Abstract
AIM: To examine familial aggregation of irritable bowel syndrome (IBS) via parental reinforcement/modeling of symptoms, coping, psychological distress, and exposure to stress.
METHODS: Mothers of children between the ages of 8 and 15 years with and without IBS were identified through the Group Health Cooperative of Puget Sound. Mothers completed questionnaires, including the Child Behavior Checklist (child psychological distress), the Family Inventory of Life Events (family exposure to stress), SCL-90R (mother psychological distress), and the Pain Response Inventory (beliefs about pain). Children were interviewed separately from their parents and completed the Pain Beliefs Questionnaire (beliefs about pain), Pain Response Inventory (coping) and Child Symptom Checklist [gastrointestinal (GI) symptoms]. In addition, health care utilization data was obtained from the automated database of Group Health Cooperative. Mothers with IBS (n = 207) and their 296 children were compared to 240 control mothers and their 335 children, while controlling for age and education.
RESULTS: Hypothesis 1: reinforcement of expression of GI problems is only related to GI symptoms, but not others (cold symptoms) in children. There was no significant correlation between parental reinforcement of symptoms and child expression of GI or other symptoms. Hypothesis 2: modeling of GI symptoms is related to GI but not non-GI symptom reporting in children. Children of parents with IBS reported more non-GI (8.97 vs 6.70, P < 0.01) as well as more GI (3.24 vs 2.27, P < 0.01) symptoms. Total health care visits made by the mother correlated with visits made by the child (rho = 0.35, P < 0.001 for cases, rho = 0.26, P < 0.001 for controls). Hypothesis 3: children learn to share the methods of coping with illness that their mothers exhibit. Methods used by children to cope with stomachaches differed from methods used by their mothers. Only 2/16 scales showed weak but significant correlations (stoicism rho = 0.13, P < 0.05; acceptance rho = 0.13, P < 0.05). Hypothesis 4: mothers and children share psychological traits such as anxiety, depression, and somatization. Child psychological distress correlated with mother’s psychological distress (rho = 0.41, P < 0.001 for cases, rho= 0.38, P < 0.001 for controls). Hypothesis 5: stress that affects the whole family might explain the similarities between mothers and their children. Family exposure to stress was not a significant predictor of children’s symptom reports. Hypothesis 6: the intergenerational transmission of GI illness behavior may be due to multiple mechanisms. Regression analysis identified multiple independent predictors of the child’s GI complaints, which were similar to the predictors of the child’s non-GI symptoms (mother’s IBS status, child psychological symptoms, child catastrophizing, and child age).
CONCLUSION: Multiple factors influence the reporting of children’s gastrointestinal and non-gastrointestinal symptoms. The clustering of illness within families is best understood using a model that incorporates all these factors.
Keywords: Abdominal pain, Coping, Illness behaviors, Psychological distress, Social learning, Stress
Core tip: Irritable bowel syndrome tends to run in families. In previous studies, we found that this phenomenon could be explained by reinforcement and modeling of gastrointestinal illness behavior by parents. The current study extend these findings by examining various psychosocial influences on intergenerational transmission. We found that multiple psychosocial similarities between the mother and child may explain familial aggregation, including the mother’s modeling of irritable bowel syndrome symptoms, shared psychological distress, and shared family stress.
INTRODUCTION
Irritable bowel syndrome (IBS) tends to cluster in families[1-5]. The children of mothers with IBS are more likely than the children in control families to report bothersome gastrointestinal (GI) symptoms, to miss school for GI symptoms, and to be brought to the doctor for GI symptoms[1,2] We have referred to this phenomenon as the intergenerational transmission of GI illness behavior.
In a series of studies extending over more than 30 years, we[1-3,6-11] and others[12-15] have attempted to identify psychosocial factors that could explain how GI illness behavior is passed from one generation to another. In previous studies, we found that this phenomenon could be explained by social learning in the form of reinforcement and modeling of GI illness behavior by parents[1,2,6-8]. In the current study, we want to extend our previous reports by examining various psychosocial influences on intergenerational transmission. These include five categories. (1) Reinforcement of illness behaviors: multiple studies have shown that parental protective behaviors can increase pain and disability in children with GI symptoms[16-20]. This suggests that selective attention to expression of GI problems or limiting the child’s normal activities and responsibilities may unintentionally reinforce illness behaviors; (2) Modeling of illness behaviors: the observation that children of mothers who have IBS report more GI symptoms than the children of control mothers suggests that social learning through modeling processes may also contribute to the intergenerational transmission of GI illness behavior[2]; (3) Shared methods of coping with illness: children may learn to interpret somatic symptoms in the same way as their parents (i.e., as threatening or non-threatening) and to cope with abdominal pain in a similar way; (4) Shared psychological phenomena: Psychological distress is known to be associated with somatic symptoms. Mothers and their children may have similar psychological traits that predispose them to report somatic symptoms; and (5) Psychological stress: studies in adults and children have shown that exposure to stress is associated with an increased tendency to report GI and other somatic symptoms[21-27]; thus, stress affecting the whole family could explain similarities in symptom reports between mothers and children.
A previous report of this study has been published[1], which supported the social learning hypothesis (category 2 from above) by showing that when parents respond solicitously to their children’s GI complaints, their children are more likely to describe themselves as having serious GI symptoms, and they are more likely to miss school because of reported GI symptoms.
The aim of the analyses presented in this report is to look more broadly at several psychosocial influences on symptom reporting by examining several variables together. First, we will determine if transmission of mother to child is specific to GI symptoms or generalizes to other symptoms as well. Our first hypothesis is that reinforcement of expression of GI problems is related only to GI symptom reporting, and not to reporting of other symptoms in children. Secondly, we hypothesize that modeling of GI symptoms is related to GI but not non-GI symptom reporting in children. For this we will examine if IBS mothers have children who not only report increased GI symptoms, but also report increased cold symptoms compared to controls. The focus on cold symptoms is in line with previous research in adults[6], which found that IBS patients recalled their parents responding with empathy and concern to both GI and cold symptoms. Research in children has focused exclusively on GI symptoms so far. Our next three hypotheses examine similarities between mother and child that may explain shared GI symptoms. The third hypothesis is that children learn to share the methods of coping with illness that their mothers exhibit. Our fourth hypothesis states that mothers and children share psychological traits, such as anxiety, depression, and somatization, and our fifth hypothesis examines if family stress might explain the GI similarities between mothers and their children. Lastly, we will examine if the intergenerational transmission of GI illness behavior may be due to multiple mechanisms.
MATERIALS AND METHODS
This study is a secondary data analysis of an existing dataset. The methods described below are based on the original data collection and recruitment methods.
Subjects
The electronic medical records of Group Health Cooperative of Puget Sound were used to identify all women who had received a diagnosis of IBS or abdominal pain at a clinic visit during the preceding two years and who had one or more children between the ages of 8 and 15 years. Women with a diagnosis of IBS were sent a letter explaining the study and notifying them that they would be contacted by telephone unless they declined by returning a postcard. Women with a diagnosis of abdominal pain received a letter explaining the study, but were not contacted unless they returned a postcard confirming that they had symptoms consistent with IBS (we assumed that less than half would satisfy diagnostic criteria for IBS). Potential subjects were screened by phone to insure that the mother met Rome I criteria for IBS diagnosis[28]. These criteria are as follows: ≥ 3 mo of continuous or recurrent abdominal pain that is relieved with defecation and/or changes in stooling frequency or consistency as well as two or more of altered stool frequency, form, or passage, passing mucus, and/or bloating on one-fourth of occasions or days[29].
Control families were selected from the electronic medical records by identifying women who did not have a clinic visit during the preceding two years for IBS, abdominal pain, constipation, or diarrhea, and who had children within the 8-15 years-old age range. Controls were also screened by telephone interview to insure that neither the mother nor any adult family member met Rome I criteria for IBS.
Additional inclusion criteria that applied to both cases and controls were ascertained in the telephone interview: (1) mother was the child’s legal guardian and the child lived with her at least half of the time during the preceding two years; (2) the child did not have a developmental disability requiring full-time special education; and (3) no family member had a diagnosis of ulcerative colitis or Crohn’s disease. At the conclusion of the telephone interview, subjects were scheduled for an in-person interview. All eligible children willing to participate were enrolled in the study, allowing inclusion of multiple children per family.
This study was reviewed and approved by the Institutional Review Boards of Group Health Cooperative, the University of Washington, and the University of North Carolina.
Procedure and measures
Children and their mothers completed a battery of tests[1]. Children were interviewed separately from their parents by a trained interviewer.
Child measures: Pain Beliefs Questionnaire (CPBQ), this questionnaire measures children’s beliefs about their own abdominal pain[30]. This measure contains 32 statements concerning stomachaches. A trained interviewer asked the child to respond to each statement by rating how true it was for their stomach aches. There were five possible answers ranging from “not at all true” to “very true”. Out of seven different subscales, we included only the subscales for condition seriousness and condition frequency. The CPBQ has been found to be valid and reliable[31]. A sample question is: “My stomachaches mean I have a serious illness”.
Pain Response Inventory (PRI), child version, this questionnaire measures how children cope with abdominal pain[32]. A sample question is: “If I have a stomachache or other stomach problems, I try hard to do something about it”. The PRI assesses three broad pain coping factors, active, passive, and accommodative, each with subscales representing specific strategies for coping with pain, including a five-item catastrophizing subscale. The PRI has good internal reliability and validity[32].
Child Symptom Checklist (CSCL), the CSCL lists the 17 most common symptoms, including five GI symptoms from the Children’s Somatization Inventory[33]. The child is asked to rate on a scale from 0-4 how much he or she was bothered by each symptom in the past two weeks. For example: “In the last 2 wk, how much were you bothered by pain in your stomach or abdomen?” The Children Somatization Inventory has excellent validity and reliability[33,34]. For this study, we added seven upper-respiratory symptoms: having a cold, runny nose, stuffy nose, sneezing, sore throat, coughing, and chest congestion. The questions coincide with respiratory questions on the Common Cold Questionnaire (general symptoms on this questionnaire such as “fevers” were not included)[35], which has been validated in children with asthma. We added the item “having a cold.” The use of cold questions was modeled after research in adults, in which childhood reinforcement of cold symptoms reinforced adult cold symptoms but were independent of adult bowel symptoms[6,7]. Given that reinforcement of cold symptoms has previously been shown to be unrelated to reinforcement of bowel symptoms, the use of cold symptoms can measure the specificity of learned illness behaviors in children.
The CSCL inventory was scored for three subscales, GI symptoms, cold symptoms, and non-GI/non-cold symptoms. Scale scores were computed by summing ratings for all items on the scale. Psychometric properties for the original questionnaire are good[34,36].
Parental report of child distress: The mother was asked to complete the Child Behavior Checklist (CBCL) for each child who participated in the survey[37]. This inventory contains 112 symptoms or behavior problems, and mothers were asked to respond by indicating whether these occurred “never,” “sometimes,” or “often.” A sample question is: “Acts too young for his/her age.” The CBCL can be scored for two global scales, internalizing and externalizing, as well as nine subscales. In this study, the internalizing scale was used because it is conceptually most similar to the global symptom index of the SCL-90R used to test the mothers, and the T-scores transformations[38] were used so that boys and girls could be pooled together in the same analyses. The CBCL was also scored for the somatization, anxiety, and depression subscales for comparison to adult psychological scales. The CBCL has been widely validated[37].
Parent questionnaires: Family Inventory of Life Events (FILE), this is a parent-report form that assesses potentially stressful negative life events experienced by family members in the previous year[39]. For example: “Increased conflict with in-laws or relatives”. McCubbin et al[39] reported that internal consistency is 0.81 and four-week test-retest reliability is 0.80. Agreement between family members on the occurrence of events supports the validity of the FILE.
SCL-90R, the anxiety, depression, and somatization subscales of the SCL-90R were used to assess psychological distress in the mother[40]. Derogatis[40] reports high test-retest reliability and convergent validity. Derogatis and Cleary[37] also demonstrated a theoretically consistent factor structure. A sample item is “How much were you bothered by feeling fearful?”
PRI, adult version: the PRI was reworded to assess the mother’s characteristic responses to her own abdominal pain[32].
Adult Response to Child Symptoms (ARCS), solicitous responding to GI and cold complaints were measured by the Protective subscale of the ARCS[41], which was completed by the mother. A sample question from this scale is: “When your child has a stomachache or abdominal pain/cold, how often do you tell your child he/she doesn’t have to finish all of his/her homework?” The ARCS has high internal consistency and validity has been established for the Protective subscale[42,43].
Health care utilization data
The automated database of Group Health Cooperative was used to calculate the total number of ambulatory visits made by the child and by the mother for any illness and the total number of visits for a lower GI indication during a three-year period. This period extended from the date of the interview back two years in time and forward one year in time.
Data analysis
Many analyses below compare children of case and control mothers. As these groups were significantly different for age and education, these two variables were entered as covariates in statistical tests comparing the two groups to control for these differences.
Hypothesis 1: Reinforcement of expression of GI problems is related to GI but not other symptom reporting in children. This was evaluated by comparing cases and controls with respect to the scales of the ARCS, which measures solicitous responses to expression of GI symptoms and solicitous responses to cold symptoms. Nonparametric (Spearman) correlations were used to compare mother’s scores on the solicitousness scales of the ARCS to symptom reports of children.
Hypothesis 2: Modeling of GI symptoms is related to GI but not non-GI symptom reporting in children. This was evaluated by F-tests comparing case and control mothers and their children with respect to the frequency of medical clinic visits for different categories of illness. Nonparametric (Spearman) correlations were used to compare health care visits in children to health care visits by their mothers.
Hypothesis 3: Children learn to share the methods of coping with illness that their mothers exhibit. This was tested by computing nonparametric correlations between the coping scale scores of children on the PRI to the coping scale scores of their mothers on the adult version of the same inventory.
Hypothesis 4: Mothers and children share psychological traits such as anxiety, depression, and somatization. This was tested by computing nonparametric correlations between children and their mothers on these psychological scales.
Hypothesis 5: Stress that affects the whole family might explain the similarities between mothers and their children. This was assessed by computing the correlation between the FILE[39] and the GI and non-GI subscales of the CSCL. All children were included in these analyses.
Hypothesis 6: The intergenerational transmission of GI illness behavior may be due to multiple mechanisms, and some of the factors discussed above (e.g., stress and anxiety) may be correlated with each other. Therefore, separate regression analyses were used to identify independent child and mother characteristics that predict GI and non-GI symptom reporting in children. To reduce the number of independent variables in these analyses, we first computed the nonparametric correlations of the dependent measures with all psychosocial variables measured and selected the variables with significant (P < 0.05) correlations with either dependent variable for inclusion in the regression analyses. The same set of predictor variables were used in both regression analyses.
RESULTS
Demographics
Table 1 gives the demographic characteristics of the children and shows that the two groups were comparable. The average age of the 240 control mothers was 45.5 ± 0.4 years, and average age of the 207 IBS mothers was 41.8 ± 0.5 years (P < 0.01). Sixty percent of control mothers had completed college compared to 36% of IBS mothers (P < 0.001). Age and education of mothers was controlled for in between-group comparisons. The average number of children in the family was 2.1 ± 0.1 for controls and 2.0 ± 0.1 for case families.
Table 1.
Characteristics of the sample
| Characteristics | Case | Control |
| Children, n | 296 | 335 |
| Age, yr (mean ± SD) | 11.89 ± 2.62 | 11.84 ± 2.49 |
| Male sex, % | 48.6 | 49 |
| Ethnicity, % | ||
| Caucasian | 77.5 | 82.6 |
| African American | 5.8 | 5.7 |
| Asian | 6.1 | 8.7 |
| Hispanic | 4.8 | 2.4 |
| Native American | 0.7 | 0.3 |
Table 2 shows that symptoms and health care visits were strongly correlated among children and parents, supporting the intergenerational transmission of expression of GI problems symptoms. The next set of analyses will aim to determine the psychosocial mechanisms by which this transmission may happen.
Table 2.
Number of medical clinic visit for each symptom category by mothers and children in case and control families, and correlation between number of mother and child visits
| Symptom category |
Case families |
Control families |
Combined samples |
||||||
| Mother | Child | rho | Mother | Child | rho | All mothers | All children | rho | |
| mean ± SE | mean ± SE | mean ± SE | mean ± SE | mean ± SE | mean ± SE | ||||
| Gastrointestinal | 3.27 ± 0.18c | 0.61 ± 0.16a | 0.064 | 0.20 ± 0.03 | 0.20 ± 0.05 | 0.042 | 1.62 ± 0.11 | 0.39 ± 0.08 | 0.219e |
| Upper respiratory infection | 2.07 ± 0.14c | 1.97 ± 0.15c | 0.290e | 0.74 ± 0.06 | 1.08 ± 0.09 | 0.326e | 1.37 ± 0.08 | 1.50 ± 0.09 | 0.355e |
| Asthma | 0.60 ± 0.13c | 0.48 ± 0.10 | 0.203e | 0.09 ± 0.02 | 0.30 ± 0.08 | 0.180e | 0.32 ± 0.06 | 0.37 ± 0.06 | 0.204e |
| Headache | 1.47 ± 0.42b | 0.25 ± 0.06 | 0.056 | 0.22 ± 0.06 | 0.14 ± 0.04 | 0.097 | 0.76 ± 0.20 | 0.19 ± 0.03 | 0.089d |
| Back pain | 1.43 ± 0.23c | 0.17 ± 0.04 | 0.168d | 0.31 ± 0.05 | 0.12 ± 0.03 | -0.038 | 0.77 ± 0.09 | 0.14 ± 0.02 | 0.080d |
| All outpatient visits | 30.25 ± 1.53c | 12.90 ± 0.80c | 0.348e | 10.74 ± 0.43 | 8.45 ± 0.49 | 0.260e | 19.80 ± 0.083 | 10.50 ± 0.46 | 0.375e |
P < 0.05 case vs control;
P < 0.01 case vs control;
P < 0.001 case vs control;
P < 0.05 mother vs child;
P < 0.001 mother vs child.
Do mothers with IBS exclusively reinforce expression of GI problems?
We investigated whether case mothers only behave in a solicitous fashion in response to illness behaviors related to GI symptoms. Contrary to hypothesis, there were no differences between case and control mothers for solicitous responses to expression of GI symptoms [29.10 ± 0.64 vs 28.40 ± 0.63, F(1/608) = 0.23, P = 0.631], or cold symptoms [29.39 ± 0.64 vs 29.29 ± 0.59, F(1/611), P = 1.542]. There was no significant correlation between the ARCS Protective scale for GI illness behavior and scores on this GI symptom scale (rho= 0.01), nor was there a significant correlation between the ARCS Protective scale for cold illness behavior and scores on the cold symptom scale (rho = 0.06).
Do mothers with IBS exclusively model GI symptoms?
The question addressed was whether case mothers modeled only GI illness behavior (i.e., modeled a unique class of illness behaviors) or whether they also displayed other types of illness behavior for possible imitation by their children. Table 2 shows that, in addition to excess clinic visits for GI symptoms, case mothers made more clinic visits than control mothers for all types of disorders evaluated, including upper respiratory symptoms, asthma, headaches, and back pain. In a three-year period, the case mothers made three times as many health care visits overall compared to the control mothers, and visits with a GI diagnosis accounted for only 3/19 excess health care visits (see Table 2).
Table 2 also provides data on whether case children showed selective increases in medical clinic visits for GI symptoms vs whether they showed increases in all types of health care visits. Case children had significantly more overall health care visits than controls (12.90 visits/3 years vs 8.45 visits/3 years; P < 0.001), and they also had significantly more clinic visits for upper respiratory infections (P < 0.001). In addition, Table 2 shows (last column) that the frequency of clinic visits made by children was significantly correlated with the number of clinic visits made by their parents across all disease categories, a finding that is consistent with social learning but does not show it to be specific to GI complaints.
Do children model the coping mechanisms and other illness-related cognitions of their mothers?
Correlations between children and their mothers on the scales of the PRI were generally very low. Among case children and their parents, only 2/16 scales showed statistically significant correlations; these were stoicism (rho = 0.13; P < 0.05) and acceptance (rho = 0.10; P < 0.05).
Do children share psychological traits with their mothers?
Table 3 shows the average scores on the psychological dimensions of overall psychological distress, anxiety, depression, and somatization in both mothers and children. Case mothers had significantly higher scores on all scales compared to control mothers, and case children had significantly higher scores on all scales compared to control children (all P < 0.05). For each of these psychological scales, the scores of children were significantly correlated with the scores of their mothers.
Table 3.
Psychological traits in children and their mothers
| Psychological trait |
Case families |
Control families |
Combined samples |
||||||
| Mother | Child | rho | Mother | Child | rho | All mothers | All children | rho | |
| mean ± SE | mean ± SE | mean ± SE | mean ± SE | mean ± SE | mean ± SE | ||||
| Global psychological distress | 2.81 ± 0.10a | 55.16 ± 0.62a | 0.414b | 1.22 ± 0.07 | 48.46 ± 0.53 | 0.376b | 1.99 ± 0.07 | 51.65 ± 0.42 | 0.484b |
| Anxiety | 0.66 ± 0.04a | 4.64 ± 0.25a | 0.314b | 0.30 ± 0.02 | 2.65 ± 0.17 | 0.354b | 0.46 ± 0.02 | 3.60 ± 0.15 | 0.393b |
| Depression | 1.01 ± 0.04a | 2.20 ± 0.15a | 0.282b | 0.48 ± 0.03 | 1.29 ± 0.09 | 0.301b | 0.77 ± 0.03 | 1.72 ± 0.09 | 0.345b |
| Somatization | 1.15 ± 0.04a | 3.24 ± 0.16a | 0.366b | 0.45 ± 0.02 | 1.73 ± 0.10 | 0.157b | 0.78 ± 0.03 | 2.43 ± 0.10 | 0.374b |
P < 0.001 case vs control;
P < 0.001 mother vs child.
Effects of shared family stress on the child’s symptom reports: The FILE score for family stress correlated significantly with the GI Symptom subscale of the CSCL (rho = 0.10, P < 0.05), though the correlation is unlikely to be clinically meaningful.
Regression analysis to identify contributors to child symptom reports: In order to determine which child and parental factors are most important contributors to child expression of GI and non-GI problems, two regression analysis was performed: one with the GI symptom subscale and the other with the other symptom subscale of the CSCL as the dependent variable. Variables were included independent of whether mother-child overlap was found. This was in order to determine which of the variables were the most likely to influence reported symptoms. The variables which were found to make significant independent contributions to the symptom reports of the child are shown in Figure 1. The total variance that could be explained by this combination of variables was 12% for GI symptom reports and 16% for non-GI symptom reports. In general, the same variables predicted both GI symptom reports and non-GI symptom reports of the child, and the standardized betas show that these variables contributed to both types of symptom reports in a similar way. An exception was child’s age, which was positively correlated only with non-GI symptoms. In addition, mother’s IBS severity contributed only to child GI symptoms.
Figure 1.
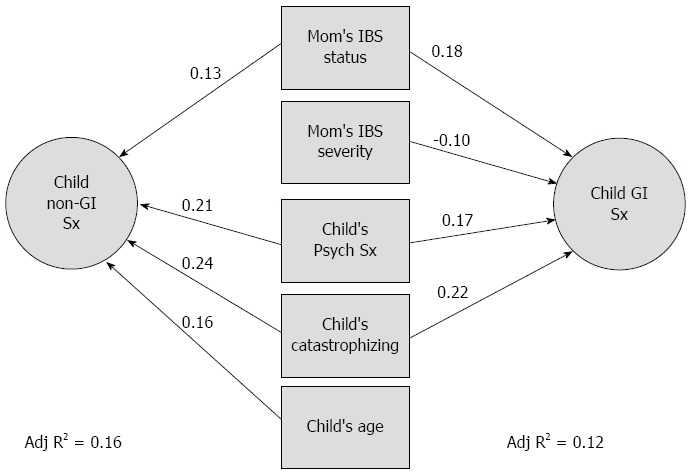
Comparison of regression analyses used to identify independent predictors of children’s expression of gastrointestinal symptoms (right side of figure) and children’s non-gastrointestinal symptoms (left side of figure). Numbers beside arrows represent the beta weights for these predictors. IBS: Irritable bowel syndrome; Sx: Symptoms.
DISCUSSION
There is a striking tendency for IBS to cluster within families. We evaluated five psychosocial hypotheses that may contribute to the intergenerational transmission of illness behaviors.
Modeling
We hypothesized that a child may learn expression of GI symptoms through the observation of a model’s behavior (i.e., the mother). This implies that the role model displays a specific behavior pattern and that the child selectively emulates this behavior pattern. When we tested the specificity of modeling by mothers, we found little evidence for it: mothers with IBS consulted physicians more often than control mothers for a wide range of somatic complaints, and only about 16% of their excess health care utilization was for GI symptoms. It was therefore not surprising to find that the children of IBS mothers reported excess somatic complaints that were not specific to GI as well: only about 10% of their excess visits were for GI diagnoses. The correlations between the number of health care visits by mothers and their children for all types of illness were more robust than the correlations between mother and child for GI visits. These data are consistent with the hypothesis that the intergenerational transmission of illness behavior may occur through modeling, but a diffuse pattern of comorbidity dominates the association. Many studies have previously found that pain, and IBS in particular, clusters in families[2,44], corroborating the current findings.
Reinforcement of illness behaviors
Another way a child may learn from a parent is when the parent reinforces expression of GI problems in their children by giving special attention when the child complains of a stomachache. Multiple studies have shown that parental protective behaviors can increase pain and disability in children with GI symptoms[16-20,44]. What is new in the current study is that we predicted that the correlation between mother’s solicitous responses and child-reported symptoms would be stronger for GI symptoms than for cold symptoms. However, neither correlation exceeded 0.10, and there was no difference between them. We also previously found that parental solicitous response to child GI symptoms is not associated with reported abdominal pain frequency, but rather with the child’s perception of the seriousness of the symptoms[1]. The current study only focused on the reported occurrence of symptoms and did not examine which factors influence interpretation of the seriousness of symptoms. These differences in factors measured in this vs our earlier work may explain the difference in findings on the relationship between solicitousness and reported GI symptoms reported here. Furthermore, behavioral theory predicts that solicitousness is associated with changes in pain behaviors, but this study did not directly measure pain behavior per se, but reported symptoms.
The finding that both modeling and reinforcement of somatic symptoms was not different for cold and GI symptoms suggests that the intergenerational transmission of illness behavior from IBS mothers to their children is the transmission of a general pattern of somatic complaints and not a specific tendency to report GI symptoms. This is in contrast to studies in which adults were asked about their childhood experiences. In this case, specific patterns of symptoms were reported: adults who remember their parents reinforcing cold symptoms, reported more cold symptoms but not GI symptoms, while adults who remember parents reinforcing GI symptoms reported more GI but not cold symptoms[7]. It needs to be investigated if this discrepancy with our current findings is due to recall issues in adulthood or to developmental differences in the effects of parental reinforcement.
Cognitions and coping styles
We found no support for the hypothesis that intergenerational transmission of GI illness behavior is explained by the child adopting the methods used by the mother to cope with the threats posed by illness. There were no meaningful correlations between mothers and their children on the PRI. The mother’s use of passive coping strategies was found to be negatively correlated with symptom reporting by the child. This implies it is obverse, namely that mothers who are not passive, but rather actively seek to solve their own stomachaches, are more likely to have children who make multiple somatic complaints.
Psychological traits
Both adults[45] and children[46] with functional GI disorders are known to have higher levels of psychological distress, and it has been suggested that psychological symptoms, such as depression, anxiety, and somatization, may predispose patients to report more somatic symptoms of many kinds. We found that mothers and their children are remarkably similar to each other in the psychological symptoms they display, even though there are marked methodological differences between the SCL-90R used to assess psychological symptoms in adults and the CBCL used to assess behavior problems in children. These findings are in line with studies that have shown intergenerational transmission of psychological disorders such as anxiety and depression[47,48].
It is not known how children come to exhibit the same psychological symptoms as their mothers, although heredity and social learning through such mechanisms as modeling are possibilities. It is also unclear how these similarities in psychological traits can explain the intergenerational transmission of GI complaints. It is possible that children learn to emulate their mothers’ hypervigilance for noticing somatic sensations and their tendency to attribute disease significance to these sensations. Consistent with this speculation, there was a positive correlation between mothers and children for somatization. However, the correlations for somatization were no stronger than the correlations for anxiety and depression or for psychological symptom severity in general. Purposefully designed studies are needed to address the ways in which psychological traits are transmitted between generations, and the ways in which they influence GI symptom reporting.
Stress
Family stress was significantly correlated with GI symptom reports by the child; however, the correlations were relatively weak and likely to be of little clinical significance.
Multiple factors predicting child GI symptoms
Regression analyses show that there are multiple psychosocial factors that make independent contributions to the prediction of children’s symptom reports. The same psychosocial factors predict both GI and non-GI symptom reports by the child. These include both characteristics of the mother (her IBS status and severity) and characteristics of the child (his or her overall level of psychological distress and tendency catastrophize). We would like to emphasize that catastrophizing about stomachaches by the child was associated with an increased tendency to report both GI and non-GI symptoms. This has been reported for adults[49], but has not previously been confirmed in children.
Study limitations
A limitation of this study was a modest participation rate. The necessity of obtaining consent from two (or more) family members (i.e., the mother and each eligible child) was an important factor influencing the level of participation. A second limitation was that the control group of mothers was older and more educated than the cases. We controlled statistically for this limitation in our analyses, but we cannot rule out that it may still have affected our outcomes. A third limitation was that only mothers were studied; other research has demonstrated that the health status of the father may have as great an influence on the illness behavior of the child as the mother[1]. Moreover, this study was designed with the intent of explaining the intergenerational transmission of illness behavior. However, our study was retrospective in nature and, therefore, a cause and effect cannot be confirmed. The findings we report in this manuscript should be regarded as exploratory, and should be confirmed in further prospective studies.
Other limitations relate to the challenges of assessing symptoms in children and the fact that methods used to assess psychological symptoms and coping in children were only approximately equivalent to methods used in their mothers. These methodological limitations may have contributed to the relatively low correlations and regression coefficients we observed.
In our previous publications, we emphasized the significance of modeling and reinforcement for the clustering of functional GI symptoms within families. The important contribution of the present study is that we expanded our understanding of the many ways multiple factors, including psychological phenomena, can influence a child’s response to somatic feelings. Mothers with IBS and their children are alike in their tendency to report most types of somatic symptoms, including both GI and non-GI symptoms. Children are also similar to their mothers in the severity and types of psychological traits they have, and psychological traits in the child are associated with increased symptom reports. Mothers and children in this study were not found to share cognitions and coping styles with pain. However, even if parents and children did not share similar coping, we found that less passivity on the part of the mother, and a tendency to catastrophize about illness on the part of the child, was associated with more somatic symptom reports. Thus, it appears that there are multiple independent factors or behavior patterns that may be passed or shared between parent and child that contribute to the clustering of illness within families. Future research, and the potential for this research to contribute to our understanding, would benefit from including this more comprehensive, multidimensional perspective on this phenomenon.
COMMENTS
Background
Irritable bowel syndrome (IBS) is a chronic condition characterized by abdominal pain and changes in stool. IBS often runs in families. One reason for this is that children may inadvertently learn symptoms from their parents. Research has shown that when parents are sick themselves or respond with a lot of empathy and sympathy to the child’s symptoms, they may communicate that gastrointestinal symptoms are important and should be attended to.
Research frontiers
Parents play an important role in child’s symptoms. Parents drive a large part of the disability because they make the decision to take the child out of school and/or consult a doctor. In addition, the way parents react to their own symptoms and their child’s symptoms has been found to predict child’s abdominal pain level. Current research is exploring the many ways in which parents contribute to child’s symptoms and how to help parents in managing their child’s symptoms.
Innovations and breakthroughs
Previous studies have mainly focused on children learning through observing parental reactions to their own pain and to the child’s pain. However, children may learn from or share other characteristics with their parents that may put them at risk for developing IBS. For example, stress, psychological symptoms, and how one copes with the gastrointestinal symptoms have been found to be important predictors of symptom severity. It is not known if these characteristics are shared by parent and child.
Applications
The current study explored if multiple psychosocial mechanisms may explain how gastrointestinal symptoms are transmitted from parent to child. The authors found that learning of symptoms was not specific to gastrointestinal symptoms but to other symptoms as well, indicating that children of parents with IBS learn to attend to all symptoms, not just those related to IBS. In addition, the authors found that parents and children shared similar levels of psychological symptoms, which may indirectly increase gastrointestinal symptoms. Parents and children did not share the same methods of coping with symptoms, nor did family stress predict child symptoms. Thus, children of parents with IBS may be at increased risk of gastrointestinal symptoms because they learn to attend to all symptoms from their parents and because they share similar psychological symptoms, which may indirectly increase gastrointestinal symptoms. The transmission of parent to child is best understood within a model that incorporates both these factors.
Terminology
Modelling is learning that occurs when a child observes and copies parental reactions to parent symptoms. Reinforcement is learning that occurs when the child receives positive or negative reactions of the parent to the child’s symptoms.
Peer-review
This is an interesting article looking at the relationship between maternal and child somatic symptoms in the setting of IBS.
Footnotes
Supported by NIH, No. RO1 HD36069, No. RO1 DK31369, and No. R24 67674.
Ethics approval: This study was reviewed and approved by the Institutional Review Boards of Group Health Cooperative, the University of Washington, and the University of North Carolina.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: August 23, 2014
First decision: September 27, 2014
Article in press: December 22, 2014
P- Reviewer: McCloskey K S- Editor: Yu J L- Editor: AmEditor E- Editor: Liu XM
References
- 1.Levy RL, Whitehead WE, Walker LS, Von Korff M, Feld AD, Garner M, Christie D. Increased somatic complaints and health-care utilization in children: effects of parent IBS status and parent response to gastrointestinal symptoms. Am J Gastroenterol. 2004;99:2442–2451. doi: 10.1111/j.1572-0241.2004.40478.x. [DOI] [PubMed] [Google Scholar]
- 2.Levy RL, Whitehead WE, Von Korff MR, Feld AD. Intergenerational transmission of gastrointestinal illness behavior. Am J Gastroenterol. 2000;95:451–456. doi: 10.1111/j.1572-0241.2000.01766.x. [DOI] [PubMed] [Google Scholar]
- 3.Levy RL, Jones KR, Whitehead WE, Feld SI, Talley NJ, Corey LA. Irritable bowel syndrome in twins: heredity and social learning both contribute to etiology. Gastroenterology. 2001;121:799–804. doi: 10.1053/gast.2001.27995. [DOI] [PubMed] [Google Scholar]
- 4.Locke GR, Zinsmeister AR, Talley NJ, Fett SL, Melton LJ. Familial association in adults with functional gastrointestinal disorders. Mayo Clin Proc. 2000;75:907–912. doi: 10.4065/75.9.907. [DOI] [PubMed] [Google Scholar]
- 5.Morris-Yates A, Talley NJ, Boyce PM, Nandurkar S, Andrews G. Evidence of a genetic contribution to functional bowel disorder. Am J Gastroenterol. 1998;93:1311–1317. doi: 10.1111/j.1572-0241.1998.440_j.x. [DOI] [PubMed] [Google Scholar]
- 6.Whitehead WE, Winget C, Fedoravicius AS, Wooley S, Blackwell B. Learned illness behavior in patients with irritable bowel syndrome and peptic ulcer. Dig Dis Sci. 1982;27:202–208. doi: 10.1007/BF01296915. [DOI] [PubMed] [Google Scholar]
- 7.Whitehead WE, Crowell MD, Heller BR, Robinson JC, Schuster MM, Horn S. Modeling and reinforcement of the sick role during childhood predicts adult illness behavior. Psychosom Med. 1994;56:541–550. doi: 10.1097/00006842-199411000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Walker LS, Claar RL, Garber J. Social consequences of children’s pain: when do they encourage symptom maintenance? J Pediatr Psychol. 2002;27:689–698. doi: 10.1093/jpepsy/27.8.689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Levy RL. Exploring the intergenerational transmission of illness behavior: from observations to experimental intervention. Ann Behav Med. 2011;41:174–182. doi: 10.1007/s12160-010-9254-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Levy RL, Langer SL, Walker LS, Romano JM, Christie DL, Youssef N, DuPen MM, Feld AD, Ballard SA, Welsh EM, et al. Cognitive-behavioral therapy for children with functional abdominal pain and their parents decreases pain and other symptoms. Am J Gastroenterol. 2010;105:946–956. doi: 10.1038/ajg.2010.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Levy RL, Langer SL, Whitehead WE. Social learning contributions to the etiology and treatment of functional abdominal pain and inflammatory bowel disease in children and adults. World J Gastroenterol. 2007;13:2397–2403. doi: 10.3748/wjg.v13.i17.2397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Koloski NA, Boyce PM, Talley NJ. Is health care seeking for irritable bowel syndrome and functional dyspepsia a socially learned response to illness? Dig Dis Sci. 2005;50:153–162. doi: 10.1007/s10620-005-1294-9. [DOI] [PubMed] [Google Scholar]
- 13.Crane C, Martin M. Social learning, affective state and passive coping in irritable bowel syndrome and inflammatory bowel disease. Gen Hosp Psychiatry. 2004;26:50–58. doi: 10.1016/j.genhosppsych.2003.07.005. [DOI] [PubMed] [Google Scholar]
- 14.Lowman BC, Drossman DA, Cramer EM, McKee DC. Recollection of childhood events in adults with irritable bowel syndrome. J Clin Gastroenterol. 1987;9:324–330. doi: 10.1097/00004836-198706000-00017. [DOI] [PubMed] [Google Scholar]
- 15.Crane C, Martin M. Illness-related parenting in mothers with functional gastrointestinal symptoms. Am J Gastroenterol. 2004;99:694–702. doi: 10.1111/j.1572-0241.2004.04137.x. [DOI] [PubMed] [Google Scholar]
- 16.Claar RL, Simons LE, Logan DE. Parental response to children’s pain: the moderating impact of children’s emotional distress on symptoms and disability. Pain. 2008;138:172–179. doi: 10.1016/j.pain.2007.12.005. [DOI] [PubMed] [Google Scholar]
- 17.Simons LE, Claar RL, Logan DL. Chronic pain in adolescence: parental responses, adolescent coping, and their impact on adolescent’s pain behaviors. J Pediatr Psychol. 2008;33:894–904. doi: 10.1093/jpepsy/jsn029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Logan DE, Simons LE, Carpino EA. Too sick for school? Parent influences on school functioning among children with chronic pain. Pain. 2012;153:437–443. doi: 10.1016/j.pain.2011.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sieberg CB, Williams S, Simons LE. Do parent protective responses mediate the relation between parent distress and child functional disability among children with chronic pain? J Pediatr Psychol. 2011;36:1043–1051. doi: 10.1093/jpepsy/jsr043. [DOI] [PubMed] [Google Scholar]
- 20.Guite JW, McCue RL, Sherker JL, Sherry DD, Rose JB. Relationships among pain, protective parental responses, and disability for adolescents with chronic musculoskeletal pain: the mediating role of pain catastrophizing. Clin J Pain. 2011;27:775–781. doi: 10.1097/AJP.0b013e31821d8fb4. [DOI] [PubMed] [Google Scholar]
- 21.Bennett EJ, Tennant CC, Piesse C, Badcock CA, Kellow JE. Level of chronic life stress predicts clinical outcome in irritable bowel syndrome. Gut. 1998;43:256–261. [Google Scholar]
- 22.Dancey CP, Taghavi M, Fox RJ. The relationship between daily stress and symptoms of irritable bowel: a time-series approach. J Psychosom Res. 1998;44:537–545. doi: 10.1016/s0022-3999(97)00255-9. [DOI] [PubMed] [Google Scholar]
- 23.Whitehead WE, Crowell MD, Robinson JC, Heller BR, Schuster MM. Effects of stressful life events on bowel symptoms: subjects with irritable bowel syndrome compared with subjects without bowel dysfunction. Gut. 1992;33:825–830. doi: 10.1136/gut.33.6.825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Boey CC, Goh KL. The significance of life-events as contributing factors in childhood recurrent abdominal pain in an urban community in Malaysia. J Psychosom Res. 2001;51:559–562. doi: 10.1016/s0022-3999(01)00232-x. [DOI] [PubMed] [Google Scholar]
- 25.Sharrer VW, Ryan-Wenger NM. Measurements of stress and coping among school-aged children with and without recurrent abdominal pain. J Sch Health. 1991;61:86–91. doi: 10.1111/j.1746-1561.1991.tb03243.x. [DOI] [PubMed] [Google Scholar]
- 26.Walker LS, Garber J, Smith CA, Van Slyke DA, Claar RL. The relation of daily stressors to somatic and emotional symptoms in children with and without recurrent abdominal pain. J Consult Clin Psychol. 2001;69:85–91. [PMC free article] [PubMed] [Google Scholar]
- 27.Dufton LM, Konik B, Colletti R, Stanger C, Boyer M, Morrow S, Compas BE. Effects of stress on pain threshold and tolerance in children with recurrent abdominal pain. Pain. 2008;136:38–43. doi: 10.1016/j.pain.2007.06.012. [DOI] [PubMed] [Google Scholar]
- 28.Thompson WG, Longstreth GF, Drossman DA, Heaton KW, Irvine EJ, Müller-Lissner SA. Functional bowel disorders and functional abdominal pain. Gut. 1999;45 Suppl 2:II43–II47. doi: 10.1136/gut.45.2008.ii43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Drossman DA, Richter JE, Talley NJ, Thompson WG, Corazziari E, Whitehead WE. The Functional Gastrointestinal Disorders. Boston: Little, Brown and Company; 1994. [Google Scholar]
- 30.Van Slyke DA, Smith CA, Waker LS, Garber J. The development and validation of the Children’s Pain Belief Questionnaire. Child Health Psychology Conference: Gainsville, Florida; 1997. [Google Scholar]
- 31.Walker LS, Smith CA, Garber J, Claar RL. Testing a model of pain appraisal and coping in children with chronic abdominal pain. Health Psychol. 2005;24:364–374. doi: 10.1037/0278-6133.24.4.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Walker LS, Smith CA, Garber J, Van Slyke DA. Development and validation of the Pain Response Inventory for children. Psychol Assessmen. 1997;9:392–405. [Google Scholar]
- 33.Walker LS, Garber J, Greene JW. Somatization symptoms in pediatric abdominal pain patients: relation to chronicity of abdominal pain and parent somatization. J Abnorm Child Psychol. 1991;19:379–394. doi: 10.1007/BF00919084. [DOI] [PubMed] [Google Scholar]
- 34.Garber J, Walker LS, Zeman J. Somatization symptoms in a community sample of children and adolescents: Further validation of the Children’s Somatization Inventory. Psychol Assessment. 1991;3:588–595. [Google Scholar]
- 35.Powell H, Smart J, Wood LG, Grissell T, Shafren DR, Hensley MJ, Gibson PG. Validity of the common cold questionnaire (CCQ) in asthma exacerbations. PLoS One. 2008;3:e1802. doi: 10.1371/journal.pone.0001802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Walker LS, Garber J, Greene JW. Somatic complaints in pediatric patients: a prospective study of the role of negative life events, child social and academic competence, and parental somatic symptoms. J Consult Clin Psychol. 1994;62:1213–1221. doi: 10.1037//0022-006x.62.6.1213. [DOI] [PubMed] [Google Scholar]
- 37.Achenbach TM. Manual for the Child Behavior Checklist/4-18 and 1991 Profile. Burlington: VT University of Vermont Department of Psychiatry; 1991. [Google Scholar]
- 38.Derogatis LR, Cleary PA. Factorial invariance across gender for the primary symptom dimensions of the SCL-90. Br J Soc Clin Psychol. 1977;16:347–356. doi: 10.1111/j.2044-8260.1977.tb00241.x. [DOI] [PubMed] [Google Scholar]
- 39.McCubbin H, Patterson J, Wilson L. Family Inventory of Life Events and Changes (FILE) In: McCubbin HI, Thompson AI, McCubbin MA, editors. Family Assessment: Resiliency, coping and adaptation-inventories for research and practice. Madison: University of Wisconsin System; 1996. pp. 103–178. [Google Scholar]
- 40.Derogatis LR. NCS Pearson, Inc; 2000. BSI 18 Brief Symptom Inventory 18: Administration, scoring, and procedures manual. [Google Scholar]
- 41.Walker LS, Zeman JL. Parental response to child illness behavior. J Pediatr Psychol. 1992;17:49–71. doi: 10.1093/jpepsy/17.1.49. [DOI] [PubMed] [Google Scholar]
- 42.Van Slyke DA, Walker LS. Mothers’ responses to children’s pain. Clin J Pain. 2006;22:387–391. doi: 10.1097/01.ajp.0000205257.80044.01. [DOI] [PubMed] [Google Scholar]
- 43.Walker LS, Levy RL, Whitehead WE. Validation of a measure of protective parent responses to children’s pain. Clin J Pain. 2006;22:712–716. doi: 10.1097/01.ajp.0000210916.18536.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Palermo TM, Valrie CR, Karlson CW. Family and parent influences on pediatric chronic pain: a developmental perspective. Am Psychol. 2014;69:142–152. doi: 10.1037/a0035216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Drossman DA, Creed FH, Olden KW, Svedlund J, Toner BB, Whitehead WE. Psychosocial aspects of the functional gastrointestinal disorders. Gut. 1999;45 Suppl 2:II25–II30. doi: 10.1136/gut.45.2008.ii25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Garber J, Zeman J, Walker LS. Recurrent abdominal pain in children: psychiatric diagnoses and parental psychopathology. J Am Acad Child Adolesc Psychiatry. 1990;29:648–656. doi: 10.1097/00004583-199007000-00021. [DOI] [PubMed] [Google Scholar]
- 47.Beardslee WR, Gladstone TR, O’Connor EE. Transmission and prevention of mood disorders among children of affectively ill parents: a review. J Am Acad Child Adolesc Psychiatry. 2011;50:1098–1109. doi: 10.1016/j.jaac.2011.07.020. [DOI] [PubMed] [Google Scholar]
- 48.Bögels SM, Brechman-Toussaint ML. Family issues in child anxiety: attachment, family functioning, parental rearing and beliefs. Clin Psychol Rev. 2006;26:834–856. doi: 10.1016/j.cpr.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 49.van Tilburg MA, Palsson OS, Whitehead WE. Which psychological factors exacerbate irritable bowel syndrome? Development of a comprehensive model. J Psychosom Res. 2013;74:486–492. doi: 10.1016/j.jpsychores.2013.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]


