Key Clinical Message
Hypohydrotic ectodermal dysplasia is a hereditary disorder, which affects ectodermal derivatives. It manifests several abnormalities of the teeth, and is commonly inherited through female carriers. This case report presents a patient with compromised esthetics and function. A multidisciplinary approach was planned involving an oral pathologist, endodontist, orthodontist and a prosthodontist.
Keywords: Ectodermal dysplasia, esthetics, function, hypodontia, multidisciplinary
Introduction
Ectodermal dysplasia is a heterogenous group of disorder characterized by developmental dystrophies affecting ectodermal derivatives such as teeth, hair, nails, skin, and sweat glands in varying degrees 1. Ectodermal dysplasia syndrome was first described in the medical literature by Thurman in 1848 2. But the term was coined by Weech in 1929. Most cases are caused by mutation in the EDA gene which are inherited in an X-linked recessive pattern affecting males and is inherited through female carriers. It can also occur due to deletion of certain genes located on different chromosomes. They can occur in people without history in which de novo mutation has occurred. These disorders are relatively rare with an estimated incidence of 1–7 cases per 100,000 live births. More than 170 different subtypes of ectodermal dysplasia have been identified 3. A distinct form of X-linked hypohydrotic ectodermal dysplasia is associated with immune deficiency. Clinical signs include trichodysplasia (abnormal hair) in 91% of cases, tooth agenesis in 80%, onychodysplasia (abnormal hair) in 75%, and dyshidrosis (abnormal sweat glands) in 42% 4. Signs and symptoms are not very evident until infancy or childhood. The affected individual shows normal life expectancy and normal intelligence.
There are two syndromes associated with ectodermal dysplasia based on the presence or absence of sweat glands:
Hypohydrotic (Anhydrotic) ectodermal dysplasia – Sweat glands are deficient: Christ–Siemens Tourine Syndrome, and Hydrotic ectodermal dysplasia – Sweat glands are not affected: Clouston Syndrome 3,5.
Classification of Ectodermal Dysplasia
According to the presence or absence of four primary structures ectodermal dysplasia (ED) defects are classified into different subgroups 6:
ED1: Trichodysplasia (hair dysplasia)
ED2: Dental dysplasia
ED3: Onychodysplasia (nail dysplasia)
ED4: Dyshidrosis (sweat gland dysplasia)
Based on the above, the 150 different types of ectodermal dysplasias are categorized into one of the following subgroups made up from the primary ED defects 6:
Subgroup 1-2-3-4
Subgroup 1-2-3
Subgroup 1-2-4
Subgroup 1-2
Subgroup 1-3
Subgroup 1-4
Subgroup 2-3-4
Subgroup 2-3
Subgroup 2-4
Subgroup 3
Subgroup 4
The most common ectodermal dysplasias are hypohidrotic (anhidrotic) ED which falls under subgroup 1-2-3-4 and hydrotic ED which comes under subgroup 1-2-3. The three most recognized ectodermal dysplasia syndromes fall into the subgroup 1-2-3-4, as they show features from all four of the primary ED defects. They are as follows:
Ectrodactyly-ED-clefting syndrome
Rapp–Hodgkin hypohidrotic ED
Ankyloblepharon, ectodermal defects, cleft lip/palate (AEC) or Hay–Wells syndrome 6
Ectodermal dysplasia typically affects the four organs primarily involved viz, hair, nails, teeth, and sweat glands (Table1) 6.
Table 1.
Organs affected by ectodermal dysplasia
| Affected organ | Features |
|---|---|
| Hair |
|
| Nails |
|
| Teeth |
|
| Sweat glands |
|
Genetics of Ectodermal Dysplasia
The gene encoding for a protein expressed in keratinocytes, hair follicles, and sweat glands is defective. The hair may be absent or sparse and reduction or absence of sweat glands results in the inability to regulate body temperature. Nails are often brittle and thin. Teeth show abnormal morphogenesis or may be absent. Usually patient presents with hypodontia, hypoplasia, retained deciduous teeth, and facial disfigurement 7.
Hypohidrotic ectodermal dysplasia as the most common type seems to show an X-linked inheritance pattern with the gene mapping to Xq12-q13; therefore, males are more susceptible than females. The gene that causes Hydrotic ED has been identified to be GJB6 which encodes for connexin-30. GJB6 has been mapped to the pericentrometric region of chromosome 13q. The Hydrotic type is inherited in an autosomal dominant pattern 3,8. The cloning of genes has led to the identification of a novel transmembrane protein ectodysplasia (TNF family ligand) and receptor edar (TNF receptor). This TNF ligand and receptor have a developmental regulatory role. These are associated with epithelial mesenchymal interactions and signaling pathways that regulate ectodermal appendage formation and organogenesis during the initiation of development 9.
Prenatal Diagnosis
The diagnosis has been made on fetal skin biopsy, obtained by fetoscopy by 20 weeks gestation after determination of the sex of the fetus. Histological analysis demonstrates complete lack of or reduction in the number of pilosebaceous follicles and the lack of sweat glands primordia in multiple skin biopsies. The interpretation of the biopsies will be difficult since there is normal regional variability of the distribution of skin appendages of fetal skin, and that sweat gland primordia only begin to develop at around 20 week gestation. Disadvantage of this procedure is that it is technique sensitive and is of considerable risk to the pregnancy 10.
Case Report
This is a case report of a 24-year-old female patient who visited the Department of Prosthodontics, Pushpagiri College of Dental Sciences, Thiruvalla; with complaints of retained deciduous and missing permanent teeth since childhood, which gave an unesthetic facial appearance.
Medical and Family History
Both her parents were normal and had no history of such a condition. They had consanguineous marriage. Amongst her two male siblings, one was diagnosed with ectodermal dysplasia. A thorough family history was recorded and none of the existing family members or the previous generations had a similar problem. The medical history was otherwise unremarkable.
Dental History
Some of the deciduous teeth were shed normally, others were retained. This patient was assessed clinically and radiographically. Among the permanent teeth, few were missing 11,12 (Table2). The problems associated with partial anodontia were difficulty in chewing and unesthetic appearance. (Figs1 and 2). The alveolar process was diminished and the lower arch was considerably under developed.
Table 2.
Complement of Teeth
| Maxillary arch | |||||||||||||||
| Right side | Left side | ||||||||||||||
| M | M | E | R | R | E | R | E | E | R | E | M | M | E | M | M |
| 8 | 7 | 6 | E | D | 3 | B | 1 | 1 | B | 3 | 4 | 5 | 6 | 7 | 8 |
| Mandibular arch | |||||||||||||||
| Right side | Left side | ||||||||||||||
| 8 | 7 | 6 | 5 | 4 | C | B | A | A | B | C | 4 | 5 | 6 | 7 | 8 |
| M | M | E | E | E | R | R | R | R | R | R | E | E | E | M | M |
E, Erupted teeth; R, Retained deciduous teeth; M, Missing teeth.
Figure 1.
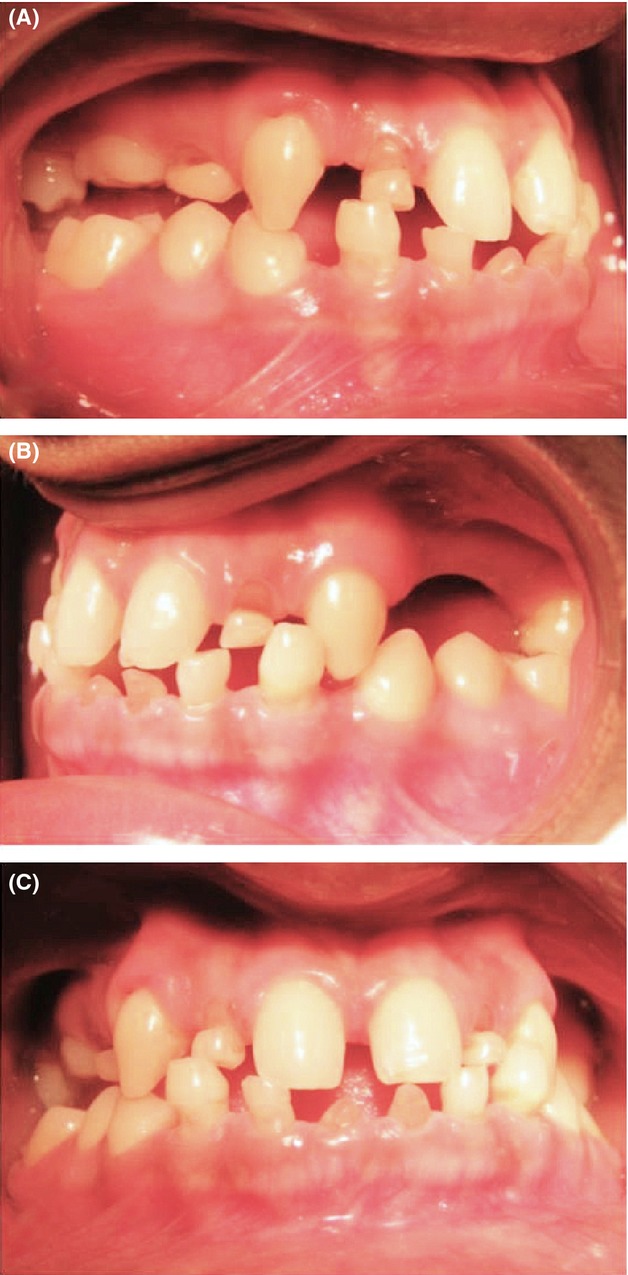
Intraoral Occlusion, (A) - Left Side, (B) - Right Side, (C) - Anterior.
Figure 2.
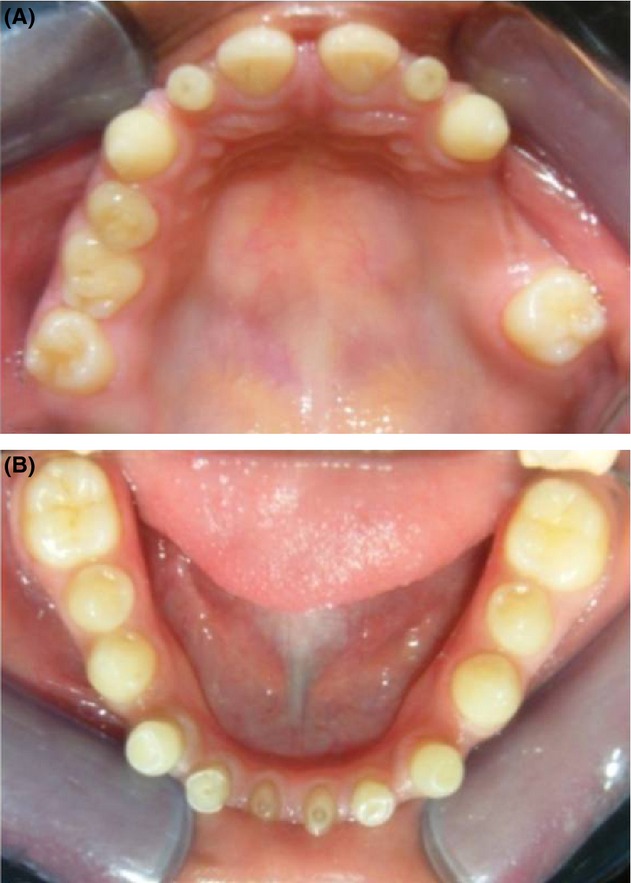
Intraoral View (A) - Maxillary Arch (B)- Mandibular Arch.
Clinical Manifestations
On external examination, the patient's jaws were normal, but had sparse hair and eyebrows. There were no deformities of the hands, fingers or ears. Patient's orthopantomograph (OPG) revealed few missing and retained teeth (Fig.3). The deciduous lateral incisors and molars were retained in the maxillary arch, and deciduous anteriors were retained in the mandibular arch, (Table2). Her anterior teeth were in edge to edge relation. Most of the permanent teeth were missing. The patient complained that she had reduced sweating and frequent episodes of fever. Her vital signs were normal and there were no other signs of disability. The case was discussed with an oral pathologist to confirm this as a case of hypohydrotic ectodermal dysplasia.
Figure 3.
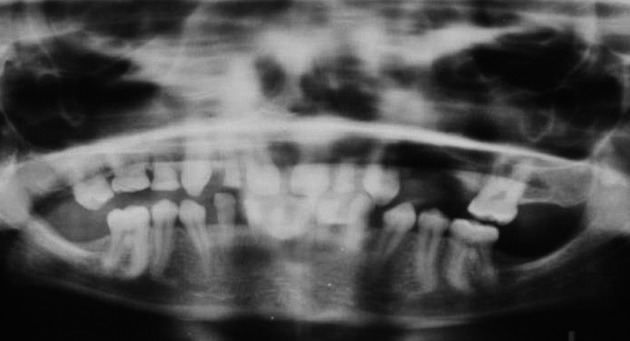
Orthopantamograph of the patient.
Management
For the successful treatment of the patient, a multidisciplinary team effort is vital which involved an orthodontist, an endodontist, and a prosthodontist 13,14. Therapeutic options normally range from partial dentures followed by extensive restorative and prosthetic treatment, which involves bone grafting and dental implants. The definitive treatment plan included fixed, removable, implant-retained prostheses or a combination of these options. Endosseous implants were a better option, but the patient was unable to afford the cost of the treatment 15.
After multidisciplinary consultations were conducted, a treatment plan with five stages was designed. In Stage 1, the case was discussed with an endodontist and it was decided to restore the deciduous teeth with composite resin without any invasive endodontic procedure. After initial restorative and prophylactic measures, primary impressions were recorded using alginate impression material (3M ESPE®) and diagnostic models were prepared in Dental Stone (Plaster Class III – Goldstone®, Asian Chemicals, Veraval Industrial Area, Rajkot, Gujarat). Patient was not willing for extraction of deciduous teeth, so it was planned to retain the upper deciduous teeth.
In stage 2, Facebow transfer was done and the diagnostic casts were mounted on a semi-adjustable articulator with centric occlusion records. Since the upper and lower anterior teeth were in edge to edge relation, we planned for an orthodontic correction (Fig.4). Patient was referred to the department of orthodontics for adjunctive orthodontic correction in order to facilitate prosthodontic rehabilitation 13,16. Protraction of upper anteriors was planned to give an adequate overjet. Initial leveling and aligning was achieved in round Nickel Titanium arch wires. Later round and rectangular S.S arch wires were used with protraction mechanics to achieve proclination for the overjet. Mesialization was done to close the diastema and it was retained in position by giving a bonded palatal retainer. Maxillary canines were also mesialized to correct the spacing for the lateral incisors.
Figure 4.

Othodontic correction.
After the adjuvant orthodontic treatment, in stage 3 diagnostic wax-up was done on the mounted casts. Since the deciduous teeth were retained, there was spacing between the anterior teeth and patient was apprehensive about the esthetics. So we decided to give a provisional prosthesis 17,18. It was decided to increase the vertical dimension by 2 mm to achieve anterior guidance and to open the bite to prevent interference with lower anteriors during protrusive movement. Initially, tooth preparation was done and temporary crowns were given on the upper deciduous lateral incisors and temporary fixed dental prosthesis was given on upper right deciduous molars (D and E), using autopolymerizing acrylic resin (Rapid Repair, Asian Acrylates, Mumbai, INDIA). In the upper left quadrant, a temporary fixed dental prosthesis was given in relation to 3, 4, 5, and 6. The bite was raised by 2 mm. Since the roots of lower anterior deciduous teeth were resorbed, we planned to extract it and a removable partial denture was made to replace them.
In stage 4, after 4 weeks, the patient was recalled and clinical examination revealed she had adjusted to the new vertical dimension. Since the upper prosthesis was given on deciduous teeth, we decided to give the final prosthesis in heat cure acrylic resin. The upper temporary crowns were removed and final impressions were made in addition silicone impression material (Aquasil® Soft Putty – Regular Set and Aquasil® LV Type III Light Bodied consistency, Dentsply®). Permanent heat cure acrylic crowns were fabricated in the new vertical dimension in relation to B, D, E on the right side and B, 3, 4, 5, 6 on the left side on the upper arch using heat cure acrylic denture material and heat cure cross-linked liquid (Orthoplast®). Facebow transfer was done and the casts prepared in die stone (Class IV dental stone – Pearlstone®, Asian Chemicals) were mounted in the new vertical dimension for fabricating the permanent restorations in the lower arch. The lower partial denture was removed and tooth preparation was done on the first and second premolars on either side (34, 35 and 44, 45). Impressions were recorded and provisional restoration was given. The patient was asked to report after 48 h for making further occlusal corrections. She was subsequently reviewed after 1 week; 1 month, and 3 months for periodic evaluation.
In stage 5, final oral rehabilitation was accomplished with full coverage metal ceramic fixed dental prosthesis in the lower arch (Fig.5). The establishment of normal facial characteristics and smile improved the patient's emotional and psychological profile.
Figure 5.
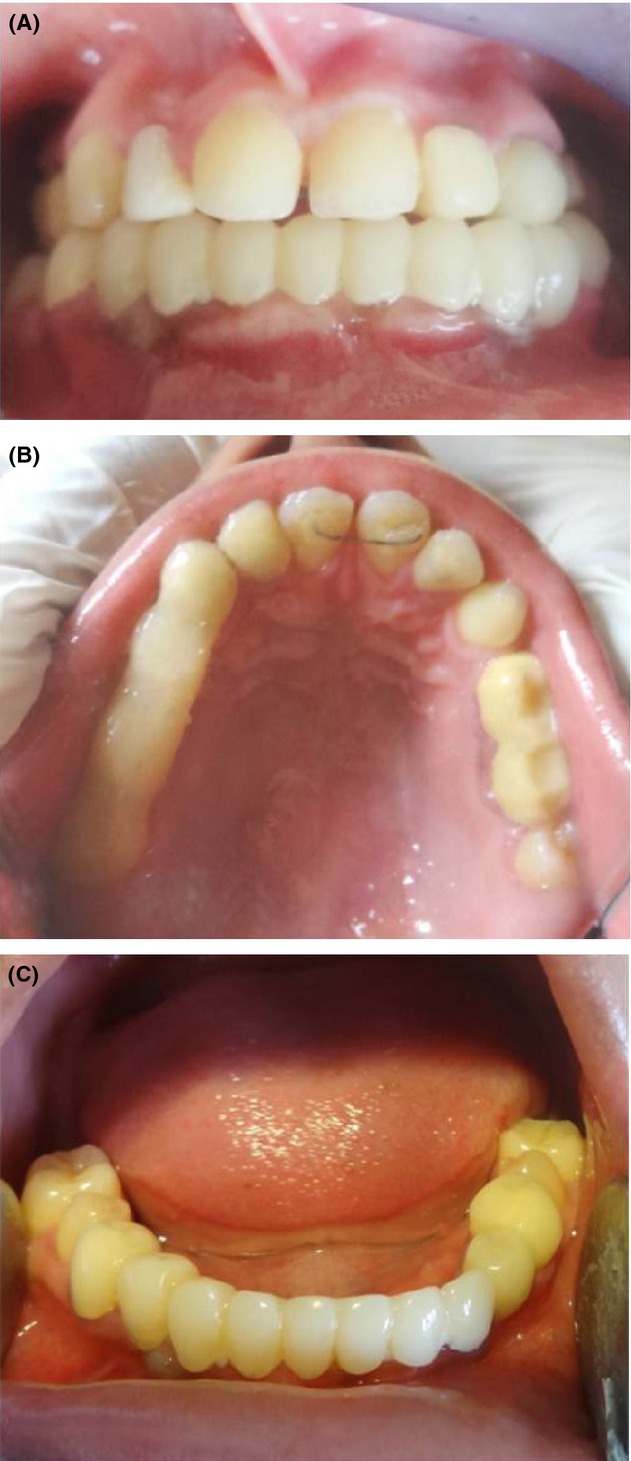
(A) - Occlussion after correction, (B) - Maxillary Arch, (C) - Mandibular Arch.
Discussion
This case report is of a patient who presented with hypodontia and retained deciduous teeth. Since she was not willing for extraction, maxillary deciduous teeth were retained in order to prevent alveolar bone resorption. Although implant restoration in patients with ectodermal dysplasia has become a more common practice, multiple issues must be considered. Among these are the position of the maxilla and the mandible relative to one another, the position of the remaining teeth in the arches, the volume of bone present, and age of the patient 19,20. Prosthodontic treatment was planned to increase the lost vertical dimension of face and to improve the esthetics. In this case, fixed orthodontics was implemented as an adjunctive treatment in order to establish ideal anterior dental relations 13,16. Later the treatment was completed with a fixed dental prosthesis, which significantly improved the patient's appearance, function and psychological well-being 21. This is a minimally invasive and cost-effective treatment modality.
Conclusion
Patients with ectodermal dysplasia present with multiple restorative issues. A multidisciplinary approach involving various clinical modalities is required to render a comprehensive dental care. Treatment decisions of dental team depend on patient's needs, wishes, and the willingness to undergo minor or major treatment and also on the economic possibilities. Different prosthetic options may be indicated and the patients need to be encouraged for an appropriate treatment. Deciding factors for endosseous implants are patient's systemic health, adequate bone volume, and socio-economic conditions. Prosthetic rehabilitation may include removable or fixed prosthesis which is a cost-effective treatment modality. Though implants are the ideal choice for partial anodontia, this case was treated in a conservative and minimally invasive method. Orthodontic treatment in combination with prosthetic rehabilitation of the patient will support the normal functions, esthetics, and psycho-social well-being. Eventually the patient was satisfied with the prosthesis as function was re-established and esthetics was not compromised. Long-term success depends on regular recall appointments and meticulous maintenance of oral and prosthetic hygiene.
Acknowledgments
We thank the patient for her cooperation and consent for publishing the photographs.
Conflict of Interest
None declared.
References
- Jain D, Jain S, Kumar A. Rahangdale T. Hypohidrotic ectodermal dysplasia: prosthetic and endodontic management. Int. J. Clin. Pediatr. Dent. 2010;3:63–67. doi: 10.5005/jp-journals-10005-1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yenisey M, Guler A. Unal U. Orthodontic and prosthodontic treatment of ectodermal dysplasia: a case report. Br. Dent. J. 2004;196:11–12. doi: 10.1038/sj.bdj.4811344. [DOI] [PubMed] [Google Scholar]
- Hekmatfar S, Jafari K, Meshki R. Badakhsh S. Dental management of ectodermal dysplasia: two clinical case reports. J. Dent. Res. Dent. Clin. Dent. Prospect. 2012;6:108–112. doi: 10.5681/joddd.2012.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holbrook KA. Structural abnormalities of the epidermally derived appendages in skin from patients with ectodermal dysplasia: insight into developmental errors. In: Salinas CF, Optiz JM, Paul NW, editors. Recent advances in ectodermal dysplasia. New York: Alan R. Liss; 1988. pp. 15–44. [PubMed] [Google Scholar]
- Singh G, Kumar A, Sharma V. Dhamej M. Ectodermal dysplasia: a case report. Indian J. Stomatol. 2012;3:187–189. [Google Scholar]
- Ngan V. Ectodermal dysplasia. Derm Net. New Zealand. Facts about the skin from New Zealand Trust. Available from: http://www.dermnetnz.org/hair-nails-sweat/ectodermal-dysplasia.html (accessed October 10, 2014)
- Everet FG, Jump EB, Sutherland WF, Savara BS. Suher T. Anhydrotic ectoddermal dysplasia with anodontia: a study of two families. J. Am. Dent. Assoc. 1952;44:173–186. doi: 10.1016/s0002-8177(52)42009-7. [DOI] [PubMed] [Google Scholar]
- Rajendran R. Diseases of the skin. In: Rajendran R, Sivapathasundaram B, editors. Shafer's text book of oral pathology. 6th ed. Lajput Nagar, New Delhi: Elesevier; 2009. pp. 797–798. [Google Scholar]
- Laurikkala J, Mikkola M, Mustonen T, Aberg T, Koppinen P, Pispa J, et al. TNF Signaling via the ligand receptor pair ectodysplasin and edar controls the function of epithelial signaling centre and is regulated by Wnt and Activin during tooth organogenesis. Dev. Biol. 2001;229:443–455. doi: 10.1006/dbio.2000.9955. [DOI] [PubMed] [Google Scholar]
- Bergendal B, Koch G, Kurol J. Wänndahl G. 1998. , and Consensus conference on ectodermal dysplasia with special reference to dental treatment. The Institute for Postgraduate Dental Education, Jönköping, Sweden.
- Suprabha BS. Hereditary ectodermal dysplasia: a case report. J. Indian Soc. Pedod. Prev. Dent. 2002;20:37–40. [PubMed] [Google Scholar]
- Pigno MA, Blackman RB, Cronin RJ., Jr Cavazos E. Prosthodontic management of ectodermal dysplasia: a review of the literature. J. Prosthet. Dent. 1996;76:541–545. doi: 10.1016/s0022-3913(96)90015-3. [DOI] [PubMed] [Google Scholar]
- Badavannar AN, Manvi SF. Belludi A. Multidisplinary approach to ectodermal dysplasia: a case report. Int. J. Contemp. Dent. 2011;2:74–76. [Google Scholar]
- Sickels JEV, Raybould YP. Hicks P. Interdisciplinary management of patients with ectodermal dysplasia. J. Oral Implantol. 2010;36:239–245. doi: 10.1563/AAID-JOI-D-09-00043R1. [DOI] [PubMed] [Google Scholar]
- Guckes AD, Brahims JS, McCarthy GR, Rudy SF. Cooper LT. Using endosseous dental implants for patients with ectodermal dysplasia. J. Am. Dent. Assoc. 1991;122:59–62. doi: 10.14219/jada.archive.1991.0307. [DOI] [PubMed] [Google Scholar]
- Loannidu–Marathiotou I, Kotsiomoiti E. Gioka C. The contribution of orthodontics to the prosthodontic treatment to ectodermal dysplasia: a long term clinical report. J. Am. Dent. Assoc. 2011;141:1340–1345. doi: 10.14219/jada.archive.2010.0078. [DOI] [PubMed] [Google Scholar]
- Wimdehy AM. Morris JC. An alternative treatment with the overlay removable partial denture: a clinical report. J. Prosthet. Dent. 1998;79:249–253. doi: 10.1016/s0022-3913(98)70232-x. [DOI] [PubMed] [Google Scholar]
- Pavarina AC, Machado AL, Vergani CE. Gampaolo ET. Overlay removable partial denture for a patient with ectodermal dysplasia: a clinical report. J. Prosthet. Dent. 2001;86:574–577. doi: 10.1067/mpr.2001.119981. [DOI] [PubMed] [Google Scholar]
- Tarjan I, Gabris K. Rozsa N. Early prosthetic treatment of patients with ectodermal dysplasia: a clinical report. J. Prosthet. Dent. 2005;93:419–424. doi: 10.1016/j.prosdent.2005.01.012. [DOI] [PubMed] [Google Scholar]
- Roshan Kumar P, Srivatsa G. Kashinath KR. Prosthodontic management of ectodermal dysplasia: a case report. Indian J. Compr. Dent. Care. 2011;1:86–88. [Google Scholar]
- Kirtley GE. Restoring esthetics and function in an edentulous patient with ectodermal dysplasia. Compend. Contin. Educ. Dent. 2011;32:82–84. , 86, 88. [PubMed] [Google Scholar]


