Abstract
Presacral teratoma is extremely rare in adults. A 35-year-old lady was diagnosed with presacral teratoma on MRI abdomen and pelvis. The tumour was enucleated laparoscopically, this being the first such case to be reported in India and fifth case in world literature. Though traditionally, anterior approach of the presacral tumours meant laparotomy, but recently, laparoscopy has been reported as a safe and effective option for these tumours with the advantages of a magnified view in the narrow pelvis, easier development of natural planes by pneumoperitoneum, faster recovery and less complications if expertise is available.
Keywords: Presacral teratoma in adult, MRI, Laparoscopic removal, Advantage
Sacrococcygeal teratoma in adults occurs at a rate between 1 in 40,000 and 63,000 with a female preponderance of 3:1 [1]. According to Altman Classification, they are of four types: type I tumours are predominantly external; type II are predominantly external but have a small but intrapelvic component; type III are predominantly intrapelvic, with a small external mass; and type IV tumours are entirely internal, otherwise known as retrorectal or presacral teratoma. Type IV tumours are excised by posterior (perineal), anterior (abdominal) or combined approach. Laparoscopic management of such cases is a new addition in surgical armamentarium. Very few cases have been reported to be successful in this endeavour.
Case Report
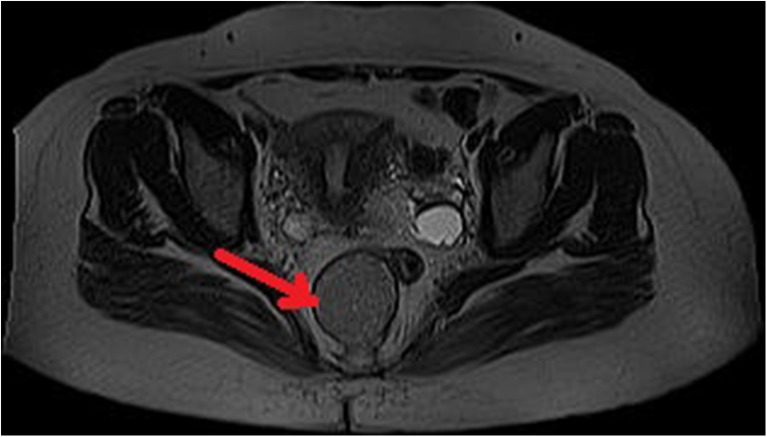
A 35-year-old lady presented with dull aching pain in the lower abdomen. On per rectal examination, lower part of a tense cystic mass was palpated which was nontender and had restricted mobility; rectal mucosa was not involved. There was no evidence of neurologic involvement. Transvaginal sonography followed by MRI abdomen and pelvis showed “well defined lesion of about 6.7X4.4X4.7cm size, in presacral space extending inferiorly posterior to the anal canal. It appeared hypointense on T1 weighted imaging with multiple calcific foci and hyperintense in T2 weighted images. There was no evidence of post contrast enhancement of the lesion, involvement of adjacent structures or intraspinal extension (Fig. 1).” Serum tumour markers, including human chorionic gonadotropin, alpha-fetoprotein, carcinoembryonic antigen, lactate dehydrogenase and CA 125 were in normal range. The patient was taken up for laparoscopic excision based on clinical and radiological findings. In brief, the patient was placed in the modified lithotomy position. Access was gained with a 10-mm supraumbilical port followed by two 5-mm ports in the left and right lower quadrant 2 cm medial and above the anterior superior iliac spine and another 5-mm port 1 cm lateral to midline at the same level. The abdomen was insufflated to a pressure of 12 mmHg with CO2. Uterus was anteverted and deviated to the right with a vaginal manipulator and the rectum was deviated to the right side with a rectal probe. The mesorectal dissection from the sacral promontory was continued up to the level of the levator ani muscles keeping medial to the left ureter. The cyst was made prominent by pushing it towards the left by an assistant’s finger in the rectum (Fig. 2). The cyst was enucleated using an ultrasonic scalpel. The contents of the cyst were aspirated and the cyst wall was removed in an Endobag. The rectal wall was not breached, and the presacral fascia was fully intact. Operative time was 135 min and blood loss was approximately 100 ml. The patient was discharged after 24 h. Histopathology of the tumour showed mature cystic teratoma with squamous epithelial lining, keratin material and muscle tissue beneath it. One year after the surgery, the patient is now asymptomatic without clinical and imaging signs of local or regional recurrence.
Fig. 1.
T1 weighted image of the presacral cyst (pointed with the arrow) showing clear planes between cyst and adjacent structures
Fig. 2.

Presacral tumour after mesorectal dissection (shown with the cannula)
Discussion
MRI, because of its multiplanar imaging capability as well as its good soft tissue contrast, is a helpful technique to define the extent of the retrorectal tumour and its relationship to the surrounding structures so as to choose the best surgical approach. In this case, MRI showed calcifications within a completely cystic mass, clear planes between the lesion and the adjacent structures suggesting that this was a benign tumour, most probably teratoma. For these lesions, complete surgical excision is the best diagnostic and therapeutic option [2]. Surgical approaches used for excision may be anterior (abdominal), posterior or combined each with their own advantages depending on the location of the tumour and the surgeon’s expertise. Digital rectal examination is helpful to choose the approach. If the superior border of tumour can be palpated, the posterior approach can be performed successfully; otherwise, anterior approach is preferable because of less injury to the sphincter [3]. Though traditionally, anterior approach meant laparotomy, but recently, laparoscopy has been reported as a safe and effective option for presacral tumours with the advantages of a magnified view in the narrow pelvis, easier development of natural planes by pneumoperitoneum, faster recovery, and less complications such as bleeding, postoperative pain, adhesion and better cosmesis. Till now, only four cases of retrorectal teratoma excised solely by laparoscopy have been reported in world literature [4–7]. Though traditionally, in laparotomy, excision of coccyx was being done; due to the rarity of such cases, no firm guideline exists. In none, the previously reported laparoscopic removal of retrorectal teratoma coccyx was excised, so in this case also, only the mass was excised. One year after surgery, the patient is now symptom and recurrence free. This is the first of such case to be reported in India. In none of the cases previously reported, there was any complication or recurrence of the lesion. We suggest that if expertise is available, laparoscopic removal of presacral teratoma should be considered.
Acknowledgments
Conflict of Interest
None.
References
- 1.Paramythiotis D, Papavramidis TS, Michalopoulos A, Papadopoulos VN, Apostolidis S, Televantou D, Hytiroglou P. Chronic constipation due to presacral teratoma in a 36-year-old woman: a case report. J Med Case Rep. 2010;4:23. doi: 10.1186/1752-1947-4-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dunn KB. Retrorectal tumors. Surg Clin N Am. 2010;90:163–171. doi: 10.1016/j.suc.2009.09.009. [DOI] [PubMed] [Google Scholar]
- 3.Murdock J, Abbas MA. Laparoscopic abdomino-paracoccygeal resection of anorectal cystic teratoma. JSLS. 2010;14(4):583–586. doi: 10.4293/108680810X12924466008600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bong-Hyeon Kye H-JK, Lee I-K, Kim D-H, Dae-Youn Won W-KK, Seong-Taek O. A laparoscopic excision of a retrorectal cystic teratoma: a case report. J Korean Soc Coloproctol. 2009;25(6):441–444. doi: 10.3393/jksc.2009.25.6.441. [DOI] [Google Scholar]
- 5.Chen Y, Xu H, Li Y, Li J, Wang D, Yuan J, Liang Z. Laparoscopic resection of presacral teratomas. J Minim Invasive Gynecol. 2008;15(5):649–651. doi: 10.1016/j.jmig.2008.06.011. [DOI] [PubMed] [Google Scholar]
- 6.Krzysztof Szyllo NL. Sacrococcygeal teratoma—case report and review of the literature. Am J Case Rep. 2013;14:1–5. doi: 10.12659/AJCR.883727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tsutsui A, Nakamura T, Mitomi H, Onozato W, Sato T, Ozawa H, Naito M, Ikeda A, Ihara A, Watanabe M. Successful laparoscopic resection of a sacrococcygeal teratoma in an adult: report of a case. Surg Today. 2011;41(4):572–575. doi: 10.1007/s00595-010-4274-4. [DOI] [PubMed] [Google Scholar]