Abstract
Adherence to cardiac health behaviors is a critical predictor of prognosis in the months following an acute coronary syndrome (ACS). However, there has been minimal concomitant study of multiple nonadherence risk factors, as assessed via record review, structured assessments, and qualitative interviews, among hospitalized ACS patients. Accordingly, we completed an exploratory mixed methods study with 22 individuals who were admitted for ACS and had suboptimal pre-ACS adherence to physical activity, heart-healthy diet, and/or medications, defined by a Medical Outcomes Study Specific Adherence Scale (MOS SAS) score <15/18. During hospitalization, participants underwent quantitative assessments of sociodemographic, medical, and psychological variables, followed by in-depth semi-structured interviews to explore intentions, plans, and perceived barriers related to post-discharge health behavior changes. The MOS SAS was readministered at 3 months and participants were designated as persistently nonadherent (MOS SAS<15; n=9) or newly adherent (n=13). Interviews were transcribed and coded by trained raters via content analysis, and quantitative variables were compared between groups using chi-square analysis and independent-samples t-tests. On our primary qualitative analysis, we found that participants with vaguely described intentions/plans regarding health behavior change, and those who focused on barriers to change that were perceived as static, were more likely to be persistently nonadherent. On exploratory quantitative analyses, greater medical burden, diabetes, depressive symptoms, and low optimism/positive affect at baseline were associated with subsequent post-ACS nonadherence (all p<.05). In conclusion, this appears to be the first study to prospectively examine all of these constructs in hospitalized ACS patients, and we found that specific factors were associated with nonadherence to key health behaviors 3 months later. It may therefore be possible to predict future nonadherence in ACS patients, even during hospitalization, and specific interventions during admission may be indicated to prevent adverse outcomes among patients at highest risk for post-ACS nonadherence.
Keywords: acute coronary syndrome, health behavior, mixed methods, optimism, positive affect
Acute coronary syndromes (ACS)—myocardial infarction or unstable angina—result in one million hospitalizations annually in the U.S. alone (Go et al., 2014). ACS patients who subsequently increase physical activity, follow a low-fat diet, and reliably take medications have substantially lower rates of recurrent events and mortality (Chow et al., 2010; Gehi, Ali, Na, & Whooley, 2007). However, the majority of ACS patients are non-adherent to medication, diet, or activity recommendations (Chow et al., 2010; Lee, Abdullah, Bulgiba, & Zainal Abidin, 2013; Roger et al., 2011). It is critical to promptly identify risk factors for nonadherence to health behaviors in ACS patients.
Patients’ initial post-ACS intentions and plans to change health behaviors likely indicate subsequent adherence. Prior studies examined intention to change health behaviors post-ACS (Blanchard et al., 2003; Reges et al., 2013), but have not performed multiple assessments or gathered detailed information about patients’ characteristics, perceptions, and goals. Only one study interviewed hospitalized ACS patients (Fors, Dudas, & Ekman, 2014), but to our knowledge, none have inquired about patients’ health behavior goals during admission. We completed an exploratory mixed methods study of hospitalized ACS patients who had been suboptimally adherent to heart-healthy diet, activity, and/or medications to assess predictors of subsequent adherence.
Methods
Design
We enrolled ACS patients who had been suboptimally adherent to health behaviors (medications, activity, and/or diet) assessed using the Medical Outcomes Study Specific Adherence Scale [MOS SAS (DiMatteo, Hays, & Sherbourne, 1992)]. During hospitalization for ACS, quantitative assessment and qualitative interviews assessed whether: (i) participants’ intentions/plans regarding health behavior change, (ii) perceived barriers to change, and (iii) baseline characteristics were linked with nonadherence 3 months later. We assessed participants 3 months post-discharge because health behavior adherence over this timeframe is linked to improved oxygen uptake and fewer readmissions (Canyon & Meshgin, 2008; Moholdt et al., 2009).
Study criteria and recruitment
Eligible patients were English-speaking adults hospitalized in an urban academic hospital between March-August 2013 who met established ACS criteria (Bertrand et al., 2000; Theroux & Fuster, 1998). We excluded patients with cognitive deficits (six-item screen [(Callahan, Unverzagt, Hui, Perkins, & Hendrie, 2002)]) or medical conditions precluding interview. Procedures were approved by the hospital’s Institutional Review Board.
Data collection
Participant characteristics and quantitative assessments
Demographic and medical data were obtained at enrollment via self-report and record review. To avoid influencing self-report data through qualitative interview questions/probes, participants first completed quantitative assessments. These measured: (a) baseline health behaviors (MOS SAS-measured diet, activity, and medication adherence over the prior month; suboptimal adherence was defined as <15/18), (b) anxiety and depression (Hospital Anxiety and Depression Scale [HADS (Bjelland, Dahl, Haug, & Neckelmann, 2002)]), (c) optimism (Life Orientation Test-Revised [LOT-R (Scheier, Carver, & Bridges, 1994)]), and (d) positive affect (Positive And Negative Affect Schedule [PANAS (Watson, Clark, & Tellegen, 1988)] ). The MOS SAS was repeated via phone at 3 months, and participants were classified as newly adherent if the follow-up MOS was ≥15; the remainder were classified as persistently nonadherent.
Qualitative interviews
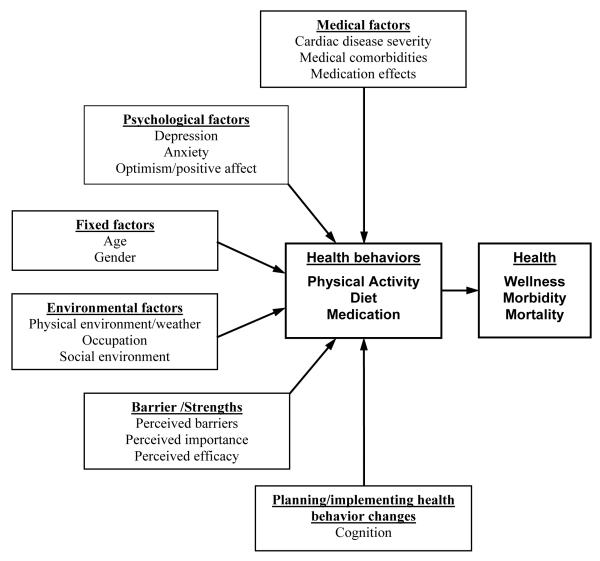
Participants then engaged in semi-structured, hour-long qualitative interviews in the hospital. We followed COREQ quality guidelines (Tong, Sainsbury, & Craig, 2007) and additional techniques to ensure rigor, including supervision from an experienced qualitative researcher (EP), pilot testing, and iterative questioning (Kavalieratos et al., 2014). Figure 1 outlines an adapted model (Bouchard & Shephard, 1994) regarding contributors to post-ACS health behavior adherence covered by the quantitative and interview assessments. Interviews (Table 1) utilized open-ended questions and probes regarding pre-ACS health behaviors, facilitators/barriers to behavior change, and plans for post-ACS health behavior. Patients were typically interviewed following cardiac catheterization (mean 2.55 days post-admission). Interviews were audiotaped, transcribed, and reviewed by study staff for clarity/completeness, and performed until thematic saturation was reached.
Figure 1. Model of contributors to cardiac health behaviors.
Adapted from C. Bouchard and R. J. Shephard (1994), “Physical activity, fitness, and health: The model and key concepts” in Physical Activity, Fitness, and Health: International Proceedings and Consensus Statement, edited by C. Bouchard, R. J. Shephard, and T. Stephens (Champaign, Ill.: Human Kinetics).
Table 1.
Sample questions from qualitative interview guide
| Domain | Sample questions |
|---|---|
| Baseline health behaviors | Before this hospitalization, what did you do to stay healthy? |
|
Probes as required, based
on participant response |
Can you tell me what your typical [exercise routine, diet] was like? Did you take medication regularly before this hospitalization? |
| What sort of [exercising, dieting] have you done in the past? | |
| Were there other ways in which you were physically active (for patients who did not exercise)? |
|
| Can you tell me about a time when you succeeded at [becoming more active, eating a healthy diet, taking medication]? What exactly did you do? |
|
|
| |
| Health goals | After this hospitalization, what will you do to stay healthy? Is there anything that you will change? |
| Of these, which do you think is most important for you to do to stay healthy now? | |
| Do you have any specific ideas about how you might make this change? | |
| Physical activity | Sometimes people with a heart problem like yours want to increase their physical activity. Is that true for you, or not so much? |
| Diet | What are your thoughts about sticking to a low-fat diet (or previously mentioned diet goal) moving forward? |
| Medication | Do you feel like you will need to be more on top of your medications? |
|
| |
|
Past barriers to health
behavior completion |
(From success question) What made it easy? What made it hard? What made it difficult for you to continue? |
| What made it difficult for you to [exercise, diet]? What prevented you from [exercising, eating a healthy diet]? |
|
| Perceived future barriers | Going forward, do you anticipate any difficulties with [becoming more active, eating a healthy diet, taking your medications]? |
Analysis
Qualitative (primary) analysis: Association of plans, perceptions, and barriers with subsequent adherence
A coding framework was generated using directed content analysis (Hsieh & Shannon, 2005). Four content areas were explored: (1) intention to change health behaviors, (2) specificity of behavior change plans, (3) type of plan, and (4) perceived barriers. Transcribed interviews were uploaded into NVivo 10 (QSR International) for content analysis, and coded independently by two researchers (kappa=0.89). Discrepancies were resolved via discussion, transcript review, and arbitration (EP).
Quantitative (exploratory) analysis: Association of baseline variables with subsequent adherence
Baseline characteristics and self-report variables were compared between participants who became adherent at three months, and those who remained nonadherent, using independent-samples t-tests for continuous and chi-square analysis for categorical variables, using Stata 11 (StataCorp: College Station, TX); sample size did not allow multivariate analysis given the risk of overfitting. P<0.05 (two-tailed) was considered significant.
Results
Participant characteristics (Table 2)
Table 2.
Baseline characteristics and psychological assessments
|
Total (n=22) N (%)* |
Persistent nonadherence (n=9) N (%)* |
Post-ACS adherence (n=13) N (%)* |
Test statistic |
P value | |
|---|---|---|---|---|---|
| Demographic variables | |||||
| Age, mean (SD) | 63.9 (12.1) | 68.1 (10.5) | 60.9 (12.6) | t=1.40 | 0.17 |
| Male | 13 (59.1) | 4 (44.4) | 9 (69.2) | χ2=1.35 | 0.25 |
| White | 17 (77.3) | 7 (77.8) | 10 (76.9) | χ2=2.20 | 0.53 |
| Married | 15 (68.2) | 6 (66.7) | 9 (69.2) | χ2=0.21 | 0.90 |
|
| |||||
| Medical variables related to current admission | |||||
| MI admission diagnosis | 9 (40.9) | 4 (44.4) | 5 (38.5) | χ2=0.08 | 0.78 |
| Length of stay, mean (SD) | 3.1 (3.2) | 2 (0.9) | 3.9 (4.0) | t=1.41 | 0.17 |
| Prior ACS | 13 (59.1) | 6 (66.7) | 7 (53.8) | χ2=0.36 | 0.55 |
| Peak troponin, mean (SD) | 0.2 (0.4) | 0.2 (0.4) | 0.2 (0.4) | t=0.002 | 0.99 |
| LVEF, mean (SD) | 0.6 (0.1) | 0.6 (0.1) | 0.6 (0.1) | t=0.49 | 0.63 |
|
| |||||
| Medical history | |||||
| Charlson index, mean (SD) | 1.9 (1.04) | 2.6 (1.1) | 1.5 (0.8) | t=2.51 | 0.02 |
| BMI, mean (SD) | 30.2 (5.3) | 31.5 (6.7) | 29.2 (3.9) | t=0.95 | 0.36 |
| Diabetes mellitus | 9 (40.9) | 6 (66.7) | 3 (23.1) | χ2=4.18 | 0.04 |
| Current smoker | 1 (4.6) | 0 | 1 (7.7) | χ2=0.73 | 0.39 |
| Hyperlipidemia | 18 (81.8) | 7 (77.8) | 11 (84.6) | χ2=0.17 | 0.68 |
| Hypertension | 19 (86.4) | 9 (100) | 10 (76.9) | χ2=2.40 | 0.12 |
|
| |||||
| Medications at discharge | |||||
| ASA | 21 (95.4) | 9 (100) | 12 (92.3) | χ2=0.73 | 0.39 |
| Beta blocker | 21 (95.4) | 9 (100) | 12 (92.3) | χ2=0.73 | 0.39 |
| ACE inhibitor/ARB | 12 (54.6) | 7 (77.8) | 5 (38.5) | χ2=3.32 | 0.07 |
| Antiplatelet agents | 13 (59.1) | 6 (66.7) | 7 (53.8) | χ2=0.36 | 0.55 |
| Statin | 21 (95.4) | 8 (88.9) | 13 (100) | χ2=1.51 | 0.22 |
|
| |||||
| Baseline scores (mean [SD]) | |||||
| MOS SAS Total (out of 18) | 10.6 (2.9) | 9.7 (2.4) | 11.2 (3.1) | t=1.27 | 0.22 |
| MOS SAS Exercise (out of 6) | 1.7 (0.9) | 1.3 (0.7) | 2 (0.9) | χ2=1.84 | 0.08 |
| MOS SAS Diet (out of 6) | 3.5 (1.8) | 2.8 (1.7) | 4 (1.7) | χ2=1.63 | 0.12 |
| MOS SAS Medications (out of 6) | 5.4 (1.4) | 5.6 (1.01) | 5.2 (1.6) | χ2=0.54 | 0.59 |
| LOT-R Total (out of 30) | 24.9 (6.5) | 21.2 (8.8) | 27.4 (2.3) | t=2.43 | 0.03 |
| LOT-R Optimism (out of 15) | 12.5 (3.8) | 10.2 (5.1) | 14 (1.2) | t=2.62 | 0.02 |
| LOT-R Pessimism (out of 15) | 12.4 (3.6) | 11 (4.7) | 13.4 (2.3) | t=1.60 | 0.12 |
| PANAS (out of 50) | 36.7 (9.2) | 30.6 (11) | 40.9 (4.3) | t=3.10 | 0.006 |
| HADS Total (out of 42) | 14.5 (8) | 18.1 (8.2) | 12.1 (7.2) | t=1.83 | 0.08 |
| HADS Anxiety (out of 21) | 9.3 (4.8) | 10.6 (4.4) | 8.4 (5) | t=1.04 | 0.31 |
| HADS Depression (out of 21) | 5.3 (4.3) | 7.6 (4.9) | 3.7 (3.2) | t=2.25 | 0.04 |
Unless otherwise noted.
Note. ACE Inhibitor/ARB=Angiotensin Converting Enzyme Inhibitor / Angiotensin Receptor Blocker; ACS=Acute Coronary Syndrome; ASA=Aspirin; BMI=Body Mass Index; HADS=Hospital Anxiety and Depression Scale; LOT-R=Life Orientation Test Revised; LVEF=Left Ventricular Ejection Fraction; MI=Myocardial Infarction; MOS SAS=Medical Outcomes Study Specific Adherence Scale; PANAS=Positive and Negative Affect Schedule; SD=Standard Deviation
Participants’ mean age was 63.9 +/− 12.1 years; most were white (77%) and male (59%). Among the 22 initially-nonadherent participants, 13 (59%) became adherent at 3 months. Patients who became adherent had greater improvement on MOS SAS (5.7+/−1.0 vs. 2.4+/−1.0; t=2.21; p=.04).
Qualitative outcomes (See Table 3 for representative participant quotes)
Table 3.
Representative quotations for each content area from qualitative interviews
| Intention to change health behaviors |
| • Persistent nonadherers had made more conditional and general statements about their behavior change and cited others as recommending change: |
|
“[The hospital staff] recommend that I go see a nutritionist and I take some sort of post-cardiac
exercise program.” |
| • Participants who subsequently became adherent used direct statements and expressed an internal drive to make change: |
|
“I’m going to be a lot more dedicated to each part of the program. There’s bound to be an
exercise part of it, there’s bound to be a diet part of it. There’s bound to be stress reduction.” |
| Specificity of plans for health behavior change |
| • Participants who became adherers had clear, attainable, and focused goals that were specific about timing (walking 30 minutes a day), and content (e.g., high protein diet). |
|
“I’ve got the exercise bike…thirty minutes of exercise at lunch—at least twenty. I always take the
stairs to work and will continue to do that.” |
| Type of plan |
| • Participants who remained nonadherent had focused on restriction/sacrifice while in the hospital: |
|
“Eating low sodium, staying away from a lot of food… the doctor was saying I really gotta stay
away from the rice, the Chinese, because I love it all… so I have to get away from all that.” |
| • New adherers had focused on addition of foods or new structured group-based activities: |
|
“In September, I will sign up again with the aerobic and weight lifting class…after my daughter
leaves next week, I will sign up for yoga until September.” |
| Perceived barriers to health behavior completion |
| • Those who remained nonadherers had identified static factors over which they perceived little control: |
|
“You know I got the arthritis. I’m seventy years old. I’m not going to go out and go crazy…with
exercises and stuff.” |
| • New adherers acknowledged logistic issues but expressed specific plans to address these barriers: |
|
“I won’t be able to exercise much because of work, but I have my exercise ball that I brought up
with me so I’ll use it…Make sure that I get some exercise in three times a week.” |
Participants who were persistent nonadherers had made more conditional or uncertain statements about their intention to change (e.g., I hope, I should), and the drive to change often came from others. Participants who became adherent discussed behavior change using non-ambiguous action statements (e.g., I have to, I am going to), and expressed personal commitment (e.g., I have made a deal with myself).
Persistent nonadherers made general statements regarding plans to change (I will eat less, I want to start exercising). Conversely, participants who became adherers had clear and attainable goals that were specific about timing (e.g., walking 30 minutes daily) and content (e.g., high-protein diet).
Participants who remained nonadherent focused on restriction/sacrifice, especially regarding diet (e.g., I will avoid bad foods, I will eat less salt). New adherers focused on substitutions or addition (e.g., vegetables instead of meat; more fish) and on structured group-based activities such as exercise classes or cardiac rehabilitation.
Those who remained nonadherers had identified static factors over which they perceived little control, such as chronic/pre-existing medical conditions, as behavior change barriers. While new adherers acknowledged logistic issues (e.g., work, weather) as potential barriers to activity and healthy eating, there were far fewer statements that signaled resignation.
Quantitative Outcomes
No demographic variables were associated with subsequent adherence (Table 2). In contrast, greater medical morbidity (Charlson Comorbidity Index [(Charleson, Pompei, Ales, & MacKenzie, 1987)]) and diabetes were associated with persistent nonadherence. Furthermore, lower baseline depression (HADS), and greater optimism (LOT-R) and positive affect (PANAS) were associated with new adherence.
Discussion
To our knowledge, this is the first mixed methods study to concurrently examine numerous sociodemographic and psychological variables’ association with health behaviors in hospitalized ACS patients at high risk for nonadherence. Patients who were unsure about their ability or willingness to change, had less specific plans about behavior change, or cited others recommending change typically remained nonadherent. These findings are consistent with studies in other cohorts (Blanchard et al., 2003; Lourenco, Rodrigues, Spana, Gallani, & Cornelio, 2012; Petter, Blanchard, Kemp, Mazoff, & Ferrier, 2009), but the vulnerable nature of this study’s population has substantial clinical significance.
In addition, participants who identified fixed characteristics perceived as barriers (age, comorbidities) were less likely to become adherent, as were those who focused on sacrifice/removal of foods. The latter may represent the costly psychological effects of ‘losing’ an enjoyed item with no compensation/replacement (Reach, 2013), or it may simply have signaled that such patients had less extensively considered alternative options.
On quantitative analyses, medical comorbidity, diabetes, and depressive symptoms predicted nonadherence, consistent with prior literature in ACS (Cramer, 2004; Hernandez-Ronquillo, Tellez-Zenteno, Garduno-Espinosa, & Gonzalez-Acevez, 2003; Ziegelstein et al., 2000). A novel finding was that optimism and positive affect were associated with new adherence. Positive psychological constructs, independent of depression, have been linked to physical activity and healthy eating (Giltay, Geleijnse, Zitman, Buijsse, & Kromhout, 2007; Kelloniemi, Ek, & Laitinen, 2005; Tinker et al., 2007) and optimism has been prospectively associated with superior cardiac outcomes (Rasmussen, Scheier, & Greenhouse, 2009; Tindle, Davis, & Kuller, 2010). However, this appears to be the first study identifying connections between optimism and health behaviors post-ACS.
Because post-ACS nonadherence is associated with morbidity and mortality, it is critical to identify high-risk patients during hospitalization. One major implication of this study is that—even during hospitalization—specific factors identify patients as high-risk for nonadherence to key post-ACS health behaviors.
Regarding limitations, this exploratory study occurred at an academic medical center, and the sample size limited power to detect between-group differences. However, several significant associations emerged on quantitative analysis, and thematic saturation was observed on qualitative analysis, consistent with studies in smaller samples (Abramsohn et al., 2013; Guest, Bruce, & Johnson, 2006). Though a small change in MOS SAS could result in conversion to new adherer status, mean change in new adherers was six points, a clinically meaningful change.
In conclusion, among ACS patients with suboptimal baseline adherence, specific factors during hospitalization could predict post-ACS health behavior nonadherence. Clinical teams could target behavior change for these patients at highest risk of dangerous nonadherence.
References
- Abramsohn EM, Decker C, Garavalia B, Garavalia L, Gosch K, Krumholz HM, Lindau ST. “I’m not just a heart, i’m a whole person here”: a qualitative study to improve sexual outcomes in women with myocardial infarction. Journal of the American Heart Association. 2013;2(4):e000199. doi: 10.1161/JAHA.113.000199. doi: 10.1161/JAHA.113.000199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertrand ME, Simoons ML, Fox KA, Wallentin LC, Hamm CW, McFadden E, Ruzyllo W. Management of acute coronary syndromes: acute coronary syndromes without persistent ST segment elevation; recommendations of the Task Force of the European Society of Cardiology. European Heart Journal. 2000;21(17):1406–1432. doi: 10.1053/euhj.2000.2301. doi: 10.1053/euhj.2000.2301. [DOI] [PubMed] [Google Scholar]
- Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. Journal of Psychosomatic Research. 2002;52(2):69–77. doi: 10.1016/s0022-3999(01)00296-3. doi: S0022399901002963 [pii] [DOI] [PubMed] [Google Scholar]
- Blanchard CM, Courneya KS, Rodgers WM, Fraser SN, Murray TC, Daub B, Black B. Is the theory of planned behavior a useful framework for understanding exercise adherence during phase II cardiac rehabilitation? Journal of Cardiopulmonary Rehabilitation. 2003;23(1):29–39. doi: 10.1097/00008483-200301000-00007. [DOI] [PubMed] [Google Scholar]
- Bouchard C, Shephard RJ. Physical activity, fitness, and health: The model and key concepts. In: Bouchard C, Shephard RJ, Stephens T, editors. Physical Activity, Fitness, and Health: International Proceedings and Consensus Statement. Hukan Kinectics; Champaign, IL: 1994. [Google Scholar]
- Callahan CM, Unverzagt FW, Hui SL, Perkins AJ, Hendrie HC. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Medical Care. 2002;40(9):771–781. doi: 10.1097/00005650-200209000-00007. doi: 10.1097/01.MLR.0000024610.33213.C8. [DOI] [PubMed] [Google Scholar]
- Canyon S, Meshgin N. Cardiac rehabilitation - reducing hospital readmissions through community based programs. Australian Family Physician. 2008;37(7):575–577. [PubMed] [Google Scholar]
- Chow CK, Jolly S, Rao-Melacini P, Fox KA, Anand SS, Yusuf S. Association of diet, exercise, and smoking modification with risk of early cardiovascular events after acute coronary syndromes. Circulation. 2010;121(6):750–758. doi: 10.1161/CIRCULATIONAHA.109.891523. doi: 10.1161/CIRCULATIONAHA.109.891523. [DOI] [PubMed] [Google Scholar]
- Cramer JA. A systematic review of adherence with medications for diabetes. Diabetes Care. 2004;27(5):1218–1224. doi: 10.2337/diacare.27.5.1218. [DOI] [PubMed] [Google Scholar]
- DiMatteo MR, Hays RD, Sherbourne CD. Adherence to cancer regimens: implications for treating the older patient. Oncology. 1992;6(2 Suppl):50–57. [PubMed] [Google Scholar]
- Fors A, Dudas K, Ekman I. Life is lived forwards and understood backwards--experiences of being affected by acute coronary syndrome: a narrative analysis. International Journal of Nursing Studies. 2014;51(3):430–437. doi: 10.1016/j.ijnurstu.2013.06.012. doi: 10.1016/j.ijnurstu.2013.06.012. [DOI] [PubMed] [Google Scholar]
- Gehi AK, Ali S, Na B, Whooley MA. Self-reported medication adherence and cardiovascular events in patients with stable coronary heart disease: the heart and soul study. Archives of Internal Medicine. 2007;167(16):1798–1803. doi: 10.1001/archinte.167.16.1798. doi: 10.1001/archinte.167.16.1798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giltay EJ, Geleijnse JM, Zitman FG, Buijsse B, Kromhout D. Lifestyle and dietary correlates of dispositional optimism in men: The Zutphen Elderly Study. Journal of Psychosomatic Research. 2007;63(5):483–490. doi: 10.1016/j.jpsychores.2007.07.014. doi: 10.1016/j.jpsychores.2007.07.014. [DOI] [PubMed] [Google Scholar]
- Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, Stroke Statistics S. Heart disease and stroke statistics--2014 update: a report from the american heart association. Circulation. 2014;129(3):e28–e292. doi: 10.1161/01.cir.0000441139.02102.80. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guest G, Bruce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field Methods. 2006;18:59–82. [Google Scholar]
- Hernandez-Ronquillo L, Tellez-Zenteno JF, Garduno-Espinosa J, Gonzalez-Acevez E. Factors associated with therapy noncompliance in type-2 diabetes patients. Salud Pública de México. 2003;45(3):191–197. doi: 10.1590/s0036-36342003000300008. [DOI] [PubMed] [Google Scholar]
- Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qualitative Health Research. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- Kavalieratos D, Mitchell EM, Carey TS, Dev S, Biddle AK, Reeve BB, Weinberger M. “Not the ‘grim reaper service’”: an assessment of provider knowledge, attitudes, and perceptions regarding palliative care referral barriers in heart failure. Journal of the American Heart Association. 2014;3(1):e000544. doi: 10.1161/JAHA.113.000544. doi: 10.1161/JAHA.113.000544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelloniemi H, Ek E, Laitinen J. Optimism, dietary habits, body mass index and smoking among young Finnish adults. Appetite. 2005;45(2):169–176. doi: 10.1016/j.appet.2005.05.001. doi: 10.1016/j.appet.2005.05.001. [DOI] [PubMed] [Google Scholar]
- Lee WL, Abdullah KL, Bulgiba AM, Zainal Abidin I. Prevalence and predictors of patient adherence to health recommendations after acute coronary syndrome: data for targeted interventions? European Journal of Cardiovascular Nursing. 2013;12(6):512–520. doi: 10.1177/1474515112470056. doi: 10.1177/1474515112470056. [DOI] [PubMed] [Google Scholar]
- Lourenco LB, Rodrigues RC, Spana TM, Gallani MC, Cornelio ME. Action and coping plans related to the behavior of adherence to drug therapy among coronary heart disease outpatients. Revista Latino-Americana de Enfermagem. 2012;20(5):821–829. doi: 10.1590/s0104-11692012000500002. [DOI] [PubMed] [Google Scholar]
- Moholdt TT, Amundsen BH, Rustad LA, Wahba A, Lovo KT, Gullikstad LR, Slordahl SA. Aerobic interval training versus continuous moderate exercise after coronary artery bypass surgery: a randomized study of cardiovascular effects and quality of life. American Heart Journal. 2009;158(6):1031–1037. doi: 10.1016/j.ahj.2009.10.003. doi: 10.1016/j.ahj.2009.10.003. [DOI] [PubMed] [Google Scholar]
- Petter M, Blanchard C, Kemp KA, Mazoff AS, Ferrier SN. Correlates of exercise among coronary heart disease patients: review, implications and future directions. European Journal of Cardiovascular Prevention. 2009;16(5):515–526. doi: 10.1097/HJR.0b013e3283299585. doi: 10.1097/HJR.0b013e3283299585. [DOI] [PubMed] [Google Scholar]
- Rasmussen HN, Scheier MF, Greenhouse JB. Optimism and physical health: a meta-analytic review. Annals of Behavioral Medicine. 2009;37(3):239–256. doi: 10.1007/s12160-009-9111-x. doi: 10.1007/s12160-009-9111-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reach G. A psychophysical account of patient non-adherence to medical prescriptions. The case of insulin dose adjustment. Diabetes & Metabolism. 2013;39(1):50–55. doi: 10.1016/j.diabet.2012.08.009. doi: 10.1016/j.diabet.2012.08.009. [DOI] [PubMed] [Google Scholar]
- Reges O, Vilchinsky N, Leibowitz M, Khaskia A, Mosseri M, Kark JD. Illness cognition as a predictor of exercise habits and participation in cardiac prevention and rehabilitation programs after acute coronary syndrome. BMC Public Health. 2013;13:956. doi: 10.1186/1471-2458-13-956. doi: 10.1186/1471-2458-13-956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roger VL, Go AS, Lloyd-Jones DM, Adams RJ, Berry JD, Brown TM, Wylie-Rosett J. Heart disease and stroke statistics--2011 update: a report from the American Heart Association. Circulation. 2011;123(4):e18–e209. doi: 10.1161/CIR.0b013e3182009701. doi: 10.1161/CIR.0b013e3182009701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the Life Orientation Test. Journal of Personality and Social Psychology. 1994;67(6):1063–1078. doi: 10.1037//0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- Shenton AK. Strategies for ensuring trustworthiness in qualitative research projects. Education and Information Technologies. 2004;22:63–76. [Google Scholar]
- Theroux P, Fuster V. Acute coronary syndromes: unstable angina and non-Q-wave myocardial infarction. Circulation. 1998;97(12):1195–1206. doi: 10.1161/01.cir.97.12.1195. [DOI] [PubMed] [Google Scholar]
- Tindle H, Davis E, Kuller L. Attitudes and cardiovascular disease. Maturitas. 2010;67(2):108–113. doi: 10.1016/j.maturitas.2010.04.020. doi: 10.1016/j.maturitas.2010.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tinker LF, Rosal MC, Young AF, Perri MG, Patterson RE, Van Horn L, Wu L. Predictors of dietary change and maintenance in the Women’s Health Initiative Dietary Modification Trial. Journal of the American Dietetic Association. 2007;107(7):1155–1166. doi: 10.1016/j.jada.2007.04.010. doi: 10.1016/j.jada.2007.04.010. [DOI] [PubMed] [Google Scholar]
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. International Journal for Quality in Health Care. 2007;19(6):349–357. doi: 10.1093/intqhc/mzm042. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. Journal of Personality and Social Psychology. 1988;54(6):1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Ziegelstein RC, Fauerbach JA, Stevens SS, Romanelli J, Richter DP, Bush DE. Patients with depression are less likely to follow recommendations to reduce cardiac risk during recovery from a myocardial infarction. Archives of Internal Medicine. 2000;160(12):1818–1823. doi: 10.1001/archinte.160.12.1818. doi: ioi90446 [pii] [DOI] [PubMed] [Google Scholar]