Abstract
Purpose
There is evidence that the management of chronic non-cancer pain (CNCP) in primary care is far from being optimal. A 1-day workshop was held to explore the perceptions of key actors regarding the challenges and priority interventions to improve CNCP management in primary care.
Methods
Using the Chronic Care Model as a conceptual framework, physicians (n=6), pharmacists (n=6), nurses (n=6), physiotherapists (n=6), psychologists (n=6), pain specialists (n=6), patients (n=3), family members (n=3), decision makers and managers (n=4), and pain researchers (n=7) took part in seven focus groups and five nominal groups.
Results
Challenges identified in focus group discussions were related to five dimensions: knowledge gap, “work in silos”, lack of awareness that CNCP represents an important clinical problem, difficulties in access to health professionals and services, and patient empowerment needs. Based on the nominal group discussions, the following priority interventions were identified: interdisciplinary continuing education, interdisciplinary treatment approach, regional expert leadership, creation and definition of care paths, and patient education programs.
Conclusion
Barriers to optimal management of CNCP in primary care are numerous. Improving its management cannot be envisioned without considering multifaceted interventions targeting several dimensions of the Chronic Care Model and focusing on both clinicians and patients.
Keywords: chronic pain, community-based participatory research, health service accessibility, patient-centered care, primary health care
Introduction
In Canada, approximately 25% of the population suffers from chronic non-cancer pain (CNCP).1 This disorder is associated with anxiety, depression, reduced productivity, and increased health care costs.1–5 Patient satisfaction regarding treatment efficacy and information on treatment is low.6 Current clinical guidelines for CNCP recommend multifaceted interventions delivered by various health professionals, including primary care physicians, pharmacists, nurses, physiotherapists, kinesiologists, and psychologists.7–11 Recent studies indicate chronic pain is often undertreated, and management practices do not always conform to current practice guidelines.12–18
Considering CNCP as a chronic disease, its management could be addressed through the use of the Chronic Care Model (CCM),19 a multi-dimensional guide to designing effective chronic care.20 The CCM recommends building chronic health care based on six dimensions, namely: 1) self-management support; 2) delivery system design; 3) decision support; 4) clinical information systems; 5) community resources and policies; and 6) health care organization. Positive effects on care processes and clinical outcomes of CCM-based interventions have been reported.21,22 However, the CCM is a general model, each dimension can be addressed in several alternative ways, and there is no evidence-based algorithm to determine how to prioritize and translate these elements into specific interventions adapted to a particular clinical context. To our knowledge, the CCM has also never been explicitly used to specifically improve CNCP management in primary care.19
When designing knowledge translation interventions based on practice guidelines, it is recommended to address the specific challenges and the context of care.23 Participatory research approaches involving primary care actors have also been recommended to learn about potential challenges to optimal disease management.24,25 These approaches could thus be used to translate CCM dimensions and practice guidelines into interventions that meet the needs of patients and family members, are appropriate to the context of primary care, and appeal to clinicians. A participatory workshop has previously been used to identify challenges of and priority interventions inspired by the CCM for improving cardiovascular disease prevention in primary care.25
We therefore organized a 1-day workshop involving members of the primary care and pain management community, including patients and family members, with the objective to identify challenges to optimal CNCP management, as posited by the CCM, and to identify priority interventions to improve its management in primary care. In this article, we report the results of this participatory workshop. These results will be used to develop and assess an intervention program in primary care, as part of a broader research program aiming at improving the management of CNCP – ie, the program ACCORD.
Methods
Participant recruitment and sampling
Physicians (n=6); pharmacists (n=6); nurses (n=6); physiotherapists (n=6); psychologists (n=6); pain specialists (n=6); patients (n=3); family members (n=3); decision makers and managers (n=4); and pain researchers (n=7) were recruited to participate in a 1-day workshop held in Laval, Quebec, Canada, on April 30, 2010. Pain specialists included one physician, one psychologist, one nurse, one pharmacist, one kinesiologist, and one physiotherapist, all of them being actively involved in following patients with CNCP in the primary sector of care. All the participants (total =53) were purposively selected, based on their general experience in primary care and chronic pain. Participants of each category were recruited to represent diverse contexts of care in various regions of the Province of Quebec (Montréal, Laval, Mauricie, Montérégie, Lanaudière, and Laurentides) and clinical settings (family medicine groups, conventional medical clinics, family medicine units, and local community service centers) through the Réseau universitaire intégré de santé (RUIS) of the Université de Montréal. Decision makers and managers working within a health and social services center (Centre de santé et de services sociaux, CSSS) or a health and social services agency (Agence de la santé et des services sociaux, ASSS) were selected based on their role and active involvement in health care organization. Pain researchers were selected by the principal investigators and co-investigators. We partnered with the Quebec Association for Chronic Pain (Association québécoise de douleur chronique) and Quebec Federation of Seniors (Fédération de l’âge d’or du Québec) to recruit patients and family members. In addition, clinicians could also refer their eligible patients for participation in this study. Patients recruited met with six inclusion criteria: 1) be 18 years or older; 2) reported CNCP for at least 6 months; 3) felt pain at least twice a week; 4) reported an average pain intensity in the past 7 days of at least 4 on a 0–10 intensity numerical scale (0= no pain; 10= the worst possible pain);26 5) had an active prescription from a primary care physician for one or more pain medication; and 6) spoke and understood French. Patients were excluded if they met any of the following criteria: 1) suffered cancer-related pain; 2) reported having only migraines or chronic headaches; or 3) had a disabling physical or mental disorder that prevented giving informed consent and/or active participation in the workshop.
This participatory research was approved by the Research Ethics Committee of the Centre de santé et de services sociaux de Laval. All participants signed an informed consent form. A CAD $500 financial compensation was offered to all participants except researchers, decision makers and managers. Transportation and hotel accommodation were paid for participants from outside Montreal.
Workshop
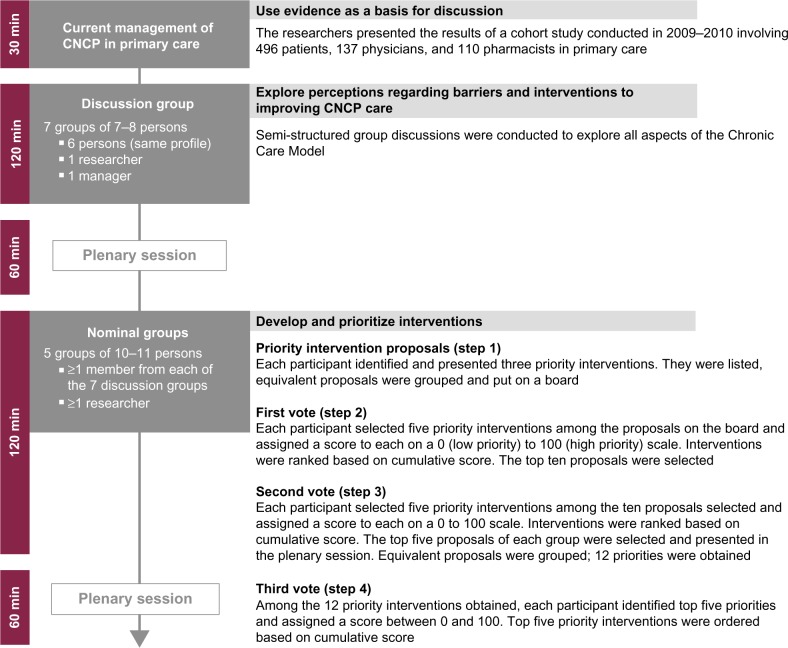
The workshop included three sets of activities: 1) presentation of the current management strategies in primary care; 2) focus group discussions; and 3) nominal group discussions.27 The workshop schedule and descriptions of activities are shown in Figure 1. The composition of the focus and nominal groups was predetermined by pain researchers, based on participant expertise and experience. All discussions were audio-recorded and were conducted by qualitative-research professionals from the Ad hoc Research firm who acted as facilitators.
Figure 1.
Workshop schedule and descriptions of activities.
Abbreviations: min, minutes; CNCP, chronic non-cancer pain.
Presentation of the current management strategies of CNCP in primary care
All participants attended a 30-minute presentation summarizing the results of a cohort study, performed in primary care in Quebec during Phase I of the program ACCORD.6,28,29 The presentation emphasized complexity of the health profile of patients followed-up in primary care for chronic pain, practice gaps, as well as the relatively low level of pain knowledge, inappropriate attitudes and beliefs of clinicians regarding CNCP, and low levels of patient satisfaction. Physical, psychosocial, and economic impacts of chronic pain were also evidenced. In addition, participants were provided with two clinical vignettes describing typical primary care CNCP patients (Supplementary material). They were asked to keep in mind the above results and these two clinical vignettes throughout the rest of the workshop.
Focus group discussions
A total of seven parallel focus groups were conducted. Each group included a decision maker, a researcher, and six other participants from the same discipline (eg, primary care physicians) or profile (eg, patients). The homogenous grouping of participants allowed them to voice innovative suggestions for interventions pertaining to their own clinical practice or experience. Within each CCM-related domain, participants were asked to: 1) indicate what they perceived as the most important challenges in CNCP management; and 2) propose specific interventions or practice changes to improve CNCP management. Organization of care and services delivery had to be discussed first in all groups. For each group, pain researchers purposively pre-selected and pre-assigned two additional CCM-related domains for discussion, taking into consideration participant preference and expertise (Table 1). Participants were provided with a list of possible interventions for the two clinical vignettes corresponding to each CCM domain. In a plenary session, each facilitator summarized the discussed challenges and proposed interventions.
Table 1.
Order of domains of the Chronic Care Model discussed in each focus group
| Focus group | Delivery system design | Decision support | Clinical information systems | Self-management support | Community resources and policies |
|---|---|---|---|---|---|
| Physicians | 1st | 2nd | 3rd | ||
| Pharmacists | 1st | 2nd | 3rd | ||
| Nurses | 1st | 3rd | 2nd | ||
| Physiotherapists | 1st | 3rd | 2nd | ||
| Psychologists | 1st | 3rd | 2nd | ||
| Pain specialists | 1st | 2nd | 3rd | ||
| Patients and family members | 1st | 2nd | 3rd |
Nominal group discussions
Five nominal groups, each including all types of participants, were formed to identify priority interventions to improve the management of CNCP. Nominal groups went through a four step process (Figure 1). Steps 1 to 3 were conducted within each of the five nominal groups while step 4 involved all participants in a plenary session. Step 1 – priority intervention proposals: all participants were asked to select three interventions and order them in terms of priority. The facilitator listed all the collected interventions on a large board, and led discussions with the participants to pool similar interventions and clarify them if needed. Step 2 – first vote: each participant had to select five priority interventions from the list and scored them by distributing 100 points according to their importance. An intervention could be given 0 to 100 points by each participant (0= not important, 100= very important). The total number of points distributed by each participant could not exceed 100. Facilitator calculated the “total score” of each intervention – ie, the sum of all points all participants had given to an intervention. The number of “votes” for each intervention was also calculated. A top ten list of interventions was made based on the total score. In order to have an understanding of the justification of the scores and votes, participants were asked to voice their opinion on the list and explain their rating. Step 3 – second vote: participants were asked to select five priority interventions in the previous top ten list, and to distribute 100 points according to their relative importance. The facilitator calculated total scores and votes, and listed top five interventions based on total score. Step 4 – third vote: in a plenary session, each facilitator (acting as representative of the five nominal groups) presented their top five interventions to all participants. Interventions from all five nominal groups were pooled together, and equivalent interventions were merged. At the end of the process, there were 12 single interventions. For the last time, all participants were asked to rate five priority interventions among the 12, by distributing 100 points to those five interventions. The total score and number of votes of each priority intervention were calculated.
Analyses
Focus group discussions at step 1, intervention proposals, scores and votes made in each nominal group at step 2, the five priority interventions selected in each nominal group at step 3, and the results of step 4 were summarized. Priorities identified in step 4, were classified by researchers in broader themes. Thereafter, thematic qualitative analyses30 were done manually. Priorities were retrospectively used to thematically review the nominal and focus group audio-recordings to gain a better understanding of the reasons for which those priorities were selected.
Results
Participation of the primary care community
As mentioned earlier, 53 members of the primary care community (clinicians, managers, patients, family members, and researchers) took part in this participatory research. Table 2 describes their respective background, the region they came from, and the work environment of the health care professionals and managers. All participants attended the initial presentation and participated in the focus and nominal groups.
Table 2.
Participants’ characteristics
| Physicians | Pharmacists | Nurses | Physiotherapists | Psychologists | Pain specialists | Patients | Family members | Decision makers | Pain researchers | |
|---|---|---|---|---|---|---|---|---|---|---|
| Number (n) | 6 | 6 | 6 | 6 | 6 | 6 | 3 | 3 | 4 | 7 |
| Sex, women, n (%) | 3(50) | 5(83) | 6(100) | 1(17) | 5(83) | 5(83) | 2(67) | 2(67) | 1(25) | 6(86) |
| Practice type (n) | ||||||||||
| Medical clinic | 3 | – | 2 | – | – | – | – | – | – | – |
| GMF/UMF | 2 | 3 | 2 | – | – | – | – | – | – | – |
| CLSC | – | – | – | – | 1 | – | – | – | – | – |
| Hospitals | 1 | – | – | 2 | 4 | 6 | – | – | – | – |
| Private clinics | – | – | – | 4 | 1 | – | – | – | – | – |
| Pharmacies | – | 2 | 1 | – | – | – | – | – | – | – |
| Pharmaceutics | – | 1 | 1 | – | – | – | – | – | – | – |
| Ministry of health | – | – | – | – | – | – | – | – | 1 | – |
| Health agency | – | – | – | – | – | – | – | – | 3 | – |
| Region (n) | ||||||||||
| 03 – Capitale Nationale (Quebec) | – | – | – | 1 | – | – | – | – | 2 | – |
| 04 – Mauricie | – | – | 1 | – | – | – | – | – | – | – |
| 05 – Estrie | 1 | – | – | – | 2 | 2 | – | – | 1 | 1 |
| 06 – Montreal | 2 | 2 | 2 | 4 | 1 | 4 | 2 | 1 | – | 5 |
| 08 – Abitibi-Témiscamingue | – | – | – | – | – | – | – | – | – | 1 |
| 11 – Gaspésie-îles-de-la-Madeleine | – | 1 | 1 | – | – | – | – | – | 1 | – |
| 12 – Chaudière-Appalaches | – | – | – | – | 1 | – | – | – | – | – |
| 13 – Laval | – | 3 | 2 | – | – | – | 1 | 2 | – | – |
| 15 – Laurentides | – | – | – | 1 | 1 | – | – | – | – | – |
| 16 – Montérégie | 3 | – | – | – | 1 | – | – | – | – | – |
Abbreviations: CLSC, Centre local de services communautaires (local community services center); GMF/UMF, Groupe de médecine familiale/Unité de médecine familiale (family medicine group/family medicine unit).
Challenges to pain management in primary care
In focus group discussions, participants identified challenges related to five dimensions: 1) knowledge gap; 2) “work in silos”; 3) lack of awareness that CNCP represents an important clinical problem; 4) difficulties in access to health professionals and services; and 5) patient empowerment needs. The right panel of Table 3 shows illustrative quotes for each dimension.
Table 3.
Challenges in the management of chronic non-cancer pain in primary care, grouped by dimension, with illustrative participants’ quotes for each dimension
| Dimension | Quotes |
|---|---|
| Knowledge gap | |
| Poor knowledge and lack of training on pain Lack of valid assessment tools Lack of clear treatment protocol |
“Primary care does not understand what specialists ask, and patient is caught in this mess.” [Pain specialist] “Physicians are not aware of chronic pain because it is unfamiliar to them and because they don’t have the knowledge; they seem uncomfortable and helpless. The question of training is in my opinion a key element that should be further developed in primary care.” [Researcher] “There are very good screening questionnaires, but people don’t know about them.” [Nurse] “There are [treatment protocols], but they are not well known. The college [of physicians] produced three documents on chronic pain in the last 4–5 years. When you look at the appendices, many could definitely be used, and people don’t use them.” [Primary care physician] |
| “Work in silos” | |
| Lack of time and resources for physicians Lack of communication Difficulties in managing the medical record |
“The main obstacle for me is [lack of] time and isolation. I feel alone working in my office and caring for those patients. Lack of connections with everything: tools, community network, professional network, other physicians.” [Primary care physician] “There is no one linking with family physician, like a care manager, informing patient, coordinating patient care.” [Pain specialist] “I find the multidimensional aspect that comes with chronic pain is not addressed. Following-up on chronic pain cases in private practice is, for me all alone, extremely difficult.” [Psychologist] “It takes a shared electronic file, including the list of medications that have been tried, with failures and secondary effects, to prevent repeating errors. It would also help physicians.” [Nurse] “For the pharmacists to really do their job, they need to have access to diagnoses, laboratory results, and intentions to treat.” [Pharmacist] “I think the problem is record management […] Either we don’t do it, or we don’t do it adequately.” [Primary care physician] |
| Lack of awareness regarding chronic non-cancer pain | |
| Little or no societal and clinical recognition of pain as a disease | “For many people who do not have chronic pain, the concept of chronic pain is something quite cranky. It is not science. I think perceptions of it are blurred, unproven, unaccepted. We feel it is untrue: those people are not truly suffering. And that’s what patients tell us, they are not believed.” [Primary care physician] “We don’t like to spend time assessing pain: it takes long and it is boring hearing someone in your office saying ‘Oh, I don’t sleep well, and I am not able to do this and that […]’, etc.” [Nurse] |
| Difficulties in access to health professionals and services | |
| Lack of care paths Lack of information on resources |
“Getting to see a specialist takes time. And you see your husband suffering – he can’t be sitting for long. And seeing him suffering, he’s chronic, it’s been going on for a long time.” [Family member] “What is difficult for us, when we need expertise, we can’t access. When we want to send the patients to an expert or to a team who can make an assessment – because we have tried many things we thought could help, and they didn’t work, we haven’t access.” [Primary care physician] |
| Patient empowerment needs | |
| Patient isolation Lack of community resources Lack of awareness of existing community resources |
“Last week, I read an article on fibromyalgia. It was such a relief to read about a public people with a context of chronic pain. It was comforting because I was feeling like I am not alone on this planet.” [Patient] “We have just talked about support and isolation. Well, I think it is the case. There is a need to get together, and not to feel all alone.” [Psychologist] “We have to give patients a sense of being in control again.” [Nurse] “I often realize when patients come to the pain clinic that no one has taken time to explain many things, occupational therapy, posture, self-management of medications. And they are waiting for someone to save them.” [Physiotherapist] |
Participants reported a knowledge gap in CNCP in primary care due to a lack of clinician training and continuing education and of supportive tools to assess and treat CNCP in primary care. Difficulties to organize interdisciplinary care in current clinical settings were also reported. Some participants believed practice guidelines are missing for CNCP management. However, some participants pointed out that such guidelines and tools do exist but many health care professionals have a limited knowledge of them. One more challenge to CNCP management is “work in silos” where clinicians feel isolated and unsupported. The situation is exacerbated by poorly implemented clinical information systems and the absence of feedback on patient follow-up by other health professionals.
The results also showed that there was a lack of awareness of CNCP as an important clinical problem among clinicians. Pain is difficult to diagnose, and there is a perception that the definitions and causes of various types of chronic pain are blurred or unproven. Providing care to patients with chronic pain is time consuming, and there is also a suspicion that patients may fake or exaggerate their pain.
The participants further reported that many difficulties in access to health professionals and services, and to community resources are due to the lack of clearly defined care paths and limited information on available resources like pain specialists and multidisciplinary pain treatment clinics. In addition, clinicians are unaware of community resources for pain management. Finally, patients continue to be viewed (or view themselves) as care consumers rather than active partners in their treatment. Patients’ empowerment needs are not addressed, and many of them are unaware of basic self-management strategies that could contribute to improve their pain. Furthermore, available health care facilities and community resources are often unknown to the patients and their family members. As a result, patients feel isolated, helpless, and out of control.
Priority interventions for better pain management in primary care
Table 4 shows the 12 priority interventions selected by all nominal groups. Interventions are classified in six themes. Under each theme, interventions are ordered by total score and by number of votes obtained in the final plenary session. An illustrative quote for each priority intervention is provided on the right panel.
Table 4.
Priority interventions identified grouped by intervention theme, with total score, votes and illustrative participant’s quote for each priority intervention
| Intervention themes | Total score (votes) | Quotes |
|---|---|---|
| Interdisciplinary continuing education | ||
| Provide multidisciplinary clinical teams with uniform, standardized continuing education program on chronic non-cancer pain (CNCP) (eg, know-how, skills) | 991 (37) | “Training must address how we work together, what teamwork is and who will take the lead over the intervention. After that, the role of each individual.” [Primary care physician] |
| Provide standardized tools for synthesis and follow-up to be filled out by clinicians and patients to consistently transfer information in a shared language | 775 (37) | “We need an interdisciplinary electronic record, accessible to diverse clinicians, interfaced.” [Pharmacist] “When patient would forget pain logbook, it would be no problem, it would be computerized.” [Pharmacist] |
| Enhance clinical expertise by providing a bank of information shared with all clinicians and patients (eg, website) | 291 (19) | “We should have an electronic decision-support tool; 1 can’t believe we are starting again to look in the books. We need an e-library, if you’re querying arthritis, you have the latest guidelines, tools for patients etc.” [Nurse] |
| Interdisciplinary approach | ||
| Train care managers in pain management | 442 (22) | “There should be pain management nurses in primary care. We should be able to intervene more efficaciously, and we should also involve and educate patients, remind them, and check for secondary effects.” [Nurse] |
| Develop an accessible and affordable approach to interdisciplinary collaboration | 330(18) | “Quite often, when physicians practice in silos, they let go those patients. It goes a lot better when physicians do interdisciplinary practice, we share the follow-up of patients with multiple challenges, and thus it frees up physician time.” [Nurse] |
| Widen the range of professional responsibility of clinicians (other than the physician) to overcome bottlenecks and increase efficiency | 313 (16) | “Shared care, physiotherapist should be able to prescribe radiographies, and certain anti-inflammatory medications. Bill 90 allows nurses to do many things.” [Physiotherapist] |
| Perform psychosocial assessment at the moment chronic pain is diagnosed | 125(6) | “There should be a psychosocial assessment. It would allow orienting […] because psychosocial events often taint patient’s reaction to treatment or to events.” [Psychologist] |
| Regional expert | ||
| Identify regional experts and train them to disseminate information and support clinicians | 551 (30) | “Just like we did in palliative care, we appointed a regional physician in charge, who takes on regional leadership. He reaches for expertise. There has to be regional leadership instead of saying ‘the Health Agency will do it’. The Health Agency is no one, it’s a building.” [Primary care physician] |
| Care path | ||
| Define roles and responsibilities of primary, secondary, and tertiary care and establish care paths to improve access to specialized resources in CNCP treatment | 599 (25) | “Service corridors must be made between two departments, and be supported by both Health Agencies that have come to sit and listen to each other. One receives, one refers, and one refers back, so there must be agreements between departments.” [Primary care physician] |
| Self-care support | ||
| Promote the active participation of patients in their treatment through education adapted to their needs (eg, aggravating factors, self-management of pain, alternative therapies) | 312(16) | “I answer [other patients’] emails. I tell them they must not stay in bed, they must continue exercise, see their doctor, and we don’t speak of curing chronic pain, we speak of soothing. The objectives must not be too high, and we still must have objectives. And you have to go smoothly with exercising so that people don’t opt out.” [Patient] |
| Establish a paper or web logbook for patients and clinicians | 272(17) | “They are given digital instruments. They fill out a logbook of their day and their medication use. I cannot work without the patient.” [Primary care physician] |
| Specific guideline | ||
| Systematically assess pain as the fifth vital sign | 30(2) | “People speak a lot of the four vital signs and in my opinion there should be five: pain is the fifth … Then it would be important to formalize it and to have a systematic assessment model.” [Nurse] |
Participants recommended developing joint continuing education programs. They should be offered simultaneously to clinicians of various disciplines in order to standardize their knowledge, to get the opportunity to know each other and their respective area of expertise, and to develop a common language. For example, the use of pain scales should be a standard across disciplines to harmonize evaluation and communication of clinical information on pain. Standardized tools such as interdisciplinary electronic records need to be implemented, and clinicians should be trained to use them optimally and appropriately. Clinical expertise should also be enhanced by facilitating patient and clinician access to instruments that are aligned with current clinical guidelines, and by providing electronic decision-support tools.
With regards to the interdisciplinary approach, participants believed primary care nurses should be trained in pain management to support the interdisciplinary approach. It was recommended to widen the range of professional responsibility of clinicians other than the physician to ensure access to and affordability of pain management. Pain diagnoses should be complemented with psychosocial assessments to identify patient needs so as to treat co-morbidities commonly associated with chronic pain (eg, anxiety or depression).
Participants recommended identifying regional pain experts (“champions”) who could disseminate knowledge and bring support to clinicians when needed. Additional training and support need to be offered to these experts on efficient knowledge dissemination strategies and outreach techniques.
Defining care paths in terms of corridors of services across the continuum of care was also recommended. It is a complex process that requires the involvement of primary, secondary, and tertiary care actors to come up with agreements on referral and follow-up modalities.
In order to develop a greater sense of being in control, patients should be involved as active partners in their treatment and taught pain self-management strategies through individual or group education sessions. Patients’ pain-logbook was recommended to support self-monitoring of their disease and improve communication with the different health care professionals.
Discussion
Various types of primary care actors, including patients and family members, took part in this participatory research and contributed to identifying challenges to chronic pain management in primary care along with priority interventions to overcome them. The main challenges included knowledge gap, “work in silos”, lack of awareness regarding chronic pain, difficulties in access to health professionals and services, and to increase patients’ empowerment.
Participants recommended patient-centered interventions aligned with five dimensions of the CCM. To empower patients, it was proposed to promote their active participation in treatment through patient education and to use a paper or web pain-logbook for both patients and clinicians. Improving delivery system design through interdisciplinary collaboration and team work was proposed, to be supported with decision-support tools (eg, standardized evaluation forms, updated guidelines) and clinical information systems (eg, electronic medical records). Interdisciplinary continuing education was also deemed necessary for clinicians to become familiar with use of such tools, and to develop interprofessional collaborative practices in pain management. Taking advantage of the leadership and peer support role of pain experts in the primary care community was also recommended. Participants probably considered that CNCP management need not be addressed by creating new structures in the health system, because they did not suggest any intervention at the level of health care organization.
Awareness and education are keys
While the societal and individual burden of chronic pain is increasingly recognized, the need to provide continuing education on pain management has been emphasized.31 In this research, participants thought credible chronic pain experts should be appointed in each region to take on clinical leadership in order to increase awareness of CNCP and its individual and social burden, to inspire a desire to aim at improving care for patients with CNCP, to disseminate knowledge, and to provide expertise to support other clinicians. A pilot study showed this approach is promising.32
In recent surveys, primary care clinicians demonstrated low levels of knowledge in the field of pain assessment and treatment, and voiced a need for supportive clinical tools and training.14,18 Those findings suggest that clinicians may have inappropriate beliefs on chronic pain, or feel insufficiently knowledgeable or supported to provide appropriate care and services. Participants in this workshop believed that interactive, interdisciplinary, patient-centered, continuing education programs are necessary to fill the knowledge gap, foster mutual acquaintance, develop common discourses among health professionals and thereby, ensure appropriate transmission of information among clinicians. University faculties have developed interdisciplinary education programs, but those programs are usually not available in interdisciplinary continuing education.29,33–35 However, these training programs by themselves are probably insufficient to improve the process, quality and coordination of care, if one wants to improve chronic pain management in primary care.36
Patient empowerment is the overarching priority
While there are prejudices and preconceived ideas about chronic pain and its treatment in the general population and in the health care system as well,37 many patients with CNCP also have erroneous beliefs and judgmental attitudes regarding their disease. Patients may hide their disease and avoid taking pain killers, an attitude they associate with courage and self-control.38,39 Others constantly look for the “magic” pill or treatment while it is well established that a combination of therapeutic modalities is more likely to be successful. Patient education programs along with provision of self-management strategies are needed to empower patients and thereby confer on them a role of active partner in their treatment rather than simply a consumer of care.
Interdisciplinary collaboration is necessary for better care
It is generally thought that increasing interdisciplinary collaboration will suppress useless intermediary steps, and will improve care. The efficacy of nurse-led pain management in primary care has been demonstrated.40 A study suggests pharmacist-nurse collaboration in chronic pain management could improve patient outcomes and experience, and optimize resource use.41 Pharmacist-led interventions (eg, medication review) are promising and more research is needed to support expanding roles for pharmacists in pain management.42 Psychologist-physician collaboration is modestly but significantly more efficient for CNCP management than usual care.43 Timely referrals to consultations for back and neck pain with physiotherapist, chiropractor, or osteopath improve patient self-management and satisfaction, and allow reduction of medication and primary care consultations.44 Interdisciplinary collaboration requires increasing professional autonomy of non-physician clinicians and redefining their roles in consultation with physicians, other clinicians, and health authorities concerned, which currently are major issues in health care policy in Canada.45 Participants in this study recommended the use of clinical tools such as collective prescriptions to support interprofessional collaboration.
Partnerships are essential to ensure access to care
Access to and waiting time for consultation in multidisciplinary pain treatment clinics are problematic in Canada.46 Median waiting time in Canada is 6 months (ranging from 2 to 14) in 2007.46 A study involving more than 700 patients on waitlists of large university-affiliated pain clinics across Canada has highlighted the severe impairment these patients experience in terms of pain intensity and interference, psychological distress (depression and suicidal ideation, anxiety, anger), and poor quality of life.47 The economic burden of chronic pain has also been shown to be substantial in patients on waitlists of multidisciplinary pain clinics. The mean monthly cost has been estimated at CAD $3,112 per patient.48 Deficient interdisciplinary communication across the continuum of care may explain a part of problems experienced with patient referrals and prioritization along with delayed treatments.49
In 2009, as an attempt to solve this problem and help lift the burden of CNCP, the Quebec Health Ministry designated four Pain Centers of Expertise (PCE) across the province with the mandate of improving the management of chronic pain by implementing an integrated and hierarchical continuum of services. Each PCE includes: 1) one or more tertiary care multidisciplinary pain treatment clinic affiliated with one tertiary care rehabilitation center; 2) designated regional secondary pain clinics; and 3) designated local primary care clinics. A series of corridors of services covering the three sectors of care have been or are in the process of being established within each PCE. In addition, a provincial committee involving the PCE medical directors, their coordinators, clinicians, managers, and decision makers of the Health Ministry is mandated to develop common and uniform strategies to improve accessibility, continuity, complementarity, and quality across all sectors of care as well as to reduce variability in the clinical practices and improve process management. These initiatives include: 1) implementation of standardized consultation forms; 2) provision of evidence-based practice guidelines for the treatment of various types of CNCP syndromes and patient clinical pathways across the continuum of care; 3) provision of a formal telephone consultation service for family physicians who wish to discuss cases with pain specialists; 4) production of a patient health care booklet; 5) directory of pain self-management programs available in the community; and 6) introduction of new communication tools including the creation of intranet websites.
Qualitative and participatory methods: strengths and limitations
Our conclusions are compatible with those of another participatory research study on CNCP management in primary care where implementing treatment guidelines and clinical tools, improving processes for opioid prescription renewals, enhancing patient self-management, and involving care managers in primary settings were recommended.19 However, that study used a Delphi method and involved only physicians and care managers. In contrast, we used focus and nominal group discussions to involve a broader range of actors concerned with chronic pain management in primary care with the aim of developing an intervention for CNCP management inspired by the CCM and adapted to the context of this sector of care. We were able to have participants from ten of 17 of Quebec’s administrative regions, in rural and urban areas.
In focus group discussions, participants could share their views with peers. The inclusion of patients and family members in mixed, balanced, facilitated, and non-judgmental nominal groups of primary care actors is an innovative aspect of our research. Nominal group discussions allowed participants to make and be exposed to a wide range of creative proposals, and then select the most relevant by voting on and ranking proposed interventions. The nominal group technique is generally seen as unthreatening and depersonalized,27 and is therefore suitable to raise the expression of minority opinions. Participants had multiple occasions to hear suggestions and arguments put forward by other members of the groups, and thus elaborate a critical reconsideration of their initial views. Nevertheless, the findings of this qualitative and participatory research are context-bound and participants were purposively selected and may not be representative of the entire population. Results must be interpreted in the context of the primary care experienced in Quebec, Canada.
Conclusion
Lack of awareness that CNCP constitutes an important clinical problem coupled with the presence of knowledge gaps in the assessment and management of this type of disorder represent major barriers to the establishment of interdisciplinary collaboration and patient-centered shared care. Pain education needs of both patients and clinicians must therefore be addressed. For carers, interdisciplinary training should help in developing common basic knowledge and shared language that will allow them to provide patients with appropriate treatment. Teaching self-management strategies to patients is crucial to emphasize the importance of optimal self-care, increase empowerment, and make them active partners within the clinical team. These results may constitute a starting point toward the development and implementation of new policies for the management of chronic pain patients in primary care and are of wide interest not only for the community but also for all the health professionals dealing with these patients.
Supplementary material
| Clinical vignette 1 | Clinical vignette 2 |
|---|---|
| Mrs Collette Comeau, aged 45, is married and has a full-time position as a medical archivist. She has two children, aged 8 and 12. Her husband is a pharmaceutical representative and has to spend many days a week away from home. Mrs Comeau has been suffering from fibromyalgia for 20 years. Pains spread over her whole body; they appeared without any precise causal event. She suffers from pains every day. On a scale from 0 to 10 where 0 represents “no pain” and 10 represents the “worst possible pain”, her average pain level is about 5 and varies from 0 to 7 depending on the time of day; it is weaker in the morning and increases throughout the day. Her pains considerably disturb her sleeping, and wake her up suddenly almost every night. Her pains interfere with her daily activities. She is often irritable, which interferes with her relationships with others. At work, she is not always fully efficacious, and she stays home about 10 days a year. She often refuses to participate in social and entertainment activities because of her pain. Mrs Comeau wants to remain independent. She often hesitates to ask for help. She does not believe she has power over her pain. Still, she believes her medication helps and medicine could perhaps one day completely relieve her pain. |
Mr Jacques Levasseur, aged 68, is widowed and retired. He lives alone at home. He has three children and seven grandchildren who occasionally come to visit him. He suffers from arthritis for 10 years already. His pain is in all his joints, in particular in his knees. Although he always feels some pain (about 2 on a scale of 0 to 10), pain is not constant. Many times a week, pain becomes very acute, up to 9. His pain particularly interferes with walking and doing house-keeping tasks. Pain often prevents his sleeping and makes him sullen. His sudden mood swings affect his relationships with others. He often refuses to participate in social activities. Before pain appeared, he loved to play golf. Now, he does not dare play anymore, because he is afraid pain will worsen if he walks much. Mr Levasseur has little hope of one day being totally relieved. He often feels helpless, and useless. |
| Medical history | Medical history |
| ➢ Pain control strategies ○ Psychotherapy, several years ago ○ Distraction techniques a few times a week ○ Yoga twice a week ➢ Medical follow-up ○ Family physician ○ Not followed-up by a specialist physician ○ No consultations for physiotherapy, ergotherapy, massotherapy, or chiropractic ➢ Medications ○ Herbal tea for constipation ○ Antiemetic medication (against nausea) ○ Anti-acid medication (against heartburn) ○ Fentanyl patches (75 μg every 2 days) and 150 mg of pregabalin every day |
➢ Pain control strategies ○ Relaxation techniques ➢ Medical follow-up ○ Family physician ○ Has already consulted physiotherapists, occupational therapists, chiropractors, and osteopaths, without success ➢ Medications ○ Acetaminophen a few times a week ○ Muscle relaxant ○ Anti-inflammatory medication (Celebrex 200 mg) |
Footnotes
Research funding
Canadian Institutes of Health Research (CIHR) in partnership with AstraZeneca, Pfizer Canada Inc., Janssen-Ortho, Merck Frost Canada Ltd, and Purdue Pharma.
Disclosure
Marie-Claude Laliberté is an employee of AbbVie Corporation and owns AbbVie shares. At the time of analysis, she was a PhD student in pharmaceutical sciences at Université de Montréal. The other authors have no conflicts of interest to declare.
References
- 1.Boulanger A, Clark AJ, Squire P, Cui E, Horbay GL. Chronic pain in Canada: have we improved our management of chronic noncancer pain? Pain Res Manag. 2007;12(1):39–47. doi: 10.1155/2007/762180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reed C, Hong J, Novick D, Lenox-Smith A, Happich M. Health care costs before and after diagnosis of depression in patients with unexplained pain: a retrospective cohort study using the United Kingdom General Practice Research Database. Clinicoecon Outcomes Res. 2013;5:37–47. doi: 10.2147/ceor.s38323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Watson L, Baird J, Hosel V, Peveler R. The effect of concurrent pain on the management of patients with depression: an analysis of NHS healthcare resource utilisation using the GPRD database. Int J Clin Pract. 2009;63(5):698–706. doi: 10.1111/j.1742-1241.2009.02017.x. [DOI] [PubMed] [Google Scholar]
- 4.Gureje O, Von Korff M, Simon GE, Gater R. Persistent pain and well-being: a World Health Organization Study in Primary Care. JAMA. 1998;280(2):147–151. doi: 10.1001/jama.280.2.147. [DOI] [PubMed] [Google Scholar]
- 5.Rashiq S, Dick BD. Factors associated with chronic noncancer pain in the Canadian population. Pain Res Manag. 2009;14(6):454–460. doi: 10.1155/2009/919628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jouini G, Choiniere M, Martin E, et al. Pharmacotherapeutic management of chronic noncancer pain in primary care: lessons for pharmacists. J Pain Res. 2014;7:163–173. doi: 10.2147/JPR.S56884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chou R, Fanciullo GJ, Fine PG, et al. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain. 2009;10(2):113–130. doi: 10.1016/j.jpain.2008.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chou R, Qaseem A, Snow V, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147(7):478–491. doi: 10.7326/0003-4819-147-7-200710020-00006. [DOI] [PubMed] [Google Scholar]
- 9.Williams NH, Amoakwa E, Burton K, et al. The Hip and Knee Book: developing an active management booklet for hip and knee osteoarthritis. Br J Gen Pract. 2010;60(571):64–82. doi: 10.3399/bjgp10X483166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ho KY, Chua NH, George JM, et al. Evidence-based guidelines on the use of opioids in chronic non-cancer pain – a consensus statement by the Pain Association of Singapore Task Force. Ann Acad Med Singapore. 2013;42(3):138–152. [PubMed] [Google Scholar]
- 11.Frank JW, Bair MJ, Becker WC, Krebs EE, Liebschutz JM, Alford DP. Update in pain medicine for primary care providers: A narrative review, 2010–2012. Pain Med. 2014;15(3):425–431. doi: 10.1111/pme.12337. [DOI] [PubMed] [Google Scholar]
- 12.Williams CM, Maher CG, Hancock MJ, et al. Low back pain and best practice care: A survey of general practice physicians. Arch Intern Med. 2010;170(3):271–277. doi: 10.1001/archinternmed.2009.507. [DOI] [PubMed] [Google Scholar]
- 13.McDonald DD, Walsh S. Older adult osteoarthritis pain management: Results from the 2008 National Ambulatory Medical Care Survey. J Am Acad Nurse Pract. 2012;24(2):107–112. doi: 10.1111/j.1745-7599.2011.00676.x. [DOI] [PubMed] [Google Scholar]
- 14.Porucznik C, Johnson E, Rolfs R, Sauer B. Opioid prescribing knowledge and practices: provider survey following promulgation of guidelines-Utah, 2011. J Opioid Manag. 2013;9(3):217–224. doi: 10.5055/jom.2013.0162. [DOI] [PubMed] [Google Scholar]
- 15.Hall GC, Morant SV, Carroll D, Gabriel ZL, McQuay HJ. An observational descriptive study of the epidemiology and treatment of neuropathic pain in a UK general population. BMC Fam Pract. 2013;14:28. doi: 10.1186/1471-2296-14-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Breuer B, Cruciani R, Portenoy RK. Pain management by primary care physicians, pain physicians, chiropractors, and acupuncturists: a national survey. South Med J. 2010;103(8):738–747. doi: 10.1097/SMJ.0b013e3181e74ede. [DOI] [PubMed] [Google Scholar]
- 17.Mafi JN, McCarthy EP, Davis RB, Landon BE. Worsening trends in the management and treatment of back pain. JAMA Intern Med. 2013;173(17):1573–1581. doi: 10.1001/jamainternmed.2013.8992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Allen MJ, Asbridge MM, Macdougall PC, Furlan AD, Tugalev O. Self-reported practices in opioid management of chronic noncancer pain: a survey of Canadian family physicians. Pain Res Manag. 2013;18(4):177–184. doi: 10.1155/2013/528645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Clark LG, Upshur CC. Family medicine physicians’ views of how to improve chronic pain management. J Am Board Fam Med. 2007;20(5):479–482. doi: 10.3122/jabfm.2007.05.070029. [DOI] [PubMed] [Google Scholar]
- 20.Wagner EH. Chronic disease management: what will it take to improve care for chronic illness? Eff Clin Pract. 1998;1(1):2–4. [PubMed] [Google Scholar]
- 21.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: the chronic care model, part 2. JAMA. 2002;288(15):1909–1914. doi: 10.1001/jama.288.15.1909. [DOI] [PubMed] [Google Scholar]
- 22.Coleman K, Austin BT, Brach C, Wagner EH. Evidence on the Chronic Care Model in the new millennium. Health Aff (Millwood) 2009;28(1):75–85. doi: 10.1377/hlthaff.28.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Straus S, Tetroe J, Graham ID. Knowledge Translation in Health Care – Moving from Evidence to Practice. London: Wiley-Blackwell; 2009. [Google Scholar]
- 24.Leykum LK, Pugh JA, Lanham HJ, Harmon J, McDaniel RR., Jr Implementation research design: integrating participatory action research into randomized controlled trials. Implement Sci. 2009;4:69. doi: 10.1186/1748-5908-4-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lalonde L, Goudreau J, Hudon E, et al. Priorities for action to improve cardiovascular preventive care of patients with multimorbid conditions in primary care – a participatory action research project. Fam Pract. 2012;29(6):733–741. doi: 10.1093/fampra/cms021. [DOI] [PubMed] [Google Scholar]
- 26.Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore. 1994;23(2):129–138. [PubMed] [Google Scholar]
- 27.van de Ven AH, Delbecq AL. The nominal group as a research instrument for exploratory health studies. Am J Public Health. 1972;62(3):337–342. doi: 10.2105/ajph.62.3.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lalonde L, Choiniere M, Martin E, Berbiche D, Perreault S, Lussier D. Costs of moderate to severe chronic pain in primary care patients – a study of the ACCORD Program. J Pain Res. 2014;7:389–403. doi: 10.2147/JPR.S55388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lalonde L, Leroux-Lapointe V, Choiniere M, et al. Knowledge, attitudes and beliefs about chronic noncancer pain in primary care: A Canadian survey of physicians and pharmacists. Pain Res Manag. 2014;19(5):241–250. doi: 10.1155/2014/760145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vaismoradi M, Turunen H, Bondas T. Content analysis and thematic analysis: Implications for conducting a qualitative descriptive study. Nurs Health Sci. 2013;15(3):398–405. doi: 10.1111/nhs.12048. [DOI] [PubMed] [Google Scholar]
- 31.Breivik H, Eisenberg E, O’Brien T, OPENMinds The individual and societal burden of chronic pain in Europe: the case for strategic prioritisation and action to improve knowledge and availability of appropriate care. BMC Public Health. 2013;13:1229. doi: 10.1186/1471-2458-13-1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chelimsky TC, Fischer RL, Levin JB, Cheren MI, Marsh SK, Janata JW. The primary practice physician program for chronic pain ((c) 4PCP): outcomes of a primary physician-pain specialist collaboration for community-based training and support. Clin J Pain. 2013;29(12):1036–1043. doi: 10.1097/AJP.0b013e3182851584. [DOI] [PubMed] [Google Scholar]
- 33.Allen M, Macleod T, Zwicker B, Chiarot M, Critchley C. Interprofessional education in chronic non-cancer pain. J Interprof Care. 2011;25(3):221–222. doi: 10.3109/13561820.2011.552134. [DOI] [PubMed] [Google Scholar]
- 34.Aston SJ, Rheault W, Arenson C, et al. Interprofessional education: a review and analysis of programs from three academic health centers. Acad Med. 2012;87(7):949–955. doi: 10.1097/ACM.0b013e3182583374. [DOI] [PubMed] [Google Scholar]
- 35.Lundon K, Shupak R, Reeves S, Schneider R, McIlroy JH. The Advanced Clinician Practitioner in Arthritis Care program: an interprofessional model for transfer of knowledge for advanced practice practitioners. J Interprof Care. 2009;23(2):198–200. doi: 10.1080/13561820802379987. [DOI] [PubMed] [Google Scholar]
- 36.Ospina MB, Taenzer P, Rashiq S, et al. A systematic review of the effectiveness of knowledge translation interventions for chronic noncancer pain management. Pain Res Manag. 2013;18(6):e129–e141. doi: 10.1155/2013/120784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.The Ennis Centre for pain management. Ennis J. The Prejudice Against Chronic Pain. The Ennis Centre for pain management; 2008. [Accessed September 8, 2014]. Available from: http://www.enniscentre.com/wp-content/uploads/2012/04/Prejudice-again-chronic-pain.pdf. [Google Scholar]
- 38.Cornally N, McCarthy G. Chronic pain: The help-seeking behavior, attitudes, and beliefs of older adults living in the community. Pain Manag Nurs. 2011;12(4):206–217. doi: 10.1016/j.pmn.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 39.Allcock N, Elkan R, Williams J. Patients referred to a pain management clinic: beliefs, expectations and priorities. J Adv Nurs. 2007;60(3):248–256. doi: 10.1111/j.1365-2648.2007.04400.x. [DOI] [PubMed] [Google Scholar]
- 40.Courtenay M, Carey N. The impact and effectiveness of nurse-led care in the management of acute and chronic pain: a review of the literature. J Clin Nurs. 2008;17(15):2001–2013. doi: 10.1111/j.1365-2702.2008.02361.x. [DOI] [PubMed] [Google Scholar]
- 41.Briggs M, Closs SJ, Marczewski K, Barratt J. A feasibility study of a combined nurse/pharmacist-led chronic pain clinic in primary care. Qual Prim Care. 2008;16(2):91–94. [PubMed] [Google Scholar]
- 42.Hadi MA, Alldred DP, Briggs M, Munyombwe T, Closs SJ. Effectiveness of Pharmacist-led Medication Review in Chronic Pain Management: Systematic Review and Meta-analysis. Clin J Pain. 2014;30(11):1006–1014. doi: 10.1097/AJP.0000000000000063. [DOI] [PubMed] [Google Scholar]
- 43.Dobscha SK, Corson K, Perrin NA, et al. Collaborative care for chronic pain in primary care: a cluster randomized trial. JAMA. 2009;301(12):1242–1252. doi: 10.1001/jama.2009.377. [DOI] [PubMed] [Google Scholar]
- 44.Gurden M, Morelli M, Sharp G, Baker K, Betts N, Bolton J. Evaluation of a general practitioner referral service for manual treatment of back and neck pain. Prim Health Care Res Dev. 2012;13(03):204–210. doi: 10.1017/S1463423611000648. [DOI] [PubMed] [Google Scholar]
- 45.Canadian Health Services Research Foundation. Oandasan I, Baker R, Bosco C, et al. Teamwork in Healthcare: Promoting Effective Teamwork in Healthcare in Canada – Policy Synthesis and Recommendations. Canadian Health Services Research Foundation; 2006. [Accessed February 23, 2015]. Available from: http://www.cfhi-fcass.ca/Migrated/PDF/ResearchReports/CommissionedResearch/teamwork-synthesis-report_e.pdf. [Google Scholar]
- 46.Peng P, Choiniere M, Dion D, et al. Challenges in accessing multidisciplinary pain treatment facilities in Canada. Can J Anaesth. 2007;54(12):977–984. doi: 10.1007/BF03016631. [DOI] [PubMed] [Google Scholar]
- 47.Choiniere M, Dion D, Peng P, et al. The Canadian STOP-PAIN project – Part 1: Who are the patients on the waitlists of multidisciplinary pain treatment facilities? Can J Anaesth. 2010;57(6):539–548. doi: 10.1007/s12630-010-9305-5. [DOI] [PubMed] [Google Scholar]
- 48.Guerriere DN, Choiniere M, Dion D, et al. The Canadian STOP-PAIN project – Part 2: What is the cost of pain for patients on waitlists of multidisciplinary pain treatment facilities? Can J Anaesth. 2010;57(6):549–558. doi: 10.1007/s12630-010-9306-4. [DOI] [PubMed] [Google Scholar]
- 49.Wåhlberg H, Valle PC, Malm S, Broderstad AR. Practical health cooperation – the impact of a referral template on quality of care and health care co-operation: study protocol for a cluster randomized controlled trial. Trials. 2013;7(14):7. doi: 10.1186/1745-6215-14-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
| Clinical vignette 1 | Clinical vignette 2 |
|---|---|
| Mrs Collette Comeau, aged 45, is married and has a full-time position as a medical archivist. She has two children, aged 8 and 12. Her husband is a pharmaceutical representative and has to spend many days a week away from home. Mrs Comeau has been suffering from fibromyalgia for 20 years. Pains spread over her whole body; they appeared without any precise causal event. She suffers from pains every day. On a scale from 0 to 10 where 0 represents “no pain” and 10 represents the “worst possible pain”, her average pain level is about 5 and varies from 0 to 7 depending on the time of day; it is weaker in the morning and increases throughout the day. Her pains considerably disturb her sleeping, and wake her up suddenly almost every night. Her pains interfere with her daily activities. She is often irritable, which interferes with her relationships with others. At work, she is not always fully efficacious, and she stays home about 10 days a year. She often refuses to participate in social and entertainment activities because of her pain. Mrs Comeau wants to remain independent. She often hesitates to ask for help. She does not believe she has power over her pain. Still, she believes her medication helps and medicine could perhaps one day completely relieve her pain. |
Mr Jacques Levasseur, aged 68, is widowed and retired. He lives alone at home. He has three children and seven grandchildren who occasionally come to visit him. He suffers from arthritis for 10 years already. His pain is in all his joints, in particular in his knees. Although he always feels some pain (about 2 on a scale of 0 to 10), pain is not constant. Many times a week, pain becomes very acute, up to 9. His pain particularly interferes with walking and doing house-keeping tasks. Pain often prevents his sleeping and makes him sullen. His sudden mood swings affect his relationships with others. He often refuses to participate in social activities. Before pain appeared, he loved to play golf. Now, he does not dare play anymore, because he is afraid pain will worsen if he walks much. Mr Levasseur has little hope of one day being totally relieved. He often feels helpless, and useless. |
| Medical history | Medical history |
| ➢ Pain control strategies ○ Psychotherapy, several years ago ○ Distraction techniques a few times a week ○ Yoga twice a week ➢ Medical follow-up ○ Family physician ○ Not followed-up by a specialist physician ○ No consultations for physiotherapy, ergotherapy, massotherapy, or chiropractic ➢ Medications ○ Herbal tea for constipation ○ Antiemetic medication (against nausea) ○ Anti-acid medication (against heartburn) ○ Fentanyl patches (75 μg every 2 days) and 150 mg of pregabalin every day |
➢ Pain control strategies ○ Relaxation techniques ➢ Medical follow-up ○ Family physician ○ Has already consulted physiotherapists, occupational therapists, chiropractors, and osteopaths, without success ➢ Medications ○ Acetaminophen a few times a week ○ Muscle relaxant ○ Anti-inflammatory medication (Celebrex 200 mg) |