INTRODUCTION
Nearly 27 million adult Americans have osteoarthritis (OA) (Lawrence et al., 2008), which involves the degeneration of the joint components and surfaces, and is frequently associated with pain, inflammation, and decreased range of motion in the joint. Adult onset rheumatoid arthritis (RA) is a systemic inflammatory autoimmune disease affecting joints that often causes stiffness, swelling, pain, and loss of joint function. Arthritis pain is associated with psychological and psychosocial distress (Benka et al., 2012; Nicassio et al., 2011; Somers et al., 2009) which may result in depression and fatigue from a lack of control over daily living (Simpson et al., 2005). Additionally, anxiety and depression can exacerbate the experience and perception of pain (Smith & Zautra, 2008).
Self-management programs targeting pain and pain-related distress generally apply principles of Cognitive Behavioral Therapy (CBT), which focuses on changing thoughts and behaviors, or self-efficacy. Self-efficacy, derived from Social Cognitive Theory (SCT; Bandura 1977, 1997) is a prominent theoretical model in the arthritis literature and has been proposed as an organizing concept for self-management in other chronic diseases (Marks et al., 2005). Improving self-efficacy, which involves developing task-specific knowledge and skills, as well as confidence in one’s ability to accomplish the task in a specific environment (Marks, 2001), has been a focus for change in studies of arthritis pain. Self-efficacy beliefs, learned through personal experience, are specific for each self-management behavior (e.g., exercising, relaxation, positive self-statements, avoidance of catastrophizing; Jensen et al., 2003).
There is evidence that participation in self management programs is beneficial; for example, studies of in person CBT pain management programs show positive effects on pain, catastrophizing, coping, disability and patient functioning (Burns, Kubilus, Bruehl, Harden, & Lofland, 2003; Molton et al., 2007; Smeets et al., 2006; Williams et al., 2012). Self-management programs for arthritis and chronic disease that have been conducted face-to-face have shown the following outcomes in randomized controlled trials (RCTs): increased pain self-efficacy, decreased depression, anxiety, and/or pain (see metaanalysis by Dixon et al., 2007) and increased health behaviors (Lorig et al., 2001). Online self-management programs have the potential to overcome some of the limitations of face-to-face self-management programs such as inaccessibility, lack of trained personnel and a group-format delivery (Bodenheimer et al., 2002; Newman et al., 2004). Additionally, the Internet is increasingly accessible and is used often for obtaining health information (Fox, 2007). A Cochrane Collaboration review of computer-delivered interventions for people with a wide variety of chronic diseases found improvements in knowledge, perceived social support, health behaviors, and clinical outcomes (Murray et al., 2005).
There are few empirically-based arthritis-specific online sites focused on arthritis self-management. In randomized controlled trials (RCTs) of adults, Lorig et al. (2008) found improvement in health distress, activity limitation, global health, and self-efficacy. A pilot RCT of an internet-based self management program for adolescents with arthritis found that participants in the experimental condition reported lower pain intensity at post treatment follow up compared to participants in the attention control condition (Stinson et al., 2010).
painACTION is an online self-management program that seeks to assist adults who have various types of chronic pain, including back pain, cancer pain, neuropathic pain, migraine pain, and arthritis pain by increasing coping, self-management, and communication skills using the principles of CBT and based on SCT (Bandura 1977, 1997). Each module of the program includes content specific to that type of pain plus shared tools (e.g., a pain tracker) that has undergone independent efficacy testing: back pain (Chiauzzi et al., 2010), migraine pain (Bromberg et al., 2011), and neuropathic pain (DasMahapatra et al., 2013). These RCTs have found that use of painACTION is associated with: (a) decreased negative symptoms associated with chronic pain, e.g., stress, anxiety, depression, and pain levels, and (b) increased positive affect, coping skills, and self-efficacy among patients who are self-managing pain.
Prior to developing the arthritis module for painACTION, we conducted a qualitative assessment of the needs of 32 people with arthritis and 12 practitioners to learn what was important to include in an online self-management program (Trudeau et al., 2010). Concept Mapping of qualitative data revealed that the information about self management and chronic pain in the literature and in the other modules on painACTION was desired by this audience. When development of the arthritis module was complete, we conducted a randomized controlled trial to test the efficacy of this program for people with arthritis pain. It was hypothesized that participants randomized to the painACTION intervention would report: increased positive cognitions (i.e., pain self-efficacy and pain awareness), reduced negative cognitions (i.e., pain catastrophizing); increased frequency of self-management behaviors (i.e., exercise, cognitive symptom management, communication with physicians); and reduced pain and improved functioning compared to those in a wait-list control condition.
In addition to testing the primary hypotheses, several secondary analyses were conducted. Secondary outcomes pertaining to affect, coping skills, well-being, and global impression of change were explored. As recommended by Turner et al., (2007), we conducted exploratory analyses of potential moderators to see if this intervention was particularly helpful to patients with certain demographic or patient characteristics because they may experience pain and pain management differently. For example, research has indicated that fatigue had a greater impact on pain in patients with RA and fibromyalgia syndrome compared to patients with OA (Zautra et al., 2007). We also looked at level of user engagement because, in the painACTION study with adults with migraine headaches (Bromberg et al., 2011), the high-dose group reported significantly increased self efficacy at post-intervention compared to the low-dose group.
MATERIALS & METHODS
The study protocol and all recruitment materials were reviewed and approved on August 26, 2011 by an independent institutional review board (New England Institutional Review Board, Newton, MA). Participant recruitment began on September 8, 2011, and the collection of follow-up data ended on November 11, 2012. [ClinicalTrials.gov Identifier: NCT01463189]
Participants
Participants were recruited through IRB-approved recruitment flyers distributed to doctors’ offices, senior citizen service organizations, and events conducted by the Arthritis Foundation – Massachusetts Chapter. An electronic version of the IRB-approved flyer was also disseminated on the Internet through a variety of methods: (1) email announcements and web postings through the American Chronic Pain Association and the Alliance of State Pain Initiatives to their respective membership (ASPI); (2) advertising targeted to search terms using Google Adwords; (3) listing the study with ClinicalTrials.gov; (4) message boards such as Facebook and Craig’s List; and (5) distribution of study information to health professionals involved in pain management who are registered at PainEDU (an educational website for health care professionals site run by Inflexxion) through the newsletter.
Inclusion criteria for study participants were as follows: (1) at least 18 years of age; (2) able to read and speak English; (3) able to provide informed consent; (4) reliable Internet and email access; (5) a self-reported doctor diagnosis of arthritis such as osteoarthritis (OA), rheumatoid arthritis (RA), ankylosing spondylitis (AS), or other arthritic conditions (e.g., psoriatic arthritis); and (6) pain intensity or impaired functioning of 4 or higher on the 0 to 10 Numeric Rating Scale (McCaffery & Beebe, 1993), because a score of 4 or higher generally is associated with moderate or high level of pain. Exclusion criteria were: (1) participation in another Inflexxion pain management study; (2) participation in an online research study related to arthritis in the past year; (3) currently in pain from a recent injury; and (4) hospitalization for reasons related to mental health in the past year.
Data were collected via the online data collection software Vovici 6 Enterprise Edition (Vovici Corporation, 2012) and stored in a secure database. Participants completed the online assessments at a location of their convenience; they were encouraged to help protect their confidentiality by completing the online questionnaire on their own personal computer and in a private place. They were compensated a total of $250 for completing all assessments.
Procedures
The study is a parallel group design with two conditions. Participants who met the eligibility criteria, completed the online consent form, and were reached for the enrollment confirmation call were randomized to either the experimental condition (eight site visits over four weeks, plus one visit per month for five months) or the wait-list control condition. We used stratified block randomization (Kernan et al., 1999) to decrease the likelihood of imbalance between conditions. The randomization factors were: (1) gender and (2) type of arthritis. A random sequence was computer-generated for 2 (male, female) × 2 (OA only, RA and/or other) = 4 strata with block size of 4 and equal allocation to each of the two conditions. The random allocation sequence was generated by the study data manager; the research coordinator (RW) enrolled and assigned participants to conditions. There was no blinding after assignment to condition because all measures are self-report.
Experimental condition. Participants in this condition were given access to painACTION.com, a web-based patient education intervention whose development was guided by principles of CBT. All content in painACTION.com is expert-reviewed and approved. Content delivery is multi-faceted. Major areas of content matter are: informational articles designed to enhance both knowledge and patient-provider communication; self-check assessments that give chronic pain patients the ability to help determine confidence and awareness about self-efficacy; lessons that deal with specific issues that face chronic pain patients and how to better navigate those hurdles; personal stories that allow for sharing of thoughts, feelings, and anecdotal solutions from other patients suffering with similar conditions; and, tools that can help provide chronic pain patients with skill sets to help navigate their chronic pain experiences and interactions with healthcare providers.
Participants in the experimental condition were provided with a username and password to access the painACTION site, and asked to complete a minimum of two 20-minute sessions on the site per week for four weeks (eight sessions in total), plus a minimum of five 20-minute follow-up sessions (one per month for 5 months). Specific tasks per session were recommended based on the hypothesized outcomes. For example, content intended to increase positive cognitions (e.g., pain self-efficacy) included “Arthritis-friendly tips and tools for easier living” and “Setting goals to improve your quality of life.” Articles selected to help reduce negative cognitions (e.g., pain catastrophizing) included “When your brain helps the pain: Cognitive therapy in action” and “What’s the worst that could happen?” Tools recommended to increase frequency of self-management behaviors included “Fun ways to be physically active when you have arthritis,” “Chair yoga,” and “Patient-doctor talk.” Please go to www.painaction.com to see these examples.
Each participant logged in with a personal identification code; therefore it was possible to track each user’s session dates and session times (minutes spent) on the website through usage information on the server. Participant site usage was closely monitored by the research coordinator (RW), and weekly reminders were sent to participants to complete the required sessions. Participants who missed sessions or spent insufficient time were sent email reminders. Phone calls were made to participants who were not using the site to ascertain if inactivity was due to technical problems accessing the site versus lack of interest or engagement.
Control condition. Participants in the control condition were assigned to a waiting list and provided access to the intervention after they completed the final study assessments.
Via informed consent, participants in both conditions were encouraged to continue whatever medical treatment they have been receiving as this study was not a replacement treatment. In addition, they were welcome to seek additional medical treatment during the study.
Measures
Demographic Questionnaire. Participants were asked to indicate their age, gender, race, ethnicity, marital status, level of education, current employment status, and annual household income. This information was gathered at baseline and was used to describe the study participants, as well as to explore potential covariates in outcome analyses.
Primary outcomes
Cognitions
The Arthritis Self-efficacy Scale (Lorig et al., 1989) is an 8-item questionnaire that assesses a patient’s level of confidence to manage arthritis pain. This scale is rated on a 1 to 10 scale ranging from 1 = very uncertain to 10 = very certain. This questionnaire has demonstrated internal reliability with the alpha coefficient of .92.
The Pain Catastrophizing Scale (PCS) (Sullivan et al., 1995) is an empirically validated (D’Eon et al., 2004; Osman et al., 2000) 13-item scale that measures three elements of catastrophizing (i.e., rumination, magnification, and helplessness) and provides a catastrophizing total score. Items are rated from 0 to 4 (0 = not at all, 4 = all the time).
The Pain Awareness Questionnaire (Berman et al., 2009) is a 7-item questionnaire that assesses a patient’s awareness of their current pain. It is on a 0 to 4 scale: 0 = not sure to 4 = most of the time. The internal consistency was between .68 for baseline, .58 for follow up, and .81 for data combined from both time points.
Self-Management Behaviors
Exercise Behaviors (Lorig et al., 1996) is a 6-item questionnaire assessing the total time a patient had participated in various forms of exercise. This scale is rated on a 0 to 4 scale: 0 = none to 4 = more than 3 hours per week. It has demonstrated test retest reliability in two domains: strengthening (Cronbach’s α = 0.56) and aerobic exercise (Cronbach’s α = 0.72).
Cognitive Symptom Management (Lorig et al., 1996) is a 6-item questionnaire assessing a patient’s ability to manage their symptoms. This scale is rated on a 0 to 5 scale: 0 = never to 5 = always. The questionnaire has demonstrated test-retest reliability with an alpha coefficient of .83 and internal consistency reliability with an alpha coefficient of .75.
Communication with Physicians (Lorig et al., 1996) is a 3-item scale assessing a patient’s communication with their physicians. This scale is rated on a 0 to 5 scale: 0 = never to 5 = always. The questionnaire has demonstrated test retest reliability with an alpha coefficient of .89 and internal consistency with an alpha coefficient of .73.
Pain
Brief Pain Inventory – Short Form (BPI-SF) (Cleeland & Ryan, 1994) uses a 0 to 10 numeric rating scale to obtain information on the intensity of pain, the degree to which pain interferes with function, pain relief, pain quality, and the patient’s perception of the cause of pain. It has two subscales: 1) The Pain Severity Score has four items (worst, least, average and current pain) that measure the average level of pain intensity for the patient. 2) The Pain Interference Score has seven items that measure how much pain interferes with daily life, such as general activities, mood, walking, work, relationships, sleep and enjoyment of life. The BPI’s reliability and validity were originally established with samples of cancer pain patients, but have now been founds for chronic non-cancer pain, including arthritis (Keller et al., 2004; Mendoza et al., 2006).
Secondary outcomes
The Depression Anxiety Stress Scales (DASS-21, (Lovibond & Lovibond, 1995) is a 21-item questionnaire with three subscales: depression, anxiety, and stress. This scale has consistently good psychometric properties (Antony et al., 1998; Crawford & Henry, 2003) with various populations, including older primary care patients specifically (Gloster et al., 2008).
The Chronic Pain Coping Inventory (CPCI-42) (Romano et al., 2003) is an empirically validated, abbreviated version of the original CPCI (Jensen et al., 1995). The individual is asked to indicate the frequency of use of behavioral and cognitive coping strategies to cope with pain on 42 items including eight subscales: Guarding, Resting, Asking for Assistance, Relaxation, Task Persistence, Exercise/Stretching, Seeking Social Support, and Coping Self-Statements.
The Arthritis Impact Measurement Scale-2-SF (Guillemin et al., 1999) is a 26-item scale that measures five domains of health status (i.e., Physical, Symptom, Affect, Social Interaction, Role) on a 5-point Likert scale during the previous 4 weeks for persons with arthritis. It has been found to be reliable and valid for persons with RA (Guillemin et al., 1999; ten Klooster et al., 2008) and OA (Ren et al., 1999).
Patient Global Impression of Change Scale (Guy, 1976) is an outcome measure of the patient’s impression of improvement with treatment and consists of a single-item self-rating (7-point scale, “very much improved” to “very much worse”) of a participant’s perceived response to an intervention. Specifically, participants were asked about how much improvement they experienced with pain treatment during the study. Improvement in PGIC is related to reduced chronic pain intensity (Farrar et al., 2001).
Data for the number of minutes spent on the website and pages viewed were collected for participants in the experimental condition.
Statistical Analysis
The study design was a parallel group RCT comparing two conditions (experimental vs. control) over 4 time points (baseline, one month follow up, three month follow up, and six month follow up). We used linear mixed model (LMM) approach to test differences between conditions for each outcome. Advantages of using LMM are: (a) LMM automatically handles missing data by maximum likelihood (Allison, 2012) and (b) LMM accounts for covariance among repeated measures.
Descriptive statistics (mean, standard deviation, frequency, etc.) were computed for demographic variables for the entire study sample and stratified by conditions. Next, we tested for mean differences between conditions (experimental vs. control) over time on each outcome. Each model included the following fixed effects: (1) condition (experimental vs. control), (2) time (baseline, one month follow up, three month follow up and six month follow up), and (3) condition-BY-time interaction. The model treated time as a repeated measures variable to allow for covariation across time points. Statistical focus of these analyses was the interaction effect, condition-BY-time, as this effect tests differences between conditions over time.
Exploratory analyses were conducted to test for moderation (effect modification), i.e., we tested whether the magnitude of intervention effects were different for certain covariates, namely gender (male vs. female), age (≤50 years vs. >50 years), race (white vs. non-white), baseline pain intensity (average baseline pain ≤6 vs. >6), and Arthritis type (OA vs. RA and other).
Exploratory models were constructed by adding the putative moderator (e.g., gender) as a main effect and all possible two-way and three-way interaction terms (e.g. gender-BY-time, gender-BY-condition, gender-BY-condition-BY-time). Post-hoc analyses were conducted in the presence of a significant three-way interaction.
Finally, we performed exploratory analyses to test the effect of user engagement on outcomes. This was done by testing the condition-BY-time effect for each outcome using a new condition variable with three levels: control, low engagement, high engagement. Low engagement and high engagement levels were derived from the total number of minutes spent on painACTION website. A median split (median = 204.5 minutes) was done to categorize experimental participants into low engagement and high engagement levels because the total number of minutes on the site variable (M = 288.4, SD = 356.5, Range = 0 through 2746.5) included measurement error caused by individuals not actively closing out of a specific page.
The study was originally powered to control for Type I error with respect to the primary analyses. As recommended by Turner et al., (2007), the authors performed exploratory analyses to evaluate the possibility of moderating effects. Since the sample size necessary to adequately power these supplemental analyses was not part of the original study design, the authors performed these analyses without controlling for Type I error, as this would likely result in a concomitant inflation of Type II error. Therefore, the level of significance was set at α=.05 for each secondary analysis of the data. However, it should be noted that within each secondary analysis, post-hoc tests were adjusted for Type I error by applying a well-established simulation method, considered superior to the Bonferroni correction (Westfall, Tobias, & Wolfinger, 2011). All analyses were performed using the GLIMMIX procedure in SAS, version 9.3 (SAS Institute, 2011; Schabenberger, 2005).
RESULTS
Participant Selection
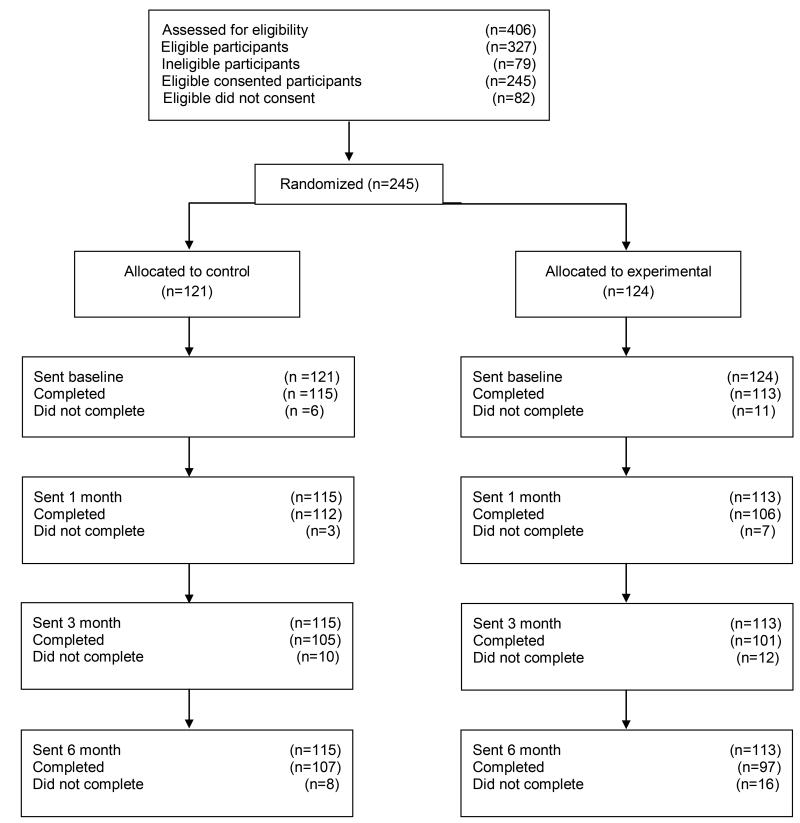
Four hundred and six (406) subjects were assessed for eligibility, of which 335 participants met the inclusion criteria. Eight subjects were registered users of the painACTION website and hence excluded from the study. Of the remaining 327 subjects, 245 consented to participate and were randomized into either the experimental or control condition. After randomization, 16 participants did not complete baseline (i.e., dropped out) and one participant was terminated from the study for attempting to enroll in the study multiple times, resulting in the final sample of 228 allocated to experiment (n=113) and control (n=115) conditions. In the experimental condition, the attrition rate at one month follow up, three month follow up and six month follow up was 6.2%, 10.6% and 14.2% respectively. Among participants assigned to the control condition, the attrition rate at one month follow up, three month follow up and six month follow up was 2.6%, 8.7% and 6.8% respectively. In accordance with the Consolidated Standards of Reporting Trials group (www.consort-statement.org), participant enrollment and follow-up through the study is documented in Figure 1. Because the study was designed with an intent-to-treat approach, the goal was to follow as many participants as possible, regardless of their completion of intervention. The majority of the participants completed all the follow up assessments (n = 195) resulting in an overall retention rate greater than 85%.
Figure 1. Consolidated Standards of Reporting Trials flow diagram.
Participant Characteristics
Baseline descriptive characteristics of the study sample are presented in Table 1. There were no differences in demographic characteristics of the participants by condition.
Table 1.
Baseline characteristics of the study participants
| Total N=228 n(%) |
Control n=115 n(%) |
Experimental n=113 n(%) |
Test Statistic† |
p‡ | |
|---|---|---|---|---|---|
| Age (years, Mean ± SD) | 49.9 ± 11.6 | 49.6 ± 10.9 | 50.3 ± 12.3 | 0.43 | 0.66 |
| Gender | |||||
| Male | 72(31.6) | 34(29.6) | 38(33.6) | 0.44 | 0.51 |
| Female | 156(68.4) | 81(70.4) | 75(66.4) | ||
| Race | |||||
| Black/AA | 17(7.5) | 7(6.1) | 10(8.9) | 4.52 | 0.34 |
| White | 199(87.3) | 100(87.0) | 99(87.6) | ||
| Native Hawaiian/Pacific Islander | 1(0.4) | 0(0.0) | 1(0.9) | ||
| Native American/Alaska Native | 2(0.9) | 2(1.7) | 0(0.0) | ||
| Other | 9(3.9) | 6(5.2) | 3(2.6) | ||
| Ethnicity | |||||
| Hispanic/Latino | 29(12.7) | 16(13.9) | 13(11.5) | 0.30 | 0.58 |
| Education | |||||
| 11th grade or less | 2(0.9) | 1(0.9) | 1(0.9) | 6.67 | 0.25 |
| High school or GED | 33(14.5) | 15(13.0) | 18(15.9) | ||
| 2 years college/AA degree/technical training |
53(23.2) | 34(29.6) | 19(16.8) | ||
| College graduate (BA or BS) | 101(44.3) | 50(43.5) | 51(45.1) | ||
| Master’s degree | 33(14.5) | 13(11.3) | 20(17.6) | ||
| Doctorate/MD/JD | 6 (2.6) | 2(1.7) | 4(3.5) | ||
| Income | |||||
| $24,999 or less | 22(9.7) | 8(7.0) | 14(12.4) | 8.0 | 0.33 |
| 25,000-49,999 | 40(17.5) | 23(20.0) | 17(15.0) | ||
| 50,000-74,999 | 38(16.7) | 25(21.7) | 13(11.5) | ||
| 75,000-99,999 | 60(26.3) | 27(23.5) | 33(29.2) | ||
| 100,000-149,999 | 36(15.8) | 17(14.8) | 19(16.8) | ||
| 150,000-199,999 | 11(4.8) | 4(3.4) | 7(6.2) | ||
| 200,000 or more | 5(2.2) | 3(2.6) | 2(1.8) | ||
| Not answered | 16(7.0) | 8(7.0) | 8(7.1) | ||
| Marital Status | |||||
| Never married | 36(15.8) | 19(16.5) | 17(15.0) | 4.4 | 0.62 |
| Married | 126(55.3) | 61(53.0) | 65(57.5) | ||
| Separated | 5(2.2) | 3(2.6) | 2(1.7) | ||
| Divorced | 40(17.5) | 19(16.5) | 21(18.6) | ||
| Widowed | 7(3.1) | 5(4.4) | 2(1.8) | ||
| Remarried | 4(1.7) | 1(0.9) | 3(2.7) | ||
| Living with partner | 10(4.4) | 7(6.1) | 3(2.7) | ||
| Employment | |||||
| Full time | 134(58.8) | 71(61.7) | 63(55.7) | 1.3 | 0.97 |
| Part time | 29(12.7) | 13(11.3) | 16(14.2) | ||
| Unemployed | 13(5.7) | 6(5.2) | 7(6.2) | ||
| Disabled | 18(7.9) | 8(7.0) | 10(8.8) | ||
| Homemaker | 9(3.9) | 4(3.5) | 5(4.4) | ||
| Retired | 18(7.9) | 9(7.8) | 9(8.0) | ||
| Student | 7(3.1) | 4(3.5) | 3(2.7) | ||
| Arthritis Type€ | 0.04 | 0.85 | |||
| Osteoarthritis only | 134 (59.0) | 68 (59.7) | 66 (58.4) | ||
| Rheumatoid Arthritis or Other | 93 (41.0) | 46 (40.3) | 47 (41.6) | ||
| Arthritic Condition | |||||
Test statistics is t-test for continuous variable age and χ2 for categorical variables, comparing control and intervention groups.
p-values pertain to tests for difference between control and intervention groups.
One subject did not specify type of arthritis
Treatment Effects
Primary Outcomes
Linear mixed models (LMM) were run to ascertain whether the participants in the experimental condition, as compared to participants in the control condition, evidenced a significantly greater mean change over time on these primary outcomes: cognitions (self-efficacy; awareness of pain; pain catastrophizing), self-management behaviors (exercise behaviors; cognitive symptom management; communication with physician) and pain (pain intensity; pain interference) (see results in Table 2).
Table 2.
Least square means and standard errors for all outcome measures
| Control | Experimental | |||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | Post | 3-month | 6-month | Baseline | Post | 3-month | 6-month | |
|
|
||||||||
| Primary Outcomes | ||||||||
|
Cognitions
| ||||||||
| ASEQ | ||||||||
| Mean score |
5.54(0.16) | 5.55(0.16)Δa | 5.79(0.17) | 5.80(0.17)Δc | 5.40(0.16) | 5.94(0.16)Δa | 6.05(0.17) | 6.32(0.18)Δc |
| PCS | ||||||||
| Total score |
17.36(1.0 8) |
16.97(1.1 0) |
16.13(1.1 3) | 16.41(1.1 5)Δc | 19.68(1.0 9) |
17.42(1.1 2) | 16.16(1.1 5) |
14.31(1.1 8)Δc |
| Rumination | 6.23(0.40) | 6.20(0.40) | 5.83(0.43)Δb | 6.13(0.43)Δc | 7.01(0.40) | 6.04(0.41) | 5.45(0.44)Δb | 5.04(0.45)Δc |
| Magnificati on |
3.90(0.27) | 3.80(0.26) | 3.70(0.27) | 3.76(0.28)Δc | 4.47(0.27) | 4.10(0.27) | 3.74(0.28) | 3.24(0.29)Δc |
| Helplessne ss |
7.23(0.49) | 7.00(0.51) | 6.58(0.51) | 6.51(0.52)Δc | 8.20(0.50) | 7.26(0.52) | 6.92(0.52) | 5.98(0.53)Δc |
| PAQ | ||||||||
| Total score |
20.88(0.3 2) |
21.14(0.3 7) |
21.40(0.3 7) |
21.75(0.4 1) |
20.72(0.3 3) |
21.76(0.3 8) |
22.40(0.3 8) |
22.70(0.4 2) |
| Confidence | 5.25(0.12) | 5.50(0.13) | 5.61(0.14) | 5.74(0.14) | 5.33(0.13) | 5.83(0.13) | 5.97(0.14) | 6.09(0.15) |
| Response | 15.63(0.2 6) |
15.64(0.2 8) |
15.79(0.2 7) |
16.01(0.2 9) |
15.39(0.2 6) |
15.93(0.2 9) |
16.42(0.2 7) |
16.60(0.3 1) |
|
Self- manageme nt behaviors | ||||||||
| Exercise behavior (min) | ||||||||
| Stretching | 73.82(5.9 4) |
70.98(5.7 3) |
73.07(6.0 4) |
74.39(5.9 7) |
63.72(5.9 7) |
60.22(5.8 7) |
66.11(6.1 6) |
66.87(6.1 8) |
| Aerobic exercise |
158.22(15 .22) |
165.08(17 .21) |
162.69(15 .72) |
186.95(16 .98) |
155.71(15 .34) |
173.35(17 .51) |
155.13(15 .96) |
187.97(17 .46) |
| Cognitive symptom manageme nt | ||||||||
| Mean score |
1.89(0.09) | 1.96(0.08) | 1.95(0.09) | 2.04(0.09) | 1.91(0.09) | 2.09(0.08) | 2.25(0.09) | 2.26(0.10) |
| Communic ation with physicians | ||||||||
| Mean score |
3.00 (0.10) |
2.92(0.10) | 3.18(0.11) | 3.17(0.11) | 3.13(0.10) | 3.11(0.10) | 3.28(0.11) | 3.29(0.11) |
| Pain | ||||||||
| BPI | ||||||||
| Pain Severity |
5.42(0.14) | 5.11(0.16) | 4.84(0.19) | 4.89(0.17) | 5.34(0.15) | 5.00(0.16) | 4.70(0.19) | 4.53(0.18) |
| Pain Interferenc e |
5.65(0.20) | 4.85(0.22) | 4.70(0.24) | 4.34(0.22) | 5.36(0.20) | 4.84(0.23) | 4.65(0.24) | 4.28(0.23) |
| Secondary Outcomes | ||||||||
| DASS | ||||||||
| Depression | 10.00(0.83) | 9.92(0.90) | 9.41(0.89) | 9.26(0.86) | 12.23(0.84) | 11.64(0.92) | ||
| Anxiety | 8.42(0.75) | 8.69(0.80) | 7.63(0.74) | 7.86(0.79) | 10.46(0.76) | 10.26(0.82) | ||
| Stress | 14.03(0.78) | 13.94(0.78) | 13.21(0.87) | 13.71(0.88) | 14.92(0.78) | 14.90(0.80) | ||
| CPCI | 2.52(0.18) | 2.49(0.17) | 2.48(0.18) | 2.45(0.19) | 2.84(0.19) | 3.00(0.17) | ||
| Assistance | ||||||||
| Coping | 3.94(0.18) | 3.84(0.18) | 3.89(0.18) | 4.02(0.19) | 3.92(0.18) | 4.16(0.18) | ||
| Exercise | 2.95(0.18) | 3.10(0.17) | 3.23(0.17) | 3.42(0.19) | 2.75(0.18) | 3.09(0.17) | ||
| Guarding | 3.59(0.15) | 3.28(0.15) | 3.44(0.16) | 3.41(0.17) | 3.75(0.15) | 3.52(0.15) | ||
| Persistence | 4.02(0.16) | 3.95(0.15) | 4.01(0.16) | 4.16(0.17) | 3.81(0.16) | 3.92(0.16) | ||
| Relaxation | 2.35(0.16) | 2.42(0.16) | 2.56(0.17)Δb | 2.55(0.17) | 2.38(0.16) | 2.87(0.16) | ||
| Resting | 3.89(0.17) | 3.74(0.17) | 3.74(0.18) | 3.70(0.19) | 3.97(0.17) | 3.84(0.17) | ||
| Social | 2.82(0.18) | 3.01(0.17) | 2.81(0.18) | 2.96(0.19) | 2.90(0.18) | 3.15(0.18) | ||
| AIMS | ||||||||
| Physical | 2.82(0.14) | 2.71(0.15) | 2.67(0.15) | 2.75(0.15) | 2.85(0.14) | 2.75(0.15) | ||
| Symptom | 5.78(0.21) | 5.24(0.22) | 5.17(0.24) | 5.30(0.23) | 5.76(0.21) | 5.16(0.23) | ||
| Affect | 4.10(0.17) | 4.03(0.18) | 3.88(0.18) | 3.90(0.19) | 4.42(0.17) | 4.12(0.19) | ||
| Social | 5.43(0.17) | 5.36(0.17) | 5.36(0.18) | 5.20(0.18) | 5.27(0.18) | 5.26(0.18) | ||
| Work | 2.93(0.25) | 2.13(0.25) | 2.43(0.31) | 2.28(0.28) | 2.65(0.27) | 2.46(0.26) | ||
| PGIC | 3.55(0.08)a | 3.50(0.10)b | 3.29(0.10)c | 3.11(0.08)a | ||||
Pairwise post hoc contrasts between experimental and control groups at each time point for PGIC and for the mean change in differences for all other outcomes. Least square means are presented rather than unadjusted means because we used mixed models to incorporate covariance among repeated measures.
Unique superscripts indicate significant pairwise post hoc tests (p < 0.05)
change for condition-BY-time compared to baseline
ASEQ = Arthritis Self-Efficacy Questionnaire; AIMS = Arthritis Impact Measurement Scale; BPI = Brief Pain Inventory; CPCI = Chronic Pain Coping Inventory; DASS = Depression
Significant condition-BY-time effect was noted for self-efficacy and pain catastrophizing but not for confidence in ability to manage pain and awareness of responses to pain. Specifically, a significant overall effect of condition-BY-time was noted for arthritis self-efficacy (F3, 226=3.05, p=0.0293) as measured by ASEQ. Post hoc comparisons revealed that the participants in the experimental condition reported a greater increase in ASEQ mean score from baseline to one month follow up (ES = 0.53, t=2.64, p=0.0222), and baseline to six month follow up assessment (ES = 0.66, t=2.75, p=0.0164), as compared to the control participants. Further, a significant condition-BY-time effect was found for pain catastrophizing as measured by PCS for total score (F3, 226=4.32, p=0.0055); as well as the subscales: rumination (F3, 226=4.41 p=0.0049), magnification (F3, 226=3.87, p=0.0100), and helplessness (F3, 226=2.72, p=0.0453). Post hoc tests revealed that the experimental condition reported a greater decrease in total score from baseline to six month follow up (ES = −4.22, t=−3.53, p=0.0013); a greater decrease in rumination from baseline to three month follow up (ES = −1.16, t=−2.55, p=0.0304) and baseline to six month follow up (ES = −1.87, t=−3.56, p=0.0012); a greater decrease in magnification from baseline to six month follow up assessment (ES = −1.09, t=−3.26, p=0.0037); and, a greater decrease in helplessness from baseline to six month follow up (ES = −1.5, t=−2.63, p=0.0238), as compared to the control condition.
LMMs did not reveal any condition-BY-time effect for the self-management behavior variables: amount of time spent in the past week doing exercise behaviors, the use of cognitive stress reduction (pain reduction) techniques, or reported communication with physicians.
There were also no statistically significant condition-BY-time effects for pain intensity and physical functioning as measured by BPI.
Secondary Outcomes
Differential effects of the experimental (website intervention) and the control condition over time was measured using LMMs on the following secondary outcomes pertaining to affect, coping skills, well-being, global impression of change, and user engagement.
LMMs run on each of the three subscales of the DASS did not reveal any significant effect of condition-BY-time on the depression, anxiety and stress subscales of the DASS. It should be noted that for the depression subscale the overall condition-BY-time effect yielded a p-value of 0.0577; post hoc planned comparisons showed that the experimental condition participants evidenced greater reduction in depression from baseline to six month follow-up compared to the control condition participants (ES = −2.78, t=−2.50, p=0.0333,).
A significant condition-BY-time effect was noted for the relaxation subscale of the CPCI (F3, 226=3.07, p=0.0287). Post hoc tests revealed that the experimental condition reported a greater increase in relaxation from baseline to 3 month follow-up assessment (t=2.99, p=0.0083), as compared to the control condition.
LMMs did not reveal any condition-BY-time effect for AIMS, i.e., no significant change was noted for daily life activities during the past month between the two conditions.
Significant effects were found for treatment (F1,220=20.0, p<0.0001) on participants’ global impression of change. Compared to the control group, website participants reported a more improved average impression of change at the follow up assessments for one month (ES = −0.44, t=3.83, p=0.0025), three month (ES = −0.44, t=3.06, p=0.0368), and six month (ES = −0.61, t=4.18, p<0.0001).
Moderation Analyses
Arthritis type (OA vs. RA and other) was identified as a moderator of intervention effects on the outcomes. Notably, significant three way-interactions were evidenced for the Pain Catastrophizing total score (F3,223=2.80, p=0.0411) and the magnification subscale (F3,223=2.84, p=0.039). Post-hoc comparisons revealed that participants in the experimental condition with Osteoarthritis only showed a reduction in the Pain Catastrophizing total score (t=−2.82, p=0.0282) and magnification subscale (t=−2.91, p=0.0222) from baseline to six month follow up; whereas no such change was noted for Other types of Arthritis (RA and others). Gender, age, race, and baseline pain intensity did not moderate intervention effects on the outcomes.
User Engagement Analyses
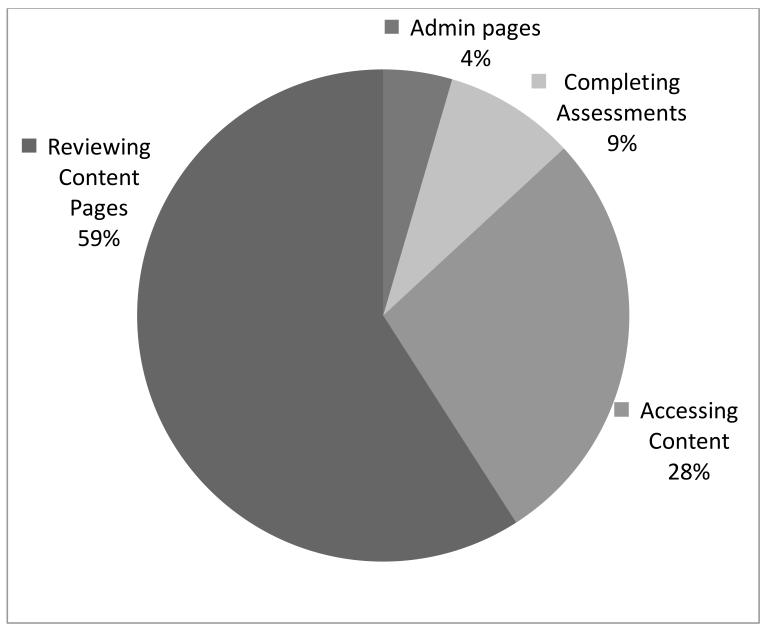
Participants in the experimental condition were asked to complete a minimum of 20 minutes on the site two times per week for four weeks which equals a total use of 160 minutes; 57.5% used the site for at least 160 minutes during the study. A review of page view data indicated that of the 44682 pages viewed in the study. 8.6% were completing assessments (e.g., Daily Pain Tracker); 27.8% were accessing content (via the personalized recommendation page [“My Page”] or the pain-specific libraries); and 59.1% were reviewing program content (e.g., articles, lesson pages, tools). The other 4.4% of the pages viewed were administrative activities, including logging in (n=1357, 3%). See Figure 2. NOTE: Only three participants in the intervention did not use the website.
Figure 2. User engagement: Number and percentage of page views per task type (total page views in study = 44682).
User engagement (low engagement versus high engagement using median minutes used) was significantly associated with improved outcomes between baseline and six month follow up.
Pain-Catastrophizing. Results from LMM revealed a significant engagement-BY-time effect for the Pain-Catastrophizing total score (F6, 225 = 2.77, p = 0 .0129) as well as the rumination (F6, 225 = 2.40, p = 0 .0287) and magnification (F6, 225 = 2.58, p = 0 .0196) subscales. Compared with controls, participants who used the site the most reported a significant decrease in total score (t=−3.49, p=0.0050), rumination (t=−3.41, p= 0.0068), and magnification (t=−2.94, p=0.0272) from baseline to six month assessment, whereas no significant change was noted in the low engagement group relative to the control condition.
Cognitive Symptom Management. Results from LMM revealed a significant engagement-BY-time effect for Cognitive Symptom Management (F6, 225 = 3.58, P 0.0021). Compared with controls, participants who used the site the most reported greater increases in Cognitive Symptom Management from baseline to three month assessment (t = 3.64, p = 0.0029) and baseline to six month assessment (t=3.05, p = 0.0188); whereas no significant change was noted in the low engagement group relative to the control condition. When comparing the low and high engagement group, it was noted that high engagement participants reported significantly greater increases in Cognitive Symptom Management compared with low engagement participants, from baseline to three month follow up (t = 2.89, p = 0.0300) and baseline to six month follow up (t=2.93, p = 0.0270).
Communication with Physician. Results from LMM revealed a significant engagement-BY-time effect for Communication with Physician scale (F6, 225 = 2.43, P 0.0271). When comparing the low and high engagers, it was noted that high engagers reported significantly greater increases in Communication with Physician compared with low engagers, from baseline to six month follow up (t = 2.75, p = 0.0448).
DISCUSSION
The original goal of this study was to expand painACTION’s relevance and reach to people with arthritis pain. This activity extended previous work on painACTION with other pain patient populations: back pain (Chiauzzi et al., 2010), migraine pain (Bromberg et al., 2011), and neuropathic pain (DasMahapatra et al., 2013). Unlike other studies of painACTION, we did not find that arthritis pain participants in the experimental condition had significantly greater change over time in worst pain (Chiauzzi et al., 2010; DasMahapatra et al., 2013), pain severity (DasMahapatra et al., 2013), pain interference (DasMahapatra et al., 2013), stress (Bromberg et al., 2011; Chiauzzi et al., 2010), and depression (Bromberg et al., 2011; DasMahapatra et al., 2013) than those in the control condition. Like these other studies, arthritis pain participants in the experimental condition had significantly greater change over time in self-efficacy to manage pain (Bromberg et al., 2011; DasMahapatra et al., 2013), global impression of change (Chiauzzi et al., 2010), pain catastrophizing (Bromberg et al., 2011), and use of the coping strategies of coping self-statements (Chiauzzi et al., 2010) and relaxation (Bromberg et al., 2011) than those in the control condition. Differences between painACTION – Arthritis and other pain modules on the site were somewhat expected given the different populations but the lack of changes in health outcomes in the arthritis pain sample is disappointing.
Changes were only found between conditions for two of the primary outcomes in this study: self-efficacy and catastrophizing. Self-efficacy, or the confidence one has in the ability to manage arthritis pain, is a primary outcome of a well-studied self-management program for arthritis delivered in groups (Lorig et al., 2005) and has been described as the goal of self-management education programs (Bodenheimer et al., 2002). Lorig et al. (2008) found increases in self-efficacy in the online intervention group at six month follow-up compared to the treatment-as-usual group; these findings were maintained at one year.
Pain catastrophizing is described as negative emotional and cognitive processes (Edwards et al., 2006) and has been associated with a variety of negative health outcomes, which include increases in pain severity, affective distress, muscle and joint tenderness, and pain-related disability (see review by Edwards et al., 2006). Catastrophizing has been proposed as an important variable for understanding osteoarthritis and rheumatologic pain conditions (Edwards et al., 2006; Somers et al., 2009). Our intervention showed decreases in pain catastrophizing between the intervention and control groups. Interestingly, participants in the experimental condition with OA showed significantly greater reductions in pain catastrophizing from baseline to 6 months compared to individuals with RA or another arthritic condition. The manner in which catastrophizing is related to outcomes remains uncertain. Catastrophizing has been proposed as a mediator of depression and treatment outcome of CBT (Smeets et al., 2006), and a mediator or moderator of treatment in rheumatologic disease (Edwards et al., 2010).
Other important hypothesized outcomes were not significant in our study, including pain intensity, arthritis-related well-being, health behaviors, and pain awareness. Nonsignificant findings in terms of pain intensity are similar to other trials, where only small changes or no changes in pain are found (Macea et al., 2010).
Individuals in the intervention group with high engagement (i.e., more than 205 minutes on the site) showed greater improvement in pain catastrophizing, cognitive symptom management and communication with physicians than did individuals who spent less time on the site. As a subsequent review of the painACTION page view data indicated active user interaction with the content pages (e.g., articles, lessons, tools), perhaps requiring more than 160 minutes of initial program exposure (i.e., two times per week for 20 minutes for four weeks) might have resulted in additional significant outcomes.
Another possible explanation for the absence of results related to pain and health behaviors is that the required activities on the site were more focused toward the outcomes that were significant than those that were not. Our measure of self-efficacy was a broad measure developed for arthritis, so self-efficacy for pain and functioning –the intended targets of the experimental intervention -- were only parts of that measure. In addition, measures that were used to test the Arthritis Self-Management Program (ASMP; e.g., Lorig et al., 2008) were chosen for this study to be consistent with published literature. Of note, the ASMP focuses on making weekly action plans with weekly accountability to peers and peer-leaders. A recent qualitative analysis of a similar program with 277 individuals with chronic disease showed action plans focused primarily on health behaviors (exercise 59%; healthy eating/weight loss 32%; Lorig et al., 2014). This is a much more intensive intervention than the independent (i.e., no interaction with peers or peer-leaders) online patient education experience provided by painACTION which appears to have been helpful only in changing cognitive factors.
Exploratory analyses of potential moderators were also not significant. This lack of significant results for demographic variables as moderators is consistent with previous work on CBT interventions (McCracken & Turk, 2002), including a recently published secondary analysis of the collective data from painACTION studies (DasMahapatra et al., 2014).
Limitations of this study include the following: recruitment from primarily online sources, reliance on a self-reported doctor diagnosis of arthritis, the lack of cultural diversity in the participant population, the potential influence of unmeasured variables on use of the intervention, and differential results for some outcomes across time. Because differences were found in a previous painACTION study between online recruits and those from a pain center (Chiauzzi et al., 2010), our primarily online sample may not be generalizable to a sample recruited from a clinical practice. Reliance on a self-reported doctor diagnosis of arthritis was a compromise in rigor motivated by the feasibility of collecting national data with a limited timeframe and budget. We included moderate level of pain as an inclusion criteria and reviewed reports of website use by the intervention group to confirm that intervention group participants were using the site. Additionally, our sample was primarily educated, white women who have a high SES, similar to other studies in arthritis pain (Bruce et al., 2007). The website is publically available but it is important to reach individuals beyond this specific cohort to increase use of self-management strategies for pain.
Given these limitations, the other significant secondary outcomes that were found are interpreted with caution. There were significant increases in coping through relaxation and impression of global change between the intervention and control groups. Relaxation has been shown to be helpful in changing pain for individuals with RA when compared to CBT over 12 months (Barsky et al., 2010). The directed portion of our intervention included multimedia presentations of relaxation, a guided imagery tool, and chair yoga, which may have increased the use of this strategy in the intervention group over the 3 months. However, use of this strategy did not persist to the six-month follow-up. Additionally, the reported use of other coping strategies was not significantly different between the intervention and control groups. A recent review suggests that when considered longitudinally, the evidence for coping strategies predicting psychological distress in RA is weak (Vriezekolk et al., 2011). Clearly the impact of coping strategies was small in our study for unknown reasons. It could be that the study attracted individuals who coped in an action-oriented manner as manifested by their willingness to participate in the study and/or that the content was not delivered in a manner that promoted knowledge of coping versus the development of coping skills. Further research is needed to clarify coping outcomes from CBT-guided self management delivered in an online educational format. Interestingly, participants’ impression of global change was different in the intervention group compared to the control group at all follow-up periods indicating that they thought their use of painACTION had a positive impact.
The question remains open about how participation in independent (i.e., no active peer or peer leader support) online self management programs impacts living with arthritis pain. In this sample of adults with arthritis pain, we observed changes in self-efficacy and catastrophizing, but not in the level of worst pain as found in painACTION studies of adults with back pain (Chiauzzi et al., 2010) and adults with neuropathic pain (DasMahapatra et al., 2013). Perhaps those with arthritis pain who receive an independent online self management intervention require more than six months’ time for cognitive changes in self-efficacy and catastrophizing to impact reported pain level; studies with longer follow up periods would be required to test this hypothesis. Additionally, future investigations of online interventions with this population could emphasize setting specific personal health behavior goals that are tracked and monitored over time to help maximize the potential impact on pain.
INFORMED CONSENT STATEMENT
‘All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 (5). Informed consent was obtained from all patients for being included in the study.’
ACKNOWLEDGEMENTS
The authors would like to thank the following individuals for their contributions to this project: Ted Fields, Suzanne Gauthier, Penney Cowan, Mila Pavek, Emil Chiauzzi, Jonas Bromberg, Synne Wing Venuti, Evelyn Corsini, and Pedro Teixeira. Thanks also to the reviewers who provided input on previous drafts.
Research Funding: This work was supported by a grant from the National Institutes of Arthritis and Musculoskeletal and Skin Diseases (5R44AR061191-03). The funders had no part in designing the study, the collection of data and its analysis, or in the decision to complete or write this manuscript.
Footnotes
CONFLICT OF INTEREST STATEMENT
Conflicts of Interest: KT and KZ are current employees of Inflexxion, Inc., Newton, MA. RW, RB, and PD were employees of Inflexxion, Inc., Newton, MA at the time this study was conducted. LP has no conflicts to report.
REFERENCES
- Allison PD. [Accessed August 1, 2013];Handling missing data by maximum likelihood [Statistical Horizons SAS Global Forum] 2012 Available at: http://www.statisticalhorizons.com/wpcontent/uploads/MissingDataByML.pdf.
- Antony MM, Bieling PJ, Cox BJ, Enns MW, Swinson RP. Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scales (DASS) in clinical groups and a community sample. Psychological Assessment. 1998;10:176–181. [Google Scholar]
- Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychological Reviews. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: The exercise of control. Freeman; New York: 1997. [Google Scholar]
- Barsky AJ, Ahern DK, Orav EJ, Nestoriuc Y, Liang MH, Berman IT, Wilk KG. A Randomized Trial of Three Psychosocial Treatments for the Symptoms of Rheumatoid Arthritis. Seminars in Arthritis and Rheumatism. 2010;40(3):222–232. doi: 10.1016/j.semarthrit.2010.04.001. doi:10.1016/j.semarthrit.2010.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benka J, Nagyova I, Rosenberger J, Calfova A, Macejova Z, Middel B, Groothoff JW. Social support and psychological distress in rheumatoid arthritis: a 4-year prospective study. Disability and Rehabilitation. 2012;34(9):754–61. doi: 10.3109/09638288.2011.619618. doi:10.3109/09638288.2011.619618. [DOI] [PubMed] [Google Scholar]
- Berman RLH, Iris MA, Bode R, Drengenberg C. The effectiveness of an online mind-body intervention for older adults with chronic pain. The Journal of Pain : Official Journal of the American Pain Society. 2009;10(1):68–79. doi: 10.1016/j.jpain.2008.07.006. doi:10.1016/j.jpain.2008.07.006. [DOI] [PubMed] [Google Scholar]
- Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA : The Journal of the American Medical Association. 2002;288(19):2469–75. doi: 10.1001/jama.288.19.2469. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/12435261. [DOI] [PubMed] [Google Scholar]
- Bromberg J, Wood ME, Black RA, Surette DA, Zacharoff KL, Chiauzzi EJ. A Randomized Trial of a Web-Based Intervention to Improve Migraine Self-Management and Coping. Headache. 2011;42:244–261. doi: 10.1111/j.1526-4610.2011.02031.x. doi:10.1111/j.1526-4610.2011.02031.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruce B, Lorig K, Laurent D. Participation in patient self-management programs. Arthritis and Rheumatism. 2007;57(5):851–4. doi: 10.1002/art.22776. doi:10.1002/art.22776. [DOI] [PubMed] [Google Scholar]
- Burns JW, Kubilus A, Bruehl S, et al. Do changes in cognitive factors influence outcome following multidisciplinary treatment for chronic pain? A cross-lagged panel analysis. Journal of Consulting and Clinical Psychology. 2003;71(1):81–91. doi: 10.1037//0022-006x.71.1.81. [DOI] [PubMed] [Google Scholar]
- Chiauzzi E, Pujol LA, Wood M, Bond K, Black R, Yiu E, Zacharoff K. painACTION-Back Pain : A Self-Management Website for People with Chronic Back Pain. 2010:1044–1058. doi: 10.1111/j.1526-4637.2010.00879.x. [DOI] [PubMed] [Google Scholar]
- Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Annals of the Academy of Medicine, Singapore. 1994;23(2):129–38. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/8080219. [PubMed] [Google Scholar]
- Crawford JR, Henry JD. The Depression Anxiety Stress Scales (DASS): normative data and latent structure in a large non-clinical sample. The British Journal of Clinical Psychology / the British Psychological Society. 2003;42(Pt 2):111–31. doi: 10.1348/014466503321903544. doi:10.1348/014466503321903544. [DOI] [PubMed] [Google Scholar]
- D’Eon JL, Harris CA, Ellis JA. Testing factorial validity and gender invariance of the pain catastrophizing scale. Journal of Behavioral Medicine. 2004;27(4):361–72. doi: 10.1023/b:jobm.0000042410.34535.64. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/15559733. [DOI] [PubMed] [Google Scholar]
- DasMahapatra P, Chiauzzi E, Pujol LM, Los C, Trudeau KJ. Mediators and moderators of chronic pain outcomes in an online self-management program. Clinical Journal of Pain. 2014 doi: 10.1097/AJP.0000000000000125. doi: 10.1097/AJP.0000000000000125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DasMahapatra P, Bromberg J, Black R, Venuti S, Zacharoff K. Self-Management Website for people with Chronic Neuropathic Pain: Findings from a Randomized Controlled Trial. MA; Newton: 2013. [Google Scholar]
- Dixon KE, Keefe FJ, Scipio CD, Perri LM, Abernethy AP. Psychological interventions for arthritis pain management in adults: A metaanalysis. Health Psychology. 2007;26:241–250. doi: 10.1037/0278-6133.26.3.241. [DOI] [PubMed] [Google Scholar]
- Edwards RR, Bingham CO, Bathon J, Haythornthwaite JA. Catastrophizing and pain in arthritis, fibromyalgia, and other rheumatic diseases. Arthritis and Rheumatism. 2006;55(2):325–32. doi: 10.1002/art.21865. doi:10.1002/art.21865. [DOI] [PubMed] [Google Scholar]
- Edwards RR, Giles J, Bingham CO, Campbell C, Haythornthwaite JA, Bathon J. Moderators of the negative effects of catastrophizing in arthritis. Pain Medicine (Malden, Mass.) 2010;11(4):591–9. doi: 10.1111/j.1526-4637.2010.00804.x. doi:10.1111/j.1526-4637.2010.00804.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farrar JT, Young JP, LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94(2):149–58. doi: 10.1016/S0304-3959(01)00349-9. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11690728. [DOI] [PubMed] [Google Scholar]
- Fox S. Online health search 2006. 2007 Retrieved March 22, 2007, from http://www.pewinternet.org/pdfs/PIP_Online_Health_2006.pdf.
- Gloster AT, Rhoades HM, Novy D, Klotsche J, Senior A, Kunik M, Stanley MA. Psychometric properties of the Depression Anxiety and Stress Scale-21 in older primary care patients. Journal of Affective Disorders. 2008;110(3):248–59. doi: 10.1016/j.jad.2008.01.023. doi:10.1016/j.jad.2008.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guillemin F, Challier B, Urlacher F, Vançon G, Pourel J. Quality of life in ankylosing spondylitis: validation of the ankylosing spondylitis Arthritis Impact Measurement Scales 2, a modified Arthritis Impact Measurement Scales Questionnaire. Arthritis Care and Research : The Official Journal of the Arthritis Health Professions Association. 1999;12(3):157–62. doi: 10.1002/1529-0131(199906)12:3<157::aid-art2>3.0.co;2-r. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10513505. [DOI] [PubMed] [Google Scholar]
- Guy W. ECDEU Assessment Manual for Psychopharmacology. U.S. Department of Health, Education, and Welfare; Rockville, MD: 1976. [Google Scholar]
- Jensen MP, Neilson WR, Kerns RD. Toward the development of a motivational model of pain self-management. The Journal of Pain. 2003;4:477–492. doi: 10.1016/s1526-5900(03)00779-x. [DOI] [PubMed] [Google Scholar]
- Jensen MP, Turner JA, Romano JM, Strom SE. The Chronic Pain Coping Inventory: development and preliminary validation. Pain. 1995;60(2):203–16. doi: 10.1016/0304-3959(94)00118-X. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/7784106. [DOI] [PubMed] [Google Scholar]
- Keller S, Bann CM, Dodd SL, Schein J, Mendoza TR, Cleeland CS. Validity of the brief pain inventory for use in documenting the outcomes of patients with noncancer pain. The Clinical Journal of Pain. 2004;20(5):309–18. doi: 10.1097/00002508-200409000-00005. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/15322437. [DOI] [PubMed] [Google Scholar]
- Kernan WN, Viscoli CM, Makuch RW, Brass LM, Horwitz RI. Stratified randomization for clinical trials. Journal of Clinical Epidemiology. 1999;52(1):19–26. doi: 10.1016/s0895-4356(98)00138-3. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/9973070. [DOI] [PubMed] [Google Scholar]
- Lawrence RC, Felson DT, Helmick CG, Arnold LM, Choi H, Deyo R. a,, Wolfe F. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis and Rheumatism. 2008;58(1):26–35. doi: 10.1002/art.23176. doi:10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorig K, Chastain RL, Ung E, Shoor S, Holman HR. Development and evaluation of a scale to measure perceived self-efficacy in people with arthritis. Arthritis and Rheumatism. 1989;32(1):37–44. doi: 10.1002/anr.1780320107. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/2912463. [DOI] [PubMed] [Google Scholar]
- Lorig K, Laurent DD, Plant K, Krishnan E, Ritter PL. The components of action planning and their associations with behavior and health outcomes. Chronic Illness. 2014;10:50–59. doi: 10.1177/1742395313495572. doi: 10.1177/1742395313495572. [DOI] [PubMed] [Google Scholar]
- Lorig KR, Ritter PL, Laurent DD, Plant K. The internet-based arthritis self-management program: a one-year randomized trial for patients with arthritis or fibromyalgia. Arthritis and Rheumatism. 2008;59(7):1009–17. doi: 10.1002/art.23817. doi:10.1002/art.23817. [DOI] [PubMed] [Google Scholar]
- Lorig KR, Ritter P, Stewart AL, Sobel DS, Brown BW, Bandura A, et al. Chronic disease self-management program: 2-year health status and health care utilization outcomes. Medical Care. 2001;39(11):1217–23. doi: 10.1097/00005650-200111000-00008. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11606875. [DOI] [PubMed] [Google Scholar]
- Lorig K, Ritter PL, Plant K. A disease-specific self-help program compared with a generalized chronic disease self-help program for arthritis patients. Arthritis and Rheumatism. 2005;53(6):950–7. doi: 10.1002/art.21604. doi:10.1002/art.21604. [DOI] [PubMed] [Google Scholar]
- Lorig K, Stewart A, Ritter P, Gonzalez V, Laurent D, Lynch J. Outcome Measures for Health Education and Other Health Care Interventions: SAG Publications, Inc.; Thousand Oaks, CA: 1996. Retrieved from http://www.sagepub.com/books/Book5623. [Google Scholar]
- Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales. 2nd ed. Psychology Foundation; Sydney: 1995. [Google Scholar]
- Macea DD, Gajos K, Daglia A. The Efficacy of Web-Based Cognitive Behavioral Interventions for Chronic Pain: A Systematic Review and Meta-Analysis. The Journal of Pain. 2010;11(10):917–929. doi: 10.1016/j.jpain.2010.06.005. doi:10.1016/j.jpain.2010.06.005. [DOI] [PubMed] [Google Scholar]
- Marks R. Efficacy theory and its utility in arthritis rehabilitation: review and recommendations. Disability and Rehabilitation. 2001;23(7):271–80. doi: 10.1080/09638280010004162. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11354579. [DOI] [PubMed] [Google Scholar]
- Marks R, Allegrante JP, Lorig K. A review and synthesis of research evidence for self-efficacy-enhancing interventions for reducing chronic disability: Implications for health education practice (Part I) Health Promotions Practice. 2005a;6:37–43. doi: 10.1177/1524839904266790. [DOI] [PubMed] [Google Scholar]
- McCaffery M, Beebe A. Pain: Clinical Manual for Nursing Practice. V. V. Mosby Company; Baltimore, M.D.: 1993. [Google Scholar]
- McCracken LM, Turk DC. Behavioral and cognitive-behavioral treatment for chronic pain: Outcome, predictors of outcome, and treatment process. Spine. 2002;27(22):2564–2573. doi: 10.1097/00007632-200211150-00033. [DOI] [PubMed] [Google Scholar]
- Mendoza T, Mayne T, Rublee D, Cleeland C. Reliability and validity of a modified Brief Pain Inventory short form in patients with osteoarthritis. European Journal of Pain (London, England) 2006;10(4):353–61. doi: 10.1016/j.ejpain.2005.06.002. doi:10.1016/j.ejpain.2005.06.002. [DOI] [PubMed] [Google Scholar]
- Molton IR, Graham C, Stoelb BL, Jensen MP. Current psychological approaches to the management of chronic pain. Current Opinion in Anaesthesiology. 2007;20(5):485–9. doi: 10.1097/ACO.0b013e3282ef6b40. doi:10.1097/ACO.0b013e3282ef6b40. [DOI] [PubMed] [Google Scholar]
- Murray E, Burns J, See Tai S, Lai R, Nazareth I. Interactive Health Communication Applications for people with chronic disease (Review) Cochrane Database Of Systematic Reviews. 2005;(4) doi: 10.1002/14651858.CD004274.pub4. Art. No.: CD004274. doi:10.1002/14651858.CD004274.pub4. [DOI] [PubMed] [Google Scholar]
- Newman S, Steed L, Mulligan K. Self-management interventions for chronic illness. Lancet. 2004;364(9444):1523–37. doi: 10.1016/S0140-6736(04)17277-2. doi:10.1016/S0140-6736(04)17277-2. [DOI] [PubMed] [Google Scholar]
- Nicassio PM, Kay MA, Custodio MK, Irwin MR, Olmstead R, Weisman MH. An evaluation of a biopsychosocial framework for health-related quality of life and disability in rheumatoid arthritis. Journal of Psychosomatic Research. 2011;71(2):79–85. doi: 10.1016/j.jpsychores.2011.01.008. doi:10.1016/j.jpsychores.2011.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osman A, Barrios FX, Gutierrez PM, Kopper BA, Merrifield T, Grittmann L. The Pain Catastrophizing Scale: further psychometric evaluation with adult samples. Journal of Behavioral Medicine. 2000;23(4):351–65. doi: 10.1023/a:1005548801037. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10984864. [DOI] [PubMed] [Google Scholar]
- Ren XS, Kazis L, Meenan RF. Short-form Arthritis Impact Measurement Scales 2: tests of reliability and validity among patients with osteoarthritis. Arthritis Care and Research : The Official Journal of the Arthritis Health Professions Association. 1999;12(3):163–71. doi: 10.1002/1529-0131(199906)12:3<163::aid-art3>3.0.co;2-z. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10513506. [DOI] [PubMed] [Google Scholar]
- Romano JM, Jensen MP, Turner JA. The chronic pain coping inventory-42 : reliability and validity. Pain. 2003;104:65–73. doi: 10.1016/s0304-3959(02)00466-9. doi:10.1016/S0304-3959(02)00466-9. [DOI] [PubMed] [Google Scholar]
- SAS Institute . Sas 9.3 System Options: Reference. SAS Institute; 2011. p. 336. Retrieved from http://books.google.com/books?id=x2mkj8YTYa0C&pgis=1. [Google Scholar]
- Schabenberger O. Introducing the GLIMMIX Procedure for Generalized Linear Mixed Models; Proceedings of the Thirtieth Annual SAS Users Group International Conference; Cary, NC: SAS Institute Inc. 2005. [Google Scholar]
- Simpson C, Franks C, Morrison C, Lempp H. The patient’s journey: rheumatoid arthritis. BMJ (Clinical Research Ed.) 2005;331(7521):887–9. doi: 10.1136/bmj.331.7521.887. doi:10.1136/bmj.331.7521.887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smeets RJEM, Vlaeyen JWS, Kester ADM, Knottnerus JA. Reduction of pain catastrophizing mediates the outcome of both physical and cognitive-behavioral treatment in chronic low back pain. The Journal of Pain : Official Journal of the American Pain Society. 2006;7(4):261–71. doi: 10.1016/j.jpain.2005.10.011. doi:10.1016/j.jpain.2005.10.011. [DOI] [PubMed] [Google Scholar]
- Smith BW, Zautra AJ. Vulnerability and Resilience in Women With Arthritis : Test of a Two-Factor Model. J Consult Clin Psychol. 2008;76(5):799–810. doi: 10.1037/0022-006X.76.5.799. doi:10.1037/0022-006X.76.5.799. [DOI] [PubMed] [Google Scholar]
- Somers TJ, Keefe FJ, Godiwala N, Hoyler GH. Psychosocial factors and the pain experience of osteoarthritis patients: new findings and new directions. Current Opinion in Rheumatology. 2009;21(5):501–6. doi: 10.1097/BOR.0b013e32832ed704. doi:10.1097/BOR.0b013e32832ed704. [DOI] [PubMed] [Google Scholar]
- Stinson JN, McGrath PJ, Hodnett ED, Feldman BM, Duffy CM, Huber LB, White ME. An internet-based self-management program with telephone support for adolescents with arthritis: A pilot randomized controlled trial. Journal of Rheumatology. 2010;37:1944–1952. doi: 10.3899/jrheum.091327. [DOI] [PubMed] [Google Scholar]
- Sullivan MJL, Bishop SR, Pivik J. The Pain Catastrophizing Scale: Development and Validation. Psychological Assessment. 1995;7(4):524–32. Retrieved from http://www.eric.ed.gov/ERICWebPortal/search/detailmini.jsp?_nfpb=true&_&ERICExtSearch_SearchValue_0=EJ523917&ERICExtSearch_SearchType_0=no&accno=EJ523917. [Google Scholar]
- Ten Klooster PM, Veehof MM, Taal E, van Riel PLCM, van de Laar MAFJ. Confirmatory factor analysis of the Arthritis Impact Measurement Scales 2 short form in patients with rheumatoid arthritis. Arthritis and Rheumatism. 2008;59(5):692–8. doi: 10.1002/art.23569. doi:10.1002/art.23569. [DOI] [PubMed] [Google Scholar]
- Trudeau KJ, Ainscough JL, Pujol LA, Charity S. What arthritis pain practitioners and patients want in an online self-management programme. Musculoskeletal Care. 2010;8(4):189–196. doi: 10.1002/msc.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vovici Corporation . Vovici 6. Vovici Corporation; Herndon, VA: 2012. [Google Scholar]
- Vriezekolk JE, van Lankveld WGJM, Geenen R, van den Ende CHM. Longitudinal association between coping and psychological distress in rheumatoid arthritis: a systematic review. Annals of the Rheumatic Diseases. 2011;70(7):1243–50. doi: 10.1136/ard.2010.143271. doi:10.1136/ard.2010.143271. [DOI] [PubMed] [Google Scholar]
- Westfall PH, Tobias RRD, Wolfinger RD. Multiple comparisons and multiple tests using SAS. 2nd ed. SAS Institute; Cary, NC: 2011. p. 625. Retrieved from http://books.google.com/books/about/Multiple_comparisons_and_multiple_tests.html?id=pnWf5pWYjSEC&pgis=1. [Google Scholar]
- Williams A, Eccleston C, Morley S. Psychological therapies for the management of chronic pain (excluding headache) in adults (Review) Cochrane Database Syst Rev. 2012;11:CD007407. doi: 10.1002/14651858.CD007407.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zautra AJ, Fasman R, Parish BP, Davis MC. Daily fatigue in women with osteoarthritis, rheumatoid arthritis, and fibromyalgia. Pain. 2007;128(1-2):128–135. doi: 10.1016/j.pain.2006.09.004. doi:10.1016/j.pain.2006.09.004. [DOI] [PubMed] [Google Scholar]