Abstract
Spinal cord compression is a not uncommon complication of metastatic prostate cancer. Intracranial metastasis of prostatic adenocarcinoma is however unusual. We report a case of a 67-year-old man with metastatic prostate carcinoma, who presented with a 3-day history of lower limb weakness and collapse. Neurological assessment demonstrated increased tone and reduced power in both legs. As he had typical signs and symptoms of spinal cord compression, an MRI of the spine was performed; this demonstrated no evidence of cord compression. A subsequent CT of the brain demonstrated an extensive parafalcine metastasis. This revealed an extensive enhancing mass extending bilaterally along almost the entire length of the falx cerebri, measuring up to 3 cm in width and associated with marked white matter oedema in the adjacent brain bilaterally. Unfortunately, this man succumbed to his illness a few days later. The imaging findings are presented and highlight the importance of brain imaging in patients presenting with suspected cord compression due to prostatic metastatic disease when MR of the spine shows no evidence of cord compression.
Keywords: Prostate cancer, Spinal cord compression, Intracranial metastases, Oncology
Case Report
A 67-year-old retired man presented to the Urology Outpatients with bony pain and a PSA of 472 μg/l. His bone scan and cross-sectional imaging confirmed bony and liver mets; he was duly commenced on hormone therapy. Over the next 4 months, his PSA reduced from 472 to 7.3 μg/l and remained largely asymptomatic. Six months later, however, he presented acutely to the Emergency Department with a 3-day history of lower limb weakness and collapse. There was no history of pain or paraesthesia. Neurological examination revealed increased tone and reduced power in both legs with brisk knee and ankle reflexes. The rest of his examination was normal, he had normal vital signs and his baseline blood tests were unremarkable. He was admitted to the hospital and started on dexamethasone on the basis of suspected spinal cord compression. An urgent MRI of the spine was ordered; this showed several vertebral body metastases, but no overt evidence of cord compression.
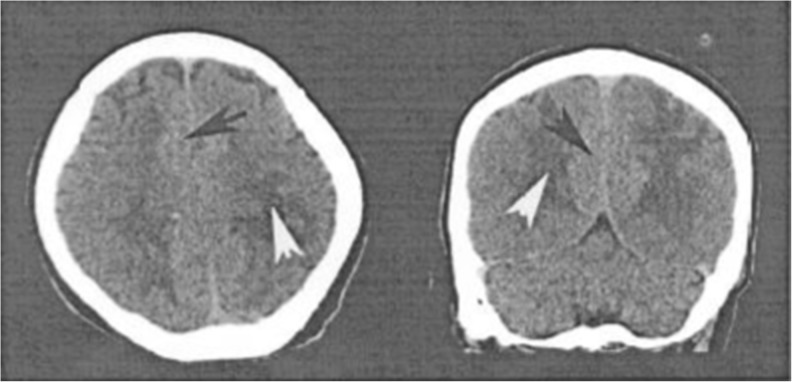
He was discharged home, but represented 1 month later with worsening weakness of his legs and haematuria. He had a soft abdomen and a normal genital examination. His PSA at this time had risen to 245 μg/l. A repeat MR of the spine again showed no evidence of cord compression. At this stage, computerised tomography (CT) of the brain was performed. This revealed an extensive enhancing mass extending bilaterally along almost the entire length of the falx cerebri, measuring up to 3 cm in width and associated with marked white matter oedema in the adjacent brain bilaterally (Fig. 1). This image is compared to a normal subject (Fig. 2). The findings were considered to be in keeping with a large parafalcine prostatic metastasis. The principal differential diagnosis on the basis of the imaging findings, a meningioma, was considered unlikely clinically. He deteriorated over the next 3 days and died. A post-mortem was not conducted.
Fig.1.
Axial (left) and coronal (right) CT images through the brain showing the irregular parafalcine mass (black arrows) along the falx cerebri with considerable mass effect and adjacent white matter oedema (white arrows)
Fig.2.
Images from a normal subject for comparison
Discussion
Intracranial metastatic disease from prostate cancer is rare, occurring in <1 % of patients. The most common site for metastatic deposit is leptomeningeal [1] with prostate metastases having been reported as mimicking a subdural or extradural haematoma [2, 3] or a meningioma [4]. Neurological symptoms at presentation are usually non-focal and include confusion, short-term memory loss and headache. These symptoms are related to intracranial hypertension. Less frequently, patients may present with hemiparesis, aphasia or seizures [5]. It is usually a terminal event with death usually following within 1 year due to advanced systemic disease [5]. This is the only case in the literature to present in this fashion, and the speed to which the patient deteriorated is most unfortunate.
This case highlights the need for CT or MR imaging of the brain to be performed in a patient presenting with suspected cord compression due to prostatic metastatic disease when MR of the spine shows no evidence of cord compression. Rare presentations do occur, particularly in the context of metastatic disease and cross-sectional imaging is advised in such cases to avoid missed or delayed diagnoses.
References
- 1.Sutton MA, Watkins HL, Green LK, Kadmon D. Intracranial metastasis as the first manifestation of prostate cancer. Urology. 1996;48:789–793. doi: 10.1016/S0090-4295(96)00238-5. [DOI] [PubMed] [Google Scholar]
- 2.Tomlin JM, Alleyne CH. Transdural metastasis from adenocarcinoma of the prostate mimicking subdural haematoma: case report. Surg Neurol. 2002;58:329–331. doi: 10.1016/S0090-3019(02)00835-2. [DOI] [PubMed] [Google Scholar]
- 3.Dorsi MJ, Zenonos G, Hsu W, Huang J. Dural prostate adenocarcinoma metastasis with subdural mimicking the appearance of an epidural haematoma. Clin Neurol Neurosurg. 2010;112:501–504. doi: 10.1016/j.clineuro.2010.02.009. [DOI] [PubMed] [Google Scholar]
- 4.Jain A, Ablett M, Wardrop P. Vanishing tumour of the internal auditory meatus. J Laryngol Otol. 2009;123:563–565. doi: 10.1017/S0022215108003447. [DOI] [PubMed] [Google Scholar]
- 5.Tremont-Lukats IW, Bobustuc G, Lagos GK, Lolas K, Kyritsis AP, Puduvalli VK. Brain metastasis from prostate carcinoma the M.D. Anderson Cancer Center experience. Cancer. 2003;92:363–368. doi: 10.1002/cncr.11522. [DOI] [PubMed] [Google Scholar]