Abstract
Objectives
The purpose of this paper was to systematically review the literature investigating the relationship between perceived racism/discrimination and health among black American women.
Methods
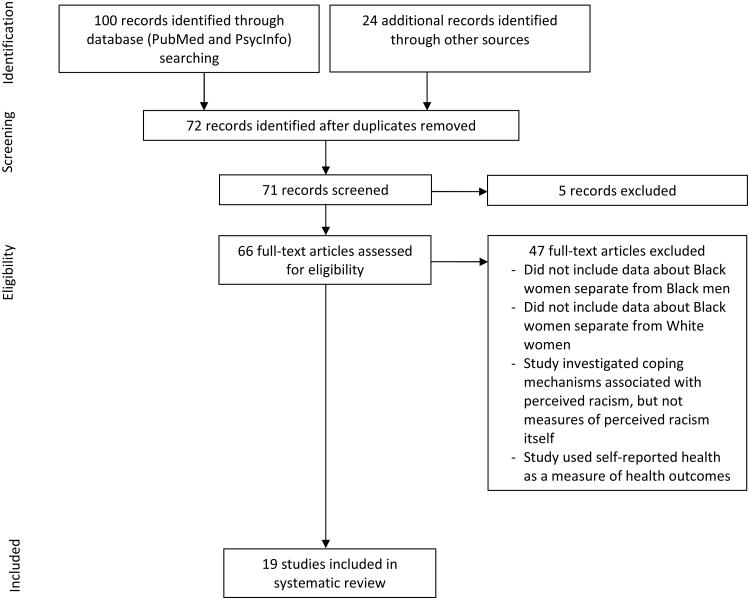
Searches for empirical studies published from January 2003 to December 2013 were conducted using PubMed and PsycInfo. Articles were assessed for possible inclusion using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2009 framework. In addition, the Agency for Healthcare Research and Quality (AHRQ) system for rating the strength of scientific evidence was used to assess the quality of studies included in the review.
Results
Nineteen studies met criteria for review. There was mixed evidence for general relationships between perceived racism/discrimination and health. Consistent evidence was found for the relationship between adverse birth outcomes, illness incidence, and cancer or tumor risk and perceived racism/discrimination. Inconsistent findings were found for the relationship between perceived racism/discrimination and heart disease risk factors. There was no evidence to support the relationship between perceived racism/discrimination and high blood pressure.
Conclusions
There is mixed evidence to support the association between perceived racism/discrimination and overall objective health outcomes among black American women. The strongest relationship was seen between perceived racism/discrimination and adverse birth outcomes. Better understanding the relationship between health and racism/discrimination can aid in identifying race-based risk factors developing primary prevention strategies. Future studies should aim to investigate the role of perceived racism/discrimination as a specific chronic stressor within discrete pathogenesis models.
Keywords: Women, racism, discrimination, health
Over the years, studies have investigated the health disparities that exist in the United States, particularly between black Americans and their white counterparts [1-4]. Research has shown that blacks are at a higher risk for premature death compared to whites in America, due in part to the higher rates of diseases such as diabetes, heart disease, hypertension, and obesity [1, 5]. It is believed that a number of factors work in tandem to create these disparities, such as cultural lifestyle patterns, inherited health risks, social inequalities, and stereotype threat [1, 6].
In addition, there have been a number of theories suggesting that the deleterious effects of racism may contribute both directly and indirectly to these health disparities. Studies have shown the relationship between encounters of racist events, physiological activity, and health outcomes [7]. However, no systematic reviews have focused solely on its impact on black women in America. This is surprising given the evolving area of research showing the relationship between racism and low birth weight [8], heart disease [9], and breast cancer incidence [10] in women.
The purpose of this review is to critically review the existing research that focuses on the relationship between perceived racism and health outcomes among black American women over the last decade using the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) 2009 framework [11]. In addition, the Agency for Healthcare Research and Quality (AHRQ) system for rating the strength of scientific evidence [12] was used to assess the quality of studies included in the review.
Methods
Defining and Measuring Racism and Discrimination
While there is no universal definition of racism, the one that will be used for this review defines racism as “beliefs, attitudes, institutional arrangements, and acts that tend to denigrate individuals or groups because of phenotypic characteristics or ethnic group affiliation” [5]. This definition of racism includes both intergroup (racism from members of another ethnic group) and intragroup (racism from members of the same ethnic group) racism. A related concept, racial discrimination, occurs when one unfavorably distinguishes someone from others based upon race [13]. Racism is considered to be a cognitive concept involving thoughts and beliefs, while discrimination is the action that stems from those thoughts and beliefs [14]. Given the interrelatedness of these two concepts, both racism and discrimination will be examined in this review. Further, as the perception of racism and discrimination are paramount to the theoretical foundation of racism as a stressor [5], only studies that measure racism and discrimination directly at an individual level through self-report as a primary measure will be included in this review.
There are also variables that serve as mediators, including racism as a perceived stressor, coping responses, and psychological and physiological stress responses [5]. Based on the original Lazarus and Folkman model of stress [15], the effects of a potential stressor depend on the person's perception of the event as stressful and their subsequent coping responses. In the case of racism, one must first perceive the external stimuli as involving racism to be considered a stressor. Further, the coping responses employed by the person can also mediate the relationship between events and health outcomes, with maladaptive coping leading to increased stress responses and adaptive coping possibly diminishing stress responses. The repeated combination of perceived racism and maladaptive coping may result in poor health outcomes by increasing and prolonging sympathetic nervous system responses. Finally, psychological responses (e.g., anger) and physiological responses (e.g., impact on the immune system) also serve as mediators in the relationship between external stimuli and health outcomes [5]. The purpose of this review is to broadly assess the relationship between perceived racism/discrimination and health outcomes among black women, thus mediators and moderators will not be addressed when reviewing studies.
Study Selection
Articles were assessed for possible inclusion using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2009 framework [11]. The PRISMA framework was developed to improve the reporting of both systematic reviews and meta-analyses. It consists of a 27-item checklist and four-phase flow diagram. The included studies were assessed using the AHRQ system for measuring the strength of scientific studies. This system evaluates eight domains of an observational research study: study question, study population, exposure of interest, outcome measurement, statistical analyses, results, discussion, and disclosure of funding or sponsorship. Each domain is assessed for meeting minimum requirements and a score (up to eight points) is given to represent the strength of the scientific evidence for each publication [12].
Studies included for review assess the relationship between perceived racism or discrimination and a variety of objective health outcomes (e.g., blood pressure, heart disease, preterm birth) among black American women. While self-reported health status is considered to be an appropriate indicator of health in some populations [16], this review was limited to more specific clinical health outcomes.
Search Strategy
Pubmed and PsycInfo were searched from January 2003 to December 2013 using a combination of the key words: “perceived discrimination”, “perceived racism”, “African American women”, “health outcomes”, “health”, and “disease”. Reference sections of review articles and identified studies were searched to identify additional articles for inclusion. Empirical studies that investigated health outcomes in both black men and women or women of different racial groups were considered for review if the authors gave data specifically about black women separate from black men or women of other races.
Results
Search Results
The combined searches from Pubmed and PsycInfo as well as other data sources resulted in 124 studies for potential inclusion. Article titles and abstracts were reviewed and after removal of duplicates and articles deemed not applicable, 66 articles were read in full. Of these articles, 47 were excluded due to not including data about women separate from men, not including data about black women separate from women of other races, using self-reported health status as a measure of health outcomes, or investigating coping mechanisms associated with perceived racism but not measures of perceived racism itself. Nineteen articles were retained for inclusion in the systematic review. See Figure 1 for the PRISMA diagram and Table 1 for a summary table of the studies.
Figure 1.
PRISMA diagram.
Table 1.
| Authors | Year | Title | Location | Participants | Measure of health outcome | Racism/discrimination measure | Results | AHRQ score | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Heart Disease Risk Factors | ||||||||||||
| Albert, Ravenell, Glynn, Khera, Halevy, & de Lemos | 2008 | Cardiovas cular risk indicators and perceived race/ethnic discrimination in the Dallas Heart Study | Dallas, TX | 1,475 male and female participants (790 black participants) from the Dallas Heart Study | CVD risk factors: C- Reactive Protein, aortic plaque area and wall thickness, and coronary calcium (CAC) | Have you ever been discriminated against due to your race/ethnicity? (responses: yes, no, or don't know) | No association | 8/8 | ||||
| Lewis et al. | 2006 | Chronic Exposure to Everyday Discrimination and Coronary Artery Calcification in African-American Women: The SWAN Heart Study | United States | 181 black women from the SWAN study | Coronary Artery Calcification | Modified version of the Detroit Area Study Everyday Discrimination Scale [56] | Positive association | 8/8 | ||||
| Troxel, Matthews, Bromberger, & Sutton-Tyrrell | 2003 | Chronic Stress Burden, Discrimination, and Subclinical Carotid Artery Disease in African American and Caucasian Women | Pittsburg, PA | 334 black and white women (109 black women) from the SWAN study | Carotid intima-media thickness (IMT) and presence of arterial plaque | Modified version of the Detroit Area Study Everyday Discrimination Scale [56] | Mode rate positive association | 8/8 | ||||
| Blood Pressure | ||||||||||||
| Brown, Matthews, Bromberger, & Chang | 2006 | The Relation between Perceived Unfair Treatment and Blood Pressure in Racially/Ethnically Diverse Sample of Women | United States | 3,300 women (934 black women) from the SWAN study | One time-point blood pressure measurement | Modified version of the Detroit Area Study Everyday Discrimination Scale [56] | No association | 8/8 | ||||
| Cozier et al. | 2006 | Racial Discrimination and the Incidence of Hypertension in US Black Women | United States | 30,330 black women from the Black Women's Health Study | Diagnosis of hypertension or reported use of antihypertensive medication | Exposure to personally mediated and institutionalized racism; adapted from the Detroit Area Study Everyday Discrimination Scale [56] | No association | 8/8 | ||||
| Clark & Adams | 2004 | Moderating Effects of Perceived Racism on John Henryism and Blood Pressure Reactivity in Black Female College Students | Midwest United States | 117 black women | Blood pressure reactivity during an ethnicity-relevant speaking task | Modified version of the Racism and Life Experiences Scale [57, 58] | No association | 8/8 | ||||
| Birth Outcomes | ||||||||||||
| Collins, David, Handler, Wall, & Andes | 2004 | Very Low Birthweight in African American Infants: The Role of Maternal Exposure to Interpersonal Racial Discrimination | Chicago, IL | 312 black women | Giving birth to very low birth weight (VLBW) preterm infants | Lifetime and pregnancy exposure to racial discrimination across five domains; adapted from Krieger (1990) [59] & McNeilly (1996) [60] | Positive association | 8/8 | ||||
| Dailey | 2009 | Social Stressors and Strengths as Predictors of Infant Birth Weight in Low-Income African American Women | California | 108 black women | Birth weight of infant | Everyday Discrimination Scale [61] | No association | 8/8 | ||||
| Dole et al. | 2004 | Psychosocial factors and Preterm birth among African American and white women in central North Carolina | North Carolina | 1,898 black and White women (724 black women) | Giving birth to a preterm infant | Exposure to discrimination across six domains; adapted from Krieger (1990) [59] and Krieger & Sidney (1996) [41] | Positive association | 8/8 | ||||
| Dominguez, Dunkel-Schetter, Glynn, Hobel & Sandman | 2008 | Racial Differences in Birth Outcomes: The Role of General, Pregnancy, and Racism Stress | Los Angeles county, CA | 51 black and 73 white women | Giving birth to a low birth weight preterm infant | Exposure to discrimination; adapted from Krieger (1990) [59] | Positive association | 8/8 | ||||
| Mustillo, Krieger, Gunderson, Sidney, McCreath, & Kiefe | 2004 | Self-Reported Experiences of Racial Discrimination and Black-White Differences in Preterm and Low-Birthweight Deliveries: The CARDIA Study | United States | 352 black and white women (198 black women) from the CARDIA study | Giving birth to a low birth weight or preterm infant | Exposure to discrimination; adapted from Krieger (1990) [59] and Krieger & Sidney (1996) [41] | Positive association | 8/8 | ||||
| Rankin, David, & Collins | 2011 | African American women's exposure to interpersonal racial discrimination in public settings and preterm birth: The effect of coping behaviors | Chicago, IL | 277 black women | Giving birth to a low birth weight preterm infant | Modified version of the Perceived Racism Scale [60] | Positive association | 8/8 | ||||
| Cancer and Tumor Incidence | ||||||||||||
| Taylor et al. | 2007 | Racial Discrimination and Breast Cancer Incidence in US Black Women: The Black Women's Health Study | United States | 49,161 black women from the Black Women's Health Study | Self-reported breast cancer diagnosis or death from breast cancer | Exposure to everyday and major discrimination; adapted from the Detroit Area Study Everyday Discrimination Scale [56] | Conditional association | 8/8 | ||||
| Wise et al. | 2007 | Perceived Racial Discrimination and Risk of Uterine Leiomyomata | United States | 22,002 black women from the Black Women's Health Study | Self-reported diagnosis of “uterine fibroids” and whether their diagnosis was confirmed by “pelvic examination” or “ultrasound/hysterectomy” | Exposure to lifetime and everyday discrimination; adapted from the Detroit Area Study Everyday Discrimination Scale [56] | Positive association | 8/8 | ||||
| Weight Change and Body Fat Distribution | ||||||||||||
| Cozier, Wise, Palmer, & Rosenberg | 2009 | Perceived Racism in Relation to Weight Change in the Black Women's Health Study | United States | 43,103 black Women from the Black Women's Health Study | Cumulative eight year change and waist circumference | Exposure to everyday and lifetime racism; adapted from the Detroit Area Study Everyday Discrimination Scale [56] | Positive association | 8/8 | ||||
| Vines et al. | 2007 | Associations of Abdominal Fat With Perceived Racism and Passive Emotional Responses to Racism in African American Women | United States | 450 black women from the National Institute of Environmental Health Sciences Uterine Fibroid Study | Waist-hip ratio (WHR) | Telephone-Administered Perceived Racism Scale [62] | Negative association | 8/8 | ||||
| Other Health Outcomes | ||||||||||||
| Albert, et al. | 2010 | Perceptions of Race/Ethnic Discrimination in Relation to Mortality Among Black Women: Results From the Black Women's Health Study | United States | 48,924 black women from the Black Women's Health Study | Mortality during follow-up from 1997 to 2005 | Exposure to discrimination; adapted from the Detroit Area Study Everyday Discrimination Scale [56] | No association | 8/8 | ||||
| Christian, Iams, Porter, & Glaser | 2012 | Epstein-Barr virus reactivation during pregnancy and postpartum: Effects of race and racial discrimination | Columbus, OH | 38 black and 18 women of other races | Epstein-Barr Virus (EBV) titers | The Experiences of Discrimination (EOD) scale [59, 41, 64] | Conditional association | 7/8 | ||||
| Kwate, Valdimarsdoltir, Guevarra, & Bovbjerg | 2003 | Experiences of racist events are associated with negative health consequences for African American women | New York | 71 black women | Self-reported lifetime history of disease occurrence and frequency of colds in the past three weeks | Schedule of Racist Events (SRE) [66] | Positive association | 7/8 | ||||
Measuring Race
Of the 19 studies reviewed, 11 provided information regarding how they measured participant race. All of these studies relied on self-defined race; however the nomenclature and administration of racial definition questions varied throughout the studies. Four studies used self-defined African American race from the study questionnaire [17-20], two studies used self-defined African American or black race from the study questionnaire [8, 21], one study used self-defined non-Hispanic black race from the study questionnaire [22], one study used self-defined non-Hispanic black/African American race from the study questionnaire [23], and two studies used self-defined African American race from their medical records [24, 25]. In addition, one study used self-defined race from the study questionnaire but did not provide the racial vocabulary used [26].
Heart Disease Risk Factors
There were three studies that investigated the relationship between perceived racism/discrimination and heart disease risk factors. Specific outcomes included c-reactive protein, aortic plaque area and thickness, coronary calcium [22], coronary artery calcification [23], carotid intima–media thickness (IMT), and presence of arterial plaque [27]. The Albert et al. study [22] investigated the results from 790 black women taken from the Dallas Heart Study, the Lewis et al. study [23] included 181 black women that were part of the Study of Women's Health Across the Nation (SWAN) study, and the Troxel et al. study [27] also used data obtained from the SWAN study, but the authors analyzed data from 109 black women. Results of these studies showed that there were no significant relationships between perceived discrimination and coronary calcium positive status, elevated c-reactive protein levels [22], or IMT [27]; moderate relationships were observed between chronic discrimination and presence of arterial plaque; and there were significant positive relationships between chronic discrimination and presence of coronary artery calcification [23]. All three studies in this area received an 8/8 score on the AHRQ system of scientific assessment. These scores indicate that the studies assessing the relationship between perceived racism/discrimination and heart disease risk factors provide a good overall quality of evidence in this area. See Table 1 for AHRQ scores of individual studies.
Blood Pressure
There were three studies that investigated the relationship between perceived racism/discrimination and blood pressure. The Brown et al. study [17] analyzed data from 934 black women that were part of the SWAN study, the Cozier et al. study [28] had a sample size of 30,330 black women taken from the Black Women's Health Study, and the Clark and Adams study [29] included 117 black women from a predominately white college. Results of these studies showed that there were no significant relationships between perceived racism/discrimination and baseline blood pressure [17], blood pressure reactivity during an ethnically-related speech task [29], or incidence of hypertension [28]. The studies in this area received an average score of 8/8 on the AHRQ system of scientific assessment. This average score indicates that the studies assessing the relationship between perceived racism/discrimination and blood pressure provide a good overall quality of evidence in this area.
Birth Outcomes
There were six studies that investigated the relationship between perceived racism/discrimination and adverse birth outcomes (i.e., preterm birth and low birth weight infants). The sample sizes for these studies ranged from 51 [8] to 724 [20] black women. One study showed no significant relationship between perceived racism/discrimination and infant birth weight [19]; however, the other studies found significant associations between perceived racism/discrimination and birth weight and or/preterm birth [8, 30, 25, 20, 24]. Further, many of these studies indicated a dose-response relationship between perceived racism/discrimination and birth outcomes [24, 20, 30]. The studies in this area received an average score of 8/8 on the AHRQ system of scientific assessment. This average score indicates that the studies assessing the relationship between perceived racism/discrimination and birth outcomes provide a good overall quality of evidence in this area.
Cancer and Tumor Incidence
There were two studies that investigated the relationship between perceived racism/discrimination and heart disease risk factors. The Taylor et al. [10] and Wise et al. [31] studies analyzed data from 49,161 and 22,002 black women from the Black Women's Health Study, respectively. Results of the first study [10] showed that associations between perceived racism/discrimination and breast cancer incidence were dependent on type of discrimination and age. Specifically, higher rates of breast cancer incidence were only found among women who reported discrimination on the job or in all three domains measured (e.g., housing, job, and police). In addition, there was a stronger relationship between perceived discrimination and breast cancer incidence among women younger than 50. Results of the second study [31] showed a significant, positive dose-response association between perceived racism/discrimination and risk of uterine myomas (i.e., uterine fibroids). The studies in this area received an average score of 8/8 on the AHRQ system of scientific assessment. This average score indicates that the studies assessing the relationship between perceived racism/discrimination and cancer/tumor incidence provide a good overall quality of evidence in this area.
Weight Change and Body Fat Distribution
There were two studies that investigated the relationship between perceived racism/discrimination, weight, and body fat distribution. The study samples were 43,103 black women from the Black Women's Health Study [32] and 450 black women from the National Institute of Environmental Health Sciences Uterine Fibroid Study [21]. Results of the first study [32] showed that there was a significant positive association between perceived racism/discrimination and both weight change and waist circumference change over an eight year period. Results from the second study [21] found a significant negative association between perceived racism/discrimination and abdominal fat, a finding that was in direct opposition to the stated hypothesis. The studies in this area received an average score of 8/8 on the AHRQ system of scientific assessment. This average score indicates that the studies assessing the relationship between perceived racism/discrimination, weight change and body fat distribution provide a good overall quality of evidence in this area.
Other Health Outcomes
There were three studies that investigated the relationship between perceived racism/discrimination and other health outcomes (e.g., all-cause death, Epstein-Barr virus (EBV) reactivation, and illness incidence). The Albert et al. study [33] analyzed data from 48,924 black women as part of the Black Women's Health Study, the Christian et al. study [18] included 38 black women, and the Kwate et al. study [26] included 71 black women. Results of these studies showed that there was not a significant association between perceived racism/discrimination and all-cause mortality [33], but significant positive associations were observed between perceived racism/discrimination, EBV titers during the last two trimesters of pregnancy, lifetime diagnoses of physical illnesses, and occurrence/frequency of common colds. The studies in this area received an average score of 7.3/8 on the AHRQ system of scientific assessment. This average score indicates that the studies assessing the relationship between perceived racism/discrimination and other health outcomes provide a good overall quality of evidence in this area.
Discussion
The overall findings of this review suggest that there is mixed evidence for the relationship between perceived racism/discrimination and health outcomes among black women. The strongest evidence for this relationship comes from research regarding birth outcomes. Specifically, five out of the six studies reviewed found a significant negative association between perceived racism/discrimination and infant birth weight and gestational age. Further, the results of these studies also suggest a dose-response relationship, with more frequent or lifetime exposure to discrimination having a larger effect on birth outcomes. These findings are consistent with a previous systematic review that found evidence for the positive relationship between perceived racial discrimination, low/very low birth weight, and preterm birth [34]. In addition, consistent evidence was found for the relationship between perceived racism/discrimination and illness incidence (e.g., disease occurrence, history of common colds, and EBV reactivation) but not for the possible association between perceived racial discrimination and all-cause mortality.
Further, the findings of these studies suggest a possible association between perceived racism/discrimination and cancer or tumor risk. While there is no previous research linking cancer or tumor incidence and perceived racism/discrimination, numerous studies have shown the disparities in cancer incidence and mortality between blacks and whites [3, 35-37]. This may be due to the direct physiological effects of racism and discrimination. However, the relationship may be accounted for by the association between racism/discrimination and screening behaviors. For example, study found that perceived racial discrimination was associated with not receiving a Pap test but there was no association with other cancer screenings, such as mammograms and colposcopy [38].
Inconsistent findings were found for the possible relationship between heart disease risk factors and perceived racism/discrimination. This is consistent with previous research also showing mixed evidence for the relationship between perceived racism/discrimination and heart disease risk factors among both men and women. These earlier findings range from positive associations with c-reactive protein levels [39], negative associations with coronary artery calcification [40], and no associations with multiple risk factors [22].
The results of the studies show mixed results for the association between perceived racism/discrimination, weight gain, and body fat distribution. There is a dearth of previous literature investigating the relationship between perceived racism/discrimination and obesity measures. One study [41] found a relationship between perceived chronic discrimination and abdominal obesity among Irish, Jewish, Polish, and Italian white Americans. However, similar to the findings of the present review, this study found no association among black Americans.
Finally, there were no findings to support the relationship between perceived racism/discrimination and blood pressure in this population. These findings are somewhat inconsistent with a prior systematic review that found moderate associations between perceived racism/discrimination and blood pressure among both men and women [42]. Further, previous research investigating this relationship in black women found a positive association between perceived racial discrimination and blood pressure [43].
Overall, the results of the AHRQ assessment indicate that the methodology of the studies were good. This suggests that the mixed evidence found for the relationship between perceived racism/discrimination is likely not due to poor methodology or extraneous variables. The mixed results of this systematic review indicate that the relationship between perceived racism/discrimination and health outcomes may only be applicable to certain types of illnesses or diseases. Additional research looking at these health outcomes with mixed evidence may also help to clarify these relationships.
A number of theories may be used to explain a direct physiological relationship between perceived racism/discrimination and health outcomes. It is hypothesized that repeated exposure to actual or perceived racism and discrimination serve as chronic stressors for blacks that can start a cascade of physiological responses resulting in disease and early death [1, 5]. This chronic stressor may then impact health outcomes via direct physiological mechanisms. There are a number of theoretical pathogenesis models to conceptualize this relationship between stress and health, including allostatic load [44, 45], immunosuppression [46-48], and gluco-corticoid-resistance models [49]. These models point to different physiological effects of stress to explain its impact on health and thus may not all be applicable to the unique stressor of perceived racism/discrimination.
While the findings of these studies may partially support a relationship between perceived racism/discrimination and health via possible physiological mechanisms, it is important to acknowledge the impact of behaviors as well. It is possible that the stress of discrimination may lead to poor coping behaviors such as tobacco and alcohol use that in turn impacts health outcomes. It is important for future studies control for these behavioral factors as well as aim to better understand the complex relationship between perceived racism/discrimination, health behaviors, and health outcomes. Further, measurement of racism/discrimination may have impacted the results of this review. Future research should aim to use consistent measures of racism and discrimination in an effort to better compare studies.
The mixed findings may also be due to the differences in coping. Defining racism and discrimination as a stressor requires that the individual perceive the event as racist or discriminatory [5]. Similarly, it may also be the way in which the individual copes with the racist event that contributes to the physiological or behavioral responses. Coping responses considered to be adaptive attenuate the psychological and physiological effects of stress and thus may moderate the effects that the stressor has on the body [5]. Assessing coping styles may help to account for the differing effects of perceived racism/discrimination on health outcomes; however, this factor was outside the scope of this review. Further, there is no one coping style deemed effective for every individual to mitigate the effects of perceived racism. Adaptive coping styles may vary by culture, context, and individual [50], making it difficult to control for adaptive coping styles. Future research in this area should investigate both the deleterious and protective effects of different coping styles on health outcomes.
The results of this systematic review are limited by the data obtained from the individual studies, such as method of measuring race. All of the studies that described how they defined race used self-defined race to classify women as black or African American. No studies aimed to further delineate black or African American into different groups, such as those of black Caribbean or Hispanic black descent. The collapsing of different racial categories is a weakness of this review as it restricts the ability to investigate intragroup differences between those self-described as black or African American. Future research in this area should aim to provide additional race categories in an effort to identify differences among those broadly categorized as black or African American.
In addition, a weakness of this systematic review is that it includes data from studies with a large range of sample sizes. The studies reviewed included sample sizes ranging from 38 [18] to 49,161 [10] black women. Caution should be used when comparing the results of studies with such differing sample sizes; however, this review included studies of all sizes in an effort to provide a comprehensive review of the literature. Limiting a review to studies with larger sample sizes may have resulted in the focus on only specific health outcomes while disregarding others. While the smaller studies may not have as much statistical power, the findings of such studies are of interest and provide a basis for larger studies about the relationship between perceived racism/discrimination and these health outcomes.
This systematic review suggests that perceived racism and discrimination may impact a number of health outcomes among black women; however, there are a number of areas that lack consistent evidence and would benefit from continued research. Very few studies investigated the relationship between perceived racism/discrimination and health outcomes within a specific pathogenesis model. Given that the different models may be more appropriate for some health outcomes compared to others, it is important to examine relationships within the framework of these different models. For example, research has suggested that inflammation may play a part in the occurrence of spontaneous preterm birth [51, 52]. The gluco-corticoid resistance model states that chronic stress may decrease the immune response and increase inflammation over time by diminishing the immune system's sensitivity to glucocorticoid hormones normally involved in regulating the inflammation response. This inability to regulate can then result in excess inflammation throughout the body [49]. Future studies could investigate perceived racism/discrimination as a chronic stressor that impacts health outcomes such as preterm birth via specific pathogenesis models such as this.
While past research has investigated the relationship between chronic stressors and health, future research should extend this research to examine perceived racism/discrimination as a specific type of chronic stressor. This is especially important amongst black women, as some theorists have suggested that they may identify with multiple minority groups and in turn experience higher levels of distress from the combination of racial and gender discrimination [53-55]. By better understanding the unique role of perceived racism and discrimination in health outcomes, we can identify possible race-based risk factors for diseases and primary prevention. This knowledge can also aid in reducing medical mistrust, which can have a direct effect on understanding of, and adherence to, medical advice that may impact satisfaction with care and quality of life [56, 57].
Acknowledgments
Note: Research reported in this publication was supported by the Eunice Kennedy Shriver National Institute of Child Health & Development of the National Institutes of Health under Award Number K12HD052027. The content is soley the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of Interest Statement: Dr. VanHoose is supported by the Eunice Kennedy Shriver National Institute of Child Health & Development of the National Institutes of Health under Award Number K12HD052027. Dr. Johnson and Ms. Black declare that they have no conflict of interest.
References
- 1.Mays VM, Cochran SD, Barnes NW. Race, race-based discrimination, and health outcomes among African Americans. Annual Review of Psychology. 2007;58:201–25. doi: 10.1146/annurev.psych.57.102904.190212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. Journal of Behavioral Medicine. 2009;32(1):20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ward E, Jemal A, Cokkinides V, Singh GK, Cardinez C, Ghafoor A, et al. Cancer disparities by race/ethnicity and socioeconomic status. CA: A Cancer Journal for Clinicians. 2004;54(2):78–93. doi: 10.3322/canjclin.54.2.78. [DOI] [PubMed] [Google Scholar]
- 4.Geronimus AT, Bound J, Waidmann TA, Hillemeier MM, Burns PB. Excess mortality among blacks and whites in the United States. New England Journal of Medicine. 1996;335(21):1552–8. doi: 10.1056/NEJM199611213352102. [DOI] [PubMed] [Google Scholar]
- 5.Clark R, Anderson NB, Clark VR, Williams DR. Racism as a stressor for African Americans: A biopsychosocial model. American psychologist. 1999;54(10):805–16. doi: 10.1037//0003-066x.54.10.805. [DOI] [PubMed] [Google Scholar]
- 6.Burgess DJ, Warren J, Phelan S, Dovidio J, Ryn Mv. Stereotype threat and health disparities: What medical educators and future physicians need to know. Journal of General Internal Medicine. 2010;25(2):169–77. doi: 10.1007/s11606-009-1221-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harrell JP, Hall S, Taliaferro J. Physiological responses to racism and discrimination: An assessment of the evidence. American Journal of Public Health. 2003;93(2):243–8. doi: 10.2105/ajph.93.2.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dominguez TP, Dunkel-Schetter C, Glynn LM, Hobel C, Sandman CA. Racial differences in birth outcomes: the role of general, pregnancy, and racism stress. Health psychology. 2008;27(2):194–203. doi: 10.1037/0278-6133.27.2.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Saban KL, Hoppensteadt D, Bryant FB, DeVon HA. Social determinants and heat shock protein-70 among African American and non-Hispanic white women with atherosclerosis: A pilot study. Biological Research for Nursing. 2013 doi: 10.1177/1099800413491422. [DOI] [PubMed] [Google Scholar]
- 10.Taylor TR, Williams CD, Makambi KH, Mouton C, Harrell JP, Cozier Y, et al. Racial discrimination and breast cancer incidence in US black women: The black women's health study. American Journal of Epidemiology. 2007;166(1):46–54. doi: 10.1093/aje/kwm056. [DOI] [PubMed] [Google Scholar]
- 11.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of Internal Medicine. 2009;151(4):264–9. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 12.West SL, King V, Carey TS, Lohr KN, McKoy N, Sutton SF, et al. Systems to rate the strength of scientific evidence. Agency for Healthcare Research and Quality, US Department of Health and Human Services; 2002. [PMC free article] [PubMed] [Google Scholar]
- 13.Krieger N. Embodying inequality: A review of concepts, measures, and methods for studying health consequences of discrimination. International Journal of Health Services. 1999;29(2):295–352. doi: 10.2190/M11W-VWXE-KQM9-G97Q. [DOI] [PubMed] [Google Scholar]
- 14.Gee GC, Ro A. Racism and discrimination. In: Trinh-Shevrin C, Islam NS, Rey MJ, editors. Asian American communities and health: Context, research, policy, and action. San Fransisco, CA: Jossey-Bass; 2009. pp. 364–402. [Google Scholar]
- 15.Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer Publishing Company; 1984. [Google Scholar]
- 16.Miilunpalo S, Vuori I, Oja P, Pasanen M, Urponen H. Self-rated health status as a health measure: The predictive value of self-reported health status on the use of physician services and on mortality in the working-age population. Journal of clinical epidemiology. 1997;50(5):517–28. doi: 10.1016/s0895-4356(97)00045-0. [DOI] [PubMed] [Google Scholar]
- 17.Brown C, Matthews KA, Bromberger JT, Chang Y. The relation between perceived unfair treatment and blood pressure in a racially/ethnically diverse sample of women. American Journal of Epidemiology. 2006;164(3):257–62. doi: 10.1093/aje/kwj196. [DOI] [PubMed] [Google Scholar]
- 18.Christian LM, Iams JD, Porter K, Glaser R. Epstein-Barr virus reactivation during pregnancy and postpartum: Effects of race and racial discrimination. Brain, Behavior, and Immunity. 2012;26:1280–7. doi: 10.1016/j.bbi.2012.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dailey DE. Social stressors and strengths as predictors of infant birth weight in low-income African American women. Nursing Research. 2009;58(5):340–7. doi: 10.1097/NNR.0b013e3181ac1599. [DOI] [PubMed] [Google Scholar]
- 20.Dole N, Savitz DA, Siega-Riz AM, Hertz-Picciotto I, McMahon MJ, Buekens P. Psychosocial factors and preterm birth among African American and White women in central North Carolina. American Journal of Public Health. 2004;94(8):1358–65. doi: 10.2105/ajph.94.8.1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vines AI, Baird DD, Stevens J, Hertz-Picciotto I, Light KC, McNeilly M. Associations of abdominal fat with perceived racism and passive emotional responses to racism in African American women. Journal Information. 2007;97(3):526–30. doi: 10.2105/AJPH.2005.080663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Albert MA, Ravenell J, Glynn RJ, Khera A, Halevy N, de Lemos JA. Cardiovascular risk indicators and perceived race/ethnic discrimination in the Dallas Heart Study. American Heart Journal. 2008;156(6):1103–9. doi: 10.1016/j.ahj.2008.07.027. [DOI] [PubMed] [Google Scholar]
- 23.Lewis TT, Everson-Rose SA, Powell LH, Matthews KA, Brown C, Karavolos K, et al. Chronic exposure to everyday discrimination and coronary artery calcification in African-American women: the SWAN Heart Study. Psychosomatic Medicine. 2006;68(3):362–8. doi: 10.1097/01.psy.0000221360.94700.16. [DOI] [PubMed] [Google Scholar]
- 24.Collins JW, David RJ, Handler A, Wall S, Andes S. Very low birthweight in African American infants: The role of maternal exposure to interpersonal racial discrimination. American Journal of Public Health. 2004;94(12):2132–8. doi: 10.2105/ajph.94.12.2132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rankin KM, David RJ, Collins JW., Jr African American Women's Exposure to Interpersonal Racial Discrimination in Public Settings and Preterm Birth: The Effect of Coping Behaviors. Ethnicity and Disease. 2011;21(3):370–6. [PubMed] [Google Scholar]
- 26.Kwate NOA, Valdimarsdottir HB, Guevarra JS, Bovbjerg DH. Experiences of racist events are associated with negative health consequences for African American women. Journal of the National Medical Association. 2003;95(6):450–60. [PMC free article] [PubMed] [Google Scholar]
- 27.Troxel WM, Matthews KA, Bromberger JT, Sutton-Tyrrell K. Chronic stress burden, discrimination, and subclinical carotid artery disease in African American and Caucasian women. Health Psychology. 2003;22(3):300–9. doi: 10.1037/0278-6133.22.3.300. [DOI] [PubMed] [Google Scholar]
- 28.Cozier Y, Palmer JR, Horton NJ, Fredman L, Wise LA, Rosenberg L. Racial discrimination and the incidence of hypertension in US black women. Annals of Epidemiology. 2006;16(9):681–7. doi: 10.1016/j.annepidem.2005.11.008. [DOI] [PubMed] [Google Scholar]
- 29.Clark R, Adams JH. Moderating effects of perceived racism on John Henryism and blood pressure reactivity in Black female college students. Annals of Behavioral Medicine. 2004;28(2):126–31. doi: 10.1207/s15324796abm2802_8. [DOI] [PubMed] [Google Scholar]
- 30.Mustillo S, Krieger N, Gunderson EP, Sidney S, McCreath H, Kiefe CI. Self-reported experiences of racial discrimination and Black-White differences in preterm and low-birthweight deliveries: the CARDIA Study. American Journal of Public Health. 2004;94(12):2125–31. doi: 10.2105/ajph.94.12.2125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wise LA, Palmer JR, Cozier YC, Hunt MO, Stewart EA, Rosenberg L. Perceived racial discrimination and risk of uterine leiomyomata. Epidemiology. 2007;18(6):747. doi: 10.1097/EDE.0b013e3181567e92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cozier YC, Wise LA, Palmer JR, Rosenberg L. Perceived racism in relation to weight change in the Black Women's Health Study. Annals of epidemiology. 2009;19(6):379–87. doi: 10.1016/j.annepidem.2009.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Albert MA, Cozier Y, Ridker PM, Palmer JR, Glynn RJ, Rose L, et al. Perceptions of race/ethnic discrimination in relation to mortality among black women: results from the Black Women's Health Study. Archives of Internal Medicine. 2010;170(10):896–904. doi: 10.1001/archinternmed.2010.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Giurgescu C, McFarlin BL, Lomax J, Craddock C, Albrecht A. Racial discrimination and the Black-White gap in adverse birth outcomes: A review. Journal of Midwifery & Women's Health. 2011;56(4):362–70. doi: 10.1111/j.1542-2011.2011.00034.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Agrawal S, Bhupinderjit A, Bhutani MS, Boardman L, Nguyen C, Romero Y, et al. Colorectal cancer in African Americans. The American Journal of Gastroenterology. 2005;100(3):515–23. doi: 10.1111/j.1572-0241.2005.41829.x. [DOI] [PubMed] [Google Scholar]
- 36.Williams DR, Jackson PB. Social sources of racial disparities in health. Health Affairs. 2005;24(2):325–34. doi: 10.1377/hlthaff.24.2.325. [DOI] [PubMed] [Google Scholar]
- 37.Palmer RC, Schneider EC. Social disparities across the continuum of colorectal cancer: A systematic review. Cancer Causes & Control. 2005;16(1):55–61. doi: 10.1007/s10552-004-1253-3. [DOI] [PubMed] [Google Scholar]
- 38.Mouton CP, Carter-Nolan PL, Makambi KH, Taylor TR, Palmer JR, Rosenberg L, et al. Impact of perceived racial discrimination on health screening in black women. Journal of Health Care for the Poor and Underserved. 2010;21(1):287–300. doi: 10.1353/hpu.0.0273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lewis TT, Aiello AE, Leurgans S, Kelly J, Barnes LL. Self-reported experiences of everyday discrimination are associated with elevated C-reactive protein levels in older African-American adults. Brain, behavior, and immunity. 2010;24(3):438–43. doi: 10.1016/j.bbi.2009.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Everage NJ, Gjelsvik A, McGarvey ST, Linkletter CD, Loucks EB. Inverse associations between perceived racism and coronary artery calcification. Annals of epidemiology. 2012;22(3):183–90. doi: 10.1016/j.annepidem.2012.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hunte HE, Williams DR. The association between perceived discrimination and obesity in a population-based multiracial and multiethnic adult sample. American Journal of Public Health. 2009;99(7):1285–92. doi: 10.2105/AJPH.2007.128090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Williams DR, Neighbors H. Racism, discrimination and hypertension: evidence and needed research. Ethnicity and Disease. 2001;11(4):800–16. [PubMed] [Google Scholar]
- 43.Krieger N, Sidney S. Racial discrimination and blood pressure: The CARDIA Study of young black and white adults. American Journal of Public Health. 1996;86(10):1370–8. doi: 10.2105/ajph.86.10.1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Korte SM, Koolhaas JM, Wingfield JC, McEwen BS. The Darwinian concept of stress: Benefits of allostasis and costs of allostatic load and the trade-offs in health and disease. Neuroscience & Biobehavioral Reviews. 2005;29(1):3–38. doi: 10.1016/j.neubiorev.2004.08.009. [DOI] [PubMed] [Google Scholar]
- 45.McEwen BS. Stress, adaptation, and disease: Allostasis and allostatic load. Annals of the New York Academy of Sciences. 1998;840(1):33–44. doi: 10.1111/j.1749-6632.1998.tb09546.x. [DOI] [PubMed] [Google Scholar]
- 46.Cohen S, Herbert TB. Health psychology: Psychological factors and physical disease from the perspective of human psychoneuroimmunology. Annual Review of Psychology. 1996;47(1):113–42. doi: 10.1146/annurev.psych.47.1.113. [DOI] [PubMed] [Google Scholar]
- 47.Maier SF, Watkins LR, Fleshner M. Psychoneuroimmunology: The interface between behavior, brain, and immunity. American Psychologist. 1994;49(12):1004–17. doi: 10.1037//0003-066x.49.12.1004. [DOI] [PubMed] [Google Scholar]
- 48.Segerstrom SC, Miller GE. Psychological stress and the human immune system: A meta-analytic study of 30 years of inquiry. Psychological Bulletin. 2004;130(4):601–30. doi: 10.1037/0033-2909.130.4.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Miller GE, Cohen S, Ritchey AK. Chronic psychological stress and the regulation of pro-inflammatory cytokines: A glucocorticoid-resistance model. Health Psychology. 2002;21(6):531–41. doi: 10.1037//0278-6133.21.6.531. [DOI] [PubMed] [Google Scholar]
- 50.Pascoe EA, Smart Richman L. Perceived discrimination and health: a meta-analytic review. Psychological bulletin. 2009;135(4):531. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wadhwa PD, Culhane JF, Rauh V, Barve SS, Hogan V, Sandman CA, et al. Stress, infection and preterm birth: a biobehavioural perspective. Paediatric and Perinatal Epidemiology. 2001;15(s2):17–29. doi: 10.1046/j.1365-3016.2001.00005.x. [DOI] [PubMed] [Google Scholar]
- 52.Romero R, Espinoza J, Gonçalves L, Kusanovic JP, Friel L, Hassan S, editors. Seminars in reproductive medicine. Thieme; 2007. The role of inflammation and infection in preterm birth. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jones HL, Cross WE, DeFour DC. Race-related stress, racial identity attitudes, and mental health among Black women. Journal of Black Psychology. 2007;33(2):208–31. [Google Scholar]
- 54.Thomas AJ, Witherspoon KM, Speight SL. Gendered racism, psychological distress, and coping styles of African American women. Cultural Diversity and Ethnic Minority Psychology. 2008;14(4):307. doi: 10.1037/1099-9809.14.4.307. [DOI] [PubMed] [Google Scholar]
- 55.St Jean Y, Feagin JR. Double burden: Black women and everyday racism. Armonk, NY: M. E. Sharpe; 1998. [Google Scholar]
- 56.Thompson HS, Valdimarsdottir HB, Winkel G, Jandorf L, Redd W. The Group-Based Medical Mistrust Scale: psychometric properties and association with breast cancer screening. Preventive medicine. 2004;38(2):209–18. doi: 10.1016/j.ypmed.2003.09.041. [DOI] [PubMed] [Google Scholar]
- 57.LaVeist TA, Nickerson KJ, Bowie JV. Attitudes about racism, medical mistrust, and satisfaction with care among African American and white cardiac patients. Medical Care Research and Review. 2000;57(4 suppl):146–61. doi: 10.1177/1077558700057001S07. [DOI] [PubMed] [Google Scholar]
- 58.Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health socio-economic status, stress and discrimination. Journal of Health Psychology. 1997;2(3):335–51. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- 59.Harrell SP, Merchant MA, Young SA. Annual Convention of the American Psychological Association. Chicago, IL: 1997. Psychometric properties of the Racism and Life Experiences Scales (RaLES) [Google Scholar]
- 60.Harrell SP. The racism and life experience scales. Unpublished manuscript. 1997 [Google Scholar]
- 61.Krieger N. Racial and gender discrimination: risk factors for high blood pressure? Social science & medicine. 1990;30(12):1273–81. doi: 10.1016/0277-9536(90)90307-e. [DOI] [PubMed] [Google Scholar]
- 62.McNeilly MD, Anderson NB, Armstead CA, Clark R, Corbett M, Robinson EL, et al. The perceived racism scale: A multidimensional assessment of the experience of white racism among African Americans. Ethnicity & Disease. 1996;6(1-2):154–66. [PubMed] [Google Scholar]
- 63.Forman TA, Williams DR, Jackson JS, Gardner C. Race, place, and discrimination. Perspectives on Social Problems. 1997;9:231–61. [Google Scholar]
- 64.Vines AI, McNeilly MD, Stevens J, Hertz-Picciotto I, Bohlig M, Baird DD. Development and reliability of a Telephone-Administered Perceived Racism Scale (TPRS): a tool for epidemiological use. Ethnicity & disease. 2001;11(2):251–62. [PMC free article] [PubMed] [Google Scholar]
- 65.Krieger N, Smith K, Naishadham D, Hartman C, Barbeau EM. Experiences of discrimination: Validity and reliability of a self-report measure for population health research on racism and health. Social science & medicine. 2005;61(7):1576–96. doi: 10.1016/j.socscimed.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 66.Landrine H, Klonoff EA. The schedule of racist events: A measure of racial discrimination and a study of its negative physical and mental health consequences. Journal of Black Psychology. 1996;22(2):144–68. [Google Scholar]