Abstract
The Fukushima Daiichi Nuclear Power Plant (NPP) 1 was severely damaged from the chain reaction of the Great East Japan Earthquake and Tsunami on 11 March 2011, and the consequent meltdown and hydrogen gas explosions. This resulted in the worst nuclear accident since the Chernobyl accident of 1986. Just as in the case of Chernobyl, emergency workers were recruited to conduct a wide range of tasks, including disaster response, rescuing activities, NPP containment, and radiation decontamination. This paper describes the types and efficacy of the various occupational health interventions introduced to the Fukushima NPP radiation workers. Such interventions were implemented in order to prevent unnecessary radiation overexposure and associated adverse health effects and work injuries. Less than 1% of all emergency workers were exposed to external radiation of >100 mSv, and to date no deaths or health adversities from radiation have been reported for those workers. Several occupational health interventions were conducted, including setting of new regulatory exposure limits, improving workers' radiation dosimetry, administration of stable iodine, running an occupational health tracking system, and improving occupational medicine and preventative care. Those interventions were not only vital for preventing unnecessary radiation, but also for managing other general health issues such as mental health, heat illness and infectious diseases. Long-term administration of the aforementioned occupational health interventions is essential to ensure the ongoing support and care for these workers, who were put under one of the most severe occupational health risk conditions ever encountered.
Keywords: occupational radiation exposure, Fukushima, nuclear disaster, radioprotection, public health
INTRODUCTION
The Fukushima Daiichi Nuclear Power Plant (NPP) 1, which is owned and operated by the Tokyo Electric Power Company (TEPCO) was severely damaged by the Great East Japan Earthquake and Tsunami on 11 March 2011. The tsunami destroyed the direct current power supply, resulting in complete loss of the power supplied to the NPP cooling systems. Consequently, the overheated NPP reactor cores that underwent a meltdown and hydrogen gas explosions dispersed large amounts of radionuclide materials into the vicinity [1]. The Japanese Government then declared a nuclear emergency, and TEPCO undertook emergency work to stabilize and cool off the nuclear reactor, during which various occupational health risks were encountered. The government declared that the affected plant had been stabilized on 16 December 2011. Approximately 20 000 workers were engaged in the various jobs to mitigate the accident inside the TEPCO Fukushima Daiichi nuclear power station from 14 March to 16 December 2011. During this period, the dose limit for the emergency work was temporarily increased from 100 mSv to 250 mSv. The Ministry of Health, Labour and Welfare (MHLW) defined these workers as emergency workers [2].
On the other hand, in the Chernobyl accident, ∼600 workers who were involved in emergency work on 26 April 1986 when the accident happened were defined as emergency workers [3]. In addition, >500 000 workers were involved in the recovery operation work, including the cleanup of the Chernobyl accident site.
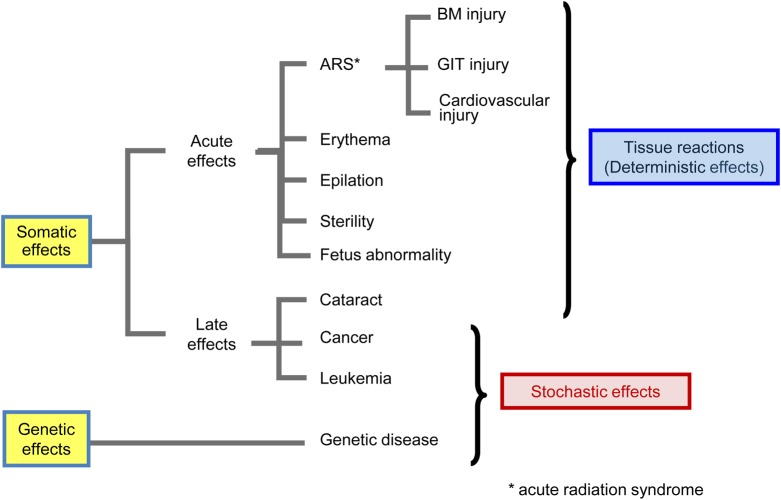
There are two main pathways of exposure to ionizing radiation (hereafter shortened to ‘radiation’) in humans: ‘external’ exposure of radioactive materials from outside the body, and ‘internal’ exposure via consumption or inhalation of contaminated materials. The health hazards resulting from radiation exposure are usually classified into two categories: ‘deterministic effects’ and ‘stochastic effects’ [4]. Deterministic effects are now referred to as ‘tissue reactions’, because it is increasingly recognized that some of these effects are not determined solely at the time of irradiation but can develop after exposure [5]. Tissue reactions cause erythema, epilation, fetus abnormality, sterility, and acute radiation syndrome (ARS), which includes bone marrow (BM), gastrointestinal tract (GIT) and cardiovascular disorders (Fig. 1) [4]. Threshold doses for tissue reactions depend on tissues and the severity of tissue reactions depends on radiation dose. The radiation exposure threshold has been estimated at ∼100 mSv for fetal abnormalities and 120–200 mSv for severe mental retardation, based on the results from health surveys of the atomic bomb survivors of Hiroshima and Nagasaki who were exposed in utero [6]. There is no evidence of a significant increase in transgenerational genetic effects following radiation exposure of the atomic-bomb survivors in Hiroshima and Nagasaki, or of patients who have received radiotherapy [7, 8].
Fig. 1.
Human effects of radiation. The effects of radiation are usually classified into two categories: ‘tissue reactions’ and ‘stochastic effects’. Tissue reactions cause erythema, epilation, fetus abnormality, sterility, acute radiation syndrome (ARS) including bone marrow (BM) injury, gastrointestinal tract (GIT) injury and cardiovascular injury. Stochastic effects cause solid cancer and leukemia.
On the other hand, it can be assumed that stochastic effects have no threshold and are proportional to the absorbed dose. Such exposures could cause cancers such as leukemia (Fig. 1) [4]. Among the 237 Chernobyl emergency workers, ARS was verified in 134 of these individuals. Of these 134 patients, 28 died within the first four months, and there have been four confirmed cases of solid cancer, three cases of myelodysplastic syndrome, one case of acute myelomonoblastic leukemia and one case of chronic myeloid leukemia [3].
According to the large cohort study of the Russian recovery operation workers (>142 000), a total of 48 cases of leukemia (including chronic lymphatic leukemia) were diagnosed in the period 1986–1993. For the larger number of emergency and recovery operation workers, there are indications of an increased incidence of leukemia and cataracts among those who received higher doses, although further clarification of the epidemiological information is still needed. Cancer risks for human exposure to radiation are estimated by using the Life Span Study Cohort from the atomic bomb survivors of Hiroshima and Nagasaki [9]. Their cancer risks increased dose dependently [9]. However, radiation risks below ∼100 mSv are not able to be estimated directly from the epidemiological data.
Therefore, workers who were exposed to doses exceeding the dose limit for normal radiation work during the period of emergency work may have to be investigated for the possible increase of occurrence of late-onset health impairments, including cancer [10].
Although little is known about the health risks involved with low-dose radiation, associated cancer risks at such an exposure level tend to be lower than for high-dose radiation, and the effects of long-term low-dose exposure are generally milder than those of short-term high-dose exposure to the same total dose [11]. The International Commission of Radiological Protection (ICRP) applies a Dose and Dose Rate Effectiveness Factor (DDREF) of 2 to allow for the reduced effectiveness of low-dose-rate radiation [10]. WHO and the United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR) published the report for the cancer risk of radiation workers involved in the Fukushima accident [12, 13]. For those few emergency workers who received very high doses to the thyroid (∼11 Gy), a notable risk of thyroid cancer is estimated, especially for young workers. However, any increased incidence of cancer in relation to the Fukushima accident is expected to be undetectable because of small variations being hidden by the normal statistical fluctuations in cancer incidence. Epidemiological studies require a large sample size to statistically detect the risks of low-dose radiation; hence, the risks associated with low doses of radiation remain uncertain [14, 15].
MHLW recently summarized the aim of long-term health monitoring of Fukushima workers [16]. Such surveillance could clarify the health risks associated with long-term and low-dose radiation exposure. This paper describes and outlines the occupational health interventions used to prevent unnecessary radiation exposure and related health adversities for the Fukushima NPP radiation workers, and evaluates the efficacy of those programs in preventing radiation harm and other occupational injuries. It is important to note that, since the interventions were exclusively public health activities and not research studies, no consent was obtained from the workers to incorporate their surveillance data into health risk assessments.
DOSE RESTRICTIONS
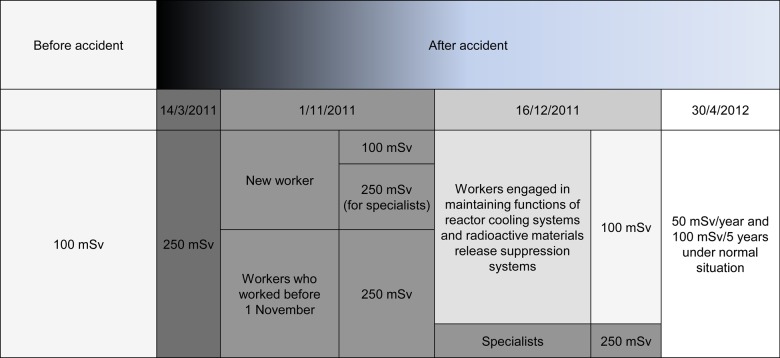
It is expected that the radiation exposures of radiation workers are higher than that of the public in any nuclear or radiological incident [17]. Health risks associated with long-term radiation exposure have become a major concern after the Fukushima accident. The ICRP generally recommends the occupational dose limit is an effective dose of 20 mSv/year, averaged over 5-year periods, without exceeding 50 mSv in any single year in a planned exposure situation [10]. In an emergency exposure situation, such as the serious accident at the Fukushima NPP, the reference level of occupational exposure in emergency could be 500 mSv or 1000 mSv except during life-saving actions if urgent rescue operations are required [10, 18]. Considering their recommendations, the Radiation Council in Japan debated raising the emergency dose limits from 100 mSv to 250 mSv, even before the Fukushima accident, in order to maximize general public protection and minimize any large consequence to the public from the nuclear disasters, because an exposure dose of <250 mSv may not cause acute radiation symptoms (Fig. 2) [19]. This was not instituted until 14 March 2011, days after the Fukushima NPP disaster. From 1 November 2011, emergency dose limits were further modified to 100 mSv for any new emergency workers. After 16 December 2011, dose limits for all emergency workers were restored to 100 mSv under normal working conditions, with the exemption of 250 mSv for specialists highly trained and experienced in operating the reactor cooling systems and in maintaining the facilities for suppressing the radioactive material emissions. This exemption was eventually removed on 30 April 2012. As the Japanese Government ordered decontamination work and the management of the resulting radioactive wastes for the NPP and affected areas in Fukushima Prefecture, radiation protection of the decontamination workers was also mandated [20]. The total dose limit for these workers was set at 100 mSv for 5 years, not exceeding 50 mSv for any one year. In the early phase after the Fukushima accident, recovery of the cooling system was the first priority for minimizing the risk of reactor explosion, even though the workers involved were thought to be exposed to high doses of radiation in the carrying out of this task. After that, the workers were engaged in stabilization of the reactor, mitigation of radioactive materials emission to the environment, and water decontamination. Radiation exposure limits for emergency work should be modified according to their duties, even within an emergency exposure situation. However, these exposure limits heavily rely on accurate dose measurements. Accurate dose measurements and exposure dose control for emergency workers are extremely important in order to ensure proper radiation protection.
Fig. 2.
Dose limits of workers. The dose limit was set for emergency workers according to their work and starting time, following ICRP recommendations.
IMPROVED DOSIMETRY
There were difficulties in accurate radiation dose measurements after the Fukushima accident because many personal dosimeters were lost due to the tsunami [21]. Therefore, personal dose calculations were initially performed from a combination of manual dose measurements and work task recordings for each worker [21, 22]. Manual dose calculations were conducted by allocating only one personal dosimeter to each working group within the same workspace area during the period of 15–30 March 2011 [21]. The major drawback to this approach was that it overlooked some extreme exposures for individual workers, since highly radioactive contaminated waste was widely and sporadically dispersed during this period. In response to this issue, MHLW instructed TEPCO to provide each and every worker with a personal dosimeter, and TEPCO collected some dosimeters from other domestic NPPs. The manual dose calculations resulted in a substantial delay in obtaining accurate measurements of individual exposure doses. Eventually, MHLW delegated the consolidation of the radiation dose management to private corporations and organized a dedicated team to search for former emergency workers for whom contact had been lost. Furthermore, MHLW introduced emergency preparedness guidelines in case another similar accident occurs [21, 22].
ADMINISTRATION OF STABLE POTASSIUM IODINE
Stable iodine can block the uptake of radioactive iodine by the thyroid [23]. Medical interviews were required for the workers and the public to screen out those with iodine hypersensitivity due to allergic reactions or thyroid disease. The Nuclear Safety Commission of Japan advised that workers who were exposed to an equivalent dose of 100 mSv to the thyroid should take stable iodine in the form of a 100-mg KI tablet on the first day and a 50-mg KI tablet every subsequent day for a maximum of 14 days. Later on, the Nuclear Regulation Authority mandated the predistribution of KI by the local government in response to future radiation accidents [24]. Approximately 2000 workers at the NPP were given KI during the emergency response phase. Although most of them took fewer than 10 tablets, the maximum taken by any one worker was 87 tablets [25]. A thyroid function test was carried out for 229 workers who continuously received KI for 14 days or a total of >20 tablets. The thyroid dose for each worker has not been identified. Thyroid dysfunction, such as increased levels of thyroid-stimulating hormone and decreased levels of thyroxin, was only transiently observed in the emergency workers. These parameters returned to normal values after KI distribution was terminated.
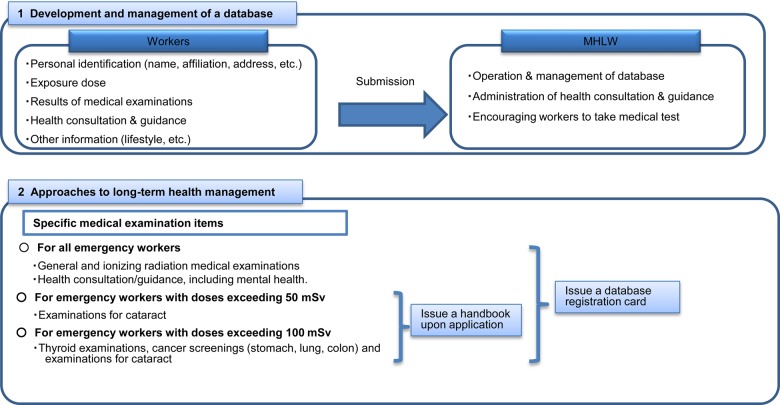
OCCUPATIONAL HEALTH TRACKING
MHLW established an occupational health tracking system to follow up the workers at Fukushima Daiichi NPP in order to identify any incident-related diseases as early as possible and determine the health risks caused by radiation exposure (Fig. 3). MHLW established guidelines for maintaining and improving the health of emergency workers at the TEPCO Fukushima Daiichi NPP on 11 October 2011. These guidelines describe methods for sustaining long-term health, development of an occupational health tracking database, and many other forms of support provided by the government for emergency workers [26]. All emergency workers are required by law to receive basic medical examinations during and after their involvement in radiation work. Workers exposed to an effective radiation dose >50 mSv received eye lens examinations, and those exposed to an effective radiation dose >100 mSv additionally had thyroid tests and cancer screenings. MHLW and TEPCO are tracking 97.6% of all emergency workers (18 874 out of a total of 19 346) for their long-term health control and cancer screening following these guidelines.
Fig. 3.
Long-term health care for emergency workers. Since the emergency dose limit increase to 250 mSv, long-term health care of emergency workers has been provided by the government. Medical examination will be carried out according to the exposure doses of workers.
OCCUPATIONAL MEDICINE AND PREVENTATIVE CARE
The medical center within the NPP was damaged and was inaccessible to workers due to heavy destruction by the tsunami [27]. As the Fukushima Prefectural Labor Bureau demanded TEPCO support the workers' mental and physical health, a total of 34 supporting physicians were then sent from the Japanese Association for Acute Medicine from 4 April to 31 August of 2011 [27]. The National Radiation Emergency Medical System of Japan consists of networks of primary, secondary and tertiary radiation emergency medical centers established by the Japanese government after the Tokai-mura accident of 1999. However, some primary radiation emergency medical centers could not be utilized because they were located within the 20-km evacuation zone of the NPP.
In fact, radiation adversities were not the only health concerns. Many workers were required to be on standby beyond their normal working hours in case of any unexpected emergencies. They were forced to sleep all crowded together on the floor in a seismically resistant building or in a gymnasium of the Fukushima Daiichi NPP. Occupational health physicians and nurses were recruited to provide mental health checkups and consultations for workers under such hardships [28]. Although MHLW demanded TEPCO to undertake daily work from 2–5 p.m. [22], during July and August which are the hottest months of summer, workers were later allowed some flexibility. They were allowed to take sufficient breaks and shift their working time to early mornings during those months.
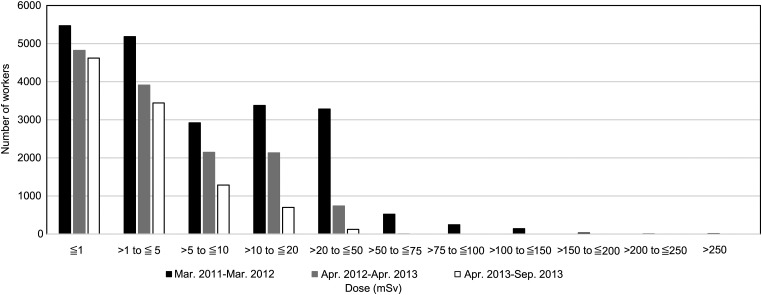
RADIATION DOSE ESTIMATION
Among the 31 383 workers who worked at the Fukushima NPP, only 173 had a cumulative effective dose (combining internal and external radiation exposure) of >100 mSv from March 2011 to December 2013 (Fig. 4, Table 1). Six emergency workers exceeded the dose limit of 250 mSv, and the maximum dose was only 670.36 mSv during the first month after the Fukushima incident (Fig. 4, Table 1) [21, 29]. The maximum cumulative dose for workers was 678.8 mSv from March 2011 to September 2013 (Table 1). WHO summarized a detailed assessment of internal exposure and thyroid doses of those workers [12, 30]. For the highest exposure, it was found that 590 mSv of the total dose was from internal exposure (Table 2). This worker's high internal exposure was presumably due to improper use of the charcoal filter cartridge in the respiratory protective equipment. Thyroid doses from 131I for workers until 5 February 2012 are shown in Table 3. No workers exceeded a cumulative effective dose of 100 mSv after April 2011. The average effective dose amongst emergency workers during the Fukushima incident was 12.44 mSv, and 65% of the workers were exposed to a radiation dose of <10 mSv; almost 99% of the workers at the Fukushima NPP were exposed to a radiation dose of <100 mSv (Fig. 4). Biodosimetry using the dicentric chromosome assay was carried out by the National Institute of Radiological Sciences from 21 March – 1 July 2011 for 12 emergency workers who were thought to have been exposed to a high dose of radiation. The results showed that the estimated maximum exposure dose for emergency workers was <300 mGy, with a mean value of ∼101 mGy [31]. No ARS was observed among these workers. Whole-body counter measurements of decontamination workers revealed that the levels of internal Cs, 134Cs and 137Cs, exposure among the decontamination workers were below detection limits [32].
Fig. 4.
Radiation exposure doses of workers at Fukushima incident. Aotal of 31 383 workers were engaged in emergency work after the Fukushima incident. During the first month after Fukushima incidence, 173 workers exceeded 100 mSv of combined cumulative effective dose of internal and external radiation exposure (highest was 670.36 mSv). Thereafter, workers who were exposed to >100 mSv were not reported. The average effective dose was 12.5 mSv amongst emergency workers from March 2011 to September 2013 at Fukushima incident.
Table 1.
Cumulative effective dose of internal and external radiation exposure
| Dose (mSv) | Mar | Apr | May | Jun | Jul | Aug | Sep | Mar 2011 – Sep 2013 |
|---|---|---|---|---|---|---|---|---|
| >250 | 6 | 0 | 0 | 0 | 0 | 0 | 0 | 6 |
| >200 to ≦250 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 3 |
| >150 to ≦200 | 17 | 0 | 0 | 0 | 0 | 0 | 0 | 26 |
| >100 to ≦150 | 80 | 0 | 0 | 0 | 0 | 0 | 0 | 138 |
| >75 to ≦100 | 108 | 0 | 0 | 1 | 0 | 0 | 0 | 345 |
| >50 to ≦75 | 186 | 1 | 0 | 0 | 1 | 0 | 0 | 1045 |
| >20 to ≦50 | 900 | 189 | 94 | 65 | 34 | 25 | 22 | 4569 |
| >10 to ≦20 | 991 | 613 | 420 | 373 | 213 | 181 | 142 | 4167 |
| >5 to ≦10 | 635 | 1474 | 967 | 836 | 634 | 539 | 435 | 3961 |
| >1 to ≦5 | 584 | 1748 | 3130 | 3299 | 3345 | 3379 | 3198 | 7184 |
| ≦1 | 465 | 1831 | 2671 | 3004 | 3506 | 3358 | 3374 | 8369 |
| Total | 3974 | 5856 | 7282 | 7578 | 7733 | 7482 | 7171 | 29813 |
| Maximum (mSv) | 670.36 | 59.6 | 48.8 | 89.5 | 56.76 | 35.1 | 33.4 | 678.8 |
| Average (mSv) | 21.36 | 4.95 | 3.31 | 2.91 | 2.27 | 2.1 | 1.92 | 12.5 |
Table 2.
Effective dose of internal radiation exposure
| Effective Dose (mSv) | Workers |
|---|---|
| >250 | 5 |
| >200 to ≦250 | 1 |
| >150 to ≦200 | 1 |
| >100 to ≦150 | 5 |
| >50 to ≦100 | 79 |
| >20 to ≦50 | 288 |
| >10 to ≦20 | 762 |
| >5 to ≦10 | 740 |
| ≦5 | 21291 |
| Total | 23172 |
| Maximum (mSv) | 590 |
Table 3.
Thyroid dose for workers
| Thyroid Dose (mSv) | Workers |
|---|---|
| >10000 | 2 |
| >2000 to ≦10000 | 10 |
| >1000 to ≦2000 | 32 |
| >500 to ≦1000 | 50 |
| >200 to ≦500 | 69 |
| >100 to ≦200 | 15 |
| 100 | 344 |
| Total | 522 |
HEALTH PROBLEMS OF EMERGENCY WORKERS
No deaths have been reported for the Fukushima NPP emergency workers as a result of radiation exposure. Neither were any cases of acute health problems resulting exclusively from radiation exposure reported. Therefore, the occurrence of deterministic risks is thought to have been minimized in those workers. Fortunately, the Fukushima area residents and emergency responders have not been exposed to radiation doses higher than the threshold for tissue reaction induction.
In addition to radiation risks, workers engaged in response and recovery efforts were exposed to multiple non-radiation health risks. Many of them may have other physical and mental health problems [28, 33, 34]. For example, the risk of heat illness was relatively higher in these workers, as they worked long hours under the blazing sun while wearing heavy equipment for radioprotection [34]. Workers also faced severe psychological stress stemming from the fear of additional explosions at the Fukushima NPP and subsequent exposure to high doses of radiation [33]. Occupational health interventions for emergency radiation workers should incorporate all of the potential occupational health and safety concerns, and not be limited to radiation risks. During the first month after the accident, 25 workers became sick or injured from non-radiation causes, and 31 workers complained of poor general health. One worker even suffered a heart attack on 14 May 2011, unrelated to radiation exposure. After these findings were evaluated, non-radiation-associated occupational injuries were kept minimal, and mental health concerns were addressed.
EVALUATING OCCUPATIONAL HEALTH INTERVENTIONS BASED ON PREPAREDNESS
The Japanese MHLW encouraged the implementation of several occupational health interventions after the Fukushima NPP accident, including the promulgation of new radiation exposure limits regarding the exceptional Ordinance on Prevention of Ionizing Radiation Hazards in response to the situation resulting from Tohoku–Pacific Ocean Earthquake in 2011, improving radiation dosimetry, stable iodine administration, developing an occupational health tracking system, and providing occupational medicine and preventative care. These efforts have been successful at minimizing workers' radiation exposures and associated adversities, as is evidenced by the <1% of workers who were exposed to a radiation dose of >100 mSv (173 of 31 383 workers) and the complete absence of any reported deaths or injuries linked to radiation exposure.
In the Chernobyl accident, 134 cases of ARS were diagnosed among NPP employees and first responders, who were exposed to a radiation dose >6.5 Gy [35], but no cases of ARS were reported amongst the general public [36]. The average effective dose from external irradiation was 120 mSv among the 530 000 workers engaged in decontamination work after the Chernobyl accident [36]. In 1999, a nuclear accident occurred at the uranium conversion plant in Tokai-mura, Japan. Three workers were severely exposed to neutron and γ-rays and subsequently developed ARS [37]. In comparison with the Chernobyl and Tokai-mura accidents, it can be said that the radiation exposure of emergency workers for the Fukushima accident was relatively minimized.
Based on experiences at Fukushima, a storage space must be placed within a safe and reasonable distance from any NPP to accommodate supplies and equipment for medical facilities that are part of an NPP. Furthermore, the relevant parties in the council of the medical care system should conduct specialized medical examinations as suitable for the range of emergency work situations. WHO reported that mental, psychological and central nervous system changes in workers following the Chernobyl accident were due to the psychological stress resulting from the fear of radiation exposure [38]. A similar scenario can be outlined for the Fukushima case as well. It is necessary to continue monitoring mental health amongst radiation emergency workers and to provide proper mental health care services [26]. It is important to provide effective health care services, not only for prevention of unnecessary radiation exposure but also for treating other health risks, such as heat disorders and infectious diseases.
From lessons learned about emergency work at the TEPCO-run Fukushima Daiichi NPP, a standard guideline is required for preparedness in managing occupational exposure that can be applied in the event of any nuclear disasters. Sufficient occupational health protection measures and systematic preparation for radiation exposure management must be specified in such guidelines. In the Fukushima accident, the tsunami destroyed exposure control systems that were located in the Fukushima NPP and lost radiation-monitoring materials. In order to resolve this issue, various experts contributed to the establishment of a network of systems to support the radiation protection of workers by controlling the radiation exposure of emergency workers. Control department and monitoring systems should be prepared assuming the case of insufficient materials resulting from major complex disasters. In order to minimize the radiation exposure of the workers, decontamination should be started after measuring the workers' baseline radiation dose, and conducted under the direct orders of an operation leader in accordance with a proper work plan.
CONCLUSION
The Japanese national government and the main companies involved in the radiation emergency response held great concern for the health of all emergency workers, as is evident from the establishment or revision of occupational health interventions to protect their health. While almost all workers were exposed to a low radiation dose (<100 mSv), long-term occupational health interventions, including general medical checks and mental health care, have been successful in protecting their health. To date, no deaths or radiation adversities have been reported amongst the radiation emergency workers. Ongoing long-term occupational health interventions are necessary to physically, mentally and morally care for the emergency workers who put their health and lives at high risk to protect the nation at large.
FUNDING
This study was partially supported by the Japanese Ministry of Health, Labour, and Welfare. Funding to pay the Open Access publication charges for this article was provided by the Japanese Ministry of Health, Labour, and Welfare.
ACKNOWLEDGEMENTS
We are thankful for the cooperation of the many leaders in the local governments who facilitated these public health actions regarding the Fukushima accident.
REFERENCES
- 1. MEXT and DOE. Results of airborne monitoring by the Ministry of Education, Culture, Sports, Science and Technology and the U.S. Department of Energy. 6 May 2011. http://www.mext.go.jp/component/english/__icsFiles/afieldfile/2011/05/10/1304797_0506.pdf. (8 February 2013, date last accessed).
- 2.MHLW. Policies for epidemiological studies targeting emergency workers at the TEPCO Fukushima Daiichi Nuclear Power Plant have been compiled. Office for Radiation Protection of Workers, Industrial Safety and Health Department, Labour Standards Bureau, 4 June 2014. Japanese Ministry of Health, Labour and Welfare. http://www.mhlw.go.jp/english/topics/2011eq/workers/tepco/lhc/pr_140604.html (31 August 2014, date last accessed).
- 3.UNSCEAR. Sources and effects of ionizing radiation. UNSCEAR 2000 Report . New York: United Nations, 2000. [Google Scholar]
- 4.Hall EJ, Giaccia AJ. Radiobiology for the radiologist. 6th edn Philadelphia: Lippincott Williams & Wilkins, 2006. [Google Scholar]
- 5.ICRP. Statement on tissue reactions. ICRP Publication 118. Ann ICRP 2012;41 (1–2). http://www.icrp.org/docs/icrp%20statement%20on%20tissue%20reactions.pdf (25 February 2014, date last accessed). [DOI] [PubMed] [Google Scholar]
- 6.Otake M, Schull WJ, Lee S. Threshold for radiation-related severe mental retardation in prenatally exposed A-bomb survivors: a re-analysis. Int J Radiat Biol 1996;70:755–763. [DOI] [PubMed] [Google Scholar]
- 7.Neel JV, Schull WJ. The Children of Atomic Bomb Survivors: A Genetic Study. Washington, DC: The National Academies Press, 1991. [PubMed] [Google Scholar]
- 8.Boice JD, Jr, Tawn EJ, Winther JF, et al. Genetic effects of radiotherapy for childhood cancer. Health Phys 2003;85:65–80. [DOI] [PubMed] [Google Scholar]
- 9.Ozasa K, Shimizu Y, Suyama A, et al. Studies of the mortality of atomic bomb survivors, Report 14, 1950–2003: an overview of cancer and noncancer diseases. Radiat Res 2012;177:229–43. [DOI] [PubMed] [Google Scholar]
- 10.ICRP. The 2007 Recommendations of the International Commission on Radiological Protection. ICRP Publication 103. Ann ICRP 2007;37 (2–4). [DOI] [PubMed] [Google Scholar]
- 11.ICRP. Low-dose extrapolation of radiation-related cancer risk. ICRP Publication 99 Ann ICRP 2005;35 (4). [DOI] [PubMed] [Google Scholar]
- 12.WHO. Health risk assessment from the nuclear accident after the 2011 Great East Japan earthquake and tsunami, based on a preliminary dose estimation. WHO, Geneva, 2014. [Google Scholar]
- 13.UNSCEAR. UNSCEAR 2013 Report. Volume I Report to the General Assembly Scientific Annex A: Levels and effects of radiation exposure due to the nuclear accident after the 2011 great East-Japan earthquake and tsunami. New York: United Nations, 2013. [Google Scholar]
- 14.Brenner DJ, Doll R, Goodhead DT, et al. Cancer risks attributable to low doses of ionizing radiation: assessing what we really know. Proc Natl Acad Sci U S A 2003;100:13761–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mullenders L, Atkinson M, Paretzke H, et al. Assessing cancer risks of low-dose radiation. Nat Rev Cancer 2009;9:596–604. [DOI] [PubMed] [Google Scholar]
- 16.MHLW. A proposal for epidemiological study among workers in the TEPCO Fukushima Daiichi Nuclear Power Plant. Ministry of Health, Labour and Welfare. http://www.mhlw.go.jp/file/04-Houdouhappyou-11303000-Roudoukijunkyokuanzeneiseibu-Roudoueiseika/0000047451.pdf (11 June 2014, date last accessed) (in Japanese).
- 17.ICRP. General principles for the radiation protection of workers. Radiological protection policy for the disposal of radioactive waste. ICRP Publication 77. Ann ICRP 1997;27 (S1). [Google Scholar]
- 18.ICRP. 1990 Recommendations of the International Commission on Radiological Protection. ICRP Publication 60. Ann ICRP 1991;21 (1–3). [PubMed] [Google Scholar]
- 19.Radiation Council in Japan. Considering ICRP 2007 recommendations for radiation regulation. http://www.nsr.go.jp/archive/mext/b_menu/shingi/housha/toushin/__icsFiles/afieldfile/2011/03/07/1302851_1.pdf. (11 June 2014, date last accessed) (in Japanese).
- 20.Yasui S. Establishment of new regulations for radiological protection for decontamination work involving radioactive fallout emitted by the Fukushima Daiichi APP accident. J Occup Environ Hyg 2013;10:D119–24. [DOI] [PubMed] [Google Scholar]
- 21.Yasui S. Lessons learned: Radiological protection for emergency workers at the TEPCO Fukushima Daiichi APP (part 1). J Occup Environ Hyg 2013;10:D151–8. [DOI] [PubMed] [Google Scholar]
- 22.MHLW. Response and action taken by the Ministry of Health, Labour and Welfare of Japan on radiation protection for workers involved in the TEPCO Fukushima Daiichi Nuclear Power Plant Accident. Ministry of Health, Labour and Welfare. http://www.mhlw.go.jp/english/topics/2011eq/workers/tepco/rp/irpw.pdf (12 February 2014, date last accessed).
- 23.Sternthal E, Lipworth L, Stanley B, et al. Suppression of thyroid radioiodine uptake by various doses of stable iodide. New Engl J Med 1980;303:1083–8. [DOI] [PubMed] [Google Scholar]
- 24.Nuclear Regulation Authority. Instruction of administration of a stable iodine tablet. http://www.nsr.go.jp/activity/bousai/iodine_tablet/index.html (13 November 2013, date last accessed) (in Japanese).
- 25.Nuclear Safety Commission. Administration of stable potassium iodide in emergency workers at Fukushima incident. http://www.nsr.go.jp/archive/nsc/senmon/shidai/hibakubun/hibakubun030/siryo4-3.pdf (13 November 2013, date last accessed) (in Japanese).
- 26.Yasui S. Lessons learned: medical and health care management for emergency workers at the TEPCO Fukushima Daiichi APP accident. J Occup Environ Hyg 2014;11:D49–58. [DOI] [PubMed] [Google Scholar]
- 27.Morimura N, Asari Y, Yamaguchi Y, et al. Emergency/disaster medical support in the restoration project for the Fukushima nuclear power plant accident. Emerg Med J 2013;30:997–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wada K, Yoshikawa T, Hayashi T, et al. Emergency response technical work at Fukushima Dai-ichi nuclear power plant: occupational health challenges posed by the nuclear disaster. Occup Environ Med 2012;69:599–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.MHLW. Exposure dose distribution of the workers at Fukushima Daiichi Nuclear Power Plant http://www.mhlw.go.jp/english/topics/2011eq/workers/irpw/index.html (16 February 2014, date last accessed).
- 30.Yasui S. Lessons learned: radiological protection for emergency workers at the TEPCO Fukushima Daiichi APP (part 2). J Occup Environ Hyg 2013;10:D163–D71. [DOI] [PubMed] [Google Scholar]
- 31.Suto Y, Hirai M, Akiyama M, et al. Biodosimetry of restoration workers for the Tokyo Electric Power Company (TEPCO) Fukushima Daiichi nuclear power station accident. Health Physics 2013;105:366–73. [DOI] [PubMed] [Google Scholar]
- 32.Tsubokura M, Nihei M, Sato K, et al. Measurement of internal radiation exposure among decontamination workers in villages near the crippled Fukushima Daiichi Nuclear Power Plant. Health Phys 2013;105:379–81. [DOI] [PubMed] [Google Scholar]
- 33.Matsuoka Y, Nishi D, Nakaya N, et al. Concern over radiation exposure and psychological distress among rescue workers following the Great East Japan Earthquake. BMC Public Health 2012;12:249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mori K, Tateishi S, Hiraoka K, et al. How Occupational Health can contribute in a disaster and what we should prepare for the future–lessons learned through support activities of a medical school at the Fukushima Daiichi Nuclear Power Plant in Summer 2011. J Occup Health 2013;55:6–10. [DOI] [PubMed] [Google Scholar]
- 35.Mettler FA, Jr, Gus'kova AK, Gusev I. Health effects in those with acute radiation sickness from the Chernobyl accident. Health Phys 2007;93:462–9. [DOI] [PubMed] [Google Scholar]
- 36.Balonov M. The Chernobyl accident as a source of new radiological knowledge: implications for Fukushima rehabilitation and research programmes. J Radiol Protect 2013;33:27–40. [DOI] [PubMed] [Google Scholar]
- 37.Akashi M, Hirama T, Tanosaki S, et al. Initial symptoms of acute radiation syndrome in the JCO criticality accident in Tokai-mura. J Radiat Res 2001;42 Suppl: S157–66. [DOI] [PubMed] [Google Scholar]
- 38.WHO. Health effects of the Chernobyl accident and special health care programmes. Report of the UN Chernobyl Forum Expert Group “Health”. Bennett B, Repacholi M, Carr Z. (eds). WHO, Geneva, 2006. [Google Scholar]