Abstract
The medial patellofemoral ligament (MPFL) ensures stability of the patella against lateral forces. In cases of recurrent lateral patellar luxation, surgical reconstruction of the MPFL has an important role in treating lateral patellar instability. Several biomechanical studies have presented valuable pieces of information about various techniques for re-creating this medial patellofemoral complex mainly using the gracilis tendon as an autograft. However, with the increasing number of MPFL reconstructions, there are also an increasing number of patients requiring revision MPFL reconstruction. Therefore alternative graft options may become more relevant. Furthermore, the gracilis tendon as a tubular graft may not be able to fully restore patellofemoral kinematics compared with the native MPFL. This article introduces a surgical technique using the fascia lata as an alternative graft option for the anatomic reconstruction of the MPFL.
The medial patellofemoral ligament (MPFL) is known as the main stabilizer against lateral displacement of the patella in near extension.1, 2, 3, 4 Luxation of the patella mainly results in a disruption of the MPFL, which has been found to alter patellar kinematics and contact pressure.5, 6 Therefore reconstruction of the MPFL has become a more popular surgical intervention worldwide,7 leading to good clinical short-term as well as midterm outcomes with low dislocation rates and excellent functional results.8, 9, 10, 11
However, because the surgical technique is not trivial, complication rates of up to 26% have been described in the literature.12 Therefore there is also an increased need for alternative grafts for revision surgery. Moreover, the gracilis tendon's shape is tubular and is thus not comparable with the natural MPFL's appearance, which is more sheetlike. Furthermore, most commonly used grafts are stronger and stiffer than the native MPFL.13 This condition may not reproduce kinematics comparable with the native MPFL. Moreover, malpositioning and over-tensioning of the graft may result in increased retropatellar contact pressure, as well as an increased medial tilt of the patella, leading to subsequent degeneration of the patellofemoral joint.13, 14, 15 This article introduces a surgical technique using the fascia lata as an alternative autograft or allograft for anatomic reconstruction of the MPFL.
Surgical Technique
Before the fascia lata graft is harvested, an arthroscopy of the knee is performed to evaluate the quality of the patellofemoral cartilage, dynamic lateralization, and patellar tilt. Moreover, a diagnostic arthroscopy is performed to rule out other pathologies.16
To expose a part of the tractus iliotibialis, a 6-cm-long incision is performed at the lateral thigh approximately 4 fingerbreadths above the upper border of the patella (Fig 1, Video 1). After blunt preparation onto the fascia lata, which presents as gleaming and tense, an area of 10 mm in width and 12 cm in length is marked. This marked part of the fascia is detached using a sharp scalpel and a blunt clip. To prevent any perforation or tearing of the desired part of the fascia lata, the clip fixates and maintains tension on the fascia lata while the release from the muscle is performed using the scalpel. To be able to reach the full length of the transplant with an exact incision, a Langenbeck clip is used to retain as well as to move the skin to the proximal and distal end of the cut (Fig 2). After the fascia lata graft has been released from the muscle, the remaining gap is closed without tension with No. 4-0 resorbable suture wire (Fig 3).
Fig 1.
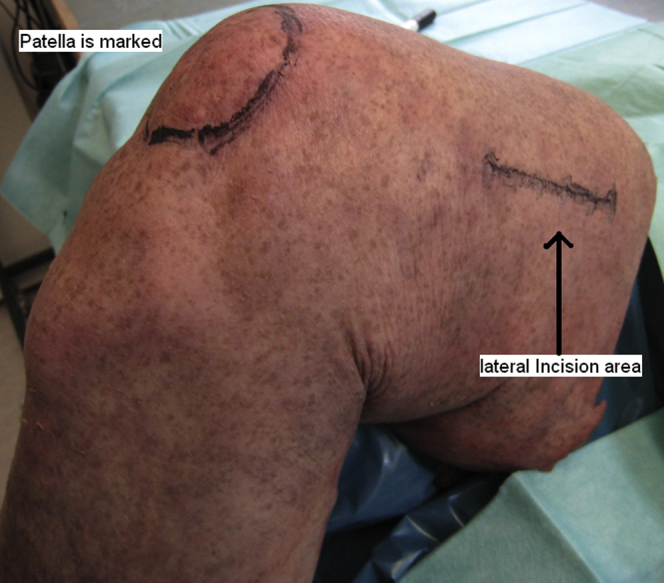
View of cadaveric specimen from lateral side. The patella is marked with a circle. The lateral incision for harvesting of the fascia lata autograft is marked approximately 4 fingerbreadths above the patella.
Fig 2.

View from lateral side. The proximal (femoral) side is on the right, and the distal (tibial) side is on the left. The subcutaneous tissue is opened. The fascia lata is exposed and presents as gleaming and tense. An area of 10 mm in width and 12 cm in length is identified and marked with a felt pen. Two Langenbeck clips retain and move the skin in the desired direction.
Fig 3.

View from lateral side. The proximal (femoral) side is on the right, and the distal (tibial) side is on the left. After harvesting, the remaining tractus iliotibialis is closed using a thin, absorbable, continuous suture. The subcutaneous tissue is also closed with thin, absorbable sutures in the next step.
The harvested autograft is cleared of fat and muscle tissue at full length using a blunt scissor, scratching carefully over its surface to avoid perforating it (Fig 4). Next, the fascia lata is split into 2 pieces with a scalpel, resulting in 2 identical grafts with a dimension of 5 mm in width and 12 cm in length (Fig 5). Each of the grafts is attached on each pole using a nonabsorbable suture (No. 2 FiberWire; Arthrex, Naples, FL) with a whipstitch technique. The attachment area on each pole should not exceed the length of 1 cm to prevent thickening and shortening of the useful part of the graft.
Fig 4.

Harvested fascia lata autograft with a length of 12 cm and width of 10 mm. This graft is cleared of muscle and fat using a blunt scissor.
Fig 5.

The autograft is divided into 2 separate grafts that are sutured at each end using a whipstitch technique, creating 2 grafts of 5 mm in width and 12 cm in length. Each end should not appear too bulky because of possible non-fitting inside the created tunnels. If bulkiness is present, cutting with a preparation scissor is recommended without weakening the suture's fixation.
To prepare the patellar insertion point of the MPFL, a 2-cm incision is performed along the medial margin of the patella.17 Next, the tissue above the patellar bone is removed with a Luer forceps. To create 2 holes inside the proximal two-thirds of the patella for the fixation of the graft, 2 guidewires are drilled tangential and parallel to each other at the patellar medial margin, with care taken not to fracture the patellar bone or perforate the chondral joint surface. Therefore an image amplifier should be used to verify the exact positioning on lateral and anteroposterior views. With a channeled 4-mm drill and the assistance of the guidewires, two 25-mm-deep caves are then created (Fig 6). To fasten the end of the first graft inside the proximal tunnel, a 4.75-mm Bio-SwiveLock anchor (Arthrex) is used. The sutures that are attached to the graft's pole are carried through the lug at the tip of the anchor first and strongly fastened at the screwdriver. The assistant then stabilizes the patella manually while the surgeon is inserting the anchor with regulated force inside the tunnel. It is important to keep tension on the fixated sutures so that the graft can submerge deep enough inside the tunnel. Accordingly, 1 end of the second fascia lata graft is attached inside the distal hole. The anchor screws have to disappear completely to prevent irritation of the soft parts at the medial margin, as well as to ensure the graft's proper fixation. This technique is comparable with the surgical technique described by Schöttle et al.18
Fig 6.

View from medial side. The proximal (femoral) side is on the right, and the distal (tibial) side is on the left. The skin incision is enlarged for demonstration purposes. The joint capsule remains untouched and intact. After the patellar bone has been cleared of tissue with a Luer forceps, the 2 tunnels inside the upper two-thirds of the patellar medial margin are created, parallel to each other.
Next, a tunnel is created between the second and third layers of the native MPFL's position to transfer the free ends of both grafts to the femoral attachment of the MPFL19 (Fig 7). The medial epicondyle is palpated in 30° of knee flexion, and a 2-cm skin incision is performed at this point next to the adductor tubercle. After blunt preparation of the tunnel with care taken to protect the joint capsule, the tip of an arcuate Kocher forceps is moved from the patellar insertion side to the medial epicondyle exit. A loop from a shuttle wire is fixed at the forceps and carried to the patellar exit. With this shuttle wire, the free ends of both grafts can now be transferred through the tunnel next to the medial epicondyle while trying to prevent rotation or contortion of both grafts (Fig 8).
Fig 7.

View from medial side. The proximal (femoral) side is on the left, and the distal (tibial) side is on the right. The grafts are fixed at the medial patella with 2 press-fit anchors (4.75-mm SwiveLock). The remaining FiberWire sutures at the patella can be cut with a scalpel. The free ends of each graft are shuttled to the femoral incision side through the second and third layers of the original medial patellofemoral ligament (MPFL) in the next step.
Fig 8.

View from medial side. Proximal (femoral) side is on the left and the distal (tibial) side with the tuberositas tibiae (Tub. tib.) is on the left. The grafts are shuttled between the second and third layers of the original medial patellofemoral ligament (MPFL) to the femoral attachment point. Final femoral fixation follows using a bioabsorbable interference screw.
Next, the anatomic femoral insertion point of the MPFL has to be identified under fluoroscopic control with the use of a radiographic image amplifier on a straight lateral view. According to Schöttle et al.,20 the radiographic landmark is identified slightly anterior to an elongation of the posterior femoral cortex between the proximal origin of the medial condyle and the most posterior point of the Blumensaat line (Fig 9). At this MPFL femoral insertion point, a guidewire with a lug at its end is drilled into the femoral bone until it exits on the lateral side approximately in range of the lateral epicondyle. After verification of the correct tunnel position under fluoroscopic control, the femoral tunnel is created, using a cannulated drill that is 1 mm larger than the diameter of the ends of both grafts, until it reaches the lateral corticalis. When one is removing the cannulated drill, the guidewire should be fixed manually so that it does not exit the tunnel; otherwise, it may be very difficult to replace it. Then, the sutured ends of both grafts are guided into the tunnel with a shuttle wire using the eyelet of the guidewire, which is pulled through the tunnel to exit on the lateral femoral side. During this process, both of the graft's ends are forced into the drill hole, with special attention taken not to twist the grafts.
Fig 9.

Radiographic image of straight lateral view. The femoral insertion point is determined under fluoroscopic control. The elongation of the femoral posterior cortex and the most posterior point of the Blumensaat line are marked in red. (MPFL, medial patellofemoral ligament.)
Finally, the grafts are fixed inside the femur at 30° of knee flexion with adequate tension by pulling the sutures from the lateral side.21 The sutures are temporarily fixed laterally with a Kocher clamp to control adequate tension of the grafts as well as patellar movement in the trochlea manually during passive knee flexion and extension while lateral forces against the patella are performed. Here, it is possible to strain each graft on its own without affecting the other graft. Special care is taken not to over-tension the graft. After the correct tension and position of the grafts have been examined, a 6-mm bioabsorbable interference screw (Arthrex) ensures secure fixation inside the femoral bone, followed by a final check to prevent overcorrection or over-tensioning.14 The grafts should not be contorted, and free motility has to be guaranteed. After all of the necessary steps have been completed, the wounds are closed with thin, nonresorbable sutures.
The postoperative phase includes fixation of the knee with a brace allowing for passive mobilization of the knee up to 90° of flexion. Furthermore, active quadriceps muscle training in full extension is performed with a physiotherapist. For the first 6 postoperative weeks, partial weight bearing is recommended with 15 kg. After 6 weeks, full range of motion is allowed with no restriction, as well as a pain-dependent increase in load.
Discussion
Rupture of the MPFL was discovered as the main pathoanatomic condition after a lateral patellar dislocation.22, 23, 24, 25, 26 To restore this main passive stabilizing structure of the patella, it is common to use other biological structures to replace the natural MPFL's function. Thus re-creation of the MPFL has been researched for many years, and many different techniques using autografts have been published. According to Schöttle et al.,18 the indications for MPFL reconstruction are recurrent patellar dislocations or subluxations, as well as a single dislocation with a persistent positive apprehension test. The important point of our article was to introduce reconstruction of the MPFL with a part of the fascia lata as an alternative graft to the gracilis tendon. The reason behind this was to find an anatomic structure whose shape and biomechanical kinematics are very similar to the original tissue and that has a ubiquitous disposability in patients (Table 1).
Table 1.
Overview of Presented Technique
| Indications |
| Recurrent lateral patellar luxation/subluxation |
| Primary patellar dislocation with persistent positive apprehension test |
| Revision surgery in patients with previous autologous anterior cruciate ligament replacement with gracilis or semitendinosus graft |
| Contraindications |
| Severe rotational malalignment |
| Severe trochlear dysplasia, type B-D according to Dejour classification |
| Advantages |
| Possibility of anatomic reconstruction of MPFL |
| Minimally invasive technique |
| Easy harvest and preparation of autograft |
| Ubiquitous disposability of fascia lata graft |
| No weakening of other structures required |
| Preservation of tendon grafts (gracilis and semitendinosus) |
| Possibility of reconstructing MPFL in revision cases (in case there are no tendons left as autografts) |
| Pitfalls and risks |
| Problem 1: There is a risk of traumatic patellar fracture or cartilage damage during the creation of both tunnels inside the medial upper two-thirds of the patella. |
| Solution 1: Using an image intensifier intraoperatively with anteroposterior and straight lateral views during the drilling of the guidewire should minimize the risk of perforating the cartilage. Furthermore, it is possible to manually check the exit of the guidewire on the lateral patellar margin. The second guidewire should be placed parallel to the first guidewire. Finally, the tunnels created with the 4-mm drill should not exit at the lateral patellar margin to prevent weakening of the bone. |
| Problem 2: Over-tensioning of the grafts may lead to cartilage damage and pain, followed by premature arthrosis of the knee. |
| Solution 2: Intraoperative manual checking of the graft's tension during multiple passive extension and flexion movements combined with fluoroscopic control and a tangential radiographic image of the patella should point out if the strain is too high. If so, easy removal and reimplantation of the femoral bioabsorbable screw always allow re-evaluation of the tension. |
| Key point |
| It is very important to find the correct femoral insertion point of the MPFL described in the article to ensure proper fixation and tension of the reconstructed MPFL and, consequently, the desired function. |
| Tips |
| Using an image intensifier with a straight lateral view is vital for finding the femoral insertion area of the native MPFL. |
| After reconstruction, using fluoroscopic control allows one to intraoperatively evaluate the kinematics of the patella during extension and flexion, as well as its position in relation to the femoral trochlea. |
| The graft is implanted at 30° of knee flexion, where the MPFL provides the main stabilizing function of the patella. Here, it is possible to check the tension of the graft manually. If one is applying lateral forces on the patella, it should not overreach the lateral femoral condyle. |
| Postoperative treatment |
| Fore the first 6 postoperative weeks, passive mobilization up to 90° of flexion combined with partial weight bearing with 15 kg, as well as active quadriceps muscle training in full extension, is recommended. |
| After 6 weeks, full range of motion, as well as a pain-dependent increase in load, is allowed. |
MPFL, medial patellofemoral ligament.
The native MPFL is a sheetlike ligament whose length ranges from 4.5 to 6.5 cm and whose width ranges from 1.0 to 3.2 cm.5, 17, 27, 28, 29 Furthermore, the MPFL's origin on the medial patellar side is considered wider than the femoral insertion area above the epicondylus medialis.17, 21, 27 These size requirements can be easily met by exactly cutting the requested quadratic shape of the 2 bundles from the tractus iliotibialis.
The presented 2-bundle technique is performed to imitate the natural MPFL's shape and kinematics as much as possible to improve the restoration of patellofemoral kinematics during knee flexion without risking a dislocation. It has also been shown that patellar rotation and stability increase when using this technique in comparison with a single-bundle technique.8, 9, 21, 30, 31 In addition, both of the free grafts can be situated at the original position of the MPFL between the second and third medial layers. The so-created triangle with the use of the thin fascia lata is matchable to the native MPFL's anatomy.1 Fluoroscopy is mandatory during reconstruction to achieve anatomically correct positioning of the graft's insertion.18
Another advantage of the fascia lata in contrast to the most frequently used grafts for MPFL reconstruction, that is, the gracilis, quadriceps, or semitendinosus tendon, lies in the comparable shape and biomechanical similarity to the native MPFL.32, 33, 34 The gracilis or semitendinosus tendon's shape can be considered tubular and longer than needed, whereas the fascia lata presents the shape of an aponeurosis.35, 36 A biomechanical study has recently shown that cordlike grafts cannot completely replace the MPFL's natural functional behavior. As a result, the different patellar kinematics can lead to increased patellofemoral pressure, which can be followed by pain and subsequent patellofemoral osteoarthritis. Another explanation for these complications is the higher stiffness and varying diameter of the semitendinosus or gracilis tendons compared with the fascia lata.14, 37, 38 Nevertheless, if one is using the presented technique, care must also be taken to ensure the correct tension of the grafts after their fixation with the interference screw. The reason lies in the possibility of an accidental over-tensioning of the graft during the insertion of the implant. Over-tensioning at this point could also lead to painful motion and the aforementioned complications. Furthermore, an overcorrection has to be excluded to prevent medial patellar subluxation, which could lead to complete graft failure as well as cartilage damage on the medial patellar facet.14 Therefore intraoperative evaluation of the patellar movement during extension and flexion is mandatory to eliminate possible complications.
As mentioned earlier, the ubiquitous disposability and easy method of harvesting the fascia lata should not be underestimated. Some studies have presented other possible grafts whose shape can be compared with the original MPFL. For example, a strip of the medial retinaculum or a slip of the superficial quadriceps tendon would imitate the native MPFL, but the advantage of also using such sheetlike grafts was clouded by removing them from their origin and negating their natural function in stabilizing patellar tracking.39, 40 In contrast to these structures, the fascia lata as an autograft can be removed without weakening the restraining forces against lateral patellar dislocation.41 In addition, the gracilis and semitendinosus tendons may be preserved in athletes who are at risk of requiring other ligament replacements in the future or whose anterior cruciate ligament also has to be reconstructed. Moreover, in patients with the need for revision surgery or recurrent patellar instability, the fascia lata is still a viable alternative because of its availability in almost every patient. These facts should be pondered when choosing the method for reconstruction of the MPFL with an autograft.
The described surgical technique with a sheet of the fascia lata offers an alternative autograft for anatomic MPFL reconstruction without weakening other structures and allows early functional rehabilitation. Furthermore, it is possible to preserve tendons such as the semitendinosus or gracilis for the contingency of traumatic rupture of the anterior cruciate ligament or reconstruction of the MPFL in patients who require revision MPFL reconstruction because of failed previous procedures. Therefore the presented minimally invasive technique with the possibility of harvesting the fascia lata in almost every patient offers a viable alternative for anatomic reconstruction of the MPFL.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
(1) Required equipment for medial patellofemoral ligament (MPFL) reconstruction (also described in the text). (2) Marking of the incision area followed by a lateral 6-cm incision approximately 4 fingerbreadths above the patella. (3) Blunt preparation onto the fascia lata. (4) Detachment of the fascia lata part at the desired area of 10 mm in width and 12 cm in length. (5) Closure of the gap without tension with a resorbable suture wire. (6) Preparation of the graft (clearing of fat and muscle tissue, cutting into 2 pieces of 5 mm in width and 12 cm in length, and attaching the grafts on each pole with No. 2 FiberWire). (7) Creation of a 2-cm incision at the medial margin of the patella, with removal of the soft tissue until the patellar bone is clearly visible. (8) Placement of the 2 guidewires at the proximal two-thirds of the medial patellar margin, parallel to each other (the correct position can be verified under fluoroscopic control on a straight lateral view). (9) Creation of two 25-mm-deep caves inside the patella using a 4-mm drill. (10) Fixation of the first graft using a 4.75-mm Bio-SwiveLock anchor, with implantation of the screw until it is completely embedded inside the tunnel. (11) Fixation of the second graft inside the distal tunnel according to the first graft. (12) Finding the femoral insertion point of the MPFL using fluoroscopic control on a straight lateral view, and performing a small skin incision. (13) Creation of a tunnel between the second and third layers of the original MPFL from the patella to the femoral incision point. (14) Transfer of both grafts through the tunnel to the exit at the femoral point using a shuttle wire. (15) Drilling of a guidewire from the medial insertion point until it exits on the lateral side. (16) Creation of the femoral tunnel using a drill that is 1 mm larger than the diameter of both ends of the grafts. (17) Placement of the grafts inside the tunnel using a shuttle wire, and pulling of the guidewire from the lateral side. (18) Careful assessment to ensure that the grafts are not contorted or twisted. (19) Application of the correct tension of each graft on its own by pulling at the shuttle wires and then fixing the wires with a clip and evaluating the patellar movement during manual flexion and extension of the knee. (20) Placement of a bioabsorbable screw, followed by a final check of the patellofemoral kinematics. (21) Skin closure.
References
- 1.Schmeling A. Aktuelle Aspekte der patellofemoralen Instabilität. SFA Arthroskopie Aktuell. 2010;23:1–27. [Google Scholar]
- 2.Andrish J. The biomechanics of patellofemoral stability. J Knee Surg. 2004;17:35–39. doi: 10.1055/s-0030-1247147. [DOI] [PubMed] [Google Scholar]
- 3.Warren L.F., Marshall J.L. The supporting structures and layers on the medial side of the knee: An anatomical analysis. J Bone Joint Surg Am. 1979;61:56–62. [PubMed] [Google Scholar]
- 4.Panagiotopoulos E., Strzelczyk P., Herrmann M. Cadaveric study on static medial patellar stabilizers: The dynamizing role of the vastus medialis obliquus on medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2006;14:7–12. doi: 10.1007/s00167-005-0631-z. [DOI] [PubMed] [Google Scholar]
- 5.Philippot R., Chouteau J., Wegrzyn J. Medial patellofemoral ligament anatomy: Implications for its surgical reconstruction. Knee Surg Sports Traumatol Arthrosc. 2009;17:475–479. doi: 10.1007/s00167-009-0722-3. [DOI] [PubMed] [Google Scholar]
- 6.Steiner T.M., Torga-Spak R., Teitge R.A. Medial patellofemoral ligament reconstruction in patients with lateral patellar instability and trochlear dysplasia. Am J Sports Med. 2006;34:1254–1261. doi: 10.1177/0363546505285584. [DOI] [PubMed] [Google Scholar]
- 7.Stephen J.M., Kaider D., Lumpaopong P. The effect of femoral tunnel position and graft tension on patellar contact mechanics and kinematics after medial patellofemoral ligament reconstruction. Am J Sports Med. 2014;42:364–372. doi: 10.1177/0363546513509230. [DOI] [PubMed] [Google Scholar]
- 8.Drez D., Edwards T.B., Williams C.S. Results of medial patellofemoral ligament reconstruction in the treatment of patellar dislocation. Arthroscopy. 2001;17:298–306. doi: 10.1053/jars.2001.21490. [DOI] [PubMed] [Google Scholar]
- 9.Ellera Gomes J.L., Stigler Marczyk L.R., César de César Medial patellofemoral ligament reconstruction with semitendinosus autograft for chronic patellar instability: A follow-up study. Arthroscopy. 2004;20:147–151. doi: 10.1016/j.arthro.2003.11.006. [DOI] [PubMed] [Google Scholar]
- 10.Nomura E., Inoue M., Kobayashi S. Long-term follow-up and knee osteoarthritis change after medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2007;35:1851–1858. doi: 10.1177/0363546507306161. [DOI] [PubMed] [Google Scholar]
- 11.Schöttle P.B., Fucentese S.F., Romero J. Clinical and radiological outcome of MPFL reconstruction with a semitendinosus autograft for patellar instability. Knee Surg Sports Traumatol Arthrosc. 2005;13:516–521. doi: 10.1007/s00167-005-0659-0. [DOI] [PubMed] [Google Scholar]
- 12.Shah J.N., Howard J.S., Flanigan D.C. A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2012;40:1916–1923. doi: 10.1177/0363546512442330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beck P., Brown N.A., Greis P.E. Patellofemoral contact pressures and lateral patellar translation after medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35:1557–1563. doi: 10.1177/0363546507300872. [DOI] [PubMed] [Google Scholar]
- 14.Elias J.J., Cosgarea A.J. Technical errors during medial patellofemoral ligament reconstruction could overload medial patellofemoral cartilage: A computational analysis. Am J Sports Med. 2006;34:1478–1485. doi: 10.1177/0363546506287486. [DOI] [PubMed] [Google Scholar]
- 15.Smith T.O., Song F., Donell S.T. Operative versus non-operative management of patellar dislocation. A meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2011;19:988–998. doi: 10.1007/s00167-010-1355-2. [DOI] [PubMed] [Google Scholar]
- 16.Schöttle P.B., Scheffler S.U., Schwarck A. Arthroscopic medial retinacular repair after patellar dislocation with and without underlying trochlear dysplasia: A preliminary report. Arthroscopy. 2006;22:1192–1198. doi: 10.1016/j.arthro.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 17.Steensen R.N., Dopirak R.M., McDonald W.G., III The anatomy and isometry of the medial patellofemoral ligament: Implications for reconstruction. Am J Sports Med. 2004;32:1509–1513. doi: 10.1177/0363546503261505. [DOI] [PubMed] [Google Scholar]
- 18.Schöttle P.B., Romero J., Schmeling A. Technical note: Anatomical reconstruction of the medial patellofemoral ligament using a free gracilis autograft. Arch Orthop Trauma Surg. 2008;128:479–484. doi: 10.1007/s00402-007-0300-4. [DOI] [PubMed] [Google Scholar]
- 19.Warren L.A., Marshall J.L., Girgis F. The prime static stabilizer of the medial side of the knee. J Bone Joint Surg Am. 1974;56:665–674. [PubMed] [Google Scholar]
- 20.Schöttle P.B., Schmeling A., Rosenstiel N. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35:801–804. doi: 10.1177/0363546506296415. [DOI] [PubMed] [Google Scholar]
- 21.Amis A.A., Firer P., Mountney J. Anatomy and biomechanics of the medial patellofemoral ligament. Knee. 2003;10:215–220. doi: 10.1016/s0968-0160(03)00006-1. [DOI] [PubMed] [Google Scholar]
- 22.Elias D.A., White L.M., Fithian D.C. Acute lateral patellar dislocation at MR imaging: Injury patterns of medial patellar soft tissue restraints and osteochondral injuries of the inferomedial patella. Radiology. 2002;225:736–743. doi: 10.1148/radiol.2253011578. [DOI] [PubMed] [Google Scholar]
- 23.Sallay P.I., Poggi J., Speer K.P. Acute dislocation of the patella. A correlative pathoanatomic study. Am J Sports Med. 1996;24:52–60. doi: 10.1177/036354659602400110. [DOI] [PubMed] [Google Scholar]
- 24.Sanders T.G., Morrison W.B., Singleton B.A. Medial patellofemoral ligament injury following acute transient dislocation of the patella: MR findings with surgical correlation in 14 patients. J Comput Assist Tomogr. 2001;25:957–962. doi: 10.1097/00004728-200111000-00021. [DOI] [PubMed] [Google Scholar]
- 25.Desio S.M., Burks R.T., Bachus K.N. Soft-tissue restraints to lateral patellar translation in the human knee. Am J Sports Med. 1998;26:59–65. doi: 10.1177/03635465980260012701. [DOI] [PubMed] [Google Scholar]
- 26.Nomura E., Horiuchi Y., Inoue M. Correlation of MR imaging findings and open exploration of medial patellofemoral ligament injuries in acute patellar dislocations. Knee. 2002;9:139–149. doi: 10.1016/s0968-0160(02)00002-9. [DOI] [PubMed] [Google Scholar]
- 27.Nomura E., Inoue M., Osada N. Anatomical analysis of the medial patellofemoral ligament of the knee, especially the femoral attachment. Knee Surg Sports Traumatol Arthrosc. 2005;13:510–515. doi: 10.1007/s00167-004-0607-4. [DOI] [PubMed] [Google Scholar]
- 28.Nomura E., Horiuchi Y., Kihara M. Medial patellofemoral ligament restraint in lateral patellar translation and reconstruction. Knee. 2000;7:121–127. doi: 10.1016/s0968-0160(00)00038-7. [DOI] [PubMed] [Google Scholar]
- 29.Smirk C., Morris H. The anatomy and reconstruction of the medial patellofemoral ligament. Knee. 2003;10:221–227. doi: 10.1016/s0968-0160(03)00038-3. [DOI] [PubMed] [Google Scholar]
- 30.Avikainen V.J., Nikku R.K., Seppänen-Lehmonen T.K. Adductor magnus tenodesis for patellar dislocation. Technique and preliminary results. Clin Orthop Relat Res. 1993;(297):12–16. [PubMed] [Google Scholar]
- 31.Deie M., Ochi M., Sumen Y. A long-term follow-up study after medial patellofemoral ligament reconstruction using the transferred semitendinosus tendon for patellar dislocation. Knee Surg Sports Traumatol Arthrosc. 2005;13:522–528. doi: 10.1007/s00167-005-0641-x. [DOI] [PubMed] [Google Scholar]
- 32.Giordano M., Falciglia F., Aulisa A.G. Patellar dislocation in skeletally immature patients: Semitendinosus and gracilis augmentation for combined medial patellofemoral and medial patellotibial ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2012;20:1594–1598. doi: 10.1007/s00167-011-1784-6. [DOI] [PubMed] [Google Scholar]
- 33.Nelitz M., Dreyhaupt J., Reichel H. Anatomic reconstruction of the medial patellofemoral ligament in children and adolescents with open growth plates: Surgical technique and clinical outcome. Am J Sports Med. 2013;41:58–63. doi: 10.1177/0363546512463683. [DOI] [PubMed] [Google Scholar]
- 34.Siebold R., Borbon C.A. Arthroscopic extraarticular reconstruction of the medial patellofemoral ligament with gracilis tendon autograft—Surgical technique. Knee Surg Sports Traumatol Arthrosc. 2012;20:1245–1251. doi: 10.1007/s00167-012-1968-8. [DOI] [PubMed] [Google Scholar]
- 35.Tohyama H., Beynnon B.D., Johnson R.J. Morphometry of the semitendinosus and gracilis tendons with application to anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 1993;1:143–147. doi: 10.1007/BF01560195. [DOI] [PubMed] [Google Scholar]
- 36.Xie G., Huangfu X., Zhao J. Prediction of the graft size of 4-stranded semitendinosus tendon and 4-stranded gracilis tendon for anterior cruciate ligament reconstruction: A Chinese Han patient study. Am J Sports Med. 2012;40:1161–1166. doi: 10.1177/0363546511435627. [DOI] [PubMed] [Google Scholar]
- 37.Ntagiopoulos P.G., Sharma B., Bignozzi S. Are the tubular grafts in the femoral tunnel in an anatomical or isometric position in the reconstruction of medial patellofemoral ligament? Int Orthop. 2013;37:1933–1941. doi: 10.1007/s00264-013-1938-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Thaunat M., Erasmus P.J. Management of overtight medial patellofemoral ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2009;17:480–483. doi: 10.1007/s00167-008-0702-z. [DOI] [PubMed] [Google Scholar]
- 39.Cossey A.J., Paterson R. A new technique for reconstructing the medial patellofemoral ligament. Knee. 2005;12:93–98. doi: 10.1016/j.knee.2004.05.003. [DOI] [PubMed] [Google Scholar]
- 40.Goyal D. Medial patellofemoral ligament reconstruction: The superficial quad technique. Am J Sports Med. 2013;41:1022–1029. doi: 10.1177/0363546513477828. [DOI] [PubMed] [Google Scholar]
- 41.Zaffagnini S., Muccioli G.M.M., Grassi A. Minimally invasive medial patellofemoral ligament reconstruction with fascia lata allograft: Surgical technique. Knee Surg Sports Traumatol Arthrosc. 2014;22:2426–2430. doi: 10.1007/s00167-014-2940-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(1) Required equipment for medial patellofemoral ligament (MPFL) reconstruction (also described in the text). (2) Marking of the incision area followed by a lateral 6-cm incision approximately 4 fingerbreadths above the patella. (3) Blunt preparation onto the fascia lata. (4) Detachment of the fascia lata part at the desired area of 10 mm in width and 12 cm in length. (5) Closure of the gap without tension with a resorbable suture wire. (6) Preparation of the graft (clearing of fat and muscle tissue, cutting into 2 pieces of 5 mm in width and 12 cm in length, and attaching the grafts on each pole with No. 2 FiberWire). (7) Creation of a 2-cm incision at the medial margin of the patella, with removal of the soft tissue until the patellar bone is clearly visible. (8) Placement of the 2 guidewires at the proximal two-thirds of the medial patellar margin, parallel to each other (the correct position can be verified under fluoroscopic control on a straight lateral view). (9) Creation of two 25-mm-deep caves inside the patella using a 4-mm drill. (10) Fixation of the first graft using a 4.75-mm Bio-SwiveLock anchor, with implantation of the screw until it is completely embedded inside the tunnel. (11) Fixation of the second graft inside the distal tunnel according to the first graft. (12) Finding the femoral insertion point of the MPFL using fluoroscopic control on a straight lateral view, and performing a small skin incision. (13) Creation of a tunnel between the second and third layers of the original MPFL from the patella to the femoral incision point. (14) Transfer of both grafts through the tunnel to the exit at the femoral point using a shuttle wire. (15) Drilling of a guidewire from the medial insertion point until it exits on the lateral side. (16) Creation of the femoral tunnel using a drill that is 1 mm larger than the diameter of both ends of the grafts. (17) Placement of the grafts inside the tunnel using a shuttle wire, and pulling of the guidewire from the lateral side. (18) Careful assessment to ensure that the grafts are not contorted or twisted. (19) Application of the correct tension of each graft on its own by pulling at the shuttle wires and then fixing the wires with a clip and evaluating the patellar movement during manual flexion and extension of the knee. (20) Placement of a bioabsorbable screw, followed by a final check of the patellofemoral kinematics. (21) Skin closure.


