Abstract
Introduction
Temporary skeletal anchorage devices now offer the possibility of closing anterior open bites and decreasing anterior face height by intruding maxillary posterior teeth, but data for treatment outcomes are lacking. This article presents outcomes and posttreatment changes for consecutive patients treated with a standardized technique.
Methods
The sample included 33 consecutive patients who had intrusion of maxillary posterior teeth with a maxillary occlusal splint and nickel-titanium coil springs to temporary anchorage devices in the zygomatic buttress area, buccal and apical to the maxillary molars. Of this group, 30 had adequate cephalograms available for the period of treatment, 27 had cephalograms including 1-year posttreatment, and 25 had cephalograms from 2 years or longer.
Results
During splint therapy, the mean molar intrusion was 2.3 mm. The mean decrease in anterior face height was 1.6 mm, less than expected because of a 0.6-mm mean eruption of the mandibular molars. During the postintrusion orthodontics, the mean change in maxillary molar position was a 0.2-mm extrusion, and there was a mean 0.5-mm increase in face height. Positive overbite was maintained in all patients, with a slight elongation (<2 mm) of the incisors contributing to this. During the 1 year of posttreatment retention, the mean changes were a further eruption of 0.5 mm of the maxillary molars, whereas the mandibular molars intruded by 0.6 mm, and there was a small decrease in anterior face height. Changes beyond 1 year posttreatment were small and attributable to growth rather than relapse in tooth positions.
Conclusions
Intrusion of the maxillary posterior teeth can give satisfactory correction of moderately severe anterior open bites, but 0.5 to 1.5 mm of reeruption of these teeth is likely to occur. Controlling the vertical position of the mandibular molars so that they do not erupt as the maxillary teeth are intruded is important in obtaining a decrease in face height.
Skeletal open bite, often called the long-face syndrome or condition, is regarded as a challenging orthodontic problem to correct. Many orthodontic treatment modalities have been used to close anterior open bites, such as extractions, multiloop edgewise arch-wires, high-pull headgear, chincups, bite-blocks, and functional appliances,1–6 but relapse is common, and even the combination of headgear and a functional appliance is ineffective in changing the skeletal pattern.7 Orthognathic surgery to reposition the maxilla superiorly has been the only way to create significant rotation of the mandible upward and forward, decreasing anterior face height along with correction of the open bite. Recently, temporary anchorage devices (TADs), including miniplates and miniscrews, have been used to intrude the maxillary posterior teeth to allow autorotation of the mandible to close an anterior open bite.8–12
There have been only a few reports of outcomes with this approach beyond individual case reports. Kuroda et al13 concluded in an early article on this method that molar intrusion with TADs is as successful as surgery, but this was based on a small sample of 10 subjects. In a case series of 9 patients treated with maxillary posterior intrusion who had open bites that remained closed, Sugawara et al14 reported a 27% to 30% relapse of the maxillary molars within 1 year. Baek et al15 reported a maxillary molar relapse of 23% and an overbite relapse of 17% over 3 years in a case series of 9 anterior open-bite patients. Deguchi et al16 reported a 22% maxillary molar relapse and an overbite relapse of 13% over 2 years in a study comparing 15 patients treated with TADs and pre-molar extractions with 15 patients treated with conventional edgewise treatment and premolar extractions. In a report using an earlier intrusion sample from the University of North Carolina with a mixture of lingual arch and splint stabilization during intrusion, Profitt et al17 noted that clinically significant reeruption of intruded maxillary molars occurred in about half the patients by 1 year post-surgery. There have been no other previous reports of stability longer than 1 year that included more than 10 consecutively treated patients with the same treatment protocol.
The purposes of this study were to (1) document in a series of consecutively treated patients the amounts of molar intrusion, open-bite correction, and decrease in anterior face height obtained with TADs (miniplates or miniscrews) at the base of the zygomatic buttress and delivery of the intrusion force to a splint covering the maxillary posterior teeth; and (2) evaluate the stability of the intrusion from the completion of active intrusion to the end of orthodontic treatment, at 1 year posttreatment, and at 2 years or longer posttreatment.
MATERIAL AND METHODS
The initial sample consisted of 33 consecutive patients with open bite and long face treated by intrusion of the maxillary posterior teeth in the private orthodontic practice of the senior author (N.R.S.) in Boone, NC, from September 21, 2005, to September 26, 2012. The routine clinical protocol included lateral cephalometric radiographs at the beginning of intrusion (T1), at its completion when the maxillary splint was removed (T2), at the completion of orthodontic treatment (T3), at the 1-year recall (T4), and at 2 or more years posttreatment (T5).
All open-bite patients who accepted treatment with this protocol (TADs and intrusive force to an occlusal splint) were included in the initial sample. This was a retrospective observation study, not a randomized clinical trial; the consecutive-patients approach was to verify that these patients were not selected on the basis of their treatment outcome. Three of the initial 33 patients were dropped because an adequate cephalogram was not obtained at T2 or T3. The final sample consisted of 11 male and 19 female subjects. Three of them did not return for a 1-year cephalogram, so 1-year data were available for 27 patients. Twenty-five of these patients returned for a cephalogram at 2 or more years posttreatment. Their sex distribution, initial open-bite severity, age, and treatment timing characteristics are shown in Table I.
Table I.
Characteristics of the sample
| N (%) | Mean | SD | Range | |
|---|---|---|---|---|
| Female | 19 (63) | |||
| Male | 11 (37) | |||
| Growing patients (<age 20) | 15 (50) | |||
| Age at start of treatment (y) | 30 | 24.1 | 10.7 | 12.7–48.1 |
| Initial overbite (mm) | 30 | −1.2 | 1.7 | −5.0 to 1.8 |
| Time in splint treatment (y) | 30 | 0.5 | 0.1 | 0.3–0.8 |
| Total time in treatment (y) | 30 | 1.6 | 0.6 | 0.5–2.8 |
| Debond to 1-y ceph (T3–T4) (y) | 27 | 1.0 | 0.1 | 0.7–1.3 |
| Debond to >2-y ceph (T3–T5) (y) | 25 | 2.5 | 0.7 | 1.5–4.8 |
Ceph, Cephalogram.
The clinical technique used with these patients is described in some detail in a recent publication,18 and the treatment steps are shown in Figure 1. In brief summary, all patients had a maxillary intrusion splint (AOB-I buccal splint; AOA Laboratories, Sturtevant, Wis) that was bonded to the maxillary teeth, TADs (miniscrews or miniplates) bilaterally at the base of the zygomatic arch, and nickel-titanium coil springs to deliver the intrusive force to the splint (Fig 1, B). Nickel-titanium coil springs with similar forces were used with both miniplates and miniscrews. After the completion of intrusion and removal of the splint, a continuous edgewise wire was placed in all maxillary brackets, and the molars were ligature-tied to the TADs (Fig 1, C). After completion of orthodontic treatment (Fig 1, D), a suck-down retainer with buttons bonded lingual to the maxillary molars was provided the same day and worn nightly with elastics to the buccal TADs (Fig 1, E). Three weeks later, an occlusal coverage AOB hooked retainer (AOA Laboratories) (Fig 1, F) was provided, with elastics worn nightly to the buccal TADs for the first 6 months. Then the retainer was worn without elastics indefinitely.
Fig 1.
A, A 40-year-old man with an anterior open bite with occlusion only on first and second molars; B, intrusion with an AOB-I buccal splint with 2 nickel-titanium coil springs (150 g) attached to the second and fourth hooks of the AOB-I and buccal TADs bilaterally; C, occlusal relationship after intrusion with the AOB splint with molars ligature-tied to the TAD; D, final occlusal relationship at deband (treatment time was 20 months); E, immediate retention with lingual fixed retainers and a suck-down retainer with buttons bonded lingual to the maxillary molars worn nightly with elastics to the buccal TADs for 3 weeks; F, after 3 weeks, an AOB hooked retainer was provided and worn nightly for 6 months with elastics to the bilateral TADs and then continued without elastics indefinitely with the TADs removed; G, after 2 years of retention, the anterior open bite remained closed.
For 16 patients, Vector TAS miniscrews (length, 8 mm; diameter, 1.4 mm; Ormco, Orange, Calif) were placed by the orthodontist (N.R.S.) on the buccal side between either the second premolar and the first molar or the first and second molars, and they were loaded immediately. The other 14 patients had miniplates placed by the same surgeon. The choice of miniplates vs miniscrews was based on whether the patient also had a Class II or Class III malocclusion in conjunction with the anterior open bite. Miniplates with screws placed above the maxillary roots were chosen if translation of molars was necessary to correct the malocclusion. Of the 14 patients with miniplates, 12 had Leibinger Skeletal Anchoring miniplates (Stryker, Kalamazoo, Mich) retained by 3 screws and 2 had C-Tube OrthoAnchor miniplates (KLS Martin, Jacksonville, Fla) retained by 2 screws. The miniplates were loaded 18.7 ± 13.9 days later (range, 7–56 days). Intrusion was continued until a positive overbite was obtained. There were no failures of miniplate anchorage; in 1 patient, a miniscrew that was becoming loose was immediately replaced so that there was no interruption in the intrusion force during active intrusion treatment. In another patient, one miniscrew fell out the day after the patient was debanded and was not replaced, and the other miniscrew was not used during retention.
Statistical analysis
All cephalograms were digitized by a skilled technician at the University of North Carolina. Seven measurements were made at each of 5 time points to evaluate the skeletal and dental changes from intrusion and the amount of change after intrusion.
In this study, the outcomes of interest were the 7 cephalometric variables shown in Table II. Each outcome was analyzed separately by a marginal multivariate regression model with covariates (visit, age at initial visit categorized as younger vs older than 20, sex, and the pairwise interactions of age by visit and sex by visit). The interactions were included to assess whether the pattern of change for age and sex was similar over time. Considering the repeated measure property of the outcomes, the general estimating equation method with an autoregressive working correlation matrix was used. Interactions were removed if they were not statistically significant, and a reduced model was run. Significant interactions were assessed using graphic plots. The level of significance was set at 0.05 for all analyses.
Table II.
Changes in cephalometric variables
| Variable |
Initial to splint out (n = 30)
|
Splint out to debond (n = 30)
|
Debond to 1 year (n = 27)
|
Debond to >2 years (n = 25)
|
||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| LAFH (ANS-Me) (mm) | −1.6 | 2.2 | 0.5 | 2.1 | −0.2 | 1.4 | −0.3 | 1.4 |
|
| ||||||||
| GoGn-SN (°) | −1.2 | 1.0 | 0.2 | 1.1 | 0.0 | 0.9 | 0.0 | 0.8 |
|
| ||||||||
| Overbite (mm) | 2.2 | 1.6 | 0.9 | 1.3 | −0.3 | 0.8 | −0.4 | 1.1 |
|
| ||||||||
| U1-PP (mm) | 0.3 | 1.8 | 0.7 | 1.9 | −0.3 | 1.0 | −0.3 | 1.2 |
|
| ||||||||
| U6-PP (mm) | −2.3 | 1.4 | 0.2 | 1.1 | 0.5 | 1.1 | 0.5 | 1.2 |
|
| ||||||||
| L6-GoGn (mm) | 0.6 | 1.6 | 0.7 | 0.8 | −0.6 | 1.3 | −0.3 | 1.3 |
|
| ||||||||
| L1-GoGn (mm) | 0.6 | 1.0 | 0.8 | 1.2 | −0.2 | 0.9 | −0.1 | 1.2 |
RESULTS
The analysis showed that the pattern of response over time for the younger and older subjects was statistically significantly different for mandibular incisor to mandibular plane (P =0.0002), mandibular molar to mandibular plane (P =0.02), mandibular plane angle (P =0.01), and anterior face height (P = 0.03). In all instances, there were greater changes in the younger group. The pattern of response over time was also statistically significantly different for the sexes, with greater changes in the male patients for mandibular incisor to mandibular plane, mandibular molar to mandibular plane, and maxillary molar to palatal plane (P <0.0001 for all 3). Change in overbite was not linked to age or sex.
The means and standard deviations for changes between T1 and T2 for selected cephalometric variables are shown in Table II. The mean change in the vertical position of the maxillary molar during active intrusion was 2.3 mm, which in turn decreased the mean anterior face height and the mandibular plane angle by 1.6 mm and 1.2°, respectively. The mean change for the mandibular molar was 0.6 mm of extrusion, and the mean change in overbite was an increase of 2.2 mm.
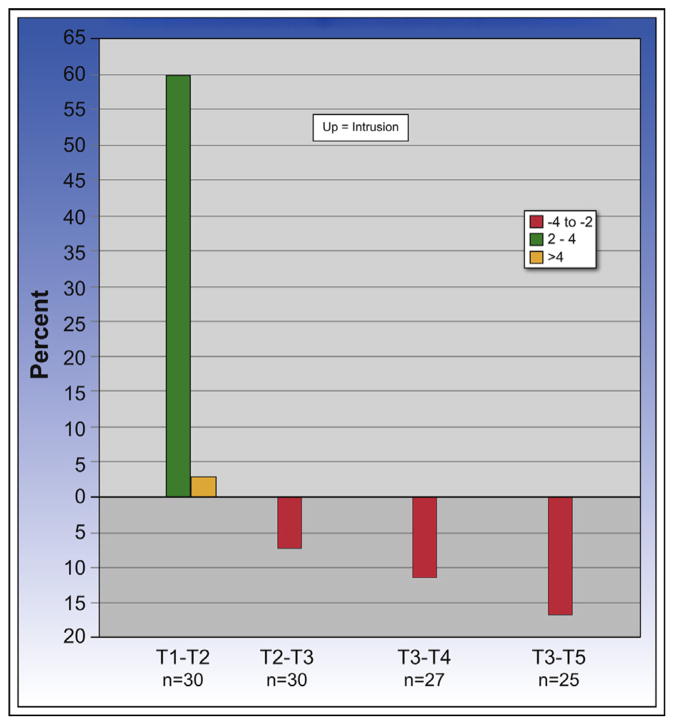
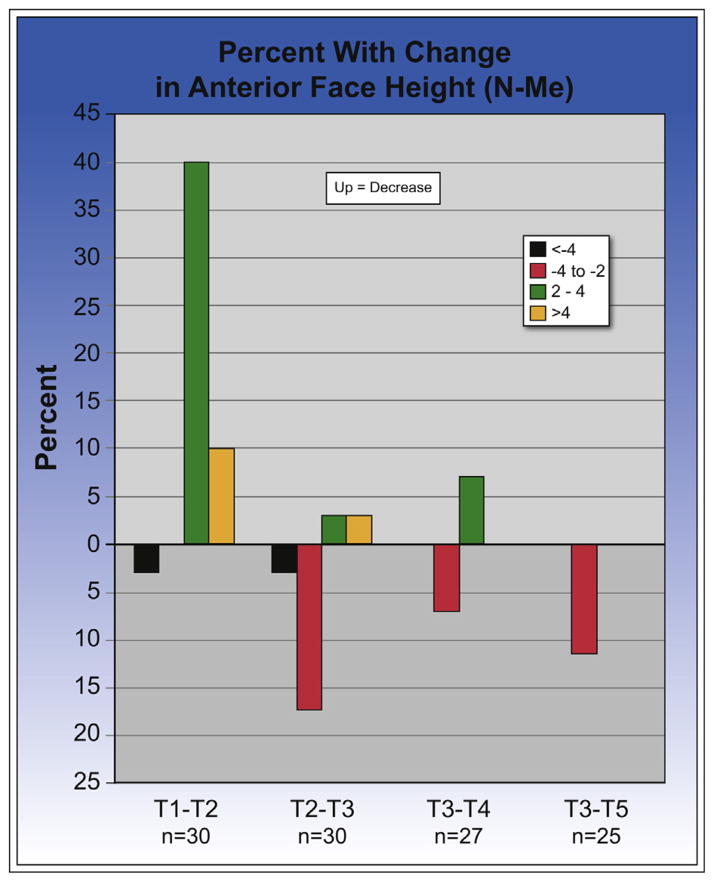
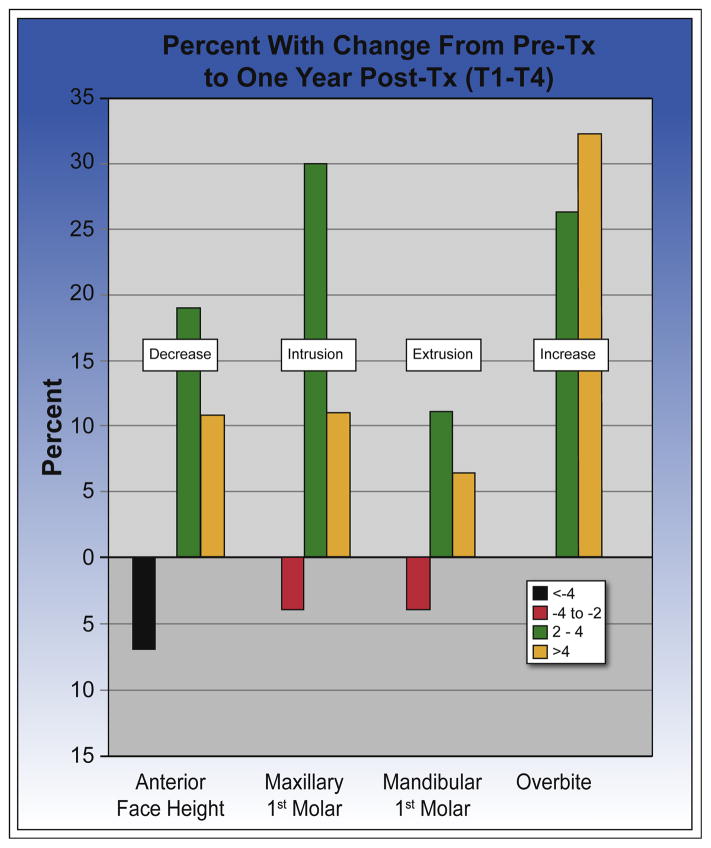
The response in a group of patients to what seemed to be identical treatment often is understood better by looking at the percentage of the patient population who had clinically significant (>2 mm) or highly clinically significant (>4 mm) changes. During active intrusion (T1–T2), 18 of the 30 patients (60%) had 2 to 4 mm of intrusion of the maxillary first molars, and 1 patient (3%) had greater than 4 mm of intrusion (Fig 2). Two patients (7%) had greater than 4 mm of extrusion of the mandibular molars, and 1 patient had 2 to 4 mm of extrusion (ie, the mandibular molars erupted that much while the maxillary molars were being intruded) (Fig 3). Twelve patients (40%) experienced 2 to 4 mm of decrease in anterior face height, and 3 (10%) had a decrease greater than 4 mm (Fig 4). The percentage with change in overbite was similar to that for anterior face height: 12 patients had 2 to 4 mm of increase in overbite, and 5 had a greater than 4-mm increase.
Fig 2.
Percent with change in the maxillary first molar distance from the palatal plane. Note that 60% of the patients had the molar intruded 2 to 4 mm during the splint therapy for intrusion (T1–T2), but only 1 patient had greater than 4 mm of intrusion. During the postintrusion orthodontic treatment, only 2 patients (7%) had 2 to 4 mm of reeruption of the maxillary molars; during the first posttreatment year (T3–T4), 3 patients (11%) had 2 to 4 mm of downward movement, most likely caused by continued vertical growth. From the end of treatment to the more than 2-year recall, 4 patients (16%) had 2 to 4 mm of downward movement, which was also largely due to vertical growth.
Fig 3.
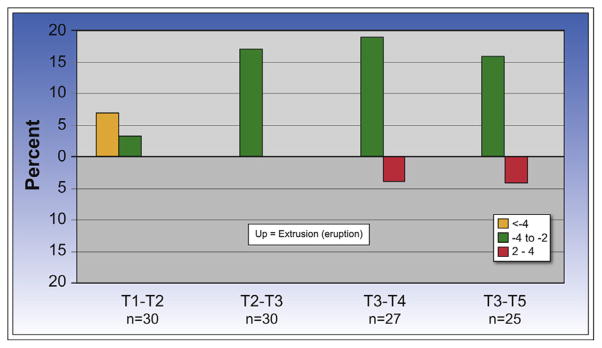
Percent with change in the mandibular first molar distance from the mandibular plane. During splint therapy (T1–T2), 2 patients had greater than 4 mm of eruption of the mandibular first molars (7%), and 1 (3%) had 2 to 4 mm of eruption. During postintrusion orthodontics (T2–T3), 5 (17%) had 2 to 4 mm of eruption. During the first posttreatment year (T3–T4), 5 (19%) had an eruption of 2 to 4 mm, but 1 patient had an eruption of 2 to 4 mm. During the second posttreatment year, 4 (16%) had 2 to 4 mm of eruption, and 1 had 2 to 4 mm of intrusion.
Fig 4.
Percent with postintrusion changes in anterior face height. During T1 to T2, 40% of the patients had 2 to 4 mm of decrease in face height, and another 10% had greater than 4 mm. From T2 to T3, 17% of the patients had 2 to 4 mm of increase, and 1 (3%) had greater than a 4-mm increase. In the T3 to T4 period, 2 patients had 2 to 4 mm of increase, 2 had 2 to 4 mm of decrease, and 12% had increases from T3 to T5. During treatment, the change was largely reeruption of the intruded molars; after treatment, vertical growth in the younger patients was a major contributor to the change.
There were changes during the postintrusion orthodontic treatment (T2–T3). After removal of the AOB splint, the maxillary molars were ligature-tied to the TADs to hold the position of the maxillary molars while orthodontic treatment was completed. The mean change in maxillary molar position was 0.3 mm of relapse: ie, extrusion (Table II). The mean change in mandibular molar position was an extrusion (eruption) of 0.7 mm, and the mean change in the face height was a 0.2-mm increase. The maxillary incisors and the mandibular incisors had mean elongations of 0.7 and 0.8 mm, respectively. The mean change in overbite was an increase of another 0.9 mm.
The variability in response is shown well in the percentages of patients with changes. Two patients (7%) had 2 to 4 mm of extrusion of the maxillary molars after the splint was removed (Fig 2), and 5 (17%) experienced 2 to 4 mm of eruption of the mandibular molars (Fig 3); these changes accompanied postintrusion increases in anterior face height of 2 to 4 mm in 5 patients (17%) and greater than 4 mm in 1 patient (Fig 4). Eight patients had 2 to 4 mm of mandibular incisor elongation, 6 patients had 2 to 4 mm of maxillary incisor elongation, and 1 patient had greater than 4 mm of maxillary incisor elongation. Six patients had greater than a 2-mm increase in overbite.
From the end of treatment during 1 year of retention (T3–T4), the mean changes were a 0.2-mm decrease for anterior face height and a 0.3-mm decrease for overbite (Table II). The mean change in maxillary molar position was a further eruption of 0.5 mm, whereas for the mandibular molar, it was an intrusion of 0.6 mm.
Some patients had changes large enough to be clinically significant: 3 patients (11%) had 2 to 4 mm of eruption of the maxillary molars (Fig 2); 5 patients (19%) showed 2 to 4 mm of extrusion of the mandibular molars, and 1 patient had intrusion of the mandibular molars of 2 to 4 mm (Fig 3); and 2 patients (7%) showed 2 to 4 mm of increase in anterior face height, whereas 2 had greater than a 2-mm decrease (Fig 4). None of the patients had greater than a 2-mm change in the vertical position of the mandibular incisors or in overbite, but 1 patient had 2 to 4 mm of elongation of the maxillary incisors, and another had 2 to 4 mm of intrusion of these teeth.
Figure 5 shows the percentages of patients with clinically significant changes from T1 to T4 for anterior face height, maxillary and mandibular molars, and overbite. Anterior face height showed 2 to 4 mm of decrease in 5 patients (19%) and a highly clinically significant decrease greater than 4 mm in 3 patients (11%), but 2 patients (7%) also had greater than a 4-mm increase in face height. In evaluating this, it is important to remember that vertical growth occurred after intrusion in the younger patients. Maxillary molar intrusions of 2 to 4 mm occurred in 30% of the patients; this was greater than 4 mm in 11%, and the same percentage of patients had 2 to 4 mm of mandibular molar eruption. At the 1-year follow-up, no patient had an open bite, 26% had 2 to 4 mm of increase in overbite, and 33% had greater than a 4-mm increase in overbite.
Fig 5.
The percentage of patients with clinically significant (>2 mm) changes from pretreatment to 1 year post-treatment. The percentage with greater than a 2-mm decrease in anterior face height was greater than the percentage with greater than a 2-mm intrusion of the maxillary first molar, but much less than twice as great as would be suggested by the geometry of the mandible. The number of patients with greater than 2 mm of eruption of the mandibular first molar accounts for the discrepancy. The percent with greater than a 4-mm increase in overbite is higher than the percent with greater than a 4-mm decrease in anterior face height; elongation of incisors is the reason for that.
For patients who were out of treatment for 2 years or longer (T3–T5), the mean changes in anterior face height, overbite, and vertical position of both maxillary and mandibular first molars were within a fraction of a millimeter of the 1-year changes (Table II). The percentages of patients with changes also were similar between the 1-year (T4) and 2-years-or-longer (T5) groups. At T5, 3 patients (12%) had 2 to 4 mm of decrease in anterior face height, and none had an increase; 2 patients had 2 to 4 mm of decrease in overbite, and 1 patient had 2 to 4 mm of increase; 4 patients (16%) had 2 to 4 mm of eruption of the maxillary molars; and 4 patients had 2 to 4 mm of intrusion of the mandibular molars, and 1 patient had 2 to 4 mm of eruption.
DISCUSSION
The marginal multivariate regression indicated statistically significant but small differences between younger and older subjects as well as between male and female patients in the response to treatment, particularly with regard to the changes in the position of both the mandible and the mandibular teeth. The relationship to age is not surprising because the younger patients had mandibular growth during and after the intrusion procedure; the relationship to sex probably occurred because girls are more mature than boys of the same age, and their growth declines to adult levels at a younger age. Because of these differences in the patterns of change, however, one cannot be precisely sure of the cause of changes in mandibular position and mandibular dentition. This must be kept in mind in the interpretation of the mandibular changes.
Positive overbite of at least 1 mm was achieved for all patients from T1 to T2. The amount of intrusion needed to obtain a positive overbite varied with the severity of the initial open bite; this explains the differences in the amount of posterior intrusion. From jaw geometry, 2 mm of intrusion posteriorly should result in about 4 mm of anterior open-bite closure. In this study, the mean change in maxillary molar position was 2.3 mm of intrusion, so one would expect a change in overbite greater than 4 mm, but the mean change was only 2.2 mm.
There are 2 possible explanations for this. First, eruption of the mandibular posterior teeth while the maxillary teeth are being intruded would decrease the jaw rotation that would reduce overbite. The data show that greater than a 2-mm eruption of the mandibular molars occurred in 3 patients (10%) during intrusion. One advantage of using the splint is that it tends to impede eruption of the mandibular teeth, but to be sure that molar extrusion cannot occur, these teeth can be ligature-tied or chained to mandibular miniscrews during maxillary intrusion treatment.14,17 Bilateral mandibular TADs to control or intrude the mandibular molars are recommended for patients with severe long face or open bite.
Second, the AOB splint is typically fabricated to cover the maxillary premolars and molars and not the canines. Thus, the intrusion force is applied to all posterior teeth, whereas the canines and the incisors are not affected. In some patients, when the splint is removed, the canines are the only teeth that contact, a posterior open bite is present, and the potential increase in overbite is not fully expressed because of the premature contact of the canines (Fig 6). Our experience suggests that some intrusion of the maxillary canines often is needed, and when this is the case, it would improve mandibular rotation to include them in the fabrication of the AOB splint or have an archwire from first premolar to first premolar so that the canines are intruded slightly along with the intrusion of the first premolars (Fig 1, B).
Fig 6.
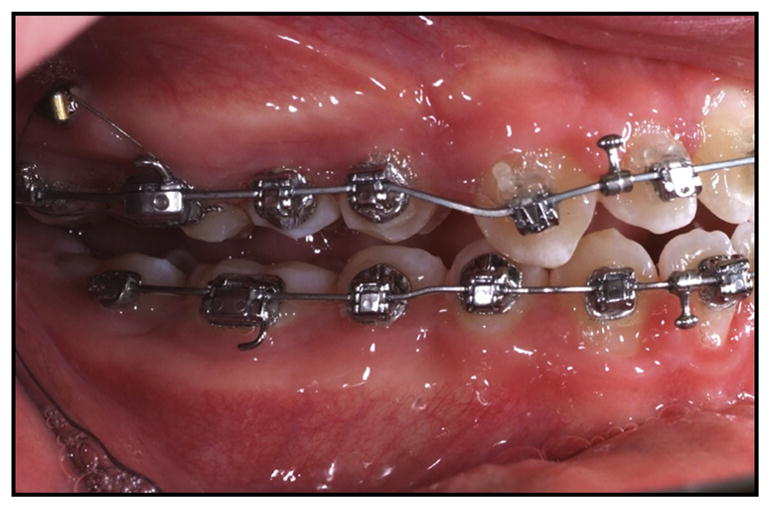
When the posterior occlusal covering splint is removed after intrusion, the canines are frequently the only teeth that contact; this causes a posterior open bite and a less positive overbite than what otherwise would have been expressed after molar intrusion treatment.
Clinical observation suggests that the rate of intrusion decreases with time, but no good data are available to document this. It is difficult to justify multiple cephalograms during intrusion and difficult to measure the rate of intrusion directly with adequate accuracy. One possibility is that as a tooth is intruded, cortical rather than medullary bone is likely to be encountered, especially in patients in whom the downward movement of the maxillary teeth during growth was due primarily to growth of the maxilla, not to supereruption of the teeth.
Although the maximum amount of intrusion that can be obtained is unknown, the greatest intrusion in this sample was 6.7 mm during 10 months of intrusive force with the splint. However, in this same nongrowing adult patient, the mandibular molars extruded 6.2 mm, and the anterior face height decreased by only 1.3 mm.
During T2 to T3, when the splint is removed, eruption of the maxillary posterior teeth is inhibited by tying the archwire to the TAD, but the mandibular molars are free to erupt, especially if canine interference creates a temporary posterior open bite.
During this time period, the maxillary first molars were relatively stable, but 2 patients had 2 to 4 mm of eruption (Fig 2). For the mandibular first molars, the mean change was 0.7 mm of eruption, and almost 20% of the patients had greater than 2 mm of eruption (Fig 3). Both the maxillary and mandibular incisors also showed eruption during the postintrusion orthodontics, with mean changes for the maxillary incisor of 0.7 mm, 2 to 4 mm of eruption in 6 patients (22%), and greater than 4 mm in 1 patient. This is not necessarily undesirable; elongating the maxillary incisors to obtain optimal display of the incisors is a necessary part of treatment for some patients. For the mandibular incisors, 2 patients had increases of 2 to 4 mm and 1 patient had greater than a 4-mm increase. Eruption of the incisors was a factor in maintaining a positive overbite and the main reason that the mean change in overbite during fixed appliance treatment was an increase of 0.8 mm.
Sugawara et al14 reported a 30% relapse of the mandibular molars at 1 year posttreatment, and Baek et al15 reported a 23% relapse of the maxillary molars over a 3-year retention period, with 80% of the relapse occurring during the first year. Since these findings were previously known, many patients in our study were left with a mild posterior open bite after intrusion and after treatment to allow for some relapse of the maxillary molars. The percentage with clinically significant relapse of the maxillary molars was relatively small: 11% of our patients showed greater than 2 mm of eruption after 1 year and 16% at 2 years. This also was the case for relapse in overbite: 15% and 22% of the patients showed relapses in overbite greater than 1 mm after 1 year and 22% at 2 years, but none had greater than a 2-mm change (Table II).
During retention, an anterior open-bite retainer with occlusal coverage was given to the patients. It is interesting that the mandibular molars that erupted during active orthodontics often intruded after the appliance was removed. It is possible that this was related to biting pressure on the occlusal coverage retainer.
Sugawara et al14 and Baek et al15 reported extrusions of incisors during retention to help maintain or deepen the bite that counteracted the bite opening caused by molar eruption. In our study, 4% and 8% of our patients showed intrusions, not extrusion, of the maxillary incisors greater than 2 mm after 1 year and 2 years, respectively. It is likely that the incisors that were elongated during treatment relapsed during retention.
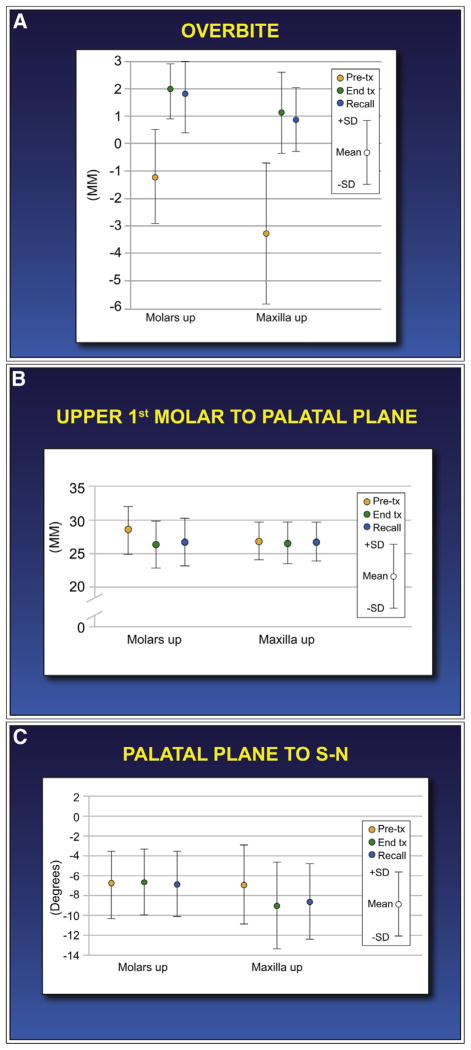
There were some clinical implications in the comparisons with orthognathic surgery outcomes. Selected outcomes in 37 patients who had a LeFort I osteotomy at the University of North Carolina during the same time period as the intrusion patients are compared in Figure 7. The patients selected for surgery had significantly larger open bites before treatment. Correction of the open bite created an average of 1 mm of overbite in both the surgery and intrusion patients. There was some posttreatment decrease in overbite in both groups, but less than would have been expected from the amount of downward movement of the molars because of compensatory elongation of the maxillary and mandibular incisors: ie, elongation of the incisors occurred in the surgery and intrusion patients as a way to maintain overbite. The findings from this surgery sample are consistent with previous reports on postsurgical stability.19–21
Fig 7.
Comparison of changes from pretreatment to 1 year posttreatment in the patients with molar intrusion with a sample of patients treated with LeFort I osteotomy to superiorly reposition the mandible: A, the average severity of the open bite before surgery was greater than for the intrusion patients, but the correction to positive overbite was almost exactly the same for the 2 groups, and the amount of posttreatment change also was similar; B, during intrusion, one would expect the distance from the maxillary molar to the palatal plane to decrease, but this distance should not change because of a maxillary osteotomy; this is what occurred. This distance was similar for the surgery and intrusion patients: ie, both groups experienced downward eruption of the molars to about the same extent. C, Change (°) in the orientation of the palatal plane to the S-N line; this would not be expected to change in the intrusion patients and did not; it did change in the surgery patients since the maxilla was usually rotated at surgery. The intrusion patients had a zero orientation, much closer to normal than the surgery patients.
As one would expect, the surgery patients had no change in the relationship between the maxillary first molar and the palatal plane, whereas the intrusion patients had a significant decrease (Fig 7). In contrast, the intrusion patients showed no change in the inclination of the palatal plane to SN, but the surgery patients had an increase in this angle as the posterior maxilla was elevated. The mandibular plane angle had little change in the intrusion patients and an average decrease of 2.5° for the surgery patients. In the first posttreatment year, there was a slightly greater downward movement of the maxillary molars in the surgery group than in the intrusion patients. It seems reasonable that in the surgery group this was largely due to the slight downward repositioning of the maxilla and to the reeruption of the teeth in the intrusion group. Beyond 1 year post-surgery, downward movement of the maxilla, much like a resumption of the original pattern of growth, was observed in about 20% of the patients.21
In this study, the maxillary first molars were intruded by 2.3 mm during active intrusion; this was the same as Deguchi et al16 reported in a study of 15 patients and similar to the 2.4 mm that Baek et al15 reported for 9 patients. Kuroda et al13 reported an average 3.3° decrease of the MPA for the group treated with surgery and no change in the group treated with TADs. Akan et al,22 in a more recent report of 19 patients in whom intrusion force was delivered to an occlusal splint, reported a mean intrusion of 3.4 mm and a 3.8° decrease in the MPA, but they presented no data beyond the period of active intrusion.
CONCLUSIONS
Intrusion of maxillary posterior teeth can give satisfactory correction of moderately severe anterior open bite, with elimination of 5 to 6 mm of open bite, but some of the change in the position of the mandible is likely to be lost after treatment as the intruded teeth reerupt by 0.5 to 1.5 mm.
Controlling the vertical position of the mandibular molars, so that they do not erupt as the maxillary teeth are being intruded, is important in obtaining a decrease in face height.
Part of the open-bite correction in most patients with molar intrusion is slight incisor elongation, which is rarely as much as 2 mm and never more than that. This occurs primarily during the finishing phase of treatment.
In comparison with maxillary molar intrusion as accomplished in this study, LeFort I surgery is more likely to produce shortening of anterior face height.
Acknowledgments
We thank Debora Price for digitizing the cephalograms and developing the intrusion and surgery data bases, Sean Chen for the logistic regression calculations, Luke Current and Amanda Pritchard for their assistance in compiling the cephalograms for analysis, and Gibson McCall, Turner Hull, and Camilla Tulloch for their pilot investigations.
Supported in part by NIH grant DE-02115 from the National Institute of Dental and Craniofacial Research.
Footnotes
All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest, and none were reported.
References
- 1.Janson G, Valarelli FP, Henriques JF, de Freitas MR, Cancado RH. Stability of anterior open bite nonextraction treatment in the permanent dentition. Am J Orthod Dentofacial Orthop. 2003;124:265–76. doi: 10.1016/s0889-5406(03)00449-9. [DOI] [PubMed] [Google Scholar]
- 2.Kuster R, Ingervall B. The effect of treatment of skeletal open bite with two types of bite-blocks. Eur J Orthod. 1992;14:489–99. doi: 10.1093/ejo/14.6.489. [DOI] [PubMed] [Google Scholar]
- 3.Iscan HN, Dincer M, Gultan A, Meral O, Taner-Sarisoy L. Effects of vertical chincup therapy on the mandibular morphology in open-bite patients. Am J Orthod Dentofacial Orthop. 2002;122:506–11. doi: 10.1067/mod.2002.128643. [DOI] [PubMed] [Google Scholar]
- 4.Kim YH, Han UK, Lim DD, Serraon ML. Stability of anterior openbite correction with multiloop edwise archwire therapy: a cephalometric follow-up study. Am J Orthod Dentofacial Orthop. 2000;118:43–54. doi: 10.1067/mod.2000.104830. [DOI] [PubMed] [Google Scholar]
- 5.Küçükkeleş N, Acar A, Demirkaya AA, Evrenol B, Enacar A. Cephalometric evaluation of open bite treatment with NiTi archwires and anterior elastics. Am J Orthod Dentofacial Orthop. 1999;116:555–62. doi: 10.1016/s0889-5406(99)70189-7. [DOI] [PubMed] [Google Scholar]
- 6.Kiliaridis S, Egermark I, Thilander B. Anterior open bite treatment with magnets. Eur J Orthod. 1990;12:447–57. doi: 10.1093/ejo/12.4.447. [DOI] [PubMed] [Google Scholar]
- 7.Freeman CS, McNamara JA, Jr, Baccetti T, Franchi L, Graff TW. Treatment effects of the bionator and high-pull facebow combination followed by fixed appliances in patients with increased vertical dimensions. Am J Orthod Dentofacial Orthop. 2007;131:184–95. doi: 10.1016/j.ajodo.2005.04.043. [DOI] [PubMed] [Google Scholar]
- 8.Sherwood KH, Burch JG, Thompson WJ. Closing anterior open bites by intruding molars with titanium miniplate anchorage. Am J Orthod Dentofacial Orthop. 2002;122:593–600. doi: 10.1067/mod.2002.128641. [DOI] [PubMed] [Google Scholar]
- 9.Erverdi N, Keles A, Nanda R. The use of skeletal anchorage in open bite treatment: a cephalometric evaluation. Angle Orthod. 2004;74:381–90. doi: 10.1043/0003-3219(2004)074<0381:TUOSAI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 10.Erverdi N, Usumez S, Solak A. New generation open-bite treatment with zygomatic anchorage. Angle Orthod. 2006;76:519–26. doi: 10.1043/0003-3219(2006)076[0519:NGOTWZ]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 11.Park H, Kwon O, Sung J. Nonextraction treatment of an open bite with microscrew implant anchorage. Am J Orthod Dentofacial Orthop. 2006;130:391–402. doi: 10.1016/j.ajodo.2005.07.014. [DOI] [PubMed] [Google Scholar]
- 12.Xun C, Zeng X, Wang X. Microscrew anchorage in skeletal anterior open bite treatment. Angle Orthod. 2007;77:47–56. doi: 10.2319/010906-14R.1. [DOI] [PubMed] [Google Scholar]
- 13.Kuroda S, Sakai Y, Tamamura N, Deguchi T, Takano-Yamamoto T. Treatment of severe anterior open bite with skeletal anchorage in adults: comparison with orthognathic surgery outcomes. Am J Orthod Dentofacial Orthop. 2007;132:599–605. doi: 10.1016/j.ajodo.2005.11.046. [DOI] [PubMed] [Google Scholar]
- 14.Sugawara J, Baik UB, Umemori M, Takahashi I, Nagasaka H, Kawamura H, et al. Treatment and posttreatment dentoalveolar changes following intrusion of mandibular molars with application of a skeletal anchorage system (SAS) for open bite correction. Int J Adult Orthod Orthognath Surg. 2002;17:243–53. [PubMed] [Google Scholar]
- 15.Baek MS, Choi YJ, Yu HS, Lee KJ, Kwak J, Park YC. Long-term stability of anterior open-bite treatment by intrusion of maxillary posterior teeth. Am J Orthod Dentofacial Orthop. 2010;138:396, e1–9. doi: 10.1016/j.ajodo.2010.04.023. [DOI] [PubMed] [Google Scholar]
- 16.Deguchi T, Kurosaka H, Oikawa H, Kuroda S, Takahashi I, Yamashiro T, et al. Comparison of orthodontic treatment outcomes in adults with skeletal open bite between conventional edgewise treatment and implant-anchored orthodontics. Am J Orthod Dentofacial Orthop. 2011;139(Suppl):S60–8. doi: 10.1016/j.ajodo.2009.04.029. [DOI] [PubMed] [Google Scholar]
- 17.Proffit WR, Scheffler N, McCall GG. Skeletal anchorage: its possible impact on orthognathic surgery. In: McNamara JA Jr, editor. Looking forward… looking back. Monograph 50. Ann Arbor: Center for Human Growth and Development; University of Michigan; 2014. Craniofacial Growth Series. [Google Scholar]
- 18.Scheffler NR, Proffit WR. Skeletal anchorage technique for intrusion of maxillary posterior teeth in treatment of anterior open bite. J Clin Orthod. 2014;48:158–68. [PubMed] [Google Scholar]
- 19.Proffit WR, Phillips C, Turvey TA. Stability following superior repositioning of the maxilla. Am J Orthod Dentofacial Orthop. 1987;92:151–63. doi: 10.1016/0889-5406(87)90370-2. [DOI] [PubMed] [Google Scholar]
- 20.Bailey LJ, Phillips C, Proffit WR, Turvey TA. Stability following superior repositioning of the maxilla by LeFort I osteotomy: five year follow-up. Int J Adult Orthod Orthognath Surg. 1994;9:163–74. [PubMed] [Google Scholar]
- 21.Proffit WR, Phillips C. Physiologic responses to treatment and postsurgical stability. In: Proffit WR, White RP Jr, Sarver DM, editors. Contemporary treatment of dentofacial deformity. St Louis: Mosby; 2003. pp. 646–76. [Google Scholar]
- 22.Akan S, Kocaderelli I, Aktas A, Tasar F. Effects of maxillary molar intrusion with zygomatic anchorage on the stomatognathic system in anterior open bite patients. Eur J Orthod. 2013;35:93–102. doi: 10.1093/ejo/cjr081. [DOI] [PubMed] [Google Scholar]