Significance
Current antiviral treatments for chronic hepatitis B virus (HBV) infection are effective in suppressing production of virus, but they have poor efficacy in promoting the elimination of infection. Hence, most patients with chronic HBV infection are maintained on antiviral therapies indefinitely. There is much interest in identifying treatments that promote the clearance of infected hepatocytes, thus purging the HBV DNA reservoir in the liver. Here, we show that the clinical-stage drug birinapant, which antagonizes host cell inhibitor of apoptosis proteins (cIAPs), preferentially promotes the killing of HBV-infected hepatocytes in a mouse model of HBV. Therefore, birinapant and other antagonists of cIAPs may be efficacious in the treatment of chronic HBV infection and may promote elimination of virus.
Keywords: hepatitis B virus, cellular inhibitor of apoptosis proteins, TNF, birinapant, Smac mimetic
Abstract
We have shown that cellular inhibitor of apoptosis proteins (cIAPs) impair clearance of hepatitis B virus (HBV) infection by preventing TNF-mediated killing/death of infected cells. A key question, with profound therapeutic implications, is whether this finding can be translated to the development of drugs that promote elimination of infected cells. Drug inhibitors of cIAPs were developed as cancer therapeutics to promote TNF-mediated tumor killing. These drugs are also known as Smac mimetics, because they mimic the action of the endogenous protein Smac/Diablo that antagonizes cIAP function. Here, we show using an immunocompetent mouse model of chronic HBV infection that birinapant and other Smac mimetics are able to rapidly reduce serum HBV DNA and serum HBV surface antigen, and they promote the elimination of hepatocytes containing HBV core antigen. The efficacy of Smac mimetics in treating HBV infection is dependent on their chemistry, host CD4+ T cells, and TNF. Birinapant enhances the ability of entecavir, an antiviral nucleoside analog, to reduce viral DNA production in HBV-infected animals. These results indicate that birinapant and other Smac mimetics may have efficacy in treating HBV infection and perhaps, other intracellular infections.
Studies using animal models indicate that TNF is an important effector cytokine that promotes clearance of hepatitis B virus (HBV) infection (1, 2). Compelling human data show that HBV-infected patients, particularly those with detectable serum HBV surface antigen (HBsAg), are at increased risk of HBV reactivation when treated with TNF antagonists (3, 4). Therefore, therapeutics that augment the mechanisms through which TNF constrains HBV could be of great benefit to patients with chronic HBV infection. Cellular inhibitor of apoptosis proteins (cIAPs) regulate TNF signaling by promoting NF-κB activation downstream of TNF receptor 1 (TNFR1) ligation, and this activation, in turn, promotes cell survival and antagonizes the cell death-inducing potential of TNF (5). When the function of cIAPs is antagonized, TNF-mediated ligation of TNFR1 causes cell death (6–8). Inhibitors of cIAPs promote TNF-mediated death of primary cancer cells in vitro and in xenograft models (9–13). However, there is considerable controversy regarding the effects of Smac mimetics on and the potential deleterious consequences for immunity to infection (14, 15).
There are three major mammalian inhibitor of apoptosis proteins (IAPs) called cellular inhibitor of apoptosis protein 1 and 2 (cIAP1 and cIAP2) and X-linked inhibitor of apoptosis protein (XIAP). Mice that are deficient in cIAP1 and cIAP2 in the liver show enhanced and efficient clearance of HBV infection (1). This major finding raises the possibility of targeting IAPs to promote HBV clearance in patients, but several key issues need to be addressed. In this study, we examine these issues, and we specifically investigate if antagonizing IAPs after chronic infection has been established recapitulates the outcomes in cIAP-deficient mice. Small-molecule inhibitors differ in terms of their specific chemical properties, and it would be of interest to know if these differences impact their efficacy in HBV infection. In contrast to conditionally gene-targeted mice, a drug antagonist would interfere with IAP function both intermittently and in tissues beyond the liver. The impact of this and potential collateral consequences, therefore, need to be addressed. It is also critical to establish that the drug candidates have a mechanism of action consistent with the on-target effects predicated through gene-targeting experiments. Our study examines and addresses the issues raised above, and our preclinical data indicate that the cIAP antagonist birinapant and perhaps, other Smac mimetics may have therapeutic efficacy in the treatment of chronic HBV infection.
Results
cIAPs Antagonists Promote HBV Clearance.
There are two classes of cIAP inhibitors undergoing evaluation in cancer clinical trials: monovalent and bivalent IAP inhibitors. The latter inhibitors were developed in an attempt to more faithfully mimic the action of the endogenous Smac/Diablo. Birinapant is a potent bivalent antagonist of cIAP1, and it also antagonizes cIAP2 but to a lesser degree (11, 12). Similarly, GT13072 is a potent bivalent cIAP antagonist (16), whereas LCL-161 is a monovalent Smac mimetic.
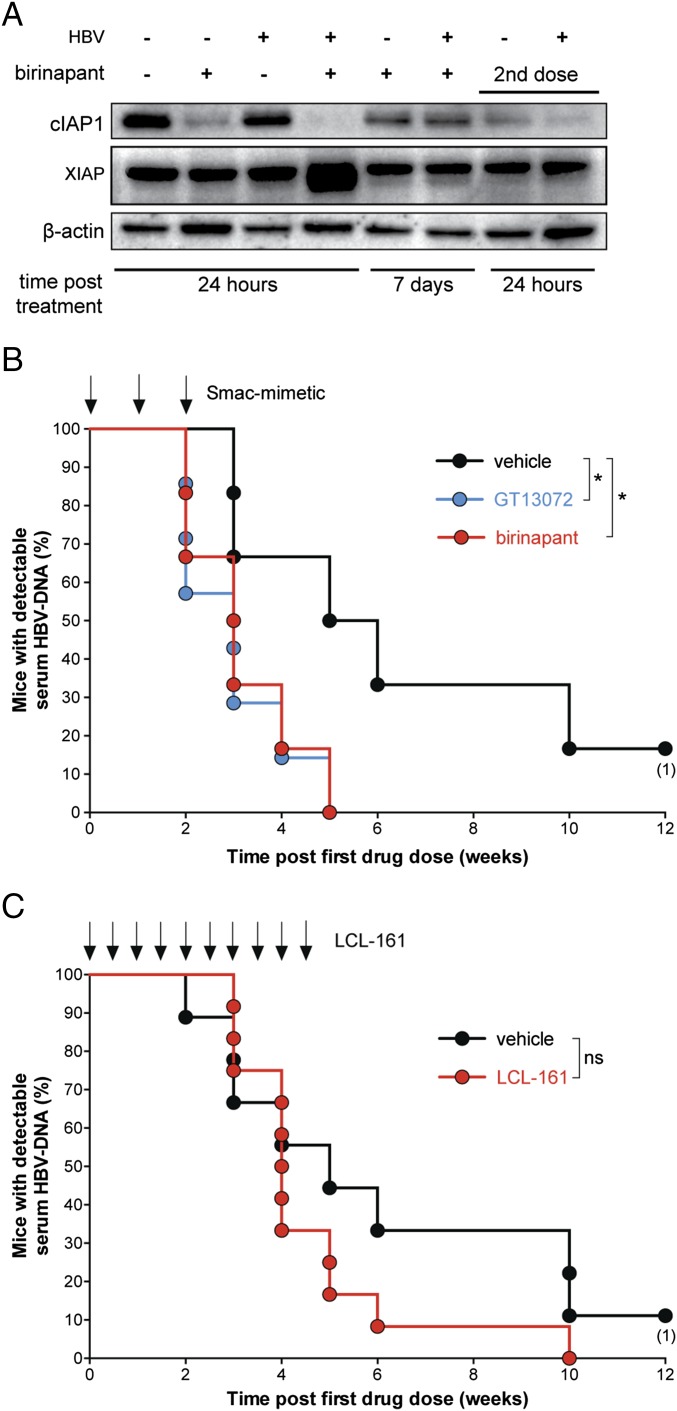
To examine the in vivo efficacy of Smac mimetics in the treatment of HBV infection, we used an immunocompetent mouse model of chronic HBV infection (1, 17, 18). The model mimics aspects of variability seen in human serum HBV DNA levels during infection, because not all mice, even within strains, behave identically (1). This aspect of the model may better predict outcomes in clinical studies. Mice were hydrodynamically injected with a plasmid containing the HBV genome to establish chronic HBV infection. A single dose of birinapant was administered 7 d after HBV infection was induced in mice, and we found that treatment efficiently reduced liver cIAP1 protein levels within 24 h of injection (Fig. 1A). Similarly, a single dose of LCL-161 was able to lower cIAP1 levels in the liver of mice (Fig. S1A). Smac mimetics are known to promote the ubiquitination and proteasomal degradation of cIAP1 (11, 12). Seven days after the administration of a single dose of birinapant, the levels of intrahepatic cIAP1 returned to baseline. When animals were treated with a second dose of birinapant, the protein levels of cIAP1 were quickly reduced again compared with untreated animals (Fig. 1A). These results indicated that in vivo treatment with birinapant caused a reduction in cIAP1 in the liver of both naïve and HBV-infected mice, consistent with the predicted on-target effects of this drug.
Fig. 1.
Birinapant promotes clearance of HBV. (A) Western blot analysis of protein levels in the liver of HBV-infected mice 1 wk postinduction of infection or uninfected mice at the indicated time points after a single dose of birinapant treatment and a second dose of birinapant administered 7 d after the first dose. (B) Proportion of animals and time when mice treated with the indicated compound starting 1 wk after induction of infection and administered once weekly for 3 wk first achieved an undetectable serum HBV DNA level (n = 6–7 for each group). (C) Proportion of animals and time when mice treated with the indicated compound starting 1 wk after induction of infection and administered as indicated (arrows) first achieved an undetectable serum HBV DNA level (n = 9–12 for each group). Vehicle treatment differed across experiments [(B) weekly DMSO injections or (C) daily gavage with vehicle], and therefore, results should not be compared across experiments. Numbers below dots in time to event analyses represent remaining mice that have been censored. Data are representative of (A) three or (B and C) two independent experiments. (B and C) Experiments were performed blinded. ns, not significant. *P < 0.05 (log-rank Mantel–Cox test).
To examine the consequences of antagonizing cIAPs during the course of HBV infection in mice, we treated animals with weekly doses of birinapant or GT13072 for 3 wk commencing 1 wk after induction of infection. Both drugs promoted the rapid control of HBV infection, such that all mice had undetectable serum HBV DNA levels by 5 wk compared with vehicle-treated mice, which continued to have HBV DNA detectable in serum beyond 12 wk (Fig. 1B). We performed a dose–response analysis and determined that a dose of 10 mg/kg birinapant (per dose) was sufficient to promote the rapid control of HBV infection (Fig. S1B). A previous report has indicated that at least one Smac mimetic can impair immune responses to pathogens and cause protracted infection (15). To address this discrepancy, we tested the monovalent compound used in those experiments, LCL-161, and examined its effects in our HBV model. We found that LCL-161 did not behave like bivalent compounds birinapant and GT13072, because there was no difference in its ability to reduce serum HBV DNA levels compared with mice treated with vehicle (Fig. 1C). Our data are consistent with the previous report (15), and these results may indicate that differences in chemistry, including a compound’s mono- or bivalent nature, impact on the efficacy of Smac mimetics; furthermore, the efficacy of Smac mimetics may be context- or infection-dependent. Our data clearly show that birinapant and chemically related Smac mimetics have in vivo efficacy in promoting the initial clearance of HBV infection in a mouse model, and this clearance of HBV was associated with birinapant’s ability to antagonize cIAPs.
TNF Is Required for Birinapant’s Efficacy.
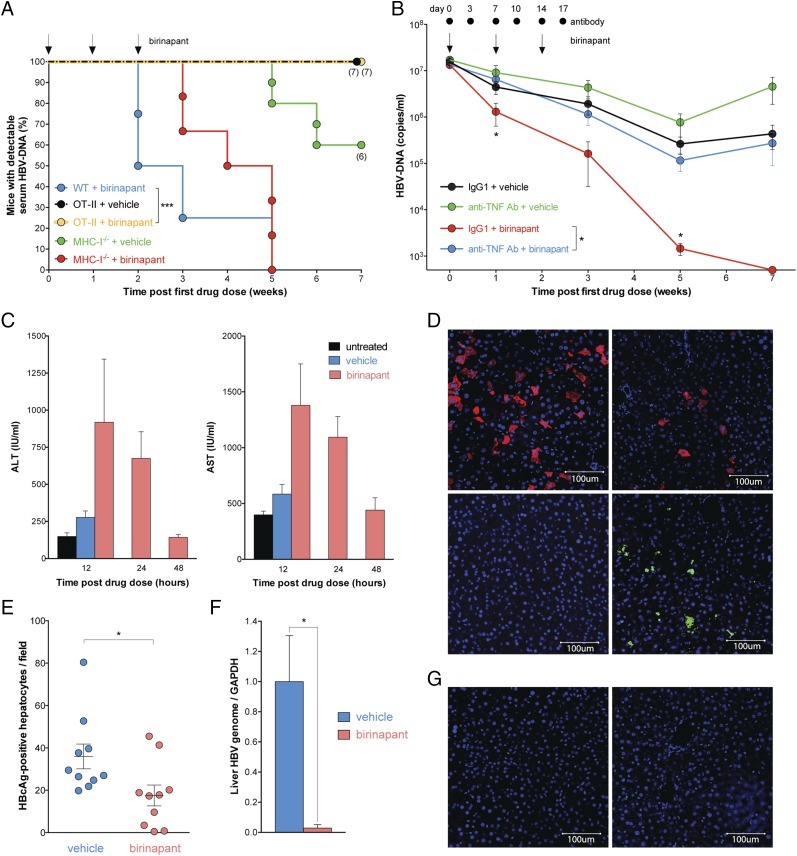
To investigate how birinapant constrained HBV infection in vivo, we used gene-targeted mice to dissect potential effector mechanisms. We have shown that OT-II transgenic mice, which have a highly skewed CD4+ T-cell receptor repertoire restricting antigen recognition to chicken ovalbumin, have persistently high serum HBV DNA levels compared with WT mice during HBV infection (1). We tested the efficacy of birinapant in OT-II HBV-infected mice and found that the drug was not able to lower serum HBV DNA levels compared with vehicle-treated control animals (Fig. 2A and Fig. S2A). These results indicated that birinapant’s efficacy in controlling HBV infection was dependent on a CD4+ T-cell repertoire capable of recognizing HBV. We also examined the requirement for CD8+ T cells in promoting birinapant’s activity. Mice with targeted mutations in H-2Kb and H-2Db lack MHC class Ia expression and have a >80% reduction in CD8+ T-cell numbers (19). These mice have highly impaired cytotoxic T-cell responses. We infected MHC class Ia-deficient mice with HBV and found that birinapant was still able to rapidly reduce serum HBV DNA loads in MHC class Ia-deficient mice infected with HBV (Fig. 2A and Fig. S2A). Therefore, CD8+ T-cell cytotoxic activity was not required, but CD4+ T cells, possessing unrestricted T-cell receptor repertoires capable of recognizing HBV, were essential for birinapant’s efficacy in controlling HBV.
Fig. 2.
Birinapant sensitizes HBV-infected hepatocytes to TNF-mediated killing. (A) Proportion of animals and time when mice with the specified genotypes treated with birinapant or vehicle commencing 1 wk after induction of infection at the times indicated by arrows first achieved an undetectable serum HBV DNA level (n = 4–10 in each group). (B) Serial serum HBV DNA levels in C57BL/6 mice treated with birinapant (arrows) and TNF-neutralizing antibody or isotype control (dots) commencing 1 wk after induction of infection (n = 7–16 per group). (C) Serum transaminase levels quantified at the indicated times in HBV-infected untreated mice or mice treated with a single dose of birinapant (10 mg/kg) or vehicle 1 wk postinduction of infection (n = 4–5 in each group). (D) Immunofluorescence staining (blue DAPI and red HBcAg in Upper and blue DAPI and green TUNEL in Lower) of liver sections from HBV-infected C57BL/6 mice 12 h after treatment with (Right) a single dose of 10 mg/kg birinapant or (Left) vehicle administered 2 wk postinduction of infection (representative of n = 6 each group). (E) Number of HBV-infected hepatocytes (described and treated as in D) expressing HBcAg (n = 10 for each group). (F) RT-PCR of HBV DNA relative to GAPDH in the liver of infected C57BL/6 mice treated with birinapant or vehicle (as described in A above) 7 wk after induction of infection (n = 5 in each group). (G) Immunofluorescence staining (blue DAPI and green TUNEL) of liver sections from uninfected C57BL/6 mice 12 h after treatment with a single dose of (Right) 10 mg/kg birinapant or (Left) vehicle (representative of n = 3 in each group). Numbers below dots in time to event analyses represent remaining mice that have been censored. (A–E and G) Graphs show means and SEMs, and data are representative of two independent experiments. (A–C) Experiments were performed blinded. ALT, alanine aminotransferase; AST, aspartate aminotransferase. *P < 0.05; ***P < 0.001 (A, log-rank Mantel–Cox test; B, unpaired two-tailed t test with Holm–Sidak correction; E, unpaired two-tailed t test; and F, Mann–Whitney test).
CD4+ T cells directly and indirectly contribute to TNF production, and therefore, we examined if TNF was necessary for birinapant’s activity in lowering serum HBV DNA levels. We administered TNF-neutralizing antibodies contemporaneously with birinapant treatment in HBV-infected animals and found that antagonizing TNF caused birinapant to lose its efficacy, and it was no longer able to rapidly lower serum HBV DNA levels (Fig. 2B). To determine if IFN-γ was also required for birinapant’s efficacy in lowering serum HBV DNA levels, we induced HBV infection in IFN-γ–deficient mice and treated them with birinapant. Birinapant treatment was able to lower HBV DNA levels in IFN-γ–deficient mice compared with vehicle-treated controls (Fig. S1B). Our data show that birinapant lowered HBV DNA levels in mice through a TNF-dependent but IFN-γ–independent mechanism.
Birinapant Promotes Preferential Killing of HBV-Infected Hepatocytes.
The drop in serum HBV DNA levels seen in birinapant-treated mice, even after a single dose, was associated with elevations in serum alanine transaminase and aspartate aminotransferase, but these elevations did not reach statistical significance (P = 0.23, unpaired two-tailed t test). Importantly, birinapant’s effect on aspartate aminotransferase and alanine transaminase levels was transient, and within 48 h, transaminase levels returned to baseline (Fig. 2C). These data indicate that birinapant was not causing substantial collateral liver damage.
A single dose of birinapant was sufficient to decrease the number of HBV core antigen (HBcAg) -expressing hepatocytes, and this decrease was associated with an increase in the number of TUNEL-positive cells (Fig. 2 D and E). Additionally, birinapant treatment caused a 35-fold reduction in the amount of HBV genome in the liver of infected mice compared with vehicle-treated animals, but some residual HBV could still be detected after three doses of birinapant, despite the clearance of serum HBV DNA and liver HBcAg (Fig. 2 D–F). We speculate that this residual HBV genome in the liver of birinapant-treated mice represents transcriptionally inactive/silenced integrated HBV DNA that can become transcriptionally active to produce HBV DNA at later stages (Fig. S3). In patients, integrated forms of HBV DNA are not thought to contribute to virus production, because they are subgenomic fragments, whereas in our mouse model, full-length HBV DNA has the capacity to integrate into the mouse genome because of the adeno-associated virus-inverted terminal repeats flanking the HBV sequence. Interestingly, if some of these quiescent cells in the liver of mice became virologically active and began producing HBV DNA, it seemed that they were rapidly cleared by an endogenous mechanism (Fig. S3). Birinapant treatment was associated with a modest accumulation of CD4+ and CD8+ T cells in the liver of infected mice, but this accumulation did not reach statistical significance (P > 0.05) (Fig. S2C), and we did not observe any differences in serum cytokine levels between birinapant-treated and control animals (Fig. S2D). Collectively, the data indicate that birinapant was causing the death of infected hepatocytes, and this death was associated with immune cell infiltration. Birinapant seems to preferentially promote killing/death of HBV-infected hepatocytes, because we did not observe any TUNEL-positive cells in uninfected mice treated with birinapant (Fig. 2G). This specificity for infected hepatocytes may be caused by the up-regulation of TNFR1 on infected compared with uninfected hepatocytes (1), which may sensitize infected cells to the TNF-dependent death-inducing effects of birinapant. Additionally, immune cells will confer specificity, because they preferentially target areas of infection.
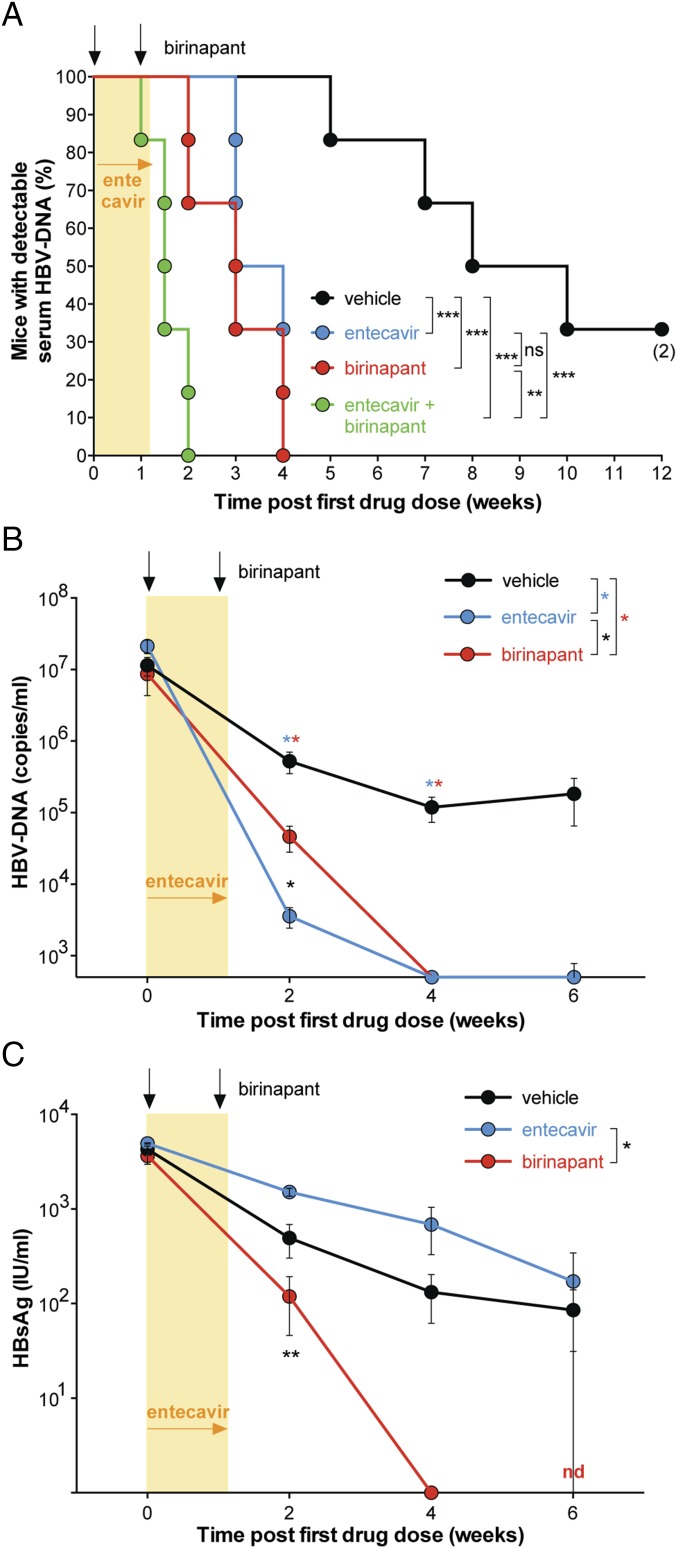
Birinapant Improves Efficacy of Entecavir.
We next investigated if birinapant retained its efficacy combined with current antiviral treatments and whether the combination could elicit more profound control of serum HBV DNA levels in infected animals. We found that the combination of entecavir and birinapant was more efficacious than either drug alone in promoting the very rapid initial clearance of serum HBV DNA in infected animals (Fig. 3A and Fig. S3). Although entecavir as a single agent caused a drop in serum HBV DNA to below our limit of detection (500 copies/mL) within 4 wk of the first treatment, the drug had minimal impact on serum HBsAg levels compared with levels in control-treated animals (Fig. 3 B and C). In contrast, birinapant as a single agent caused both serum HBV DNA and serum HBsAg levels to fall below our detection limit within 4 wk of treatment (Fig. 3 B and C). The combination of these drugs was well-tolerated: there was no overt evidence of toxicity when entecavir and birinapant were coadministered to mice. These data indicate that birinapant and entecavir controlled HBV infection through distinct mechanisms and that combined treatment increased efficacy in reducing serum HBV DNA levels compared with monotherapy with either entecavir or birinapant.
Fig. 3.
Birinapant enhances the efficacy of entecavir. (A) Proportion of animals and time when C57BL/6 mice treated with the specified compounds (shaded area, entecavir; arrows, birinapant doses starting 1 wk after induction of infection) first achieved an undetectable serum HBV DNA level (n = 6 for each group). (B and C) A direct comparison of (B) serum HBV DNA and (C) serum HBsAg levels in the same animals during the course of infection/treatment described in A above (n = 6 for each group). Numbers below dots in time to event analyses represent remaining mice that have been censored. Vehicle-treated mice in A received both injectable and oral vehicles, and birinapant- and entecavir-treated mice received the corresponding vehicle; therefore, these mice should not be compared across other experiments. Graphs show means and SEMs. Experiments were performed blinded. nd, Not detected; ns, not significant. *P < 0.05; **P < 0.01; ***P < 0.001 (A, log-rank Mantel–Cox test; and B and C, unpaired two-tailed t test with Holm–Sidak correction).
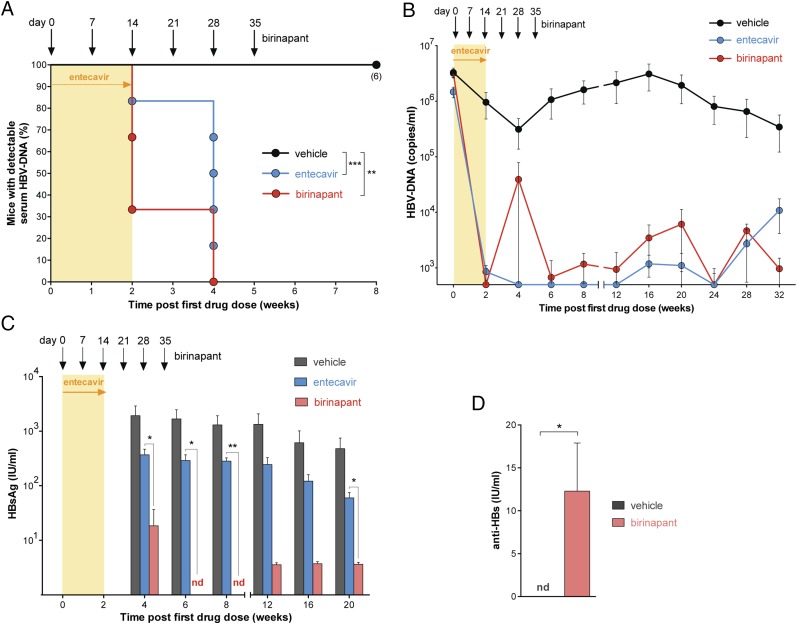
The genetic background of mice affects an animal’s ability to control HBV. C3H mice (endotoxin-sensitive strain) have persistently elevated levels of serum HBV DNA, because they are unable to control infection compared with C57BL/6 mice (1). Despite this genetic predisposition that prevents C3H mice from controlling HBV infection, birinapant treatment lowered serum HBV DNA and HBsAg in these animals (Fig. 4 A–C). Although entecavir was also able to lower HBV DNA levels in C3H mice, it had very limited impact on serum HBsAg compared with birinapant treatment, which caused a drop in HBsAg to levels below our limit of detection (Fig. 4C). A major feature that distinguishes birinapant from entacavir was the clearance of HBsAg and production of serum HBV surface antibody (HBsAb) in all C3H mice receiving birinapant but not C3H mice treated with entecavir (Fig. 4 C and D). Seroconversion (loss of HBsAg and acquisition of HBsAb) is the primary clinical therapeutic goal, and our preclinical data suggest that brinapant is capable of facilitating this outcome.
Fig. 4.
Birinapant promotes seroconversion. (A) Proportion of animals and time when C3H mice treated with the specified compounds (shaded area, entecavir; arrows, birinapant doses starting 1 wk after infection) first achieved an undetectable serum HBV DNA level (n = 3–6 for each group). (B) Serial measurement of serum HBV DNA levels in C3H mice treated as described in A above (n = 3–6 for each group). (C) Serum HBsAg levels in C3H mice treated as described in A (n = 3–6). (D) HBsAb in C3H mice treated with birinapant or vehicle as described in A quantified 7 wk after commencement of drug (n = 4–5). Numbers below dots in time to event analyses represent remaining mice that have been censored. Graphs show means and SEMs. Experiments were performed blinded. *P < 0.05; **P < 0.01; ***P < 0.001 (A, log-rank Mantel–Cox test; C, unpaired two-tailed t-test with Holm–Sidak correction; and D, unpaired two-tailed t test).
Discussion
We have previously shown that cIAPs act as restriction factors preventing TNF-mediated elimination of HBV (1). Birinapant and other Smac mimetics can antagonize cIAPs, and we have now shown that these drugs can promote the clearance of serum HBV DNA levels in two preclinical models of HBV. In C57BL/6 mice that exhibit spontaneous partial control of HBV and C3H mice that have no endogenous capacity to control HBV, birinapant treatment led to clearance of serum HBsAg- and HBcAg-expressing hepatocytes and a reduction in the amount of HBV genome in infected livers.
Birinapant’s efficacy in clearing infection was attenuated in mice that had a highly skewed repertoire of CD4+ T cells that could not respond to HBV. Patients with chronic HBV do possess CD4+ T cells with specificities for HBV, and these cells have variable functional activity when examined ex vivo (20). Based on our data, we would predict that birinapant might have a spectrum of efficacy in HBV-infected patients and that responses may correlate with the quantity and quality of HBV-specific CD4+ T cells. Modifying the duration of birinapant treatment in patients could accommodate this potential variability in responses and optimize efficacy.
Circulating virions produced in patients chronically infected with HBV have the capacity to reinfect hepatocytes and/or infect naïve hepatocytes. Circulating virions produced in our mouse model cannot reinfect or infect naïve mouse hepatocytes, because these cells lack the cognate HBV receptor. This attribute of our model emulates that of patients chronically infected with HBV that are treated with HBV polymerase inhibitors, such as entecavir and tenofovir, that are now standard of care. These patients usually have undetectable viral loads, and hence, reinfection or infection of naïve hepatocytes is not clinically relevant. Importantly, birinapant treatment improved entecavir’s ability to reduce serum HBV DNA levels in animals. The increased efficacy of entecavir combined with birinapant compared with either drug when used alone may be because of entecavir’s ability to promote a rapid reduction in HBV DNA, and this reduction in viremia may enhance antiviral immunity (21–24) and in turn, promote birinapant’s efficacy. In contrast to entecavir, birinapant promoted the clearance of HBsAg and the acquisition of HBsAb in mice.
We have previously shown that the HBV-containing plasmid used to induce infection in our animal models does not persist as the transcriptional template for HBV. Possible persistent transcriptional templates in our models include the formation of episomal HBV DNA or integration of HBV into the mouse genome. The nature of the transcriptional template is unimportant, because birinapant kills HBV-containing hepatocytes, thus eliminating the HBV genome, regardless of what form it takes.
Our data indicate that birinapant and possibly, other Smac mimetics may be efficacious in treating people with chronic HBV infection, and this efficacy can be enhanced by the additional use of current antiviral drugs. Birinapant may also have efficacy in the treatment of other intracellular infections.
Materials and Methods
Mice and Induction of HBV Infection.
The Walter and Eliza Hall Institute of Medical Research Animal Ethics Committee reviewed and approved all animal experiments. Induction of HBV infection has been described previously (1). Additional details are provided in SI Materials and Methods.
Drug and Antibody Treatment.
The following doses were used: 30 mg/kg birinapant dissolved in DMSO (unless otherwise stated) injected i.p. one time per week, 15 mg/kg GT13072 dissolved in DMSO injected i.p. one time per week, 50 mg/kg LCL-161 [dissolved in 30% (vol/vol) 0.1 M HCl, 70% (vol/vol) 0.1 M NaOAc (pH 4.63)] orally two times per week for a total of 10 doses, 3.2 mg/kg entecavir (crushed in peanut oil) orally daily for 1–2 wk, and 200 μg TNF-neutralizing antibodies (rat IgG1 XT22) i.p. Injection of a rat IgG isotype was used as a control.
Biochemistry, Serology, Histology, Flow Cytometry, Cytokine Assays, Western Blots, and Genome Quantification.
Sample preparation and analysis are described in SI Materials and Methods.
Statistical Analysis.
Prism 6.0d software (Graph Pad Software) was used to perform statistical tests. Groups were compared using an unpaired two-tailed t test, and Holm–Sidak correction was applied for multiple comparisons. Nonparametric data were analyzed using the Mann–Whitney test, and time to event analyses were performed using the log-rank Mantel–Cox test.
Supplementary Material
Acknowledgments
We thank Stephen Condon, Peter Revill, and Stephen Locarnini for discussions. Pei-Jer Chen and Ding-Shinn Chen constructed the hepatitis B virus infection vector for hydrodynamic infection. Linda Earnest-Silveira, Danielle Colledge, Xin Li, and Nadia Warner provided laboratory support. This work was supported by Australian Research Council Future Fellowship Award (to U.N.) and Grant FT1301000166; National Health and Medical Research Council Australia Career Development Award 637350 and Grants 541902 (to J.S.), 1006592 (to M.P.), 1045549 (to M.P.), and 1065626 (to M.P.); the Victorian State Government Operational Infrastructure Support; and the Independent Research Institutes Infrastructure Support Scheme of the Australian Government National Health and Medical Research Council.
Footnotes
Conflict of interest statement: The Walter and Eliza Hall Institute of Medical Research has a research license agreement with TetraLogic Pharmaceuticals Corporation, Inc., the manufacturer of the cellular inhibitor of apoptosis protein antagonist birinapant. TetraLogic Pharmaceuticals Corporation, Inc. has filed a patent cooperation treaty application on behalf of The Walter and Eliza Hall Institute of Medical Research. J.S. is on the scientific advisory board of and M.P. provides consultative advice to TetraLogic Pharmaceuticals Corporation, Inc. J.S. has options on a small number of shares in TetraLogic Pharmaceuticals Corporation, Inc. C.G.B. is employed by TetraLogic Pharmaceuticals Corporation, Inc.
This article is a PNAS Direct Submission.
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1502400112/-/DCSupplemental.
References
- 1.Ebert G, et al. Cellular inhibitor of apoptosis proteins prevent clearance of hepatitis B virus. Proc Natl Acad Sci USA. 2015;112:5797–5802. doi: 10.1073/pnas.1502390112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yang PL, et al. Immune effectors required for hepatitis B virus clearance. Proc Natl Acad Sci USA. 2010;107(2):798–802. doi: 10.1073/pnas.0913498107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee YH, Bae SC, Song GG. Hepatitis B virus (HBV) reactivation in rheumatic patients with hepatitis core antigen (HBV occult carriers) undergoing anti-tumor necrosis factor therapy. Clin Exp Rheumatol. 2013;31(1):118–121. [PubMed] [Google Scholar]
- 4.Lan JL, et al. Kinetics of viral loads and risk of hepatitis B virus reactivation in hepatitis B core antibody-positive rheumatoid arthritis patients undergoing anti-tumour necrosis factor alpha therapy. Ann Rheum Dis. 2011;70(10):1719–1725. doi: 10.1136/ard.2010.148783. [DOI] [PubMed] [Google Scholar]
- 5.Silke J. The regulation of TNF signalling: What a tangled web we weave. Curr Opin Immunol. 2011;23(5):620–626. doi: 10.1016/j.coi.2011.08.002. [DOI] [PubMed] [Google Scholar]
- 6.Vince JE, et al. IAP antagonists target cIAP1 to induce TNFalpha-dependent apoptosis. Cell. 2007;131(4):682–693. doi: 10.1016/j.cell.2007.10.037. [DOI] [PubMed] [Google Scholar]
- 7.Wang L, Du F, Wang X. TNF-alpha induces two distinct caspase-8 activation pathways. Cell. 2008;133(4):693–703. doi: 10.1016/j.cell.2008.03.036. [DOI] [PubMed] [Google Scholar]
- 8.Petersen SL, et al. Autocrine TNFalpha signaling renders human cancer cells susceptible to Smac-mimetic-induced apoptosis. Cancer Cell. 2007;12(5):445–456. doi: 10.1016/j.ccr.2007.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Allensworth JL, Sauer SJ, Lyerly HK, Morse MA, Devi GR. Smac mimetic Birinapant induces apoptosis and enhances TRAIL potency in inflammatory breast cancer cells in an IAP-dependent and TNF-α-independent mechanism. Breast Cancer Res Treat. 2013;137(2):359–371. doi: 10.1007/s10549-012-2352-6. [DOI] [PubMed] [Google Scholar]
- 10.Carter BZ, et al. Synergistic targeting of AML stem/progenitor cells with IAP antagonist birinapant and demethylating agents. J Natl Cancer Inst. 2014;106(2):djt440. doi: 10.1093/jnci/djt440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Condon SM, et al. Birinapant, a smac-mimetic with improved tolerability for the treatment of solid tumors and hematological malignancies. J Med Chem. 2014;57(9):3666–3677. doi: 10.1021/jm500176w. [DOI] [PubMed] [Google Scholar]
- 12.Krepler C, et al. The novel SMAC mimetic birinapant exhibits potent activity against human melanoma cells. Clin Cancer Res. 2013;19(7):1784–1794. doi: 10.1158/1078-0432.CCR-12-2518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Benetatos CA, et al. Birinapant (TL32711), a bivalent SMAC mimetic, targets TRAF2-associated cIAPs, abrogates TNF-induced NF-κB activation, and is active in patient-derived xenograft models. Mol Cancer Ther. 2014;13(4):867–879. doi: 10.1158/1535-7163.MCT-13-0798. [DOI] [PubMed] [Google Scholar]
- 14.Dougan M, et al. IAP inhibitors enhance co-stimulation to promote tumor immunity. J Exp Med. 2010;207(10):2195–2206. doi: 10.1084/jem.20101123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gentle IE, et al. Inhibitors of apoptosis proteins (IAPs) are required for effective T-cell expansion/survival during antiviral immunity in mice. Blood. 2014;123(5):659–668. doi: 10.1182/blood-2013-01-479543. [DOI] [PubMed] [Google Scholar]
- 16.Fan LX, et al. Smac-mimetic-induced epithelial cell death reduces the growth of renal cysts. J Am Soc Nephrol. 2013;24(12):2010–2022. doi: 10.1681/ASN.2013020176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lin YJ, et al. Hepatitis B virus core antigen determines viral persistence in a C57BL/6 mouse model. Proc Natl Acad Sci USA. 2010;107(20):9340–9345. doi: 10.1073/pnas.1004762107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Huang LR, Wu HL, Chen PJ, Chen DS. An immunocompetent mouse model for the tolerance of human chronic hepatitis B virus infection. Proc Natl Acad Sci USA. 2006;103(47):17862–17867. doi: 10.1073/pnas.0608578103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pérarnau B, et al. Single H2Kb, H2Db and double H2KbDb knockout mice: Peripheral CD8+ T cell repertoire and anti-lymphocytic choriomeningitis virus cytolytic responses. Eur J Immunol. 1999;29(4):1243–1252. doi: 10.1002/(SICI)1521-4141(199904)29:04<1243::AID-IMMU1243>3.0.CO;2-A. [DOI] [PubMed] [Google Scholar]
- 20.Schmidt J, Blum HE, Thimme R. T-cell responses in hepatitis B and C virus infection: Similarities and differences. Emerg Microbe Infect. 2013;2:e15. doi: 10.1038/emi.2013.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wilson EB, et al. Blockade of chronic type I interferon signaling to control persistent LCMV infection. Science. 2013;340(6129):202–207. doi: 10.1126/science.1235208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Teijaro JR, et al. Persistent LCMV infection is controlled by blockade of type I interferon signaling. Science. 2013;340(6129):207–211. doi: 10.1126/science.1235214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Komarova NL, Barnes E, Klenerman P, Wodarz D. Boosting immunity by antiviral drug therapy: A simple relationship among timing, efficacy, and success. Proc Natl Acad Sci USA. 2003;100(4):1855–1860. doi: 10.1073/pnas.0337483100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bertoletti A, Gehring AJ. The immune response during hepatitis B virus infection. J Gen Virol. 2006;87(Pt 6):1439–1449. doi: 10.1099/vir.0.81920-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.