Abstract
Food insecurity and drug use are closely connected in the context of poverty, and both have been suggested to interfere with HIV medication adherence among people living with HIV/AIDS (PLWH). Yet the potential interaction between the two factors on adherence has not been examined. For this study we collected longitudinal data on HIV medication adherence among PLWH in Atlanta, GA, to assess a possible synergistic effect between the two factors on HIV medication adherence. People informed about the study came to the research site and completed an audio computer-assisted self-interview and instructions for pill counting. Over the next five weeks participants received three unscheduled follow-up phone assessments conducted two weeks apart to collect pill counts of their HIV medication. The prevalence of food insecurity was 60% (488) and that of drug use was 33% (274) in the sample of 809 participants. Among 770 participants who completed follow-up phone assessments, both food insecurity and drug use were associated with HIV medication adherence after adjusting for socio-demographic characteristics. The negative association between drug use and adherence persisted after further adjusting for health-related characteristics. Moreover, drug use appeared to moderate the effect of food insufficiency on adherence, with drug users who were food insufficient being the least likely to achieve 85% adherence. Results from the current study demonstrate a synergism between food insecurity and drug use that may impede adherence among PLWH. The findings imply that the disruptive effects of food insecurity and drug use on adherence are likely to be intensified with the presence of each other, and encourage interventions to address the problem of HIV medication adherence from a multi-faceted perspective that takes into account detrimental combination of problem factors.
Keywords: Food insecurity, Drug use, HIV, ART, Adherence
INTRODUCTION
Food insecurity, defined as ‘limited or uncertain availability of nutritionally adequate and safe foods, or limited ability to acquire acceptable foods in socially acceptable ways’, is prevalent among people living with HIV/AIDS (PLWH), including those living in resource rich countries (USDA, 2006). The prevalence of food insecurity among PLWH in the United States and Canada is estimated to exceed 50% (Normen et al., 2005; Weiser, Bangsberg, et al., 2009; Weiser, Fernandes, et al., 2009). Growing evidence links food insecurity to incomplete and unsuccessful HIV treatment (Au et al., 2006; Weiser, Fernandes, et al., 2009; Weiser et al., 2011). Two prospective studies have shown that food insecurity predicts non-adherence (adherence rate lower than 90%) to HIV medication among PLWH in rural Uganda and among homeless PLWH in USA (Weiser, Fernandes, et al., 2009; Weiser, Frongillo, et al., 2009). Similar findings were also reported in a cross-sectional study in which food insecurity was associated with less than 95% of adherence among PLWH in Congo (Musumari et al., 2014). Although one cross-sectional study failed to show an association between food insecurity and non-adherence (Anema et al., 2013), most research supports a relationship between the two.
Food insecurity is one of several co-occurring adverse conditions of poverty that affects anti-retroviral therapy (ART) adherence (Leaver, Bargh, Dunn, & Hwang, 2007; Miller et al., 2011; Piot, Greener, & Russell, 2007). Among other poverty-related characteristics, illicit drug use is intimately related to food insecurity (Hendricks & Gorbach, 2009). Approximately 30%-70% of drug using-individuals experience some level of food insecurity (Anema et al., 2013; Anema et al., 2010; Strike, Rudzinski, Patterson, & Millson, 2012). Moreover, both drug use and food insecurity have been found to compromise pharmacokinetic efficacy of ART, reduce immunological response, and increase mortality of PLWH (Anema, Vogenthaler, Frongillo, Kadiyala, & Weiser, 2009; Antoniou & Tseng, 2002). A recent study of injection drug users living with HIV showed that those who were food insecure when first initiating ART were twice as likely to die compared to those who were food secure (Anema et al., 2013). Similar to food insecurity, drug use was also associated with poorer adherence. One study for example found drug use to be associated with over a fourfold greater risk of <90% of adherence among PLWH in Los Angeles (Hinkin et al., 2007).
The interplay between food insecurity and illicit drug use can be discussed in the framework of “syndemics” – the co-occurrence of multiple interactive health-related problems that interact at biological and social level (Singer & Clair, 2003). The emergence of a syndemic is of particular concern in public health because it represents an aggregation of adverse conditions and the potential for multiple conditions to synergize and exacerbate burden of disease (Alcabes, Schoenbaum, & Klein, 1993; Ensoli & Sirianni, 2002; Rose, Sinka, Watson, Mortimer, & Charlett, 2002). While previous research has examined the co-occurrence of HIV infection, food insecurity and substance use, we are not aware of any study to examine the potential synergistic effect between substance use and food insecurity on HIV treatment adherence.
The current study seeks to fill an important gap in research by assessing the moderating effects of substance use on the association between food insecurity and anti-retroviral therapy adherence in PLWH. Adherence to ART is a critical predictor of treatment success and HIV-related survival. Sub-optimal adherence will lead to a series of clinical consequences including failure of viral suppression, emergence of drug resistance, increased progression of disease and greater mortality (Bartlett, 2002; Sethi, Celentano, Gange, Moore, & Gallant, 2003; Wood et al., 2006). Consistently higher ART adherence is also essential to reducing the risk of sexual transmission of HIV (Cohen et al., 2011). Based on previous research findings and given the implications of a potential interactive relationship between co-existing health problems in the framework of syndemics, we hypothesize that the combination of food insecurity and active substance use may have more detrimental effects on health behaviors and health outcomes than either condition alone. Specifically, we hypothesized that food insecurity and drug use would both be associated with poorer ART adherence among PLWH. In addition, we predicted that the association between food insecurity and ART adherence would be moderated by drug use, such that drug-using individuals who experience food insecurity would demonstrate the poorest levels of ART adherence relative to others who are either food insecure or using drugs, or neither food insecure nor using drugs.
METHOD
Research setting
The site of the study was in Atlanta, Georgia, which had 23,138 reported cases of HIV infection, with an incidence rate of 30.3 per 100,000 population in 2010. This number exceeds the average rate of 19.6 per 100,000 population in major US cities. The poverty rate (24.4%) in Atlanta was also much higher than the average rate (13.7%) in the state of Georgia. The research base for the current study was located in a local community in Atlanta.
Participant Recruitment and Eligibility
Participants were informed about the study by word-of-mouth and through flyers at AIDS social service providers and infectious disease clinics. Each participant was given three study flyers to distribute to other PLWH they know. Eligible participants needed to be age 18 or older, being HIV positive and were currently taking HIV medication. All potential participants were asked to present proof of positive HIV status, and show a photo ID with matching ART prescription bottle. Eligible participants were provided with informed voluntary written consent to participate.
Procedures
The study was conducted in the pre-randomization period of an intervention trial for the purpose of collecting prospective baseline measures of ART adherence among potential participants. The entire study lasted approximately five weeks. Eligible participants first went through an informed consent process after which they were trained in the study procedures. Participants consented into the study then completed an audio computer-assisted self-interview (ACASCI). Each participant was then provided with a service-restricted cell phone for project contacts and emergency use (e.g. 911). Over the next month each participant was given three unscheduled phone assessments conducted two weeks apart. The phone assessments were conducted by trained phone assessors and primarily measured ART adherence using unannounced pill counts. Participants also provided their most recent HIV RNA (viral load) and CD4 cell counts from their medical records. The study procedures were approved by the University of Connecticut Institutional Review Board.
Measures
Demographic Characteristics
Participants provided basic demographic information regarding their age, sex, level of education (from 6th grade to completed college), annual income, ethnicity and etc.
Food Insecurity
We used eight items from the US Food Security Scale that have been validated in the past research and used by the US Census Bureau (Coates, Swindale, & Bilinsky, 2007). Food insecurity indicators were collected with respect to whether the participant had ever experienced a series of situations related to food insufficiency and food security. A detailed list of the indicators can be found in Table 1.
Table 1.
Distribution of food insecurity indicators by drug-using status*
| Drug users (N=274) |
Non-drug users (N=535) |
|
|---|---|---|
|
|
||
| Items of food insecurity* | %(n) | %(n) |
| 1. Worried if food would run out before having money to buy more. |
64.23(176) | 48.22(258) |
| 2. Food didn't last and didn't have money to get more. |
66.42(182) | 48.22(258) |
| 3. Couldn't afford to eat balanced meals. |
61.31(168) | 44.67(239) |
| 4. Adults in household cut meal size for not having money for food. |
46.72(128) | 30.84(165) |
| 5. Eat less than one felt like eating for not having money for food. |
53.28(146) | 32.90(176) |
| 6. Being hungry without eating for not being able to afford food. |
40.88(112) | 21.50(115) |
| 7. Lose weight for not having enough money for food. |
34.67(95) | 15.70(84) |
| 8. Adults in household not eat for a whole day for no money for food. |
20.44(56) | 10.09(54) |
Distribution of each indicator differs by drug-using status at significance level of p=0.001
Current Drug Use
Drugs assessed in the study were marijuana, powder/ crack cocaine, poppers/nitrite inhalants, methamphetamine/crystal meth, and any injected drugs. Participants were asked the frequency by which they use each drug in the past month. Those who had used any one of the listed drugs at least once in the past month were categorized into the drug-using group, while those who reported zero use of all drugs were placed into non-drug-using group.
Alcohol use
The 3-item Consumption Subscale of the Alcohol Use Disorder Identification Test (AUDIT-C) was used to assess frequency and quantity of alcohol use (Maisto, Conigliaro, McNeil, Kraemer, & Kelley, 2000). The final score is on a scale of 0-12 and men with a score of 4 or more or women with a score of 3 or more were considered as heavy drinkers.
ART Side Effects
We measured side effects of ART through 11 symptoms including nausea, diarrhea, stomach pain, and etc. Responses to each item ranged between 0=not experiencing to 3=severely experiencing and were summed into a final composite score with higher scores indicating stronger side effects (Carrieri, Villes, & 2007).
Depression
We used the 20-item Center for Epidemiologic Studies Depression Scale (CES-D) to assess symptoms of depression (Radloff, 1977). Based on the established scoring system, the final score (0-60) was categorized into no depression (<15), mild to moderate depression (15-21), and major depression (>21).
Adherence Self-efficacy
This 14-item measure (Cronbach’s alpha = 0.95) was adapted from the HIV Adherence Self-Efficacy Scale (HIV-ASES) with two additional items (i.e. “How certain are you that you can follow your doctor’s order?”; “How certain are you that you can keep your next doctor’s appointment?”).
ART Adherence
Telephone-based unannounced pill counts have been validated as a reliable and accurate measure of HIV treatment adherence (Kalichman et al., 2008). Each participant was given an office-based training session in the procedure of pill counting at baseline. Pill counts were conducted for each of the antiretroviral medications taken by the participants. Pharmacy information from pill bottles of each medication was also obtained to verify the number of pills dispensed between calls. Adherence was calculated as the ratio (percentage) of pills counted relative to pills prescribed, taking into account the number of pills dispensed. Two consecutive pill counts were necessary for computing one adherence data point and the three assessments produced two adherence data points for each participant. Optimal adherence is defined as having an adherence ratio at 85% of ART medications taken over the 4 week period (Bangsberg, Kroetz, & Deeks, 2007).
CD4 Cell Count and Viral Load
We used medical record-abstracted values of most recent absolute CD4 cell counts and PCR determined viral load. Chart-abstracted values were used for continuous absolute measures of CD4 count and viral loads with <75 copies/ml being coded as undetectable viral load.
Analysis
Data were analyzed using Stata (version 12) (StataCorp., 2011). In the initial descriptive analyses, we compared people with and without food insecurity among drug users and non-drug users respectively. For the ease of description, we categorized education into below and above college level, CD4 cell count into above or below 200, and viral load into undetectable or detectable. Side effects and adherence self-efficacy were dichotomized at the median. We also report descriptive statistics by adherence status, using Wilcoxon rank-sum test for continuous variables, and χ2 test for categorical variables. We then assessed bivariate associations of optimal adherence with relevant variables, using generalized estimating equation (GEE) modeling for logistic regression with robust variance estimator to adjust for within-participants correlation. All variables were kept in their observed forms during regression analysis, expect for viral load which was log transformed.
In the multivariate GEE analysis, we adopted a hierarchical multiple regression approach by dividing variables into three blocks. The first block “food and drug” was initially introduced in the model, followed by block 2 “social demographic characteristics”, and then block 3 “biomarkers and adherence-related characteristics”. Variables were selected into multiple regression models based on previous literature and bivariate associations, as well as examination of multi-collinearity, and QIC (quasilikelihood under the independence model criterion) score (Pan, 2001). Educational level, income and gender were therefore excluded from the models for being unassociated with adherence and costly to model parsimony. CD4 cell count was kept in the model given its conceptual relevancy despite of being insignificantly associated with adherence in the current sample. To test the existence of a potential interaction between food insecurity and substance use on ART adherence, we introduced an interaction term in the final model after controlling for relevant variables. All models were adjusted for the two time-points of data collection. A sensitivity analysis was also performed using 90% and 95% cut-off point for optimal adherence and the results were not materially different from analysis using 85% adherence.
RESULTS
Distribution of Food Insecurity Indicators by Drug-using Status
The percentages of participants experiencing each indicator of food insecurity are shown by drug-using status in Table 1. The indicators were listed in an increased order of severity, and there was a declining trend in the prevalence of each condition as the severity increased. Drug-using participants were significantly more likely to experience each condition of food insecurity compared to non-drug users.
Food Insecurity and Relevant Characteristics by Drug-using Status
Among 809 study participants, 488 (60.32%) were food insecure and 274 (33.87%) were current drug users. The prevalence of food insecurity was 71.53% within drug users, and 54.58% within non-drug users. Food insecurity and drug use overlapped among 196 (24.23%) participants. Table 2 compares the demographic, health and psychosocial characteristics of participants who were food secure and insecure by drug-using status. We found that participants who were food insecure were younger, with less people above 50 years of age than those who had sufficient food. Food insecure participants were more likely to have severe depressive symptoms, experience side effects from ART and express lower adherence self-efficacy. Overall 75.38% of food insecure participants failed to achieve optimal adherence, and a comparable proportion (71.72%) of drug using participants also failed to do so. Patterns of moderation by drug using status also emerged in descriptive analysis. Nearly half (47.06%) of the food insecure drug users did not achieve optimal adherence, but this proportion dropped to 25.54% among people who were both food secure and not using drugs. Among drug users, participants who were food insecure were more likely to have detectable viral load as compared to those who were food secure. Among non-drug users, participants who were food insecure appeared to have earned less income, and have lower level of CD4 cell counts than those who were food secure.
Table 2.
Baseline characteristics of participants by status of food security and substance use (N=813)
| HIV+ Drug Users | HIV+ Non-drug Users | |||||
|---|---|---|---|---|---|---|
|
|
||||||
| Food secure (n=78) |
Food insecure (n=196) |
p-value | Food secure (n=243) |
Food insecure (n=291) |
p-value | |
| Age | 0.003 | <0.001 | ||||
| ≤30 | 10.26(8) | 8.67(17) | 2.88(7) | 7.90(23) | ||
| 30-50 | 37.18(29) | 59.18(116) | 41.98(102) | 55.67(162) | ||
| ≥50 | 52.56(41) | 32.14(63) | 55.14(134) | 36.43(106) | ||
| Gender | 0.066 | 0.897 | ||||
| Female | 10.26(8) | 19.49(38) | 35.12(85) | 34.59(101) | ||
| Male | 89.74(70) | 80.51(158) | 64.99(157) | 65.41(191) | ||
| Education | 0.567 | 0.602 | ||||
| Below college | 48.72(38) | 44.90(89) | 52.26(127) | 50.00(146) | ||
| College and above | 51.28(40) | 55.10(108) | 47.74(116) | 50.00(146) | ||
| Annual income | 0.543 | 0.003 | ||||
| $0-$10,000 | 64.10(50) | 66.84(131) | 58.85(143) | 72.16(210) | ||
| $11,000-$20,000 | 25.64(20) | 27.55(54) | 30.45(74) | 21.65(63) | ||
| $21,000-$30,000 | 6.41(5) | 4.08(8) | 4.94(12) | 4.47(13) | ||
| Over $30,000 | 3.85(3) | 1.53(3) | 5.76(14) | 1.72(5) | ||
| Ethnicity | 0.941 | 0.558 | ||||
| Non-African-American | 11.54(9) | 11.22(22) | 7.82(19) | 9.25(27) | ||
| African-American | 88.46(69) | 88.78(174) | 92.18(224) | 90.75(265) | ||
| Side effect (range: 0-36) | <0.001 | <0.001 | ||||
| ≤5 | 74.36(58) | 38.27(75) | 74.07(180) | 45.55(133) | ||
| >5 | 25.64(20) | 61.73(121) | 25.93(63) | 54.45(159) | ||
| CD4 cell count | 0.588 | 0.053 | ||||
| ≤200 | 14.85(11) | 17.65(33) | 12.89(29) | 19.54(53) | ||
| >200 | 85.14(63) | 82.35(154) | 87.11(196) | 80.66(221) | ||
| Viral load | 0.001 | 0.333 | ||||
| Undetectable (<75) | 66.22(49) | 43.09(81) | 56.89(128) | 52.55(144) | ||
| Detectable (≥75) | 33.78(25) | 56.91(107) | 43.11(97) | 47.45(130) | ||
| Heavy drinker | 0.147 | 0.474 | ||||
| No | 75.64(59) | 66.67(130) | 88.38(213) | 86.30(252) | ||
| Yes | 24.36(19) | 33.33(65) | 11.62(28) | 13.70(40) | ||
| Adherence self-efficacy | <0.001 | <0.001 | ||||
| <8 | 33.33(26) | 66.67(130) | 34.98(85) | 55.48(162) | ||
| ≥8 | 66.67(52) | 33.33(65) | 65.02(158) | 44.52(130) | ||
| Depression | <0.001 | <0.001 | ||||
| None | 57.69(45) | 20.92(41) | 60.08(146) | 28.77(84) | ||
| Mild/moderate | 25.64(20) | 24.49(48) | 20.99(51) | 25.34(74) | ||
| Major | 16.67(13) | 54.59(108) | 18.93(46) | 45.89(134) | ||
| Average adherence ≥ 85% | 0.001 | 0.483 | ||||
| No | 24.66(18) | 47.06(88) | 25.54(59) | 28.32(79) | ||
| Yes | 75.34(55) | 52.94(99) | 74.46(172) | 71.68(200) | ||
Bivariate Associations between Optimal Adherence and Relevant Factors
Participant characteristics by optimal adherence are shown in Table 3. Follow-up adherence data were available among 770 participants. On average, a total of 244 (31.69%) participants failed to achieve optimal adherence. Both food insecurity and drug use were negatively associated with optimal adherence. Participants who achieved optimal adherence were older on average than those who did not. Participants who reported higher adherence self-efficacy were more likely to be adherent, while those who took more HIV medications per day, reported more side effects, had higher viral load and engaged in heavy drinking were less likely to achieve optimal adherence.
Table 3.
Bi-variate analysis of optimal adherence using GEE with robust variance estimator
| Average adherence<85% |
Average adherence≥85% |
Optimal adherence (≥85%) | |||
|---|---|---|---|---|---|
|
|
|||||
| (n=244) | (n=526) | P-value | OR | 95%CI | |
| Food and Drug | |||||
| Food insecurity (n, %) | 0.002 | ||||
| No | 25.33(77) | 74.67(227) | REF | REF | |
| Yes | 35.84(167) | 64.16(299) | 0.62** | (0.47-0.81) | |
| Drug use (n, %) | <0.001 | ||||
| No | 27.06(138) | 72.94(372) | REF | REF | |
| Yes | 40.77(106) | 59.23(154) | 0.53*** | (0.41-0.70) | |
| Social Demographic | |||||
| Characteristics | |||||
| Age (mean, sd) | 45.57(9.54) | 47.64(8.34) | 0.013 | 1.03*** | (1.01-1.04) |
| Gender | 0.682 | ||||
| Female (n, %) | 32.783(72) | 67.27(148) | REF | REF | |
| Male (n, %) | 31.20(171) | 68.80(377) | 0.96 | (0.72-1.28) | |
| Education (mean, sd) | 12.52(1.85) | 12.67(1.77) | 0.310 | 1.04 | (0.97-1.12) |
| Ethnicity (n, %) | 0.627 | ||||
| Non-African-American | 27.03(20) | 72.97(54) | REF | REF | |
| African-American | 32.18(224) | 67.82(472) | 0.65 | (0.30-2.74) | |
| Annual income (n, %) | 0.854 | ||||
| $0-$10,000 | 31.30(159) | 68.70(349) | REF | REF | |
| $11,000-$20,000 | 31.22(64) | 68.78(141) | 0.95 | (0.71-1.27) | |
| $21,000-$30,000 | 36.11(13) | 63.89(23) | 0.76 | (0.42-1.40) | |
| Over $30,000 | 38.10(8) | 61.90(13) | 0.60 | (0.34-1.62) | |
| Health and adherence-related | |||||
| characteristics | |||||
| Side effect (mean, sd) | 7.13(5.87) | 5.76(5.54) | 0.001 | 0.97** | (0.95-0.99) |
| CD4 cell count | 0.681 | ||||
| ≤200 | 33.06(40) | 66.94(81) | REF | REF | |
| >200 | 31.16(191) | 68.84(422) | 1.05 | (0.97-1.13) | |
| Viral load (logmean, sd) | 4.80(2.15) | 4.45(1.87) | 0.025 | 0.91** | (0.85-0.97) |
| Heavy drinker (n, %) | 0.001 | ||||
| No | 28.96(181) | 71.04(444) | REF | REF | |
| Yes | 42.96(61) | 57.04(81) | 0.56*** | (0.41-0.76) | |
| Adherence self-efficacy | 7.41(1.98) | 7.91(1.94) | <0.001 | 1.11*** | (1.04-1.19) |
| Depression (n, %) | 0.001 | ||||
| None | 26.07(79) | 73.93(224) | REF | REF | |
| Mild/moderate | 28.65(53) | 71.35(132) | 0.82 | (0.58-1.16) | |
| Major | 39.72(112) | 60.28(170) | 0.59** | (0.44-0.80) | |
*p<0.05,
p<0.01,
p<0.001.
Multivariate Modeling of Food Insecurity, Drug use, and Optimal Adherence
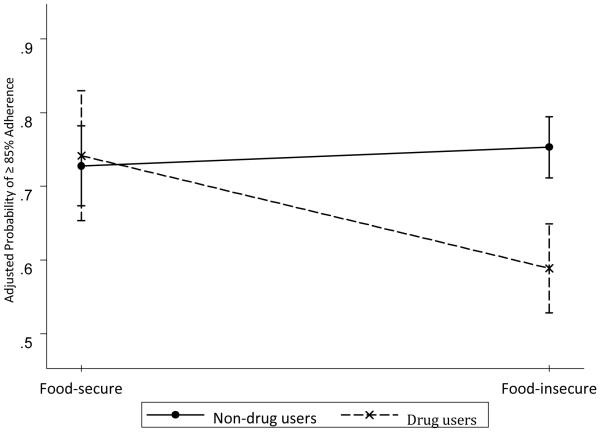
Results of multivariate analyses are presented in Table 4. Food insecurity and drug use were both associated with lower odds of optimal adherence in Model 1(AOR: 0.68, 95%CI: 0.51-0.89 for food insecurity, AOR: 0.57, 95%CI: 0.43-0.74 for drug use). The inclusion of social demographic characteristics in Model 2 did not affect the magnitude and statistical significance of the two associations. Controlling for health characteristics and adherence-related factors in Model 3 diminished the effect of food insecurity on adherence to be non-significant, but the association between drug use and adherence still remained (AOR: 0.61, 95%CI: 0.46-0.81). We also observed a significant moderating effect of drug use on the relationship between food insecurity and treatment adherence (see Figure 1). As reflected in Model 4, food insecurity was not associated with adherence for non-drug users, but among people who were currently using drugs, food insecurity was associated with a 50% drop in the odds of optimal adherence (AOR: 0.50, 95%CI: 0.29-0.87). In addition to food insecurity and drug use, factors also associated with suboptimal adherence were: age, ethnicity, number of HIV medications, and heavy drinking. Each year in age was associated with a 2% increase in the odds of optimal adherence (AOR: 1.02, 95%CI: 1.00-1.04); compared to non-African-American, African-American participants were half as likely to achieve optimal adherence (AOR: 0.53, 95%CI: 0.30-0.93); and heavy drinkers were 32% less likely to achieve optimal adherence as non- or light drinkers (AOR: 0.68, 95%CI: 0.49-0.95). These associations were stable across models 3 and model 4.
Table 4.
Multivariate analysis of optimal adherence using random-effects models with robust variance estimator
| Model 1 | Model 2 | Model 3 | Model 4 | |||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| Optimal adherence | Optimal adherence | Optimal adherence | Optimal adherence | |||||
|
| ||||||||
| Variable name | AOR1 | 95%CI | AOR1 | 95%CI | AOR1 | 95%CI | AOR1 | 95%CI |
| Food and drug | ||||||||
| Food insecurity | 0.68** | (0.51-0.89) | 0.73* | (0.55-0.96) | 0.92 | (0.67-1.26) | 1.20 | (0.83-1.74) |
| Drug use | 0.57*** | (0.43-0.74) | 0.57*** | (0.44-0.75) | 0.61** | (0.46-0.81) | 1.12 | (0.65-1.92) |
| Food insecurity × drug use | -- | -- | -- | -- | -- | -- | 0.42** | (0.22-0.79) |
| Social demographic characteristics | ||||||||
| Age | -- | -- | 1.02** | (1.01-1.04) | 1.02* | (1.00-1.04) | 1.02* | (1.00-1.04) |
| Ethnicity | (0.37-1.04) | (0.30-0.94) | (0.30-0.93) | |||||
| (African-American) | 0.63Δ | 0.53* | 0.53* | |||||
| Health and adherence-related | ||||||||
| characteristics | ||||||||
| Side effect | -- | -- | -- | -- | 1.00 | (0.97-1.02) | 0.99 | (0.97-1.02) |
| CD4 cell count >200 | -- | -- | -- | -- | 1.01 | (0.69-1.47) | 1.02 | (0.70-1.49) |
| Log viral load | -- | -- | -- | -- | 0.96 | (0.89-1.03) | 0.96 | (0.90-1.03) |
| Heavy drinker | -- | -- | -- | -- | 0.67* | (0.48-0.93) | 0.68* | (0.49-0.95) |
| Adherence self-efficacy | 1.06 | (0.98-1.14) | 1.05 | (0.97-1.13) | ||||
| Depression | -- | -- | -- | -- | ||||
| No depression | -- | -- | -- | -- | REF | REF | REF | REF |
| Mild/moderate | -- | -- | -- | -- | 0.96 | (0.66-1.40) | 0.97 | (0.67-1.42) |
| Major | -- | -- | -- | -- | 0.83 | (0.57-1.18) | 0.85 | (0.59-1.23) |
| Visit | 0.93 | (0.78-1.11) | 0.93 | (0.78-1.11) | 0.95 | (0.79-1.15) | 0.95 | (0.79-1.15) |
p<0.1,
p<0.05,
p<0.01,
p<0.001;
Adjusted odds ratio.
Figure 1.
Food insecurity–drug use interaction on probability of optimal adherence (with 95% CI), adjusting for all covariates.
DISCUSSION
This study represents one of the first efforts to explore the interaction between food insecurity and drug use in relation to ART adherence. Findings from the current study demonstrated a synergism between food insecurity and drug use that may impede adherence among PLWH. Both food insecurity and drug use were prevalent within the sample, but it is noticeable that the prevalence of food insecurity is exceptionally high given that the study population is from a resource rich country. The proportion of people who were food insecure nearly doubled that of drug use. Food insecurity and drug use overlapped among a quarter of the participants, who were much less likely to achieve optimal adherence as compared to people with only one or none of the adherence risk factors.
Younger age was associated with poor ART adherence in the current study. This finding was consistent with those from other studies. Being younger has been found to be associated with lower compliance to HIV treatment among HIV/AIDS outpatients in French and among HIV seropositive injection drug users in Canada (Peretti-Watel et al., 2006; Shannon et al., 2011). Also age as a reflection of longevity may be positively associated with adherence because PLWH who were more adherent were more likely to live longer. Some researchers suggest that younger PLWH were less adherent because they perceived low treatment utility (Barclay et al., 2007), or they could not afford their medical visits and medication copayments (Hadland et al., 2012). We therefore encourage future studies to further explore these possibilities.
The interaction between substance use and food insecurity found in the current study may imply that the association between food insecurity and adherence is not a simple and isolated relationship, and rather it needs to be understood in the context of potential moderators. In fact, a close examination of previous studies suggests a pattern of food insecurity as being a barrier among PLWH with certain characteristics. A cross-sectional study from France, for example, reported that food insecurity was associated with non-adherence among heterosexual men but not women (Peretti-Watel et al., 2006). A prospective study from the US documented an adverse effect of food insecurity on adherence among people who live outside the city but not inside (Kalichman et al., 2011). Similarly, the current study showed that food insecurity predicted suboptimal adherence among drug users but not non-drug users. These findings suggest that the disruptive effect of food insecurity on adherence is likely to be intensified with the presence of another intersecting factor. Studies are needed to identify the interplay among factors that may lower ART adherence synergistically in combination with food insecurity.
Our finding that food insecurity was particularly detrimental to ART adherence among individuals using illicit drugs suggests a mutual enhancement between food insecurity and substance use. This finding coincides with the concern of an intertwining relationship between food insecurity and illicit drug use in the HIV epidemic. Researchers have proposed several mechanisms that may underlie the mutually enhancing relationship between food insecurity and drug use. Drug addiction for example may alter dietary consumption patterns and lead to fewer meals (Himmelgreen et al., 1998) and significantly less energy consumption (Campa et al., 2005). Apart from being calorically insufficient, diets of illicit drug users also tend to be poor in quality (Campa et al., 2005), and many of the drug users actually rely on food distribution services for subsistence (Romero-Daza N., Himmelgreen D.A., Pérez-Escamilla R., Segura-Millán S., & M., 1999). These situations are further aggravated by an increasingly chaotic lifestyle among drug users (Campa et al., 2005; Weiser, Bangsberg, et al., 2009). Additionally, we also speculate that the synergistic effect between food insecurity and drug use may be due to their competitive relationship over resources. Drug addiction creates a basic physiological need, in parallel to hunger and the need for food. Resolving these two physiologic needs with limited resources will be more taxing than satisfying either of the two needs alone, especially for people struggling with HIV infection. Therefore a combination of the two factors may pose greater threat for PLWH regarding their medication adherence. This potential mechanism is in need of future research as it indicates avenues for simultaneous interventions to address food insecurity and drug use.
The findings from the current study should be interpreted in light of the following limitations. Except for ART adherence, viral load, and CD4 cell count, all other measures were collected through self-report and may be subject to social desirability and recall bias. Of particular importance is the use of self-report for assessing illegal drug use. Thus, the rates of substance use, where were high in this sample, may be suppressed and should be considered a lower-bound estimate. In addition, our study is based on a convenience sample of PLWH in one southern US city and caution is warranted before generalizing the findings from this study to other PLWH. Additionally, food insecurity and drug use were only measured at baseline, we were unable to assess the effect of changes in the status of food sufficiency or drug use on ART adherence. We also do not know the nutritional quality of participants’ food or the accurate frequency and dosing of drug use. With these limitations in mind, the current research provides implications for understanding the interrelationship between food insecurity and drug use from the perspective of HIV treatment management.
The value of HIV treatment adherence lies not only in the restoration and maintenance of health among PLWH, but also in the reduction of HIV transmission. The criticality of treatment adherence has posed an urgency to identify modifiable factors associated with ART non-adherence. Food insecurity and illicit drug use are both associated with ART non-adherence. Yet the negative impact of both factors on ART adherence may be further amplified by their co-occurrence. Multiple adverse conditions may therefore pose significant threats to improving HIV treatment engagement, adherence, and prevention. Interventions should be the focus of efforts to improve ART adherence and HIV-related health outcomes. Of particularly urgency are interventions that address co-occurring conditions of poverty as these approaches will offer considerable opportunities to improve ART adherence. Food insecurity interventions such as free food assistance and micronutrient supplementations may be viewed as gateway to adherence interventions, especially among HIV infected drug users. Adherence intervention may seek collaboration with food distribution programs to provide food and nutrition support to food insecure PLWH, along with its effort to alleviate the negative impact of drug use on HIV medication adherence. Establishing food security and reducing drug use simultaneously should be expected to resolve the synergistic effects of multiple impediments and improve mediation adherence. Coordination between multiple social programs to address co-occurring issues among PLWH may help to generate a stronger overall effect on improving HIV medication adherence and treatment outcomes.
Acknowledgments
*Funding: This project was supported by National Institute of Drug Abuse Grant R01-DA017399.
Reference
- Alcabes P, Schoenbaum EE, Klein RS. Correlates of the rate of decline of CD4+ lymphocytes among injection drug users infected with the human immunodeficiency virus. American Journal of Epidemiology. 1993;137:989–1000. doi: 10.1093/oxfordjournals.aje.a116771. [DOI] [PubMed] [Google Scholar]
- Anema A, Chan K, Chen Y, Weiser S, Montaner JS, Hogg RS. Relationship between food insecurity and mortality among HIV-positive injection drug users receiving antiretroviral therapy in British Columbia, Canada. Plos One. 2013;8:e61277. doi: 10.1371/journal.pone.0061277. doi: 10.1371/journal.pone.0061277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anema A, Vogenthaler N, Frongillo EA, Kadiyala S, Weiser SD. Food insecurity and HIV/AIDS: current knowledge, gaps, and research priorities. Current HIV/AIDS Reports. 2009;6:224–231. doi: 10.1007/s11904-009-0030-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anema A, Wood E, Weiser SD, Qi J, Montaner JS, Kerr T. Hunger and associated harms among injection drug users in an urban Canadian setting. Substance Abuse Treatment, Prevention, and Policy. 2010;5:20. doi: 10.1186/1747-597X-5-20. doi: 10.1186/1747-597X-5-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antoniou T, Tseng AL. Interactions between recreational drugs and antiretroviral agents. Annals of Pharmacotherapy. 2002;36:1598–1613. doi: 10.1345/aph.1A447. [DOI] [PubMed] [Google Scholar]
- Au JT, Kayitenkore K, Shutes E, Karita E, Peters PJ, Tichacek A, Allen SA. Access to adequate nutrition is a major potential obstacle to antiretroviral adherence among HIV-infected individuals in Rwanda. AIDS. 2006;20:2116–2118. doi: 10.1097/01.aids.0000247580.16073.1b. doi: 10.1097/01.aids.0000247580.16073.1b. [DOI] [PubMed] [Google Scholar]
- Bangsberg DR, Kroetz DL, Deeks SG. Adherence-resistance relationships to combination HIV antiretroviral therapy. Current HIV/AIDS Reports. 2007;4:65–72. doi: 10.1007/s11904-007-0010-0. [DOI] [PubMed] [Google Scholar]
- Barclay TR, Hinkin CH, Castellon SA, Mason KI, Reinhard MJ, Marion SD, Durvasula RS. Age-associated predictors of medication adherence in HIV-positive adults: health beliefs, self-efficacy, and neurocognitive status. Health Psychology. 2007;2:40–49. doi: 10.1037/0278-6133.26.1.40. doi: 10.1037/0278-6133.26.1.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartlett JA. Addressing the challenges of adherence. Journal of Acquired Immune Deficiency Syndromes. 2002;29(Suppl 1):S2–10. doi: 10.1097/00126334-200202011-00002. [DOI] [PubMed] [Google Scholar]
- Campa A, Yang Z, Lai S, Xue L, Phillips JC, Sales S, Baum MK. HIV-related wasting in HIV-infected drug users in the era of highly active antiretroviral therapy. Clinical Infectious Diseases. 2005;41:1179–1185. doi: 10.1086/444499. doi: 10.1086/444499. [DOI] [PubMed] [Google Scholar]
- Carrieri MP, Villes V, et al. Self-reported side-effects of anti-retroviral treatment among IDUs: a 7-year longitudinal study (APROCO-COPILOTE COHORT ANRS CO-8) International Journal of Drug Policy. 2007;18:288–295. doi: 10.1016/j.drugpo.2007.01.014. [DOI] [PubMed] [Google Scholar]
- Coates J, Swindale A, Bilinsky P. Household Food Insecurity Access Scale (HFIAS) for Measurement of Food Access: Indicator Guide. 2007 Retrieved June, 1, 2014. [Google Scholar]
- Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, Team HS. Prevention of HIV-1 infection with early antiretroviral therapy. The New England Journal of Medicine. 2011;365:493–505. doi: 10.1056/NEJMoa1105243. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ensoli F, Sirianni MC. HIV/HCV co-infection: clinical and therapeutic challenges. AIDS. 2002;16:1419–1420. doi: 10.1097/00002030-200207050-00014. [DOI] [PubMed] [Google Scholar]
- Hadland SE, Milloy MJ, Kerr T, Zhang R, Guillemi S, Hogg RS, Wood E. Young age predicts poor antiretroviral adherence and viral load suppression among injection drug users. AIDS Patient Care STDS. 2012;26:274–280. doi: 10.1089/apc.2011.0196. doi: 10.1089/apc.2011.0196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendricks K, Gorbach S. Nutrition issues in chronic drug users living with HIV infection. Addiction Science & Clinical Practice. 2009;5:16–23. doi: 10.1151/ascp095116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Himmelgreen DA, Perez-Escamilla R, Segura-Millan S, Romero-Daza N, Tanasescu M, Singer M. A comparison of the nutritional status and food security of drug-using and non-drug-using Hispanic women in Hartford, Connecticut. American Journal of Physical Anthropology. 1998;107:351–361. doi: 10.1002/(SICI)1096-8644(199811)107:3<351::AID-AJPA10>3.0.CO;2-7. doi: 10.1002/(SICI)1096-8644(199811)107:3<351::AID-AJPA10>3.0.CO;2-7. [DOI] [PubMed] [Google Scholar]
- Hinkin CH, Barclay TR, Castellon SA, Levine AJ, Durvasula RS, Marion SD, Longshore D. Drug use and medication adherence among HIV-1 infected individuals. AIDS Behavior. 2007;11:185–194. doi: 10.1007/s10461-006-9152-0. doi: 10.1007/s10461-006-9152-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Amaral CM, Cherry C, Flanagan J, Pope H, Eaton L, Schinazi RF. Monitoring medication adherence by unannounced pill counts conducted by telephone: reliability and criterion-related validity. HIV Clinical Trials. 2008;9:298–308. doi: 10.1310/hct0905-298. doi: 10.1310/hct0905-298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Pellowski J, Kalichman MO, Cherry C, Detorio M, Caliendo AM, Schinazi RF. Food insufficiency and medication adherence among people living with HIV/AIDS in urban and peri-urban settings. Prevention Science. 2011;12:324–332. doi: 10.1007/s11121-011-0222-9. doi: 10.1007/s11121-011-0222-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leaver CA, Bargh G, Dunn JR, Hwang SW. The effects of housing status on health-related outcomes in people living with HIV: a systematic review of the literature. AIDS Behavior. 2007;11(6 Suppl):85–100. doi: 10.1007/s10461-007-9246-3. doi: 10.1007/s10461-007-9246-3. [DOI] [PubMed] [Google Scholar]
- Maisto SA, Conigliaro J, McNeil M, Kraemer K, Kelley ME. An empirical investigation of the factor structure of the AUDIT. Psychological Assessment. 2000;12:346–353. doi: 10.1037//1040-3590.12.3.346. [DOI] [PubMed] [Google Scholar]
- Miller CL, Bangsberg DR, Tuller DM, Senkungu J, Kawuma A, Frongillo EA, Weiser SD. Food insecurity and sexual risk in an HIV endemic community in Uganda. AIDS Behavior. 2011;15:1512–1519. doi: 10.1007/s10461-010-9693-0. doi: 10.1007/s10461-010-9693-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musumari PM, Wouters E, Kayembe PK, Kiumbu Nzita M, Mbikayi SM, Suguimoto SP, Kihara M. Food insecurity is associated with increased risk of non-adherence to antiretroviral therapy among HIV-infected adults in the Democratic Republic of Congo: a cross-sectional study. PLoS One. 2014;9:e85327. doi: 10.1371/journal.pone.0085327. doi: 10.1371/journal.pone.0085327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Normen L, Chan K, Braitstein P, Anema A, Bondy G, Montaner JS, Hogg RS. Food insecurity and hunger are prevalent among HIV-positive individuals in British Columbia, Canada. Journal of Nutrition. 2005;135:820–825. doi: 10.1093/jn/135.4.820. [DOI] [PubMed] [Google Scholar]
- Pan W. Akaike's information criterion in generalized estimating equations. Biometrics. 2001;57:120–125. doi: 10.1111/j.0006-341x.2001.00120.x. [DOI] [PubMed] [Google Scholar]
- Peretti-Watel P, Spire B, Schiltz MA, Bouhnik AD, Heard I, Lert F, Group V. Vulnerability, unsafe sex and non-adherence to HAART: evidence from a large sample of French HIV/AIDS outpatients. Social Science & Medicine. 2006;62:2420–2433. doi: 10.1016/j.socscimed.2005.10.020. doi: 10.1016/j.socscimed.2005.10.020. [DOI] [PubMed] [Google Scholar]
- Piot P, Greener R, Russell S. Squaring the circle: AIDS, poverty, and human development. PLoS Med. 2007;4:1571–1575. doi: 10.1371/journal.pmed.0040314. doi: 10.1371/journal.pmed.0040314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Romero-Daza N, Himmelgreen DA, Pérez-Escamilla R, Segura-Millán S, M. S. Food habits of drug-using Puerto Rican women in inner-city Hartford. Medical Anthropology: Cross-Cultural Studies in Health and Illness. 1999;18:281–298. [Google Scholar]
- Rose AM, Sinka K, Watson JM, Mortimer JY, Charlett A. An estimate of the contribution of HIV infection to the recent rise in tuberculosis in England and Wales. Thorax. 2002;57:442–445. doi: 10.1136/thorax.57.5.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sethi AK, Celentano DD, Gange SJ, Moore RD, Gallant JE. Association between adherence to antiretroviral therapy and human immunodeficiency virus drug resistance. Clinical Infectious Diseases. 2003;37:1112–1118. doi: 10.1086/378301. doi: 10.1086/378301. [DOI] [PubMed] [Google Scholar]
- Shannon K, Kerr T, Milloy MJ, Anema A, Zhang R, Montaner JS, Wood E. Severe food insecurity is associated with elevated unprotected sex among HIV-seropositive injection drug users independent of HAART use. AIDS. 2011;25:2037–2042. doi: 10.1097/QAD.0b013e32834b35c9. doi: 10.1097/QAD.0b013e32834b35c9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer M, Clair S. Syndemics and public health: reconceptualizing disease in bio-social context. Medical Anthropology Quarterly. 2003;17:423–441. doi: 10.1525/maq.2003.17.4.423. [DOI] [PubMed] [Google Scholar]
- StataCorp . Stata Statistical Software: Release 12. StataCorp LP; College Station,TX: 2011. [Google Scholar]
- Strike C, Rudzinski K, Patterson J, Millson M. Frequent food insecurity among injection drug users: correlates and concerns. BMC Public Health. 2012;12:1058. doi: 10.1186/1471-2458-12-1058. doi: 10.1186/1471-2458-12-1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- USDA . Food Insecurity and Hunger in the United States: An Assessment of the Measure. National Academies Press; 2006. [Google Scholar]
- Weiser SD, Bangsberg DR, Kegeles S, Ragland K, Kushel MB, Frongillo EA. Food insecurity among homeless and marginally housed individuals living with HIV/AIDS in San Francisco. AIDS Behavior. 2009;13:841–848. doi: 10.1007/s10461-009-9597-z. doi: 10.1007/s10461-009-9597-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiser SD, Fernandes KA, Brandson EK, Lima VD, Anema A, Bangsberg DR, Hogg RS. The association between food insecurity and mortality among HIV-infected individuals on HAART. Journal of Acquired Immune Deficiency Syndromes. 2009;52:342–349. doi: 10.1097/QAI.0b013e3181b627c2. doi: 10.1097/QAI.0b013e3181b627c2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiser SD, Frongillo EA, Ragland K, Hogg RS, Riley ED, Bangsberg DR. Food insecurity is associated with incomplete HIV RNA suppression among homeless and marginally housed HIV-infected individuals in San Francisco. Journal of General Internal Medicine. 2009;24:14–20. doi: 10.1007/s11606-008-0824-5. doi: 10.1007/s11606-008-0824-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiser SD, Young SL, Cohen CR, Kushel MB, Tsai AC, Tien PC, Bangsberg DR. Conceptual framework for understanding the bidirectional links between food insecurity and HIV/AIDS. The American Journal of Clinical Nutrition. 2011;94:1729S–1739S. doi: 10.3945/ajcn.111.012070. doi: 10.3945/ajcn.111.012070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood E, Hogg RS, Yip B, Moore D, Harrigan PR, Montaner JS. Impact of baseline viral load and adherence on survival of HIV-infected adults with baseline CD4 cell counts > or = 200 cells/microl. AIDS. 2006;20:1117–1123. doi: 10.1097/01.aids.0000226951.49353.ed. doi: 10.1097/01.aids.0000226951.49353.ed. [DOI] [PubMed] [Google Scholar]