Abstract
Purpose
One goal in repairing Zone 1 flexor digitorum profundus (FDP) injuries is to create a tendon-bone construct strong enough to allow early rehabilitation while minimizing morbidity. This study introduces an alternative all-inside suture repair technique and compares it biomechanically with pull-out suture and double suture anchor repairs.
Methods
Repairs were performed on thirty cadaver fingers. In all-inside suture repairs (n=8), the FDP tendon was attached to bone with two 3-0 Ethibond sutures and tied over the dorsal aspect of distal phalanx. Pull-out suture repairs (n=8) were performed with 2-0 Prolene suture and tied over a dorsal button. There were two suture anchor repair groups: Arthrex Micro Corkscrew anchors preloaded with 2-0 FiberWire suture (n=7) and Depuy Micro Mitek anchors preloaded with 3-0 Orthocord suture (n=7). Repair constructs were tested using a servohydraulic materials testing system and loaded until the repair lost 75% of its strength.
Results
There were no statistically significant differences in tensile stiffness, ultimate load, or work to failure between the repairs. Failure mode was suture stretch and gap formation >2mm at the repair site for all pull-out suture repairs and 7 of 8 all-inside suture repairs. Two of the Arthrex Micro Corkscrew repairs and five of the Depuy Micro Mitek repairs failed by anchor pull out.
Conclusions
This cadaveric biomechanical study showed no difference in tensile stiffness, ultimate load, and work to failures between an all-inside suture repair technique for zone 1 FDP repairs and previously described pull-out suture and suture anchor repair techniques. The all-inside suture technique also has the advantages of avoiding an external button and the cost of anchors. Therefore, it should be considered as an alternative to other techniques.
Clinical Relevance
This study introduces a new FDP reattachment technique that avoids some of the complications of current techniques.
Keywords: flexor digitorum profundus avulsion, flexor digitorum profundus repair, flexor tendon repair, tendon attachment to bone
Introduction
Zone I flexor digitorum profundus (FDP) tendon injuries often require advancing and attaching the tendon stump to the distal phalanx. When performing this repair, one goal is to produce a tendon-bone construct strong enough to allow early rehabilitation while minimizing short and long-term morbidity. Although multiple techniques for reattachment have been described, each has inherent limitations (1).
A commonly used method of zone 1 flexor tendon repair involves a pull-out suture (2). This suture is advanced through the nail and tied over a button. Problems with this technique include patient tolerance and concerns about infection (3). Suture anchor repairs are another described repair method. Several studies have compared the biomechanical properties of suture anchor repairs with the pull-out suture repair (1, 4, 5). However, a cadaveric study (6) suggested that anchors might be contraindicated in osteoporotic bone due to increased failure through anchor pull out. Concerns about anchor pull out, dorsal anchor penetration in smaller digits, intra-articular anchor placement, and anchor cost suggest the need for other alternative methods. A recent review article concluded that, based on the current available literature, neither the pull- out suture repair nor the anchor repair can be universally recommended as the optimal treatment for zone I FDP avulsions (7).
This biomechanical cadaveric study introduced an alternative all-inside suture technique for the repair of zone 1 FDP avulsions. This technique, which has not been described previously in the literature, involves reattaching tendon to bone with sutures that are pulled through the distal phalanx and tied dorsally with the suture knot buried within the terminal extensor tendon. This study biomechanically compared the all-inside suture repair to pull-out suture and suture anchor repairs in terms of tensile strength, ultimate load, and work to failure. It was hypothesized that the all-inside suture technique would provide at least equivalent strength to previously described methods.
Materials and Methods
Materials
We obtained 36 index, middle, and ring fingers from 6 adult (4 female and 2 male) cadavers and randomly selected 30 for testing. The cadavers were preserved lightly with formaldehyde and were stored at −20°C. Donor ages ranged from 70 to 92 years (mean 81 years). None of the donors had gross upper extremity abnormalities or known histories of musculoskeletal illness.
Prior to testing, hands were thawed to room temperature. The distal phalanges of the index, middle, and ring fingers were disarticulated at the distal interphalangeal joint with the terminal insertion of the FDP tendon intact. The FDP tendon was transected in the palm 5 centimeters proximal its insertion and dissected from its connections to the proximal and middle phalanges including the vincula and volar plate. Nails, skin, and the majority of subcutaneous tissue were removed from each distal phalanx.
FDP reattachment procedures
FDP tendons were transected at their insertion sites and reattached to bone using one of four techniques: 1.) pull-out 2-0 Prolene suture (Ethicon, Somerville, NJ) with a 14mm polypropylene dorsal button (Ethicon, Somerville, NJ), 2.) two Arthrex Micro Corkscrew Anchors (Arthrex, Naples, FL) with 2-0 FiberWire sutures, 3.) two DePuy Mitek Micro Anchors (DePuy Mitek, Raynham, MA) with 3-0 Orthocord sutures, or 4.) 3-0 Ethibond (Ethicon, Somerville, NJ) all-inside suture technique. A single surgeon performed all repairs.
The pull-out repair used two 2-0 Prolene sutures. The first suture was passed using a modified Kessler technique from the radial one-fourth of the transected tendon to the ulnar one-fourth of the tendon. The second suture was passed using a modified Kessler technique from the ulnar to the radial aspect of the tendon. Care was taken not to cut the first suture when the second suture was placed. Stitches were placed so the transverse limbs were one centimeter from the transected end of the tendon. Two Keith needles were drilled from volar to dorsal in the distal phalanx through the central portion of the bone in the region of the sterile matrix. A bony bridge was left between the needles. The prolene sutures were passed through the bone with Keith needles and tied over a button using four knots.
The suture anchor repairs were completed with either two Mitek Micro anchors preloaded with 3-0 Orthocord sutures or two Arthrex Micro Corkscrew anchors preloaded with 2-0 Fiberwire sutures in each digit. Anchors were placed at the radial and ulnar aspects of the FDP insertion site and angled 30 degrees proximally using the drill bits included in the package. The two suture strands from each anchor were placed along the tendon edges using the MGH/ modified Becker technique (8). The stitches crossed three times on each side and were tied on the tendon edges 15mm proximal to the FDP insertion site using four knots.
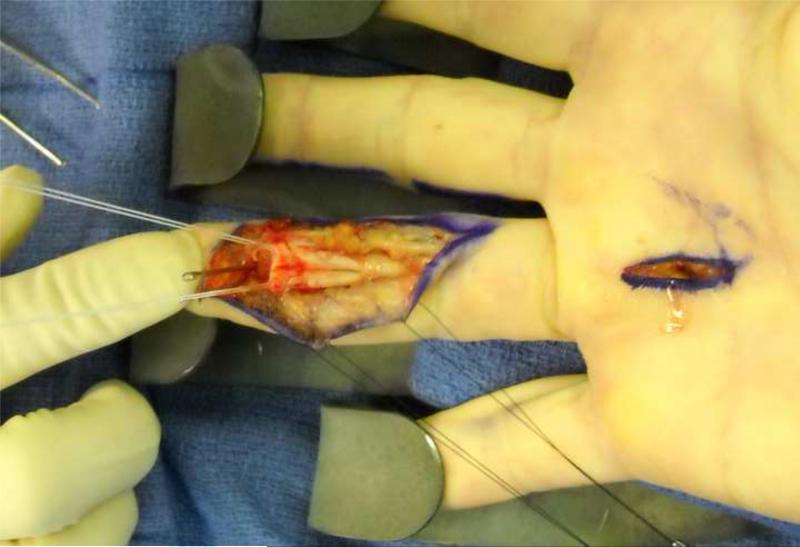
The all-inside suture repairs were performed with two 3-0 Ethibond sutures. Stitches were placed using the MGH/ modified Becker method along the radial and ulnar tendon aspects. The stitches crossed three times on each side starting 15mm proximal to the transected tendon and then exited distally. Two Keith needles were drilled from volar to dorsal through the distal phalanx, exiting proximal to the nail matrix. Lack of articular penetration was verified by direct visualization. The sutures were pulled through the bone with the Keith needles and tied directly over the distal phalanx within the extensor tendon insertion using four knots (Figures 1a and 1b).
Figure 1.
Clinical example of the all-inside suture technique with A) Ethibond sutures placed in tendon and Keith needles in position and B) at the initiation of the pull through of the sutures.
Mechanical Testing
The repaired constructs were tested at room temperature using an Instron DynaMight 8841 servohydraulic materials testing system (Instron; Norwood, MA). Eight of the 30 constructs were tested immediately after the repair was performed. The other 22 constructs were frozen at −20°C after repair and then thawed to room temperature for testing. No construct underwent more than one freeze-thaw cycle after repair.
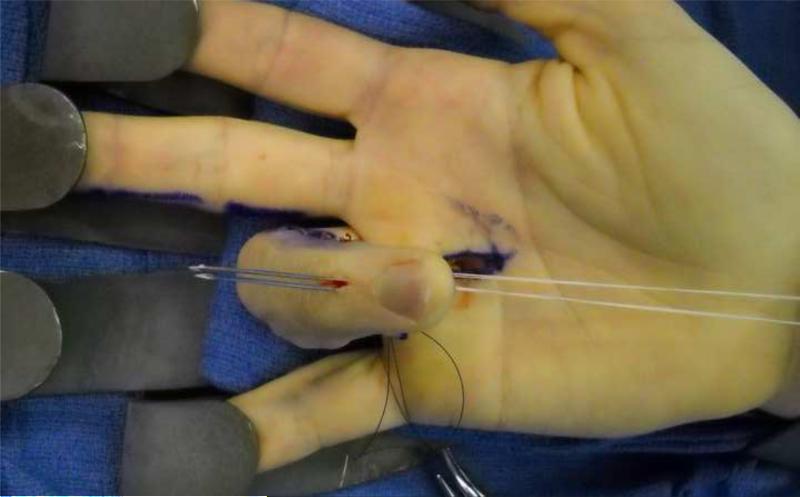
In preparation for testing, sandpaper was affixed with cyanoacrylate to the distal 3 millimeters of the distal phalanx and to the proximal 10 millimeters of the tendon stump. Both the distal phalanx and the proximal tendon were held in pressure clamps that were hand tightened. Care was taken not to interfere with any of the repaired interfaces during preparation (Figure 2).
Figure 2.
Mechanical Testing Setup with all-inside suture repair. Sandpaper was affixed with cyanoacrylate to the distal 3 millimeters of the distal phalanx and to the proximal 10 millimeters of the tendon stump. Pressure clamps were used to secure the proximal end of the tendon and the distal end of the distal phalanx.
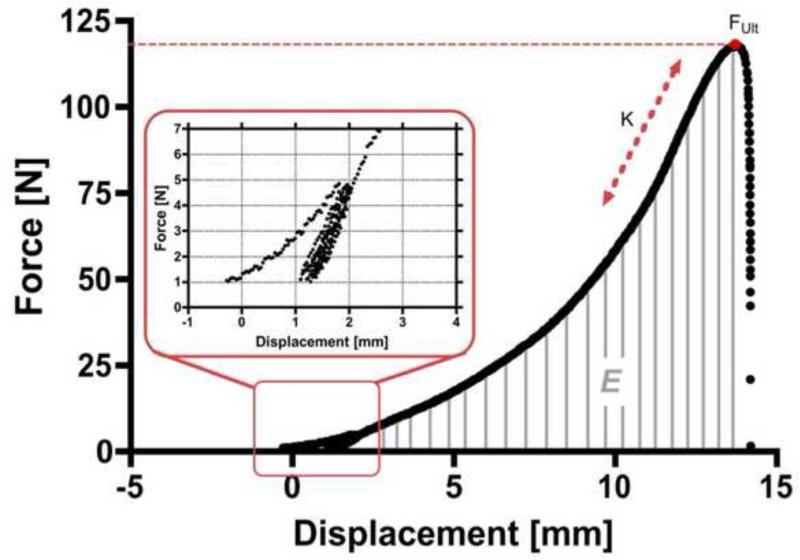
For each construct, the samples were loaded at a rate of 0.1mm/ sec until the load measured 1N. The samples were preconditioned using five cycles at 1-5 N tension at a rate of 0.375 mm/sec. Preconditioning was done to minimize changes in tendon elongation during subsequent tests since tendons are viscoelastic. A similar preconditioning protocol was used in previous studies (6). After preconditioning, the sample was loaded at a rate of 0.375mm/sec on a single displacement ramp until the repair lost 75% of its ultimate strength, which was the highest strength measured by the Instron machine for each sample. Seventy-five percent was chosen based on preliminary testing. During preliminary testing, one sample from each repair type was tested either until the repair lost either 75% or 100% of its ultimate strength. All preliminary samples retrieved after the repairs lost 75% of their ultimate strength showed gapping of >2mm at the bone-tendon junction. The direction of loading was parallel to the shaft and perpendicular to the base of the distal phalanx. The stiffness (K), ultimate force (FUlt) and work to failure (E) were measured (Figure 3). Additionally, mode of failure was noted. When suture breakage and anchor pull out were not seen, the gap between the volar bone and the FDP tendon was measured with a ruler (Fine Science Tools; Foster City, CA).
Figure 3.
Force versus Displacement Curve. Representative force versus displacement curve depicting the applied preload (inset) and the stiffness (K), ultimate force (FUlt) and work to failure (E).
Statistical Analysis
All statistics were performed using Prism v4.0c (Graphpad Software; La Jolla, CA). Normality of the data was tested using a D'Agostino & Pearson omnibus normality test. The tensile stress and ultimate load were found to be non-normally distributed. Therefore, a Kruskal-Wallis nonparametric analysis of variance (ANOVA) test was used to compare the tensile stress and ultimate load between the repair groups. Since the energy to failure was normally distributed, a one-way ANOVA test was used for this comparison.
Results
Failure Modes
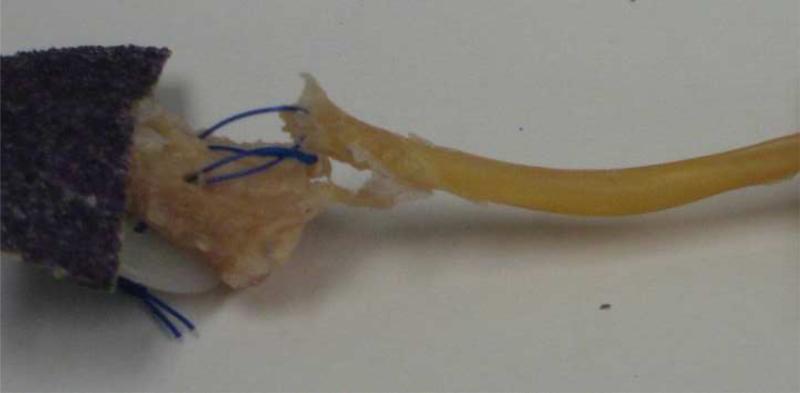
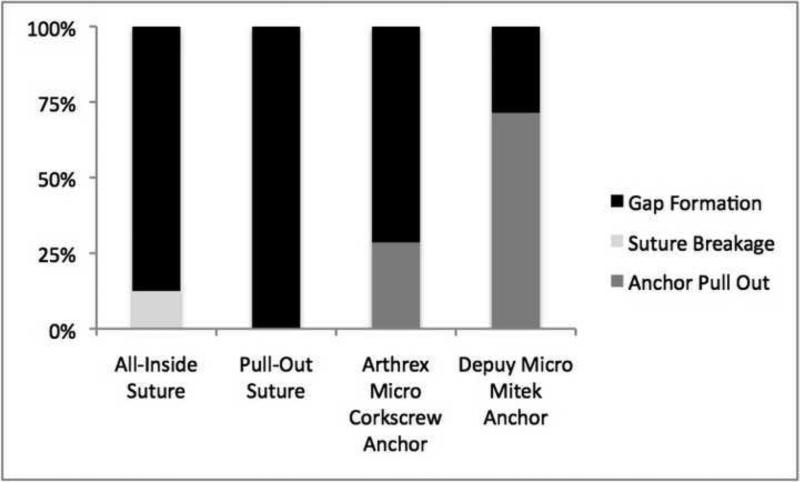
All the pull-out suture repairs failed through repair site gap formation (Figure 4). A gap of at least 2mm was measured between the volar bone and tendon in all samples. During the formation of these gaps, none of the sutures completely pulled through the tendon. When samples were examined after testing, sutures were not broken at the repair site. For the all-inside suture repairs, 7/8 failed with gap formation at the repair site and a single all-inside suture repair failure by suture breakage (Figure 5). In contrast, the anchor repair failure modes were more variable with 28.6% (2/7) Arthrex Micro Corkscrew and 71.4% (5/7) of the DePuy Micro Mitek anchors failing by anchor pull out. None of the sutures pulled out of the tendon or unraveled at the knot.
Figure 4.
Example of Failure by Gap Formation. This is a picture of one of the pull-out suture samples after testing. The gap between the bone and the tendon measures greater than 2mm.
Figure 5.
Failure Mode for the Repairs. After mechanical testing, the failure mode of the FDP repairs were characterized as either gap formation, suture breakage, or anchor pull out. Suture breakage occurred in 12.5% (1 out of 8) of the all-inside suture repairs and was not seen in any of the other repair types. Anchor pull out occurred in 28.6% of the Arthrex Micro Corkscrew anchors repairs and 71.4% of the DePuy Micro Mitek Anchor repairs.
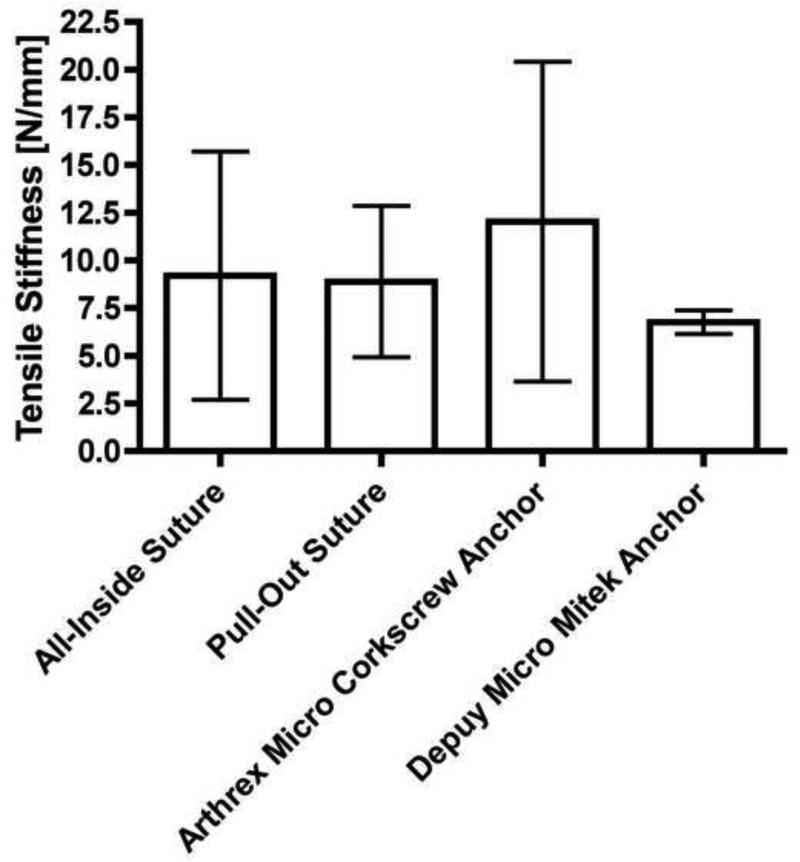
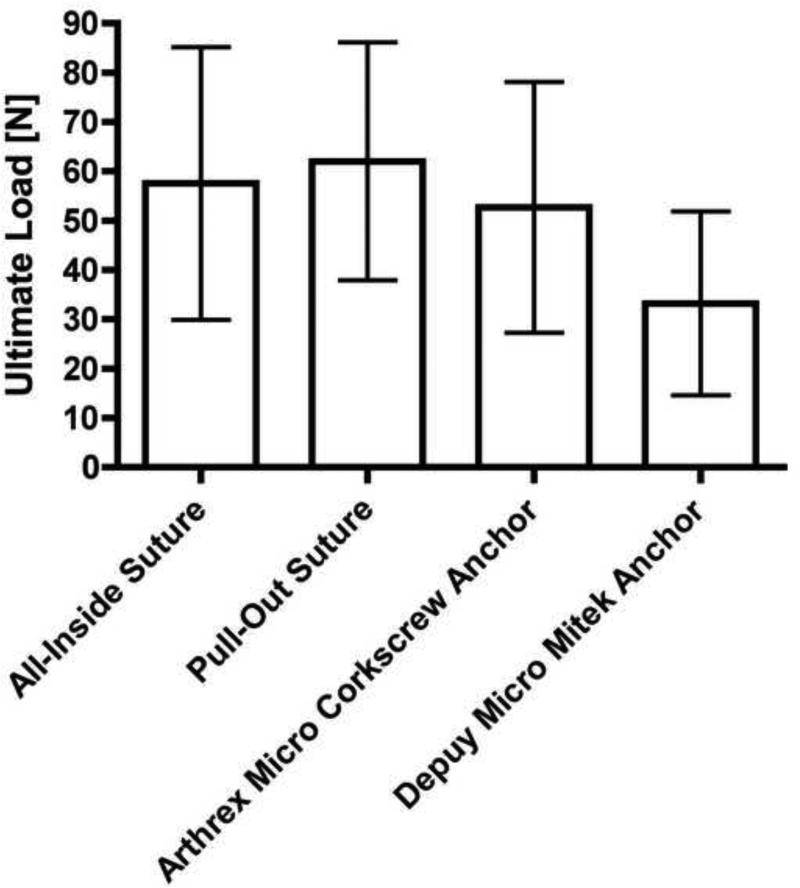
Mechanical Properties of Repairs
Mechanical testing demonstrated no differences (p > 0.1) in the tensile stiffness and ultimate load of the various repairs (Figure 6A and B). There was a trend towards increased ultimate load with the all-inside and pull-out suture repairs when compared to the suture anchor repairs.
Figure 6.
Mechanical Properties of the Repairs. The mean (A) tensile stiffness and (B) ultimate load of the repairs were calculated. No significant difference (p > 0.10) was found between groups.
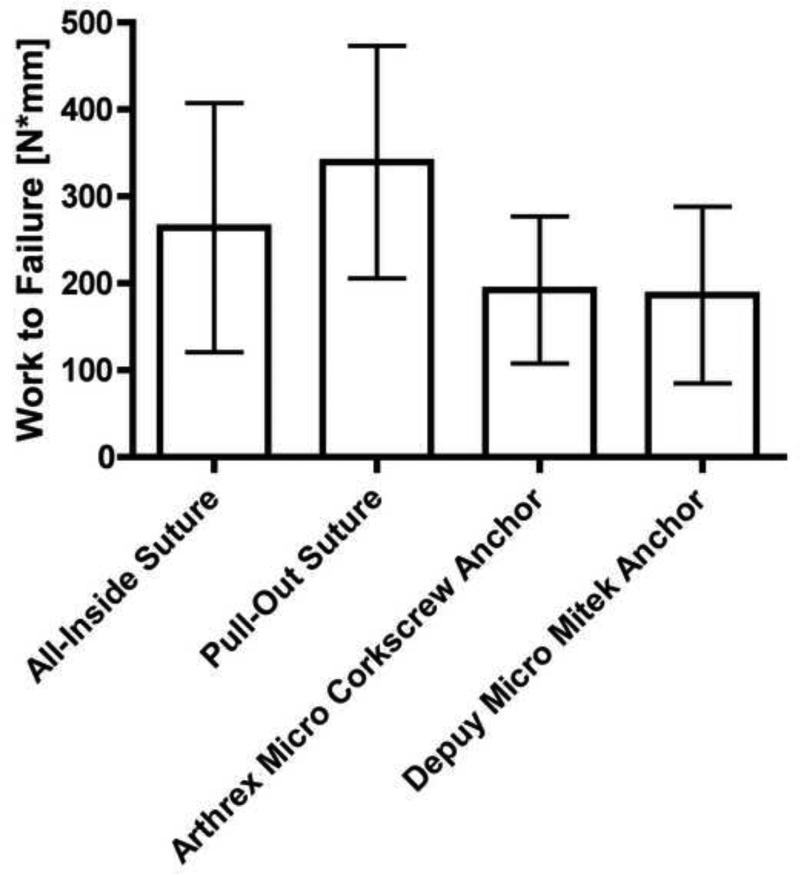
The total energy (work to failure) required before the repairs failed was not significantly different (p > 0.05) (Figure 7). The work to failure trended towards being greater for the pull-out suture and the all-inside suture repairs suggesting that the energy required to remove the anchors is less than the energy required to stretch the suture repairs.
Figure 7.
Work to Failure of the Repairs. The mean and standard deviations of the work to failure were plotted and a one-way ANOVA was used to determine differences between groups. No significant differences (p > 0.10) were found between the repair types.
Discussion
Multiple cadaveric studies have compared Zone I FDP avulsion repair methods. Brustein et al. (4) reported that attachment with 2 Mitek Micro anchors using 3-0 braided polyester with a modified 4-strand Becker stitch was superior to attachment with either a single Mitek Mini anchor with a 2-strand Bunnell stitch or a pull-out button using a 2-strand Bunnell 3-0 monofilament nylon suture. Silva et al. (5) noted that eight-strand repairs with a dorsal button had greater ultimate force and rigidity compared with four and eight-strand suture anchor repairs. Matsuzaki et al. (6) demonstrated that repairs with two suture anchors threaded with 3-0 FiberWire had greater stiffness and reduced displacement compared to pull-out repairs with no difference in force to failure. Recently, Lee et al. showed that an anchor button technique using a locking Krakow stitch with 2 retrograde anchors and a locking Krakow stitch tied over a dorsal button had less tendon- bone gapping after cyclical loading than either pull-out suture or double suture anchor repair alone (9).
Although the pull-out suture technique has been performed with good results, the use of the button has potential disadvantages. Clinical complications include nail deformities and prolonged hypersensitivity (10). Also, due to its external location, the button may be pulled and result in failure of the tendon reattachment or cause infection (3, 10).
Suture anchors provide an advantage because the repair is internal. Concerns regarding this technique include anchor pull out (5,6) and anchor penetration of the dorsal cortex or the articular surface. Ruchelsman et al. recommended use of intraoperative fluoroscopy and aiming the anchor toward the proximal-dorsal cortex to avoid anchor misplacement (7). Finally, both the pull-out suture repair and the suture anchor repair require additional equipment in the form of buttons or anchors that may not be readily available in the operating room.
Additionally, in today's health care environment, the cost of implants should be considered. At our institution, the patient's medical charges are $288 for DePuy Micro Mitek anchors and $256.50 for Arthrex Micro Corkscrew anchors. If two anchors are used, this creates an implant cost of $500 – 575. With the all-inside suture repair, the implant cost of two Keith needles ($2.18 each) and 3-0 Ethibond suture ($5.12 each) adds less than $15, similar to the cost of the pull-out suture technique.
Among the strengths of this study is that experimental variability was controlled in several ways. Because we removed the majority of the soft tissues, we were able to isolate the FDP tendon and distal phalanx interface during testing. Also, all testing was performed in the same manner on the same machine. Finally, a single surgeon completed all the repairs and testing, which allowed for consistency but may have introduced some element of bias since the surgeon was not blinded to repair method during testing and results may be variable when other surgeons use this technique.
There are several study weaknesses and additional areas for investigation. These include cadaver age, testing protocols, characterization of failure methods, suture variability, and sample size.
The average age of our cadavers was 81. Patients who are typically treated for these injuries tend to be younger. Use of this bone represents a worse case scenario. Results with better quality bone would likely be at least as good. Anchor pull out, which has been shown to occur in osteoporotic bone (6), may be less likely in younger bone. Because all of our cadavers were of similar age, bone density and joint mobility may have been similar, although these potential influences were not measured. We performed each repair at least once on each cadaver to minimize the influence of cadaver variability.
We tested the repairs using continuous rather than cyclic loading. Both testing approaches have been used in recent studies (6, 8). Cyclic loading may better represent the effect of repetitive finger motion. However, in the clinical setting, tendons weaken before they begin to accrue strength and healing eventually occurs with time between cyclic loads. This cannot be replicated in a cadaver study. Clinically, continuous loading represents failure from forceful gripping and was chosen as the method for evaluation because it allows better visualization of elongation, gap site formation, and ultimate failure.
Our study followed a similar continuous loading protocol as previous studies (6) except that we chose to test specimens until they lost 75% rather than 100% of their ultimate strength. Seventy-five percent was chosen because in preliminary testing, we found that substantial gapping (>2mm) occurred between the tendon and bone interface with this parameter. Such gapping would not be compatible with healing or accrual of strength, likely leading to clinical failure. Gap formation and elongation have been evaluated previously as reasons for failure of FDP avulsion repairs (11, 12). We chose to stop the testing prior to complete failure to better visualize where the weak point of the construct was located.
We recognize that our study methodology did not permit us to determine the exact cause of gap formation in the absence of suture failure. Our impression is gap formation was caused by suture stretch because the suture appeared thinned or even frayed in the case of braided polyester at the gap site. Recording suture diameter before and after testing would have allowed a quantitative measure to confirm or reject this impression. Suture migration within the tendon could also have contributed to gap formation, but when sutures were examined after testing, they appeared to be the same distance from the distal portion of the tendon as they were before testing. However, since exact pre-test and post-test measurements of suture distance from the distal tendon edge were not made, suture migration cannot be completely ruled out.
Additionally, although suture materials have different properties (13), we chose different sutures and suture configurations for each repair. We did this to replicate conditions from our previous operating room experience. Typically the pull-out suture repair is completed with a suture such as prolene that will slide as it is removed. For the suture anchor repairs, we used the preloaded sutures for several reasons. The anchors are rated for the sutures that are preloaded and rethreading anchors represents an off-label product use. Also, changing the suture in the operating room is not done commonly at our institution due to concerns about time and cost. For our all-inside technique, we chose Ethibond because this is what we have used clinically due to its low profile, non- absorbability, and ease of tying.
Finally, we did note variability in the results with the fingers repaired with the all-inside suture technique. This could be related to one specimen in the all-inside suture group in which the tensile stiffness was found to be more than two times the average of the other seven repairs. However, the tensile stiffness for this specimen did fall within one standard deviation of the mean. Increasing the number of specimens in each group might have minimized variability. A post-hoc power analysis indicates we would need 26 fingers per group to determine that there is no difference between groups with 90% confidence. This would have required an additional 19 cadavers, which were not available to us at this time. Also, our number of samples is comparable to what has been used in previous studies.
As with any reattachment of the FDP tendon to bone, adverse events can occur when performing the all-inside repair clinically and the surgeon must be aware of the anatomy of the area while operating. Accurate placement of Keith needles is important to avoid the germinal nail matrix, just as it is with traditional pull-out suture over the sterile matrix. While the relation of the suture to the germinal matrix was not directly assessed in this study, placing the suture within the extensor tendon should indicate the location is proximal to the matrix. Articular surface penetration is also a concern. In the clinical setting, fluoroscopy can be used to verify that this has not occurred (Figure 8).
Figure 8.
Clinical radiograph demonstrating position of Keith needles for all-inside suture repairs
The senior author has used the all-inside technique for over four years. Initially, the suture was tied on top of the extensor tendon through a longitudinal skin incision, which left the knot prominent and required knot removal under local anesthesia following healing. The technique was modified so that the knot was placed within a longitudinal incision in the extensor tendon. The extensor tendon was then reapproximated with an absorbable suture and palpated to verify that the knot was not prominent. Since this modification, it has not been necessary to remove the knot.
This study suggests that the all-inside suture repair has similar mechanical properties to both the pull-out suture repair and the double suture anchor repair. It has the advantage of being an internal repair with less implant cost than anchor repairs and therefore should be considered as an alternative method for zone 1 FDP avulsion repairs.
References
- 1.McCallister WV, Ambrose HC, Katolik LI, Trumble TE. Comparison of pullout button versus suture anchor for zone I flexor tendon repair. J Hand Surg Am. 2006;31(2):246–251. doi: 10.1016/j.jhsa.2005.10.020. [DOI] [PubMed] [Google Scholar]
- 2.Bunnell S. Surgery of the Hand. Ed 2. Lippincott; Philadephia, PA: 1948. pp. 381–466. [Google Scholar]
- 3.Guinard D, Montanier F, Thomas D, Corcella D, Moutet F. The Mantero flexor tendon repair in zone 1. J Hand Surg Br. 1999;24(2):148–151. doi: 10.1054/jhsb.1998.0173. [DOI] [PubMed] [Google Scholar]
- 4.Brustein M, Pellegrini J, Choueka J, Heminger H, Mass D. Bone suture anchors versus the pullout button for repair of distal profundus tendon injuries: a comparison of strength in human cadaveric hands. J Hand Surg Am. 2001;26(3):489–496. doi: 10.1053/jhsu.2001.24135. [DOI] [PubMed] [Google Scholar]
- 5.Silva MJ, Hollstien SB, Fayazi AH, Adler P, Gelberman RH, Boyer MI. The effects of multiple-strand suture techniques on the tensile properties of repair of the flexor digitorum profundus tendon to bone. J Bone Joint Surg Am. 1998;80(10):1507–1514. doi: 10.2106/00004623-199810000-00012. [DOI] [PubMed] [Google Scholar]
- 6.Matsuzaki H, Zaegel MA, Gelberman RH, Silva MJ. Effect of suture material and bone quality on the mechanical properties of zone I flexor tendon-bone reattachment with bone anchors. J Hand Surg Am. 2008;33(5):709–717. doi: 10.1016/j.jhsa.2008.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ruchelsman DE, Christoforou D, Wasserman B, Lee SK, Rettig ME. Avulsion injuries of the flexor digitorum profundus tendon. J Am Acad Orthop Surg. 2011;19(3):152–162. doi: 10.5435/00124635-201103000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Wilhelmi BJ, Kang RH, Wages DJ, Lee WP, May JW., Jr. Optimizing independent finger flexion with zone V flexor repairs using the Massachusetts General Hospital flexor tenorrhaphy and early protected active motion. J Hand Surg Am. 2005;30(2):230–236. doi: 10.1016/j.jhsa.2004.07.009. [DOI] [PubMed] [Google Scholar]
- 9.Lee SK, Fajardo M, Kardashian G, Klein J, Tsai P, Christoforou D. Repair of flexor digitorum profundus to distal phalanx: a biomechanical evaluation of four techniques. J Hand Surg Am. 2011;36(10):1604–1609. doi: 10.1016/j.jhsa.2011.07.017. [DOI] [PubMed] [Google Scholar]
- 10.Kang N, Marsh D, Dewar D. The morbidity of the nail over button technique for zone 1 flexor tendon repairs. Should we still be using this technique? J Hand Surg Br. 2008;33(5):566–570. doi: 10.1177/1753193408090118. [DOI] [PubMed] [Google Scholar]
- 11.Silva MJ, Hollstien SB, Brodt MD, Boyer MI, Tetro AM, Gelberman RH. Flexor digitorum profundus tendon-to-bone repair: an ex vivo biomechanical analysis of 3 pullout suture techniques. J Hand Surg Am. 1998;23(1):120–126. doi: 10.1016/S0363-5023(98)80099-3. [DOI] [PubMed] [Google Scholar]
- 12.Schreuder FB, Scougall PJ, Puchert E, Vizesi F, Walsh WR. Effect of suture material on gap formation and failure in type 1 FDP avulsion repairs in a cadaver model. Clin Biomech. 2006;21(5):481–484. doi: 10.1016/j.clinbiomech.2005.12.012. [DOI] [PubMed] [Google Scholar]
- 13.Lawrence TM, Davis TR. A biomechanical analysis of suture materials and their influence on a four-strand flexor tendon repair. J Hand Surg Am. 2005;30(4):836–841. doi: 10.1016/j.jhsa.2005.03.011. [DOI] [PubMed] [Google Scholar]