Abstract
Background
The identification of antecedents to sexual risk among youth is critical to the development and dissemination of multilevel interventions. Therefore, the aim of the present study was to examine the effect of sexual sensation-seeking on partner age, partner communication, and the sexual attitudes and behaviours of African-American female youth.
Methods
This study examined survey data collected by audio computer-assisted self-interviews from 701 young African-American females between 14 and 20 years of age. The survey consisted of items designed to measure adolescents’ sexual risk and preventive behaviours.
Results
The results of this study suggest that sexual sensation-seeking is associated with condom use among adolescent African-American females. For adolescents who reported greater sexual sensation-seeking, lower levels of sexual happiness were associated with a decreased likelihood of condom use at last intercourse (β = 1.01, P ≤ 0.05). For those reporting lower levels of sexual sensation-seeking, greater sexual enjoyment was associated with a greater likelihood of condom use at last intercourse (β = 0.93, P ≤ 0.01). Adolescents with younger sexual partners and lower levels of sexual sensation-seeking reported a higher proportion of condom use in the past 6 months (β = 0.70, P = 0.01). Higher partner communication self-efficacy and decreasing levels of sexual sensation-seeking were associated with fewer lifetime sexual partners (β = –0.54, P ≤ 0.05).
Conclusions
Future research should address the impact of these variables on adolescent relationship dynamics and sexual decision-making.
Keywords: communication, condom use, partner age, satisfaction, women, youth
Introduction
The rate of sexually transmissible infections (STIs) among adolescents and young adults has reached epidemic proportions.1 This crisis has been particularly devastating for African-American youth residing in the south-east region of the US, as this region has experienced an alarming increase in reported STI cases, including cases involving HIV infection.2 African-American females, in particular, account for approximately two-thirds of all new HIV/AIDS cases, and have infection rates that are seven times greater than their male counterparts3 and up to 20 times greater than their Caucasian counterparts.4 Moreover, research has demonstrated that African-American females are especially vulnerable to the consequences of inconsistent contraceptive use, as they experience relatively high rates of STIs and teen pregnancy, and often have dense sexual networks, leading to increased STI risk.1 To address this important public health concern, much research has been dedicated to the development and dissemination of multilevel interventions that reduce sexual risk among ethnic minority female youth through the identification and targeting of the antecedents of sexual risk.5,6
The antecedents of sexual risk are dynamic characteristics that may be greatly influenced by generational differences and, consequently, require ongoing efforts at identification.6 In their examination of the sexual risk behaviours of females, Wingood and DiClemente7 highlighted the pathways through which sociostructural factors lead to negative outcomes among women with their application of Connell's sociological theory of gender and power. In their adaptation, risk is conceptualised as the social, economic and physical factors that increase one's vulnerability to HIV infection. Among other factors, they asserted that ethnic minority status and being younger than 18 years increases one's risk of subsequent HIV infection.7 According to the theory, partner characteristics, considered social risks, are influential in women's sexual relationships, as the partner with greater actual or perceived power, often the male, may exert greater influence over certain kinds of sexual behaviours, including condom use, thereby increasing women's risk for unsafe sexual practices and STIs.7 Therefore, due to their age, ethnic minority status, and likelihood of facing financial dependency at this stage in their lives, African-American female adolescents and young women are at increased risk for infection. For these reasons, the identification of the antecedents of sexual risk within this population is particularly critical.
Using this framework, we model three antecedents that have been independently linked to sexual risk but have yet to be examined within a single study: partner age,8 partner communication9 and sexual attitudes.10 Although the identification of the antecedents to sexual risk is an important factor in the development of efficacious interventions, to date, there has been little research dedicated to understanding how sexuality-related constructs might interact with antecedents to influence sexual risk.11,12 Sexual sensation-seeking (SSS), often describing one's propensity for ‘exciting, optimal and novel levels of stimulation or arousal’,13 may be an important factor in youth risky sexual behaviour (RSB), as previous research has linked higher levels of SSS among adolescent girls to greater sexual risk, including frequent intercourse, more sexual partners and less condom use.14 Therefore, the purpose of the current study is to examine the influence of SSS on antecedents of unprotected intercourse and the number of sexual partners within a sample of young African-American females from Atlanta, Georgia, which is an area that has experienced a high seroprevalence of HIV infection among African-American women.6 Specifically, our study examines the way in which SSS might interact with partner age, partner communication and sexual attitudes to predict the condom use and number of sexual partners of young African-American females.
SSS and antecedents of sexual risk
Previous research has linked higher levels of SSS to greater sexual risk among young African-American females.12,13,15 SSS, however, is unique among other antecedents of sexual risk, as it is more akin to a biological trait and often peaks in late adolescence, showing evidence of decline over time.16 Although it is considered to be a biological trait, SSS is believed to be pliable17 and may interact with other key antecedents, including the age of a sexual partner, to influence sexual risk.
According to data from national surveys, 36–50% of adolescent girls report having a sexual partner who is ≤ 2 years older than themselves.18,19 African-American youth with older sexual partners initiate intercourse at younger ages than African-American youth with similarly aged partners.20 Compared with their peers with similarly aged partners, adolescents with older sexual partners also tend to report less condom use and are at greater risk for teen pregnancy and STIs.21,22 One study found that pregnant African-American girls with sexual partners who were ≤2 years older than themselves were approximately four times as likely as their peers with similarly aged sexual partners to be infected with Chlamydia trachomatis.21 Interestingly, the effect of partner age discordance on RSB has implications for subsequent adult sexual behaviour, as greater partner age difference at first intercourse during adolescence is associated with greater engagement in RSBs during adulthood, including a greater number of lifetime sexual partners, greater partner concurrency and less condom use.8 For adolescent females, greater partner age differences could be connected to greater power differentials within relationships, such that females may perceive themselves to have less power to negotiate condom use with an older partner and therefore report less condom use than their peers whose partners are the same age. To date, no studies have examined the interaction between SSS and partner age as they relate to sexual risk. It is likely that youth with greater SSS will report older sexual partners and higher sexual risk. In addition to partner age, quality of communication with sexual partners might also influence sexual risk.
Research has suggested that early experiences with partner communication could shape adolescents’ self-perceptions and relationship self-efficacy.23 Between 30% and 50% of adolescents fail to discuss contraceptive methods or STIs before their first sexual encounter.24,25 One study found that adolescent girls who infrequently discussed prevention methods with their sexual partners were also less likely to report consistent contraceptive use.26 These findings could suggest that youth with poor partner communication are at greater risk for STIs and unintended pregnancy, given that there is a strong link between partner communication and the use of contraceptives.24,27 Although contraceptive use among adolescents has improved in recent years,28 youth continue to struggle with inconsistency.26 Youth who have older partners or poor partner communication may perceive greater power differentials in relationships, leading to greater sexual risk, particularly as it relates to condom use. Taken together, partner communication appears to be an important determinant of sexual risk behaviour; however, additional research is needed to explore the significance of this factor within a sample of low-income African-American females. Moreover, research is needed to examine the influence of SSS on the relationship between partner communication self-efficacy and sexual risk, as youth with high SSS may have poor partner communication, leading to greater sexual risk.
Other potential determinants that have been largely understudied in the adolescent sexual behaviour literature are sexual attitudes such as sexual enjoyment and sexual happiness. Among adolescent females, there were links between greater sexual enjoyment, and more frequent intercourse and sexual experimentation.29 It is notable that more frequent intercourse and sexual experimentation may not indicate greater sexual risk among adolescent females, as it is possible that young women who prioritize their own desires for sexual pleasure and happiness may be less sensitive to a male partner's desire to refrain from condom use citing reduced pleasure if the young women themselves do not perceive condoms as affecting their own sexual pleasure. In this case, women may be more empowered to engage in less sexual risk. This hypothesis might explain the results of studies that have found links between sexual pleasure and condom use, such that women who associated condom use with decreased sexual pleasure were less likely to report condom use.30 Moreover, the relationship between SSS and reports of sexual pleasure, sexual happiness, and sexual risk are not well understood, as no research has been done on this topic to date. We acknowledge that several variables could demonstrate interactive effects with the identified antecedents but, we selected SSS due to its strong relationship with sexual risk among youth. The purpose of the current study is to examine the influence of SSS on the relationship between the aforementioned antecedents, and condom use and number of sexual partners among young African-American females.
Methods
Sample and procedure
This study was approved by the Emory University Institutional Review Board. Between June 2005 and June 2007, 701 young African-American females between the ages of 14 and 20 years old were recruited from three sexual health-based clinics servicing inner-city youth in Atlanta, Georgia, to participate in a HIV prevention program. A young African-American woman recruited participants from the clinic waiting area, explained the purpose of the study and assessed eligibility. Participants were eligible if they were African-American females, were between 14 and 20 years old, and reported having unprotected vaginal intercourse at least once in the past 6 months. Participants were excluded if they were pregnant or attempting to conceive, or if they were married. Eligible participants expressing interest in the study scheduled an appointment to return to the clinic to complete consent forms and baseline assessments. Baseline assessments were administered using audio computer-assisted self-interviews. The survey consisted of items designed to measure adolescents’ sexual risk and preventive behaviours. Biological specimens were collected and tested for common STIs and urine pregnancy screens were also conducted to ensure study eligibility. Due to rights to privacy and the confidentiality of clinic services, parental consent was waived. The current study focusses on data from the baseline assessment. Information about the HIV prevention program has been detailed in other publications.9
Measures
Sexual behaviour outcomes
There were three main behavioural outcomes in this study: condom use at last sex, the proportion of condom use in the past 6 months and lifetime number of sexual partners. To assess condom use at last sex, participants were asked if they used a condom the last time they had sex (0 = no, 1 = yes). To assess the proportion of condom use in the past 6 months, we divided the number of times a condom was used during vaginal sex in the past 6 months by the total number of reported instances of vaginal sex in the past 6 months. To assess the lifetime number of sexual partners, participants were asked, ‘In your entire life, how many guys have you had vaginal sex with?’
Antecedents of sexual risk
Partner age
One item was used to assess partner age. Participants were asked to estimate the average age of their male sexual partners. Responses were measured on a five-point scale and ranged between 1 and 4 (1 = younger than you; 2 = about the same age; 3 = older than you by 2–3 years; 4 = much older than you by 4 or more years).
Partner communication self-efficacy
Participants answered six questions about the perceived difficulty of talking with their male sexual partners about condom use and other sexual risk behaviours.31 Specifically, the six items were as follows: ‘How hard is it for you to. . .( 1) ask how many sex partners he has had, (2) ask if he is having sex with you and other women, (3) ask if he has an STI, (4) ask if he could use a condom, (5) demand that he use a condom and (6) refuse to have sex if he won't wear a condom?’ Responses ranged from 1 (very hard) to 4 (very easy). Individual scores for each item were summed to create a single composite scale (a = 0.82), with higher scores indicating higher partner communication self-efficacy.
Sexual attitudes
Sexual attitudes consisted of two measures: sexual happiness and enjoyment of sex. Sexual happiness (a = 0.82) was measured using a five-point six-item composite scale that ranged from 1 (not at all important) to 5 (extremely important). Participants were asked to answer questions about the importance of their sexual happiness. Sample questions included: ‘How important is it to your sexual happiness that you: (1) have an orgasm when engaged in sexual activity, (2) feel comfortable talking with your partner about your sexual activities, and (3) feel emotionally close to your partner as a result of your sexual activity?’ Items were summed to create a composite scale, with higher scores indicating higher levels of sexual happiness. The second measure, enjoyment of sex, was assessed by a single item on a four-point scale. Participants were asked to rate their level of physical pleasure or satisfaction from sexual intercourse with their primary sexual partner. Responses ranged from 1 (none or very little) to 3 (a great deal). Higher scores indicated greater enjoyment of sex.
Moderator of sexual risk
SSS (α = 0.76) was measured using 10 items. Participants were asked to respond to statements related to sexual thrill-seeking and adventurism. For example, participants were asked to use a four-point scale that ranged from 1 (strongly disagree) to 4 (strongly agree) to respond to the following statements: (1) ‘Having sex with a new partner is exciting to me,’ (2) ‘I enjoy the thrill of having sex in public places,’ (3) ‘Videotaping or photographing myself and my partner during sex is exciting,’ and (4) ‘I use sex toys to make sex more exciting.’ Items were summed to create a composite score, with higher scores indicating greater SSS.
Analysis plan
Data were analysed using SPSS ver. 21 (IBM Corp., Armonk, NY, USA). We used descriptive statistics (e.g. mean and s.d.) to assess participant characteristics and data quality. Predictor variables were centred before analysis. We used linear regression to examine the independent association of SSS, partner age, partner communication self-efficacy and sexual attitudes with continuous measures of sexual behaviour and logistic regression for dichotomous measures of sexual behaviour. Specifically, we created four regression models with three different measures of sexual behaviour (i.e. unprotected intercourse at last sex, proportion of unprotected intercourse in the past 6 months and number of lifetime sexual partners). Interactions between SSS and predictors were also examined. Significance for all analyses was defined by α < 0.05.
Results
Sample characteristics
The study participants were 701 African-American adolescent females with a mean (≤s.d.) age of 17.64 1.67 years. Most participants reported having sexual partners who were ≤2 years older than themselves (n = 446; 81.7%). Approximately 43% of participants (n = 237) reported condom use at last intercourse. Participants reported condom use in fewer than 50% of their sexual encounters in the past 6 months (0.49±0.35). The mean number of lifetime sexual partners was 8.14±12.8 respectively. Additional information on the descriptives is provided in Table 1.
Table 1.
Descriptives among study variables
| Mean | s.d. | |
|---|---|---|
| Partner communication | 20.61 | 3.46 |
| Partner age | 3.72 | 0.81 |
| Enjoy sex | 3.38 | 0.86 |
| Sexual sensation-seeking | 18.89 | 4.41 |
| Sexual happiness | 21.53 | 5.18 |
Multivariate models
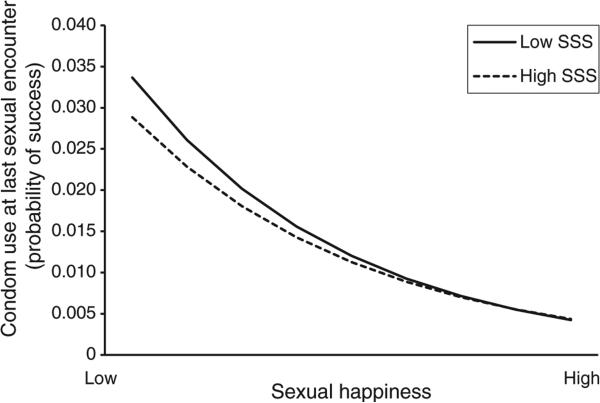
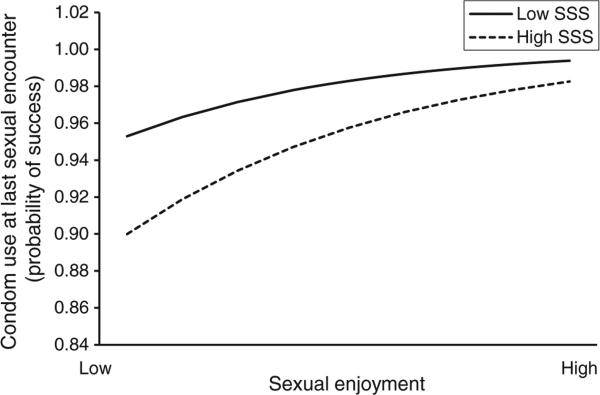
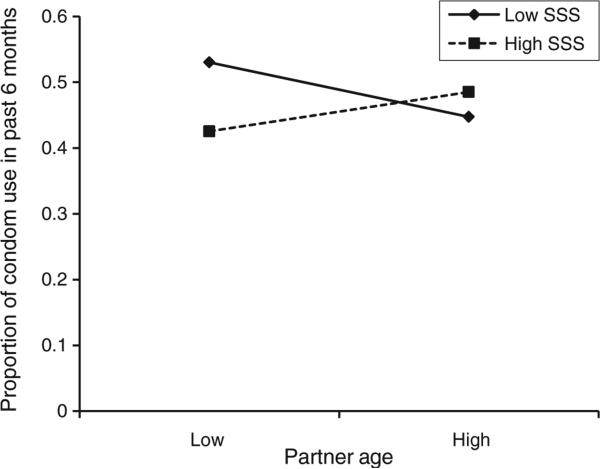
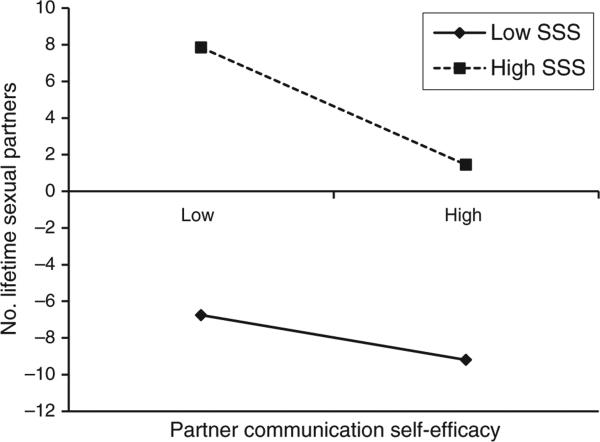
The results of the multivariate models are presented in Table 2. The logistic model predicting condom use at last sexual intercourse was statistically significant (χ2 = 25.93; P ≤ 0.05). Greater sexual enjoyment and higher levels of sexual happiness were associated with more frequent reported condom use at last intercourse. For adolescents who reported greater SSS, less emphasis on sexual happiness was associated with a decreased likelihood of condom use at last intercourse compared to those with lower SSS (P ≤ 0.05; Fig. 1). For those reporting lower levels of SSS, greater sexual enjoyment was associated with a greater likelihood of condom use at last intercourse (P ≤ 0.01; Fig. 2). The model predicting the proportion of condom use in the past 6 months was statistically significant (F(9, 536) = 3.65; P ≤ 0.001; R2 = 0.06). Youth with older partners reported a lower proportion of condom use in the past 6 months. Adolescents with younger sexual partners and lower levels of SSS reported a greater proportion of condom use in the past 6 months (β = 0.70, P ≤ 0.01; Fig. 3). The model predicting the number of lifetime sexual partners was statistically significant (F(9, 536) = 5.01; P ≤ 0.001; R2 = 0.08). Greater SSS was associated with a greater number of lifetime sexual partners. Higher levels of partner communication self-efficacy and decreasing levels of SSS were associated with fewer lifetime sexual partners (β = –0.54, P ≤ 0.05; Fig. 4).
Table 2.
Multiple regression analysis for sexual attitudes, partner communication and partner age predicting sexual risk (n = 546)
| Condom use at last sexual encounter | Proportion of condom use in the past 6 months | Lifetime sexual partners | ||||
|---|---|---|---|---|---|---|
| Exp(B) | P-value | β | P-value | β | P-value | |
| Partner communication | 0.95 | 0.66 | 0.11 | 0.52 | 0.16 | 0.34 |
| Partner age measure | 0.52 | 0.18 | –0.45 | 0.01* | 0.24 | 0.19 |
| Enjoyment of sex | 3.12 | 0.02* | –0.01 | 0.97 | –0.01 | 0.98 |
| Sexual sensation-seeking | 0.80 | 0.20 | –0.52 | 0.16 | 0.95 | 0.008** |
| Sexual happiness | 0.82 | 0.02* | –0.09 | 0.67 | 0.35 | 0.07 |
| Interaction terms | ||||||
| Partner communication × sexual sensation | 1.01 | 0.31 | 0.03 | 0.90 | –0.54 | 0.04* |
| Sexual happiness × sexual sensation | 1.01 | 0.04* | –0.01 | 0.99 | –1.82 | 0.07 |
| Enjoyment of sex × sexual sensation | 0.93 | 0.009** | –0.13 | 0.67 | 0.04 | 0.89 |
| Partner age × sexual sensation | 1.03 | 0.20 | 0.70 | 0.01* | –0.15 | 0.57 |
P<0.05
P<0.01
Fig. 1.
Interactive effect of sexual happiness and sexual sensation-seeking (SSS) on condom use at the last sexual encounter.
Fig. 2.
Interactive effect of sexual enjoyment and sexual sensation-seeking (SSS) on condom use at the last sexual encounter.
Fig. 3.
Interactive effect of partner age and sexual sensation-seeking (SSS) on the proportion of condom use in the past 6 months.
Fig. 4.
Interactive effect of partner communication and sexual sensation-seeking (SSS) on the number of lifetime sexual partners.
Discussion
Using the theory of gender and power as a framework, the purpose of the current study was to examine the impact of SSS on the relationships among partner age differences, sexual attitudes, partner communication self-efficacy, condom use and number of sexual partners among female African-American adolescents attending sexual health-based clinics in Atlanta, Georgia. Overall, the African-American female adolescents in our sample reported moderate to high levels of sexual risk, such that participants reported low proportions of condom use, less than half used a condom the last time they had sex and most reported high numbers of lifetime sexual partners. These findings point to the importance of examining the moderators of sexual risk within this population. Despite these potentially problematic behaviours, adolescent females in this study reported high levels of partner communication self-efficacy. These findings are important because they may indicate that perceived power differentials in the context of sexual intercourse may not have been an issue for these youth. Greater partner communication self-efficacy among the African-American female adolescents in this sample may be indicative of greater perceived agency in sexual relationships. Moreover, these findings may suggest that sexual risk within this population of African-American females is bidirectional rather than unidirectional (i.e. controlled by male partners), as might be the case if power differentials were perceived.
Partner age
The results of this study indicated that partner age had a significant impact on sexual risk. Consistent with previous studies,32 youth with sexual partners who were closer to their age or younger reported less sexual risk. Furthermore, for female youth with younger male partners, lower levels of SSS predicted more consistent condom use. The relationship between SSS and younger partners may reflect a shift in power in the relationship, such that females feel more empowered to insist on condom use or may be more likely to select partners who have a shared desire to avoid the negative consequences of RSB, which include STIs and unwanted pregnancy. Consistent with previous studies showing that having an older sexual partner increased sexual risk33,34 and inconsistent with studies demonstrating no effect of partner age,35 our study linked adolescents with older sexual partners to inconsistent condom use over the past 6 months. Although partner age is important, partner communication self-efficacy is also a factor in adolescents’ decision to engage in RSB.
Partner communication
For individuals with low levels of SSS, higher partner communication self-efficacy predicted fewer lifetime sexual partners. This finding extends previous research that has linked partner communication with contraceptive use.12,27,28 Adolescent females who feel comfortable asking their partners about their sexual histories and contraceptive practices may experience a sense of closeness and comfort with their partners that enables them to remain in the relationship, thus limiting the number of lifetime partners. Importantly, in our study, the relationship between parent communication and number of sexual partners was moderated by SSS, thus demonstrating that the protective role of communication was only observed among those with low levels of SSS. Like partner communication, sexual attitudes are an important factor in predicting adolescent sexual risk.
Sexual attitudes
Although our study showed that youth with lower levels of SSS who reported greater sexual enjoyment had an increased likelihood of condom use at the last sexual encounter, we also found the interaction between SSS and sexual happiness predicted increased sexual risk behaviour. For adolescents with higher levels of SSS, lower levels of sexual happiness were associated with less condom use at last sex. This finding of increased risk supports a recent study showing that higher SSS predicts a higher number of lifetime sexual partners among African-American females attending STI clinics in Georgia.36 It is possible that youth with higher levels of SSS may find it difficult to achieve lasting sexual happiness. They may be more interested in the thrill of having new sexual experiences rather than seeking emotional connection with current partners, which could lead to less consistent condom use. These findings support our premise that adolescent SSS is an important predictor of sexual risk, as the level of SSS appears to be consistently inversely related to condom use at last intercourse in the presence of other measures of sexual attitudes.
Limitations
We have noted limitations of the current study. First, self-report data is inherently subject to bias and could lead to concerns about internal and construct validity. However, using the audio computer-assisted self-interview method to gather information could reduce such bias, as shown in previous studies.37 Next, individual measures of sexual risk may be subject to bias. For example, condom use at last intercourse may not represent an adolescent's typical sexual practices, which could lead to underestimation or overestimation of behaviours. Furthermore, other measures, such as condom use over the past 6 months, may be subject to recall bias. However, we attempted to address this limitation, as well as the limitation in using a single measure within a single timeframe, by analysing multiple timeframes for each outcome measure to improve our ability to capture the diversity present in adolescent sexual behaviour. Finally, we cannot be certain that the results of our study are generalisable beyond the current sample of African-American female adolescents receiving services in Atlanta, Georgia. Thus extension of the current findings to males and other ethnic groups should be done with caution in the absence of additional research.
Conclusions
Partner age, partner communication self-efficacy and sexual attitudes are important antecedents of RSB for African-American female adolescents. However, interventions aimed at female adolescents may need to include components that are explicitly focussed on the way in which SSS tendencies may interact with antecedents of sexual risk to impact actual sexual risk. As the presence of SSS paired with some sexual attitudes (i.e. sexual happiness and sexual enjoyment) was not consistently associated with increased sexual risk, more research is needed to determine the nature of these relationships and the conditions under which sexual attitudes lead to increased risk.10,37
Footnotes
Conflicts of interest
None declared.
References
- 1.Centers for Disease Control and Prevention . Sexually transmitted disease Surveillance. U.S. Department of Health and Human Services; Atlanta: 2011. 2012. [Google Scholar]
- 2.Reif S, Geonnotti KL, Whetten K. HIV infection and AIDS in the Deep South. Am J Public Health. 2006;96:970–3. doi: 10.2105/AJPH.2005.063149. doi:10.2105/AJPH.2005.063149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Williams PB, Ekundayo O, Udezulu IE, Omishakin AM. An ethnically sensitive and gender-specific HIV/AIDS assessment of African American women: a comparative study of urban and rural American communities. Fam Community Health. 2003;26:108–23. doi: 10.1097/00003727-200304000-00004. doi:10.1097/00003727-200304000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention . A heightened national response to the HIV/AIDS crisis among African Americans. Department of Health and Human Services; Atlanta: 2007. [Google Scholar]
- 5.DiClemente RJ, Salazar LF, Crosby RA, Rosenthal SL. Prevention and control of sexually transmitted infections among adolescents: the importance of a socio-ecological perspective: a commentary. Public Health. 2005;119:825–36. doi: 10.1016/j.puhe.2004.10.015. doi:10.1016/j.puhe.2004.10.015. [DOI] [PubMed] [Google Scholar]
- 6.Crosby RA, DiClemente RJ, Wingood GM, Salazar LF, Head S, Rose E, et al. Sexual agency versus relational factors: a study of condom use antecedents among high-risk young African American women. Sex Health. 2008;5:41–7. doi: 10.1071/sh07046. doi:10.1071/SH07046. [DOI] [PubMed] [Google Scholar]
- 7.Wingood GM, DiClemente RJ. The theory of gender and power: a social structural theory for guiding public health interventions. In: DiClemente RJ, Kegler MC, editors. Emerging theories in health promotion practice and research: strategies for improving public health. Jossey-Bass; San Francisco: 2002. pp. 313–46. [Google Scholar]
- 8.Senn TE, Carey MP. Age of partner at first adolescent intercourse and adult sexual risk behavior among women. J Womens Health (Larchmt) 2011;20:61–6. doi: 10.1089/jwh.2010.2089. doi:10.1089/jwh.2010.2089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sales JM, Lang DL, DiClemente RJ, Latham TP, Wingood GM, Hardin JW. The mediating role of partner communication frequency on condom use among African American adolescent females participating in an HIV prevention intervention. Health Psychol. 2012;31:63–9. doi: 10.1037/a0025073. doi:10.1037/a0025073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rostosky SS, Dekhtyar O, Cupp PK, Anderman EM. Sexual self-concept and sexual self-efficacy in adolescents: a possible clue to promoting sexual health? J Sex Res. 2008;45:277–86. doi: 10.1080/00224490802204480. doi:10.1080/ 00224490802204480. [DOI] [PubMed] [Google Scholar]
- 11.Higgins JA, Hirsch JS. The pleasure deficit: revisiting the “sexuality connection” in reproductive health. Perspect Sex Reprod Health. 2007;39:240–7. doi: 10.1363/3924007. doi:10.1363/3924007. [DOI] [PubMed] [Google Scholar]
- 12.Sales JM, Smearman EL, Brody GH, Milhausen R, Philibert RA, DiClemente RJ. Factors associated with sexual arousal, sexual sensation seeking and sexual satisfaction among female African American adolescents. Sex Health. 2013;10:512–21. doi: 10.1071/SH13005. doi:10.1071/SH13005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kalichman SC, Johnson JR, Adair V, Rompa D, Multhauf K, Kelly JA. Sexual sensation seeking: scale development and predicting AIDS-risk behavior among homosexually active men. J Pers Assess. 1994;62:385–97. doi: 10.1207/s15327752jpa6203_1. doi:10.1207/s15327752jpa6203_1. [DOI] [PubMed] [Google Scholar]
- 14.Spitalnick JS, DiClemente RJ, Wingood GM, Crosby RA, Milhausen RR, Sales JM, et al. Brief report: sexual sensation seeking and its relationship to risky sexual behaviour among African American adolescent females. J Adolesc. 2007;30:165–73. doi: 10.1016/j.adolescence.2006.10.002. doi:10.1016/j.adolescence.2006.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Charnigo R, Noar SM, Garnett C, Crosby R, Palmgreen P, Zimmerman RS. Sensation seeking and impulsivity: combined associations with risky sexual behavior in a large sample of young adults. J Sex Res. 2013;50:480–8. doi: 10.1080/00224499.2011.652264. doi:10.1080/00224499.2011. 652264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zuckerman M. Behavioral expressions and biosocial bases of sensation seeking. Cambridge University Press; Cambridge, NY: 1994. [Google Scholar]
- 17.Crawford AM, Pentz MA, Chou CP, Li C, Dwyer JH. Parallel developmental trajectories of sensation seeking and regular substance use in adolescents. Psychol Addict Behav. 2003;17:179–92. doi: 10.1037/0893-164X.17.3.179. doi:10.1037/0893-164X.17.3.179. [DOI] [PubMed] [Google Scholar]
- 18.Ford K, Sohn W, Lepkowski J. Characteristics of adolescents’ sexual partners and their association with use of condoms and other contraceptive methods. Fam Plann Perspect. 2001;33:100–5. 132. doi:10.2307/2673765. [PubMed] [Google Scholar]
- 19.Darroch JE, Landry DJ, Oslak S. Age differences between sexual partners in the United States. Fam Plann Perspect. 1999;31:160–7. doi:10.2307/2991588. [PubMed] [Google Scholar]
- 20.Ompad DC, Strathdee SA, Celentano DD, Latkin C, Poduska JM, Kellam MD, et al. Predictors of early initiation of vaginal and oral sex among urban young adults in Baltmore, Maryland. Arch Sex Behav. 2006;35:53–65. doi: 10.1007/s10508-006-8994-x. doi:10.1007/s10508-006-8994-x. [DOI] [PubMed] [Google Scholar]
- 21.Begley E, Crosby RA, DiClemente RJ, Wingood GM, Rose E. Older partners and STD prevalence among pregnant African American teens. Sex Transm Dis. 2003;30:211–3. doi: 10.1097/00007435-200303000-00006. doi:10.1097/00007435-200303000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Manlove J, Terry-Humen E, Ikramullah E. Young teenagers and older sexual partners: correlates and consequences for males and females. Perspect Sex Reprod Health. 2006;38:197–207. doi: 10.1363/psrh.38.197.06. doi:10.13 63/3819706. [DOI] [PubMed] [Google Scholar]
- 23.Bouchey HA. Perceived romantic competence, importance of romantic domains, and psychosocial adjustment. J Clin Child Adolesc Psychol. 2007;36:503–14. doi: 10.1080/15374410701653120. doi:10.1080/15374410701653120. [DOI] [PubMed] [Google Scholar]
- 24.Ryan S, Franzetta K, Manlove J, Holcombe E. Adolescents’ discussions about contraception or STDs with partners before first sex. Perspect Sex Reprod Health. 2007;39:149–57. doi: 10.1363/3914907. doi:10.1363/39 14907. [DOI] [PubMed] [Google Scholar]
- 25.Widman L, Welsh D, McNulty JK, Little KC. Sexual communication and contraceptive use in adolescent dating couples. J Adolesc Health. 2006;39:893–9. doi: 10.1016/j.jadohealth.2006.06.003. doi:10.1016/j.jadohealth.2006.06.003. [DOI] [PubMed] [Google Scholar]
- 26.Davies SL, DiClemente RJ, Wingood GM, Person SD, Dix ES, Harrington K, et al. Predictors of inconsistent contraceptive use among adolescent girls: findings from a prospective study. J Adolesc Health. 2006;39:43–9. doi: 10.1016/j.jadohealth.2005.10.011. doi:10.1016/j.jadohealth.2005. 10.011. [DOI] [PubMed] [Google Scholar]
- 27.Bowleg L, Lucas KJ, Tschann JM. “The ball was always in his court”: an exploratory analysis of relationship scripts, sexual scripts, and condom use among African American women. Psychol Women Q. 2004;28:70–82. doi:10.1111/j.1471-6402.2004.00124.x. [Google Scholar]
- 28.Centers for Disease Control and Prevention (CDC) Trends in HIV-related risk behaviors among high school students: United States, 1991–2011. MMWR Morb Mortal Wkly Rep. 2012;61:556–60. [PubMed] [Google Scholar]
- 29.Impett EA, Tolman DL. Late adolescent girls’ sexual experiences and sexual satisfaction. J Adolesc Res. 2006;21:628–46. doi:10.1177/0743558406293964. [Google Scholar]
- 30.Higgins JA, Hoffman S, Graham CA, Sanders SA. Relationships between condoms, hormonal methods, and sexual pleasure and satisfaction: an exploratory analysis from the Women's Well-Being and Sexuality Study. Sex Health. 2008;5:321–30. doi: 10.1071/sh08021. doi:10.1071/ SH08021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wingood GM, DiClemente RJ. Partner influences and gender-related factors associated with non-condom use among young adult African American women. Am J Community Psychol. 1998;26:29–51. doi: 10.1023/a:1021830023545. doi:10.1023/A:1021830023545. [DOI] [PubMed] [Google Scholar]
- 32.Bauermeister JA, Zimmerman MA, Caldwell CH, Xue Y, Gee GC. What predicts sex partners’ age differences among African American youth? A longitudinal study from adolescence to young adulthood. J Sex Res. 2010;47:330–44. doi: 10.1080/00224490903015850. doi:10.1080/00224490903015850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Staras SA, Livingston MD, Maldonado-Molina MM, Komro KA. The influence of sexual partner on condom use among urban adolescents. J Adolesc Health. 2013;53:742–8. doi: 10.1016/j.jadohealth.2013.06.020. doi:10.1016/j.jado health.2013.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Volpe EM, Hardie TL, Cerulli C, Sommers MS, Morrison-Beedy D. What's age got to do with it? Partner age difference, power, intimate partner violence, and sexual risk in urban adolescents. J Interpers Violence. 2013;28:2068–87. doi: 10.1177/0886260512471082. doi:10.1177/0886260512471082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kissinger P, Clayton JL, O'Brien ME, Kent C, Whittington WL, Oh MK, et al. Older partners not associated with recurrence among female teenagers infected with Chlamydia trachomatis. Sex Transm Dis. 2002;29:144–9. doi: 10.1097/00007435-200203000-00004. doi:10.1097/00007435-200203000-00004. [DOI] [PubMed] [Google Scholar]
- 36.Voisin DR, Tan K, DiClemente RJ. A longitudinal examination of the relationship between sexual sensation seeking and STI-related risk factors among African American females. AIDS Educ Prev. 2013;25:124–34. doi: 10.1521/aeap.2013.25.2.124. doi:10.1521/aeap.2013.25.2.124. [DOI] [PubMed] [Google Scholar]
- 37.O'Sullivan LF, Meyer-Bahlburg HFL, McKeague IW. The development of the sexual self-concept inventory for early adolescent girls. Psychol Women Q. 2006;30:139–49. doi:10.1111/ j.1471-6402.2006.00277.x. [Google Scholar]