Abstract
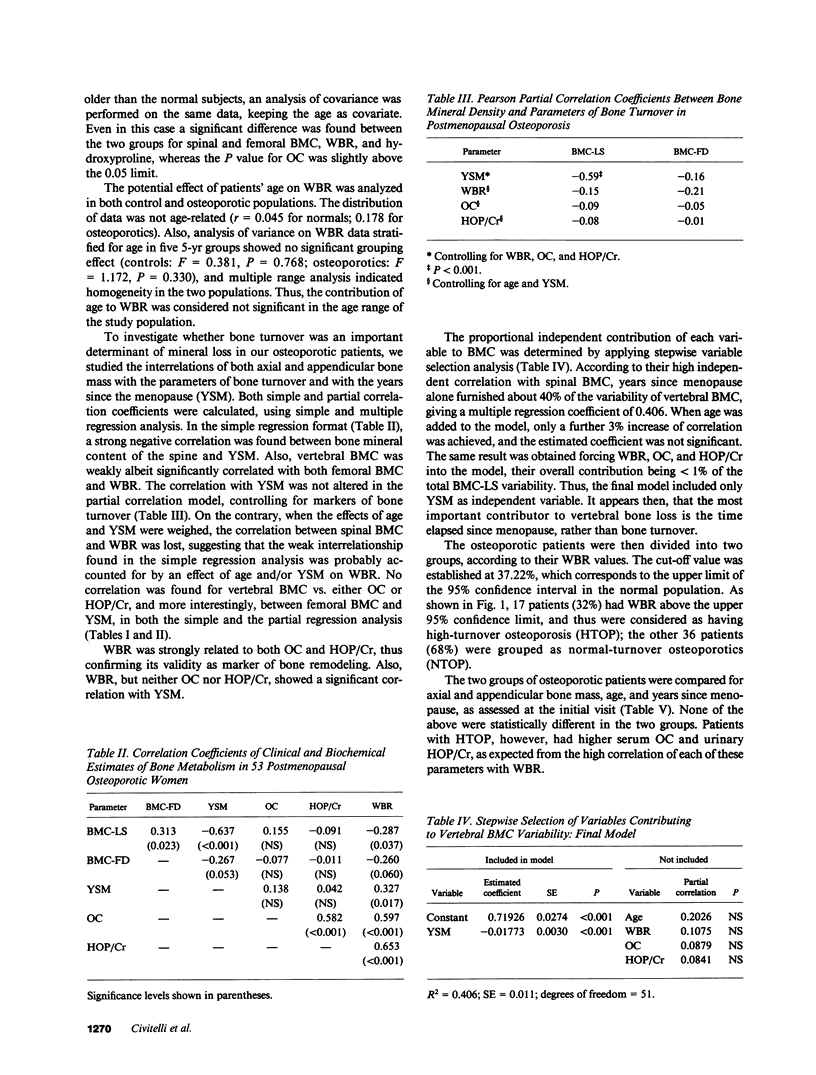
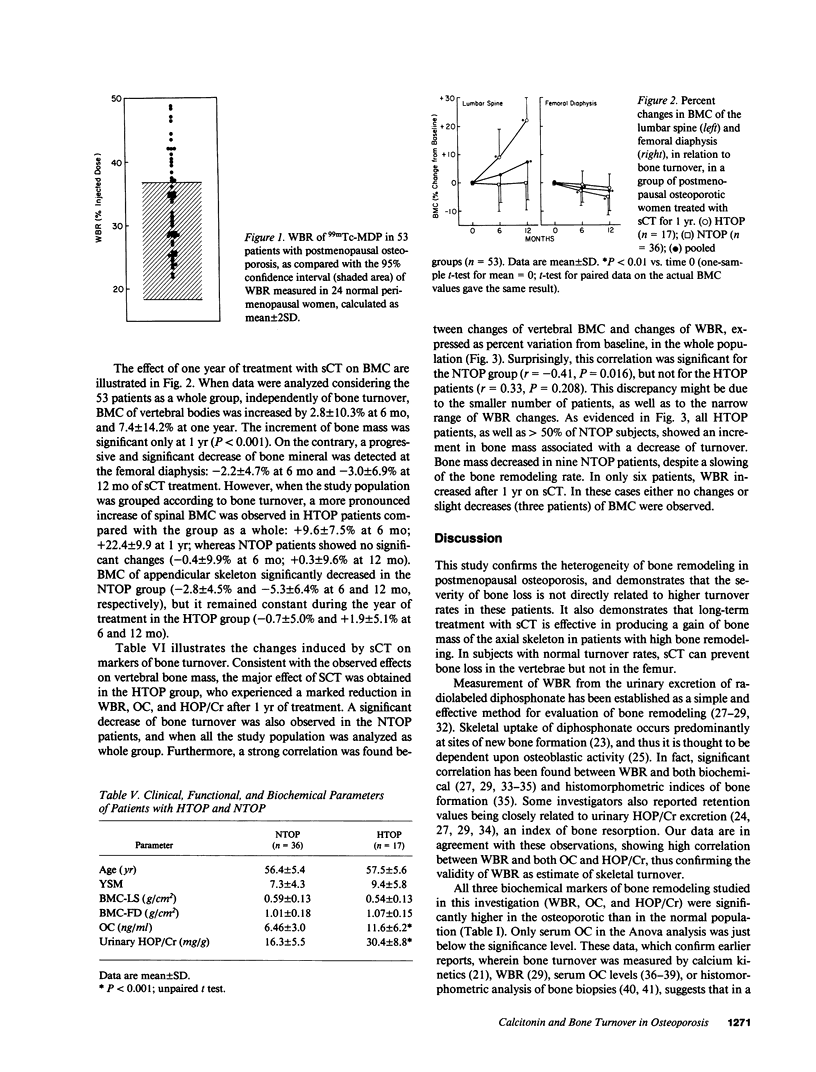
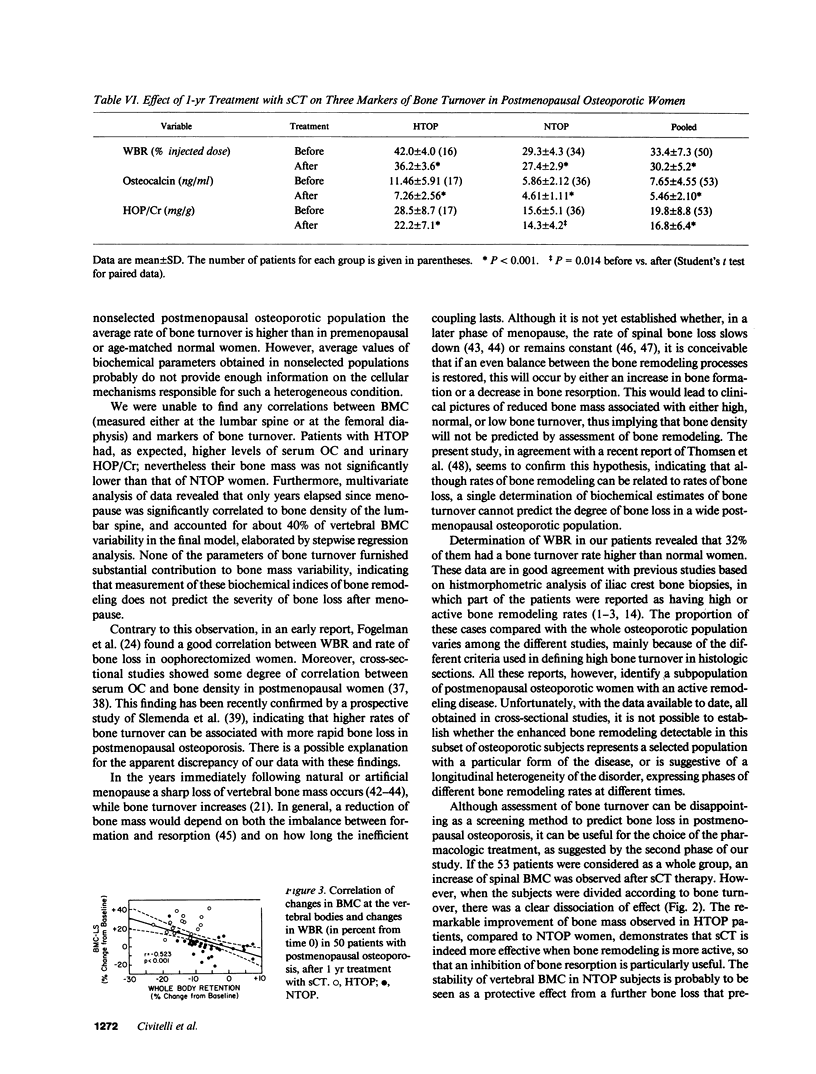
To investigate the effectiveness of calcitonin treatment of postmenopausal osteoporosis in relation to bone turnover, we examined 53 postmenopausal osteoporotic women before and after one year of therapy with salmon calcitonin (sCT), at the dose of 50 IU every other day. Baseline evaluation revealed that 17 (32%) patients had high turnover (HTOP), and 36 (68%) normal turnover osteoporosis (NTOP) as assessed by measurement of whole body retention (WBR) of 99mTc-methylene diphosphonate. The two groups did not differ in terms of bone mineral content (BMC) measured by dual photon absorptiometry at both lumbar spine and femoral diaphysis. However, HTOP patients had higher levels of serum osteocalcin (OC) and urinary hydroxyproline excretion (HOP/Cr). Multivariate regression analysis showed no correlation between parameters of bone turnover (WBR, OC, HOP/Cr) and both femoral and vertebral bone density; the latter being negatively correlated only with the years elapsed since menopause (R2 = 0.406). Treatment with sCT resulted in a significant increase of vertebral BMC in the 53 patients taken as a whole group (+/- 7%, P less than 0.001). When the results obtained in HTOP and NTOP were analyzed separately, only those with HTOP showed a marked increment of spinal BMC (+22%, P less than 0.001), NTOP subjects neither gained nor lost bone mineral during the study. Femoral BMC decreased in the whole group after sCT therapy (-3%, P less than 0.003). However, HTOP patients maintained initial BMC values, whereas those with NTOP lost a significant amount of bone during the study period (-5%, P less than 0.001). The increase of vertebral bone mass was associated with a marked depression of bone turnover detectable in both subsets of patients and in the whole group. In conclusion: (a) assessment of bone turnover cannot help predict the severity of bone loss in postmenopausal osteoporosis; (b) calcitonin therapy appears to be particularly indicated for patients with high-turnover osteoporosis, resulting in a net gain of bone mineral in the axial skeleton and a slowing of bone loss in the appendicular bones.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Austin L. A., Heath H., 3rd Calcitonin: physiology and pathophysiology. N Engl J Med. 1981 Jan 29;304(5):269–278. doi: 10.1056/NEJM198101293040505. [DOI] [PubMed] [Google Scholar]
- Binstock M. L., Mundy G. R. Effect of calcitonin and glutocorticoids in combination on the hypercalcemia of malignancy. Ann Intern Med. 1980 Aug;93(2):269–272. doi: 10.7326/0003-4819-93-2-269. [DOI] [PubMed] [Google Scholar]
- Brown J. P., Delmas P. D., Malaval L., Edouard C., Chapuy M. C., Meunier P. J. Serum bone Gla-protein: a specific marker for bone formation in postmenopausal osteoporosis. Lancet. 1984 May 19;1(8386):1091–1093. doi: 10.1016/s0140-6736(84)92506-6. [DOI] [PubMed] [Google Scholar]
- Caniggia A., Gennari C., Bencini M., Cesari L., Borrello G. Calcium metabolism and 47calcium kinetics before and after long-term thyrocalcitonin treatment in senile osteoporosis. Clin Sci. 1970 Apr;38(4):397–407. doi: 10.1042/cs0380397. [DOI] [PubMed] [Google Scholar]
- Caniggia A., Vattimo A. Kinetics of 99mtechnetium-tin-methylene-diphosphonate in normal subjects and pathological conditions: a simple index of bone metabolism. Calcif Tissue Int. 1980;30(1):5–13. doi: 10.1007/BF02408600. [DOI] [PubMed] [Google Scholar]
- Civitelli R., Agnusdei D., Nardi P., Zacchei F., Avioli L. V., Gennari C. Effects of one-year treatment with estrogens on bone mass, intestinal calcium absorption, and 25-hydroxyvitamin D-1 alpha-hydroxylase reserve in postmenopausal osteoporosis. Calcif Tissue Int. 1988 Feb;42(2):77–86. doi: 10.1007/BF02556338. [DOI] [PubMed] [Google Scholar]
- Cohn S. H., Dombrowski W., Hauser W., Klopper J., Atkins H. L. Effects of porcine calcitonin on calcium metabolism in osteoporosis. J Clin Endocrinol Metab. 1971 Nov;33(5):719–728. doi: 10.1210/jcem-33-5-719. [DOI] [PubMed] [Google Scholar]
- Delmas P. D., Wahner H. W., Mann K. G., Riggs B. L. Assessment of bone turnover in postmenopausal osteoporosis by measurement of serum bone Gla-protein. J Lab Clin Med. 1983 Oct;102(4):470–476. [PubMed] [Google Scholar]
- Epstein S., Poser J., McClintock R., Johnston C. C., Jr, Bryce G., Hui S. Differences in serum bone GLA protein with age and sex. Lancet. 1984 Feb 11;1(8372):307–310. doi: 10.1016/s0140-6736(84)90360-x. [DOI] [PubMed] [Google Scholar]
- Fogelman I., Bessent R. G., Beastall G., Boyle I. T. Estimation of skeletal involvement in primary hyperparathyroidism. Use of 24-hour whole-body retention of technetium-99m diphosphonate. Ann Intern Med. 1980 Jan;92(1):65–67. doi: 10.7326/0003-4819-92-1-65. [DOI] [PubMed] [Google Scholar]
- Fogelman I., Bessent R. G., Cohen H. N., Hart D. M., Lindsay R. Skeletal uptake of diphosphonate. Method for prediction of post-menopausal osteoporosis. Lancet. 1980 Sep 27;2(8196):667–670. doi: 10.1016/s0140-6736(80)92707-5. [DOI] [PubMed] [Google Scholar]
- Fogelman I., Bessent R. G., Turner J. G., Citrin D. L., Boyle I. T., Greig W. R. The use of whole-body retention of Tc-99m diphosphonate in the diagnosis of metabolic bone disease. J Nucl Med. 1978 Mar;19(3):270–275. [PubMed] [Google Scholar]
- Fogelman I., Bessent R. Age-related alterations in skeletal metabolism--24-hr whole-body retention of diphosphonate in 250 normal subjects: concise communication. J Nucl Med. 1982 Apr;23(4):296–300. [PubMed] [Google Scholar]
- Fogelman I. Skeletal uptake of diphosphonate: a review. Eur J Nucl Med. 1980 Dec;5(6):473–476. doi: 10.1007/BF00252034. [DOI] [PubMed] [Google Scholar]
- Frost H. M. Treatment of osteoporoses by manipulation of coherent bone cell populations. Clin Orthop Relat Res. 1979 Sep;(143):227–244. [PubMed] [Google Scholar]
- Gallagher J. C., Goldgar D., Moy A. Total bone calcium in normal women: effect of age and menopause status. J Bone Miner Res. 1987 Dec;2(6):491–496. doi: 10.1002/jbmr.5650020605. [DOI] [PubMed] [Google Scholar]
- Genant H. K., Cann C. E., Ettinger B., Gordan G. S. Quantitative computed tomography of vertebral spongiosa: a sensitive method for detecting early bone loss after oophorectomy. Ann Intern Med. 1982 Nov;97(5):699–705. doi: 10.7326/0003-4819-97-5-699. [DOI] [PubMed] [Google Scholar]
- Gruber H. E., Ivey J. L., Baylink D. J., Matthews M., Nelp W. B., Sisom K., Chesnut C. H., 3rd Long-term calcitonin therapy in postmenopausal osteoporosis. Metabolism. 1984 Apr;33(4):295–303. doi: 10.1016/0026-0495(84)90187-2. [DOI] [PubMed] [Google Scholar]
- Haddad J. G., Jr, Birge S. J., Avioli L. V. Effects of prolonged thyrocalcitonin administration on Paget's disease of bone. N Engl J Med. 1970 Sep 10;283(11):549–555. doi: 10.1056/NEJM197009102831101. [DOI] [PubMed] [Google Scholar]
- Hansson T., Roos B. Age changes in the bone mineral of the lumbar spine in normal women. Calcif Tissue Int. 1986 May;38(5):249–251. doi: 10.1007/BF02556602. [DOI] [PubMed] [Google Scholar]
- Heaney R. P., Recker R. R., Saville P. D. Menopausal changes in bone remodeling. J Lab Clin Med. 1978 Dec;92(6):964–970. [PubMed] [Google Scholar]
- Hosking D. J. Calcitonin and diphosphonate in the treatment of Paget's disease of bone. Metab Bone Dis Relat Res. 1981;3(4-5):317–326. doi: 10.1016/0221-8747(81)90048-5. [DOI] [PubMed] [Google Scholar]
- Hui S. L., Slemenda C. W., Johnston C. C., Appledorn C. R. Effects of age and menopause on vertebral bone density. Bone Miner. 1987 Apr;2(2):141–146. [PubMed] [Google Scholar]
- Hyldstrup L., McNair P., Finn Jensen G., Borg Mogensen N., Transbøl I. Measurements of whole body retention of diphosphonate and other indices of bone metabolism in 125 normals: dependency on age, sex and glomerular filtration. Scand J Clin Lab Invest. 1984 Dec;44(8):673–678. doi: 10.3109/00365518409083629. [DOI] [PubMed] [Google Scholar]
- Hyldstrup L., Mogensen N., Jensen G. F., McNair P., Transbøl I. Urinary 99m-Tc-diphosphonate excretion as a simple method to quantify bone metabolism. Scand J Clin Lab Invest. 1984 Apr;44(2):105–109. doi: 10.3109/00365518409161390. [DOI] [PubMed] [Google Scholar]
- Jowsey J., Riggs B. L., Kelly P. J., Hoffman D. L. Calcium and salmon calcitonin in treatment of osteoporosis. J Clin Endocrinol Metab. 1978 Sep;47(3):633–639. doi: 10.1210/jcem-47-3-633. [DOI] [PubMed] [Google Scholar]
- Marie P. J., Caulin F. Mechanisms underlying the effects of phosphate and calcitonin on bone histology in postmenopausal osteoporosis. Bone. 1986;7(1):17–22. doi: 10.1016/8756-3282(86)90147-x. [DOI] [PubMed] [Google Scholar]
- Mazzuoli G. F., Passeri M., Gennari C., Minisola S., Antonelli R., Valtorta C., Palummeri E., Cervellin G. F., Gonnelli S., Francini G. Effects of salmon calcitonin in postmenopausal osteoporosis: a controlled double-blind clinical study. Calcif Tissue Int. 1986 Jan;38(1):3–8. doi: 10.1007/BF02556587. [DOI] [PubMed] [Google Scholar]
- Milhaud G., Talbot J. N., Coutris G. Calcitonin treatment of post-menopausal osteoporosis. Evaluation of efficacy by principal components analysis. Biomedicine. 1975 May;22(3):223–232. [PubMed] [Google Scholar]
- Nordin B. E., Aaron J., Speed R., Crilly R. G. Bone formation and resorption as the determinants of trabecular bone volume in postmenopausal osteoporosis. Lancet. 1981 Aug 8;2(8241):277–279. doi: 10.1016/s0140-6736(81)90526-2. [DOI] [PubMed] [Google Scholar]
- PROCKOP D. J., UDENFRIEND S. A specific method for the analysis of hydroxyproline in tissues and urine. Anal Biochem. 1960 Nov;1:228–239. doi: 10.1016/0003-2697(60)90050-6. [DOI] [PubMed] [Google Scholar]
- Parfitt A. M. Quantum concept of bone remodeling and turnover: implications for the pathogenesis of osteoporosis. Calcif Tissue Int. 1979 Aug 24;28(1):1–5. doi: 10.1007/BF02441211. [DOI] [PubMed] [Google Scholar]
- Parfitt A. M. The coupling of bone formation to bone resorption: a critical analysis of the concept and of its relevance to the pathogenesis of osteoporosis. Metab Bone Dis Relat Res. 1982;4(1):1–6. doi: 10.1016/0221-8747(82)90002-9. [DOI] [PubMed] [Google Scholar]
- Pødenphant J., Johansen J. S., Thomsen K., Riis B. J., Leth A., Christiansen C. Bone turnover in spinal osteoporosis. J Bone Miner Res. 1987 Dec;2(6):497–503. doi: 10.1002/jbmr.5650020606. [DOI] [PubMed] [Google Scholar]
- Reginster J. Y., Denis D., Albert A., Deroisy R., Lecart M. P., Fontaine M. A., Lambelin P., Franchimont P. 1-Year controlled randomised trial of prevention of early postmenopausal bone loss by intranasal calcitonin. Lancet. 1987 Dec 26;2(8574):1481–1483. doi: 10.1016/s0140-6736(87)92619-5. [DOI] [PubMed] [Google Scholar]
- Riggs B. L., Wahner H. W., Dunn W. L., Mazess R. B., Offord K. P., Melton L. J., 3rd Differential changes in bone mineral density of the appendicular and axial skeleton with aging: relationship to spinal osteoporosis. J Clin Invest. 1981 Feb;67(2):328–335. doi: 10.1172/JCI110039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen J. F., Wolin D. A., Finberg L. Immobilization hypercalcemia after single limb fractures in children and adolescents. Am J Dis Child. 1978 Jun;132(6):560–564. doi: 10.1001/archpedi.1978.02120310024004. [DOI] [PubMed] [Google Scholar]
- Sjöberg H. E., Hjern B. Acute treatment with calcitonin in primary hyperparathyroidism and severe hypercalcaemia of other origin. Acta Chir Scand. 1975;141(2):90–95. [PubMed] [Google Scholar]
- Slemenda C., Hui S. L., Longcope C., Johnston C. C. Sex steroids and bone mass. A study of changes about the time of menopause. J Clin Invest. 1987 Nov;80(5):1261–1269. doi: 10.1172/JCI113201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomsen K., Johansen J., Nilas L., Christiansen C. Whole body retention of 99mTc-diphosphonate. Relation to biochemical indices of bone turnover and to total body calcium. Eur J Nucl Med. 1987;13(1):32–35. doi: 10.1007/BF00252643. [DOI] [PubMed] [Google Scholar]
- Thomsen K., Nilas L., Mogensen T., Christiansen C. Determination of bone turnover by urinary excretion of 99mTc-MDP. Eur J Nucl Med. 1986;12(7):342–345. doi: 10.1007/BF00263816. [DOI] [PubMed] [Google Scholar]
- Thomsen K., Riis B., Christiansen C. Effect of estrogen/gestagen and 24R,25-dihydroxyvitamin D3 therapy on bone formation in postmenopausal women. J Bone Miner Res. 1986 Dec;1(6):503–507. doi: 10.1002/jbmr.5650010604. [DOI] [PubMed] [Google Scholar]
- Thomsen K., Rødbro P., Christiansen C. Bone turnover determined by urinary excretion of [99mTc]diphosphonate in the prediction of postmenopausal bone loss. Bone Miner. 1987 Apr;2(2):125–131. [PubMed] [Google Scholar]
- Wener J. A., Gorton S. J., Raisz L. G. Escape from inhibition or resorption in cultures of fetal bone treated with calcitoninand parathyroid hromone. Endocrinology. 1972 Mar;90(3):752–759. doi: 10.1210/endo-90-3-752. [DOI] [PubMed] [Google Scholar]
- Whyte M. P., Bergfeld M. A., Murphy W. A., Avioli L. V., Teitelbaum S. L. Postmenopausal osteoporosis. A heterogeneous disorder as assessed by histomorphometric analysis of Iliac crest bone from untreated patients. Am J Med. 1982 Feb;72(2):193–202. doi: 10.1016/0002-9343(82)90810-5. [DOI] [PubMed] [Google Scholar]
- Yasumura S., Aloia J. F., Gundberg C. M., Yeh J., Vaswani A. N., Yuen K., Lo Monte A. F., Ellis K. J., Cohn S. H. Serum osteocalcin and total body calcium in normal pre- and postmenopausal women and postmenopausal osteoporotic patients. J Clin Endocrinol Metab. 1987 Apr;64(4):681–685. doi: 10.1210/jcem-64-4-681. [DOI] [PubMed] [Google Scholar]


