draw attention to their hands, may reinforce negative emotions and poor self-image.
Understanding the psychological effects of upper extremity differences can provide important insight into how children develop emotionally and socially, and adapt to disability. Prior studies of children with congenital hand differences have identified higher rates of depression, anxiety, and low self-esteem among children with congenital and acquired limb deficiencies. 12 23 Recent studies suggest that social adaptation is significantly correlated with functional ability and the presence of other comorbid conditions. Additionally, self-concept and self-esteem varies by gender, and the severity of the deformity.3,4 However, much less is known regarding coping mechanisms among children with congenital hand differences, and research from other pediatric disciplines can help provide context for our findings. For example, among children with burn injuries, the presence of a burn injury in a visible area, such as the hands, is more strongly associated with psychological consequences than the overall severity of the burn. 24–26 Visible differences in appearance can exacerbate normal childhood experiences, such as comparison between peers, and have powerful psychosocial ramifications, including anxiety, depressive symptoms, and social withdrawal. 7 Certain coping and parenting techniques that prior research indicates are beneficial (e.g. social/emotional support) also seemed to promote greater self-esteem among congenital hand patients. Likewise, parents in this study explained hand conditions to children in a positive way (e.g. hands are special), a technique that has been endorsed to help dissolve stigma associated with traditional terminology (e.g. deformity).7
Our study has several limitations. We collected qualitative data from semi-structured interviews of parents and children with congenital hand differences, and the collection, analysis, and interpretation of this data is subject to investigator bias. 14,20,27,28 To minimize this, all data collection was conducted by investigators not involved with the child’s clinical care, and two investigators were present for each interview. Standardized interview guides were used, and three members of the study team independently coded the transcripts, which were reconciled to ensure 80% coding accuracy. Additionally, our findings may be limited by recall bias, and we relied on the parent’s interpretation of children’s stress and coping mechanisms during early childhood. Furthermore, we did not measure stress among normative controls, and it is difficult to discern the degree of stress related to hand differences alone. Finally, our study sample was limited in size, and may not accurately represent the experiences of all children with congenital hand differences. Families that agreed to participate may be more likely to be satisfied with their reconstructive outcomes or better able to participate because of broader social networks or accommodation in work/family-related commitments compared with families whom we were unable to reach or who declined participation. Nonetheless, qualitative studies aim to generate themes that are previously un-explored but relevant to a population of interest to provide a framework for future investigation, rather than empirically test hypotheses and quantify specific health outcomes. The validity of this and other qualitative studies is more related to careful sample selection and the depth and scope of gathered data, rather than sample size as in quantitative studies. 14,15,18,19,29,30 Furthermore, we reached theoretical saturation in our thematic analysis after extensive interviews with our sample, which indicates that the number of participants was sufficient to answer our research questions. 14,16,20
Despite these limitations, our findings have important applications for children born with congenital hand anomalies. For these children, emotional stress throughout childhood is not uncommon, and is frequently associated with difficulty with social interactions and frustration with physical disability. Therefore, psychological screening for stress and maladjustment may be beneficial, in order to introduce interventions to teach positive coping (i.e. strategies that improve how children perceive themselves) at an early age to enhance self-esteem and self-concept. For example, positive coping taught through cognitive behavioral therapy techniques has been shown to significantly reduce anxiety, depression, and internalization of problems among children with visible differences. 24 Compared to conventional patient education, these techniques recognize the dynamic nature of child development and social interactions, and provide children with discrete skills that can be used to modify emotional and behavioral responses to stress. For example, cognitive behavioral therapy produces sustained improvements in coping as well as functional deficits among children with chronic conditions. 31,32
In summary, over half of children with congenital hand differences face stress throughout childhood, and of these, 50% have stress that is unrecognized by parents and caregivers. Nonetheless, parents are an important coping resource for children, and can facilitate coping that improves self-esteem by explaining hand differences in a positive manner, helping children develop a default explanation about their hands, and providing social and emotional support. Clinicians can intervene to prevent emotional stress by informing parents about potential stressors and screening for signs of unmanaged emotional stress (e.g. anxiety, anger) to identify those children who will derive benefit from supportive interventions. In this way, parents and physicians can provide children born with congenital hand differences with the tools they need to cope with stress and manage their emotional and behavioral responses in a positive manner.
Acknowledgments
Supported in part by grants from the American Foundation for Surgery of the Hand (to Dr. Kate W. Nellans) and a Michigan Institute for Clinical Health Research MICHR/CTSA Pilot Grant (to Dr. Jennifer F. Waljee), and a Midcareer Investigator Award in Patient-Oriented Research (2 K24-AR053120-06) (to Dr Kevin C Chung)
References
- 1.Martin JA, Hamilton BE, Osterman MJK, Curtin SC, Mathews TJ. Births: Final Data for 2012. National Vital Statistical Reports. 2013;62(9) [PubMed] [Google Scholar]
- 2.Black JM, Edsberg LE, Baharestani MM, et al. Pressure ulcers: avoidable or unavoidable? Results of the National Pressure Ulcer Advisory Panel Consensus Conference. Ostomy Wound Manage. 2011 Feb;57(2):24–37. [PubMed] [Google Scholar]
- 3.Andersson GB, Gillberg C, Fernell E, Johansson M, Nachemson A. Children with surgically corrected hand deformities and upper limb deficiencies: self-concept and psychological well-being. Journal of Hand Surgery (European Volume) 2011;36(9):795–801. doi: 10.1177/1753193411412869. [DOI] [PubMed] [Google Scholar]
- 4.Ardon MS, Janssen WG, Hovius SE, Stam HJ, Selles RW. Low Impact of Congenital Hand Differences on Health-Related Quality of Life. Archives of physical medicine and rehabilitation. 2012;93(2):351–357. doi: 10.1016/j.apmr.2011.09.004. [DOI] [PubMed] [Google Scholar]
- 5.Joachim G, Acorn S. Stigma of visible and invisible chronic conditions. J Adv Nurs. 2000 Jul;32(1):243–248. doi: 10.1046/j.1365-2648.2000.01466.x. [DOI] [PubMed] [Google Scholar]
- 6.Jakubietz RG, Jakubietz MG, Kloss D, Gruenert JG. Defining the basic aesthetics of the hand. Aesthetic Plast Surg. 2005 Nov-Dec;29(6):546–551. doi: 10.1007/s00266-005-0100-6. [DOI] [PubMed] [Google Scholar]
- 7.Rumsey N, Harcourt D. Visible difference amongst children and adolescents: issues and interventions. Developmental neurorehabilitation. 2007 Apr-Jun;10(2):113–123. doi: 10.1080/13638490701217396. [DOI] [PubMed] [Google Scholar]
- 8.Goldberg RT. Adjustment of children with invisible and visible handicaps: Congenital heart disease and facial burns. Journal of Counseling Psychology. 1974;21(5):428–432. [Google Scholar]
- 9.Alansari R, Bedos C, Allison P. Living with cleft lip and palate: the treatment journey. The Cleft palate-craniofacial journal : official publication of the American Cleft Palate-Craniofacial Association. 2014 Mar;51(2):222–229. doi: 10.1597/12-255. [DOI] [PubMed] [Google Scholar]
- 10.Lazarus RS, Folkman S. Stress, Appraisal, and Coping. New York, NY: Springer Publishing Company, Inc; 1984. [Google Scholar]
- 11.Chetpakdeechit W, Hallberg U, Hagberg C, Mohlin B. Social life aspects of young adults with cleft lip and palate: grounded theory approach. Acta odontologica Scandinavica. 2009;67(2):122–128. doi: 10.1080/00016350902720888. [DOI] [PubMed] [Google Scholar]
- 12.Varni JW, Setoguchi Y, Rappaport LR, Talbot D. Psychological adjustment and perceived social support in children with congenital/acquired limb deficiencies. Journal of behavioral medicine. 1992 Feb;15(1):31–44. doi: 10.1007/BF00848376. [DOI] [PubMed] [Google Scholar]
- 13.Broder H, Strauss RP. Self-concept of early primary school age children with visible or invisible defects. The Cleft palate journal. 1989 Apr;26(2):114–117. discussion 117–118. [PubMed] [Google Scholar]
- 14.Shauver MJ, Chung KC. A guide to qualitative research in plastic surgery. Plast Reconstr Surg. 2010 Sep;126(3):1089–1097. doi: 10.1097/PRS.0b013e3181e60624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Squitieri L, Larson B, Chang KW, Yang L, Chung KC. Medical decision making and patient expectations among adolescents with neonatal brachial plexus palsy and their families: a qualitative study. Plast Reconstr Surg. 2013 doi: 10.1097/PRS.0b013e31828bd52b. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sandelowski M. Sample size in qualitative research. Research in nursing & health. 1995 Apr;18(2):179–183. doi: 10.1002/nur.4770180211. [DOI] [PubMed] [Google Scholar]
- 17.Coyne IT. Sampling in qualitative research. Purposeful and theoretical sampling; merging or clear boundaries? J Adv Nurs. 1997 Sep;26(3):623–630. doi: 10.1046/j.1365-2648.1997.t01-25-00999.x. [DOI] [PubMed] [Google Scholar]
- 18.Giacomini MK, Cook DJ. Users' guides to the medical literature: XXIII. Qualitative research in health care A. Are the results of the study valid? Evidence-Based Medicine Working Group. Jama. 2000 Jul 19;284(3):357–362. doi: 10.1001/jama.284.3.357. [DOI] [PubMed] [Google Scholar]
- 19.Giacomini MK, Cook DJ. Users' guides to the medical literature: XXIII. Qualitative research in health care B. What are the results and how do they help me care for my patients? Evidence-Based Medicine Working Group. Jama. 2000 Jul 26;284(4):478–482. doi: 10.1001/jama.284.4.478. [DOI] [PubMed] [Google Scholar]
- 20.Strauss A, Corbin J. Basics of qualitative research. Thousand Oaks, CA: Sage Publications; 1998. [Google Scholar]
- 21.Kisala P, Tulsky D. Opportunities for CAT Applications in Medical Rehabilitation: Development of Targeted Item Banks. Journal of applied measurement. 2010;11(3):315–330. [PMC free article] [PubMed] [Google Scholar]
- 22.Cohen S, Janicki-Deverts D, Miller GE. Psychological stress and disease. Jama. 2007 Oct 10;298(14):1685–1687. doi: 10.1001/jama.298.14.1685. [DOI] [PubMed] [Google Scholar]
- 23.Varni JW, Rubenfeld LA, Talbot D, Setoguchi Y. Determinants of self-esteem in children with congenital/acquired limb deficiencies. J Dev Behav Pediatr. 1989 Feb;10(1):13–16. [PubMed] [Google Scholar]
- 24.Maddern LH, Cadogan JC, Emerson MP. 'Outlook': A psychological service for children with a different appearance. Clinical child psychology and psychiatry. 2006 Jul;11(3):431–443. doi: 10.1177/1359104506064987. [DOI] [PubMed] [Google Scholar]
- 25.Meyers-Paal R, Blakeney P, Robert R, et al. Physical and psychologic rehabilitation outcomes for pediatric patients who suffer 80% or more TBSA, 70% or more third degree burns. J Burn Care Rehabil. 2000 Jan-Feb;21(1 Pt 1):43–49. doi: 10.1097/00004630-200021010-00009. [DOI] [PubMed] [Google Scholar]
- 26.Blakeney P, Meyer W, 3rd, Robert R, Desai M, Wolf S, Herndon D. Long-term psychosocial adaptation of children who survive burns involving 80% or greater total body surface area. J Trauma. 1998 Apr;44(4):625–632. doi: 10.1097/00005373-199804000-00011. discussion 633–624. [DOI] [PubMed] [Google Scholar]
- 27.Creswell JW. Research design: Qualitative and quantitative approaches. London: 1994. Publications. S, ed. [Google Scholar]
- 28.Silverman D, Marvasti A. Doing qualitative research: A comprehensive guide. Sage Publications, Incorporated; 2008. [Google Scholar]
- 29.Kisala PA, Tulsky DS. Opportunities for CAT applications in medical rehabilitation: development of targeted item banks. Journal of applied measurement. 2010;11(3):315–330. [PMC free article] [PubMed] [Google Scholar]
- 30.Tammaru M, Strompl J, Maimets K, Hanson E. The value of the qualitative method for adaptation of a disease-specific quality of life assessment instrument: the case of the Rheumatoid Arthritis Quality of Life Scale (RAQoL) in Estonia. Health Qual Life Outcomes. 2004;2:69. doi: 10.1186/1477-7525-2-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hirshfeld-Becker DR, Masek B, Henin A, et al. Cognitive behavioral therapy for 4- to 7-year-old children with anxiety disorders: a randomized clinical trial. J Consult Clin Psychol. 2010 Aug;78(4):498–510. doi: 10.1037/a0019055. [DOI] [PubMed] [Google Scholar]
- 32.Kashikar-Zuck S, Sil S, Lynch-Jordan AM, et al. Changes in pain coping, catastrophizing, and coping efficacy after cognitive-behavioral therapy in children and adolescents with juvenile fibromyalgia. The journal of pain : official journal of the American Pain Society. 2013 May;14(5):492–501. doi: 10.1016/j.jpain.2012.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]