Abstract
This study examined the associations of diabetes-related distress (DRD), depressive symptoms, health-related quality of life (HRQoL), and medication adherence with glycemia, blood pressure (BP), and lipid biomarkers in adults with type 2 diabetes mellitus (T2D). This cross-sectional study was conducted in three Malaysian public health clinics in 2012–2013, recruited adult patients (aged ≥30 years) with T2D who had been diagnosed for more than one year, were on active follow-up, and had recent blood test results. Univariable and multivariable analyses were performed to identify significant associated factors for glycated hemoglobin (HbA1c) BP, and lipids. The response rate was 93.1% (700/752). The majority were females (52.8%), Malay (52.4%), and married (78.7%). DRD correlated with systolic BP (r= −0.16); depressive symptoms correlated with low-density lipoprotein cholesterol (r=0.12) and total cholesterol (r=0.13); medication adherence correlated with HbA1c (r= −0.14) and low-density lipoprotein cholesterol (r= −0.11); and HRQoL correlated with casual blood glucose (r= −0.11), high-density lipoprotein cholesterol (r= −0.13), and total cholesterol (r= −0.08). Multivariable analyses showed that HRQoL was significantly associated with casual blood glucose (adjusted B= −0.06, P=0.024); DRD was associated with systolic BP (adjusted B= −0.08, P=0.066); depressive symptoms were associated with low-density lipoprotein cholesterol (adjusted B=0.02, P=0.061), and medication adherence was associated with HbA1c (adjusted B= −0.11, P=0.082) and total cholesterol (adjusted B= −0.06, P=0.086). There were significant and distinctive associations of DRD, depressive symptoms, HRQoL, and medication adherence with glycemia, BP, and lipid biomarkers. Unexpected beneficial therapeutic effects of DRD on BP require further study. A multidisciplinary approach may be needed for risk management in adults with T2D at the primary care level.
Keywords: distress, depression, medication adherence, quality of life, type 2 diabetes mellitus, glycated hemoglobin, blood pressure, lipids
Video abstract
Introduction
It is widely known that patients living with type 2 diabetes (T2D) carry a high burden of psychosocial problems1 and psychological disorders.2–4 Worrying about the future, the possibility of complications, and feelings of guilt or anxiety when “off-track” with diabetes management are reported to be sources of significant distress.5,6
Emotional distress in people with diabetes mellitus mainly comprises diabetes-related distress (DRD) and depression.7 Among adults with T2D, DRD and depression were reported to be more prevalent and persistent than other affective disorders (anxiety, panic disorders, and dysthymia) over a period of 18 months.3 DRD is defined as patient concerns about disease management, support, emotional burden, and access to care, and is distinctively different from depression, which is not disease-specific or context-specific to diabetes care.8–10 It was suggested from previous studies that DRD could progress to depression,11 a more severe form of emotional distress, which in turn causes poor self-care activity, disease control, morbidity, and mortality.7,12 Fisher (β=0.026)10 and Aikens (adjusted β=0.34)13 reported a cross-sectional relationship between DRD and control of glycated hemoglobin (HbA1c).
Since the introduction of DRD-specific scales such the Diabetes Distress Scale (DDS-17) in 20058 and the Problem Areas In Diabetes in 1995,14 there have been increasing numbers of studies looking into the relationship between DRD and disease control in adults with T2D.15 Nevertheless, reports of patient self-reported outcome measures, such as DRD, depression, health-related quality of life (HRQoL), and medication adherence (MA) have been few in non-Western countries. As these aspects of patient are important in self-management and disease control,15–17 it is paramount that their associations are studied in patients of other cultural backgrounds. The Asia-Pacific region including Malaysia has reported an increasing prevalence of T2D.18 Abundant local data have shown that poor disease control and suboptimal clinical management are hard to overcome.19–21 This would inevitably lead to increased patient suffering and health care costs from diabetes-related complications.22,23
This study examined the associations of DRD, depression, MA, and HRQoL with the three main biomarkers of risk, namely glycemia, blood pressure (BP), and lipids in adults with T2D. As part of a larger study of emotional burden and its effect on disease control, MA, and quality of life in patients with T2D (EDDMQoL), it is hoped that this study would be informative regarding the associations between these variables to improve existing therapeutic strategies or provide grounds for a potential risk management intervention in these patients.
Materials and methods
This cross-sectional study was conducted from 2012 to 2013. In addition to a questionnaire on demography (age, gender, ethnicity, types of religion, degrees of religiosity, marital status, educational level, employment status, monthly income), exercise, and smoking status, we used a structured case record form to capture comorbidity (hypertension and hyperlipidemia/dyslipidemia), diabetes-related complications, duration of diabetes, glycemic status, and BP and lipid control, along with number and types of medication used. We also used another four questionnaires to evaluate DRD, depressive symptoms (DS), MA, and HRQoL. These questionnaires were prepared in three languages, ie, English, Malay, and Mandarin.
Setting
Participants were recruited from three public health clinics (Klinik Kesihatan Seri Kembangan, Klinik Kesihatan Dengkil, and Klinik Kesihatan Salak) in Malaysia. These health clinics were chosen because they are different in terms of patient sociodemographic characteristics and the geographical regions that they are situated in. The variability of the sites provided a broad range of patients in which to assess the relationships between the study variables.
Participants
We consecutively sampled all patients with T2D who came to the clinics. They were at least 30 years old and had to have been diagnosed more than one year earlier. Patients were on regular follow-up, had made at least three visits in the past year, and had recent blood results within the previous 3 months. We excluded patients who were pregnant or lactating, patients who had a psychiatric/psychological disorder that could impair judgment and memory, and patients who could not read or understand English, Malay, or Mandarin. Patients who fulfilled the criteria were approached and informed of the study, and written consent was secured before answering the questionnaires in the language they preferred. This cross-sectional study was approved by the Medical Research Ethics Committee, Ministry of Health, Malaysia.
Definitions of disease
The definition of T2D in this study was based on the following: either a documented diagnosis of T2D according to 1999 World Health Organization criteria24 or current treatment recorded in the patient’s card as consisting of lifestyle modification, oral hypoglycemic agents, or insulin. This information was obtained from patient case records.
Glycemic status comprised HbA1c and casual blood glucose (CBG). Hypertension was diagnosed if systolic BP was ≥130 mmHg or diastolic BP was ≥80 mmHg on each of two successive readings obtained by the clinic physicians.25 Lipid profile consisted of low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), triglycerides, and total cholesterol. Dyslipidemia refers to either an increase or decrease in concentration of one or more plasma or serum lipids (LDL-C >2.6 mmol/L, triglycerides >1.7 mmol/L, and HDL-C <1.1 mmol/L).25,26 These clinical data were retrieved from the patient’s medical record using a case record form on the same day as the patient completed the questionnaires.
Definitions of diabetes-related complications
There were five diabetes-related complications in this study; three were classified as microvascular complications, ie, retinopathy, nephropathy, and diabetic foot problems; another two were classified as macrovascular complications, ie, ischemic heart disease and cerebrovascular disease or stroke. These complications were retrieved from patients’ records. Diabetic foot problems comprised foot deformity, current ulcer, amputation, peripheral neuropathy, or peripheral vascular disease.
Diabetes-related distress
DRD was measured using the validated DDS-17.8 This instrument assesses problems and difficulties concerning diabetes during the previous month on a Likert scale from 1 (not a problem) to 6 (a very serious problem).8,27 The DDS-17 yields a total diabetes distress scale score plus four subscale scores that address different types of distress, ie, emotional burden, physician-related distress (PD), regimen-related distress, and diabetes-related interpersonal distress.8 A local translation and validation study of the Malay version of the DDS-17 showed high internal consistency (Cronbach’s α=0.94), and the test-retest reliability value was 0.33 (P=0.009). There was a significant association between mean DDS-17 item score categories (<3 versus ≥3) and HbA1c categories (<7% versus ≥7%, χ2=4.20; P=0.048). [under a journal’s review].
Depressive symptoms
Symptoms of depression were measured using the 9-item Patient Health Questionnaire (PHQ-9), which has been shown to have good construct and criterion validity in diagnosing and assessing the severity of depression.28 The PHQ-9 refers to symptoms experienced by patients during the 2 weeks prior to answering the questionnaire. As a severity measure, the PHQ-9 scores range from 0 to 27. A PHQ-9 score of 0–4 suggests none to minimal depression, 5–9 indicates mild depression, 10–14 indicates moderate depression, 15–19 indicates moderately severe depression, and 20–27 indicates severe depression. The Malay version of the PHQ-9 had been locally validated, with acceptable psychometric properties.29 The reported sensitivity was 87% (95% confidence interval [CI] 71–95), the specificity was 82% (CI 74–88), the positive likelihood ratio was 4.8 (CI 3.2–7.2), and the negative likelihood ratio was 0.16 (CI 0.06–0.40).29
Medication adherence
The 8-item Morisky Medication Adherence Scale (MMAS-8) was used to measure MA. The MMAS-8 is reliable (Cron-bach’s α=0.83), with a sensitivity of 93% and a specificity of 53%,30 and the Malay version of the MMAS-8 has been locally validated, showing a significant relationship between MMAS-8 categories and HbA1c categories (χ2=20.261; P≤0.001).31 The MMAS-8 enquires about patient’s experiences with medications during the 2 weeks prior to answering the questionnaire. The total scale has a range of 0–8, including low adherence (<6), medium adherence (6–7), and high adherence (8).
Health-related quality of life
The World Health Organization Quality of Life-Brief (WHOQOL-BREF) produces four HRQoL domains and scores,32 ie, a physical domain, a psychological domain, a social relationships domain, and an environment domain.32 There are two items that examine overall HRQoL separately: question 1 asks about an individual’s overall perception of quality of life and question 2 asks about an individual’s overall perception of his or her health. Higher scores denote higher quality of life. We arbitrarily categorized this variable into three using a 0–100 score, ie, 0–49.99 (low), 50.01–74.99 (medium), or 75–100 (high, Figure 1).
Figure 1.
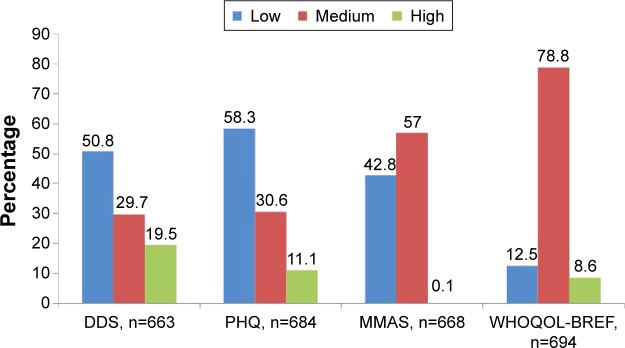
Proportion of patients according to the categories of diabetes-related distress, depressive symptoms, medication adherence, and health-related quality of life.
Abbreviations: DDS, Diabetes Distress Scale 17 items (low, no distress, mean DDS score <2; medium, moderate distress, mean DDS score 2–2.9; high, distress worthy of clinical attention, mean DDS score ≥3); PHQ, Patient Health Questionnaire 9 items (depression severity: low, no depression; PHQ score 0–4; medium, mild depression, PHQ score 5–9; high, moderate to severe depression, PHQ score 10–27); MMAS, Morisky Medication Adherence Scale 8 items (low, low adherence, MMAS score <6; medium, medium adherence, MMAS score 6–7; high, high adherence, MMAS score 8); WHOQOL-BREF, World Health Organization Quality of Life-Brief (low, 0–49.99; medium, 50.01–74.99; high, 7–100. WHOQOL-BREF categories are arbitrarily set).
Statistical analysis
The sample size was calculated using G*Power 3.1.2 software.33 Using an estimated relationship effect of r=0.16 between DRD and HbA1c,10,34 a power of 0.95, and significance at 0.05, the estimated sample size was 500. Taking into consideration 30% of incomplete/missing data in the patient medical record and incomplete questionnaires returned from patients, the sample size needed to be increased to 650.
The data analyses were done using PASW version 21.0 (SPSS, Chicago, IL, USA). Descriptive analyses were conducted to characterize the sample, and distributions were visually and quantitatively examined for normality of distribution. Since all the independent variables included were based on past studies, we further selected potential demographic and medical confounders from the univariable analyses. The dependent variables were HbA1c, CBG, systolic BP, diastolic BP, LDL-C, HDL-C, triglycerides, and total cholesterol. The associations of these disease control variables were analyzed using multivariable regression analyses, with potential confounders included in the model and using the criterion of two-tailed P<0.05. Missing data were not imputed because the available data and sample size were deemed adequately powered as evidence by the normal distributions of all the dependent variables as well as the main independent variables (DRD, DS, MA, and HRQoL). As the DDS-17 and PHQ-9 scores were moderately correlated (r=0.51, P<0.0001), they were evaluated both alone and when the other was adjusted for, because their multicol-linearity could distort their individual regression coefficients. Outliers were checked with std (standardized) residual, making sure that the minimum and maximum values did not exceed ±3. There were fewer than five outliers identified in the analyses, and as all the outliers were validated, we included all of them in the analyses. All statistical assumptions were checked and confirmed within acceptable limits.
Results
The participants’ response rate was 93.1% (700/752). The majority were females (52.8%), Malay (52.9%), married or living with partners (79.2%), had non-tertiary education (89.1%), and were earning <RM 3,000 per month (94.5%); most of the patients had some exercise and were non-smokers (Table 1). About 80% were reported to have hypertension, but use of antihypertensives was almost 90%. A similar observation was noted for dyslipidemia, with almost doubled percentage use of lipid-lowering agents compared to the prevalence of dyslipidemia (Table 1). Use of antiplatelet agents corresponded to the prevalence of complications. Table 1 shows the sociodemographic characteristics of the patients according to biomarkers of disease. Table 2 shows the differences in clinical parameters and mean scores for the DDS-17, PHQ-9, WHOQOL-BREF, and MMAS-8 in the three health clinics. Figure 1 shows the proportion of patients according to the categories of DDS-17, PHQ-9, MMAS-8, and WHOQOL-BREF. DRD and DS showed a descending pattern of distribution, with most patients reported to have mild symptoms. With regard to MA, almost all patients reported low to medium adherence with their medication. In terms of HRQoL, the majority of patients experienced a medium level of quality of life (Figure 1).
Table 1.
Sociodemographic characteristic according to the health clinics
| Total | HbA1c (%)
|
CBG (mmol/L)
|
SBP (mmHg)
|
DBP (mmHg)
|
LDL-C
|
HDL-C
|
TG
|
Total-C
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | P | Mean (SD) | P | Mean (SD) | P | Mean (SD) | P | Mean (SD) | P | Mean (SD) | P | Mean (SD) | P | Mean (SD) | P | |||
|
|
|
|
|
|
|
|
|
|||||||||||
| 8.5 (2.1) | 9.4 (3.7) | 136.9 (17.7) | 79.2 (12.2) | 3.0 (1.0) | 1.0 (0.3) | 1.9 (1.3) | 4.8 (1.2) | |||||||||||
| Gender | Female | 368 | 8.4 (2.0) | 0.253 | 9.4 (3.6) | 0.638 | 137.0 (17.6) | 0.902 | 78.8 (12.0) | 0.381 | 3.0 (1.0) | 0.084 | 1.0 (0.3) | <0.0001 | 1.8 (1.0) | 0.003 | 4.9 (1.1) | 0.119 |
| Male | 329 | 8.6 (2.3) | 9.5 (3.8) | 136.8 (17.8) | 79.6 (12.3) | 2.9 (1.0) | 0.9 (0.3) | 2.1 (1.6) | 4.7 (1.2) | |||||||||
| Ethnicity | Malay | 367 | 8.4 (2.2) | 0.138 | 9.5 (3.9) | 0.753 | 138.6 (17.9) | 0.020 | 81.0 (12.8) | <0.0001 | 3.1 (1.0) | 0.136 | 0.9 (0.3) | <0.0001 | 2.0 (1.3) | 0.214 | 4.9 (1.2) | 0.587 |
| Chinese | 162 | 8.3 (1.8) | 9.3 (3.2) | 136.1 (16.0) | 75.6 (11.5) | 2.9 (0.9) | 1.1 (0.4) | 1.8 (0.9) | 4.8 (1.0) | |||||||||
| Indian | 165 | 8.8 (2.2) | 9.6 (3.7) | 134.2 (18.5) | 78.5 (10.6) | 2.9 (1.0) | 0.9 (0.3) | 2.0 (1.5) | 4.8 (1.1) | |||||||||
| Aborigine | 3 | 7.8 (1.6) | 8.3 (1.8) | 125.7 (7.4) | 77.7 (2.1) | 1.6 (0.5) | 0.7 (0.2) | 2.0 (1.0) | 3.2 (0.5) | |||||||||
| Others | 3 | 7.1 (0.9) | 5.5 (1.1) | 130.7 (13.3) | 77.0 (14.1) | 2.3 (0.6) | 0.9 (0.2) | 1.4 (0.5) | 3.8 (0.6) | |||||||||
| Religion | No religion | 33 | 8.7 (1.8) | 0.494 | 8.6 (3.2) | 0.457 | 133.0 (14.6) | 0.053 | 73.5 (9.2) | <0.0001 | 2.8 (0.8) | 0.147 | 1.2 (0.4) | <0.0001 | 1.6 (0.7) | 0.066 | 4.7 (0.8) | 0.223 |
| Moslem | 375 | 8.4 (2.2) | 9.5 (3.9) | 138.6 (17.9) | 80.9 (12.9) | 3.1 (1.0) | 0.9 (0.3) | 2.0 (1.3) | 4.9 (1.2) | |||||||||
| Buddhist | 82 | 8.3 (2.0) | 9.9 (3.5) | 137.0 (16.4) | 76.4 (12.1) | 3.0 (1.0) | 1.1 (0.5) | 1.9 (1.1) | 5.0 (1.0) | |||||||||
| Hindu/Sikh | 149 | 8.7 (2.7) | 9.4 (3.6) | 133.6 (18.5) | 78.1 (10.2) | 3.0 (1.1) | 0.9 (0.2) | 2.1 (1.5) | 4.8 (1.2) | |||||||||
| Christian/Catholic | 22 | 8.8 (2.7) | 9.1 (3.2) | 134.5 (14.7) | 80.0 (13.2) | 2.5 (0.6) | 1.0 (0.3) | 1.3 (0.6) | 4.3 (0.7) | |||||||||
| Others | 37 | 8.1 (1.7) | 8.7 (2.6) | 136.5 (16.3) | 75.2 (10.4) | 2.7 (1.0) | 1.1 (0.3) | 1.7 (0.7) | 4.6 (1.1) | |||||||||
| Religiosity | Very agree | 294 | 8.6 (2.2) | 0.586 | 9.5 (3.5) | 0.334 | 137.5 (18.5) | 0.744 | 80.4 (12.9) | 0.065 | 3.1 (1.1) | 0.404 | 1.0 (0.3) | <0.0001 | 2.0 (1.5) | 0.272 | 4.9 (1.3) | 0.542 |
| Agree | 301 | 8.3 (2.2) | 9.5 (3.9) | 137.1 (17.6) | 78.7 (10.9) | 2.9 (0.9) | 0.9 (0.3) | 2.0 (1.2) | 4.7 (1.0) | |||||||||
| Not sure | 25 | 8.6 (1.5) | 10.0 (3.0) | 133.4 (16.0) | 78.0 (11.3) | 2.8 (0.9) | 1.0 (0.3) | 2.1 (1.2) | 4.9 (1.0) | |||||||||
| Disagree | 73 | 8.4 (1.8) | 8.6 (3.2) | 135.4 (15.6) | 75.9 (14.0) | 3.0 (0.9) | 1.2 (0.4) | 1.6 (0.6) | 4.9 (1.0) | |||||||||
| Very disagree | 3 | 9.5 (0.9) | 9.6 (2.0) | 133.0 (2.6) | 80.0 (6.1) | 2.9 (1.7) | 1.0 (0.2) | 2.0 (1.1) | 4.8 (1.4) | |||||||||
| Marital status | Married | 548 | 8.6 (2.2) | 0.067 | 9.5 (3.7) | 0.123 | 136.8 (17.7) | 0.942 | 79.9 (12.1) | 0.024 | 3.0 (1.0) | 0.642 | 1.0 (0.3) | 0.039 | 2.0 (1.3) | 0.216 | 4.8 (1.2) | 0.152 |
| Living with a partner | 3 | 8.1 (2.7) | 11.0 (4.3) | 128.3 (14.6) | 73.7 (6.7) | 2.5 (0.2) | 1.0 (0.1) | 1.3 (0.8) | 4.9 (1.3) | |||||||||
| Divorced | 13 | 8.9 (2.5) | 8.6 (3.1) | 138.2 (16.0) | 77.8 (9.5) | 3.2 (1.3) | 1.1 (90.3) | 2.7 (2.4) | 5.7 (1.7) | |||||||||
| Widowed | 98 | 8.0 (1.9) | 9.1 (3.6) | 138.0 (18.8) | 75.3 (12.3) | 3.0 (0.9) | 1.0 (0.4) | 1.7 (0.9) | 4.8 (1.0) | |||||||||
| Separated | 8 | 10.2 (2.4) | 11.2 (3.0) | 135.5 (23.1) | 79.8 (15.0) | 3.0 (1.1) | 1.0 (0.2) | 2.2 (1.4) | 5.0 (1.0) | |||||||||
| Single | 26 | 7.9 (1.6) | 7.9 (2.6) | 137.3 (15.1) | 80.5 (12.2) | 2.7 (0.8) | 1.1 (0.6) | 1.9 (1.3) | 4.5 (0.8) | |||||||||
| Educational level | Primary | 259 | 8.4 (2.2) | 0.807 | 9.4 (3.4) | 0.870 | 137.2 (19.6) | 0.673 | 77.3 (12.4) | 0.003 | 2.9 (1.0) | 0.466 | 1.0 (0.3) | <0.0001 | 1.8 (1.2) | 0.206 | 4.7 (1.1) | 0.181 |
| Secondary | 310 | 8.6 (2.2) | 9.5 (4.0) | 136.2 (16.9) | 80.2 (11.9) | 3.0 (1.0) | 1.0 (0.3) | 2.0 (1.4) | 4.9 (1.2) | |||||||||
| Tertiary | 75 | 8.5 (1.8) | 9.3 (3.3) | 136.8 (15.8) | 82.2 (11.7) | 3.1 (1.0) | 0.9 (0.20) | 2.2 (1.5) | 4.9 (1.3) | |||||||||
| Others | 45 | 8.5 (2.0) | 9.8 (3.9) | 139.5 (14.9) | 77.1 (11.9) | 2.9 (1.0) | 1.2 (0.6) | 1.9 (0.7) | 4.9 (1.0) | |||||||||
| Employment status | Employed | 315 | 8.7 (2.3) | 0.166 | 9.4 (3.7) | 0.632 | 135.3 (17.8) | 0.054 | 80.7 (12.9) | 0.004 | 3.0 (1.1) | 0.254 | 0.9 (90.3) | 0.007 | 2.1 (1.5) | 0.050 | 4.9 (1.3) | 0.600 |
| Unemployed | 11 | 8.7 (1.3) | 9.7 (3.3) | 130.5 (21.2) | 81.5 (15.1) | 3.2 (0.6) | 0.8 (0.1) | 2.3 (1.3) | 5.0 (0.8) | |||||||||
| Retired | 172 | 8.3 (1.9) | 9.7 (3.7) | 137.5 (18.4) | 76.6 (10.6) | 2.8 (1.0) | 1.0 (0.4) | 2.0 (1.2) | 4.7 (1.1) | |||||||||
| Home manager | 199 | 8.3 (2.1) | 9.2 (3.6) | 139.3 (16.5) | 78.7 (11.8) | 3.0 (1.0) | 1.0 (0.3) | 1.7 (0.9) | 4.8 (1.1) | |||||||||
| Income (RM) | No income | 157 | 8.3 (2.1) | 0.703 | 9.2 (3.2) | 0.742 | 138.0 (17.9) | 0.405 | 75.3 (11.3) | <0.0001 | 2.8 (0.9) | 0.228 | 1.0 (0.4) | 0.115 | 1.8 (1.0) | 0.412 | 4.7 (1.1) | 0.254 |
| <1,000 | 170 | 8.5 (2.1) | 9.5 (4.0) | 138.2 (919.4) | 79.4 (12.3) | 3.0 (1.0) | 1.0 (0.3) | 2.0 (1.5) | 4.8 (1.2) | |||||||||
| 1,000–2,999 | 235 | 8.5 (2.3) | 9.3 (3.5) | 135.3 (17.1) | 80.2 (12.8) | 3.0 (1.0) | 0.9 (0.2) | 2.0 (1.4) | 4.9 (1.3) | |||||||||
| 3,000–4,999 | 87 | 8.7 (2.1) | 9.9 (3.8) | 135.5 (14.6) | 82.4 (10.4) | 3.1 (1.1) | 1.0 (0.3) | 2.0 (1.3) | 4.9 (1.2) | |||||||||
| ≥5,000 | 38 | 8.3 (1.6) | 9.6 (3.3) | 136.8 (15.5) | 79.6 (11.8) | 3.0 (0.8) | 1.0 (0.3) | 1.6 (0.5) | 4.7 (0.8) | |||||||||
| Exercise | No | 295 | 8.6 (2.2) | 0.443 | 9.5 (3.9) | 0.481 | 137.7 (17.8) | 0.309 | 79.9 (12.2) | <0.0001 | 2.9 (1.0) | 0.071 | 0.9 (0.3) | 0.080 | 2.0 (1.3) | 0.325 | 4.8 (1.1) | 0.046 |
| ≤3 times/week | 232 | 8.4 (2.2) | 9.6 (3.6) | 137.2 (17.5) | 80.4 (11.8) | 3.1 (1.0) | 1.0 (0.3) | 2.0 (1.4) | 5.0 (1.2) | |||||||||
| >3 times/week | 169 | 8.3 (2.0) | 9.1 (3.4) | 135.1 (17.8) | 75.8 (12.1) | 2.9 (1.0) | 1.0 (0.4) | 1.8 (1.0) | 4.7 (1.2) | |||||||||
| Smoking | Never | 532 | 8.4 (2.1) | 0.177 | 9.4 (3.5) | 0.983 | 137.0 (917.6) | 0.808 | 79.3 (11.9) | 0.804 | 3.0 (1.0) | 0.109 | 1.0 (0.3) | 0.163 | 1.9 (1.3) | 0.393 | 4.9 (1.1) | 0.375 |
| Stopped ≤5 years | 22 | 9.1 (2.8) | 9.3 (5.6) | 139.8 (23.2) | 80.5 (13.2) | 2.7 (0.8) | 1.0 (0.4) | 2.3 (2.7) | 5.0 (1.6) | |||||||||
| Stopped >5 years | 60 | 8.1 (2.3) | 9.5 (4.0) | 136.1 (15.7) | 77.9 (12.2) | 2.7 (1.2) | 0.9 (0.2) | 2.1 (1.3) | 4.6 (1.4) | |||||||||
| Yes | 83 | 8.7 (2.0) | 9.6 (3.7) | 135.9 (18.0) | 79.0 (13.7) | 2.9 (1.0) | 1.0 (0.4) | 2.1 (1.0) | 4.8 (1.1) | |||||||||
| Alcohol consumption | Never | 607 | 8.5 (2.2) | 0.359 | 9.5 (3.7) | 0.692 | 137.0 (17.9) | 0.615 | 79.1 (12.0) | 0.844 | 3.0 (1.0) | 0.358 | 1.0 (0.3) | 0.106 | 1.9 (1.3) | 0.296 | 4.8 (1.2) | 0.105 |
| Yes | 45 | 8.4 (1.8) | 9.3 (3.7) | 134.5 (17.8) | 78.7 (13.5) | 3.0 (1.1) | 1.1 (0.5) | 2.2 (1.4) | 5.0 (1.1) | |||||||||
| Stopped drinking | 46 | 8.0 (1.8) | 9.0 (3.5) | 137.8 (15.1) | 80.1 (13.9) | 2.7 (0.9) | 0.9 (0.2) | 1.8 (0.8) | 4.5 (0.9) | |||||||||
| Hypertension | No | 149 | 8.9 (2.1) | 0.024 | 10.1 (4.6) | 0.014 | 130.3 (15.4) | <0.0001 | 79.2 (13.2) | 0.932 | 3.1 (0.9) | 0.112 | 0.9 (0.3) | 0.051 | 1.8 (1.3) | 0.193 | 4.9 (1.2) | 0.383 |
| Yes | 539 | 8.4 (2.1) | 9.3 (3.3) | 138.9 (17.8) | 79.2 (11.8) | 2.9 (1.0) | 1.0 (0.3) | 2.0 (1.3) | 4.8 (1.2) | |||||||||
| Dyslipidemia | No | 408 | 8.4 (2.1) | 0.465 | 9.6 (3.9) | 0.199 | 139.3 (18.4) | <0.0001 | 81.6 (12.6) | <0.0001 | 3.0 (0.9) | 0.277 | 0.9 (0.3) | <0.0001 | 2.0 (1.4) | 0.544 | 4.8 (1.2) | 0.929 |
| Yes | 265 | 8.6 (2.2) | 9.2 (3.2) | 133.5 (16.0) | 75.6 (10.5) | 2.9 (1.1) | 1.0 (0.3) | 1.9 (1.2) | 4.8 (1.2) | |||||||||
| Stroke/TIA | No | 681 | 8.5 (2.1) | 0.288 | 9.4 (3.7) | 0.790 | 136.8 (17.7) | 0.239 | 79.2 (12.2) | 0.974 | 3.0 (1.0) | 0.363 | 1.0 (0.3) | 0.386 | 1.9 (1.3) | 0.886 | 4.8 (1.2) | 0.699 |
| Yes | 14 | 7.8 (2.0) | 9.2 (3.0) | 142.4 (16.1) | 79.1 (11.9) | 2.6 (1.2) | 0.9 (0.1) | 2.0 (0.8) | 4.7 (1.3) | |||||||||
| Ischemic heart disease | No | 662 | 8.5 (2.2) | 0.816 | 9.4 (3.6) | 0.488 | 136.8 (17.8) | 0.430 | 79.3 (12.2) | 0.202 | 3.0 (1.0) | 0.048 | 1.0 (0.3) | 0.509 | 1.9 (1.3) | 0.784 | 4.8 (1.2) | 0.042 |
| Yes | 31 | 8.4 (1.6) | 9.9 (5.1) | 139.3 (15.7) | 76.5 (11.4) | 2.6 (90.9) | 0.9 (0.5) | 2.0 (0.7) | 4.4 (1.1) | |||||||||
| Retinopathy | No | 680 | 8.4 (2.1) | 0.013 | 9.4 (3.7) | 0.858 | 136.9 (17.8) | 0.986 | 79.3 (12.2) | 0.136 | 3.0 (1.0) | 0.191 | 1.0 (0.3) | 0.015 | 1.9 (1.3) | 0.589 | 4.8 (1.2) | 0.459 |
| Yes | 19 | 9.7 (2.2) | 9.6 (3.5) | 136.8 (14.5) | 75.1 (10.5) | 2.7 (1.1) | 1.2 (0.8) | 1.8 (0.9) | 4.6 (1.2) | |||||||||
| Nephropathy | No | 670 | 8.5 (2.2) | 0.350 | 9.4 (3.7) | 0.689 | 136.8 (17.7) | 0.807 | 79.2 (12.2) | 0.655 | 3.0 (1.0) | 0.404 | 1.0 (0.3) | 0.566 | 1.9 (1.3) | 0.997 | 4.8 (1.2) | 0.569 |
| Yes | 23 | 8.9 (1.7) | 9.7 (3.5) | 137.7 (17.3) | 78.0 (9.6) | 2.8 (1.1) | 1.0 (0.7) | 1.9 (1.2) | 4.7 (1.1) | |||||||||
| Diabetic foot problems | No | 672 | 8.5 (2.1) | 0.994 | 9.5 (3.7) | 0.065 | 137.1 (17.7) | 0.071 | 79.4 (12.3) | 0.019 | 3.0 (1.0) | 0.146 | 1.0 (0.3) | 0.047 | 1.9 (1.2) | 0.148 | 4.8 (1.2) | 0.107 |
| Yes | 22 | 8.5 (2.0) | 8.0 (3.1) | 130.2 (15.3) | 73.2 (7.3) | 2.6 (0.9) | 0.8 (0.1) | 2.4 (2.2) | 4.4 (1.1) | |||||||||
| OHA | No | 61 | 9.0 (2.5) | 0.041 | 10.1 (4.3) | 0.128 | 144.1 (20.2) | 0.001 | 78.2 (11.4) | 0.504 | 3.2 (1.2) | 0.064 | 0.9 (0.2) | 0.257 | 2.3 (1.4) | 0.040 | 5.2 (1.3) | 0.009 |
| Yes | 634 | 8.4 (2.1) | 9.4 (3.6) | 136.2 (17.3) | 79.3 (12.3) | 2.9 (1.0) | 1.0 (0.3) | 1.9 (1.3) | 4.8 (1.2) | |||||||||
| Insulin | Nil | 423 | 7.7 (1.7) | <0.0001 | 8.6 (3.0) | <0.0001 | 136.1 (16.9) | 0.075 | 80.1 (12.6) | <0.0001 | 3.0 (0.9) | 0.015 | 1.0 (0.3) | 0.433 | 1.7 (0.9) | <0.0001 | 4.7 (1.0) | 0.004 |
| 1 type | 191 | 9.6 (2.1) | 10.5 (3.4) | 136.6 (19.0) | 77.1 (10.6) | 2.9 (1.1) | 1.0 (0.4) | 2.3 (1.6) | 4.9 (1.3) | |||||||||
| 2 types | 69 | 10.2 (2.3) | 11.7 (5.5) | 141.1 (18.5) | 77.6 (12.6) | 3.3 (1.0) | 0.9 (0.2) | 2.3 (2.0) | 5.3 (1.4) | |||||||||
| ≥3 types | 11 | 8.8 (1.7) | 10.8 (5.6) | 144.8 (10.6) | 90.8 (10.1) | 3.5 (1.3) | 0.8 (0.2) | 1.9 (0.8) | 5.1 (1.5) | |||||||||
| Number of AHA agents | Nil | 82 | 8.7 (2.1) | 0.530 | 10.1 (4.6) | 0.038 | 125.7 (14.0) | <0.0001 | 78.0 (14.5) | 0.192 | 3.2 (1.0) | 0.209 | 1.0 (0.3) | 0.154 | 1.7 (1.4) | 0.057 | 4.9 (1.1) | 0.630 |
| 1 type | 206 | 8.6 (2.1) | 9.3 (3.5) | 132.8 (14.5) | 77.8 (10.6) | 3.0 (1.0) | 1.0 (0.3) | 1.8 (1.0) | 4.8 (1.1) | |||||||||
| 2 types | 204 | 8.3 (2.1) | 8.9 (93.3) | 137.3 (16.4) | 79.7 (11.7) | 2.9 (1.0) | 1.0 (0.3) | 1.9 (91.1) | 4.7 (1.1) | |||||||||
| 3 types | 144 | 8.3 (2.3) | 9.8 (3.5) | 143.8 (18.5) | 80.6 (12.8) | 2.9 (1.0) | 1.0 (0.4) | 2.2 (1.7) | 4.9 (1.3) | |||||||||
| ≥4 types | 58 | 8.5 (2.0) | 9.9 (4.0) | 148.2 (21.5) | 80.2 (13.4) | 3.1 (1.1) | 0.9 (0.2) | 2.1 (91.3) | 4.9 (1.1) | |||||||||
| Number of LLA agents | Nil | 156 | 8.5 (2.1) | 0.773 | 9.7 (4.1) | 0.417 | 137.4 (17.8) | 0.125 | 81.2 (13.8) | 0.051 | 3.1 (0.8) | 0.111 | 1.0 (0.3) | 0.608 | 1.7 (0.8) | 0.035 | 4.8 (0.9) | 0.981 |
| 1 type | 534 | 8.5 (2.1) | 9.3 (3.5) | 136.6 (17.6) | 78.6 (11.7) | 2.9 (1.0) | 1.0 (90.3) | 2.0 (1.4) | 4.8 (1.2) | |||||||||
| 2 types | 4 | 9.3 (1.0) | 11.2 (93.9) | 154.3 (15.5) | 76.3 (7.9) | 2.3 (0.7) | 0.8 (0.4) | 2.1 (1.3) | 4.9 (1.8) | |||||||||
| Number of APA agents | Nil | 616 | 8.4 (2.1) | 0.656 | 9.5 (93.7) | 0.686 | 137.1 (17.8) | 0.644 | 79.8 (12.2) | <0.0001 | 3.0 (1.0) | 0.900 | 1.0 (0.3) | 0.560 | 1.9 (1.3) | 0.866 | 4.9 (1.2) | 0.291 |
| 1 type | 74 | 8.7 (2.3) | 9.2 (93.6) | 135.1 (16.6) | 74.1 (10.7) | 2.7 (0.9) | 1.0 (0.3) | 2.0 (1.4) | 4.6 (1.2) | |||||||||
| 2 types | 2 | 8.0 (0.6) | 7.9 (3.2) | 140.5 (20.5) | 69.0 (1.4) | 2.6 (0.5) | 0.8 (0.1) | 2.0 (0.9) | 4.4 (0.8) | |||||||||
Note: P-values were for the independent t-test and analysis of variance. The bold P-values signify those that were below the significant cut-off value of <0.05.
Abbreviations: CBG, casual blood glucose; SBP, systolic blood pressure; DBP, diastolic blood pressure; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol; OHA, oral hypoglycemic agent; AHA, antihypertensive agent; LLA, lipid-lowering agent; APA, antiplatelet agent; SD, standard deviation; TG, triglycerides; TIA, transient ischemic attack.
Table 2.
Clinical variables according to the health clinics
| Health clinic, mean (SD) [valid n]
|
F | P-value | ||||
|---|---|---|---|---|---|---|
| Total | Seri Kembangan | Dengkil | Salak | |||
| Age (years) | 56.9 (10.18) [698] | 58.8 (10.21) [222] | 57.7 (11.08) [123] | 55.5 (9.64) [353] | 7.81 | <0.0001 |
| Diabetes duration (years) | 6.5 (5.71) [677] | 9.1 (7.05) [220] | 6.3 (4.34) [123] | 4.9 (4.43) [334] | 39.94 | <0.0001 |
| HPT duration (years) | 6.8 (5.80) [515] | 8.4 (6.25) [171] | 7.0 (4.59) [108] | 5.6 (5.67) [236] | 12.60 | <0.0001 |
| Dyslipidemia duration (years) | 4.2 (3.01) [250] | 4.9 (3.33) [124] | 3.4 (2.28) [113] | 5.1 (3.68) [13] | 8.87 | <0.0001 |
| HbA1c (%) | 8.5 (2.14) [621] | 8.5 (2.05) [190] | 8.6 (2.21) [121] | 8.4 (2.16) [310] | 0.13 | 0.878 |
| CBG (mmol/L) | 9.4 (3.66) [687] | 9.1 (3.12) [219] | 9.3 (3.37) [123] | 9.7 (4.05) [345] | 2.00 | 0.137 |
| SBP (mmHg) | 136.9 (17.7) [695] | 134.5 (15.1) [219] | 131.1 (17.0) [123] | 140.5 (18.6) [353] | 16.71 | <0.0001 |
| DBP (mmHg) | 79.2 (12.2) [695] | 76.6 (11.0) [219] | 76.4 (9.3) [123] | 81.7 (13.2) [353] | 16.57 | <0.0001 |
| LDL-C (mmol/L) | 3.0 (1.00) [566] | 3.0 (1.04) [201] | 2.8 (1.11) [121] | 3.0 (0.90) [244] | 1.70 | 0.184 |
| HDL-C in mmol/L | 1.0 (0.32) [569] | 1.2 (0.32) [202] | 0.9 (0.32) [122] | 0.9 (0.26) [245] | 59.24 | <0.0001 |
| Triglycerides (mmol/L) | 1.9 (1.39) [569] | 1.8 (1.07) [201] | 2.0 (1.01) [123] | 2.0 (1.54) [245] | 2.53 | 0.081 |
| Total cholesterol (mmol/L) | 4.8 (1.17) [619] | 5.0 (1.09) [203] | 4.7 (1.21) [123] | 4.8 (1.20) [293] | 2.51 | 0.082 |
| DDS-17 | 37.1 (15.98) [663] | 40.6 (17.34) [206] | 40.3 (18.46) [118] | 33.8 (13.35) [339] | 14.93 | <0.0001 |
| Emotional burden | 11.9 (5.33) [685] | 11.9 (5.65) [219] | 12.6 (6.03) [120] | 11.6 (4.84) [346] | 1.30 | 0.274 |
| Physician distress | 7.9 (4.67) [683] | 9.6 (5.67) [216] | 9.1 (4.68) [121] | 6.4 (3.29) [346] | 40.49 | <0.0001 |
| Regimen distress | 11.3 (5.20) [690] | 12.0 (5.36) [218] | 12.2 (6.06) [121] | 10.6 (4.65) [351] | 7.88 | <0.0001 |
| Interpersonal distress | 6.3 (3.65) [689] | 7.2 (4.40) [217] | 7.0 (3.95) [121] | 5.6 (2.77) [351] | 16.15 | <0.0001 |
| PHQ-9 | 4.6 (4.31) [684] | 5.5 (4.91) [218] | 4.2 (4.01) [121] | 4.2 (3.90) [345] | 7.69 | <0.0001 |
| MMAS-8 | 5.6 (1.42) [668] | 5.6 (1.45) [216] | 5.8 (1.31) [121] | 5.6 (1.45) [331] | 0.76 | 0.469 |
| WHOQOL-BREF | 55.5 (6.31) [694] | 54.9 (6.66) [218] | 55.0 (6.11) [123] | 56.0 (6.12) [353] | 2.70 | 0.068 |
| Physical health | 13.1 (1.70) [700] | 12.8 (1.80) [224] | 13.1 (1.65) [123] | 13.3 (1.64) [353] | 5.22 | 0.006 |
| Psychological health | 13.3 (1.88) [697] | 13.0 (1.91) [221] | 12.7 (2.03) [123] | 13.6 (1.73) [353] | 12.94 | <0.0001 |
| Social relationship | 14.7 (2.40) [698] | 14.7 (2.50) [222] | 15.3 (2.45) [123] | 14.5 (2.29) [353] | 5.82 | 0.003 |
| Environmental | 14.4 (2.08) [697] | 14.3 (2.47) [221] | 13.9 (1.89) [123] | 14.7 (1.83) [353] | 8.19 | <0.0001 |
Note: P-values are for the analysis of variance.
Abbreviations: DDS-17, Diabetes Distress Scale 17 items; PHQ-9, Patient Health Questionnaire 9 items; MMAS-8, 8-item Morisky Medication Adherence Scale; WHOQOL-BREF, World Health Organization Quality of Life-Brief 26 items; CBG, casual blood glucose; SBP, systolic blood pressure; DBP, diastolic blood pressure; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol; HPT, hypertension; SD, standard deviation; HbA1c, glycated hemoglobin.
In Pearson correlation analysis, the DDS-17 score correlated with systolic BP (r= −0.157, P<0.001), diastolic BP (r= −0.083, P<0.05), and HDL-C (r=0.105, P<0.05). The PD subscale score showed a significant correlation with triglycerides (r= −0.095, P<0.05) whereas the total DDS-17 score did not show any correlation. The PHQ-9 score correlated with CBG (r=0.087, P<0.05), LDL-C (r=0.115, P<0.001), HDL-C (r=0.118, P<0.001), and total cholesterol (r=0.134, P<0.001). The MMAS-8 score correlated with HbA1c (r= −0.136, P<0.001), CBG (r= −0.088, P<0.05), diastolic BP (r= −0.130, P<0.001), LDL-C (r= −0.105, P<0.05), and total cholesterol (r= −0.136, P<0.001). Total WHOQOL-BREF score correlated with CBG (r= −0.111, P<0.001), HDL-C (r= −0.125, P<0.001), and total cholesterol (r= −0.084, P<0.05). Patient age showed a significant correlation with all disease control biomarkers except for CBG (Pearson r values ranged from −0.279 to 0.133). Diabetes duration (in years) correlated with HbA1c (r=0.212, P<0.001), CBG (r=0.109, P<0.001), diastolic BP (r= −0.196, P<0.001), LDL-C (r= −0.106, P<0.05), and HDL-C (r=0.138, P<0.001).
Table 3 shows the adjusted effects of DDS-17 (and PD), PHQ-9, WHOQOL-BREF, and MMAS-8 on disease bio-markers. WHOQOL-BREF had significant effect on CBG (adjusted B= −0.06, P=0.024). Other associations that had near significant effects included MMAS-8 on HbA1c, DDS-17 on systolic BP, PHQ-9 on LDL-C, PD on triglycerides, and WHOQOL-BREF and MMAS-8 on total cholesterol.
Table 3.
Determinants of disease biomarkers
| Model | Crude B (95.0% CI) | Adjusted B (95.0% CI) | Adjusted B (95.0% CI) | Significance | Adjusted R2 |
|---|---|---|---|---|---|
| HbA1c | n=441* | n=441** | |||
| Intercept | – | – | 9.77 (8.488, 11.053) | <0.0001 | 0.308 |
| MMAS-8 | −0.21 (−0.329, −0.085) | −0.10 (−0.224, 0.018) | −0.11 (−0.224, 0.014) | 0.082 | |
| CBG | n=613† | n=613†† | |||
| Intercept | – | – | 14.83 (11.526, 18.128) | <0.0001 | 0.110 |
| PHQ-9 | 0.07 (0.010, 0.139) | 0.01 (−0.067, 0.077) | 0.01 (−0.068, 0.077) | 0.900 | |
| MMAS-8 | −0.22 (−0.419, −0.029) | −0.11 (−0.311, 0.085) | −0.10 (−0.295, 0.100) | 0.332 | |
| WHOQoL-BREF | −0.06 (−0.107, −0.021) | −0.05 (−0.103, −0.005) | −0.06 (−0.105, −0.007) | 0.024 | |
| SBP | n=623‡ | n=623‡‡ | |||
| Intercept | – | – | 146.97 (136.544, 157.397) | <0.0001 | 0.166 |
| DDS-17 | −0.17 (−0.255, −0.089) | −0.09 (−0.174, −0.008) | −0.08 (−0.161, 0.005) | 0.066 | |
| LDL-C | n=401§ | n=401§§ | |||
| Intercept | – | – | 3.87 (3.018, 4.719) | <0.0001 | 0.052 |
| PHQ-9 | 0.03 (0.007, 0.044) | 0.02 (0.000, 0.044) | 0.02 (−0.001, 0.043) | 0.061 | |
| MMAS-8 | −0.07 (−0.133, −0.015) | −0.04 (−0.110, 0.030) | −0.03 (−0.103, 0.037) | 0.356 | |
| Triglycerides | n=551‖ | n=551‖‖ | |||
| Intercept | – | – | 2.74 (1.809, 3.660) | <0.0001 | 0.073 |
| Physician distress | −0.03 (−0.049, −0.003) | −0.02 (−0.046, −0.001) | −0.02 (−0.046, 0.002) | 0.072 | |
| Total cholesterol | n=569¶ | n=569¶¶ | |||
| Intercept | – | – | 7.06 (5.816, 8.311) | <0.0001 | 0.082 |
| PHQ-9 | 0.04 (0.014, 0.056) | 0.02 (−0.006, 0.043) | 0.01 (−0.011, 0.039) | 0.265 | |
| MMAS-8 | −0.11 (−0.177, −0.046) | −0.07 (−0.139, 0.001) | −0.06 (−0.131, 0.009) | 0.086 | |
| WHOQoL-BREF | −0.02 (−0.030, −0.001) | −0.02 (−0.033, 0.001) | −0.02 (−0.032, 0.001) | 0.070 |
Notes: Variables in the model include:
age, diabetes duration, HPT duration, retinopathy, OHA, insulin;
diabetes duration, HPT, insulin, AHA agents;
age, ethnic, HPT, dyslipidemia, OHA, AHA agents
age, diabetes duration, HPT duration, ischemic heart disease, insulin;
age, gender, employment, OHA, insulin, LLA;
age, OHA, insulin, exercise, ischemic heart disease;
**, ††, ‡‡, §§, ‖‖ and ¶¶In these models, health clinic is added.
Abbreviations: DDS-17, 17-item Diabetes Distress Scale; PHQ-9, 9-item Patient Health Questionnaire; MMAS-8, 8-item Morisky Medication Adherence Scale; WHOQoL-BREF, World Health Organization Quality of Life-Brief 26 items; HPT, hypertension; OHA, oral hypoglycemic agent; AHA, antihypertensive agent; LLA, lipid-lowering agent; APA, anti-platelet agent; CI, confidence interval; HbA1c, glycated hemoglobin.
Discussion
This study examined the associations of DRD, DS, HRQoL, and MA with glycemia, BP, and lipid biomarkers in adults with T2D. There have been very few studies that have investigated these four patient self-reported outcomes in adults with T2D and a multicultural Asian background or their associations with the three important disease status variables (HbA1c, BP, and lipids) in a single setting.
Sociodemographic characteristics, including age, gender, and ethnicity and their associations with disease control were similar to those in previous reports.35–37 In contrast with other cross-sectional data from India,38 Japan,39 and the USA,10,13 we did not observe any association between DRD or DS and HbA1c. Similarly, the associations of age, gender, ethnicity, diabetes duration, and medication use with glycemia, BP, and lipid control were not in parallel with earlier registry-based studies.21,35–37,40 This could be due to small differences in subgroups of these variables in this study or expanded power in the registry-based studies due to their very large sample size. The lack of an association between DRD and glucose biomarkers might indicate the relatively small effects of DRD, which were further diluted after adjusting for other sociodemographic variables. It is possible that DRD was a psychological state of coping (similar to the effects of DDS-17 on systolic BP, and the PD subscale on triglycerides, see below) and not related to failure of self-management that could affect HbA1c. Further studies are needed to look into the role of DRD in self-management of diabetes in patients with different sociocultural backgrounds, relationship to illness perception, coping, MA, and HRQoL.41
The most intriguing results in this study were the higher DRD and the lower systolic BP, higher PD, and lower triglycerides. This consistent trend of DRD with disease biomarkers was marked, with the PD subscale showing the highest (among the DDS-17, PHQ-9, and MMAS-8) and most consistent negative correlation with HbA1c, systolic and diastolic BP, and triglycerides. A plausible explanation for these observations is that DRD might indicate a state of psychological reaction or active coping by patients, resulting in heightened self-management. It is not uncommon for doctors in health clinics to become impatient with patients who do not adhere to advice, talk less even when patients ask for more explanation, and display indifference to patients during busy clinic days.42,43 In these situations, health conscious and capable patients might become distressed, which in turn motivates themselves towards self-care. This indirect and apparent effect of DRD on systolic BP, which is a form of psychological distress related to diabetes management, needs further investigation. Earlier studies reported that DRD was associated with poor diabetes self-care,44–46 and to our best knowledge, none of these studies had made a similar association between DRD and systolic BP. Further research is needed to confirm this hypothesis, and should include measures that assess self-care activity, self-efficacy, coping, and physician behaviors at the same time.
Compared with the DDS-17, which assesses diabetes-specific emotional distress, the PHQ-9 which measures DS and thus implies higher severity of an emotional distress,7 had shown more associations with the disease biomarkers. The presence of stronger associations between the PHQ-9, LDL-C, and total cholesterol suggests that DS affects lipid control more than DRD. A similar finding was reported in the USA, ie, after multivariable analysis, DRD was associated only with HbA1c and not with BP or LDL-C.47 However, in a study from Lithuania, significant correlations were found between scores for emotional state (tension-anxiety, depression-dejection, and confusion-bewilderment) and lipid levels (total cholesterol, triglycerides, and low-density lipoprotein cholesterol) in patients with T2D, especially women.48 It is less clear whether there is any physiological link between DRD or DS and lipid metabolism compared to that is known between these emotional distress with glucose and BP.12,49 Hence, DRD or DS might influence disease control through changed self-care activity50 and health behavior, such as dietary choices, physical exercise, and adherence with therapy.51 It was possible that factors related to the local health clinics themselves, such as accessibility, comfort, health care system, attitudes of health care providers, and availability of drugs52 could affect disease control, as shown by a further reduction in effect size (>10%) after controlling for the health clinic variable.
The results for MA and disease control was consistent with those of previous studies showing a prevalent association and positive effects of MA on disease control biomarkers.53,54 Higher MA was consistently shown to be associated with HbA1c, CBG, LDL-C, and total cholesterol. The direct and potent effects of medications on these biomarkers would be expected. However, loss of MA’s effects after controlling for covariates would suggest that disease control is multifactorial.54 Indirectly, the results of this study show that other outcome measures or confounders should also be considered for DRD and DS in achieving disease control, such as diabetes self-care activity, HRQoL, and diabetes-specific quality of life.55,56 In other words, holistic diabetes care that considers both appropriate use of medications and supporting the psychological states/behaviors of patients would constitute effective diabetes care.
HRQoL as measured by WHOQOL-BREF was the only variable that had a significant effect on CBG after controlling for the other covariates. The other near significant effect of HRQoL was on total cholesterol. It is not unexpected that better HRQoL contributes to better glycemic and lipid control. Previous studies have reported a prevalent association of poor HRQoL with high HbA1c, BP, and lipids.57–59 In addition to the probable mechanisms mentioned above, it is possible that HRQoL itself could have salutogenic effects on disease control.60 This means that patients with better HRQoL would be more capable in terms of self-management, emotional well-being, and social engagement. These attributes would further translate into better health literacy and adherence to therapy, and lead to better disease control. However, the selective effect of HRQoL on CBG is hard to explain in this study. We hypothesize that patients with higher HRQoL adopt selective self-management measures depending on their perceived needs. They might implement glucose control measures more strongly in days leading up to a medical visit at the health clinic but be less stringent at other times. This possibility is suggested by the negative correlation between WHOQOL-BREF score and other disease control biomarkers. However, the small effect sizes of these observations in spite of the relatively large sample size in this study casts doubt regarding the presence of any real or clinically significant relationship between HRQoL and disease control in relatively healthy adult patients with T2D attending these public health clinics.
Limitations and strengths
There are some limitations to this study. The strict inclusion criteria might have led to selection of a study population that was healthier, more adherent, and had better disease control, given that patients who do not turn up regularly for their appointments or have recent blood investigations might consist of those with poorer psychological well being and disease control. In addition, missing data could have been occurred in differential ways across the different category of outcomes, and as such, complete case analyses strategy as adopted in this study might affect the results and conclusions. However, we believe these biases are minimal, given that the distributions (distributions) of DRD, DS, HRQoL, and MA were all normal, and the distributions of disease control biomarkers were also normally distributed, indicating inclusion of a spectrum of disease biomarkers in the study population. The DDS-17, used in this study to measure DRD, may have inadequacies similar to those found with many standardized measures of diabetes distress,14 including lack of comprehensiveness with regard to assessment of sources of diabetes distress; for example, distress attributable to starting insulin, emergence of a new complication, or the accumulated demands and burdens of self-care. This problem might have constrained the scope of T2D’s impacts on the patients.
The strength of this study includes its real-world setting, high response rate, and good sample size. A further strength is that the study population is representative of the wider T2D patient population in this country, which enables generalization of the current findings.61
Conclusion
This study has shown associations of DRD, DS, HRQoL, and MA with glycemia, BP, and lipid biomarkers in adults with T2D at the primary care level. DS, MA, and HRQoL showed the expected associations with many disease biomarkers, except between DRD and BP. Efforts to increase MA may improve disease control more effectively than psychological interventions for DRD and DS. Therefore, the effects of DRD, DS, and HRQoL on MA are worthy of further study. DRD and DS had different effects on disease control, and might need different professional support. Lastly, the possible beneficial and therapeutic effects of DRD on BP require further study to determine the possible mechanisms underpinning this relationship.
Acknowledgments
This study was funded by the Research University Grants Scheme 2 (RUGS/04-02-2105RU). The authors acknowledge the Sepang and Petaling district health offices and officers for their support of this study and the Director-General of Health for giving permission to publish this research. They also acknowledge the World Health Organization and Harith Khalid Al-Qazaz for use of WHOQOL-BREF and the MMAS-8 Malay version, respectively. We thank Rimke Vos of the Julius Center for Health Sciences and Primary Care, University Medical Center Utrecht, the Netherlands, for her input into the initial draft of this manuscript. They would like to record their appreciation of Firdaus Mukhtar, Nor-Kasmawati Jamaludin, and Fuziah Paimin for their input during the planning of the study and assistance with data collection. Finally, they thank the staff at all the clinics for facilitating the data collection.
Footnotes
Disclosure
The authors report no competing interests in this work. The study sponsor had no role in the design or conduct of the study, the writing of this report, or the decision to submit it for publication.
References
- 1.Stuckey HL, Mullan-Jensen CB, Reach G, et al. Personal accounts of the negative and adaptive psychosocial experiences of people with diabetes in the second Diabetes Attitudes, Wishes and Needs (DAWN2) Study. Diabetes Care. 2014;37:2466–2474. doi: 10.2337/dc13-2536. [DOI] [PubMed] [Google Scholar]
- 2.Das-Munshi J, Stewart R, Ismail K, Bebbington PE, Jenkins R, Prince MJ. Diabetes, common mental disorders, and disability: findings from the UK National Psychiatric Morbidity Survey. Psychosom Med. 2007;69:543–550. doi: 10.1097/PSY.0b013e3180cc3062. [DOI] [PubMed] [Google Scholar]
- 3.Fisher L, Skaff MM, Mullan JT, Arean P, Glasgow R, Masharani U. A longitudinal study of affective and anxiety disorders, depressive affect and diabetes distress in adults with type 2 diabetes. Diabet Med. 2008;25:1096–1101. doi: 10.1111/j.1464-5491.2008.02533.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee S, Chiu A, Tsang A, Chow CC, Chan WB. Treatment-related stresses and anxiety-depressive symptoms among Chinese outpatients with type 2 diabetes mellitus in Hong Kong. Diabetes Res Clin Pract. 2006;74:282–288. doi: 10.1016/j.diabres.2006.03.026. [DOI] [PubMed] [Google Scholar]
- 5.West C, McDowell J. The distress experienced by people with type 2 diabetes. Br J Community Nurs. 2002;7:606–613. doi: 10.12968/bjcn.2002.7.12.10901. [DOI] [PubMed] [Google Scholar]
- 6.Li C, Ford ES, Zhao G, Balluz LS, Berry JT, Mokdad AH. Undertreatment of mental health problems in adults with diagnosed diabetes and serious psychological distress: the behavioral risk factor surveillance system, 2007. Diabetes Care. 2010;33:1061–1064. doi: 10.2337/dc09-1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fisher L, Gonzalez JS, Polonsky WH. The confusing tale of depression and distress in patients with diabetes: a call for greater clarity and precision. Diabet Med. 2014;31:764–772. doi: 10.1111/dme.12428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Polonsky WH, Fisher L, Earles J, et al. Assessing psychosocial distress in diabetes: development of the Diabetes Distress Scale. Diabetes Care. 2005;28:626–631. doi: 10.2337/diacare.28.3.626. [DOI] [PubMed] [Google Scholar]
- 9.Fisher L, Skaff MM, Mullan JT, et al. Clinical depression versus distress among patients with type 2 diabetes: not just a question of semantics. Diabetes Care. 2007;30:542–548. doi: 10.2337/dc06-1614. [DOI] [PubMed] [Google Scholar]
- 10.Fisher L, Mullan JT, Arean P, Glasgow RE, Hessler D, Masharani U. Diabetes distress but not clinical depression or depressive symptoms is associated with glycemic control in both cross-sectional and longitudinal analyses. Diabetes Care. 2010;33:23–28. doi: 10.2337/dc09-1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Skinner TC, Carey ME, Cradock S, et al. Depressive symptoms in the first year from diagnosis of type 2 diabetes: results from the DESMOND trial. Diabet Med. 2010;27:965–967. doi: 10.1111/j.1464-5491.2010.03028.x. [DOI] [PubMed] [Google Scholar]
- 12.Holt RI, de Groot M, Lucki I, Hunter CM, Sartorius N, Golden SH. NIDDK International Conference Report on Diabetes and Depression: current understanding and future directions. Diabetes Care. 2014;37:2067–2077. doi: 10.2337/dc13-2134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aikens JE. Prospective associations between emotional distress and poor outcomes in type 2 diabetes. Diabetes Care. 2012;35:2471–2478. doi: 10.2337/dc12-0181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Polonsky WH, Anderson BJ, Lohrer PA, et al. Assessment of diabetes-related distress. Diabetes Care. 1995;18:754–760. doi: 10.2337/diacare.18.6.754. [DOI] [PubMed] [Google Scholar]
- 15.Berry E, Lockhart S, Davies M, Lindsay JR, Dempster M. Diabetes distress: understanding the hidden struggles of living with diabetes and exploring intervention strategies. Postgrad Med J. 2015 Mar 31; doi: 10.1136/postgradmedj-2014-133017. Epub. [DOI] [PubMed] [Google Scholar]
- 16.Nozaki T, Morita C, Matsubayashi S, et al. Relation between psychosocial variables and the glycemic control of patients with type 2 diabetes: a cross-sectional and prospective study. Biopsychosoc Med. 2009;3:4. doi: 10.1186/1751-0759-3-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gallo JJ, Bogner HR, Morales KH, Post EP, Ten Have T, Bruce ML. Depression, cardiovascular disease, diabetes, and two-year mortality among older, primary-care patients. Am J Geriatr Psychiatry. 2005;13:748–755. doi: 10.1176/appi.ajgp.13.9.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Whiting DR, Guariguata L, Weil C, Shaw J. IDF Diabetes Atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. 2011;94:311–321. doi: 10.1016/j.diabres.2011.10.029. [DOI] [PubMed] [Google Scholar]
- 19.Mastura I, Chew BH, Lee PY, et al. Control and treatment profiles of 70,889 adult type 2 diabetes mellitus patients in Malaysia. Int J Collab Res Intern Med Public Health. 2011;3:98–113. [Google Scholar]
- 20.Chew BH, Cheong AT, Mastura I, Rahman SASA. Diabetic hypertensive control and treatment: a descriptive report from the Audit Diabetes Control And Management (ADCM) registry. Malays Fam Physician. 2010;5:134–138. [PMC free article] [PubMed] [Google Scholar]
- 21.Chew BH, Mastura I, Lee PY, et al. Determinants of uncontrolled dyslipidaemia among adult type 2 diabetes in Malaysia: the Malaysian Diabetes Registry 2009. Diabetes Res Clin Pract. 2012;96:339–347. doi: 10.1016/j.diabres.2012.01.017. [DOI] [PubMed] [Google Scholar]
- 22.Ibrahim WN, Aljunid S, Ismail A. Cost of type 2 diabetes mellitus in selected developing countries. Malaysian Journal of Public Health Medicine. 2010;10:68–71. [Google Scholar]
- 23.Currie CJ, Morgan CL, Dixon S, et al. The financial costs of hospital care for people with diabetes who have single and multiple macrovascular complications. Diabetes Res Clin Pract. 2005;67:144–151. doi: 10.1016/j.diabres.2004.01.002. [DOI] [PubMed] [Google Scholar]
- 24.World Health Organization . Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus. Geneva, Switzerland: World Health Organization; 1999. [Accessed April 6, 2015]. (Report no. 99.2.2013-08-22 17:19:23). Available from: http://apps.who.int/iris/handle/10665/66040. [Google Scholar]
- 25.Ministry of Health Malaysia . Management of type 2 diabetes mellitus. Putrajaya, Malaysia: Technology, Health Section, Assessment Division, Medical Development; 2009. [Accessed April 7, 2015]. Available from: http://www.moh.gov.my/attachments/3878.pdf. [Google Scholar]
- 26.American Diabetes Association Standards of medical care in diabetes – 2015. Diabetes Care. 2015;38:S1–S93. doi: 10.2337/dc14-2142. [DOI] [PubMed] [Google Scholar]
- 27.Fisher L, Hessler DM, Polonsky WH, Mullan J. When is diabetes distress clinically meaningful? Establishing cut points for the Diabetes Distress Scale. Diabetes Care. 2012;35:259–264. doi: 10.2337/dc11-1572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sherina MS, Arroll B, Goodyear-Smith F. Criterion validity of the PHQ-9 (Malay version) in a primary care clinic in Malaysia. Med J Malaysia. 2012;67:309–315. [PubMed] [Google Scholar]
- 30.Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens. 2008;10:348–354. doi: 10.1111/j.1751-7176.2008.07572.x. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 31.Al-Qazaz HK, Hassali MA, Shafie AA, Sulaiman SA, Sundram S, Morisky DE. The eight-item Morisky Medication Adherence Scale MMAS: translation and validation of the Malaysian version. Diabetes Res Clin Pract. 2010;90:216–221. doi: 10.1016/j.diabres.2010.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Skevington SM, Lotfy M, O’Connell KA. The World Health Organi-zation’s WHOQOL-BREF quality of life assessment: psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual Life Res. 2004;13:299–310. doi: 10.1023/B:QURE.0000018486.91360.00. [DOI] [PubMed] [Google Scholar]
- 33.Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- 34.van Bastelaar KM, Pouwer F, Geelhoed-Duijvestijn PH, et al. Diabetes-specific emotional distress mediates the association between depressive symptoms and glycaemic control in type 1 and type 2 diabetes. Diabet Med. 2010;27:798–803. doi: 10.1111/j.1464-5491.2010.03025.x. [DOI] [PubMed] [Google Scholar]
- 35.Chew BH, Shariff-Ghazali S, Mastura I, Haniff J, Bujang MA. Age ≥60 years was an independent risk factor for diabetes-related complications despite good control of cardiovascular risk factors in patients with type 2 diabetes mellitus. Exp Gerontol. 2013;48:485–491. doi: 10.1016/j.exger.2013.02.017. [DOI] [PubMed] [Google Scholar]
- 36.Lee PY, Cheong AT, Zaiton A, et al. Does ethnicity contribute to the control of cardiovascular risk factors among patients with type 2 diabetes? Asia Pac J Public Health. 2013;25:316–325. doi: 10.1177/1010539511430521. [DOI] [PubMed] [Google Scholar]
- 37.Chew BH, Cheong AT, Ahmad Z, Mastura I. Men suffer more complications from diabetes than women despite similar glycaemic control and a better cardiovascular risk profile: the ADCM study 2008. J Mens Health. 2012;9:190–197. [Google Scholar]
- 38.Mathew CS, Dominic M, Isaac R, Jacob JJ. Prevalence of depression in consecutive patients with type 2 diabetes mellitus of 5-year duration and its impact on glycemic control. Indian J Endocrinol Metab. 2012;16:764–768. doi: 10.4103/2230-8210.100671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tsujii S, Hayashino Y, Ishii H. Diabetes distress, but not depressive symptoms, is associated with glycaemic control among Japanese patients with type 2 diabetes: Diabetes Distress and Care Registry at Tenri (DDCRT 1) Diabet Med. 2012;29:1451–1455. doi: 10.1111/j.1464-5491.2012.03647.x. [DOI] [PubMed] [Google Scholar]
- 40.Chew BH, Mastura I, Shariff-Ghazali S, et al. Determinants of uncontrolled hypertension in adult type 2 diabetes mellitus: an analysis of the Malaysian Diabetes Registry 2009. Cardiovasc Diabetol. 2012;11:54. doi: 10.1186/1475-2840-11-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McSharry J, Moss-Morris R, Kendrick T. Illness perceptions and glycaemic control in diabetes: a systematic review with meta-analysis. Diabet Med. 2011;28:1300–1310. doi: 10.1111/j.1464-5491.2011.03298.x. [DOI] [PubMed] [Google Scholar]
- 42.Tsiga E, Panagopoulou E, Sevdalis N, Montgomery A, Benos A. The influence of time pressure on adherence to guidelines in primary care: an experimental study. BMJ Open. 2013;3:pii e002700. doi: 10.1136/bmjopen-2013-002700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hajos TR, Polonsky WH, Twisk JW, Dain MP, Snoek FJ. Do physicians understand type 2 diabetes patients’ perceptions of seriousness; the emotional impact and needs for care improvement? A cross-national survey. Patient Educ Couns. 2011;85:258–263. doi: 10.1016/j.pec.2010.08.019. [DOI] [PubMed] [Google Scholar]
- 44.Ogbera A, Adeyemi-Doro A. Emotional distress is associated with poor self care in type 2 diabetes mellitus. J Diabetes. 2011;3:348–352. doi: 10.1111/j.1753-0407.2011.00156.x. [DOI] [PubMed] [Google Scholar]
- 45.Zulman DM, Rosland AM, Choi H, Langa KM, Heisler M. The influence of diabetes psychosocial attributes and self-management practices on change in diabetes status. Patient Educ Couns. 2012;87:74–80. doi: 10.1016/j.pec.2011.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Thoolen BJ, de Ridder DT, Bensing JM, Gorter KJ, Rutten GE. Psychological outcomes of patients with screen-detected type 2 diabetes: the influence of time since diagnosis and treatment intensity. Diabetes Care. 2006;29:2257–2262. doi: 10.2337/dc06-0617. [DOI] [PubMed] [Google Scholar]
- 47.Pandit AU, Bailey SC, Curtis LM, et al. Disease-related distress, self-care and clinical outcomes among low-income patients with diabetes. J Epidemiol Community Health. 2014;68:557–564. doi: 10.1136/jech-2013-203063. [DOI] [PubMed] [Google Scholar]
- 48.Lasaite L, Lasiene J, Kazanavicius G, Gostautas A. Associations of emotional state and quality of life with lipid concentration, duration of the disease, and the way of treating the disease in persons with type 2 diabetes mellitus. Medicina (Kaunas) 2009;45:85–94. Lithuanian. [PubMed] [Google Scholar]
- 49.Lloyd C, Smith J, Weinger K. Stress and diabetes: a review of the links. Diabetes Spectrum. 2005;18:121–127. [Google Scholar]
- 50.Beverly EA, Ganda OP, Ritholz MD, et al. Look who’s (not) talking: diabetic patients’ willingness to discuss self-care with physicians. Diabetes Care. 2012;35:1466–1472. doi: 10.2337/dc11-2422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Golden SH, Lazo M, Carnethon M, et al. Examining a bidirectional association between depressive symptoms and diabetes. JAMA. 2008;299:2751–2759. doi: 10.1001/jama.299.23.2751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ahola AJ, Groop PH. Barriers to self-management of diabetes. Diabet Med. 2013;30:413–420. doi: 10.1111/dme.12105. [DOI] [PubMed] [Google Scholar]
- 53.Bailey CJ, Kodack M. Patient adherence to medication requirements for therapy of type 2 diabetes. Int J Clin Pract. 2011;65:314–322. doi: 10.1111/j.1742-1241.2010.02544.x. [DOI] [PubMed] [Google Scholar]
- 54.Asche C, LaFleur J, Conner C. A review of diabetes treatment adherence and the association with clinical and economic outcomes. Clin Ther. 2011;33:74–109. doi: 10.1016/j.clinthera.2011.01.019. [DOI] [PubMed] [Google Scholar]
- 55.Tan MY, Magarey J. Self-care practices of Malaysian adults with diabetes and sub-optimal glycaemic control. Patient Educ Couns. 2008;72:252–267. doi: 10.1016/j.pec.2008.03.017. [DOI] [PubMed] [Google Scholar]
- 56.Carper MM, Traeger L, Gonzalez JS, Wexler DJ, Psaros C, Safren SA. The differential associations of depression and diabetes distress with quality of life domains in type 2 diabetes. J Behav Med. 2014;37:501–510. doi: 10.1007/s10865-013-9505-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kiadaliri AA, Najafi B, Mirmalek-Sani M. Quality of life in people with diabetes: a systematic review of studies in Iran. J Diabetes Metab Disord. 2013;12:54. doi: 10.1186/2251-6581-12-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wandell PE. Quality of life of patients with diabetes mellitus. An overview of research in primary health care in the Nordic countries. Scand J Prim Health Care. 2005;23:68–74. doi: 10.1080/02813430510015296. [DOI] [PubMed] [Google Scholar]
- 59.Papadopoulos AA, Kontodimopoulos N, Frydas A, Ikonomakis E, Niakas D. Predictors of health-related quality of life in type II diabetic patients in Greece. BMC Public Health. 2007;7:186. doi: 10.1186/1471-2458-7-186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ventegodt S, Omar HA, Merrick J. Quality of life as medicine: interventions that induce salutogenesis. A review of the literature. Soc Indic Res. 2011;100:415–433. [Google Scholar]
- 61.Non-Communicable Disease Section, Disease Control Division, Department of Public Health National Diabetes Registry Report, Volume 1:1: 2009-20122013. [Accessed April 7, 2015]. Available from: file:///C:/Users/susan/Downloads/National_Diabetes_Registry_Report_Vol_1_2009_2012.pdf.


