Abstract
Objective
To date no research has evaluated the efficacy of a stand-alone, smartphone-based intervention for individuals with an alcohol use disorder. The current pilot study evaluated the short-term outcomes of a smartphone-based intervention for alcohol use disorders compared with an internet-based brief motivational intervention plus bibliotherapy.
Method
Adults (18 to 45 years old) with an alcohol use disorder received either the Location-Based Monitoring and Intervention for Alcohol Use Disorders (LBMI-A; n = 28), a smartphone-based intervention, or the online Drinker’s Check-up plus bibliotherapy (DCU+bib; n = 26). These groups were compared using the Timeline Followback interview for percent days abstinent (PDA), percent heavy drinking days (PHDD), and drinks per week (DPW) from baseline to six weeks after the introduction of the interventions.
Results
Multilevel models revealed that the LBMI-A resulted in a significant increase in PDA over the course of the study, while the DCU+bib did not. Effect sizes for change from baseline for PDA suggest that the DCU+bib resulted in moderate a decrease, while the LBMI-A resulted in a large increase in PDA. Both interventions resulted in significant decreases in PHDD and DPW. The LBMI-A produced larger reductions in the first three to four weeks after the intervention was introduced than the DCU+bib. On weeks with greater LBMI-A usage, participants reported less DPW and PHDD.
Conclusions
Both interventions resulted in significant decreases in alcohol use over the 6-week trial, which is promising for stand-alone technology-based intervention systems aimed at individuals with an alcohol use disorder.
Keywords: smartphone application, internet, technology-based intervention, alcohol use disorder, treatment
Alcohol use disorders are quite prevalent in the US. The National Epidemiological Survey on Alcohol and Related Conditions (NESARC) found that the lifetime prevalence for an alcohol use disorder was 30.3% and the 12 month prevalence was 8.5% (Hasin, Stinson, Ogburn, & Grant, 2007). Unfortunately, this survey also found that treatment utilization was quite low, with only 14.6% of those who have ever had an alcohol use disorder receiving treatment (Cohen, Feinn, Arias, & Kranzler, 2007). Among those with an alcohol use disorder, one of the most commonly cited reasons for not seeking treatment is the belief that he or she should be strong enough to handle their problem alone (Cohen et al., 2007; Grant, 1997). Other barriers for treatment include poor or inadequate availability of services; concerns about privacy, embarrassment, or dislike of answering personal questions; treatment expense or lack of insurance; and pragmatic issues, such as work-related complications and transportation problems (Cohen et al., 2007; Grant, 1997; Tucker, 1995). These treatment barriers suggest a need to develop alternatives to traditional interventions.
Technology-based alcohol interventions may help to bridge the gap between those in need of treatment and those receiving it by providing an alternative to face-to-face interventions. Public response shows that there is a demand for these interventions (Vernon, 2010) and prior research indicates that internet-based interventions are effective in reducing alcohol consumption among problem drinkers and younger populations at risk for developing alcohol use disorders (Cunningham, 2012; Cunningham, Wild, Cordingley, van Mierlo, & Humphreys, 2009; Hester, Delaney, & Campbell, 2011; Riper et al., 2011). However, these internet-based intervention studies have not targeted those with an alcohol use disorder, therefore their efficacy for more serious drinking problems is currently unknown.
Much of what leads to continued alcohol use or relapse occurs outside the context of treatment, including exposure to alcohol-related cues or contexts, as well as stress and negative affect (Becker, 2008; Carter & Tiffany, 1999; Sinha, 2012). Smartphone-based interventions are another alternative to traditional face-to-face treatment that could provide ecological momentary interventions (Burns et al., 2011; Heron & Smyth, 2010); interventions in the actual environment in which individuals are experiencing cravings, risk of relapse, or continued drinking. Although there are currently mobile applications available to help consumers address their problematic alcohol use, there is a lack of available evidence supporting their effectiveness (Cohn, Hunter-Reel, Hagman, & Mitchell, 2011; Weaver, Horyniak, Jenkinson, Dietze, & Lim, 2013).
In this paper, we present the results of a pilot study of a self-administered, stand-alone smartphone intervention system for individuals with an alcohol use disorder, the Location-Based Monitoring and Intervention for Alcohol Use Disorders (LBMI-A). In this six-week trial the LBMI-A was compared to an internet-based, brief motivational intervention with established support for reducing alcohol use among problem drinkers, the Drinker’s Check-up (DCU, Hester, Delaney, & Campbell, 2012; Hester, Squires, & Delaney, 2005), which was supplemented with bibliotherapy that provided strategies for reducing or eliminating drinking. The bibliotherapy component was added to the DCU as we anticipated that a brief motivational intervention would be insufficient for individuals with an alcohol use disorder as opposed to problem drinkers, who have typically been the target of internet-based interventions. We hypothesized that as an ecological momentary intervention the LBMI-A would result in greater reductions in drinking compared with the DCU supplemented by bibliotherapy.
Method
Participants and Procedures
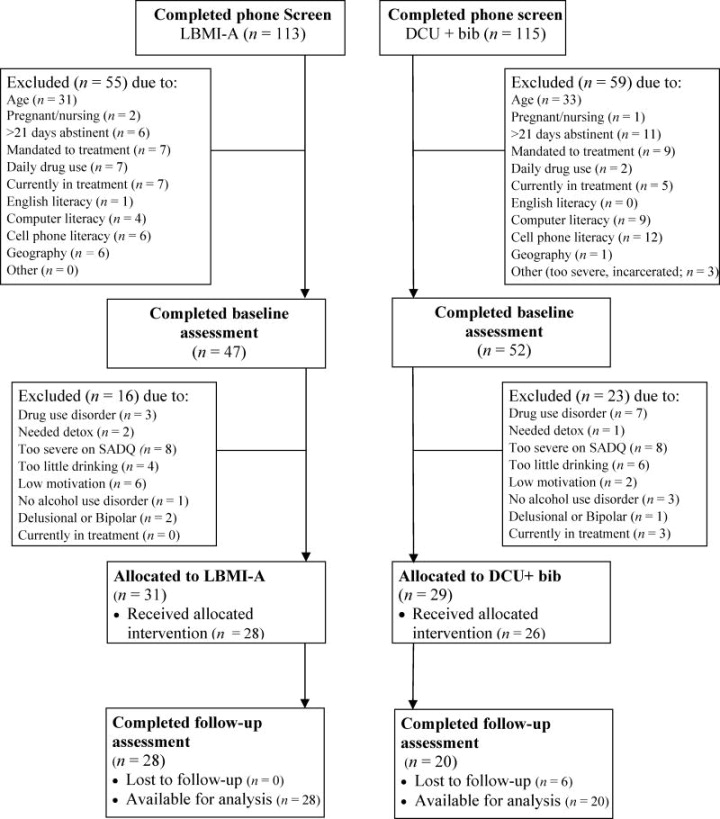
The study protocol was approved by the Institutional Review Board of the university. Participants were recruited from a Northwest community of approximately 300,000 individuals, using radio and newspaper advertisements, as well as flyers. Participants’ flow through the study is presented in Figure 1. In the study advertising we sought people experiencing “problems with alcohol” and advertised “a self-managed, technology-based intervention to help people change their drinking habits.” It was further noted that participants would not be asked to attend any face-to-face therapy sessions.
Figure 1.
Participant flow. Participant flow is presented for each group separately as the intervention groups were run sequentially. SADQ = Severity of Alcohol Dependence Questionnaire.
Participants were allocated to one of two interventions, but were not informed of the exact nature of the technology-based intervention until during the informed consent at the baseline assessment. The first 31 eligible participants were allocated to the LBMI-A intervention and the next 29 eligible were allocated to the DCU plus bibliotherapy intervention (DCU+bib). These interventions were run sequentially in this pilot study, as opposed to simultaneously with randomization, for pragmatic reasons (e.g., availability of the smartphone intervention for a limited time frame related to the expense of maintaining the system).
Interested individuals completed a brief phone screening that took approximately 5 minutes (N = 228). Individuals who met the screening criteria (N = 114), which corresponded to questions assessing study eligibility in brief (see Figure 1 for reasons for ineligibility), were scheduled for a baseline interview where full study eligibility was assessed. The baseline interview (N = 99) took 90–120 minutes.
To be included in the study participants had to meet Diagnostic and Statistical Manual of Mental Disorders 5th edition (DSM-5) diagnostic criteria for an alcohol use disorder (American Psychiatric Association, 2013) and be at least minimally motivated to change their drinking. Minimal motivation was defined as scoring above a mean of 3.0 on the contemplation, action, or maintenance subscales of the University of Rhode Island Change Assessment Scale (DiClemente & Hughes, 1990) and below a mean of 3.0 on the precontemplation subscale. This definition corresponds to participants not disagreeing that they have a problem with alcohol and at least a minimal interest in change. Selected participants also needed to be drinking a minimum of: (a) ≥14 standard drinks (females) or ≥21 standard drinks (males) on average per week over a consecutive 30 days in the 90 days prior to evaluation, and (b) ≥2 heavy drinking days (4 or more standard drinks—females, 5 or more—males) in the same 30 day period as above. Further eligibility criteria included being between the age of 18 to 45 years old and having a basic working knowledge of technology (i.e., could text and use email).
Exclusion criteria included being more than 21 days abstinent at the baseline interview; currently in alcohol or drug abuse treatment, except mutual self-help (e.g., Alcoholics Anonymous); pregnant or nursing; legally mandated to attend treatment; needing alcohol detoxification; severe alcohol dependence, as indicated by a score of 30 or above on the Severity of Alcohol Dependence Questionnaire (Stockwell, Murphy, & Hodgson, 1983); having delusions, hallucinations, or Bipolar I Disorder; or having another substance use disorder, with the exceptions of nicotine or marijuana. Individuals in early remission for another substance use disorder who had not used the given substance in the prior three months were not excluded.
Individuals who were eligible at the baseline interview (N = 60) were scheduled within a week in most cases for a one-hour appointment where they were introduced to their intervention. Participants were compensated $60 at each of the baseline and six-week follow-up assessments. LBMI-A participants also were compensated $5 for each day they completed a daily interview of alcohol consumption and cravings that was administered by the system.
Interventions
In the LBMI-A group, at the introduction to the intervention appointment, participants were provided with a customized LBMI-A enabled smartphone, that included a cellular and data plan. Participants completed the LBMI-A’s assessment and feedback module during this appointment, which allowed them to practice before taking the system to use independently. The LBMI-A system and its development have been described extensively elsewhere (Dulin, Gonzalez, King, Giroux, & Bacon, 2013; Dulin, Gonzalez, & Campbell, 2014). The overall intervention was based on existing cognitive and behavioral alcohol use disorder interventions that have empirical support for efficacy. The LBMI-A provided seven psychoeducation modules, or steps: (1) assessment and feedback, (2) high-risk locations for drinking, (3) selecting and using supportive people for change, (4) cravings and their management, (5) problem-solving skills, (6) communication and drink refusal skills, and (7) pleasurable, non-drinking activities. Following completion of a step an associated tool became available. These tools led users through immediate coping strategies during times of need (e.g., while experiencing a craving or negative mood), as well as monitoring alcohol consumption and cravings. Weekly feedback reports were provided through the LBMI-A system that allowed users to track their progress.
In the DCU+bib group participants were provided with a laptop computer during the introduction to the intervention appointment to independently complete the DCU online (www.drinkerscheckup.com). The DCU is an internet-based, brief motivation intervention that can be completed in less than one hour. It provides a comprehensive assessment of drinking and alcohol-related problems, objective and norms-based feedback, a decisional balance exercise to help resolve ambivalence about change, goal selection, brief development of a change plan, and brief interventions to facilitate change (e.g., developing alternatives to drinking), as well as links to other online interventions and resources (see Hester et al., 2005 and Hester et al., 2012 for a more extensive description of the DCU). The DCU and the assessment and feedback step of the LBMI-A were quite similar in regard to content; hence both groups received comparable interventions during the introduction to the intervention appointment. In addition to reviewing their results online, participants were given a printed copy of their DCU results and their DCU log-on information to allow them to revisit the site during the six-week follow-up period, if desired. Participants also were given a copy of a 16 page booklet, Rethinking Drinking: Alcohol and Your Health (National Institute on Alcohol Abuse and Alcoholism, 2010). This booklet has an accompanying webpage (http://rethinkingdrinking.niaaa.nih.gov) that has additional interactive worksheets and modules for handling urges, drink refusal, and recovering from a slip.
Measures
DSM-5 alcohol use disorder
For this study, the Structured Clinical Interview for DSM-IV (SCID; First, Spitzer, Gibbon, & Williams, 2002) was used to assess alcohol use disorder symptoms with the addition of a single item from the Composite International Diagnostic Interview Version 3.0 (Kessler & Üstün, 2004) that was used to assess cravings. Consistent with DSM-5 criteria, the SCID item related to legal problems was eliminated for diagnostic purposes.
Alcohol consumption
The Timeline Followback interview (TLFB; L. C. Sobell & Sobell, 1996) uses a calendar method to gather retrospective information on daily alcohol use. The 90 day version was administered at baseline and a 42 day version was administered at the post-intervention assessment. The TLFB was used to calculate the following drinking variables: percent of days abstinent (PDA), percent heavy drinking days (PHDD), and mean drinks per week (DPW) for the 42 days prior to the baseline interview and for each of the six weeks post-intervention. Heavy drinking days were defined as days with 4 or more standard drinks for women and 5 or more standard drinks for men.
Alcohol-related problems
The Short Inventory of Problems (SIP; Miller, Tonigan, & Longabaugh, 1995) is a 15-item version of the Drinkers’ Inventory of Consequences (DrInC; Miller et al., 1995). Participants rate their frequency of experiencing problems with alcohol from 0 (never/not at all) to 3 (almost daily/very much). At baseline, participants were asked to report problems they experienced in the past three months. In this study, the alpha coefficient was .85.
Motivation to change
The URICA alcohol version (DiClemente & Hughes, 1990) is a 32-item, self-report inventory that assesses motivation for change. There are four subscales: precontemplation, contemplation, action, and maintenance. Each subscale has 7 items included in the scoring (Willoughby & Edens, 1996) that are rated from 1 (strongly disagree) to 5 (strongly agree). The readiness to change score is obtained by subtracting the precontemplation score from the sum of the contemplation, action, and maintenance scores (Field, Adinoff, Harris, Ball, & Carroll, 2009). In this study, subscale alpha coefficients ranged from .80 to .87.
Severity of alcohol dependence
The SADQ (Stockwell et al., 1983) is a 20-item self-report measure of alcohol dependence severity. Items are rated from 0 (almost never) to 3 (nearly always). Scores over 30 have been shown to correlate with clinicians’ ratings of severe dependence (Stockwell, Hodgson, Edwards, Taylor, & Rankin, 1979). In this study, the alpha coefficient was .92.
Analyses
Mixed linear modelling, using SPSS 21, was used to examine the within subjects effects of time (level one) on three drinking outcome variables: PDA, PHDD, and DPW over the course of the six-week study with individuals in the LBMI-A (n = 28) and DCU+bib (n = 20) groups who completed the six-week follow-up assessment. Drinking during the six weeks prior to the study was used as a baseline measure (time 0), followed by drinking at each one-week time point after the interventions were introduced (times 1–6). First, level one models examining growth and its shape (i.e., linear, quadratic, or cubic) were developed. After growth models for each drinking variable were developed, intervention group was added at level two of each model, as well as cross-level interactions for group by time – in order to examine whether the LBMI-A (coded as 1) and DCU+bib (coded as 0) groups differed in their rate of change on the drinking variables. Race/ethnicity and total DSM-5 alcohol use disorder criteria met (grand mean centered) were included as covariates in these models given some imbalance in the groups on these baseline variables (see results). For DPW, gender (men coded as 0, women coded as 1) was additionally included in this model. Although the intervention groups were fairly balanced in regard to gender, given that National Institute on Alcohol Abuse and Alcoholism (NIAAA) recommendations for low-risk drinking in regard to DPW are gender specific (NIAAA, 2010), including gender allowed us to examine the pattern of change over time relative to these guidelines for women (≤ 7 drinks per week) and men (≤ 14 drinks per week).
We also examined models where race/ethnicity and severity of participants’ alcohol use disorder were added at level two to growth models for each drinking variable, as well as the interactions of race/ethnicity and severity of dependence with time as fixed effects. For these analyses, number of DSM-5 criteria met were used as an indicator of the severity of the participant’s alcohol use disorder (Dawson, Saha, & Grant, 2010). These analyses explored whether severity effected change over time and whether there was any difference in outcomes between White and racial or ethnic minority participants.
In order to examine the effect of LBMI-A system usage on change in drinking we examined the effect of system usage, both within and between subjects, in separate analyses for PDA, PHDD, and DPW. System usage during each week of the trial was included as a level one time-varying covariate to growth models, with system usage at baseline coded as 0 given that it preceded introduction of the intervention. System usage was recorded as occurring each time a participant launched a step (i.e., psychoeducational information) or tool (e.g., brief intervention to reduce negative affect, resist or decrease a craving, add a support person). One step (productive communication) failed to record usage and therefore could not be included in usage totals. Daily system usage was summed for each week to examine whether there was a within subjects effect for system usage. To isolate this within subjects effect, and to avoid a confound with any between subjects effect of system usage, we included total system usage (grand mean centered) over the course of the six-week trial. To examine whether individuals who used the system more had greater decreases in their drinking over time compared to those who used the system less, an interaction term for total usage over the study by (linear) time was included.
One participant in each intervention group entered formal treatment for their alcohol use disorder during the six-week trial. The time points following their enrollment in another treatment were eliminated from the analyses. All mixed linear models were estimated using restricted maximum likelihood (REML) given the small sample size (Singer & Willett, 2003). Intercept and (linear) time were included as random in all models. The models’ covariance structure for level one was factor analytic (first order) and for level two was unstructured. Models were examined for outliers on levels one and two, as well as other model assumptions (e.g., normality). For each of the DPW and PHDD variables, there were three participants who each had one outlying time point at level one relative to their other time points (defined as z scores over 3.5 for the model residuals). To reduce the influence of outliers without eliminating valid data points (Tabachnick & Fidell, 2007), these scores were changed so that they remained high or low but were no longer outlying. The results of the analyses and patterns of significance were not substantively changed, suggesting that these data points were not highly influential.
Results
Baseline Differences with Respect to Attrition
Individuals who were allocated to an intervention, but dropped out prior to receiving it (N = 6) were somewhat younger (Mage = 29.0 years, SD = 7.54) than those who received an intervention (Mage = 34.6 years, SD = 6.81; F[1,58] = 3.53, p = .065, η2 = .06) and reported somewhat lower readiness to change (M = 8.98, SD = 1.11) than those who received an intervention (M = 10.19, SD = 1.64; F[1,58] = 3.08, p = .085, η2 = .05). Pre-intervention dropouts also had a much higher PDA (M = 62.70, SD = 21.23) than those who received an intervention (M = 32.67, SD = 25.85; F[1,58] = 7.49, p = .008, η2 = .11). Individuals who completed an intervention but dropped out prior to the follow-up interview (N = 6; all in the DCU+bib group) were significantly older (Mage = 40.0 years, SD = 8.46) than those who completed the follow-up interview (Mage = 33.9 years, SD = 6.35; F[1,52] = 4.61, p = .036, η2 = .08). No other differences in baseline variables were found.
Baseline Equivalence
Groups were largely comparable (see Table 1); however, the LBMI-A group met significantly more DSM-5 alcohol use disorder symptom criteria. Based on the chi-square analysis, there was a trend for the LBMI-A group to have a greater proportion of minority participants than the DCU+bib group (contingency coefficient = .24, p = .08); 50% of the LBMI-A group were ethnic minorities compared with 25% in the DCU+bib group.
Table 1.
Comparison of Intervention Groups on Demographic and Baseline Alcohol-Related Variables
| LBMI-A (n = 28) | DCU + bib (n = 20) | Test | |
|---|---|---|---|
| Age - mean (SD) | 33.57 (6.54) | 34.30 (6.22) | t(46) = −.39 |
| Gender - % (n) | χ2(1) = .43 | ||
| Male | 53.6 (15) | 65.0 (13) | |
| Female | 46.4 (13) | 35.0 (7) | |
| Race/ethnicity - % (n) | χ2(1) = 3.05† | ||
| White | 50.0 (14) | 75.0 (15) | |
| Minority | 50.0 (14) | 25.0 (5) | |
| Alaska Native/American Indian | 25.0 (7) | 5.0 (1) | |
| African American | 7.1 (2) | 10.0 (2) | |
| Hispanic | 5.0 (1) | 5.0 (1) | |
| Native Hawaiian or other Pacific Islander | 3.4 (1) | 5.0 (1) | |
| Multiethnic | 10.7 (3) | 0 | |
| Marital status - % (n) | χ2(2) = .17 | ||
| Never married | 35.7 (10) | 35.0 (7) | |
| Married/live as married | 39.3 (11) | 35.0 (7) | |
| Divorced/separated/widowed | 25.0 (7) | 30.0 (6) | |
| Education (highest completed) - % (n) | FET = 1.79 | ||
| 10th or 11th grade | 0 (0) | 5.0 (1) | |
| High school or GED | 57.1 (16) | 45.0 (9) | |
| College degree | 42.9 (12) | 50.0 (10) | |
| Employment status - % (n) | χ2(2) = 1.09 | ||
| Employed | 78.6 (22) | 65.0 (13) | |
| Unemployed | 21.4 (6) | 35.0 (7) | |
| Severity of dependence - mean (SD) | 13.82 (6.51) | 16.50 (6.52) | t(46) = −1.40 |
| Alcohol problems - mean (SD) | 19.61 (7.88) | 17.95 (5.94) | t(46) = .79 |
| Readiness to change - mean (SD) | 9.85 (1.47) | 10.49 (1.65) | t(46) = −1.40 |
| DSM-5 alcohol use disorder criteria - mean (SD) | 7.07 (2.02) | 5.60 (1.93) | t(46) = 2.54* |
Note. FET = Fisher’s exact test.
p < .10.
p < .05.
Exposure to the Intervention
All participants in the DCU+bib group completed the DCU as it was administrated during the introduction to the intervention appointment. The majority of participants (90%) reported that they read at least one page of Rethinking Drinking and 50% read the entire booklet. Mean pages read was 8.0 (SD = 5.49) of the 13 pages of text. The booklet contained seven worksheets, 65% of the sample did at least two of these and 10% reported completing them all. The majority of DCU+bib group (85%) reported going to the Rethinking Drinking website; however, none reported completing the skills modules for resisting urges to drink or drink refusal. A quarter of the sample reported visiting additional resource websites presented on the DCU (e.g., www.moderatedrinking.org).
All participants in the LBMI-A group completed the assessment and feedback step as it was administrated during the introduction to the intervention appointment. Step usage was recorded by the LBMI-A system for all steps except productive communication, which failed to record due to a software glitch. For this step, we used data gathered during a post-intervention satisfaction survey where participants reported whether they had completed a given step. The majority of the LBMI-A group (71.4%) launched all of the LBMI-A system steps at least one time, 21.4% did six of the seven steps, and 7.1% did five steps. Unfortunately, it is not known whether a step was completed in its entirety. There were eight LBMI-A tools available within the smartphone system. The majority of participants (67.9%) used all available tools at least once, 21.4% used seven of the eight tools, and 10.7% used between 4 and 6 tools.
The majority of participants completed their step use within the first week of the study. Very few participants reviewed the psychoeducational steps (or completed them for the first time) after week 2. Mean frequency of step usage was 9.64 in week 1, 2.6 in week 2, and between .21 and .07 in subsequent weeks. Tool usage was high in week 1 (M = 27.43), declining until week 4, where usage plateaued at between 6.42 and 5.46 uses per week and was primarily restricted to completing the daily interview (on alcohol consumption and cravings) or recording drinking with the drink monitoring tool.
Drinking Outcomes
Percent days abstinent
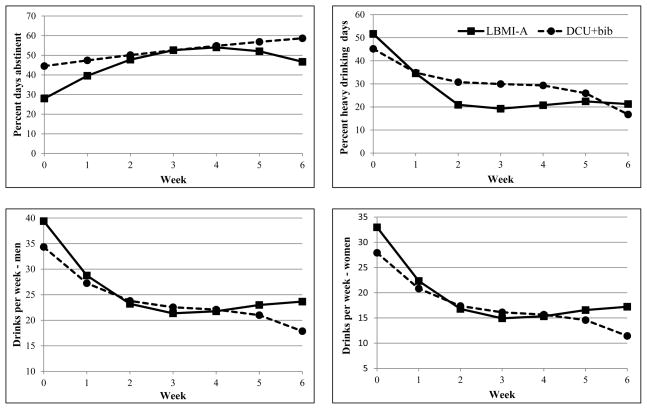
The unconditional model examining longitudinal trajectories revealed significant fixed effects for linear and quadratic growth trajectories for PDA. There was a significant effect for linear time, with PDA significantly increasing over the course of the study (B [SE] = 9.36 [1.92], p < .001). The significant quadratic effect shows that this increase in PDA diminished over time (B [SE] = −1.09 [.30], p < .001). Adding level two predictors (see Table 2), revealed that the intervention groups differed significantly at baseline, with the LBMI-A group having fewer PDAs. These groups also differed significantly in change over the course of the study, with significant linear and quadratic time by group interactions. A probe of the linear and quadratic time by group interactions revealed that only the LBMI-A group experienced an increase in PDA (B [SE] = 13.30 [2.57], p < .001) over the course of the study, with a decrease in this rate of change over time (B [SE] = −1.70 [.40], p < .001). The model implied trajectories are graphically depicted in Figure 2. The DCU+bib group did not experience significant change based on the results of the multilevel analysis, with non-significant linear (B [SE] = 3.02 [3.04], p = .324) and quadtratic effects (B [SE] = −.11, [.47], p = .818). However, simple effect sizes (Cohen’s d) for within group change from baseline PDA showed medium effect sizes from weeks 1 to 5, and a medium-large effect size for week 6 for the DCU+bib group (see Table 3). The LBMI-A group demonstrated large effect sizes for change from baseline for weeks 2 to 6.
Table 2.
Final Multilevel Model Results for Drinking Outcomes
| Drinks per week
|
Percent days abstinent
|
Percent heavy drinking days
|
||||
|---|---|---|---|---|---|---|
| Estimate | Std. Error | Estimate | Std. Error | Estimate | Std. Error | |
| Intercept | 31.14*** | 4.23 | 44.53*** | 5.34 | 45.20*** | 6.36 |
| Linear time | −9.51** | 3.10 | 3.02 | 3.04 | −14.49** | 5.24 |
| Quadratic time | 2.62* | 1.13 | −.11 | .47 | 4.64* | 1.81 |
| Cubic time | −.25* | .12 | −.50** | .18 | ||
| Group | 4.98 | 5.55 | −16.55* | 7.22 | 6.48 | 8.32 |
| Group by linear time | −4.28* | 2.14 | 10.29* | 3.98 | −8.25* | 3.85 |
| Group by quadratic time | .74* | .32 | −1.59* | .62 | 1.48* | .59 |
Note. Group was coded: DCU+bib = 0, LBMI-A = 1. Race/ethnicity and number of DSM-5 alcohol use disorder criteria met were included as mean centered covariates in each model. Gender was included in the drinks per week analysis, coded men = 0, women = 1.
p < .05.
p < .01.
p < .001.
Figure 2.
Model implied trajectories for percent days abstinent, percent heavy drinking days, and drinks per week for men and women. Baseline drinking levels are represented by week 0.
Table 3.
Effect Size (Cohen’s d) for Change from Baseline by Week
| Time | LBMI-A
|
DCU+bib
|
||||
|---|---|---|---|---|---|---|
| PDA | PHDD | DPW | PDA | PHDD | DPW | |
| Week 1 | .60 | .83 | .75 | .61 | .57 | .64 |
| Week 2 | .85 | .85 | .84 | .56 | .65 | .64 |
| Week 3 | 1.15 | 1.01 | .90 | .54 | .69 | .73 |
| Week 4 | 1.26 | 1.09 | 1.04 | .42 | .57 | .60 |
| Week 5 | 1.03 | .89 | .92 | .63 | .77 | .84 |
| Week 6 | .93 | .94 | .84 | .76 | 1.10 | .98 |
Note. PDA = percent days abstinent, DPW = drinks per week, PHDD = percent heavy drinking days.
Percent heavy drinking days (PHDD)
The unconditional model examining longitudinal trajectories revealed significant fixed effects for linear, quadratic, and cubic growth for PHDD. Over the course of the study PHDD significantly decreased (B [SE] = −19.45 [4.72], p < .001). The significant quadratic effect shows that this decrease in PHDD became less pronounced over time (B [SE] = 5.59 [1.75], p = .002). The significant cubic component shows that this diminished rate of change itself slowed over time (B [SE] = −.52 [.18], p = .006). Adding level two predictors, the intervention groups did not differ significantly at baseline in PHDD. However, there were significant linear and quadratic time by group interactions. The cubic time by group interaction was non-significant and not retained in the final model. A probe of the linear time by group interaction revealed that in the LBMI-A group, time was associated with a greater decrease in PHDD (B [SE] = −22.74 [4.99], p < .001) than for the DCU + bib group (B [SE] = −14.49 [5.23], p = .007). A probe of the quadratic time by group interaction suggests that there was a greater diminishment of change in PHDD in the LBMI-A group (B [SE] = 6.12 [1.80], p = .001) compared with the DCU+bib group (B [SE] = 4.64 [1.81], p = .013; see Figure 2).
Cohen’s d for within group change from baseline PHDD for each week (see Table 3) showed medium effect sizes from weeks 1 to 4, and large effect sizes for weeks 5 and 6 for the DCU+bib group. The LBMI-A group demonstrated large effect sizes at each time point.
Drinks per week
The unconditional model examining longitudinal trajectories revealed significant fixed effects for linear, quadratric, and cubic growth trajectories for DPW. There was a significant reduction in DPW over the course of the study (B [SE] = −11.93 [2.73], p < .001). The significant quadratic effect shows that this reduction in drinking diminished over time (B [SE] = 2.97 [1.13], p = .010). The significant cubic component shows that this diminished rate of change itself slowed over time (B [SE] = −.24 [.12], p = .049). Adding level two predictors, the intervention groups did not differ significantly at baseline in DPW (see Table 2). However, there were significant linear and quadratic time by group interactions. The cubic time by group interaction was non-significant and not retained in the final model. A probe of the linear time by group interaction revealed that for both groups, time was associated with fewer DPW, with the LBMI-A group showing greater reductions in DPW (B [SE] = −13.79 [2.97], p < .001) than the DCU+bib group (B [SE] = −9.51 [3.10], p = .003). A probe of the quadratic time by group interaction suggests that there also was a greater diminishment of change in DPW in the LBMI-A group (B [SE] = 3.36 [1.12], p = .004) compared with the DCU+bib group (B [SE] = 2.62 [1.13], p = .022). Thus it appears the LBMI-A group had a more rapid decrease in DPW and also a more rapid deceleration in their change relative to the DCU+bib group.
Cohen’s d for within group change from baseline DPW shows medium effect sizes for change from baseline for weeks 1 through 4, and a large effect size for weeks 5 and 6 for the DCU+bib group. The LBMI-A group demonstrated a medium effect sizes at week 1 followed by large effect sizes at each subsequent time point.
No significant gender by time interactions were found, suggesting women and men did not differ significantly in their rate of change. Men (coded as 0) and women (coded as 1) also did not differ significantly at baseline (B [SE] = −6.37 [4.50], p = .165). For the pragmatic value of examining participants’ drinking relative to NIAAA drinking guidelines, this information was used to graphically depict the model implied trajectories for men and women (see Figure 2).
Effect of severity and race
Race/ethnicity and severity of dependence, as indicated by number of DSM-5 criteria met, and the interaction of these variables with time were included at level two to growth models for DPW, PHDD, and PDA. Neither race/ethnicity nor severity of dependence interacted significantly with time, with all p values exceeding .10, suggesting that the change over time in this sample was not effected by either severity or race/ethnicity.
Effect of LBMI-A system usage on drinking
For DPW, when the LBMI-A group was analyzed separately from the DCU+bib group to develop growth trajectories, linear and quadratic time components were significant, while the cubic was not. Adding LBMI-A usage variables to this growth model, while controlling for the (grand mean centered) effects of race/ethnicity, gender, and number of DSM-5 alcohol use disorder criteria met, there was a significant within subjects effect with a greater reduction in drinking during weeks when individuals used the system more often (B [SE] = −.17 [.08], p = .037). There was a significant between subjects effect for system usage at baseline, suggesting that individuals who drank more at baseline also used the system more overall (B [SE] = .18 [.07], p = .023). There were no significant interaction between time and overall LBMI-A usage (B [SE] = −.01 [.01], p = .424). This suggests that participants who used the system more did not differ from individuals who used the system less in regard to reductions in drinks per week over the course of the study. After controlling for within and between subjects effects for LBMI-A usage, linear (B [SE] = −8.68 [1.36], p < .001) and quadratic time (B [SE] = 1.03 [.21], p < .001) were still significantly associated with DPW, suggesting that reductions in DPW over the course of the study was not entirely accounted for by amount of system usage.
For PHDD, linear and quadratic time components were significant in the growth model, while the cubic was not. There was a significant within subjects effect (B [SE] = − .31 [.12], p = .017), with individuals experiencing a greater reduction in PHDD during weeks they used the system more. There also was a significant between subjects effect for system usage (B [SE] = .31 [.10], p = .005). Individuals who had greater PHDD at baseline used the LBMI-A system more. A significant time by overall LBMI-A usage interaction was found, B (SE) = −.04 (.02), p = .040, and was probed at one standard deviation above and below the mean for overall system usage (Preacher, Curran, & Bauer, 2006). This analysis revealed that individuals who used the system more had greater reductions in PHDD over the course of the study (B [SE] = −14.14 [2.30], p < .001) compared with individuals who used the system less (B [SE] = −11.26 [2.30], p < .001), although LBMI-A system usage was associated with significant change in PHDD over time for both. Linear time (B [SE] = −12.70 [2.20], p < .001) was still significantly associated with PHDD after including LBMI-A usage, suggesting that change in PHDD was not entirely accounted for by the frequency of system usage.
For PDA, linear and quadratic growth terms were significant. No significant within subjects effect was found for LBMI-A usage (B [SE] = .13 [.12], p = .300) and no significant time by overall LBMI-A usage effect was found (B [SE] = .001 [.03], p = .965). Thus it would appear that while the LBMI-A group had a significant increase in PDA, it did not covary with the amount that participants used the system.
Discussion
This is the first study to our knowledge that has examined a self-administered, standalone technology-based intervention with a sample of participants who met criteria for an alcohol use disorder. Prior studies in this vein utilized problem drinkers. The results suggest that both interventions helped participants to significantly reduce their drinking levels. The results of this study also suggest differences in the outcomes between the interventions. The LBMI-A produced a significant increase in PDA over the course of this six-week study, while the DCU+bib intervention did not according to the multivariate analyses. However, given the small sample size in this pilot study, it is important to also consider effect sizes. An examination of simple effect sizes for change from baseline suggests that the DCU+bib resulted in a moderate PDA increase post-intervention, while the LBMI-A resulted in a large increase in PDA.
Both interventions resulted in significant decreases in the amount of alcohol consumed each week and in the number of heavy drinking days, with the LBMI-A producing larger reductions in the first weeks after the intervention was introduced. However, the reduction in frequency of heavy drinking and amount of alcohol consumed per week appears to have plateaued at week three, particularly for the LBMI-A. Despite this rapid plateau in change, effect sizes suggest large reductions in DPW and PHDD compared with baseline, particularly for the LBMI-A group.
Most internet-based alcohol interventions have been undertaken with at-risk and problem drinkers, who likely did not have the same level of severity as participants in this study. These studies also had longer follow-up assessments than that utilized in the current study, making it difficult to draw direct comparisons. However, the large effect sizes found in this study are consistent with three month outcomes for a comparable abstinence-based web-application for problem drinkers (Hester, Lenberg, Campbell, & Delaney, 2013). Given that participants’ outcomes in this pilot study were only examined for six weeks it is unknown whether the changes found will be maintained and long-term follow-up studies are needed.
Unlike traditional, weekly outpatient treatment for alcohol use disorders, LBMI-A users had complete control over how quickly they progressed through the intervention, as well as when and how much they would use it as a tool to facilitate their change. We found that during weeks with greater LBMI-A usage participants experienced a greater reduction in DPW and PHDD. One theorized benefit of this smartphone intervention was that it could be used as a tool to reduce drinking when and where it actually occurs, outside of a treatment setting. The finding that participants reduced their drinking more during weeks when they used the system more may indicate that it served this purpose. Several other explanations exist for the effects found, one of which is that greater motivation to change spurred both greater system use and the observed reductions in drinking in the first few weeks after being introduced to the intervention. However, it is noteworthy that change in the LBMI-A group was steeper in the first weeks after the intervention was introduced compared with the DCU+bib group. This may suggest that the change associated with the LBMI-A use was not solely due to motivation associated with seeking out help to change one’s drinking. Regardless of the precise mechanism of action, LBMI-A system use appears to have been beneficial.
Greater LBMI-A system use also was found to be associated with between subjects differences, suggesting that overall greater utilization of the intervention produced greater improvements over the course of the study. Individuals who were higher in DPW and those higher in PHDD at baseline were found to have used the system more over the course of the study. This may indicate that those who needed the system more, namely those who drank more at the outset of the intervention, used the system more to reduce their drinking. This greater system use appears to have been to good effect, as those who used the system more did better in regard to reducing their PHDD over the course of the study compared with those who used the system less. In contrast, there was no apparent dose effect for system use either between or within subjects for PDA; however, LBMI-A participants were found to have increased their PDA to a greater extent than DCU+bib participants. This may suggest that there was an overall effect for the intervention, but that there was not a greater benefit associated with greater use in producing more days abstinent.
Participants greatly reduced their use of the LBMI-A system after two to three weeks. This could in part be attributable to their reduction in drinking, such that there was less need to use the LBMI-A’s tools to help them manage their behavior or cravings after week 3. However, on average, participants at the end of the trial were still drinking heavily one to two times per week as well as were exceeding NIAAA guidelines for low-risk drinking and hence would have benefitted from further reductions in their drinking.
One potential factor that may have limited continued use of the LBMI-A system was that it was largely passive. Few prompts were given to remind or encourage system users to keep interacting with the system and its tools after the psychoeducational steps were introduced. In a previous study, LBMI-A users indicated that more system prompts would have been a positive addition to the intervention (Giroux, Bacon, King, Dulin, & Gonzalez, in press). The results of this study suggest that outcomes may be improved when using a self-administered intervention such as the LBMI-A by keeping users actively engaged for a longer period of time. One way to keep a system user interacting and potentially making continued improvements for a longer period of time would be greater prompting. Such prompting could be built into the intervention itself, or the system could be supplemented by contact with a treatment provider (e.g., through traditional face-to-face meetings or via phone, email, or text). Another important strategy for encouraging engagement and use is to provide the intervention as a downloadable app on users’ personal smartphone, which would increase the likelihood that it would be carried with them in most circumstances. In this pilot study participants were provided with an LBMI-A enabled phone for use during the six-week trial, this proved to be a substantial barrier to system usage. Many participants noted that they frequently left the study phone at home as they did not want to lose it or have the burden of carrying their personal phone and the study phone (Dulin et al., 2014; Giroux et al., in press). Further research is needed to examine how to get maximal gains from technology-based interventions such as the LBMI-A and what should be the proscribed length of time for users to actively use the system, as well as to examine the long-term outcomes of using a smartphone-based intervention for alcohol use disorders.
Based on the number of DSM-5 criteria met for an alcohol use disorder by participants in this sample, 75% had a severe alcohol use disorder (i.e., met 6 or more criteria; American Psychiatric Association, 2013). However, it is important to note that participants who were severely dependent based on the SADQ, which primarily measures physical dependence, were excluded from this trial. Therefore, the results cannot be generalized to the full range of dependence. In this study sample, severity based on DSM-5 symptoms was not significantly associated with change over time, suggesting that these interventions are not only for those with mild problems with alcohol. Future studies should include a fuller range of alcohol use disorder severities in order to evaluate whether self-administered, technology-based interventions are helpful for individuals with a more severe alcohol use disorder that includes physical dependency.
In this study, groups were not treated the same in regard to monitoring of drinking during the study based on nature of the interventions they received. In the LBMI-A group, as part of their intervention participants were instructed to record their drinking and cravings in vivo, as well as prompted by the system each day to complete an interview that asked about their drinking and cravings the previous day to make corrections or additions to their in vivo self-monitoring. Additionally, participants were compensated for completing these assessments. In this sense, the LBMI-A participants’ drinking was monitored throughout the study. This information was used by the system to provide feedback regarding changes to their drinking through weekly feedback reports, likely further increasing their sense of being monitored. The DCU+bib group was not monitored after being introduced to the intervention with the exception of a mid-study (week 3) safety call by project staff to all participants to ensure there were not adverse outcomes in this otherwise unmonitored intervention with alcohol use disordered individuals (none occurred). The methods used in this study introduced the potential for differences between the groups in regard to reactivity of assessment, which has been found in numerous alcohol studies (see Schrimsher & Filtz, 2011). At week 5 participants were called by study staff to remind them of their upcoming follow-up assessment appointment. For the DCU+bib group, being reminded that they would again be assessed in regard to their drinking may have prompted participants in this group to change their drinking in anticipation of the assessment. An examination of the multilevel model implied trajectories, as well as the effect sizes for the DCU+bib group, shows a sudden decrease in drinking between weeks 5 and 6 that is not evident in the LBMI-A group, who may have been less reactive to being reminded of an upcoming assessment of their drinking at the follow-up interview given their ongoing assessment during the study.
Additional limitations included a relatively small sample size; differential dropout, as all post-intervention dropouts occurred in the DCU+bib group; and interventions that were not run simultaneously with random assignment. Participants also were compensated differentially based on group, with the LBMI-A group offered an incentive to record their daily drinking and cravings. A more methodologically rigorous, randomized controlled trial with long-term follow-up is needed to further evaluate the efficacy of the LBMI-A.
The results of this study suggest the promise for technology-based interventions to meet the needs of the many individuals with an alcohol use disorder who do not want to or cannot attend formal treatment. Although such interventions may not be adequate for all, the cost-effectiveness and accessibility of these approaches warrant consideration of a stepped care approach, where more intensive face-to-face interventions are recommended to those unable to adequately change their drinking through self-directed methods (M. B. Sobell & Sobell, 2000).
Public health significance.
Technology-based interventions for individuals with alcohol use disorders hold the potential to help bridge the wide gap between those needing treatment and those actually receiving it. This study found that both an internet-based intervention supplemented with an information pamphlet and a smartphone-based intervention resulted in decreased alcohol use over the 6-week trial.
Acknowledgments
Funding for this work was provided by National Institute on Alcohol Abuse and Alcoholism Grant RC2AA019422, awarded to Patrick L. Dulin and Vivian M. Gonzalez. Dr. Dulin is the primary owner of a company that produced Step Away, an iPhone app for self-managed change that was partly informed by results from this study and other research pertaining to LBMI-A features that users reported to be most and least helpful.
Special thanks to R. Lorraine Collins, Gerard J. Connors, Stephen A. Maisto, and Paul Stasiewicz for their assistance in the development of the LBMI-A system.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- Becker HC. Alcohol dependence, withdrawal, and relapse. Alcohol Research & Health. 2008;31:348–361. [PMC free article] [PubMed] [Google Scholar]
- Burns MN, Begale M, Duffecy J, Gergle D, Karr CJ, Giangrande E, Mohr DC. Harnessing context sensing to develop a mobile intervention for depression. Journal of Medical Internet Research. 2011;13:158–174. doi: 10.2196/jmir.1838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter BL, Tiffany ST. Meta-analysis of cue-reactivity in addiction research. Addiction. 1999;94:327–340. doi: 10.1046/j.1360-0443.1999.9433273.x. [DOI] [PubMed] [Google Scholar]
- Cohen E, Feinn R, Arias A, Kranzler HR. Alcohol treatment utilization: Findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug and Alcohol Dependence. 2007;86:214–221. doi: 10.1016/j.drugalcdep.2006.06.008. [DOI] [PubMed] [Google Scholar]
- Cohn AM, Hunter-Reel D, Hagman BT, Mitchell J. Promoting behavior change from alcohol use through mobile technology: The future of ecological momentary assessment. Alcoholism: Clinical and Experimental Research. 2011;35:2209–2215. doi: 10.1111/j.1530-0277.2011.01571.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham JA. Comparison of two internet-based interventions for problem drinkers: Randomized controlled trial. Journal of Medical Internet Research. 2012;14:24–30. doi: 10.2196/jmir.2090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham JA, Wild TC, Cordingley J, van Mierlo T, Humphreys K. A randomized controlled trial of an internet-based intervention for alcohol abusers. Addiction. 2009;104:2023–2032. doi: 10.1111/j.1360-0443.2009.02726.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson DA, Saha TD, Grant BF. A multidimensional assessment of the validity and utility of alcohol use disorder severity as determined by item response theory models. Drug and Alcohol Dependence. 2010;107:31–38. doi: 10.1016/j.drugalcdep.2009.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiClemente CC, Hughes SO. Stages of change profile in alcoholism treatment. Journal of Substance Abuse. 1990;2:217–235. doi: 10.1016/s0899-3289(05)80057-4. [DOI] [PubMed] [Google Scholar]
- Dulin PL, Gonzalez VM, Campbell K. Results of a pilot test of a self-administered smartphone-based treatment system for alcohol use disorders: Usability and early outcomes. Substance Abuse. 2014;35:168–175. doi: 10.1080/08897077.2013.821437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dulin PL, Gonzalez VM, King DK, Giroux D, Bacon S. Development of a smartphone-based, self-administered intervention system for alcohol use disorders. Alcoholism Treatment Quarterly. 2013;31:321–336. doi: 10.1080/07347324.2013.800425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field CA, Adinoff B, Harris TR, Ball SA, Carroll KM. Construct, concurrent and predictive validity of the URICA: Data from two multi-site clinical trials. Drug and Alcohol Dependence. 2009;101:115–123. doi: 10.1016/j.drugalcdep.2008.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, research version, non-patient edition. (SCID-I/NP) New York: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- Giroux D, Bacon S, King D, Dulin PL, Gonzalez VM. Examining perceptions of a smartphone-based system for alcohol use disorders. Telemedicine and e-Health. doi: 10.1089/tmj.2013.0222. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF. Barriers to alcoholism treatment: Reasons for not seeking treatment in a general population sample. Journal of Studies on Alcohol. 1997;58:365–371. doi: 10.15288/jsa.1997.58.365. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2007;64:830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- Heron KE, Smyth JM. Ecological momentary interventions: Incorporating mobile technology into psychosocial and health behaviour treatments. British Journal of Health Psychology. 2010;15:1–39. doi: 10.1348/135910709X466063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hester RK, Delaney HD, Campbell W. ModerateDrinking.com and moderation management: Outcomes of a randomized clinical trial with non-dependent problem drinkers. Journal of Consulting and Clinical Psychology. 2011;79:215–224. doi: 10.1037/a0022487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hester RK, Delaney HD, Campbell W. The College Drinker’s Check-up: Outcomes of two randomized clinical trials of a computer-delivered intervention. Psychology of Addictive Behaviors. 2012;26:1–12. doi: 10.1037/a0024753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hester RK, Lenberg KL, Campbell W, Delaney HD. Overcoming addictions, a web-based application, and SMART recovery, an online and in-person mutual help group for problem drinkers, part 1: Three-month outcomes of a randomized controlled trial. Journal of Medical Internet Research. 2013;15:11–25. doi: 10.2196/jmir.2565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hester RK, Squires DD, Delaney HD. The Drinker’s Check-up: 12-month outcomes of a controlled clinical trial of a stand-alone software program for problem drinkers. Journal of Substance Abuse Treatment. 2005;28:159–169. doi: 10.1016/j.jsat.2004.12.002. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Üstün TB. The World Mental Health (WMH) survey initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) International Journal of Methods in Psychiatric Research. 2004;13:93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Tonigan JS, Longabaugh R. The Drinker Inventory of Consequences (DrInC): An instrument for assessing adverse consequences of alcohol abuse. Rockville, MD: Department of Health and Human Services; 1995. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. Rethinking drinking: Alcohol and your health (NIH publication no. 10-3770) Washington, DC: Government Printing Office; 2010. Available at http://rethinkingdrinking.niaaa.nih.gov/ [Google Scholar]
- Preacher KJ, Curran PJ, Bauer DJ. Computational tools for probing interactions in multiple linear regression, multilevel modeling, and latent curve analysis. Journal of Educational and Behavioral Statistics. 2006;31:437–448. [Google Scholar]
- Riper H, Spek V, Boon B, Conijn B, Kramer J, Martin-Abello K, Smit F. Effectiveness of E-self-help interventions for curbing adult problem drinking: A meta-analysis. Journal of Medical Internet Research. 2011;13:44–56. doi: 10.2196/jmir.1691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schrimsher GW, Filtz K. Assessment reactivity: Can assessment of alcohol use during research be an active treatment? Alcoholism Treatment Quarterly. 2011;29:108–115. doi: 10.1080/07347324.2011.557983. [DOI] [Google Scholar]
- Singer JD, Willett JB. Applied longitudinal data analysis: Modeling change and event occurrence. New York, NY: Oxford University Press; 2003. [Google Scholar]
- Sinha R. How does stress lead to risk of alcohol relapse? Alcohol Research: Current Reviews. 2012;34:432–440. doi: 10.35946/arcr.v34.4.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline Followback user’s guide: A calendar method for assessing alcohol and drug use. Toronto, Canada: Addiction Research Foundation; 1996. [Google Scholar]
- Sobell MB, Sobell LC. Stepped care as a heuristic approach to the treatment of alcohol problems. Journal of Consulting and Clinical Psychology. 2000;68:573–579. doi: 10.1037/0022-006X.68.4.573. [DOI] [PubMed] [Google Scholar]
- Stockwell T, Hodgson R, Edwards G, Taylor C, Rankin H. The development of a questionnaire to measure severity of alcohol dependence. British Journal of Addiction. 1979;74:79–87. doi: 10.1111/j.1360-0443.1979.tb02415.x. [DOI] [PubMed] [Google Scholar]
- Stockwell T, Murphy D, Hodgson R. The Severity of Alcohol Dependence Questionnaire: Its use, reliability and validity. British Journal of Addiction. 1983;78:145–155. doi: 10.1111/j.1360-0443.1983.tb05502.x. [DOI] [PubMed] [Google Scholar]
- Tabachnick B, Fidell L. Using multivariate statistics. 5. Boston, MA: Allyn & Bacon/Pearson Education; 2007. [Google Scholar]
- Tucker JA. Predictors of help-seeking and the temporal relationship of help to recovery among treated and untreated recovered problem drinkers. Addiction. 1995;90:805–809. doi: 10.1046/j.1360-0443.1995.9068057.x. [DOI] [PubMed] [Google Scholar]
- Vernon ML. A review of computer-based alcohol problem services designed for the general public. Journal of Substance Abuse Treatment. 2010;38:203–211. doi: 10.1016/j.jsat.2009.11.001f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weaver ER, Horyniak DR, Jenkinson R, Dietze P, Lim MSC. “Let’s get wasted!” and other apps: Characteristics, acceptability, and use of alcohol-related smartphone applications. JMIR Mhealth Uhealth. 2013;1:e9. doi: 10.2196/mhealth.2709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willoughby FW, Edens JF. Construct validity and predictive utility of the stages of change scale for alcoholics. Journal of Substance Abuse. 1996;8:275–291. doi: 10.1016/S0899-3289(96)90152-2. [DOI] [PubMed] [Google Scholar]