Abstract
Acculturation may influence health behaviors, yet mechanisms underlying its effect are not well understood. In this study, we describe relationships between acculturation and health behaviors among low-income housing residents, and examine whether these relationships are mediated by social and contextual factors. Residents of 20 low-income housing sites in the Boston metropolitan area completed surveys that assessed acculturative characteristics, social/contextual factors, and health behaviors. A composite acculturation scale was developed using latent class analysis, resulting in four distinct acculturative groups. Path analysis was used to examine interrelationships between acculturation, health behaviors, and social/contextual factors, specifically self-reported social ties, social support, stress, material hardship, and discrimination. Of the 828 respondents, 69% were born outside of the U.S. Less acculturated groups exhibited healthier dietary practices and were less likely to smoke than more acculturated groups. Acculturation had a direct effect on diet and smoking, but not physical activity. Acculturation also showed an indirect effect on diet through its relationship with material hardship. Our finding that material hardship mediated the relationship between acculturation and diet suggests the need to explicate the significant role of financial resources in interventions seeking to promote healthy diets among low-income immigrant groups. Future research should examine these social and contextual mediators using larger, population-based samples, preferably with longitudinal data.
Keywords: United States, acculturation, health behavior, immigrant, public housing, social context
Introduction
Acculturation has been defined as the process by which the attitudes, values, beliefs and behaviors of one culture are adopted by an individual from another (Clark & Hofsess, 1998). Often, acculturation is equated with language proficiency and preference, as well as generational status (Abraido-Lanza et al., 2005; Lopez-Class et al., 2011). Acculturation has traditionally been viewed as a process of assimilation, which assumes a unidirectional, linear trajectory in which immigrants adopt the “dominant culture” (Berry & Sam, 1997). More recently, there has been acknowledgement that acculturation is a multidimensional, reciprocal and dynamic process (Abraido-Lanza et al., 2006; Lara et al., 2005; Lopez-Class et al., 2011) that is affected by societal structures and policies (Abraido-Lanza et al., 2006; Lopez-Class et al., 2011). The concept of “acculturation” has been criticized because it is commonly conceived as an individual-level factor, potentially masking the societal-level factors that prompt, co-exist, or are the result of immigration experiences (Acevedo-Garcia et al., 2012).
Nonetheless, a large body of literature has examined relationships between acculturation, health status (Kaplan et al., 2004; Singh & Siahpush, 2002) and health behavior (Abraido-Lanza et al., 2005; Andreeva et al., 2011; Ayala et al., 2008). Increased time spent in the United States (US) has consistently been associated with increased physical activity, presumably because of changes in cultural norms (Abraido-Lanza et al., 2005; Lara et al., 2005; Perez-Escamilla & Putnik, 2007). However, acculturation may also be associated with adoption of unhealthy behaviors, for example, when a cultural group with a largely plant-based diet adopts a “Western diet” lower in fruits/vegetables and higher in saturated fats (Ayala et al., 2008; Desilets et al., 2007; Lara et al., 2005; Patil et al., 2009). Norms surrounding tobacco use may also lead to increased adoption of smoking among more acculturated groups (Bethel & Schenker, 2005).While some of these trends have strong empirical evidence (Abraido-Lanza et al., 2005; Lara et al., 2005; Perez-Escamilla & Putnik, 2007), few studies have explicitly tested theory-driven pathways by which acculturation may influence health behaviors (Abraido-Lanza et al., 2006; Mills & Caetano, 2012) or potential social and contextual factors that might mediate these relationships (Abraido-Lanza et al., 2006). In particular, there has been a call for greater use of a ‘social determinant framework’ to examine the social, political, and structural factors that influence both the circumstances and consequences of immigration (Viruell-Fuentes et al., 2012).
A major area of debate is the measurement of acculturation (Abraido-Lanza et al., 2006; Lara et al., 2005; Perez-Escamilla & Putnik, 2007). Whereas language and nativity are commonly used as proxy measures (Lara et al., 2005; Lopez-Class et al., 2011), a more comprehensive understanding of acculturation has evolved in recent years, calling for greater attention to the socio-cultural context into which individuals and groups immigrate. For example, immigration can be accompanied by disruption in social ties, decrements in socio-economic standing, increased stress, and experiences of discrimination. Social and contextual changes that accompany immigration may be important mechanisms by which acculturation exerts its influence on health behaviors (Abraido-Lanza et al., 2006). Yet, these mechanisms have largely gone unexamined and there has been a call for the use of more sophisticated statistical models in investigating such pathways (Abraido-Lanza et al., 2006; Lara et al., 2005). There has also been a call for greater attention to the socio-contextual factors that affect the experience of immigration—including environments from which and to people immigrate (Acevedo-Garcia et al., 2012). This study uses path analyses to examine associations among acculturation, social/contextual factors, and self-reported health behaviors. Our goal was to evaluate the extent to which acculturation exerts a direct effect on health behaviors, as opposed to acting indirectly through socio-contextual factors.
Conceptual Framework
Our study was guided by a conceptual model (Figure 1) based on an integrated acculturation theory (Riedel et al., 2011) and stress and coping theory (Lazarus & Folkman, 1984). These theories posit that the immigration experience is shaped by an array of health-enhancing or health-threatening resources and hazards, with social ties and support being important components of these resources. For immigrants, the strength of social resources may moderate the acculturative process, including the experience of stress, coping, and subsequent behavioral reactions (Berry & Sam, 1997). In the context of immigration, health-enhancing resources may be diminished, given one’s separation from a familiar social environment, potentially resulting in maladaptive coping behaviors (e.g., smoking, overeating).
Figure 1.
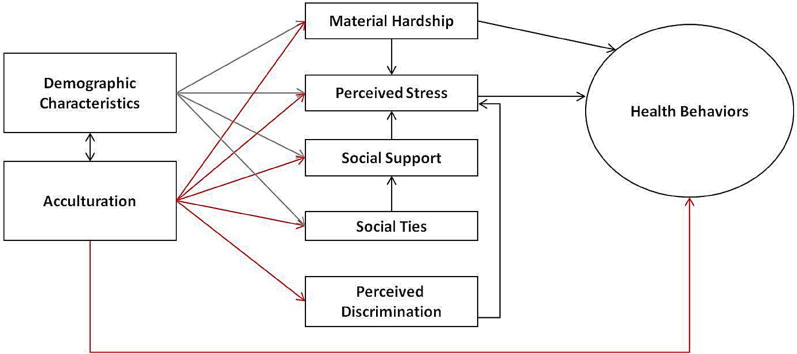
Hypothesized causal pathway: Association between acculturation, social/contextual factors and health behaviors
Stress and coping theory (Lazarus & Folkman, 1984) aligns with integrated acculturation theory, in that it emphasizes the potential for social resources and negative interactions to influence health, both directly (through peer pressures or social controls) and indirectly (by buffering stress, or affecting how an individual appraises or copes with stress) (Cohen, 2004). While social ties typically change in structure and content across the life course (Umberson et al., 2010), the nature of these changes may be particularly pronounced among immigrants. Accompanying disruptions in social ties, a lack of material resources (Hunt et al., 2004) and experiences of discrimination (Viruell-Fuentes, 2007; Viruell-Fuentes et al., 2012; Yoon et al., 2012) are common sources of stress for many groups that may function as mediators in the relationship between acculturation and health behaviors. More specifically, among less acculturated groups, material hardship and experiences of discrimination may serve as additional sources of stress, but they may also affect behavior, independent of stress. For example, material hardship may restrict access to a range of services (e.g., health care, housing) that could serve to promote, enable, or maintain health.
Methods
Setting and Sample
Data were obtained from Health in Common (HIC), an observational study designed to examine the social and environmental determinants of cancer risk among residents of low-income housing. According to the US Department of Housing and Urban Development, “low-income housing” is any housing that is limited to occupancy by persons whose family income does not exceed a preset maximum (e.g., 50% or less of the area median gross income for geographic area) (U.S. Department of Housing and Urban Development, 2012). HIC used a multi-stage cluster design, sampling households from within housing sites, and adults from within households (Kish, 1965). Surveys were conducted among 828 residents across 20 low-income housing developments (n=16–64 residents per site) in the greater Boston, MA area (response rate =49%). One adult resident was selected from each household if she/he spoke English, Spanish, or Haitian Creole and was interviewed in person between February 2007 and June 2009. The Institutional Review Board of the Dana-Farber Cancer Institute, Boston, MA, approved study protocols and procedures.
Measures
Acculturation
We used five items from the New Immigrant Survey (Jasso et al., 2003) to operationalize acculturation: (1) language(s) spoken (no English, English only, English plus another language); (2) language preference at home and with friends (English for both, English for one, English for none); (3) first language spoken or ‘native’ language (Spanish, Haitian Creole, English, other); (4) age arrived in the US (<5yrs, 5–18yrs, 19–29yrs, 30+yrs); and (5) number of years in US schools (none, some, all).
Latent class analyses (LCA) was used to determine whether groups with similar profiles were present among respondents born outside the US. The response patterns of the five acculturation items were used to categorize subjects into groups. These groups formed the acculturation categories of a categorical latent variable (a variable that cannot be directly measured), which was then used in the path analyses. Representing acculturation as a latent variable has been shown to be a valid method in creating a more comprehensive measure (Rost & Langeheine, 1997). We used the Akaike Information Criteria (AIC), Bayesian Information Criteria (BIC), and entropy indices to compare the fit of increasing class solutions (Celeux & Soromenho, 1996).
A three-class solution emerged (see Appendix for fit indices): (1) “very low” = non-US-born, non-English speakers who had no US schooling; (2) “low” = non-US-born, bilingual individuals who spent none/some of their schooling in the US; (3) “moderate” = non-US-born, English-only speakers who spent some or all of their school years in the US. In addition to these three classes, we created a fourth class to represent the “high” acculturative group, comprised of those born in the US (“US-born”).
Health Behaviors
Dietary Factors
We assessed dietary intake using Prime Screen (Rifas-Shiman et al., 2001), a brief version of the Semi-quantitative Food Frequency Questionnaire. Prime Screen has been validated against the longer version with adequate comparability (0.60) and reproducibility (0.70) (Rimm et al., 1992). Respondents reported their consumption of fruits and vegetables, 100% fruit juice, red meat, fast food, sugary snacks and sugary beverages in the last week. Because these variables were highly skewed, we calculated the z-scores for each food group by subtracting the daily servings by the mean daily servings, and dividing the result by the standard deviation. For each individual, the z-scores of red meat and junk food (sum of sugary drinks, sugary snacks, and fast food) were subtracted from the fruit and vegetable z-score, resulting in a continuous “Healthy Eating Index” (HEI), whereby positive values indicated healthier eating. Using an HEI allowed us to evaluate a range of common components in Western diet, rather than just specific foods (e.g. fruits and vegetables)
Physical Activity
We assessed both moderate and vigorous daily leisure and occupational physical activity in the last 7 days using the International Physical Activity Questionnaire (Craig et al., 2003). Test-retest reliability and criterion validity have been previously demonstrated against accelerometer data (Craig et al., 2003). Our measure of physical activity is a sum of the moderate and vigorous activity converted into hours per day.
Current Smoking
Tobacco use was measured using items from the NCI Tobacco Screener (Cantor et al., 2008). Respondents were classified as: (1) current smokers, (2) former smokers, or (3) non-smokers.
Social and Contextual Factors
Material Hardship
We conceptualized material hardship using financial insecurity and food insecurity. Financial insecurity was operationalized with the question: “In general, how do you find your household’s finances usually work out at the end of the month?” (Pearlin et al., 1981) and food insecurity with the question: “In the past 12 months, was there ever a time when there wasn’t enough money for food?” (Nord et al., 2004) These variables were combined into three categories for ease of interpretation: (1) some money left regardless of response to food insecurity (“no material hardship”); (2) just enough money left over and some money left for food (“barely making ends meet”); and (3) not enough money left over or no money for food (“material hardship”) (U.S. Census Bureau, 2008).
Perceived Stress
We measured perceived stress using four items from the Perceived Stress Scale (Cohen et al., 1983), one of the most widely used measures of stress which has demonstrated high reliability and validity across diverse samples (Cohen et al., 1983). Items assessed the frequency with which respondents felt: (1) unable to control the important things in life; (2) confident about handling personal problems; (3) things were “going your way”; and (4) difficulties were piling up so high that they could not be overcome. The final perceived stress measure is a sum of all four items (range 0–12), with higher scores indicating greater perceived stress. While Cronbach alpha scores of 0.7 and above are generally considered ideal, in our sample, the Cronbach’s alpha for these items was 0.6. Because this is among the most widely used measures of stress and has been extensively tested (Cohen et al., 1983), we elected to retain the items as a single scale.
Social Ties
We used the number of close family members, close friends, and close neighbors an individual had as our measure of social ties. Individuals received one point for each of the following: (1) having one or more close family members; (2) having one or more close friends; and (3) having one or more close family members or friends that lived in the same housing development (i.e., neighbors). Points were summed to create a composite score for social ties (range 0–3), such that higher scores indicated a greater number of social ties (Heaney & Israel, 1997).
Social Support
Social support was assessed by asking if residents had family, friends or neighbors that they “[felt] close to, [could] talk to about private things or [could] rely on for help, or [made] them feel loved or cared for” (Heaney & Israel, 1997). One point was awarded if the resident responded “yes” to having family or friend support, or “often/sometimes” to having neighbor support. The final overall social support measure ranged from 0 to 3, with higher scores representing greater levels of support.
Discrimination
Discrimination was measured using a 7-item scale that assessed experiences of discrimination based on race, ethnicity or color in three settings: work, school, and in public (Krieger et al., 2005). The Cronbach’s alpha for these items was 0.8. We created a three category score based on the number of settings where discrimination was experienced. This variable was positively skewed, and cut-points were set at 0 settings, 1–2 settings, 3+ setting (median=0 and 75th percentile=2), as used in prior research (N Krieger, 2000).
Demographic Characteristics
Age, race/ethnicity, gender, and education were measured using standard items from the 2005 HINTS demographic questionnaire (Cantor et al., 2008).
Where possible, we made efforts to utilize measures that had previously been validated or utilized among racial/ethnically diverse audiences. Items were forward-and-back translated for both cultural and linguistic appropriateness. Cognitive testing of measures was conducted among N=8 low-income housing residents in three languages (English, Spanish, Haitian Creole). In addition, items were tested in focus group discussions with all three language groups for item comprehension and cultural relevance. These individuals were not included in the study.
Analysis
We used path analysis to determine whether the data from this study supported the hypothesized relationships in our conceptual model. The paths to the model are specified as a series of linear regressions where direct, indirect, and total paths are tested simultaneously (see Figure 1). Indirect pathways are used to assess mediation and are estimated as the product of the pathway coefficient estimates along that path. The total pathways are a sum of direct and indirect pathways. Indirect effects of social/contextual factors were tested in seven pathways for health behaviors (Figure 2). For all path models, standardized coefficients were presented to examine the significance and direction of each relationship. The coefficients were standardized using the ratio of the variance of the dependent variable to that of the independent variable and represented the amount of change in the dependent variable per unit change in the independent variable in standard deviation units. Standardized coefficients allow direct comparison of the relative importance of each of the independent to the model. Positive coefficients indicated an increase in the dependent variable, while negative coefficients represented a decrease (Muthen & Muthen, 1998–2011). Adequacy of model fit was assessed using the Comparative Fit Index (CFI), Tucker-Lewis Index (TLI), Root Mean Square Error of Approximation (RMSEA), and Weighted Root Mean Square Residual (WRMR). The path model is considered to have adequate fit based on these commonly used cutoffs: CFI <0.90, TLI <0.90, RMSEA<0.06, WRMR<.90 (Hu & Bentler, 1998). Missing data was limited (≤ 1% missing in the path model). The largest amount of missing data was for physical activity, which was missing for nine subjects (1%), followed by class membership and race/ethnicity, with data missing for 4 subjects (0.5%). The analytic sample size for the path model was N= 803. Mplus software version 4.21 (Muthén & Muthén) was used to test our path model.
Figure 2.

Tested pathways between acculturation and health behavior
Results
Sample Characteristics
The majority of the sample was female (80%) and foreign-born (69%), with 41% identifying as Hispanic (41%) and 38% identifying as non-Hispanic Black. Country/region of origin (data not shown) included: US (32%), Haiti (23%), Puerto Rico (12%), and Latin America (22%). Race/ethnicity and place of birth were highly correlated (data not shown); 94% of non-Hispanic Blacks were born in Haiti and 98% of the Hispanics were born in Latin America. Among those born in the US, 26% were Hispanic, 33% non-Hispanic White, 29% non-Hispanic Black, and 13% classified as “other.” See Table 1.
Table 1.
Socio-demographic characteristics of Health in Common (HIC) sample
| Independent/covariates | Total | Healthy Eating Index | Moderate and Vigorous Activity (hr/wk) | Current Smoker |
|---|---|---|---|---|
| N (%) | Mean ±s.d. | Mean ±s.d. | N (%) | |
|
| ||||
| Overall | 828 | −0.01 ± 1.84 | 1.90 ± 1.46 | 177 (21.4%) |
|
| ||||
| Age | ||||
| 18–29 | 153(18.5%) | −0.63±1.99* | 1.99±1.52* | 42(23.7%)* |
| 30–39 | 218(26.4%) | 0.03±1.74 | 2.17±1.36 | 29(16.4%) |
| 40–49 | 169(20.5%) | 0.03±1.84 | 2.14±1.5 | 40(22.6%) |
| 50–59 | 145(17.6%) | 0.36±1.59 | 1.94±1.65 | 43(24.3%) |
| 60–70+ | 140(17%) | 0.16±1.91 | 1.06±0.92 | 23(13%) |
|
| ||||
| Gender | ||||
| Male | 169(20.4%) | −0.25±1.99* | 2±1.58 | 46(26%)* |
| Female | 659(79.6%) | 0.05±1.79 | 1.88±1.43 | 131(74%) |
|
| ||||
| Marital Status | ||||
| No | 550(66.6%) | −0.1±1.87 | 1.86±1.43 | 134(75.7%)* |
| Yes | 276(33.4%) | 0.15±1.76 | 2.01±1.53 | 43(24.3%) |
|
| ||||
| Education | ||||
| Grade | 152(20.7%) | 0.19±1.52 | 1.44±1.14* | 19(11.9%)* |
| Some HS | 123(16.7%) | −0.22±1.98 | 1.92±1.5 | 36(22.5%) |
| HS | 200(27.2%) | −0.23±1.78 | 2.09±1.53 | 44(27.5%) |
| >HS | 261(35.5%) | 0.06±1.99 | 2.11±1.56 | 61(38.1%) |
|
| ||||
| Race/Ethnicity | ||||
| Hispanic | 341(41.4%) | −0.13±1.75* | 1.95±1.48 | 64(36.6%)* |
| Non-Hispanic White | 93(11.3%) | −0.73±1.9 | 1.71±1.52 | 48(27.4%) |
| Non-Hispanic Black | 316(38.3%) | 0.35±1.84 | 1.94±1.42 | 44(25.1%) |
| Other | 74(9%) | −0.08±1.81 | 1.77±1.46 | 19(10.9%) |
|
| ||||
| Place of birth | ||||
| Haiti | 197(23.9%) | 0.57±1.57* | 1.89±1.46 | 9(5.1%) |
| Latin America | 173(21.0%) | 0.04±1.54 | 1.91±1.43 | 9(5.1%) |
| Other | 100(12.2%) | 0.32±1.60 | 1.86±1.32 | 12(6.8%) |
| Puerto Rico | 95(11.5%) | −0.14±1.79 | 1.86±1.47 | 26(14.8%) |
| U.S. | 260(31.5%) | −0.56±2.13 | 1.95±1.54 | 120(68.2%) |
|
| ||||
| Languages Spoken | ||||
| No English | 249(30.1%) | 0.26±1.56* | 1.6±1.22* | 16(9%)* |
| Bilingual | 382(46.2%) | 0.19±1.76 | 2.18±1.59 | 71(40.1%) |
| English Only | 196(23.7%) | −0.74±2.09 | 1.77±1.41 | 90(50.8%) |
|
| ||||
| Age arrived in US | ||||
| <5 | 290(35.8%) | −0.53±2.12* | 1.97±1.56 | 128(73.1%)* |
| 5–17 | 116(14.3%) | −0.13±1.64 | 1.94±1.34 | 17(9.7%) |
| 18–29 | 223(27.5%) | 0.26±1.63 | 1.98±1.46 | 21(12%) |
| 30+ | 182(22.4%) | 0.53±1.49 | 1.64±1.36 | 9(5.1%) |
|
| ||||
| School years spent in US | ||||
| None | 325(57.8%) | 0.35±1.58* | 1.72±1.39* | 29(51.8%)* |
| Some | 198(35.2%) | 0.2±1.66 | 2.09±1.4 | 15(26.8%) |
| All | 39(6.9%) | −0.34±1.78 | 2.2±1.58 | 12(21.4%) |
|
| ||||
| Acculturation Categories | ||||
| Very low | 35(4.2%) | −0.29±1.97* | 1.72±1.2* | 6(3.4%)* |
| Low | 263(31.9%) | 0.3±1.65 | 2.19±1.55 | 35(19.9%) |
| Moderate | 266(32.3%) | 0.25±1.54 | 1.61±1.26 | 15(8.5%) |
| US-born | 260(31.6%) | −0.56±2.13 | 1.95±1.54 | 120(68.2%) |
|
| ||||
| Perceived Discrimination | ||||
| 0 settings | 442(53.4%) | −0.09±1.8 | 1.65±1.34* | 94(53.1%)* |
| 1–2 settings | 232(28.1%) | 0.17±1.75 | 2.13±1.5 | 40(22.6%) |
| 3+ settings | 153(18.5%) | −0.04±2.04 | 2.29±1.61 | 43(24.3%) |
|
| ||||
| Material hardship | ||||
| No material hardship | 423(52.2%) | −0.08±1.77 | 1.97±1.50 | 100(56.5%) |
| Barely making ends meet | 252(31.1%) | 0.15±1.84 | 1.85±1.48 | 47(26.7%) |
| Material hardship | 136(16.8% | −0.11±2.00 | 1.84±1.31 | 30(22.1%) |
|
| ||||
| Social Ties | ||||
| 0 | 84(10.2%) | 0.1±1.79 | 1.82±1.37* | 12(6.8%) |
| 1 | 273(33.1%) | 0.19±1.67 | 1.76±1.4 | 54(30.5%) |
| 2 | 313(37.9%) | −0.06±1.85 | 2.1±1.56 | 68(38.4%) |
| 3 | 156(18.9%) | −0.29±2.06 | 1.78±1.39 | 43(24.3%) |
|
| ||||
| Social Support | ||||
| 0 | 57(6.9%) | 0.17±1.65 | 1.92±1.4 | 6(3.4%) |
| 1 | 205(24.8%) | 0.12±1.69 | 1.85±1.44 | 44(24.9%) |
| 2 | 306(37%) | −0.04±1.87 | 1.93±1.49 | 61(34.5%) |
| 3 | 260(31.4%) | −0.12±1.94 | 1.92±1.47 | 66(37.3%) |
|
| ||||
| Perceived Stress† | 8.49±2.68 | −0.13* | −0.02 | 8.99±2.95* |
Frequencies (%) presented for categorical outcomes and means (std) presented for continuous outcomes.
p-value ≤ 0.05.
Perceived stress is the only continuous independent variable, means are presented for categorical outcomes and the Pearson correlation is presented for continuous outcomes.
The most common countries represented in the “Latin American” category were El Salvador (n = 56), Dominican Republic (n = 44), Honduras (n =28), Guatemala (n = 14), Colombia (n = 8), Mexico (n = 6) and Brazil (n= 6). The most common countries represented in the “Other” category were Ethopia (n = 29), Jamaica (n = 9) and Somalia (n = 7), and Bangladesh (n = 5). There were less than 5 participants from all of the other countries represented under “Latin America” and “Other”.
In regard to acculturative classes, approximately equal percentages of residents were classified into “low,” “moderate,” and US-born. Only 4% were classified into the “very low” category. Respondents in the “very low” and “low” acculturation groups were more likely to be male (26% and 27%, respectively), compared to residents in the “moderate” and US-born (14% and 19%, respectively). Those born in the US were less likely to self-identify as Hispanic or Black (26% and 29%, respectively); the highest proportion of Hispanics were in the moderately acculturated group (59%). Nearly all of the residents in the low acculturated group reported that they spoke another language plus English (99%), compared with 37% in the very low acculturation class, 8% in the moderate class, and 33% in the U.S. born class. Among those who were not born in the US, half of the moderately acculturated group came to the US when they were aged 30 years or older, compared to 17% in the low acculturation class, and 14% in the very low acculturation class.
Across the entire sample, the mean dietary HEI score was −0.01 (s.d. = 1.84; range: −8.52 to 5.14). Respondents reported a mean of 1.90 (s.d. = 1.46) hours per week of total moderate and vigorous activity. About a fifth of respondents and nearly half of US-born respondents were current smokers.
Path Analysis
Acculturation, Social/Contextual Factors, and Healthy Eating Index (HEI)
The path model in Figure 3 shows relationships between acculturation, social/contextual factors, and the HEI. The direct relationship between acculturation and the HEI was statistically significant. Compared to those born in the US, those in the “very low” and “low” acculturation groups reported healthier diets (coefficients 0.6, p = 0.004; 0.7, p = 0.01, respectively).
Figure 3.
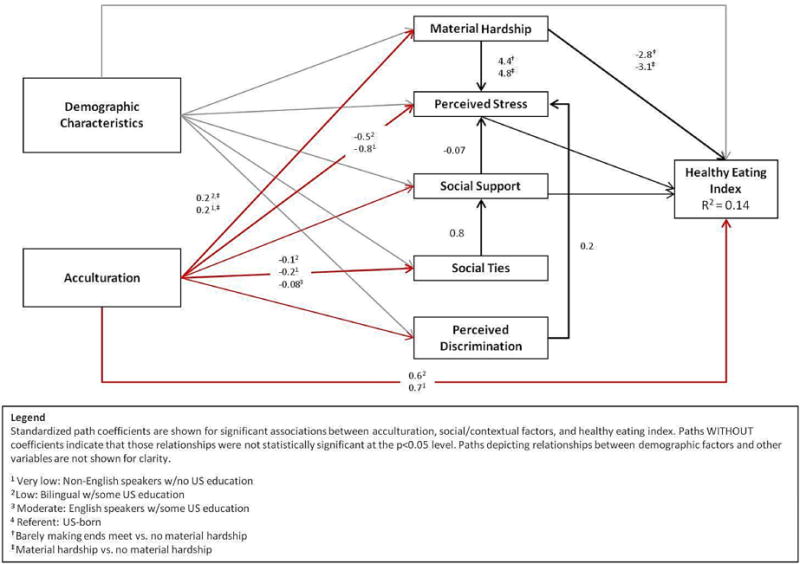
Acculturation, Social/Contextual Factors and Healthy Eating Index
The lower acculturation groups were significantly more likely to report some material hardship (coefficient 0.2, p = 0.0009 for “very low” and p = 0.0008 for “low”); yet, they also reported lower levels of stress (coefficient for “very low” −0.5, p = 0.03; “low” −0.8, p = 0.02), compared to the US-born group. Those born in the US reported a greater number of social ties. Perceived discrimination and material hardship (coefficients 0.2 p ≤ 0.001; 4.4 p = 0.009, respectively) were positively associated with perceived stress, and greater social support was associated with lower perceived stress (coefficient −0.07, p = 0.03). There was also a strong positive association between social ties and social support p ≤ 0.001. Material hardship was negatively associated with the HEI (coefficients −2.8 p = 0.04; −3.1 p = 0.03).
The path model demonstrated a good fit with the data, with the CFI at 0.994, TLI at 0.965, RMSEA at 0.55, and WRMR at 0.746. Nevertheless, the variance explained by the model was small (R2 = 0.14).
Acculturation, Social/Contextual Factors and Current Smoking
As shown in Figure 4, the direct negative association between acculturation and current smoking was statistically significant (coefficients for “very low” −0.7, p = 0.0006; “low” −0.5, p = 0.0001; “moderate” −0.02, p = 0.005). Acculturation was also negatively associated with material hardship, social support, and social ties. Residents in the “very low” and “low” acculturative groups were more likely to report some material hardship and fewer social ties compared to the US born group (coefficients 0.2 for both; p = 0.0009 for “very low” and p = 0.008 for “low”). Those in the “very low” acculturation group reported lower levels of social support compared with the US born group (coefficient −0.05, p = 0.05). Respondents categorized as “barely making ends meet” and those reporting perceived discrimination also reported greater perceived stress (coefficients 2.9, p=0.03 and 0.2 p<0.0001, respectively). This path model also demonstrated a good fit (CFI = 0.994, TLI = 0.965, RMSEA = 0.055, WRMR = 0.739). Additionally, this model explained more variance than the previous model (R2 = 0.26).
Figure 4.
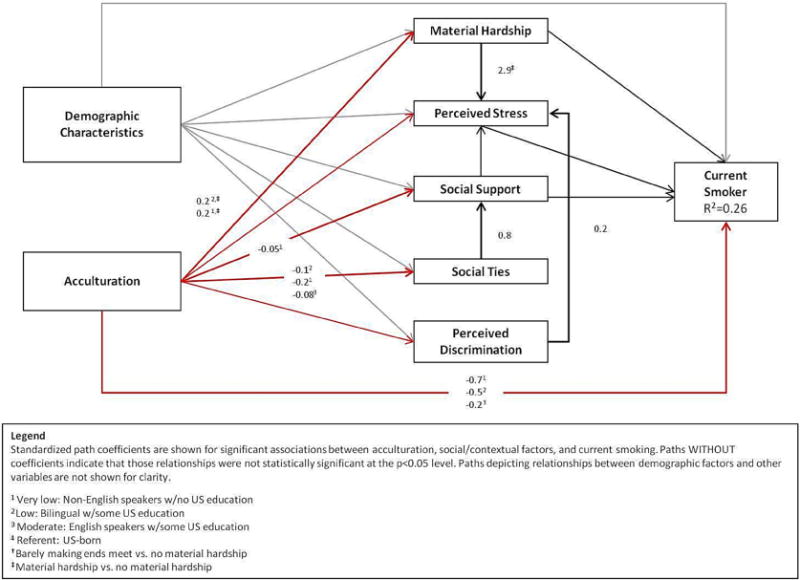
Acculturation, Social/Contextual Factors and Current Smoking
In path models HEI and Current Smoking (Figures 3 & 4), the indirect effects of acculturation on health behaviors through social/contextual factors were not statistically significant, indicating that while acculturation and the health behaviors were associated directly, this relationship was not mediated by the social/contextual factors in this study.
Acculturation, Social/Contextual Factors, and Physical Activity
Path models were not developed for acculturation and physical activity, because we found no statistically significant associations in bivariate analyses between these variables and social/contextual factors, after controlling for demographic characteristics (data not shown).
Discussion
In this large sample of low-income housing residents, we found that a composite measure of acculturation was significantly associated with dietary behaviors and current smoking, but not with physical activity. The significant pathways between acculturation and diet and between acculturation and smoking were primarily direct. While acculturation was directly associated with each of the social/contextual factors examined, its association with health behaviors was largely independent of social/contextual factors. The one exception was material hardship, which mediated the association between acculturation and diet. Social support was negatively associated with perceived stress, although this relationship was only statistically significant in the model for healthy eating.
Our results are consistent with previous studies indicating that greater acculturation is associated with poorer diets (Ayala et al., 2008; Desilets et al., 2007; Patil et al., 2009). However, our results suggest that the relationship between acculturation and diet is complex, and may be mediated by material hardship. Those who were less acculturated were more likely to report material hardship compared to the US-born group, but they were also more likely to have healthier dietary patterns. These findings support the hypothesis that, over time, respondents may change their dietary practices to align with their financial situations, opting for less expensive energy-dense, but low-nutrient, foods as they learn ways to save money after immigrating (Patil et al., 2009). For example, newly arrived families may be less likely to participate in food assistance programs (Patil et al., 2009). While participation in such programs likely helps to mitigate material hardship, participation has been associated with increased consumption of added sugars and total fats (Wilde et al., 2000) and higher BMI (Webb et al., 2008). Other factors that were not assessed in this study, including time constraints, knowledge of healthy food preparation, and access to affordable healthy foods in low-income neighborhoods (Patil et al., 2009) also likely serve as important determinants of dietary behaviors. Furthermore, food preferences have, in themselves, been suggested as an important dimension of acculturation worth exploring in future research.
Our results show no direct relationship between acculturation and physical activity. In general, previous studies have not discerned a convincing directional pattern for this association, but have found that the effect may differ across groups (Abraido-Lanza et al., 2005; Esparza et al., 2000; Gordon-Larsen et al., 2003; Lara et al., 2005) as well as across types of physical activity (e.g., leisure-time vs. occupational) (Velasquez et al., 2009). Previous research among Haitian immigrants has reported that physical inactivity is high, but the precise ways in which acculturation status influences variations in physical activity in this group is largely unknown (O’Loughlin et al., 2007). The relationship between physical activity and acculturation may operate through different mechanisms than the social/contextual factors assessed in this study – for example, through neighborhood characteristics such as perceived safety (Pichon et al., 2007). Alternatively, the lack of association between acculturation and physical activity may be attributable to measurement error given some of the difficulties assessing physical activity in this sample (Caspi et al., 2013). Finally, while we examined only total physical activity patterns, leisure versus non-leisure time physical activity may be different among different immigrants with varying acculturation levels (Berrigan et al., 2006). Distinguishing between these different types of physical activity may be important for interpreting studies involving physical activity in immigrant groups.
Consistent with prior literature (Bethel & Schenker, 2005), acculturation was directly associated with smoking behavior. US-born respondents were the most likely to be current smokers, while the least acculturated were the least likely to report being current smokers. Few studies have examined social/contextual factors that may explain this finding. In one study of women of Mexican descent (Harley & Eskenazi, 2006), those who had spent more time in the U.S had higher levels of emotional social support and were less likely to smoke. The potential mediating effect of social support on smoking behaviors was, however, not seen in our data. It is possible that social and cultural factors, such as social norms or gender roles, that were not assessed in this study could account for others’ findings (Bennett et al., 2008; Constantine et al., 2010).
Surprisingly, material hardship was also unrelated to smoking in the current study. Previous studies have found an association between financial strain and smoking in population-based studies with a wide SES range (Lindstrom et al., 2013). Since our study included a restricted income range, exposure to some degree of material hardship may have been a common and consistent experience, such that other factors (norms or cultural factors) were more important determinants of smoking behavior.
Few studies have used path models to explore direct and indirect associations among acculturation, social/contextual factors, and health behaviors. In those that have, social-relational factors—including connectedness to others and social support—have emerged as pathways through which acculturation might affect mental or general health status (Jasinskaja-Lahti & Liebkind, 2007; Riedel et al., 2011; Yoon et al., 2012). In our study, social support and social ties did not mediate the relationship between acculturation and health behaviors. The lack of significant findings may be due to low variability in these measures, given the relatively high levels of social ties and support reported within our sample. Nevertheless, social support was negatively associated with perceived stress, and perceived stress was directly influenced by material hardship. These findings provide suggestive evidence that social support might indirectly influence behaviors through material hardship. Similarly, perceived discrimination—while not independently related to health behaviors—was significantly associated with perceived stress in both the healthy eating and smoking models.
Segmented assimilation theory (Portes & Zhou, 1993) offers perspective on these complex findings. According to this theory, immigrants have multiple trajectories of adaptation and differential cultural reference groups to which they acculturate (Portes & Zhou, 1993). For example, it could be that some Haitian or Latino immigrants in our sample adopted the behavioral patterns of middle-class “mainstream” America, while others may have undergone a process of “ethnic minority acculturation” (Abraido-Lanza et al., 2006), in which they adopted the norms of other ethnic minority groups. Our models were not able to capture what may be potentially dynamic patterns of uptake of behaviors within and between immigrant groups due to the small number of subjects within each subgroup.
Segmented assimilation theory highlights some of the challenges in studying the concept of acculturation, namely, the limits of common definitions of acculturation that encourage “othering,” the risk of relying on cultural stereotypes rather than data to explain differences between groups, and a de-contextualization of culture, separate from economic contexts (Hunt et al., 2004; Viruell-Fuentes, 2007; Viruell-Fuentes et al., 2012). We relied on a standard definition of acculturation that was based on an assumed difference between a “dominant” culture and an “other” culture. An example of the limits of this is our assumption that a “Western diet” would be most commonly consumed by the “dominant” culture, and that this diet would be different from other “traditional” diets. Yet, this may not always be the case. However, our goal was not to suggest specific cultural practices that explain the gap between specific cultural communities and the “dominant” culture – a practice which risks promoting cultural stereotypes (Hunt et al., 2004). Rather, the aim was to consider the potential role of a number of interpersonal and contextual factors in the pathway between commonly used proxy measures of acculturation and health behaviors. Indeed, in finding that material hardship mediated the relationship between acculturation and dietary practices, this study supports an approach to acculturation research that acknowledges the intersectionality of migration status with other indicators of social disadvantage, such as socioeconomic position (Viruell-Fuentes et al., 2012).
Intersectionality theory posits that socially-constructed systems of oppression—based on gender, race, and/or SES—work simultaneously to produce health inequities. Prominent scholars have recently called for a research agenda in immigrant health that acknowledges “systems of oppression [that are] mutually constituted” (Viruell-Fuentes et al., 2012, p. 2101). Such an agenda would require greater attention to the influence of societal-level factors, such as immigration and labor policies, residential segregation, and structural racism, with lesser focus on what has previously been attributed to individual-level health behaviors driven by cultural practices and beliefs (Viruell-Fuentes et al., 2012).
We acknowledge this and several other limitations of this study. Our study relied on a suitable, although limited, proxy measure of acculturation that encompassed language, nativity, and US schooling (Alegria, 2009). While limited, studies have shown that proxy acculturation items can be valuable for assess acculturation in situations where use of a more comprehensive acculturation scale is impractical (Cruz et al., 2008). To minimize respondent burden, we needed to select pragmatic measures that could feasibly and reliably be assessed in a large survey. However, there is still a great need for studies that use more comprehensive assessments of acculturation that incorporate a greater range of behaviors and individual preferences, as well as studies that utilize better measures of social support and social networks (Acevedo-Garcia & Bates, 2008). Additionally, our study did not assess the variable adoption of behaviors across different context or settings. Also, we were unable to analyze differences between immigrant subgroups. This may be an important factor, particularly given that different immigrant groups exhibit diverse patterns of assimilation or cultural integration, and experience differing degrees of acceptance into the US (Reitz, 2002). Albeit limited, our assessment of perceived discrimination attempted to capture some aspects of this phenomenon. While in this sample, the measure of perceived stress had a Cronbach’s alpha of 0.60, some consider this an acceptable reliability score (Horne et al., 2001). Also, the “very low” acculturative group was comprised of only 35 individuals, making it difficult to draw any meaningful conclusions about this group. Similarly, we were unable to conduct analyses by gender, which could potentially be an important factor in the relationship among acculturation and health behaviors (Kessler & Mcleod, 1984; Umberson et al., 1996). Another limitation is the lack of validation of some of these measures among Spanish or Creole speakers. It is has been observed that immigrants report factors such as perceived discrimination in a very different manner than do US-born persons of color (Cook et al., 2009; Yip et al., 2008). Finally, like many other large-scale, community-based studies, we relied on self-reported data on health behaviors. While these have been shown to be reasonably accurate (Gorber et al., 2009; Wong et al., 2012), there is the potential for recall bias (Hebert et al., 2008).
Nonetheless, this study has a number of important strengths. It is among the few that have attempted to disentangle relationships between acculturation and social/contextual factors that may influence health behaviors. Often, studies have relied on smaller samples, assessed fewer aspects of the social context, lack theoretical frameworks (Andreeva et al., 2011; Wolin et al., 2006), and focus on a single ethnic group (i.e., Mexican-Americans) (Harley & Eskenazi, 2006; Viruell-Fuentes, 2007). We assessed a broad range of social/contextual factors drawn from a solid conceptual framework in a large sample of low-income Haitians and Latinos from Caribbean and Central American regions.
This study’s exploration of pathways through which acculturation affects health behaviors and how those pathways are affected by the social context is important for initiatives to promote health, since acculturative trajectories are individual and context-specific. While assessment of acculturation can assist with the identification of high-risk audiences for interventions, an understanding of the possible mechanisms and contexts in which acculturation exerts its influence is far more germane to public health efforts, and such factors must be considered in the design of culturally-appropriate interventions. In particular, low acculturation may enable individuals to retain some healthy behaviors, but these behaviors (for example, purchasing culturally-specific foods) may be expensive to retain over a long period of time. This study also confirms the complexity of acculturative processes and supports previous calls for more nuanced conceptualizations of immigration experiences and the influence of socio-contextual factors (Viruell-Fuentes et al., 2012).
Based on our findings, we propose a research agenda to advance the study of immigrant experiences as they relate to health. First, given the relatively small R2 in our models, it is critical to consider broader-level social/contextual factors – from neighborhood and other place-specific indicators to social norms and gender roles—that may serve as key determinants of health behaviors, over and above the construct of acculturation. There is also a need to address the macro-context of immigration policies and labor practices, which likely play key roles in immigrant health (Viruell-Fuentes, 2007). Moreover, factors beyond the social context (e.g., gene-environment interactions, spirituality/religiosity) may have important, though as yet unexamined, influences.
Second, exploring interactions between acculturation and social/contextual factors may uncover important strategies for intervening upon health habits. For example, our findings indicate that acculturation and economic circumstances may work in tandem to influence diet. Future studies should utilize measures of acculturation that examine both acculturation and enculturation, as well as items specific to the health behaviors under study (e.g., preference for traditional foods). Moreover, there is the need to consider the ways in which intersectionality operates to influence health behaviors and decisions. Such information could be used to capture the diverse patterns of behavior, both within and across ethnic groups.
Finally, using prospective studies will allow for testing of causal mechanisms underlying relationships between acculturation on health behaviors. Overall, understanding the dynamic, reciprocal and multi-dimensional aspects of immigration experiences that impact health behaviors will enable the development of effective health promotion and disease prevention programs in this growing segment of society.
Supplementary Material
Table 2.
Bivariate associations between social/contextual factors and health behaviors, HIC Study
| Independent/covariates | Healthy Eating Index | Moderate and Vigorous Activity (hr/wk) | Current Smoker |
|---|---|---|---|
| Mean ±s.d. | Mean ±s.d. | N (%) | |
|
| |||
| Overall | −0.01 ± 1.84 | 1.90 ± 1.46 | 177 (21.4%) |
|
| |||
| Age | |||
| 18–29 | −0.63±1.99* | 1.99±1.52* | 42(23.7%)* |
| 30–39 | 0.03±1.74 | 2.17±1.36 | 29(16.4%) |
| 40–49 | 0.03±1.84 | 2.14±1.5 | 40(22.6%) |
| 50–59 | 0.36±1.59 | 1.94±1.65 | 43(24.3%) |
| 60–70+ | 0.16±1.91 | 1.06±0.92 | 23(13%) |
|
| |||
| Gender | |||
| Male | −0.25±1.99* | 2±1.58 | 46(26%)* |
| Female | 0.05±1.79 | 1.88±1.43 | 131(74%) |
|
| |||
| Marital Status | |||
| No | −0.1±1.87 | 1.86±1.43 | 134(75.7%)* |
| Yes | 0.15±1.76 | 2.01±1.53 | 43(24.3%) |
|
| |||
| Education | |||
| Grade school | 0.19±1.52 | 1.44±1.14* | 19(11.9%)* |
| Some HS | −0.22±1.98 | 1.92±1.5 | 36(22.5%) |
| HS or equivalent | −0.23±1.78 | 2.09±1.53 | 44(27.5%) |
| >HS | 0.06±1.99 | 2.11±1.56 | 61(38.1%) |
|
| |||
| Race/Ethnicity | |||
| Hispanic | −0.13±1.75* | 1.95±1.48 | 64(36.6%)* |
| Non-Hispanic White | −0.73±1.9 | 1.71±1.52 | 48(27.4%) |
| Non-Hispanic Black | 0.35±1.84 | 1.94±1.42 | 44(25.1%) |
| Other | −0.08±1.81 | 1.77±1.46 | 19(10.9%) |
|
| |||
| Acculturation Categories | |||
| Very low | −0.29±1.97* | 1.72±1.2* | 6(3.4%)* |
| Low | 0.3±1.65 | 2.19±1.55 | 35(19.9%) |
| Moderate | 0.25±1.54 | 1.61±1.26 | 15(8.5%) |
| US-born | −0.56±2.13 | 1.95±1.54 | 120(68.2%) |
|
| |||
| Perceived Discrimination | |||
| 0 settings | −0.09±1.8 | 1.65±1.34* | 94(53.1%)* |
| 1–2 settings | 0.17±1.75 | 2.13±1.5 | 40(22.6%) |
| 3+ settings | −0.04±2.04 | 2.29±1.61 | 43(24.3%) |
|
| |||
| Material hardship | |||
| No material hardship | −0.08±1.77 | 1.97±1.50 | 100(56.5%) |
| Barely making ends meet | 0.15±1.84 | 1.85±1.48 | 47(26.7%) |
| Material hardship | −0.11±2.00 | 1.84±1.31 | 30(22.1%) |
|
| |||
| Social Ties | |||
| 0 | 0.1±1.79 | 1.82±1.37* | 12(6.8%) |
| 1 | 0.19±1.67 | 1.76±1.4 | 54(30.5%) |
| 2 | −0.06±1.85 | 2.1±1.56 | 68(38.4%) |
| 3 | −0.29±2.06 | 1.78±1.39 | 43(24.3%) |
|
| |||
| Social Support | |||
| 0 | 0.17±1.65 | 1.92±1.4 | 6(3.4%) |
| 1 | 0.12±1.69 | 1.85±1.44 | 44(24.9%) |
| 2 | −0.04±1.87 | 1.93±1.49 | 61(34.5%) |
| 3 | −0.12±1.94 | 1.92±1.47 | 66(37.3%) |
|
| |||
| Perceived Stress† | −0.13* | −0.02 | 8.99±2.95* |
Frequencies (%) presented for categorical outcomes and means (std) presented for continuous outcomes.
p-value ≤ 0.05.
Perceived Stress is the only continuous independent variable, means are presented for categorical outcomes and the Pearson correlation is presented for continuous outcomes.
Research Highlights.
We modeled relationships between acculturation, contextual factors and health behaviors
Acculturation was directly associated with smoking and diet
Less acculturated individuals had healthier diets and were more likely non-smokers
Material hardship may be one mechanism through which acculturation affects diet
Efforts to promote immigrant health should address household financial resources.
Acknowledgments
This research was supported by the National Cancer Institute (grant numbers R01 CA111310-01A1; K05 CA108663-05), Cooperative Agreement Number U48DP001946 from the Centers for Disease Control and Prevention the NIH/NCI Harvard Education Program in Cancer Prevention and Control (R25 CA057713), the NIH/NCI Cancer Related Health Disparities Education and Career Development Program (R25 CA163184), the NIH/NCI Reducing Social Disparities in Cancer Risk (K05 CA108663-05), and an NCI K01 career development award (Grant# CA169041-01).The findings and conclusions in this journal article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. The authors would like to thank the 20 low-income housing sites that participated in this research, and the assistance from the Cambridge, Somerville and Chelsea Public Housing Authorities. The authors also acknowledge the administrative and field staff at the Harvard School of Public Health and Dana-Farber Cancer Institute, and the study participants for their contributions to this project. They also thank Gary Adamkiewicz, Marty Alvarez-Reeves, Amy Harley, Ruth Lederman, Samuel Lipson, Carol Lowenstein, Hannah L. Mills, Laura Tom, Brianna Wadler, and Lorraine Wallace for their contributions to the overall study design and implementation.
Appendix: Summary of LCA model fit indices
| Model Fit Indices | 2 class solution | 3 class solution | 4 class solution |
|---|---|---|---|
| Akaike Information Criteria | 4521.74 | 4326.28 | 4240.93 |
| Bayesian Information Criteria | 4628.98 | 4489.29 | 4459.71 |
| Entropy | 0.79 | 0.87 | 0.88 |
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abraido-Lanza AF, Armbrister AN, Florez KR, Aguirre AN. Toward a theory-driven model of acculturation in public health research. Am J Public Health. 2006;96:1342–1346. doi: 10.2105/AJPH.2005.064980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abraido-Lanza AF, Chao MT, Florez KR. Do healthy behaviors decline with greater acculturation? Implications for the Latino mortality paradox. Soc Sci Med. 2005;61:1243–1255. doi: 10.1016/j.socscimed.2005.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Acevedo-Garcia D, Bates LM. Latino Health Paradoxes: Empirical Evidence, Explanations, Future Research, and Implications. In: Rodríguez H, Sáenz R, Menjívar C, editors. Latinas/os in the United States: Changing the Face of América. Springer US; 2008. pp. 101–113. [Google Scholar]
- Acevedo-Garcia D, Sanchez-Vaznaugh EV, Viruell-Fuentes EA, Almeida J. Integrating social epidemiology into immigrant health research: a cross-national framework. Soc Sci Med. 2012;75:2060–2068. doi: 10.1016/j.socscimed.2012.04.040. [DOI] [PubMed] [Google Scholar]
- Alegria M. The challenge of acculturation measures: what are we missing? A commentary on Thomson & Hoffman-Goetz. Social Science and Medicine. 2009;69:996–998. doi: 10.1016/j.socscimed.2009.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andreeva VA, Cockburn MG, Yaroch AL, Unger JB, Rueda R, Reynolds KD. Preliminary evidence for mediation of the association between acculturation and sun-safe behaviors. Archives of Dermatology. 2011;147:814–819. doi: 10.1001/archdermatol.2011.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayala GX, Baquero B, Klinger S. A systematic review of the relationship between acculturation and diet among Latinos in the United States: implications for future research. Journal of the American Dietetic Association. 2008;108:1330–1344. doi: 10.1016/j.jada.2008.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett GG, Wolin KY, Okechukwu CA, Arthur CM, Askew S, Sorensen G, et al. Nativity and cigarette smoking among lower income blacks: results from the Healthy Directions Study. J Immigr Minor Health. 2008;10:305–311. doi: 10.1007/s10903-007-9088-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berrigan D, Dodd K, Troiano RP, Reeve BB, Ballard-Barbash R. Physical activity and acculturation among adult Hispanics in the United States. Res Q Exerc Sport. 2006;77:147–157. doi: 10.1080/02701367.2006.10599349. [DOI] [PubMed] [Google Scholar]
- Berry JW, Sam DL. Acculturation and adaptation. In: Berry JW, Segall MH, Kigitcibasi C, editors. Handbook of Cross-cultural Psychology: Social behavior and applications. Boston: Allyn and Bacon; 1997. pp. 291–326. [Google Scholar]
- Bethel JW, Schenker MB. Acculturation and smoking patterns among Hispanics: a review. Am J Prev Med. 2005;29:143–148. doi: 10.1016/j.amepre.2005.04.014. [DOI] [PubMed] [Google Scholar]
- Cantor D, Covell J, Davis T, Park I, Rizzo L. Health Information National Trends Survey 2005 Final Report. 2008. [Google Scholar]
- Caspi CE, Kawachi I, Subramanian SV, Tucker-Seeley R, Sorensen G. The social environment and walking behavior among low-income housing residents. Soc Sci Med. 2013;80:76–84. doi: 10.1016/j.socscimed.2012.11.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Celeux G, Soromenho G. An entropy criterion for assessing the number of clusters in a mixture model. Journal of Classification. 1996;13:195–212. [Google Scholar]
- Clark L, Hofsess L. Acculturation. In: Loue S, editor. Handbook of Immigrant Health. New York: Plenum Press; 1998. pp. 37–59. [Google Scholar]
- Cohen S. Social relationships and health. American Psychologist. 2004;59:676–684. doi: 10.1037/0003-066X.59.8.676. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24:385–396. [PubMed] [Google Scholar]
- Constantine ML, Rockwood TH, Schillo BA, Alesci N, Foldes SS, Phan T, et al. Exploring the relationship between acculturation and smoking behavior within four Southeast Asian communities of Minnesota. Nicotine Tob Res. 2010;12:715–723. doi: 10.1093/ntr/ntq070. [DOI] [PubMed] [Google Scholar]
- Cook B, Alegria M, Lin JY, Guo J. Pathways and correlates connecting Latinos’ mental health with exposure to the United States. Am J Public Health. 2009;99:2247–2254. doi: 10.2105/AJPH.2008.137091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Medicine and Science in Sports and Exercise. 2003;35:1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- Cruz TH, Marshall SW, Bowling JM, Villaveces A. The Validity of a Proxy Acculturation Scale Among US Hispanics. Hispanic Journal of Behavioral Sciences. 2008;30:425–446. [Google Scholar]
- Desilets MC, Rivard M, Shatenstein B, Delisle H. Dietary transition stages based on eating patterns and diet quality among Haitians of Montreal, Canada. Public Health Nutr. 2007;10:454–463. doi: 10.1017/S1368980007222931. [DOI] [PubMed] [Google Scholar]
- Esparza J, Fox C, Harper IT, Bennett PH, Schulz LO, Valencia ME, et al. Daily energy expenditure in Mexican and USA Pima indians: low physical activity as a possible cause of obesity. International Journal of Obesity and Related Metabolic Disorders. 2000;24:55–59. doi: 10.1038/sj.ijo.0801085. [DOI] [PubMed] [Google Scholar]
- Gorber SC, Schofield-Hurwitz S, Hardt J, Levasseur G, Tremblay M. The accuracy of self-reported smoking: A systematic review of the relationship between self-reported and cotinine-assessed smoking status. Nicotine & Tobacco Research. 2009;11:12–24. doi: 10.1093/ntr/ntn010. [DOI] [PubMed] [Google Scholar]
- Gordon-Larsen P, Harris KM, Ward DS, Popkin BM. Acculturation and overweight-related behaviors among Hispanic immigrants to the US: the National Longitudinal Study of Adolescent Health. Social Science and Medicine. 2003;57:2023–2034. doi: 10.1016/s0277-9536(03)00072-8. [DOI] [PubMed] [Google Scholar]
- Harley K, Eskenazi B. Time in the United States, social support and health behaviors during pregnancy among women of Mexican descent. Soc Sci Med. 2006;62:3048–3061. doi: 10.1016/j.socscimed.2005.11.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heaney CA, Israel BA. Social networks and social support. In: Glanz K, Lewis FM, Rimer BK, editors. Health behavior and health education. San Francisco, CA: Jossey-Bass Inc; 1997. [Google Scholar]
- Hebert JR, Hurley TG, Peterson KE, Resnicow K, Thompson FE, Yaroch AL, et al. Social desirability trait influences on self-reported dietary measures among diverse participants in a multicenter multiple risk factor trial. Journal of Nutrition. 2008;138:226s–234s. doi: 10.1093/jn/138.1.226S. [DOI] [PubMed] [Google Scholar]
- Horne R, Hankins M, Jenkins R. The Satisfaction with Information about Medicines Scale (SIMS): a new measurement tool for audit and research. Quality in Health Care. 2001;10:135–140. doi: 10.1136/qhc.0100135... [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L-t, Bentler PM. Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological Methods. 1998;3:424–453. [Google Scholar]
- Hunt LM, Schneider S, Comer B. Should “acculturation” be a variable in health research? A critical review of research on US Hispanics. Soc Sci Med. 2004;59:973–986. doi: 10.1016/j.socscimed.2003.12.009. [DOI] [PubMed] [Google Scholar]
- Jasinskaja-Lahti I, Liebkind K. A Structural Model of Acculturation and Well-Being Among Immigrants from the Former USSR in Finland. European Psychologist. 2007;12:80–92. [Google Scholar]
- Jasso G, Massey D, Rosenzweig M, Smith J. The New Immigrant Survey in the US: The Experience over Time. Migration Information Source 2003 [Google Scholar]
- Kaplan MS, Huguet N, Newsom JT, McFarland BH. The association between length of residence and obesity among Hispanic immigrants. American Journal of Preventive Medicine. 2004;27:323–326. doi: 10.1016/j.amepre.2004.07.005. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Mcleod JD. Sex-Differences in Vulnerability to Undesirable Life Events. American Sociological Review. 1984;49:620–631. [Google Scholar]
- Kish L. Sampling Organizations and Groups of Unequal Sizes. American Sociological Review. 1965;30:564–572. [PubMed] [Google Scholar]
- Krieger N. Discrimination and health. In: Berkman LF, Kawachi I, editors. Social Epidemiology. New York: Oxford University Press; 2000. pp. 36–75. [Google Scholar]
- Krieger N, Smith K, Naishadham D, Hartman C, Barbeau EM. Experiences of discrimination: validity and reliability of a self-report measure for population health research on racism and health. Social Science and Medicine. 2005;61:1576–1596. doi: 10.1016/j.socscimed.2005.03.006. [DOI] [PubMed] [Google Scholar]
- Lara M, Gamboa C, Kahramanian MI, Morales LS, Bautista DE. Acculturation and Latino health in the United States: a review of the literature and its sociopolitical context. Annu Rev Public Health. 2005;26:367–397. doi: 10.1146/annurev.publhealth.26.021304.144615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus RS, Folkman S. Stress, appraisal, and coping. Springer Publishing Company; 1984. [Google Scholar]
- Lindstrom M, Moden B, Rosvall M. A life-course perspective on economic stress and tobacco smoking: a population-based study. Addiction. 2013;108:1305–1314. doi: 10.1111/add.12143. [DOI] [PubMed] [Google Scholar]
- Lopez-Class M, Castro FG, Ramirez AG. Conceptions of acculturation: a review and statement of critical issues. Soc Sci Med. 2011;72:1555–1562. doi: 10.1016/j.socscimed.2011.03.011. [DOI] [PubMed] [Google Scholar]
- Mills BA, Caetano R. Decomposing associations between acculturation and drinking in Mexican Americans. Alcohol Clin Exp Res. 2012;36:1205–1211. doi: 10.1111/j.1530-0277.2011.01712.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén L, Muthén B. Computer software. Los Angeles: author; 2007. Mplus: Statistical Analysis with Latent Variables (Version 4.21) [Google Scholar]
- Muthen LK, Muthen BO. Mplus User’s Guide. Los Angeles, CA: Muthen & Muthen; 1998–2011. [Google Scholar]
- Nord M, Andrews M, Carlson S. Household Food Security in the United States. 2004. [Google Scholar]
- O’Loughlin J, Maximova K, Tan Y, Gray-Donald K. Lifestyle risk factors for chronic disease across family origin among adults in multiethnic, low-income, urban neighborhoods. Ethnicity and Disease. 2007;17:657–663. [PubMed] [Google Scholar]
- Patil CL, Hadley C, Nahayo PD. Unpacking dietary acculturation among new Americans: results from formative research with African refugees. J Immigr Minor Health. 2009;11:342–358. doi: 10.1007/s10903-008-9120-z. [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Lieberman MA, Menaghan EG, Mullan JT. The stress process. Journal of Health and Social Behavior. 1981;22:337–356. [PubMed] [Google Scholar]
- Perez-Escamilla R, Putnik P. The role of acculturation in nutrition, lifestyle, and incidence of type 2 diabetes among Latinos. J Nutr. 2007;137:860–870. doi: 10.1093/jn/137.4.860. [DOI] [PubMed] [Google Scholar]
- Pichon LC, Arredondo EM, Roesch S, Sallis JF, Ayala GX, Elder JP. The relation of acculturation to Latinas’ perceived neighborhood safety and physical activity: a structural equation analysis. Annals of Behavioral Medicine. 2007;34:295–303. doi: 10.1007/BF02874554. [DOI] [PubMed] [Google Scholar]
- Portes A, Zhou MIN. The New Second Generation: Segmented Assimilation and its Variants. The ANNALS of the American Academy of Political and Social Science. 1993;530:74–96. [Google Scholar]
- Reitz JG. Host Societies and the Reception of Immigrants: Research Themes, Emerging Theories and Methodological Issues. International Migration Review. 2002;36:1005–1019. [Google Scholar]
- Riedel J, Wiesmann U, Hannich HJ. An integrative theoretical framework of acculturation and salutogenesis. Int Rev Psychiatry. 2011;23:555–564. doi: 10.3109/09540261.2011.637912. [DOI] [PubMed] [Google Scholar]
- Rifas-Shiman SL, Willett WC, Lobb R, Kotch J, Dart C, Gillman MW. PrimeScreen, a brief dietary screening tool: reproducibility and comparability with both a longer food frequency questionnaire and biomarkers. Public Health Nutr. 2001;4:249–254. doi: 10.1079/phn200061. [DOI] [PubMed] [Google Scholar]
- Rimm EB, Giovannucci EL, Stampfer MJ, Colditz GA, Litin LB, Willett WC. Reproducibility and validity of an expanded self-administered semiquantitative food frequency questionnaire among male health professionals. American Journal of Epidemiology. 1992;135:1114–1126. doi: 10.1093/oxfordjournals.aje.a116211. discussion 1127–1136. [DOI] [PubMed] [Google Scholar]
- Rost J, Langeheine R. A guide through latent structure models for categorical data. In: Rost J, Langeheine R, editors. Applications of Latent Trait and Latent Class Models in the Social Sciences. Waxmann Münster; 1997. [Google Scholar]
- Singh GK, Siahpush M. Ethnic-immigrant differentials in health behaviors, morbidity, and cause-specific mortality in the United States: an analysis of two national data bases. Human Biology. 2002;74:83–109. doi: 10.1353/hub.2002.0011. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. Poverty Data. US Census Bureau; 2008. [Google Scholar]
- U.S. Department of Housing and Urban Development. FY 2013 HUD Income Limits Briefing Material. 2012. [Google Scholar]
- Umberson D, Chen MCD, House JS, Hopkins K, Slaten E. The effect of social relationships on psychological well-being: Are men and women really so different? American Sociological Review. 1996;61:837–857. [Google Scholar]
- Umberson D, Crosnoe R, Reczek C. Social Relationships and Health Behavior Across the Life Course. Annual Review of Sociology, Vol 36. 2010;36:139–157. doi: 10.1146/annurev-soc-070308-120011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velasquez KS, Holahan CK, You X. Relationship of perceived environmental characteristics to leisure-time physical activity and meeting recommendations for physical activity in Texas. Prev Chronic Dis. 2009;6:A24. [PMC free article] [PubMed] [Google Scholar]
- Viruell-Fuentes EA. Beyond acculturation: immigration, discrimination, and health research among Mexicans in the United States. Social Science and Medicine. 2007;65:1524–1535. doi: 10.1016/j.socscimed.2007.05.010. [DOI] [PubMed] [Google Scholar]
- Viruell-Fuentes EA, Miranda PY, Abdulrahim S. More than culture: structural racism, intersectionality theory, and immigrant health. Soc Sci Med. 2012;75:2099–2106. doi: 10.1016/j.socscimed.2011.12.037. [DOI] [PubMed] [Google Scholar]
- Webb AL, Schiff A, Currivan D, Villamor E. Food Stamp Program participation but not food insecurity is associated with higher adult BMI in Massachusetts residents living in low-income neighbourhoods. Public Health Nutr. 2008;11:1248–1255. doi: 10.1017/S1368980008002309. [DOI] [PubMed] [Google Scholar]
- Wilde P, McNamara P, Ranney C. The Effect on Dietary Quality of Participation in the Food Stamp and WIC Programs. Food Assistance and Nutrition Research Report Number. 2000;9 [Google Scholar]
- Wolin KY, Colditz G, Stoddard AM, Emmons KM, Sorensen G. Acculturation and physical activity in a working class multiethnic population. Preventive Medicine. 2006;42:266–272. doi: 10.1016/j.ypmed.2006.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong SL, Shields M, Leatherdale S, Malaison E, Hammond D. Assessment of validity of self-reported smoking status. Health Reports. 2012;23:47–53. [PubMed] [Google Scholar]
- Yip T, Gee GC, Takeuchi DT. Racial discrimination and psychological distress: the impact of ethnic identity and age among immigrant and United States-born Asian adults. Dev Psychol. 2008;44:787–800. doi: 10.1037/0012-1649.44.3.787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon E, Hacker J, Hewitt A, Abrams M, Cleary S. Social connectedness, discrimination, and social status as mediators of acculturation/enculturation and well-being. J Couns Psychol. 2012;59:86–96. doi: 10.1037/a0025366. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


