Abstract
Background
Contrast-induced nephropathy (CIN) has been traditionally associated with increased mortality and adverse cardiovascular events. We sought to determine whether CIN has a negative impact on the long-term outcome of patients with non-ST segment elevation myocardial infarction (NSTEMI).
Methods
A total of 312 consecutive patients (mean age 59 years, 76% male) who presented with NSTEMI and had undergone an early invasive procedure were retrospectively included. CIN was defined as either a 25% or 0.5-mg/dl increase in baseline serum creatinine (Cr) 72 h after the procedure. The primary endpoint of the study was mortality in the long-term follow-up (38 months, interquartile range 30-40). The secondary endpoint consisted of mortality and myocardial infarction (MI).
Results
CIN developed in 30 (9.6%) patients. Independent predictors of CIN were the contrast volume-to-Cr clearance ratio, left ventricular ejection fraction and hemoglobin concentration. The primary (20 vs. 8.5%, p = 0.042) and secondary endpoints (33.3 vs. 17%, p = 0.029) were observed more frequently in patients with CIN during long-term follow-up. The unadjusted odds ratio (OR) of CIN was 2.55 [95% confidence intervals (CI) 1.04-6.24, p = 0.040] for mortality and 2.15 (CI 1.09-4.25, p = 0.028) for mortality/MI. However, after adjustment for confounding factors, CIN was not an independent predictor of either mortality (OR 1.62, CI 0.21-12.57, p = 0.646) or mortality/MI (OR 1.12, CI 0.31-4.0, p = 0.860).
Conclusion
The effect of CIN on the long-term outcome of patients with NSTEMI was substantially influenced by confounding factors. CIN was a marker, rather than a mediator, of increased cardiovascular risk, and the baseline renal function was more conclusive as a long-term prognosticator.
Key Words: Contrast media, Acute kidney injury, Myocardial infarction, Mortality
Introduction
Contrast-induced nephropathy (CIN) has been traditionally associated with permanent renal dysfunction, longer hospital stay, increased adverse cardiovascular events (ACEs) and mortality [1,2]. Whether after diagnostic or interventional, elective or emergent procedures, the majority of studies about long-term outcome of patients with CIN reported that development of CIN was one of the independent predictors of mortality and ACEs [3,4,5,6]. It is remarkable that the predictive power of CIN on outcome is relevant with different definitions. However, CIN is known to be a self-limiting condition, and transformation to permanent renal dysfunction is seldom, especially in patients with normal renal function [7,8]. The aim of the present work is to investigate whether CIN has a negative impact on the long-term outcome of patients with non-ST elevation myocardial infarction (NSTEMI) which is characterized by comorbidities and recurrent ACEs in the long term.
Methods
Patients
We retrospectively enrolled consecutive patients admitted with a NSTEMI diagnosis between January 2009 and December 2011. Patients who underwent coronary angiography (CA) and intervention (if necessary) as a part of an early invasive strategy were included. Exclusion criteria were (1) chronic hemodialysis therapy for end-stage renal failure, (2) presentation with acute renal failure (ARF), (3) previous exposure to a contrast agent within 7 days, and (4) patients with unstable hemodynamics or requiring an emergency coronary intervention.
In order to be included in the analysis, patients must have had one creatinine (Cr) value before and one Cr value within 72 h after the coronary procedure. Creatinine clearance (CrCl) was calculated by the Cockroft-Gault formula: [140 age] × weight (kg) / Cr (mg/dl) × 72 (corrected by 0.85 for females). Prophylactic hydration or other preventive measures (N-acetyl cysteine, sodium bicarbonate) were used at the clinicians' discretion. Low osmolar contrast agents (iopamidol or iopromide) were used throughout the study, and the choice of the contrast agent was determined by availability in our institution. The total amount of contrast media used during all procedures was recorded. Ad hoc percutaneous coronary intervention (PCI) was performed if clinically indicated. CIN was defined as either a 25% or 0.5-mg/dl increase in baseline Cr concentration. The study was approved by the local ethics committee (Clinical Research Ethics Committee of the Faculty of Medicine of Kocaeli University, No.: KOÜ KAEK 2013/19).
Follow-Up Definitions
In-hospital clinical events such as development of acute heart failure, hemodialysis, bleeding requiring transfusion, cerebrovascular accidents, re-infarction, intra-aortic balloon pump use, cardiopulmonary resuscitation and death as well as total length of hospital stay were obtained from hospital records. Long-term follow-up data was obtained from either hospital records or phone calls carried out for patients who did not attend regular outpatient visits. Patients not contacted despite of best effort were excluded from the analysis. The primary endpoint of the study was long-term all-cause mortality. The secondary endpoint consisted of mortality and nonfatal myocardial infarction (MI). All cases of MI were source-documented. Long-term follow-up ended in December 2013, and patients were considered censored if no mortality or MI was observed during the follow-up period.
Statistical Analysis
Continuous variables were presented as means (standard deviations) or medians (interquartile ranges) if they did not show normal distribution. Categorical variables were presented as percentages. Patients were divided into two groups according to the development of CIN after the coronary procedure. Comparison of the groups was performed by independent samples t test or Mann-Whitney U test for continuous variables. Categorical variables were compared by the χ2 or Fisher's exact test. Independent predictors of CIN were analyzed using multivariate logistic regression analysis. Comparison of in-hospital events was performed using the χ2 test. Long-term survival was evaluated with the Kaplan-Meier survival analysis. Differences between two groups were measured with the log-rank test. Independent correlates of long-term ACEs were analyzed using Cox-regression analysis. Results were tabulated as odds ratios (OR) with 95% confidence intervals (CI). A two-sided p value <0.05 was considered significant.
Results
Patients
A total of 520 patients were admitted with a diagnosis of NSTEMI between January 2009 and December 2011, and 446 (86%) patients were managed with early invasive management. There were 11 patients with unstable hemodynamics who required an emergency intervention, 23 patients without baseline Cr, 3 patients with previous exposure to contrast agent within 1 week and 6 patients with end-stage renal failure. Fifty-nine patients had no Cr follow-up within 72 h after coronary intervention. The remaining 346 patients were included in the study. Thirty-four of them neither had hospital follow-up records nor could be contacted by phone call and were excluded from the analysis. Baseline demographics and clinical characteristics of patients without follow-up data were comparable to the main study population. Finally, the study population consisted of 312 patients with long-term follow-up data.
Incidence and Predictors of CIN
Baseline demographic and clinical characteristics of the patients are presented in table 1. Thirty (9.6%) patients developed CIN according to the definition. Patients who developed CIN had significantly lower left ventricular ejection fraction (LVEF) and hemoglobin concentration. Baseline Cr and CrCl were not different between the two groups (table 2). However, patients with a baseline CrCl <60 ml/min and CrCl <30 ml/min were more common in the CIN group. Both groups received similar amount of contrast agent during the intervention, but the contrast volume-to-CrCl ratio was significantly higher in patients developing CIN. The severity of the coronary artery disease and the subsequent management of patients were comparable between the two groups (table 3).
Table 1.
Baseline demographics and clinical characteristics of the study population
| All patients (n = 312) | Patients with CIN (n = 30) | Patients without CIN (n = 282) | p | |
|---|---|---|---|---|
| Demographics | ||||
| Age, years | 59 (12) | 61 (13) | 59 (12) | 0.409 |
| Male gender, % | 76.0 | 70.0 | 76.6 | 0.422 |
| Hypertension, % | 62.5 | 73.3 | 63.3 | 0.197 |
| Diabetes, % | 29.6 | 36.7 | 28.8 | 0.371 |
| Smoking, % | 43.2 | 44.8 | 43.1 | 0.855 |
| Dyslipidemia, % | 51.8 | 43.3 | 52.7 | 0.331 |
| Body mass index | 28.3 (4.5) | 27.7 (3.9) | 28.4 (4.6) | 0.411 |
| Previous CABG, % | 10.6 | 13.3 | 10.3 | 0.606 |
| Previous PCI, % | 14.1 | 13.3 | 14.2 | 0.899 |
| Clinical findings | ||||
| Duration of chest pain, h | 2 (0.5–3.1) | 2 (0.75–4.5) | 1.5 (0.5–3) | 0.488 |
| Peak troponin I, ng/ml | 0.69 (0.18–2.71) | 1.05 (0.13–3.14) | 0.66 (0.18–270) | 0.397 |
| LVEF, % | 52 (10) | 47 (10) | 53 (10) | 0.006 |
| ST segment depression, % | 26.4 | 33.3 | 25.6 | 0.362 |
| Left bundle branch block, % | 5.5 | 6.7 | 5.4 | 0.768 |
| Killip class >1, % | 4.5 | 6.7 | 4.3 | 0.544 |
| SBP, mm Hg | 130 (19) | 129 (18) | 131 (21) | 0.467 |
| DBP, mm Hg | 76 (11) | 77 (12) | 74 (14) | 0.642 |
| Laboratory findings | ||||
| Serum Cr, mg/dl | 1.04 (0.90–1.22) | 1.05 (0.84–1.42) | 1.04 (0.90–1.21) | 0.194 |
| Glucose, mg/dl | 112 (95–150) | 120 (93–167) | 110 (95–147) | 0.320 |
| Total cholesterol, mg/dl | 189 (49) | 182 (59) | 189 (48) | 0.491 |
| LDL cholesterol, mg/dl | 114 (37) | 108 (42) | 115 (37) | 0.354 |
| HDL cholesterol, mg/dl | 40 (10) | 44 (13) | 40 (10) | 0.024 |
| Triglyceride, mg/dl | 153 (106–210) | 139 (94–173) | 154 (108–210) | 0.335 |
| Hemoglobin, g/dl | 13.3 (12.0–14.5) | 12.2 (10.5–13.7) | 13.3 (12.1–14.5) | 0.001 |
| WBC, 103/ml | 8.6 (7.0–10.6) | 8.6 (6.5–12.2) | 8.6 (7.0–10.4) | 0.212 |
| Platelets, 103/ml | 244 (71) | 254 (103) | 243 (66) | 0.590 |
Continuous variables are means (standard deviations) or medians (interquartile ranges).
Table 2.
Pre- and postprocedural renal functions
| Patients with CIN | Patients without CIN | p | |
|---|---|---|---|
| Baseline Cr, mg/dl | 1.05 (0.84–1.42) | 1.04 (0.90–1.21) | 0.194 |
| Baseline CrCl, ml/min | 65 (44–113) | 84 (63–105) | 0.180 |
| CrCl <90 ml/min, % | 60.0 | 57.1 | 0.759 |
| CrCl <60 ml/min, % | 40.0 | 22.7 | 0.036 |
| CrCl <30 ml/min, % | 20.0 | 1.8 | 0.001 |
| Maximum Cr, mg/dl | 1.59 (1.06–3.99) | 1.14 (0.98–1.29) | 0.003 |
| Cr at discharge, mg/dl | 1.33 (1.02–2.70) | 1.07 (0.92–1.23) | 0.001 |
Continuous variables are medians (interquartile ranges).
Table 3.
Angiographic findings and subsequent management of the study population
| Patients with CIN | Patients without CIN | p | |
|---|---|---|---|
| Contrast volume, ml | 200 (100–275) | 150 (120–215) | 0.246 |
| Contrast volume/CrCl | 2.5 (1.2–4.2) | 1.8 (1.3–2.9) | 0.024 |
| One-vessel disease, % | 20.0 | 22.3 | 0.769 |
| Two-vessel disease, % | 26.7 | 25.2 | 0.828 |
| Three-vessel disease, % | 30.0 | 31.2 | 0.892 |
| Ad hoc PCI, % | 33.3 | 30.1 | 0.538 |
| Total PCI, % | 33.3 | 34.4 | 0.618 |
| CABG, % | 26.7 | 21.2 | 0.367 |
| Medical treatment, % | 40 | 33.6 | 0.452 |
Continuous variables are medians (interquartile ranges).
Predictors of CIN were evaluated with multivariate logistic regression analysis. The stepwise model (p > 0.10 for exclusion, p < 0.05 for inclusion at each step) included baseline characteristics (age, sex, diabetes, hypertension, smoking, systolic blood pressure, baseline Cr, baseline CrCl, and LVEF) and significant variables in univariate analysis (HDL cholesterol, contrast volume-to-CrCl ratio, and hemoglobin, p < 0.05 for all). The contrast volume-to-CrCl ratio (OR 1.294, CI 1.062-1.577, p = 0.011), LVEF (OR 0.950, CI 0.911-0.990, p = 0.015) and hemoglobin concentration (OR 0.755, CI 0.601-0.949, p = 0.016) were independent predictors of CIN.
In-Hospital and Long-Term Events
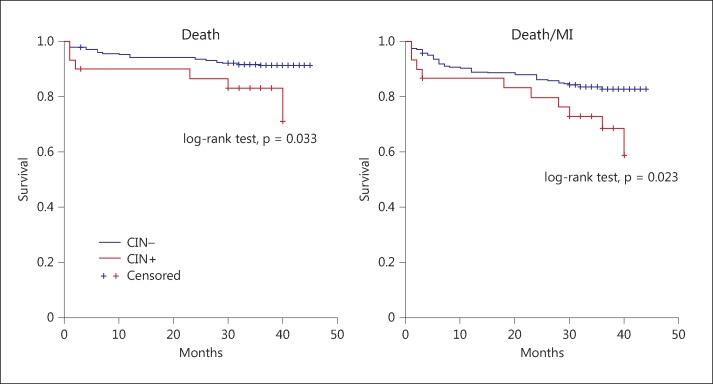
CIN patients experienced more clinical events and stayed longer in hospital compared to patients without CIN (table 4). The median follow-up time was 38 months (interquartile range 30-40). Mortality was observed in 20% of patients with CIN the in long-term follow-up, whereas it was 8.5% in patients without CIN (p = 0.042). Nonfatal MI was seen more frequently in patients with CIN compared to patients without CIN as well (23.3 vs. 10.6%, p = 0.041). When two hard endpoints were considered together, death or nonfatal MI was more frequent in patients with CIN compared to patients without CIN (33.3 vs. 17%, p = 0.029). The Kaplan-Meier survival analysis of two endpoints of the study was presented in figure 1. Time to death (log-rank test, χ2: 4.6, p = 0.033) and time to death or MI (log-rank test, χ2: 5.1, p = 0.023) were significantly shorter in patients with CIN.
Table 4.
In-hospital clinical events
| Patients with CIN | Patients without CIN | p | |
|---|---|---|---|
| Death, % | 3.3 | 1.1 | 0.334 |
| Reinfarction, % | 0 | 2.5 | 1.000 |
| Cardiopulmonary resuscitation, % | 10 | 1.4 | 0.022 |
| Supraventricular arrhythmia, % | 6.7 | 4.6 | 0.645 |
| Pulmonary edema, % | 20 | 4.3 | <0.001 |
| Intra-aortic balloon pump use, % | 3.3 | 0.4 | 0.183 |
| Bleeding requiring transfusion, % | 13.3 | 3.9 | 0.045 |
| Cerebrovascular accident, % | 3.3 | 0.7 | 0.262 |
| Hemodialysis, % | 6.7 | 0 | 0.009 |
| Length of hospital stay, days | 9 (7–16) | 7 (5–9) | 0.001 |
Continuous variables are medians (interquartile ranges).
Fig. 1.
Kaplan-Meier survival analysis of patients with and without CIN.
Predictors of Long-Term Outcome
Independent predictors of mortality and mortality or MI were analyzed using Cox regression analysis. The stepwise model included age, sex, diabetes, hypertension, smoking, previous CABG, previous PCI, cholesterol (total, LDL and HDL), duration of chest pain, peak troponin level, ST segment depression, left bundle branch block, LVEF, presence of multivessel disease, baseline Cr, CrCl, Cr at hospital discharge, CrCl at hospital discharge, hemoglobin concentration and CIN. Again p >0.100 and p <0.050 were selected for exclusion and inclusion of variables at each step, respectively. The results of the Cox-regression analysis for each endpoint are presented in table 5. While the development of CIN was associated with mortality (OR 2.550, CI 1.042-6.240, p = 0.040) and mortality or MI (OR 2.148, CI 1.087-4.247, p = 0.028) in univariate analysis, after adjustment for confounding factors, it was not independently associated with mortality and mortality or MI, suggesting that a causal relationship does not exist.
Table 5.
Independent correlates of long-term outcomes and the adjusted effect of CIN
| Wald χ2 | OR | 95% CI | p | |
|---|---|---|---|---|
| Death | ||||
| LVEF | 10.3 | 0.948 | 0.918–0.980 | 0.001 |
| CrCl | 10.3 | 0.979 | 0.967–0.992 | 0.001 |
| Duration of chest pain | 6.5 | 1.018 | 1.004–1.033 | 0.011 |
| Multivessel disease | 4.6 | 4.992 | 1.535–16.237 | 0.032 |
| Hypertension | 2.9 | 2.606 | 0.877–7.744 | 0.085 |
| CIN | 0.2 | 1.616 | 0.208–12.568 | 0.646 |
| Death/Ml | ||||
| LVEF | 17.0 | 0.947 | 0.922–0.972 | <0.001 |
| Hypertension | 9.0 | 3.485 | 1.539–7.889 | 0.003 |
| Previous PCI | 8.0 | 2.383 | 1.303–4.358 | 0.005 |
| Baseline Cr | 7.3 | 2.702 | 1.311–5.566 | 0.007 |
| Hemoglobin | 4.6 | 0.862 | 0.752–0.987 | 0.031 |
| CrCl at discharge | 4.5 | 0.990 | 0.980–0.999 | 0.034 |
| LDL cholesterol | 4.3 | 1.008 | 1.000–1.015 | 0.038 |
| Duration of chest pain | 3.9 | 1.011 | 1.000–1.021 | 0.049 |
| CIN | 0.031 | 1.121 | 0.313–4.018 | 0.860 |
Discussion
This study was composed of consecutive NSTEMI patients with all stages of renal function (CrCl <60 ml/min in 24% of patients). CIN occurred in about 10% of the study population (8% of patients with CrCl >60 ml/min, 15% of patients with CrCl <60 ml/min, p = 0.096). It is about in the middle of the published rates of CIN after coronary procedures which is as low as 2% for patients with normal renal function [2] and up to 20-30% for patients with moderate to severe renal function [7].
Previous studies have shown that CIN was associated with increased in-hospital mortality and morbidity [3,4,5,6]. We confirmed that patients with CIN suffered from more clinical events and stayed longer in hospital compared to patients without CIN. All complications of NSTEMI except reinfarction were seen more frequently in patients with CIN. However, adverse events during hospitalization or short-term follow-up should be viewed as consequences of ARF, not the contrast exposure per se. In fact, short-term outcome can be explained by acute kidney injury of any etiology [9]. Additionally, poor short-term prognosis is related to common clinical conditions predicting both CIN and ACEs (e.g., left ventricular dysfunction, anemia, renal insufficiency). In agreement with these findings, observational studies demonstrated that acute coronary syndrome patients with chronic kidney disease (CKD) were less likely to undergo CA compared to patients without CKD [10,11,12]. Concern about the adverse consequences of CIN leads providers to a suboptimal use of interventional strategies in these patients. Moreover, patients developing CIN after CA were treated rather conservatively to avoid further deterioration in renal function in observational studies as well as in daily practice. This results in a suboptimal performance of interventional procedures that can affect long-term survival adversely.
On the contrary, long-term cardiovascular risks associated with CKD are well established. Patients with CKD have more cardiovascular risk factors; however, renal insufficiency is associated with increased cardiovascular risk independent of all other measured variables [13,14]. Nonetheless, it is less clear how transient decline in renal function might increase the long-term risks aside from the fact that CIN is a marker of total burden of comorbidities. Numerous studies have associated long-term outcome with acute kidney injury after contrast exposure. Rihal et al. [15] reported that ARF after PCI was an independent correlate of in-hospital mortality. Additionally, patients with ARF after PCI showed a higher rate of mortality or MI in the 4-year follow-up. One-year ACEs were found to be significantly higher in patients with CIN in the Cardiac Angiography in Renally Impaired Patients (CARE) study which defined CIN as an increase of 25% in cystatin C, and the authors proposed a causal role for CIN [16]. Similarly, CIN was found to be one of the most powerful predictors of 1-year mortality after PCI regardless of the baseline renal functional status [17].
We have observed that in consecutive patients with NSTEMI, CIN was associated with higher long-term mortality and/or nonfatal MI. However, after adjustment for baseline clinical characteristics, CIN was not an independent predictor of mortality and/or nonfatal MI. We have also found that baseline renal function or renal function at hospital discharge was more important than the development of CIN with regard to long-term risks. The majority of previous studies, as well as the present study, which investigate long-term outcome, evaluated serum Cr only at 24-72 h or at hospital discharge. However, a study reported that 19% of CIN patients developed permanent renal dysfunction when evaluated at 3 months [18]. Other studies reported that renal function (or renal dysfunction) at 1-6 months after coronary procedures was a predictor of higher mortality [19,20]. It seems that evaluation of renal function within 72 h is too early to estimate its impact on the long-term outcome. We have found that CrCl at hospital discharge (median of 7 days in our study) could predict death/MI independently from other factors. Nevertheless, for mortality it was the baseline renal function (either Cr or CrCl) that predicted the long-term outcome. Without the knowledge of where the renal function settles after contrast exposure, proposition of predictive power of CIN is largely indirect. In our study group, we found that baseline renal function instead of CIN was predominant in determining long-term risks, possibly because the minority of patients have developed a worsening of renal function over the long-term follow-up. What we were not able to show was the temporal evolution of renal function, as the study was a retrospective analysis. We suggest that an increased incidence of CIN in high-risk patients and the fact that CIN may lead to a worse renal function over the long term underlies the predictive power of CIN on long-term outcomes described in previous studies. Alternatively, prospective studies of interventions preventing CIN that reduces the long-term consequences should demonstrate a causal relationship.
In a meta-analysis of observational studies, both mortality and ACEs were reported to be significantly higher in CIN patients after coronary procedures whether unadjusted or adjusted for baseline comorbidities [21]. In addition, the predictive power was relevant across different definitions (increase in serum Cr by 0.5 mg/dl or 25% vs. 1.0 mg/dl or 50%). Results were also similar between different clinical situations: CA, PCI, or STEMI. Pooled adjusted RR of mortality and ACEs were reported as 1.79 (CI 1.47-2.18) and 1.98 (CI 1.62-3.64), respectively. Nevertheless, the meta-analysis concluded that although a significant relationship exists between CIN and subsequent clinical outcomes, it is substantially influenced by confounding factors, and that the risk attributable to CIN is much lower than widely anticipated. Adjusted OR of death in our study (1.616, CI 0.208-12.568) was similar to what was reported in the meta-analysis, but statistically insignificant. We can propose that the effect of CIN on long-term outcomes is either absent or too small to be observed clinically.
Study Limitations
The retrospective design of this single-center study represents a limitation for several reasons: (i) kidney functions were not systematically followed in the long term. (ii) The revascularization decision might have had a big impact on the survival of patients. Especially, patients who received medical therapy alone could be regarded as such because of a poor renal function. (iii) Deterioration of renal function after CABG or PCI during follow-up could contribute to an adverse long-term outcome. (iv) The proportion of patients treated with optimal medical treatment or adherence to given medical treatment during follow-up was unknown.
Conclusion
Although CIN was associated with long-term outcomes in NSTEMI, its effect is substantially influenced by confounding factors. A causal relationship with long-term mortality or MI was either absent or too small to be clinically important in this study. CIN seems to be a marker, rather than a mediator, of increased cardiovascular risk, and the baseline renal function (serum Cr or CrCl) was a more conclusive long-term prognosticator. Permanent disturbance of kidney function, either chronic or acquired after contrast exposure, is more important than transient deterioration for long-term outcomes. Potential consequences of CIN should not preclude the performance of clinically indicated invasive procedures in high-risk patients.
Disclosure Statement
The authors declare that there are no conflicts of interest.
References
- 1.Weisbord SD, Chen H, Stone RA, Kip KE, Fine MJ, Saul MI, et al. Associations of increases in serum creatinine with mortality and length of hospital stay after coronary angiography. J Am Soc Nephrol. 2006;17:2871–2877. doi: 10.1681/ASN.2006030301. [DOI] [PubMed] [Google Scholar]
- 2.Rihal CS, Textor SC, Grill DE, Berger PB, Ting HH, Best PJ, et al. Incidence and prognostic importance of acute renal failure after percutaneous coronary intervention. Circulation. 2002;105:2259–2264. doi: 10.1161/01.cir.0000016043.87291.33. [DOI] [PubMed] [Google Scholar]
- 3.Roy P, Raya V, Okabe T, Pinto Slottow TL, Steinberg DH, Smith K, et al. Incidence, predictors, and outcomes of post-percutaneous coronary intervention nephropathy in patients with diabetes mellitus and normal baseline serum creatinine levels. Am J Cardiol. 2008;101:1544–1549. doi: 10.1016/j.amjcard.2008.02.035. [DOI] [PubMed] [Google Scholar]
- 4.Wi J, Ko YG, Kim JS, Kim BK, Choi D, Ha JW, et al. Impact of contrast-induced acute kidney injury with transient or persistent renal dysfunction on long-term outcomes of patients with acute myocardial infarction undergoing percutaneous coronary intervention. Heart. 2011;97:1753–1757. doi: 10.1136/hrt.2010.218677. [DOI] [PubMed] [Google Scholar]
- 5.Bouzas-Mosquera A, Vázquez-Rodríguez JM, Calviño-Santos R, Peteiro-Vázquez J, Flores-Ríos X, Marzoa-Rivas R, et al. Contrast-induced nephropathy and acute renal failure following urgent cardiac catheterization: incidence, risk factors, and prognosis (in Spanish) Rev Esp Cardiol. 2007;60:1026–1034. doi: 10.1157/13111234. [DOI] [PubMed] [Google Scholar]
- 6.Neyra JA, Shah S, Mooney R, Jacobsen G, Yee J, Novak JE. Contrast-induced acute kidney injury following coronary angiography: a cohort study of hospitalized patients with or without chronic kidney disease. Nephrol Dial Transplant. 2013;28:1463–1471. doi: 10.1093/ndt/gft082. [DOI] [PubMed] [Google Scholar]
- 7.McCullough PA, Wolyn R, Rocher LL, Levin RN, O'Neill WW. Acute renal failure after coronary intervention: incidence, risk factors, and relationship to mortality. Am J Med. 1997;103:368–375. doi: 10.1016/s0002-9343(97)00150-2. [DOI] [PubMed] [Google Scholar]
- 8.Perrin T, Descombes E, Cook S. Contrast-induced nephropathy in invasive cardiology. Swiss Med Wkly. 2012;142:w13608. doi: 10.4414/smw.2012.13608. [DOI] [PubMed] [Google Scholar]
- 9.Coresh J, Byrd-Holt D, Astor BC, Briggs JP, Eggers PW, Lacher DA, et al. Chronic kidney disease awareness, prevalence, and trends among US adults, 1999-2000. J Am Soc Nephrol. 2005;16:180–188. doi: 10.1681/ASN.2004070539. [DOI] [PubMed] [Google Scholar]
- 10.Chertow GM, Normand SL, McNeil BJ. ‘Renalism’: inappropriately low rates of coronary angiography in elderly individuals with renal insufficiency. J Am Soc Nephrol. 2004;15:2462–2468. doi: 10.1097/01.ASN.0000135969.33773.0B. [DOI] [PubMed] [Google Scholar]
- 11.Han JH, Chandra A, Mulgund J, Roe MT, Peterson ED, Szczech LA, et al. Chronic kidney disease in patients with non-ST-segment elevation acute coronary syndromes. Am J Med. 2006;119:248–254. doi: 10.1016/j.amjmed.2005.08.057. [DOI] [PubMed] [Google Scholar]
- 12.Goldenberg I, Subirana I, Boyko V, Vila J, Elosua R, Permanyer-Miralda G, et al. Relation between renal function and outcomes in patients with non-ST-segment elevation acute coronary syndrome: real-world data from the European Public Health Outcome Research and Indicators Collection Project. Arch Intern Med. 2010;170:888–895. doi: 10.1001/archinternmed.2010.95. [DOI] [PubMed] [Google Scholar]
- 13.Best PJM, Lennon R, Ting HH, Bell MR, Rihal CS, Holmes DR, Jr, et al. The impact of renal insufficiency on clinical outcomes in patients undergoing percutaneous coronary interventions. J Am Coll Cardiol. 2002;39:1113–1119. doi: 10.1016/s0735-1097(02)01745-x. [DOI] [PubMed] [Google Scholar]
- 14.Sadeghi HM, Stone GW, Grines CL, Mehran R, Dixon SR, Lansky AJ, et al. Impact of renal insufficiency in patients undergoing primary angioplasty for acute myocardial infarction. Circulation. 2003;108:2769–2775. doi: 10.1161/01.CIR.0000103623.63687.21. [DOI] [PubMed] [Google Scholar]
- 15.Rihal CS, Textor SC, Grill DE, Berger PB, Ting HH, Best PJ, et al. Incidence and prognostic importance of acute renal failure after percutaneous coronary intervention. Circulation. 2002;105:2259–2264. doi: 10.1161/01.cir.0000016043.87291.33. [DOI] [PubMed] [Google Scholar]
- 16.Solomon RJ, Mehran R, Natarajan MK, Doucet S, Katholi RE, Staniloae CS, et al. Contrast-induced nephropathy and long-term events: cause and effect? Clin J Am Soc Nephrol. 2009;4:1162–1169. doi: 10.2215/CJN.00550109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dangas G, Iakovou I, Nikolsky E, Aymong ED, Mintz GS, Kipshidze NN, et al. Contrast-induced nephropathy after percutaneous coronary interventions in relation to chronic kidney disease and hemodynamic variables. Am J Cardiol. 2005;95:13–19. doi: 10.1016/j.amjcard.2004.08.056. [DOI] [PubMed] [Google Scholar]
- 18.Maioli M, Toso A, Leoncini M, Gallopin M, Musilli N, Bellandi F. Persistant renal damage after contrast-induced kidney injury. Circulation. 2012;125:3099–3107. doi: 10.1161/CIRCULATIONAHA.111.085290. [DOI] [PubMed] [Google Scholar]
- 19.Nemoto N, Iwasaki M, Nakanishi M, Araki T, Utsunomiya M, Hori M, et al. Impact of continuous deterioration of kidney function 6-8 months after percutaneous coronary intervention for acute coronary syndrome. Am J Cardiol. 2014;113:1647–1651. doi: 10.1016/j.amjcard.2014.02.019. [DOI] [PubMed] [Google Scholar]
- 20.Hölscher B, Heitmeyer C, Fobker M, Breithardt G, Schaefer RM, Reinecke H. Predictors for contrast media-induced nephropathy and long-term survival: prospectively assessed data from the randomized controlled Dialysis-Versus-Diuresis (DVD) Trial. Can J Cardiol. 2008;24:845–850. doi: 10.1016/s0828-282x(08)70193-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.James MT, Samuel SM, Manning MA, Tonelli M, Ghali WA, Faris P, et al. Contrast-induced acute kidney injury and risk of adverse clinical outcomes after coronary angiography: a systematic review and meta-analysis. Circ Cardiovasc Interv. 2013;6:37–43. doi: 10.1161/CIRCINTERVENTIONS.112.974493. [DOI] [PubMed] [Google Scholar]