Abstract
Because of its strong association (r 0·85) with percentage of body fat determined by dual-energy X-ray absorptiometry, hip circumference divided by height1·5 (the body adiposity index) has recently been proposed as an index of body fatness among adults. We examined whether this proposed index was more strongly associated with skinfold thicknesses and levels of CVD risk factors (lipids, fasting insulin and glucose, and blood pressure) than was BMI among 2369 18- to 49-year-olds in the Bogalusa Heart Study. All analyses indicated that the body adiposity index was less strongly associated with skinfold thicknesses and CVD risk factors than was either waist circumference or BMI. Correlations with the skinfold sum, for example, were r 0·81 (BMI) v. r 0·75 (body adiposity index) among men, and r 0·87 (BMI) v. r 0·80 among women; P<0·001 for both differences. An overall index of seven CVD risk factors was also more strongly associated with BMI (r 0·58) and waist circumference (r 0·61) than with the body adiposity index (r 0·49). The weaker associations with the body adiposity index were observed in analyses stratified by sex, race, age and year of examination. Multivariable analyses indicated that if either BMI or waist circumference were known, the body adiposity index provided no additional information on skinfold thicknesses or risk factor levels. These findings indicate that the body adiposity index is likely to be an inferior index of adiposity than is either BMI or waist circumference.
Keywords: Obesity, BMI, Children, Lipids, Skinfolds, Hip circumference, Waist circumference
Although the limitations of BMI are well known(1), this index remains widely used as a simple indicator of adiposity, and adults with a BMI ≥ 30 kg/m2 are considered to be obese. An alternative index, termed the ‘body adiposity index’, has recently been proposed(2):
This ratio was based on the correlations of percentage of body fat (calculated from dual-energy X-ray absorptiometry) with hip circumference and height among 1733 Mexican-American adults. The power of 1·5 was chosen to maximise the correlation with percentage of body fat (r 0·79) and 18 was the estimated intercept of a regression model that predicted percentage of body fat from hip circumference/height1·5. It was concluded that this index provides a ‘direct estimate of percentage of body fat’ among both men and women without the need for further adjustment(2).
The use of hip circumference in the numerator of an adiposity index, however, is somewhat surprising. Persons with larger hip circumferences, relative to BMI, are at lower risk for CHD and total mortality(3). The use of hip circumference in the waist:hip ratio(4,5), a simple index of abdominal obesity, also suggests that at similar levels of waist circumference, persons with a larger hip circumference are at lower risk for type 2 diabetes(6 – 9) and CHD(5,10). It remains uncertain, however, whether the assessment of abdominal obesity provides information on disease risk that is independent of BMI(7,10 – 12).
The purpose of the present study is to compare the usefulness of the body adiposity index, BMI and waist circumference as indicators of adiposity. In the present cross-sectional study, we examined associations among these measures, skinfold thicknesses and levels of CVD risk factors (lipids, fasting glucose and insulin, and blood pressure) among 2369 18- to 49-year-olds who participated in the Bogalusa Heart Study. If body adiposity index were a better index of adiposity than BMI, it was expected that it would show stronger associations with the skinfold sum (triceps plus subscapular) and with levels of CVD risk factors.
Methods
Study population
The Bogalusa Heart Study is a community-based (Ward 4 of Washington Parish, Louisiana) study of CVD risk factors in early life(13). The present study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures were approved by the Tulane University Human Subjects Review Committee. Written informed consent was obtained from all subjects.
Since 1973, several cross-sectional studies of schoolchildren and adults have been conducted. The present analyses are based on adults who participated in three cross-sectional studies (1995–6, 1998–2001 and 2001–2) in which hip circumference was measured. A total of 3639 examinations were conducted, with data obtained from 2703 different persons.
We excluded 124 examinations because the subject reported having diabetes mellitus or being pregnant, and another 218 because the participant reported taking medications for high blood pressure or cholesterol. We also excluded subjects who were <18 years (n 114) or ≥ 50 years (n 5) of age, or if data were missing for circumferences, skinfolds (subscapular and triceps) or BMI (n 13). We excluded nine observations because of implausible body size values, such as a hip circumference below 25 cm or a BMI value of 23 kg/m2 together with a waist circumference of 177 cm.
These exclusions resulted in a total of 3156 examinations from 2380 different adults; 762 adults participated in two or more of the three studies. Because levels are correlated over time within an individual, we selected only one examination for each individual. We chose the examination with the largest number of valid risk factor measurements for TAG, LDL-cholesterol (LDL-C), HDL-cholesterol (HDL-C), fasting insulin, fasting glucose and blood pressure. We also required that that each subject had valid data for at least four of these seven risk factors.
The final sample size was 2369. Of these subjects, 142 were missing data for fasting levels of glucose, insulin or TAG, and were excluded from analyses of these variables as well as from analyses of the risk factor sum (see ‘Risk factors’).
General examinations
Height was measured to the nearest 0·1 cm with an Iowa Height Board, and weight to the nearest 0·1 kg using a balance beam metric scale; BMI (kg/m2) was calculated as a measure of relative weight. No adjustments were made for the weight of the gown, underwear or socks that were worn during the examination.
Each skinfold thickness and circumference was measured three times, and the mean value was used in the analyses. The thicknesses of the triceps and subscapular skinfolds were measured to the nearest millimetre with Lange Skinfold Calipers (Cambridge Scientific Industries, Inc.), and the sum of these two skinfolds was used in the analyses as an indicator of overall body fatness. Circumferences were measured using a non-stretchable tape. Waist circumference was measured midway between the rib cage and the superior border of the iliac crest, and hip circumference was measured at the greater trochanters(14,15).
The body adiposity index was calculated as (hip circumference/height1·5) − 18, with hip circumference expressed in cm and height in m(2).
Risk factors
We focused on seven risk factors in the present analyses: TAG, LDL-C, HDL-C, glucose, fasting insulin, systolic blood pressure (SBP) and diastolic blood pressure (DBP). Non-fasting values of glucose, insulin and TAG were excluded from the analyses.
Serum concentrations of total cholesterol and TAG were determined, with enzymatic procedures, in a centralised laboratory that met the requirements of the CDC Lipid Standardization Program. LDL-C and HDL-C determinations were based on a combination of heparin–calcium precipitation and agar–agarose gel electrophoresis(16). Glucose was measured enzymatically as part of a multi-chemistry (SMA20) profile. Plasma insulin determinations were performed by a RIA procedure (Phadebas Insulin Kit; Pharmacia Diagnostic AB). Right arm, sitting SBP and DBP (5th Korotkoff sound) levels were measured six times by trained observers with a mercury sphygmomanometer (Baumanometer)(17).
An overall measure of risk was obtained by summing each subject’s standardised residual across six regression models that predicted levels of LDL-C, TAG, insulin, glucose, SBP and DBP from race, sex, age and study period. The standardised residuals from a model predicting HDL-C levels were then subtracted from this variable, resulting in the risk factor sum having a mean of 0 and a standard deviation of 5·0. (The 10th and 90th percentiles were −4·6 and 5·2.) Correlation coefficients between the risk factor sum and the various risk factors ranged in magnitude from r 0·46 (LDL-C) to r 0·69 (insulin). The risk factor sum was also highly correlated (r 0·97) with the first principal component(18) of the seven risk factors.
Some analyses also examined the number of adverse risk factors. The cut-off points for this analysis were: LDL-C (≥3·36 mmol/l), TAG (≥1·68 mmol/l), HDL-C (<1·29 mmol/l among women, <1·03 mmol/l among men), fasting glucose (≥ 5·55 mmol/l), SBP (130 mmHg), DBP (85 mmHg) and a fasting insulin ≥90th percentile for a subject’s sex, race and age.
Statistical analyses
Analyses were performed using R (www.R-project.org)(19), and first examined mean (or median) levels of the body size measures (BMI, body adiposity index, waist circumference and hip circumference) and the risk factor variables (lipids, glucose, insulin and blood pressure). We then examined the intercorrelations among the body size measures.
The statistical significance of differences in the relationship of the skinfold sum to the body adiposity index, BMI, waist circumference and hip circumference was examined using a test for correlated correlations developed by Meng et al.(20) that incorporates Fisher’s Z-transformation. (This test would assess, for example, whether the magnitude of the Z-transformed correlation between the skinfold sum and the body adiposity index (r1) is equal to that between the skinfold sum and BMI (r2); H0: r1 =r2.) To adjust for race, sex, age and study differences, analyses were based on the residuals of regression models in which each body size measure was predicted by these characteristics; age was modelled using cubic splines with five knots(21).
Correlation coefficients were also used to examine the relationship of the body size measures to the risk factor sum and to levels of the individual risk factors (Table 3). To determine whether the body adiposity index provided additional information on risk factor levels, we examined the proportion of men and women who had adverse levels of at least three risk factors following the cross-classification of BMI and body adiposity index categories (Table 4). Because the strong association between these two characteristics (r approximately 0·8) resulted in few subjects with some combinations of these variables (e.g. BMI ≥ 35 kg/m2 and a low body adiposity index), quartiles of the body adiposity index were constructed within each sex and BMI category. The multiple R2 and likelihood values of various regression models were also compared to determine whether any two-variable combinations of body size measures could improve the prediction of risk factor levels beyond that achieved by a single measure (Table 5).
Table 3.
Associations (correlation coefficients) between the various measures of body size and risk factor levels
| Strata (n) | Characteristics | Risk factor sum | LDL-C | HDL-C | TAG | Insulin | Glucose | SBP | DBP |
|---|---|---|---|---|---|---|---|---|---|
| Overall (n 2367) | Body adiposity index | 0·49 | 0·23 | −0·25 | 0·21 | 0·50 | 0·26 | 0·29 | 0·27 |
| BMI | 0·58* | 0·23 | −0·30* | 0·25* | 0·61* | 0·33* | 0·35* | 0·33* | |
| Waist | 0·61* | 0·23 | −0·33* | 0·30* | 0·63* | 0·34* | 0·36* | 0·31* | |
| Sex | |||||||||
| Men (n 1043) | Body adiposity index | 0·52 | 0·28 | −0·25 | 0·25 | 0·52 | 0·26 | 0·33 | 0·30 |
| BMI | 0·59* | 0·26 | −0·31* | 0·30* | 0·60* | 0·34* | 0·38* | 0·34 | |
| Waist | 0·61* | 0·26 | −0·31* | 0·33* | 0·61* | 0·35* | 0·39* | 0·34 | |
| Women (n 1324) | Body adiposity index | 0·50 | 0·21 | −0·24 | 0·20 | 0·51 | 0·28 | 0·28 | 0·27 |
| BMI | 0·59* | 0·21 | −0·30* | 0·23 | 0·61* | 0·34* | 0·33* | 0·32* | |
| Waist | 0·62* | 0·21 | −0·34* | 0·28* | 0·64* | 0·33* | 0·34* | 0·32* | |
| Age (years) | |||||||||
| ≤ 25 (n 420) | Body adiposity index | 0·55 | 0·21 | −0·20 | 0·24 | 0·56 | 0·29 | 0·32 | 0·32 |
| BMI | 0·63* | 0·19 | −0·26* | 0·28 | 0·65* | 0·32 | 0·38* | 0·36 | |
| Waist | 0·66* | 0·20 | −0·30* | 0·31 | 0·69* | 0·33 | 0·39 | 0·34 | |
| 25–34 (n 991) | Body adiposity index | 0·49 | 0·22 | −0·25 | 0·21 | 0·50 | 0·27 | 0·30 | 0·28 |
| BMI | 0·59* | 0·22 | −0·30* | 0·25* | 0·61* | 0·34* | 0·37* | 0·34* | |
| Waist | 0·61* | 0·22 | −0·33* | 0·31* | 0·63* | 0·34* | 0·39* | 0·36* | |
| ≥ 35 (n 956) | Body adiposity index | 0·47 | 0·25 | −0·26 | 0·20 | 0·48 | 0·25 | 0·27 | 0·24 |
| BMI | 0·57* | 0·26 | −0·32* | 0·26* | 0·58* | 0·33* | 0·32* | 0·29* | |
| Waist | 0·59* | 0·26 | −0·34* | 0·30* | 0·58* | 0·35* | 0·32 | 0·29 | |
LDL-C, LDL-cholesterol; HDL-C, HDL-cholesterol; SBP, systolic blood pressure; DBP, diastolic blood pressure.
BMI or waist circumference is more strongly associated (P<0·001) with the specified risk factor variable than is the body adiposity index.
Table 4.
Prevalence of three or more risk factors according to categories of BMI and the body adiposity index (Number of subjects and percentages)
| BMI (kg/m2) | Body adiposity index quartiles*
|
||||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 (low)
|
2
|
3
|
4 (high)
|
||||||
| % | n | % | n | % | n | % | n | ||
| Men | <22·5 | 0 | 42 | 0 | 42 | 2 | 42 | 7 | 42 |
| 22·5–24·9 | 11 | 37 | 11 | 36 | 14 | 36 | 14 | 36 | |
| 25·0–29·9 | 17 | 90 | 21 | 89 | 22 | 90 | 18 | 89 | |
| 30·0–34·9 | 40 | 48 | 34 | 47 | 21 | 47 | 40 | 47 | |
| ≥35 | 48 | 29 | 50 | 28 | 61 | 28 | 57 | 28 | |
| Women | <22·5 | 0 | 82 | 5 | 81 | 4 | 82 | 5 | 82 |
| 22·5–24·9 | 15 | 55 | 4 | 56 | 0 | 56 | 4 | 56 | |
| 25·0–29·9 | 4 | 72 | 15 | 72 | 7 | 72 | 8 | 71 | |
| 30·0–34·9 | 21 | 48 | 17 | 47 | 21 | 47 | 15 | 47 | |
| ≥35 | 33 | 58 | 31 | 58 | 28 | 58 | 45 | 58 | |
Quartiles of the body adiposity index were defined within each sex and BMI category. For example, the lowest quartile of the body adiposity index among men with a BMI < 22·5 kg/m2 ranged from 13·8 to 20·5, while the lowest quartile of the body adiposity index among men with a BMI ≥ 35 kg/m2 ranged from 27·3 to 32·4. Because cut-off points for the categories of the body adiposity index vary by sex and BMI, comparisons should not be made across BMI categories.
Table 5.
Multiple R2 values for combinations of the anthropometric variables in predicting the skinfold sum and risk factor levels
| Skinfold sum | Risk factors
|
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Risk factor sum | LDL-C | HDL-C | TAG | Insulin | Glucose | SBP | DBP | ||
| n | 2369 | 2261 | 2367 | 2367 | 2293 | 2260 | 2254 | 2369 | 2369 |
| Race, sex, age, study period | 0·16* | 0 | 0·06 | 0·13 | 0·11 | 0·03 | 0·06 | 0·19 | 0·19 |
| One-variable models† | |||||||||
| BMI | 0·78 | 0·36 | 0·13 | 0·23 | 0·20 | 0·40 | 0·17 | 0·31 | 0·29 |
| Body adiposity index | 0·69 | 0·27 | 0·13 | 0·20 | 0·18 | 0·30 | 0·14 | 0·28 | 0·27 |
| Waist | 0·76 | 0·39 | 0·13 | 0·24 | 0·22 | 0·42 | 0·18 | 0·30 | 0·29 |
| Hip | 0·74 | 0·29 | 0·12 | 0·21 | 0·18 | 0·34 | 0·16 | 0·30 | 0·28 |
| Two-variable models† | |||||||||
| Waist, BMI | 0·79 | 0·40 | 0·14 | 0·24 | 0·23 | 0·43 | 0·19 | 0·32 | 0·31 |
| Waist, body adiposity index | 0·79 | 0·40 | 0·14 | 0·25 | 0·23 | 0·43 | 0·19 | 0·32 | 0·30 |
| Waist, hip | 0·78 | 0·41 | 0·14 | 0·25 | 0·25 | 0·43 | 0·19 | 0·32 | 0·30 |
| BMI, body adiposity index | 0·78 | 0·38 | 0·14 | 0·24 | 0·21 | 0·43 | 0·19 | 0·32 | 0·30 |
| BMI, hip | 0·79 | 0·38 | 0·14 | 0·24 | 0·23 | 0·42 | 0·19 | 0·31 | 0·30 |
LDL-C, LDL-cholesterol; HDL-C, HDL-cholesterol; SBP, systolic blood pressure; DBP, diastolic blood pressure.
Values are multiple R2 for a model predicting the skinfold sum or risk factor variables from race, sex, age, study period and the specified body size measure.
All one- and two-variable models also include race, sex, age and study period.
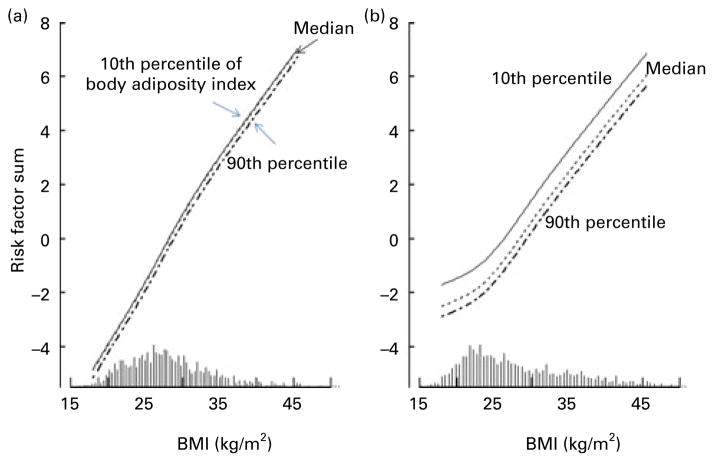
We also illustrate the joint relationship, based on regression models, of levels of BMI and the body adiposity index to the risk factor sum (Fig. 1). For this analysis, the regression of the body adiposity index v. levels of BMI, age, sex, race and study period was performed, and the resulting residuals were used to represent levels of the body adiposity index relative to BMI. Predicted levels of the risk factor sum were then plotted against levels of BMI and the (relative) body adiposity index for men and women. If the body adiposity index were a better indicator of adiposity than BMI, one would expect that at comparable BMI, persons with a higher body adiposity index would have a more adverse risk factor profile.
Fig. 1.
Predicted levels of the risk factor sum among (a) white men and (b) white women at an age of 32 years (overall mean) by levels of BMI (x-axis) and body adiposity index. Sex-specific regression models included race, age, BMI and the body adiposity index; predicted levels of the risk factor sum are shown for subjects who are at the 10th, 50th and 90th percentiles of body adiposity index. The distribution of BMI levels is shown by the histogram along the x-axis.
Results
The mean levels of various characteristics are shown in Table 1. The mean ages varied from 31 to 33 years across the race–sex groups, and 34 % of the subjects were obese (BMI ≥ 30 kg/m2). There were substantial differences in body size measures, with women having higher levels of the skinfold sum and the body adiposity index than men, and black women having higher levels than white women. (As assessed in regression models, most of the main effects and sex × race interactions for the variables in Table 1 were statistically significant.) There were also differences in risk factor levels across the race–sex groups, but these did not necessarily parallel differences in body size. Black women, for example, had the highest levels of BMI, skinfold sum and the body adiposity index, but they had the lowest levels of LDL-C and TAG, along with the highest HDL-C levels.
Table 1.
Levels of various characteristics, by race and sex (Mean values and standard deviations; medians and percentages)
| Men
|
Women
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Whites
|
Blacks
|
Whites
|
Blacks
|
|||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| n | 733 | 311 | 911 | 414 | ||||
| Age (years) | 33* | 6 | 32 | 7 | 32 | 7 | 31 | 7 |
| BMI (kg/m2) | 28 | 6 | 28 | 6 | 27 | 7 | 30 | 8 |
| Obese (%) | 31 | 29 | 29 | 45 | ||||
| Circumferences (cm) | ||||||||
| Waist | 96 | 15 | 90 | 16 | 83 | 16 | 90 | 18 |
| Hip | 106 | 10 | 105 | 12 | 106 | 14 | 111 | 16 |
| Height (cm) | 177 | 6 | 176 | 7 | 163 | 6 | 163 | 7 |
| Body adiposity index*† | 27 | 4 | 27 | 5 | 33 | 7 | 35 | 8 |
| Median | 27 | 26 | 32 | 34 | ||||
| Skinfold sum (mm) | 43 | 20 | 38 | 24 | 55 | 22 | 60 | 25 |
| LDL-C (mmol/l) | 3·27 | 0·9 | 3·02 | 1·0 | 3·09 | 0·8 | 2·93 | 0·8 |
| HDL-C (mmol/l) | 1·09 | 0·3 | 1·33 | 0·4 | 1·31 | 0·3 | 1·39 | 0·4 |
| TAG (mmol/l)† | 1·64 | 1·2 | 1·21 | 0·9 | 1·26 | 0·8 | 0·88 | 0·4 |
| Median | 1·28 | 0·96 | 1·05 | 0·80 | ||||
| Fasting insulin (ρmol/l)† | 84·9 | 61 | 77·7 | 55 | 78·2 | 57 | 100 | 74 |
| Median | 70 | 56 | 62 | 83 | ||||
| Fasting glucose (mmol/l) | 4·66 | 0·6 | 4·67 | 0·7 | 4·45 | 0·5 | 4·54 | 0·6 |
| SBP (mmHg) | 116 | 10 | 120 | 13 | 109 | 10 | 114 | 14 |
| DBP (mmHg) | 72 | 9 | 73 | 11 | 67 | 8 | 70 | 10 |
| Risk factor sum‡ | 0 | 4 | 0 | 5 | 0 | 4 | 0 | 4 |
| ≥ 3 risk factors (%)§ | 24 | 18 | 15 | 8 | ||||
LDL-C, LDL-cholesterol; HDL-C, HDL-cholesterol; SBP, systolic blood pressure; DBP, diastolic blood pressure.
Calculated as (hip circumference (cm)/height (m)1·5) − 18.
Levels of TAG, fasting insulin and the body adiposity index were the most skewed.
Because the risk factor sum is based on the residuals from regression models, the mean value is 0.
The risk factor number was the sum of adverse levels of seven risk factors: LDL-C (≥3·36 mmol/l); TAG (≥1·68 mmol/l); HDL-C (<1·29 mmol/l for women; <1·03 mmol/l for men); fasting glucose (≥5·55 mmol/l); SBP (≥130 mmHg); DBP (≥85 mmHg); insulin ≥90th percentile.
Correlations among the levels of the body size characteristics are shown in Table 2, with correlations among men in the, upper right triangle and those among women in the lower left. The skinfold sum was highly correlated with all measures except height, with BMI (men r 0·82; women r 0·87, women), waist circumference (r 0·81–0·85) and hip circumference (r 0·79–0·84) showing the strongest associations. The skinfold sum was less strongly associated with the body adiposity index (men r 0·75; women r 0·80) and showed almost no association with height (r < 0·10). As assessed by a test for the equality of correlations (H0, r1 = r2), the skinfold sum was more strongly (P<0·0001) related to BMI than to the body adiposity index. (Similar results were obtained using Spearman’s correlations and log-transformed skinfolds.) It should also be noted that whereas there was little association between the skinfold sum and height in either sex, analyses of men and women together indicated that height and the skinfold sum were inversely correlated (r – 0·19).
Table 2.
Intercorrelations among the anthropometric characteristics by sex†
| Skinfold sum‡ | Body adiposity index | BMI | Waist circumference | Hip circumference | Height | Weight | |
|---|---|---|---|---|---|---|---|
| Skinfold sum‡ | 0·75 | 0·82* | 0·81* | 0·79* | 0·04* | 0·78 | |
| Body adiposity index | 0·80 | 0·90 | 0·81 | 0·86 | −0·30 | 0·75 | |
| BMI | 0·87* | 0·93 | 0·94 | 0·92 | 0·02 | 0·94 | |
| Waist circumference | 0·85* | 0·82 | 0·93 | 0·92 | 0·17 | 0·94 | |
| Hip circumference | 0·84* | 0·90 | 0·94 | 0·90 | 0·24 | 0·94 | |
| Height | 0·06* | −0·24 | 0·02 | 0·15 | 0·20 | 0·34 | |
| Weight | 0·84* | 0·81 | 0·95 | 0·93 | 0·96 | 0·31 |
P<0·001 for H0: the correlation between specified characteristic and skinfold sum equals the correlation between the body adiposity index and the skinfold sum. Among men, for example, the skinfold sum was more strongly correlated with BMI (r 0·82) than with the body adiposity index (r 0·75), P<0·001.
Correlations among men are in the upper, right triangle; those among women are in the lower, left triangle. Correlations have been adjusted for the influence of race, age and study. With a sample size of n 1200, a correlation of r 0·095 would be statistically significant at the 0·001 level.
P values assess whether the correlation between the skinfold sum and the body adiposity index is equal to the correlation between the skinfold sum and the other characteristics.
We then examined the associations between the anthropometric characteristics and levels of the CVD risk factors (Table 3). In the entire sample, both BMI (r 0·58) and waist circumference (r 0·61) were more strongly correlated with the risk factor sum than was the body adiposity index (r 0·49); P<0·001 for both comparisons. With the exception of LDL-C levels, the body adiposity index also showed significantly weaker associations with most of the individual risk factors than did BMI or waist circumference; similar patterns were also seen within sex and age categories. No comparison indicated that the body adiposity index was more strongly associated with risk factor levels than was BMI or waist circumference. For example, among persons younger than 25 years of age, levels of LDL-C showed correlations of r 0·21 (body adiposity index), r 0·19 (BMI) and r 0·20 (waist circumference) with the measures of body size, but the P values associated with these differences were >0·80. Additional analyses indicated that within each of the three cross-sectional studies included in the present analysis, the body adiposity index was less strongly associated with risk factor levels than was either BMI or waist circumference (data not shown).
To assess whether the body adiposity index could provide additional information on risk factor levels, beyond that conveyed by BMI, we first examined the proportion of men and women who had three or more risk factors according to categories of BMI and the body adiposity index (Table 4). Because the strong correlation between BMI and the body adiposity index resulted in small numbers of persons in the low/high and high/low categories, quartiles of the body adiposity index were constructed within each BMI category. After this adjustment for BMI, there appeared to be little association between the body adiposity index and the prevalence of three or more risk factors. Among subjects who had a BMI between 30·0 and 34·9 kg/m2, for example, the prevalence of three or more risk factors was almost identical (40 %) among men who were in the lowest and highest categories of the body adiposity index quartile, while among women, the prevalence was slightly higher among those in the lowest body adiposity index quartile than among those in the highest quartile (21 v. 15 %). There was also little difference in the prevalence of multiple risk factors across quartiles of the body adiposity index among subjects who had a BMI ≥ 35 kg/m2.
The independent effects of BMI and the body adiposity index in the prediction of the risk factor sum, as estimated in regression models that included both characteristics, are shown for men (Fig. 1(a)) and women (Fig. 1(b)). The three lines in each panel indicate the predicted risk factor sum for a person who had a specified BMI (x-axis) along with a body adiposity index at either the 10th, 50th or 90th percentile (three parallel lines). For example, among men who had a body adiposity index at the 50th percentile, the predicted risk factor sum increased by about 7 units (−4 to +3) as BMI increased from 20 to 35 kg/m2. As indicated by the three curves in each panel, however, the effects of the body adiposity index were substantially weaker, and when considered together with BMI, there was almost no difference in predicted levels of the risk factor sum between men who were at the 10th or 50th percentile of body adiposity index. Among women, the predicted risk factor sum increased by about 6 units as BMI increased from 20 to 40 kg/m2, but decreased by about 1 unit (P<0·001) as the body adiposity index increased from the 10th to the 90th percentile.
The information provided by the body size measures in the prediction of levels of the skinfold sum and risk factor levels is shown in Table 5. The combination of race, sex, age, study period and BMI accounted for 78 % of the variability in the skinfold sum, for example, whereas the R2 value of a model with the body adiposity index (rather than BMI) was 0·69. Interestingly, the multiple R2 value for a model with hip circumference was also higher than that for the body adiposity index (0·74 v. 0·69). There were only very small differences (R2 0·78–0·79) in the multiple R2 values of the five models that included various combinations of the body size measures, and none was substantially higher than the R2 value of a model containing BMI alone.
For levels of the risk factors, the highest R2 values were generally obtained by models that contained waist circumference, but differences between models that contained either BMI or waist circumference were generally small. For example, the multiple R2 values for models predicting the risk factor sum were 0·39 (waist circumference), 0·36 (BMI) and 0·27 (body adiposity index). Models containing the body adiposity index had the lowest R2 values for almost all risk factors. Differences between the two-variable models were generally small, with the highest R2 values typically seen for models that combined waist circumference with either BMI or hip circumference.
Discussion
The present results indicate that among 18- to 49-year-olds, both BMI and waist circumference are more strongly associated (P<0·001) with the sum of the triceps and subscapular skinfold thicknesses and with CVD risk factors than is the recently proposed(2) body adiposity index. Of the various measures, BMI was the strongest correlate of the skinfold sum, but waist circumference showed slightly stronger associations with levels of most risk factors than did BMI. The weakest associations were consistently seen with the body adiposity index. Furthermore, in contrast to what would be expected if the body adiposity index were a better indicator of adiposity, we found that this newly proposed index provided very little (if any) information on the skinfold sum or levels of risk factors beyond that conveyed by BMI. The apparent association between the body adiposity index and the risk factor sum appears to be largely due to the association between BMI and the levels of CVD risk factors.
We also found that hip circumference (alone) showed slightly stronger associations with the skinfold sum and risk factor levels than did the body adiposity index. Among men, correlations with the skinfold sum were r 0·79 (hip circumference) and r 0·75 (body adiposity index), and among women, correlations were r 0·84 and 0·80, respectively. These associations probably reflect the very weak relationship, that we and others(22 – 24) have observed, of height to body fatness among adults. Most, but not all(25), investigators have assumed that an optimal weight–height index of obesity among adults would show little correlation with height(26).
In contrast to this weak association between body fatness and height, Bergman et al.(2) reported that dual-energy X-ray absorptiometry-estimated body fatness was more strongly associated with height (r – 0·52) than with weight (r 0·23). This inverse association formed the basis for dividing hip circumference by height(2), but much of the inverse association between height and body fatness may have been due to confounding by sex. Women are generally shorter than men and have more body fatness, so a crude (non-stratified) analysis would probably find that body fatness is inversely associated with height. For example, among 12 957 adults in the National Health and Nutrition Examination Survey (NHANES) 1999–2004, dual-energy X-ray absorptiometry-calculated percentage of body fat is inversely correlated (r – 0·50) with height; sex-specific correlations, however, between height and body fatness are r – 0·02 (men) and r – 0·10 (women) (D. S. Freedman, unpublished results). Furthermore, the difficulties in interpreting a ratio constructed on the basis of a positive association with the numerator (hip) and an inverse association with the denominator (height) are well known(27). Various regression models in the present study also indicated that the use of hip circumference and sex as separate variables resulted in higher R2 values in the prediction of skinfold sum (0·70) and the risk factor sum (0·26) than did the body adiposity index (R2 0·63 and 0·18, respectively).
Some investigators have concluded that abdominal obesity, typically assessed by waist circumference (either alone or divided by height or hip circumference), is more strongly associated with CVD risk factor levels than is BMI(28,29). The present results provide some support for this possibility, and levels of most risk factors showed slightly stronger associations with waist circumference than with BMI. The high correlation (r approximately 0·95) between BMI and waist circumference, however, can make it difficult to disentangle the effects of each measure. Furthermore, waist circumference is strongly correlated with the skinfold sum, indicating that it is a measure of both overall and abdominal obesity(4,30). The results of longitudinal studies of abdominal obesity have been inconsistent, with some finding waist circumference to be more predictive of disease than BMI(8,9,31), but others showing little difference between these two measures(6,7,12). It is also difficult to reconcile the use of hip circumference in the numerator of an adiposity index, with studies that have found that, after controlling for BMI, larger hip circumferences are protective for CHD mortality(32) and are associated with beneficial lipid levels(3), possibly due to the protective role of gluteofemoral fat(33). If the assessment of obesity-related risk by a circumference is desired(34 – 36), the results from the present study indicate that waist rather than hip (buttocks) circumference should be used.
There are several potential limitations of the present study. The sample was not randomly selected and is from a single community in Louisiana, with white adults (but not black adults) in the present study having a higher prevalence of obesity than in NHANES 1999–2003(37). Mean BMI levels in the present study, however, are comparable to those (29·5–30·0 kg/m2) reported in the study of Bergman et al.(2). We also used the sum of two skinfold thicknesses as an index of body fatness, and skinfold thicknesses have many limitations as indicators of adiposity(38,39). The body adiposity index, however, showed the weakest associations not only with the skinfold thickness sum, but also with levels of the CVD risk factors. Another possible limitation is that hip circumference in the present study was measured at the greater trochanters(14) rather than at the maximum extension of the buttocks(2), but the importance of this difference is uncertain. Among obese subjects, measurements at both locations may include the anterior abdominal wall(15); one-third of the subjects in the present study had a BMI of 30 kg/m2 or more.
In summary, we found that among 2369 18- to 49-year-olds, the body adiposity index was less strongly associated with skinfold thicknesses and with levels of CVD risk factors than was either BMI or waist circumference. These results were consistent across categories of sex, race, age and time period, and were also observed in multivariable analyses. Although these associations need to be confirmed in studies that have more accurate estimates of body fatness, the present findings suggest that the division of hip circumference by height1·5 is unlikely to be a useful index of body fatness. If the accurate measurement of weight is difficult or not possible, the measurement of waist circumference should be considered.
Acknowledgments
This study was supported by the National Institutes of Aging Grant AG-16592. The findings and conclusions in this study are those of the authors and not necessarily those of the Centers for Disease Control (CDC). D. S. F. was responsible for the data analyses, interpretation of the results, and writing of the manuscript. H. M. B. was involved in the interpretation of the results. W. H. D. was involved in the formulation of the study objectives, and in the drafting of the manuscript. P. D., S. R. S. and G. S. B. were involved in data collection, and G. S. B. was the principal investigator. All authors participated in the revision of the paper.
Abbreviations
- DBP
diastolic blood pressure
- HDL-C
HDL-cholesterol
- LDL-C
LDL-cholesterol
- SBP
systolic blood pressure
Footnotes
None of the authors has a personal or financial conflict of interest.
References
- 1.Prentice AM, Jebb SA. Beyond body mass index. Obes Rev. 2001;2:141–147. doi: 10.1046/j.1467-789x.2001.00031.x. [DOI] [PubMed] [Google Scholar]
- 2.Bergman RN, Stefanovski D, Buchanan TA, et al. A better index of body adiposity. Obesity (Silver Spring) 2011;19:1083–1089. doi: 10.1038/oby.2011.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Heitmann BL, Lissner L. Hip Hip Hurrah! Hip size inversely related to heart disease and total mortality. Obes Rev. 2011;12:478–481. doi: 10.1111/j.1467-789X.2010.00794.x. [DOI] [PubMed] [Google Scholar]
- 4.Molarius A, Seidell JC. Selection of anthropometric indicators for classification of abdominal fatness – a critical review. Int J Obes Relat Metab Disord. 1998;22:719–727. doi: 10.1038/sj.ijo.0800660. [DOI] [PubMed] [Google Scholar]
- 5.Canoy D. Coronary heart disease and body fat distribution. Curr Atheroscler Rep. 2010;12:125–133. doi: 10.1007/s11883-010-0092-9. [DOI] [PubMed] [Google Scholar]
- 6.Stevens J, Couper D, Pankow J, et al. Sensitivity and specificity of anthropometrics for the prediction of diabetes in a biracial cohort. Obes Res. 2001;9:696–705. doi: 10.1038/oby.2001.94. [DOI] [PubMed] [Google Scholar]
- 7.Tulloch-Reid MK, Williams DE, Looker HC, et al. Do measures of body fat distribution provide information on the risk of type 2 diabetes in addition to measures of general obesity? Comparison of anthropometric predictors of type 2 diabetes in Pima Indians. Diabetes Care. 2003;26:2556–2561. doi: 10.2337/diacare.26.9.2556. [DOI] [PubMed] [Google Scholar]
- 8.Wang Y, Rimm EB, Stampfer MJ, et al. Comparison of abdominal adiposity and overall obesity in predicting risk of type 2 diabetes among men. Am J Clin Nutr. 2005;81:555–563. doi: 10.1093/ajcn/81.3.555. [DOI] [PubMed] [Google Scholar]
- 9.Schulze MB, Heidemann C, Schienkiewitz A, et al. Comparison of anthropometric characteristics in predicting the incidence of type 2 diabetes in the EPIC-Potsdam study. Diabetes Care. 2006;29:1921–1923. doi: 10.2337/dc06-0895. [DOI] [PubMed] [Google Scholar]
- 10.Taylor AE, Ebrahim S, Ben-Shlomo Y, et al. Comparison of the associations of body mass index and measures of central adiposity and fat mass with coronary heart disease, diabetes, and all-cause mortality: a study using data from 4 UK cohorts. Am J Clin Nutr. 2010;91:547–556. doi: 10.3945/ajcn.2009.28757. [DOI] [PubMed] [Google Scholar]
- 11.Feller S, Boeing H, Pischon T. Body mass index, waist circumference, and the risk of type 2 diabetes mellitus: implications for routine clinical practice. Dtsch Arztebl Int. 2010;107:470–476. doi: 10.3238/arztebl.2010.0470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wormser D, Kaptoge S, Di Angelantonio E, et al. Separate and combined associations of body-mass index and abdominal adiposity with cardiovascular disease: collaborative analysis of 58 prospective studies. Lancet. 2011;377:1085–1095. doi: 10.1016/S0140-6736(11)60105-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Berenson GS, McMahan CA, Voors AW, et al. Cardiovascular Risk Factors in Children: The Early Natural History of Atherosclerosis and Essential Hypertension. New York, NY: Oxford University Press; 1980. [Google Scholar]
- 14.Harsha D. Body composition and obesity in a population of children and their influence on cardiovascular risk. In: Berenson GS, editor. Causation of Cardiovascular Risk Factors in Children. Perspectives on Cardiovascular Risk in Early Life. New York, NY: Raven Press; 1986. pp. 190–222. [Google Scholar]
- 15.Lohman TG, Roche AF, Martorell R. Anthropometric Standardization Reference Manual. Champaign, IL: Human Kinetics Books; 1988. [Google Scholar]
- 16.Srinivasan SR, Frerichs RR, Webber LS, et al. Serum lipoprotein profile in children from a biracial community: the Bogalusa Heart Study. Circulation. 1976;54:309–318. doi: 10.1161/01.cir.54.2.309. [DOI] [PubMed] [Google Scholar]
- 17.Berenson GS, Cresanta JL, Webber LS. High blood pressure in the young. Annu Rev Med. 1984;35:535–560. doi: 10.1146/annurev.me.35.020184.002535. [DOI] [PubMed] [Google Scholar]
- 18.Everitt B. An R and S-PLUS Companion to Multivariate Analysis. London: Springer; 2005. [Google Scholar]
- 19.R Development Core Team. R: A Language and Environment for Statistical Computing (version 2.14.0) Vienna: R Foundation for Statistical Computing; 2011. [Google Scholar]
- 20.Meng XL, Rosenthal R, Rubin DB. Comparing correlated correlation coefficients. Psychol Bull. 1992;111:172–174. [Google Scholar]
- 21.Harrell FE. Regression Modeling Strategies: With Applications to Linear Models, Logistic Regression, and Survival Analysis. New York, NY: Springer; 2001. [Google Scholar]
- 22.Knapik JJ, Burse RL, Vogel JA. Height, weight, percent body fat, and indices of adiposity for young men and women entering the U.S. army. Aviat Space Environ Med. 1983;54:223–231. [PubMed] [Google Scholar]
- 23.Micozzi MS, Albanes D, Jones DY, et al. Correlations of body mass indices with weight, stature, and body composition in men and women in NHANES I and II. Am J Clin Nutr. 1986;44:725–731. doi: 10.1093/ajcn/44.6.725. [DOI] [PubMed] [Google Scholar]
- 24.Flegal KM. Ratio of actual to predicted weight as an alternative to a power-type weight-height index (Benn index) Am J Clin Nutr. 1990;51:540–547. doi: 10.1093/ajcn/51.4.540. [DOI] [PubMed] [Google Scholar]
- 25.Larsson I, Henning B, Lindroos AK, et al. Optimized predictions of absolute and relative amounts of body fat from weight, height, other anthropometric predictors, and age. Am J Clin Nutr. 2006;83:252–259. doi: 10.1093/ajcn/83.2.252. [DOI] [PubMed] [Google Scholar]
- 26.Benn RT. Some mathematical properties of weight-for-height indices used as measures of adiposity. Br J Prev Soc Med. 1971;25:42–50. doi: 10.1136/jech.25.1.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Allison DB, Paultre F, Goran MI, et al. Statistical considerations regarding the use of ratios to adjust data. Int J Obes Relat Metab Disord. 1995;19:644–652. [PubMed] [Google Scholar]
- 28.Hsieh SD, Muto T. The superiority of waist-to-height ratio as an anthropometric index to evaluate clustering of coronary risk factors among non-obese men and women. Prev Med. 2005;40:216–220. doi: 10.1016/j.ypmed.2004.05.025. [DOI] [PubMed] [Google Scholar]
- 29.Bosy-Westphal A, Geisler C, Onur S, et al. Value of body fat mass vs anthropometric obesity indices in the assessment of metabolic risk factors. Int J Obes. 2006;30:475–483. doi: 10.1038/sj.ijo.0803144. [DOI] [PubMed] [Google Scholar]
- 30.Lean ME, Han TS, Deurenberg P. Predicting body composition by densitometry from simple anthropometric measurements. Am J Clin Nutr. 1996;63:4–14. doi: 10.1093/ajcn/63.1.4. [DOI] [PubMed] [Google Scholar]
- 31.Yusuf S, Hawken S, Ounpuu S, et al. Obesity and the risk of myocardial infarction in 27,000 participants from 52 countries: a case–control study. Lancet. 2005;366:1640–1649. doi: 10.1016/S0140-6736(05)67663-5. [DOI] [PubMed] [Google Scholar]
- 32.Canoy D, Wareham N, Luben R, et al. Serum lipid concentration in relation to anthropometric indices of central and peripheral fat distribution in 20,021 British men and women: results from the EPIC-Norfolk population-based cohort study. Atherosclerosis. 2006;189:420–427. doi: 10.1016/j.atherosclerosis.2005.12.027. [DOI] [PubMed] [Google Scholar]
- 33.Manolopoulos KN, Karpe F, Frayn KN. Gluteofemoral body fat as a determinant of metabolic health. Int J Obes. 2010;34:949–959. doi: 10.1038/ijo.2009.286. [DOI] [PubMed] [Google Scholar]
- 34.Ashwell M, Hsieh SD. Six reasons why the waist-to-height ratio is a rapid and effective global indicator for health risks of obesity and how its use could simplify the international public health message on obesity. Int J Food Sci Nutr. 2005;56:303–307. doi: 10.1080/09637480500195066. [DOI] [PubMed] [Google Scholar]
- 35.Kahn HS, Imperatore G, Cheng YJ. A population-based comparison of BMI percentiles and waist-to-height ratio for identifying cardiovascular risk in youth. J Pediatr. 2005;146:482–488. doi: 10.1016/j.jpeds.2004.12.028. [DOI] [PubMed] [Google Scholar]
- 36.McCarthy HD, Ashwell M. A study of central fatness using waist-to-height ratios in UK children and adolescents over two decades supports the simple message – ‘keep your waist circumference to less than half your height’. Int J Obes. 2006;30:988–992. doi: 10.1038/sj.ijo.0803226. [DOI] [PubMed] [Google Scholar]
- 37.Flegal KM, Carroll MD, Ogden CL, et al. Prevalence and trends in obesity among US adults, 1999–2000. JAMA. 2002;288:1723–1727. doi: 10.1001/jama.288.14.1723. [DOI] [PubMed] [Google Scholar]
- 38.Ulijaszek SJ, Kerr DA. Anthropometric measurement error and the assessment of nutritional status. Br J Nutr. 1999;82:165–177. doi: 10.1017/s0007114599001348. [DOI] [PubMed] [Google Scholar]
- 39.Clarys JP, Provyn S, Marfell-Jones MJ. Cadaver studies and their impact on the understanding of human adiposity. Ergonomics. 2005;48:1445–1461. doi: 10.1080/00140130500101486. [DOI] [PubMed] [Google Scholar]