Abstract
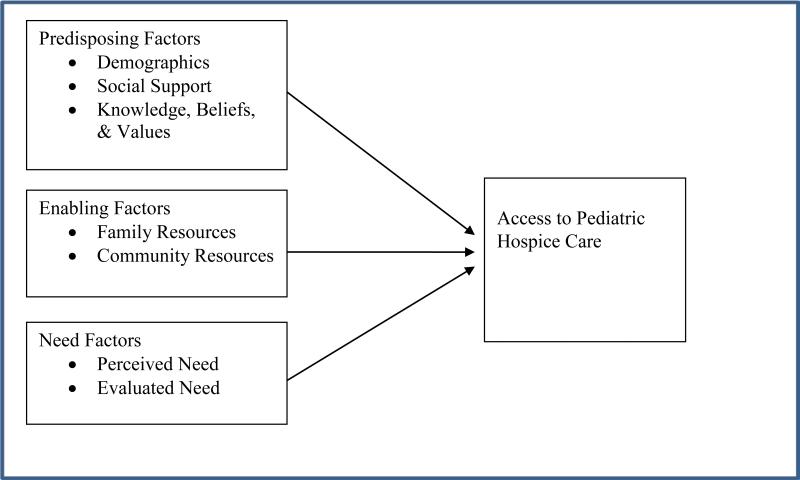
One of the many difficult moments for families of children with life-limiting illnesses is to make the decision to access pediatric hospice care. Although determinants that influence families’ decisions to access pediatric hospice care have been recently identified, the relationship between these determinants and access to pediatric hospice care have not been explicated or grounded in accepted healthcare theories or models. Using the Andersen Behavioral Healthcare Utilization Model, this article presents a conceptual model describing the determinants of hospice access. Predisposing (demographic; social support; and knowledge, beliefs, and values), enabling (family and community resources) and need (perceived and evaluated needs) factors were identified through the use of hospice literature. The relationships among these factors are described and implications of the model for future study and practice are discussed.
In the United States, approximately 44,000 children die each year.1 For those children whose deaths are attributed to health problems, families experience emotional turmoil as they must acknowledge that a child is terminally ill and dying. 2 The hope that a cure might still be an option slowly transitions to the reality of the child's impeding death.3 It is an emotional time as families seek the positive in the most current lab results while the child has stopped responding to treatment options. Individual values, parental understandings of the clinical situation, and the availability of options add to the complexity of decision making.4 The situation is often further complicated by the physician's inability to predict when a child may die because of the unique disease trajectories among pediatric conditions, which makes it difficult for physicians to conduct end-of-life conversations with families.5-7 As a consequence of this pediatric end-of-life experience, families are at increased risk for poor health-related8 and psychosocial9 related quality of life.
One of the many difficult moments for the family of a child with a life-limiting illness is to make the decision to access pediatric hospice care. Pediatric hospice care is a program of care that includes physical, emotional, social, and spiritual support services provided by an interdisciplinary health-care team for children and their families at the child's end of life.10 Enrollment into hospice care requires that children have a life expectancy of six months or less as certified by a hospice medical director, attending physician, or nurse practitioner.11 In addition, the recent passage of Concurrent Care for Children under the Affordable Care Act, has eliminated the hospice enrollment requirement that children and families discontinue curative treatment upon entering hospice.12 While enrolled in hospice, children generally receive care that reduces suffering from pain and other symptoms and improves quality of end of life.13.14 In addition, families are generally satisfied with the services provided for their children and the family support offered, such as bereavement and respite services.15
Recent qualitative studies have begun to identify common determinants that influence families’ decisions to access pediatric hospice care. Physician prognosis and comorbid conditions,3,16 community support,16 financial hardship, 17,18 and the child's suffering3,18 all contribute to the families’ decision making at the child's end of life. However, the relationship between these determinants and access to pediatric hospice care have not been explicated or grounded in accepted healthcare theories or models. A conceptual model is often used for this purpose: to summarize and integrate knowledge, define concepts, and provide explanations for causal linkages.19 Although several adult end-of-life conceptual models have been developed,20-22 there has been no exploration of the determinants linked to families’ decisions to access pediatric hospice care. Developing a multifactorial conceptual model to explain access to pediatric hospice is important for advancing the science of quality pediatric end of life care by providing a foundation for further model testing and for developing interventions aimed at improving family decision making.
Two questions are addressed in this article: (1) Can families’ decisions to access pediatric hospice care be predicted? and (2) How can models of healthcare access be used to guide pediatric hospice research and clinical practice? The main objectives of this research were to develop and justify a conceptual model that explicated the relationships between determinants and a family's decision to access hospice care for their child. This article is organized into two sections. The first section synthesizes the literature from adult and pediatric hospice care and develops a model to explain why families may access pediatric hospice care. The second section discusses future research and the implications for clinical practice.
Model Development
Background
The question posed by this study was: What determinants affect parental decision making to access (or not access) pediatric hospice care. As one of the most frequently used frameworks to examine healthcare utilization, the Andersen Behavioral Healthcare Utilization Model is relevant to this question.23,24 The Andersen Model suggests that there are three primary determinants of healthcare service utilization: (1) predisposing factors (demographics; position within social structure; and health knowledge, beliefs, and values); (2) enabling factors (financial and physical access to healthcare services); and (3) need factors (evaluated and self-perceived health status).25,26 These factors are considered the most immediate and important causes of healthcare utilization.23
Conceptual Model
The present study adapts the Andersen Model to examine the relationship among determinants and pediatric hospice access. The framework presented in Figure 1 stresses that predisposing, enabling, and need factors influence the decision of families to access pediatric hospice care. This study draws on the adult and pediatric hospice literature to explicate the relationships between the determinants of the child and family and how those may predict the use of pediatric hospice care services.
Figure 1.
Proposed Conceptual Model of Access to Pediatric Hospice Care
Predisposing factors
Predisposing factors are defined as socio-cultural characteristics of children and families that exist prior to accessing pediatric hospice care.26 These include demographics; social structures; and health knowledge, beliefs, and values.
Demographics refer to the age and gender of children. From an Andersen Model perspective, demographics represent biological imperatives associated with accessing pediatric hospice care.23,27,28 Although infants under one year of age have the highest mortality of any pediatric age group,1 their parents infrequently admit them to hospice care.29,30 One reason is that the new parent may be uncomfortable caring for a terminally ill baby at home, away from the Neonatal Intensive Care Unit (NICU). The NICU has the equipment, supplies, and trained nursing staff to monitor and care for these medically fragile infants,31 whereas parents may feel unprepared and unsure delivering complicated medical care such as ventilator support for an infant, especially if this is their first child, even with the support of a hospice team at home.32 Thus, demographics may play an important role in determining whether or not families access hospice care for their child.
Social structures include the education, ethnicity, social networks, social interactions, and culture that are inherent in the family and affect whether parents access pediatric hospice care.23,27,33 As an example, African American families continue to have low hospice utilization, which is often attributed to their racialized experience with the healthcare system.34-39 On the other hand, Hispanic families have been shown recently to be using the social structures such as strong kinship networks within Hispanic communities to navigate the healthcare system, resulting in increased healthcare utilization, including pediatric hospice care.33,40 As a result, social structures may be a determinant of parental decision making to access pediatric hospice care.
The Andersen Model suggests that the knowledge, beliefs, and values that families have about health and the healthcare system also influence pediatric hospice utilization.23 Parental healthcare knowledge may increase healthcare service access because information about services, location, and providers enables parents to make informed decisions about care access.41 More specifically, mothers may play a critical role in gathering information and articulating the family's beliefs and values, influencing whether or not hospice care is accessed. 42 In the case of pediatric hospice, it is common for terminally ill children to receive home healthcare in the early phase of their illness,10 which includes skilled nursing services, skilled therapy services, medical social services, medical supplies, and durable medical equipment.43 Of the approximately 14,500 home health and hospice agencies in 2007, 10% or 1,450 of home health agencies provide both home health and hospice care.44 It is also estimated that less than 30% of hospices provide pediatric care.45 Families who use home health care may be able learn about pediatric hospice services offered by these agencies. Therefore, if children and their families become aware of the hospice care services while in home health care, they may be more likely to transition the child to hospice as the child's health deteriorates.
Enabling factors
Enabling factors refer to family and community resources that must be available and accessible to families and children in order for them to access pediatric hospice care.
Family Resources
The Andersen Model suggests that family resources are the means and know how to access hospice services.23 Family resources may include family income, health insurance, and transportation. When families have a terminally ill child, many experience the financial hardship associated with trips to the doctor, out-of-pocket expenses, and overnight travel to hospitals.17,18 Health insurance is a mechanism by which some families are able to afford hospice care, whether it be private insurance or public insurance (e.g., Medicaid, Medicare, CHIP).33, 46-50 Insurance may mitigate the financial burden these families encounter by covering medical services, medical transportation, and equipment and supplies. Under most insurance plans, hospices cover these costs at no additional out-of-pocket expense to the family. Thus, family resources may enable families to access pediatric hospice care, and the lack of certain resources may prohibit families from accessing hospice.
Community Resources
The resources in the community are also important for families as they decide to access pediatric hospice care.17 Community resources such as available pediatric hospices and pediatric hospice staff in their particular location may be a critical component in whether or not families can even access pediatric hospice care.51-54 Children who reside outside the general hospice service area of pediatric providers cannot use that hospice's services. Although adult hospices are common in most communities in the United States,55 many areas have an inadequate supply of pediatric providers.56 One of the critical barriers to providing pediatric care is a lack of trained pediatric hospice staff.57 Pediatric hospice care necessitates that staff have specialized knowledge of pediatric health conditions, medications, and procedures,58 which are lacking on many locations. Therefore, the availability of community resources may be important for parents to actually access pediatric hospice care.
Need factors
Finally, families must recognize that there is a need in order for them to use pediatric hospice care services. Establishing a need for hospice may be based on how children and families view the child's health (perceived) as well as professional judgment about health status (evaluated).25
Perceived Need
Perceived need refers to how children and families view the general health and functional state of the child, as well as how children experience symptoms of illness and pain and whether or not the family judges the child's problems to be of sufficient magnitude to seek hospice.25 Children at end of life often have comorbidities, or additional health conditions, along with their primary diagnosis.30 For example, the disease progression among children with central nervous system tumors often includes neurological deficits, paralysis, cognitive deterioration, and behavioral alterations.59 At the end of life, these children typically experience multiple body function failures that often include uncontrolled pain, shortness of breath, and fatigue.60 At these times, many families express that they believe their child is suffering and they want to make the suffering stop.3, 18 Hospice is a care option that specializes in managing pain and other symptoms in complex medical cases such as those with multiple comorbidities.36, 48, 61, 62 As such, parents may perceive a need to access pediatric hospice care based on the comorbidities of a child.
Evaluated Need
Evaluated need represents professional medical judgment about a child's health status and the child's need for medical care.25 Children are commonly diagnosed with neuromuscular problems, cardiovascular conditions, and cancer at end of life.30 The treating physician is often the healthcare provider who will make the referral to hospice care in consultation with the family;3,16 however, determining a child's prognosis is complicated because the disease trajectories for children are generally unpredictable.63 Predicting the last 6 months of a child's life, as required by hospice admission rules, is often difficult. Given the complexity of a child's diagnosis at end of life, parents may rely on the best medical judgment of the treating physician to suggest when is the appropriate time for hospice care,3 or they may use their own intuition and judgment of the child's disease progression to decide when to access pediatric hospice care.18 Although there may be instances when the family's and physician's perception of imminent death conflict,64 parents report that when physicians provide health and prognosis information and advice, they are enabled to make autonomous decisions about their child's health care at end of life.65 Thus, the evaluated need based on the child’ diagnosis may be a critical determinant of pediatric hospice use.
Discussion
This article sought to address an important issue facing families with terminally ill children: What factors influence their decision to access pediatric hospice care? It developed a conceptual model based on the Andersen Behavioral Healthcare Utilization Model that captures the complex multifactorial determinants of accessing care. Families’ decisions to access pediatric hospice care may be affected by the predisposing, enabling, and need factors of the child and family.
The proposed framework is one of the first attempts to specify the determinants that are critical in predicting whether or not families will access pediatric hospice care. However, there are some limitations of the proposed conceptual model that can be viewed as research opportunities. First, the proposed constructs were not yet operationalized in the conceptual model. Although there is an abundance of healthcare literature that has operationalized the constructs of the Andersen Model, the predisposing, enabling, and need factors have not yet been proposed or validated in a pediatric hospice context. For example, there are challenges associated with measuring community resources. The service area of a pediatric hospice provider can vary from a specific county to a time or distance radius from the hospice office. For example, a recent study of California children who used hospice care showed that children and families generally had access to a pediatric hospice providers in their county. 66 On the other hand, children who died with a cancer diagnosis in Tennessee were found to lack access to pediatric hospice providers.56 Thus, it may be difficult to accurately compare hospice availability between states. The constructs of the model may pose challenges to researchers due to the multiplicity of measurement choices. Future conceptual research should continue to explicate these constructs.
Second, this model only demonstrates potential linear relationships of the determinants of access to pediatric hospice care. Some authors have argued that the predisposing, enabling, and need factors may interact with each other and influence utilization.67 As an example, family social supports may enhance a family's knowledge, beliefs, and values about health care. On the other hand, a lack of family resources may attenuate the families’ perceived need for pediatric hospice care. Hypothesis testing with interactions or moderating variables provides knowledge about the direction and/or strength of the relationships between different factors of interest and whether or not families access pediatric hospice care.68 Further analytical research that tests the conceptual model with interactions may provide important insight into the complex nature of family decision making for children with terminal illnesses.
Despite its drawbacks, the model suggests actionable practices by nurses to engage and support families in their decision-making process about accessing pediatric hospice care. Community resources are an example. As part of the discharge process, nurses can identify pediatric hospice providers that may assist families in understanding their options because pediatric hospices vary in the services offered.69 Healthcare professionals rarely know where pediatric hospice are located in their community and that lack of knowledge can be intensified when children and families are from out-of-state.70 Developing a resource list of pediatric hospice providers may aide families in the discharge planning process. Information on pediatric providers is often available from state Departments of Health. In addition, pediatric hospices can be identified with the assistance of pediatric end-of-life advocacy groups such as Children's Hospice and Palliative Care Coalition in California or the National Hospice and Palliative Care Organization Children's Project on Palliative/Hospice Services. Connecting with online hospice communities such as www.pallimed.org may also offer information on pediatric providers. Finally, emerging technology resources such as hospice mobile apps may identify hospice providers who offer pediatric services and map where they are located.71 Nurses have an opportunity to improve the quality of end-of-life care by educating families about resources at this difficult time.
In summary, the goal of this study was to develop a conceptual model based on the Andersen Behavioral Healthcare Utilization Model that describes how families make the decision to access pediatric hospice care. As one of the first conceptual explanations of the determinants of accessing pediatric hospice care, the Andersen Model appears to provide a useful framework for future studies examining the determinants that may influence a family's decision to access hospice care for their terminally ill child, developing cases studies of children and families accessing hospice care, and understanding trends in access to hospice care. The conceptual model proposed in this analysis provides an important conceptual foundation from which future empirical research can be developed and clinical practice enhanced.
Acknowledgement
Special thanks to Beth Schewe for her assistance with the manuscript.
Funding: This publication was made possible by Grant Number K01NR014490 from the National Institute of Nursing Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institute of Nursing Research or National Institutes of Health.
Footnotes
Declaration of Conflict of Interest:
The authors declares no conflicts of interest with respect to the authorship and/or publication of this article.
References
- 1.Hamilton BE, Hoyert DL, Martin JA, Strobino DM, Guyer B. Annual summary of vital statistics: 2010-2011. Pediatr. 2013;131(3):548–558. doi: 10.1542/peds.2012-3769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Steele R, Davies B. Impact on parents when a child has a progressive, life-threatening illness. International J Palliat Nurs. 2006;12(12):576–585. doi: 10.12968/ijpn.2006.12.12.22544. [DOI] [PubMed] [Google Scholar]
- 3.Hinds PS, Schum L, Baker JN, Wolfe J. Key factors affecting dying children and their families. J Palliat Med. 2005:8, S70–S78. doi: 10.1089/jpm.2005.8.s-70. [DOI] [PubMed] [Google Scholar]
- 4.Wolfe J, Klar N, Grier HE, Duncan J, Salem-Schatz S, Emanuel EJ, Weeks JC. Understanding of prognosis among parents of children who died of cancer: impact on treatment goals and integration of palliative care. JAMA. 2000;284:2469–2475. doi: 10.1001/jama.284.19.2469. [DOI] [PubMed] [Google Scholar]
- 5.Davies B, Sehring SA, Partridge J, Cooper B, Hughes A, Philp JC, Amidi-Nouri A, Kramer RF. Barriers to palliative care for children: Perceptions of pediatric health care providers. Pediatr. 2008;121(2):282–288. doi: 10.1542/peds.2006-3153. [DOI] [PubMed] [Google Scholar]
- 6.Fowler K, Poehling K, Billheimer D, Hamilton R, Wu H, Mulder J, Frangoul H. Hospice referral practices for children with cancer: A survey of pediatric oncologists. J Clinic Oncol. 2006;24(7):1099–1104. doi: 10.1200/JCO.2005.02.6591. [DOI] [PubMed] [Google Scholar]
- 7.Sheetz M, Sontag-Bowman M. Pediatric palliative care: An assessment of physicians' confidence in skills, desire for training, and willingness to refer for end-of-life care. AM J Hospic Palliat Care. 2008;25(2):100–105. doi: 10.1177/1049909107312592. [DOI] [PubMed] [Google Scholar]
- 8.Song J, Floyd FJ, Seltzer MM, Greenberg JS, Hong J. Long-term effects of child death on parents' health-related quality of life: A dyadic analysis. Fam Rel. 2010;59:269–282. doi: 10.1111/j.1741-3729.2010.00601.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brosig CL, Pierucci RL, Kupst MJ, Leuthner SR. Infant end-of-life care: The parents' perspective. J Perinat. 2007;27(8):510–516. doi: 10.1038/sj.jp.7211755. [DOI] [PubMed] [Google Scholar]
- 10.Institute of Medicine . When children die: Improving palliative and end-of-life care for children and their families. National Academy Press; Washington, D.C.: 2003. [Google Scholar]
- 11.Bonebrake D, Culver C, Call K, Ward-Smith P. Clinically differentiating palliative care and hospice. Clinic J Oncol Nurs. 2010;14(3):273–275. doi: 10.1188/10.CJON.273-275. [DOI] [PubMed] [Google Scholar]
- 12.Lindley LC. Health Care Reform and Concurrent Curative Care for Terminally Ill Children: A Policy Analysis. J Hospic Palliat Nurs. 2011;13(2):81–88. doi: 10.1097/NJH.0b013e318202e308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Davies B, Brenner P, Orloff S, Sumner L, Worden W. Forum: Addressing spirituality in pediatric hospice and palliative care. J Palliat Care. 2002;18(1):59–67. [PubMed] [Google Scholar]
- 14.Dickens DS. Comparing pediatric deaths with and without hospice support. Pediatr Blood Cancer. 2010;54(5):746–750. doi: 10.1002/pbc.22413. [DOI] [PubMed] [Google Scholar]
- 15.Davies B, Steele R, Collins JB, Cook K, Smith S. The impact on families of respite care in a children's hospice program. J Palliat Care. 2004;20(4):277–286. [PubMed] [Google Scholar]
- 16.Heinze KE, Nolan MT. Parental decision making for children with cancer at the end of life: A meta-ethnography. J Pediatr Oncol Nurs. 2012;29:337–345. doi: 10.1177/1043454212456905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zelcer S, Cataudella D, Cairney A, Bannister S. Palliative care of children with brain tumors: A parental perspective. Arch Pediatr Adolesc Med. 2010;164(3):225–230. doi: 10.1001/archpediatrics.2009.284. [DOI] [PubMed] [Google Scholar]
- 18.Michelson KN, Koogler T, Sullivan C, Ortega Mdel P, Hall E, Frader J. Parental views on withdrawing life-sustaining therapies in critically ill children. Arch Pediatr Adolesc Med. 2009;163(11):986–992. doi: 10.1001/archpediatrics.2009.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Earp JA, Ennett ST. Conceptual models for health education research and practice. Health Ed Research. 1991;6:163–171. doi: 10.1093/her/6.2.163. [DOI] [PubMed] [Google Scholar]
- 20.Kelley ML. Developing rural communities' capacity for palliative care: A conceptual model. J Palliat Care. 2007;23:143–153. [PubMed] [Google Scholar]
- 21.Hudson P. A conceptual model and key variables for guiding supportive interventions for family caregivers of people receiving palliative care. Palliat Support Care. 2003;1:353–365. doi: 10.1017/s1478951503030426. [DOI] [PubMed] [Google Scholar]
- 22.Prince H, Kelley ML. Developing palliative care in First Nations communities: A conceptual model to guide program development. J Palliat Care. 2009;25:238. [Google Scholar]
- 23.Andersen R. A behavioral model of families' use of health services. Center for Health Administration Studies; Chicago, IL: 1968. [Google Scholar]
- 24.Babitsch B, Gohl D, von Lengerke T. Re-visiting Andersen's behavioral model of health services use: A systematic review of studies from 1998-2011. Psychosocial Med. 2012;9 doi: 10.3205/psm000089. epub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Andersen R. Revisiting the behavioral model and access to medical care: Does it matter? J Health Soci Behav. 1995;36:1–10. [PubMed] [Google Scholar]
- 26.Andersen R, Newman JF. Societal and individual determinates of medical care utilization in the United States. Milbank Mem Fund Qtrly. 1973;51:95–124. [PubMed] [Google Scholar]
- 27.Knapp C, Shenkman E, Marcu M, Madden V, Terza J. Pediatric palliative care: describing hospice users and identifying factors that affect hospice expenditures. J Palliat Med. 2009;12:1–7. doi: 10.1089/jpm.2009.9657. [DOI] [PubMed] [Google Scholar]
- 28.Lyon M, Williams P, Woods E, Hutton N, Butler A, Sibinga E, Brady M, Oleske J. Do-not-resuscitate orders and/or hospice care, psychological health, and quality of life among children/adolescents with acquired immune deficiency syndrome. J Palliat Med. 2008;11:459–469. doi: 10.1089/jpm.2007.0148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.National Hospice & Palliative Care Organization [January 1, 2010];2009NHPCO facts and figures: Pediatric palliative and hospice care in America. Available at: http://www.nhpco.org/files/public/quality/Pediatric_Facts-Figures.pdf.
- 30.Lindley LC, Lyon ME. A profile of children with complex chronic conditions at end of life among Medicaid-beneficiaries: Implications for healthcare reform. J Palliat Med. 2013;16(11):1388–1393. doi: 10.1089/jpm.2013.0099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Abe N, Catlin A, Mihara D. End of life in the NICU: A study of ventilator withdrawal. MCN Am J Matern Child Nurs. 2001;26(3):141–146. doi: 10.1097/00005721-200105000-00010. [DOI] [PubMed] [Google Scholar]
- 32.Pritchard M, Burghen EA, Gattuso JS, West NK, Gajjar P, Srivastava DK, et al. Factors that distinguish symptoms of most concern to parent from other symptoms of dying children. J Pain an Sympt Manag. 2010;39(4):627–636. doi: 10.1016/j.jpainsymman.2009.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Thienprayoon R, Lee SC, Leonard D, Winick N. Racial and ethnic difference in hospice enrollment among children with cancer. Pediat Blood Cancer. 2013;60:1662–1666. doi: 10.1002/pbc.24590. [DOI] [PubMed] [Google Scholar]
- 34.Colon M, Lyke J. Comparison of hospice use and demographics among European Americans, African Americans, and Latinos. Am J Hospic Palliat Care. 2003;20:182–190. doi: 10.1177/104990910302000306. [DOI] [PubMed] [Google Scholar]
- 35.Connor SR. Racial disparity in hospice use in the United States in 2002. Palliat Med. 2008;22:205–213. doi: 10.1177/0269216308089305. [DOI] [PubMed] [Google Scholar]
- 36.Givens JL, Tjia J, Zhou C, Emanuel E, Ash AS. Racial and ethnic differences in hospice use among patients with heart failure. Arch Intern Med. 2010;170:427–432. doi: 10.1001/archinternmed.2009.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hardy D, Chan W, Lie C, Cormier JN, Xia R, Bruera E, Du XL. Racial disparities in the use of hospice services according to geographic residence and socioeconomic status in an elderly cohort with non-small cell lung cancer. Cancer. 2011;117:1506–1515. doi: 10.1002/cncr.25669. [DOI] [PubMed] [Google Scholar]
- 38.Karikari-Martin P, McCann JJ, Hebert LE, Haffer SC, Phillips M. Do community and caregiver factors influence hospice use at the end of life among older adults with Alzheimer disease. J Hospic Palliat Nurs. 2012;14 doi: 10.1097/NJH.0b013e3182433a15. epub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kwak J, Haley WE, Chiriboga DA. Racial differences in hospice use and in-hospital death among Medicare and Medicaid dual-eligible nursing home residents. Geront. 2008;48:32–41. doi: 10.1093/geront/48.1.32. [DOI] [PubMed] [Google Scholar]
- 40.Gamoran A, Lopez-Turley RN, Turner A, Fish R. Differences between Hispanic and non-Hispanic families in social capital and child development: First-year findings from an experimental study. Res Soc Stratif Mobil. 2011;30:97–112. doi: 10.1016/j.rssm.2011.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fieldston ES, Nadel FM, Alpern ER, Fiks AG, Shea JA, Alessandrini EA. Effects of an education and training intervention on caregiver knowledge of non-urgent pediatric complaints and on child health services utilization. Pediatr Emerg Care. 2013;29:331–336. doi: 10.1097/PEC.0b013e31828512c7. [DOI] [PubMed] [Google Scholar]
- 42.Falnes EF, Tylleskar T, de Paoli MM, Manongi R, Pigeon ME. Mothers' knowledge and utilization of prevention of mother to child transmission services in northern Tanzania. J Intern AIDS Soc. 2010;13:36. doi: 10.1186/1758-2652-13-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hollywood J, Moore KJ. Medicare's new home health services requirements. Fam Practic Manage. 2011;18(3):8. [PubMed] [Google Scholar]
- 44.Parker-Lee EY, Decker FH. National Health Statistics Report. No. 30. National Center for Health Statistics; Hyattsville, MD: 2010. Comparison of home health and hospice care agencies by organizational characteristics and services provided: United States, 2007. [PubMed] [Google Scholar]
- 45.Lindley LC, Mark BA, Lee S-Y, Domino M, Song M, Jacobson-Vann J. Factors associated with the provision of pediatric hospice care. J Pain Sympt Manag. 2013;45(4):701–711. doi: 10.1016/j.jpainsymman.2012.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lackan NA, Ostir GV, Freeman JL, Kuo YF, Zhang DD, Goodwin JS. Hospice use by Hispanics and non-Hispanic white cancer decedents. Health Serv Res. 2004;39:969–983. doi: 10.1111/j.1475-6773.2004.00267.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lackan NA, Ostir GV, Freeman JL, Mahnken JD, Goodwin JS. Decreasing variation in the use of hospice among older adults with breast, colorectal, lung, and prostate cancer. Med Care. 2004;42:116–122. doi: 10.1097/01.mlr.0000108765.86294.1b. [DOI] [PubMed] [Google Scholar]
- 48.Mack JW, Chen K, Boscoe FP, Gestin FC, Roman PJ, Weeks JC, Schymura MJ, Schrag D. Underuse of hospice care by Medicaid-insured patients with stage IV lung cancer in New York and California. J Clinic Oncol. 2013;31:2569–2579. doi: 10.1200/JCO.2012.45.9271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.McCarthy EP, Burns RB, Ngo-Metzger Q, Davis RB, Phillips RS. Hospice use among Medicare managed care and fee-for-service patients dying with cancer. JAMA. 2003;289:2238–2245. doi: 10.1001/jama.289.17.2238. [DOI] [PubMed] [Google Scholar]
- 50.Virnig BA, Fischer ES, McBean AM, Kind S. Hospice use in Medicare managed care and fee-for-service systems. AM J Manag Care. 2001;7:777–786. [PubMed] [Google Scholar]
- 51.Carlson M, Bradley E, Du Q, Morrison S. Geographic access to hospice in the United States. J Palliat Med. 2010;13:1331–1338. doi: 10.1089/jpm.2010.0209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jenkins T, Chapman K, Harshbarger D, Townsend J. Hospice use among cancer decedents in Alabama, 2002-2005. Prevent Chronic Dis. 2009;6:1–8. [PMC free article] [PubMed] [Google Scholar]
- 53.Madigan EA, Wiencek CA, Vander Schrier AL. Patterns of community-based end-of-life care in rural areas of the united states. Polic Politic, Nurs Pract. 2009;10:71–81. doi: 10.1177/1527154409333861. [DOI] [PubMed] [Google Scholar]
- 54.Virnig B, Ma H, Hartman L, Moscovice I, Carlin B. Access to home-based hospice care for rural populations: Identification of areas lacking service. J Palliat Med. 2006;9:1292–1299. doi: 10.1089/jpm.2006.9.1292. [DOI] [PubMed] [Google Scholar]
- 55.Thompson JW, Carlson MD, Bradley EH. US hospice industry experienced considerable turbulence from changes in ownership, growth, and shift to for-profit status. Health Aff. 2012;31(6):1286–1293. doi: 10.1377/hlthaff.2011.1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lindley LC, Edwards SL. Geographic access to hospice care for children with cancer in Tennessee, 2009 to 2011. Am J Hospic Palliat Med. 2014 doi: 10.1177/1049909114543641. Epub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sanchez-Varela AM, Deal AM, Hanson LC, et al. Barriers to hospice for children as perceived by hospice organizations in North Carolina. Am J Hospic Palliat Med. 2012;29:171–6. doi: 10.1177/1049909111412580. [DOI] [PubMed] [Google Scholar]
- 58.Lindley LC. Pediatric hospice care knowledge: A transaction cost perspective. JHPN. 2013;15(8):485–490. [Google Scholar]
- 59.Vallero SG, Lijoi S, Bertin D, Pittana LS, Bellini S, Rossi F, Peretta P, Basso ME, Fagioli F. End-of-Life Care in Pediatric Neuro-Oncology. Pediatr Blood cancer. 2014;61:2004–2011. doi: 10.1002/pbc.25160. [DOI] [PubMed] [Google Scholar]
- 60.Hendricks-Ferguson V. Physical symptoms of children receiving pediatric hospice care at home during the last week of life. Oncol Nurs For. 2008;35(6):e108–e115. doi: 10.1188/08.onf.e108-e115. [DOI] [PubMed] [Google Scholar]
- 61.Keating NL, Herrinton LJ, Zaslavsky AM, Liu L, Ayanian JZ. Variations in hospice use among cancer patients. J NCI. 2006;98:1053–1059. doi: 10.1093/jnci/djj298. [DOI] [PubMed] [Google Scholar]
- 62.Keating NL, Landrum MB, Guadagnoli E, Winer EP, Ayanian JZ. Care in the months before death and hospice enrollment among older women with advanced breast cancer. J Gen Intern Med. 2007;23:11–18. doi: 10.1007/s11606-007-0422-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Himelstein B. Palliative care for infants, children, adolescents, and their families. J Palliat Med. 2006;9(1):163–181. doi: 10.1089/jpm.2006.9.163. [DOI] [PubMed] [Google Scholar]
- 64.Davies B, Sehring SA, Partridge J, Cooper B, Hughes A, Philp JC, Amidi-Nouri A, Kramer RF. Barriers to palliative care for children: Perceptions of pediatric health care providers. Pediatr. 2008;121(2):282–288. doi: 10.1542/peds.2006-3153. [DOI] [PubMed] [Google Scholar]
- 65.Sullivan J, Monagle P, Gillam L. What parents want from doctors in edn0of0life decision-making for children. Arch Dis Child. 2014;99:216–20. doi: 10.1136/archdischild-2013-304249. [DOI] [PubMed] [Google Scholar]
- 66.Lindley LC, Shaw S-L. Who are the children enrolled in hospice care? J Special Pediatr Nurs. 2014;19(4):308–315. doi: 10.1111/jspn.12085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Davis MA, Weeks WB, Coulter ID. A proposed conceptual model for studying the use of complementary and alternative medicine. Alt Ther. 2011;17(5):32–36. [PubMed] [Google Scholar]
- 68.Baron R, Kenny D. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psy. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 69.Lindley LC. Trends in services among pediatric hospice providers during 2002 to 2008. Am J Hospic Palliat Med. 2013;30(1):68–74. doi: 10.1177/1049909112444001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Thompson LA, Knapp C, Madden V, Shenkman E. Pediatricians' perceptions of and preferred timing for pediatric palliative care. Pediatr. 2009;123(5):e777–e782. doi: 10.1542/peds.2008-2721. [DOI] [PubMed] [Google Scholar]
- 71.Lindley LC, Zhou W, Mack JW, Li X. Pediatric hospice and palliative care: Designing a mobile app for clinical practice. CIN: Plus. 2014;32(7):299–302. doi: 10.1097/CIN.0000000000000084. [DOI] [PMC free article] [PubMed] [Google Scholar]