Abstract
The hip capsule has been identified as an important static stabilizer of the hip joint. Despite the intrinsic bony stability of the hip socket, the capsule plays a key role in hip stability, particularly at the extremes of motion, and the iliofemoral ligament is the most important stabilizer in extension and external rotation. Patients who do not undergo capsular closure or plication may continue to complain of hip pain and dysfunction postoperatively, likely because of microinstability or muscle invagination into the capsular defect, and high-resolution magnetic resonance imaging or magnetic resonance arthrography will identify the capsular defect. Seen primarily in the revision setting, capsular defects can cause recurrent stress at the chondrolabral junction. An attempt at secondary closure can be challenging because of capsular limb adherence to the surrounding soft tissues. Therefore reconstruction may be the only possible surgical solution for this problem. We describe our new surgical technique for arthroscopic hip capsular reconstruction using iliotibial band allograft.
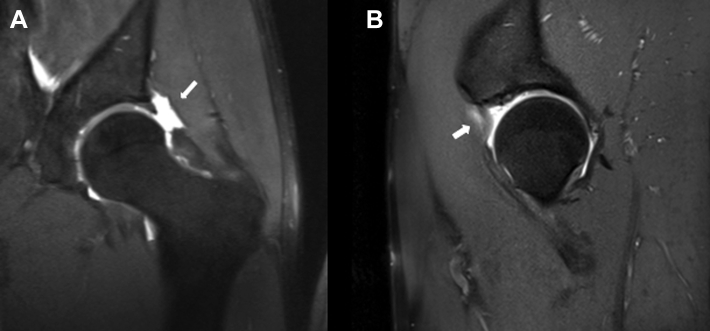
The hip capsule, consisting of the iliofemoral, ilioischial, and pubofemoral ligaments and zona orbicularis,1 has been identified as an important static stabilizer of the hip joint. During routine hip arthroscopy, management of the capsule at the conclusion of the procedure is evolving toward either capsular closure or capsular plication.2, 3 Patients who do not undergo capsular closure or plication may continue to complain of hip pain and dysfunction postoperatively, likely because of microinstability or muscle invagination into the capsular defect. High-resolution magnetic resonance imaging or magnetic resonance arthrography will identify the capsular defect, and a discussion with the patient regarding treatment options can take place (Fig 1).
Fig 1.
Magnetic resonance images showing (A) large capsular defect (arrow) on coronal view and (B) muscle herniation into capsular defect (arrow) on sagittal view.
Reconstruction of the hip capsule has been described for cases of instability after total hip arthroplasty with good results.4 There are currently no reports in the literature on capsular reconstruction in the native hip joint. We describe our new surgical technique for arthroscopic hip capsular reconstruction using iliotibial band allograft.
Surgical Technique
The key points of the technique are summarized in Table 1, and the technique is demonstrated in Video 1.
-
1.
The patient is positioned in the modified supine position (10° of flexion, 15° of internal rotation, 10° of lateral tilt, and neutral abduction).
-
2.
The procedure is conducted with the patient under spinal epidural anesthesia with propofol for complete muscular relaxation.
-
3.
Manual traction is applied through the operative hip, and light countertraction is applied to the contralateral extremity. The traction is carefully increased until the vacuum sign is present and a minimum of 1 cm of distraction is noted on fluoroscopy.
-
4.
The operative leg is adducted to neutral and the foot internally rotated so that the femoral neck is parallel to the ground.
-
5.
Two arthroscopic portals are used, anterolateral and midanterior, and a detailed inspection of the central and peripheral compartments is performed to evaluate for pathology including labral tears, chondral defects, ligamentum teres pathology, and bony impingement.
-
6.
After treatment of the pathology in the central and peripheral compartments, the capsular defect is sized and the traction is released. The graft is prepared on the back table.
-
7.
Iliotibial allograft is used because it provides a large piece of tissue to reconstruct sizeable capsular defects.
-
8.
On the back table, the allograft is folded 3 times onto itself to provide comparable thickness to the native hip capsule and is kept moist.
-
9.
One end of the graft is attached to the Graftmaster (Smith & Nephew, Andover, MA) for proper handling.
-
10.
The edges of the folded graft are sutured with No. 2-0 Vicryl (Ethicon, Somerville, NJ), making a quadrilateral shape. The No. 2-0 Vicryl runs in a figure-of-8 fashion so that the graft edges are completely surrounded.
-
11.
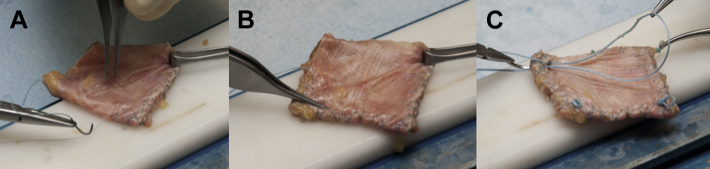
On each corner of the graft, loops are made using No. 2 Vicryl and tied over a straight mosquito clamp, with an “overhand loop” knot (Fig 2). The loops will help to facilitate intra-articular control of the graft and will be incorporated into the suture fixation.
-
12.
Distal loops are dyed in purple ink to help orientation. The graft is remeasured to confirm appropriate sizing.
-
13.
The graft is bathed in about 1 mL of platelet-rich plasma to enhance cellular healing.
-
14.
When graft preparation is complete, traction is re-established and 2 suture anchors (1 medial and 1 more lateral) are placed in the subspinal region of the acetabulum. These serve as the proximal points of fixation for the graft.
-
15.
The graft is transfixed with 1 of the suture limbs of the medial anchor and is advanced into the joint through a large cannula in the midanterior portal and then placed into position.
-
16.
After adequate positioning (Fig 3), the graft is fixed by a sliding knot and tied down to the subspinal anchor. The procedure is repeated to fix the lateral end of the graft, using the suture loop to aid in control (Fig 4).
-
17.
After adequate fixation of the graft, traction is released and the hip is brought into flexion and internal rotation.
-
18.
Side-to-side No. 2 absorbable sutures (Vicryl) are used to secure the allograft to the residual native capsule, beginning with the distal loops of the graft, with the aid of a suture-shuttling device (SutureLasso; Arthrex, Naples, FL). The number of sutures necessary depends on the size of the graft.
-
19.
The sutures are passed through the capsule limbs in a double-limb fashion and secured with racking half-hitch knots. A very small opening medially usually is left to allow for draining of any hematoma postoperatively.
-
20.
At the conclusion of the procedure, it is vital to gently take the hip through a range of motion to determine tension on the capsule and postoperative range-of-motion precautions. Table 2 shows pearls and pitfalls for this technique.
Table 1.
Key Points
| The hip capsule is an important static stabilizer of the hip. |
| At the conclusion of primary hip arthroscopy, the capsule should be closed or undergo plication. |
| Microinstability and its clinical repercussions can occur when closure of the capsule is not performed. |
| High-resolution MRI/MRA usually detects the capsular defect. |
| Successful reconstruction can be achieved in cases of instability after THA. |
| Capsular reconstruction is performed with an IT band allograft. |
IT, iliotibial; MRA, magnetic resonance arthrography; MRI, magnetic resonance imaging; THA, total hip arthroplasty.
Fig 2.
(A) The edges of the folded graft are sutured with No. 2-0 absorbable, braided suture, making a quadrilateral shape. (B) The No. 2-0 suture runs in a figure-of-8 fashion to make a complete surrounding of the graft edges. (C) On each corner of the graft, loops are made using a No. 2 absorbable, braided suture.
Fig 3.
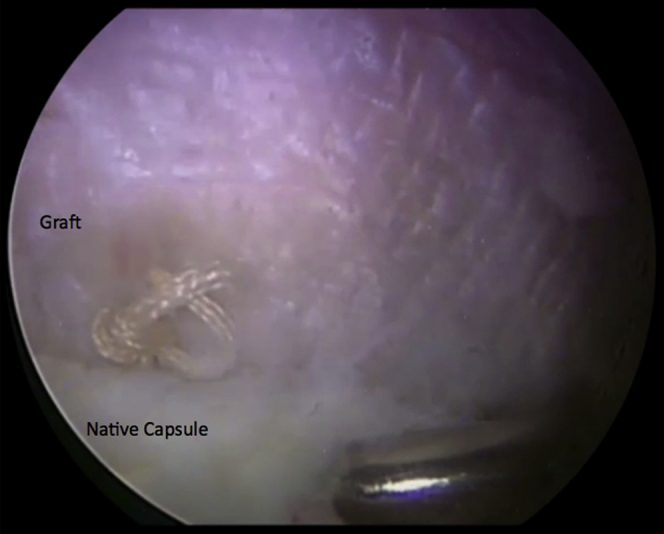
Left hip capsule as seen from midanterior portal, with patient in modified supine position. After insertion into the joint, the graft must be adequately placed in position.
Fig 4.
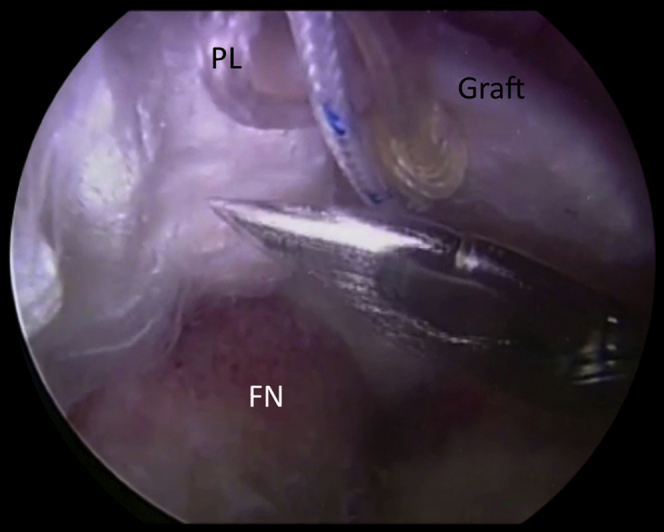
Left hip (subspinal region) seen from midanterior portal, with patient in modified supine position. The suture loops on each corner of the graft help achieve control inside the joint and adequate fixation to the subspinal region and native capsule. (FN, femoral neck; PL, proximal loop).
Table 2.
Pearls and Pitfalls to Consider During Hip Capsular Reconstruction
| Pearls |
| Use iliotibial allografts. |
| Fold the graft 3 times onto itself to provide comparable thickness to the native hip capsule. |
| Make suture loops on each corner of the folded graft. |
| Dye the distal loops with purple ink to help orientation. |
| Pitfalls |
| Introducing the graft into the joint before placing the proximal anchors in the subspinal region |
| Inadequate measurement of the capsular defect |
Discussion
Management of the hip capsule at the completion of hip arthroscopy is growing in interest in the sports medicine literature. Despite the intrinsic bony stability of the hip socket, the capsule plays a key role in hip stability, particularly at the extremes of motion.5, 6 Although the iliofemoral, ischiofemoral, and pubofemoral ligaments all play key roles in hip stability, the iliofemoral ligament is the most important stabilizer in extension and external rotation.7 Between the 12- and 3-o'clock positions on the acetabular clock-face anatomy, there is an increase in capsular thickness, with the 2-o'clock position being the thickest.7 This is the region where the capsulotomy is generally performed to access the joint during an arthroscopic hip procedure. Not addressing the capsular defect resulting from the capsulotomy, particularly in its thickest region, can result in persistent, symptomatic microinstability in the operative hip in certain cases. A surgeon may perform an extensive capsulotomy to facilitate improved access during hip arthroscopy, and we recommend capsular closure or plication at the completion of the case to restore native anatomy. Although cases of subluxation and dislocation after hip arthroscopy are rare, they are often a topic of discussion at hip arthroscopy conferences, which leads to the conclusion that these complications are under-reported.8
Besides the history of arthroscopy, patients with large defects in the capsule may have signs of instability including anterior hip pain or a sensation of giving way or catching and may present with a positive dial test. The diagnosis can be confirmed with high-resolution magnetic resonance imaging or magnetic resonance arthrography.9 Patients may also complain of an anterior “pinching” sensation, which may be due to muscle invagination into the defect.
Cases of recurrent dislocation after revision total hip arthroplasty have been described in the literature and have been managed successfully with reconstruction of the iliofemoral ligament.4 Likewise, this technique of arthroscopic capsular reconstruction has the advantage of providing a surgical solution to a challenging postoperative complication. Seen primarily in the revision setting, capsular defects can lead to microinstability and cause recurrent stress at the chondrolabral junction. An attempt at secondary closure can be challenging because of capsular limb adherence to the surrounding soft tissues. Therefore reconstruction may be the only possible surgical solution for this problem. This technique brings a very low risk of disease transmission from allograft use. The fact that not all centers have access to allografts can be considered a limitation of this technique; moreover, the procedure can be technically challenging. This arthroscopic technique is still developing, and the best clinical results are expected in the medium- and long-term, mainly in elite athletes with hip disorders.
Acknowledgment
The authors thank Barry Eckhaus and Angelica Wedell for their outstanding production of the surgical technique video. They also thank Penny S. Bortz for her help in the step-by-step preparation of the graft.
Footnotes
The authors report the following potential conflict of interest or source of funding: Steadman Philippon Research Institute receives corporate sponsorships from the following companies: Smith & Nephew, Arthrex, Siemens, ConMed, Linvatec, Össur, Synthes, and Ceterix Orthopaedics. C.A.C.T., G.A.S., K.F., K.K.B., and M.J.P. received institutional research support from Smith & Nephew, Arthrex, Siemens, Ossur. M.J.P. receives support from Smith & Nephew, MIS, Arthrosurface, DonJoy, Slack, Linvatec, HIPCO.
Supplementary Data
Surgical technique for arthroscopic capsule reconstruction in hip using iliotibial band allograft. A left-sided hip revision arthroscopy is shown, with the patient positioned in the modified supine position, and 2 arthroscopic portals are used: anterolateral and midanterior.
References
- 1.Telleria J.J., Lindsey D.P., Giori N.J., Safran M.R. A quantitative assessment of the insertional footprints of the hip joint capsular ligaments and their spanning fibers for reconstruction. Clin Anat. 2014;27:489–497. doi: 10.1002/ca.22272. [DOI] [PubMed] [Google Scholar]
- 2.Harris J.D., Slikker W., III, Gupta A.K., McCormick F.M., Nho S.J. Routine complete capsular closure during hip arthroscopy. Arthrosc Tech. 2013;2:e89–e94. doi: 10.1016/j.eats.2012.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Domb B.G., Philippon M.J., Giordano B.D. Arthroscopic capsulotomy, capsular repair, and capsular plication of the hip: Relation to atraumatic instability. Arthroscopy. 2013;29:162–173. doi: 10.1016/j.arthro.2012.04.057. [DOI] [PubMed] [Google Scholar]
- 4.Fujishiro T., Nishikawa T., Takikawa S., Saegusa Y., Yoshiya S., Kurosaka M. Reconstruction of the iliofemoral ligament with an artificial ligament for recurrent anterior dislocation of total hip arthroplasty. J Arthroplasty. 2003;18:524–527. doi: 10.1016/s0883-5403(03)00073-1. [DOI] [PubMed] [Google Scholar]
- 5.Martin H.D., Savage A., Braly B.A., Palmer I.J., Beall D.P., Kelly B. The function of the hip capsular ligaments: A quantitative report. Arthroscopy. 2008;24:188–195. doi: 10.1016/j.arthro.2007.08.024. [DOI] [PubMed] [Google Scholar]
- 6.Boykin R.E., Anz A.W., Bushnell B.D., Kocher M.S., Stubbs A.J., Philippon M.J. Hip instability. J Am Acad Orthop Surg. 2011;19:340–349. doi: 10.5435/00124635-201106000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Philippon MJ, Michalski MP, Campbell KJ, et al. A quantitative analysis of hip capsular thickness. Knee Surg Sports Traumatol Arthrosc in press, available online 10 May, 2014. doi:10.1007/s00167-014-3030-5. [DOI] [PubMed]
- 8.Harris J.D., McCormick F.M., Abrams G.D. Complications and reoperations during and after hip arthroscopy: A systematic review of 92 studies and more than 6,000 patients. Arthroscopy. 2013;29:589–595. doi: 10.1016/j.arthro.2012.11.003. [DOI] [PubMed] [Google Scholar]
- 9.McCormick F., Slikker W., III, Harris J.D. Evidence of capsular defect following hip arthroscopy. Knee Surg Sports Traumatol Arthrosc. 2014;22:902–905. doi: 10.1007/s00167-013-2591-z. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Surgical technique for arthroscopic capsule reconstruction in hip using iliotibial band allograft. A left-sided hip revision arthroscopy is shown, with the patient positioned in the modified supine position, and 2 arthroscopic portals are used: anterolateral and midanterior.