Abstract
Background
Urinary tract infections (UTIs) are common drivers of antibiotic use. The minimal effective duration of antibiotic therapy for UTIs is unknown, but any reduction is important to diminish selection pressure for antibiotic resistance, costs, and drug-related side-effects. The aim of this study was to investigate whether an algorithm based on procalcitonin (PCT) and quantitative pyuria reduces antibiotic exposure.
Methods
From April 2012 to March 2014, we conducted a factorial design randomized controlled open-label trial. Immunocompetent adults with community-acquired non-catheter-related UTI were enrolled in the emergency department of a tertiary-care 600-bed hospital in northwestern Switzerland. Clinical presentation was used to guide initiation and duration of antibiotic therapy according to current guidelines (control group) or with a PCT-pyuria-based algorithm (PCT-pyuria group).
The primary endpoint was overall antibiotic exposure within 90 days. Secondary endpoints included duration of the initial antibiotic therapy, persistent infection 7 days after end of therapy and 30 days after enrollment, recurrence and rehospitalizations within 90 days.
Results
Overall, 394 patients were screened, 228 met predefined exclusion criteria, 30 declined to participate, and 11 were not eligible. Of these, 125 (76% women) were enrolled in the intention-to-treat (ITT) analysis and 96 patients with microbiologically confirmed UTI constituted the per protocol group; 84 of 125 (67%) patients had a febrile UTI, 28 (22%) had bacteremia, 5 (4%) died, and 3 (2%) were lost to follow-up. Overall antibiotic exposure within 90 days was shorter in the PCT-pyuria group than in the control group (median 7.0 [IQR, 5.0–14.0] vs. 10.0 [IQR, 7.0–16.0] days, P = 0.011) in the ITT analysis. Mortality, rates of persistent infections, recurrences, and rehospitalizations were not different.
Conclusions
A PCT-pyuria-based algorithm reduced antibiotic exposure by 30% when compared to current guidelines without apparent negative effects on clinical outcomes.
Trial registration
Current controlled trials ISRCTN13663741, date applied: 22/05/2012, date assigned: 03/07/2012, last edited: 28/01/2014.
Electronic supplementary material
The online version of this article (doi:10.1186/s12916-015-0347-y) contains supplementary material, which is available to authorized users.
Keywords: Antibiotic stewardship, Biomarker, Procalcitonin, Urinary tract infection
Background
Urinary tract infections (UTIs) are common drivers of antibiotic use and hospitalizations. In the United States, almost 10 million outpatients are diagnosed with UTIs each year [1], and UTIs account for 16% of all infectious disease-related hospitalizations and 6% of all infectious disease-related deaths [2]. Despite various prevention strategies, recurrent UTIs are very common [3].
Any reduction of antibiotic exposure is important to diminish selection pressure for antibiotic resistance, costs, and drug-related side-effects [4]. Current guidelines for antibiotic treatment duration of febrile UTI/pyelonephritis largely reflect expert opinion [5-8], as only few intervention studies compared different durations [9-13]. Most studies in this regard were performed to establish short-term therapy in uncomplicated simple UTIs [14,15]. Motivated by the emerging antibiotic resistance of uropathogens [16-18] and the ecological effects of antibiotics, the minimal effective duration of antibiotic therapy is being challenged [19], especially in the elderly, in whom UTIs are often over diagnosed and therefore over treated. The use of biomarkers might improve the management of patients with UTIs [20].
The biomarker procalcitonin (PCT) was established for antibiotic stewardship in respiratory tract infections [21,22] and sepsis [23]. As an indicator for systemic infections [24], it showed high prognostic value to predict bacteremia in patients with urosepsis [25]. In the PRORATA trial, which documented a safe reduction of antibiotic usage through a PCT-guided strategy in patients with sepsis, UTIs were the source of infection in 7% of patients [26]. In patients with lower UTIs, PCT may need to be complemented with inflammatory surrogates of local infection such as pyuria. Normalization of pyuria in the first days after initiation of therapy correlated with a successful outcome in women with lower UTIs [27]. Therefore, we assumed that an algorithm based on PCT and pyuria could safely reduce the duration of antibiotic therapy in patients with UTIs.
Methods
Design overview
We conducted an investigator-initiated, single-center, factorial design, randomized controlled (1:1) and open-label trial. Herein, we focus on the efficacy of an algorithm based on clinical symptoms, PCT, and pyuria to safely reduce the duration of antibiotic therapy compared to current guidelines [6,15,28]. Details of the full trial design and methods have been published elsewhere [29].
The trial was conducted in accordance with the ethical principles of the Helsinki Declaration. The local ethical review committee of the Canton Aargau, Switzerland, approved the study protocol. All patients or their next-of-kin provided written informed consent.
Setting and participants
From April 2012 to March 2014, we screened all consecutive immunocompetent adults with community-acquired non-catheter-related UTIs as the main diagnosis presenting to the emergency department of the cantonal hospital of Aarau, a tertiary-care 600-bed hospital in northwestern Switzerland.
A UTI was defined by at least one clinical symptom (temperature ≥38.0°C, urinary urgency, dysuria, suprapubic pain, flank pain, costovertebral angle tenderness, nausea, and vomiting) and one urinary criterion (pyuria >20 leukocytes/μL, obtained by flow cytometry UF1000i (Sysmex) [27,30], and/or evidence of nitrite). Presence of flank pain, costovertebral angle tenderness, and/or a body temperature ≥38.0°C defined a ‘febrile UTI/pyelonephritis’; otherwise, patients were considered to have a ‘simple UTI’. The criteria for a ‘complicated UTI’ included any patient of at least 70 years, male gender, duration of symptoms of more than 7 days, previous antibiotic therapy within 30 days, at least two prior UTIs in the last 6 months or at least three during the last 12 months, any urologic intervention within 30 days, functional or anatomic abnormality, diabetes mellitus, or immunosuppressive therapy; otherwise it was referred to as an ‘uncomplicated UTI’.
Patients were excluded if they presented with other infections that required antibiotic therapy or had been treated with antibiotics within 48 hours before presentation; pregnancy; prostatitis defined as painful digital rectal examination, a prostate-specific antigen value of >4 ng/mL or ≥2× baseline before infection; foreign bodies within the urinary tract; endovascular prostheses; non-endovascular prostheses within 6 months after implantation; insufficient language skills with no possibility for translation; foreseeable non-compliance for follow-up, e.g., current drug abuse; severe immunodeficiency: neutrophils <500/μL, CD4 cells <350/μL in patients with HIV-infection, leukemia, lymphoma, myeloma, cytotoxic medications, hemodialysis, transplant patients; or life-threatening medical comorbidities leading to possible imminent death.
Randomization and interventions
The allocation of patients to either the PCT-pyuria group or the control group was based on a pre-specified computer generated randomization list and was concealed on the study website.
Clinical presentation without (control group) or with PCT and pyuria (PCT-pyuria group) was used to guide initiation and duration of antibiotic therapy. The choice of antibiotics and the minimal duration of therapy were based on recent guidelines [6,15]. The algorithm is presented in Figure 1.
Figure 1.
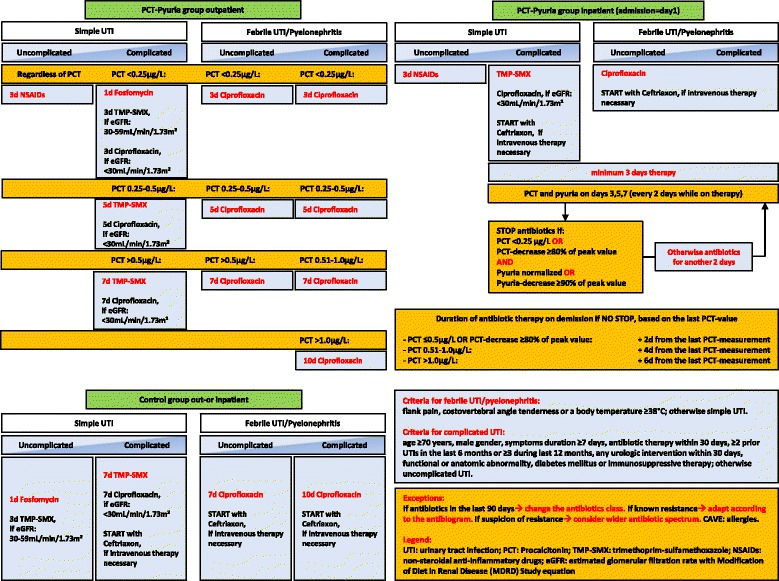
Algorithm for procalcitonin (PCT) and pyuria-guided therapy. TMP-SMX, Trimethoprim-sulfamethoxazole; NSAIDs, Non-steroidal anti-inflammatory drugs; eGFR, Estimated glomerular filtration rate with Modification of Diet in Renal Disease Study equation.
For simple UTIs, we used fosfomycin (3 g single dose) [31], trimethoprim-sulfamethoxazole (800/160 mg twice daily) for estimated glomerular filtration rates (eGFR) 30 to 59 mL/min/1.73 m2 or ciprofloxacin (250 mg twice daily) for eGFR <30 mL/min/1.73 m2. In the PCT-pyuria group, patients with uncomplicated simple UTIs were planned to receive only non-steroidal anti-inflammatory drugs (NSAIDs) for 3 days regardless of PCT-values [32,33].
For febrile UTIs/pyelonephritis, ciprofloxacin was chosen as standard oral treatment for better comparability with recent studies (500 mg orally twice daily, respectively ciprofloxacin 250 mg orally twice daily for eGFR <30 mL/min/1.73 m2), if intravenous therapy was necessary ceftriaxone (2 g once daily) was chosen. When known, antibiotic resistance profiles of prior or current pathogens were taken into account and antibiotic therapy was adjusted.
In inpatients in the PCT-pyuria group, antibiotic duration was based on absolute PCT-values and relative decreases of PCT-levels, as well as pyuria. PCT and pyuria were measured on admission in all patients; in hospitalized patients, the measurements were continued every other day till the end of antibiotic therapy. For outpatients in the PCT-pyuria group, antibiotic duration was calculated according to absolute values of PCT at baseline. In the control group, antibiotic therapy durations were recommended based on current guidelines [6,15] (Figure 1).
Urinalysis and urine culture with an antibiotic resistance profile were performed on admission. In patients with febrile UTI, blood cultures were taken prior to administration of antibiotics.
To determine microbiological cure and recurrence rates urinalysis and urine culture were performed on day 7 after end of therapy and day 30 after enrollment. Patients were instructed in collection of midstream urine for urinalysis and urine culture. These urine specimens were sent by mail and reached the laboratory within 48 hours.
Outcomes and follow-up
All endpoints were assessed at discharge from hospital and 30 and 90 days after enrollment through standardized telephone interviews by blinded members of the study team.
The primary endpoint was overall antibiotic exposure within 90 days. Each day of antibiotic therapy for any indication was counted as a full day of antibiotic exposure.
Secondary endpoints included duration of the initial antibiotic therapy; overall rate of recurrence, defined as any re-treated UTI; overall rate of rehospitalization for any cause within 90 days after enrollment; rate of persistent infection 7 days after end of therapy, defined as recovery of the initial uropathogen in the returned urine culture plus pyuria >20 leucocytes/μL in the concomitant urinalysis; and rate of persistent symptomatic infection 30 days after enrollment, defined as recovery of the initial uropathogen in the returned urine culture plus pyuria >20 leucocytes/μL in the concomitant urinalysis plus symptoms of an UTI in the 30 days phone interview.
All patients with positive urine cultures and pyuria in the follow-up samples were contacted by phone by members of the study team and advised to visit a general practitioner or an emergency room. The laboratory results were sent to the primary care providers when available, but no further guidance was given as to whether to prescribe an antibiotic.
Any serious adverse event, rehospitalization for any cause, recurrence, or death of any cause within 90 days after enrollment were monitored by the data safety and monitoring board, which consisted of three independent experts in infectious diseases, nephrology, and epidemiology.
Statistical analysis
The sample size was calculated assuming that duration of antibiotic therapy would be two days shorter in the PCT-pyuria group (8 days, standard deviation ±5) than in the control group (10 days, standard deviation ±5). Accordingly, 99 patients per arm would provide an 80% power at the 5% alpha level [29].
The primary analysis was performed including all randomized patients following an intention-to-treat (ITT) principle. The per-protocol (PP) analysis was performed in a defined population with microbiologically confirmed UTI and without patients who violated inclusion or exclusion criteria or were lost to follow-up. If the initial urine culture was missing, sterile, or contaminated but a uropathogen was isolated in concomitantly withdrawn blood cultures, the patients were still included in the PP analysis. We used predefined urine culture cut-offs for significance [29].
As the study was conceived in a two-by-two factorial design, we checked for interaction between the two randomization arms. As there was no evidence for interaction, the second randomization (proadrenomedullin-assisted site of care decision [29]) was no longer considered for this analysis.
Discrete variables were expressed as counts (percentage); continuous variables as medians and interquartile range, unless stated otherwise. For the analysis of the primary endpoint of antibiotic exposure, we used the Mann–Whitney U test for similarly shaped not normally distributed continuous data. In sensitivity analysis, we also used median regression to model the primary endpoint and adjusted the analysis for bacteremia. Logistic regression analyses of persistent infection, recurrence, and rehospitalization rates were performed to assess safety endpoints. Since this was a feasibility study we did not plan to have enough power for non-inferiority testing.
Results
We screened 394 patients, of whom 269 were not eligible due to the exclusion criteria, patient refusal, or other reasons. Thus, 125 patients were enrolled in the ITT analysis and 3 (2%) patients were lost to follow-up. As predefined, 96 (77%) patients with microbiologically confirmed UTIs and no protocol violations constituted the PP analysis (Figure 2).
Figure 2.
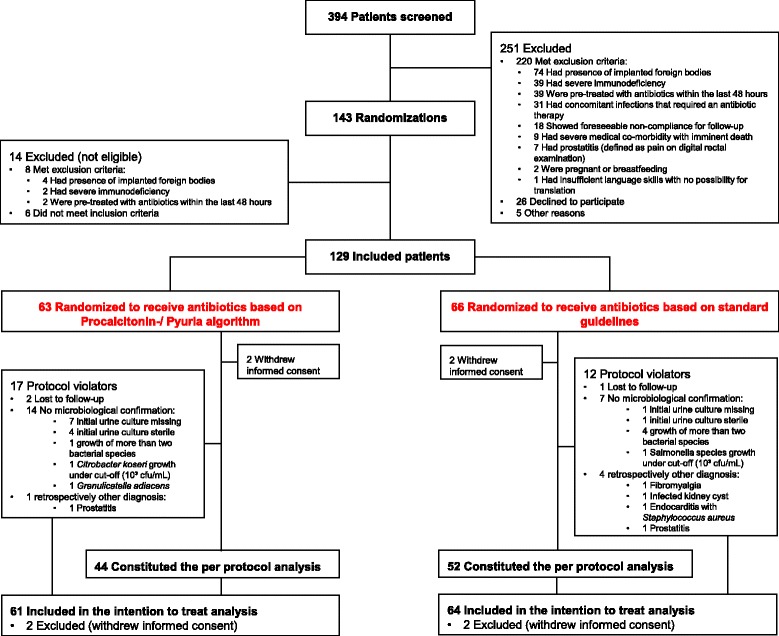
Flow diagram of patients in trial.
In five patients, the final diagnosis was retrospectively different from a UTI: one patient with an infected kidney cyst with Klebsiella oxytoca in blood cultures and two patients with prostatitis with Staphylococcus aureus in blood and urine cultures and with Escherichia coli in urine culture, respectively, received prolonged courses of antibiotics. One patient with severe sepsis due to Staphylococcus aureus endocarditis died during the initial hospitalization, and another patient was diagnosed with fibromyalgia syndrome as explanation for costovertebral angle tenderness and had a sterile urine culture.
The baseline characteristics were generally well-balanced except for the distribution of patients with bacteremia, namely 19 (30%) in the control group and 9 (15%) in the PCT-pyuria group (P = 0.045; Table 1); 95 (76%) of the 125 patients were women and 84 (67%) had a febrile UTI. The median age was 73 years (range, 19–96 years); 35 (28%) were treated as outpatients.
Table 1.
Baseline characteristics by randomization group
| Control group | PCT/Pyuria group | P value a | |
|---|---|---|---|
| n | 64 | 61 | |
| Demographics | |||
| Age, median (IQR), y | 75 (51–80) | 71 (44–81) | 0.65 |
| Females, n (%) | 52 (81%) | 43 (70%) | 0.16 |
| Charlson comorbidity index, median (IQR) | 4 (1-7) | 3 (0-6) | 0.20 |
| Clinical history, n (%) | |||
| Dysuria | 27 (42%) | 29 (48%) | 0.55 |
| Urinary urgency | 27 (43%) | 22 (36%) | 0.44 |
| Frequent urination | 23 (36%) | 24 (39%) | 0.69 |
| Flank pain | 20 (31%) | 21 (34%) | 0.71 |
| Clinical findings, median (IQR) | |||
| Confusion, n (%) | 16 (25%) | 13 (21%) | 0.63 |
| Body temperature, °C | 37.7 (36.9–38.6) | 38.2 (37.0–39.0) | 0.20 |
| Systolic blood pressure, mm Hg | 128 (110–145) | 120 (108–135) | 0.055 |
| Diastolic blood pressure, mm Hg | 69 (60–80) | 70 (60–79) | 0.85 |
| Respiratory rate, breaths/min | 16 (15–20) | 16 (14–18) | 0.18 |
| Laboratory findings, median (IQR) | |||
| Leukocyte count, × 109cells/L | 10.77 (7.83–14.34) | 12.28 (9.18–15.65) | 0.12 |
| C-reactive protein, mg/L | 34 (9–142) | 44 (7–131) | 0.84 |
| PCT, μg/L | 0.20 (0.08–1.34) | 0.32 (0.11–1.32) | 0.68 |
| PCT ≥0.25 μg/L, n (%) | 29 (45%) | 33 (54%) | 0.33 |
| Serum creatinine, μmol/L | 100 (77–136) | 93 (74–117) | 0.60 |
| Blood urea nitrogen, mmol/L | 6.5 (4.9–10.2) | 6.3 (4.6–9.3) | 0.64 |
| Bacteremic patients, n (%) | 19 (30%) | 9 (15%) | 0.045 |
| Final diagnosis, n (%) | |||
| Uncomplicated simple UTI | 6 (9%) | 2 (3%) | 0.36 |
| Complicated simple UTI | 12 (19%) | 16 (26%) | |
| Uncomplicated febrile UTI/pyelonephritis | 8 (13%) | 9 (15%) | |
| Complicated febrile UTI/pyelonephritis | 34 (53%) | 33 (54%) | |
| Other final diagnosisb | 4 (6%) | 1 (2%) | |
| Complicated UTI | 46 (72%) | 49 (80%) | 0.27 |
| Male patients | 12 (19%) | 18 (30%) | 0.16 |
| Patients older than or equal 70 years | 35 (55%) | 34 (56%) | 0.91 |
| Patients with symptoms longer than 7 days | 10 (16%) | 7 (12%) | 0.50 |
| Patients with antibiotic therapy in the last 30 days | 5 (8%) | 10 (16%) | 0.14 |
| Patients with diabetes | 16 (25%) | 8 (13%) | 0.092 |
| Patients with recurrent UTIs | 5 (8%) | 9 (15%) | 0.22 |
| Patients with urologic interventions in the last 30 days | 3 (5%) | 2 (3%) | 0.69 |
| Patients with anatomic abnormalities | 2 (3%) | 5 (8%) | 0.22 |
| Patients with immunosuppression | 0 | 2 (3%) | 0.14 |
| Patients from long-term healthcare facilities | 5 (8%) | 4 (7%) | 0.79 |
| Hospitalized patients, n (%) | 45 (70%) | 45 (74%) | 0.67 |
aχ2 test for categorical variables, 2-sample t-test for continuous variables.
bProstatitis (n = 2), infected kidney cyst (n = 1), endocarditis (n = 1), fibromyalgia syndrome (n = 1).
IQR, Interquartile range; y, Years.
Escherichia coli was identified in 72% of urine and blood culture isolates (Table 2). Ciprofloxacin and trimethoprim-sulfamethoxazole resistance in E. coli were 12% and 22%, respectively. In the PP analysis, the first-line antibiotic therapy was efficacious in 44% to 100%, as presented in Table 3.
Table 2.
Microbiological results at baseline
| Isolation of uropathogens in baseline urine culture | ||
|---|---|---|
| n (%) | Control group | PCT/Pyuria group |
| All patients (intention-to-treat) | (n = 64) | (n = 61) |
| Missing urine cultures | 2 (3%) | 8 (13%) |
| Sterile urine cultures | 4 (6%) | 4 (7%) |
| Contaminated urine cultures | 6 (9%) | 3 (5%) |
| Urine cultures with bacterial growth | 52 (82%) | 46 (75%) |
| Total no. of isolates a | 53 | 52 |
| Gram-negative uropathogen | ||
| Escherichia coli | 37/53 (70%) | 39/52 (75%) |
| Klebsiella pneumoniae | 6/53 (11%) | 3/52 (6%) |
| Citrobacter koseri | 0 | 1/52 (2%) |
| Pseudomonas aeruginosa | 0 | 1/52 (2%) |
| Proteus mirabilis | 0 | 1/52 (2%) |
| Gram-positive uropathogen | ||
| Enterococcus faecalis | 3/53 (6%) | 6/52 (12%) |
| Aerococcus urinae | 1/53 (2%) | 0 |
| Non uropathogen | ||
| Staphylococcus aureus | 3/53 (6%) | 0 |
| Lactobacillus speciesb | 2/53 (4%) | 0 |
| Granulicatella adiacens | 0 | 1/52 (2%) |
| Salmonella species | 1/53 (2%) | 0 |
| Isolation of uropathogens in baseline blood cultures | ||
| n (%) | Control group | PCT/Pyuria group |
| All patients (intention-to-treat) | (n = 64) | (n = 61) |
| Blood samples for culture obtained | 44 (69%) | 44 (72%) |
| No. (%) of contaminated blood cultures | 2/44 (5%) | 2/44 (5%) |
| Coagulase-negative staphylococci | 2/44 (5%) | 1/44 (2%) |
| Propionibacterium acnes | 0 | 1/44 (2%) |
| No. (%) of positive blood cultures | 19/44 (43%) | 9/44 (20%) |
| Gram-negative uropathogen | ||
| Escherichia coli | 14/19 (74%) | 9/9 (100%) |
| Klebsiella oxytoca | 1/19 (5%)c | 0 |
| Gram-positive uropathogen | ||
| Enterococcus faecalis | 1/19 (5%) | 0 |
| Non uropathogen | ||
| Staphylococcus aureus | 2/19 (11%)c | 0 |
| Lactobacillus species | 1/19 (5%) | 0 |
aTwo isolates in five cultures, three isolates in one culture.
bLactobacillus species was not a classical uropathogen but in one case confirmed by concomitant positive blood cultures with Lactobacillus species (4/4 samples).
cThree patients not included in the per protocol analysis with final diagnosis other than UTI: Klebsiella oxytoca in one patient with infected kidney cyst, Staphylococcus aureus in one patient with endocarditis, and one patient with prostatitis.
Table 3.
Initial antibiotic therapy by randomization group
| Control group | PCT/Pyuria group | |
|---|---|---|
| All patients (intention-to-treat) | (n = 64) | (n = 61) |
| First-line antibiotic therapy | ||
| Ciprofloxacin | 25 (39%) | 20 (33%) |
| Ceftriaxon | 18 (28%) | 18 (30%) |
| TMP-SMZ | 9 (14%) | 15 (25%) |
| Fosfomycin | 6 (9%) | 3 (5%) |
| Amoxicillin-Clavulanate | 5 (8%) | 1 (2%) |
| Other | 1 (2%) | 3 (5%) |
| NSAIDS | 0 | 1 (2%) |
| Second-line antibiotic therapy | ||
| Ciprofloxacin | 10 (16%) | 15 (25%) |
| Ceftriaxon | 4 (6%) | 4 (7%) |
| TMP-SMZ | 4 (6%) | 3 (5%) |
| Amoxicillin-Clavulanate | 4 (6%) | 3 (5%) |
| Other | 3 (5%) | 5 (8%) |
| Per-protocol population | (n = 52) | (n = 44) |
| First-line antibiotic therapy | ||
| Ciprofloxacin | 20 (38%), efficacious in 90% | 15 (34%), efficacious in 87% |
| Ceftriaxon | 17 (33%), efficacious in 76% | 14 (32%), efficacious in 64% |
| TMP-SMZ | 6 (12%), efficacious in 67% | 9 (20%), efficacious in 44% |
| Fosfomycin | 5 (10%), efficacious in 100% | 2 (5%), efficacious in 100% |
| Amoxicillin-Clavulanate | 3 (6%), efficacious in 67% | 1 (2%), efficacious in 100% |
| Other | 1 (2%) | 2 (4%) |
| NSAIDS | 0 | 1 (2%) |
| Second-line antibiotic therapy | ||
| Ciprofloxacin | 10 (19%), efficacious in 100% | 11 (25%), efficacious in 82% |
| Ceftriaxon | 3 (6%), efficacious in 67% | 4 (9%), efficacious in 100% |
| TMP-SMZ | 3 (6%), efficacious in 100% | 3 (7%), efficacious in 100% |
| Amoxicillin-Clavulanate | 4 (8%), efficacious in 100% | 2 (5%), efficacious in 100% |
| Other | 5 (10%) | 3 (7%) |
TMP-SMX, Trimethoprim-sulfamethoxazole; NSAIDs, Non-steroidal anti-inflammatory drugs.
Primary endpoint
The overall antibiotic exposure within 90 days was shorter in the PCT-pyuria group, both in the ITT analysis (7.0 vs. 10.0 days, P = 0.011) and in the PP analysis (7.0 vs. 10.0 days, P = 0.025) groups. In subgroup analyses, PCT-pyuria led to shorter antibiotic therapies in women (7.0 vs. 10.0 days, P = 0.022) and in patients with complicated febrile UTI/pyelonephritis (7.5 vs. 11.0 days, P = 0.002); for male patients, the difference did not reach statistical significance (9.0 vs. 16.0 days, P = 0.062; Table 4). The statistical analysis for predefined subgroups uncomplicated simple UTI, complicated simple UTI, and uncomplicated febrile UTI/pyelonephritis was limited by small numbers.
Table 4.
Antibiotic exposure by randomization group with subgroup analysis
| Control group | PCT/Pyuria group | P value a | |
|---|---|---|---|
| Median (IQR), days | Median (IQR), days | ||
| All patients (intention-to-treat) | (n = 64) | (n = 61) | |
| Duration of initial antibiotic therapy | 10.0 (7.0–11.0) | 6.0 (4.0–8.0) | <0.001 |
| Antibiotic exposure within 90 days | 10.0 (7.0–16.0) | 7.0 (5.0–14.0) | 0.011 |
| Per-protocol population | (n = 52) | (n = 44) | |
| Duration of initial antibiotic therapy | 10.0 (7.0–11.0) | 6.0 (4.0–7.0) | <0.001 |
| Antibiotic exposure within 90 days | 10.0 (7.5–16.0) | 7.0 (5.0–14.5) | 0.025 |
| Female patients | (n = 52) | (n = 43) | |
| Duration of initial antibiotic therapy | 9.0 (7.0–10.5) | 5.0 (4.0–7.0) | <0.001 |
| Antibiotic exposure within 90 days | 10.0 (7.0–14.0) | 7.0 (4.0–13.0) | 0.022 |
| Male patients | (n = 12) | (n = 18) | |
| Duration of initial antibiotic therapy | 11.0 (10.5–12.0) | 6.5 (5.0–9.0) | 0.003 |
| Antibiotic exposure within 90 days | 16.0 (11.0–21.0) | 9.0 (6.0–19.0) | 0.062 |
| Inpatients | (n = 45) | (n = 45) | |
| Duration of initial antibiotic therapy | 10.0 (8.0–11.0) | 7.0 (5.0–9.0) | <0.001 |
| Antibiotic exposure within 90 days | 11.0 (10.0–18.5) | 8.5 (6.5–16.5) | 0.023 |
| Uncomplicated simple UTI | (n = 6) | (n = 2) | |
| Duration of initial antibiotic therapy | 1.0 (1.0–1.0) | 0.5 (0.0–1.0) | 0.127 |
| Antibiotic exposure within 90 days | 1.0 (1.0–1.0) | 4.0 (1.0–7.0) | 0.513 |
| Complicated simple UTI | (n = 12) | (n = 16) | |
| Duration of initial antibiotic therapy | 7.0 (7.0–9.0) | 4.0 (2.5–5.5) | 0.005 |
| Antibiotic exposure within 90 days | 10.0 (8.0–12.0) | 5.5 (3.0–14.0) | 0.083 |
| Uncomplicated febrile UTI/pyelonephritis | (n = 8) | (n = 9) | |
| Duration of initial antibiotic therapy | 7.0 (7.0–7.5) | 4.0 (4.0–6.0) | 0.009 |
| Antibiotic exposure within 90 days | 7.0 (7.0–10.5) | 6.5 (4.0–11.0) | 0.238 |
| Complicated febrile UTI/pyelonephritis | (n = 34) | (n = 33) | |
| Duration of initial antibiotic therapy | 10.5 (10.0–11.0) | 7.0 (6.0–9.0) | <0.001 |
| Antibiotic exposure within 90 days | 11.0 (10.0–18.0) | 7.5 (6.5–13.5) | 0.002 |
aMann–Whitney U-test.
IQR, Interquartile range.
Secondary endpoint
The initial antibiotic therapy was shorter in the PCT-pyuria group both in the ITT and PP analysis. This applies to all subgroup analyses except for patients with uncomplicated simple UTI (n = 8; Table 4).
Safety outcomes
The clinical recurrence rate and rehospitalization rates within 90 days were similar in both groups (Table 5). Overall, five (4%) patients died, one in the PCT-pyuria group and four in the control group (Table 5). Safety outcomes were similar between the PCT-pyuria and the control group also within the subgroups of uncomplicated simple UTI, complicated simple UTI, uncomplicated febrile UTI/pyelonephritis, and complicated febrile UTI/pyelonephritis (Table 5).
Table 5.
Rates of adverse outcomes
| Control group | PCT/Pyuria group | Odds ratio | 95% CI | P value a | |
|---|---|---|---|---|---|
| All patients (intention-to-treat) | (n = 64) | (n = 61) | |||
| Recurrence | 14/63 (22%) | 15/59 (25%) | 1.19 | 0.52–2.75 | 0.68 |
| Rehospitalization | 17/63 (27%) | 15/59 (25%) | 0.92 | 0.41–2.07 | 0.85 |
| Death | 4/63 (6%) | 1/59 (2%) | 0.25 | 0.03–2.30 | 0.22 |
| Per-protocol population | (n = 52) | (n = 44) | |||
| Recurrence | 11/52 (21%) | 14/44 (32%) | 1.74 | 0.69–4.36 | 0.24 |
| Rehospitalization | 13/52 (35%) | 13/44 (41%) | 1.26 | 0.51–3.10 | 0.62 |
| Death | 1/52 (2%) | 0 | |||
| Inpatients | (n = 45) | (n = 45) | |||
| Recurrence | 11 (25%) | 13 (30%) | 1.26 | 0.49–3.22 | 0.63 |
| Rehospitalization | 15 (34%) | 13 (30%) | 0.81 | 0.28–0.96 | 0.65 |
| Uncomplicated simple UTI | (n = 6) | (n = 2) | |||
| Recurrence | 1/6 (17%) | 1/2 (50%) | 5.00 | 0.15–166.59 | 0.37 |
| Rehospitalization | 1/6 (17%) | 1/2 (50%) | 5.00 | 0.15–166.59 | 0.37 |
| Complicated simple UTI | (n = 12) | (n = 16) | |||
| Recurrence | 3/11 (27%) | 6/16 (38%) | 1.60 | 0.30–8.49 | 0.58 |
| Rehospitalization | 2/11 (18%) | 6/16 (38%) | 2.70 | 0.43–16.94 | 0.29 |
| Uncomplicated febrile UTI/pyelonephritis | (n = 8) | (n = 9) | |||
| Recurrence | 1/8 (13%) | 2/8 (25%) | 2.33 | 0.17–32.58 | 0.53 |
| Rehospitalization | 2/8 (25%) | 1/8 (13%) | 0.43 | 0.03–5.98 | 0.53 |
| Complicated febrile UTI/pyelonephritis | (n = 34) | (n = 33) | |||
| Recurrence | 8/34 (24%) | 6/32 (19%) | 0.75 | 0.23–2.47 | 0.64 |
| Rehospitalization | 11/34 (32%) | 7/32 (22%) | 0.59 | 0.19–1.77 | 0.34 |
aLogistic regression analysis.
The rate of persistent infection (6% in the control group vs. 6% in the PCT-pyuria group in ITT analysis) and of new infections 7 days after end of therapy were similar in both groups (6% in the control group vs. 6% in the PCT-pyuria group in ITT analysis). The microbiological isolates obtained from the urine cultures on day 7 after end of therapy are presented in Table 6.
Table 6.
Microbiological outcome 7 days after end of therapy
| n (%) | Control group | PCT/Pyuria group | Odds ratio | 95% CI | P value a |
|---|---|---|---|---|---|
| All patients (intention-to-treat) | (n = 64) | (n = 61) | |||
| Missing urinalysis | 10/64 (16%) | 8/61 (13%) | 0.82 | 0.30–2.22 | 0.69 |
| Missing urine cultures | 8/64 (13%) | 8/61 (13%) | 1.06 | 0.37–3.02 | 0.92 |
| Sterile urine cultures | 19/56 (34%) | 20/53 (38%) | 1.18 | 0.54–2.58 | 0.68 |
| Contaminated urine cultures b | 25/56 (45%) | 16/53 (30%) | 0.54 | 0.24–1.18 | 0.12 |
| Urine cultures with pathogen c | 12/56 (21%) | 17/53 (32%) | 1.73 | 0.73–4.09 | 0.21 |
| Colonizations | 6/53 (11%) | 8/51 (16%) | 1.46 | 0.47–4.54 | 0.52 |
| Infectionsd | 6/53 (11%) | 8/51 (16%) | 1.46 | 0.47–4.54 | 0.52 |
| Persistence of initial pathogen c | 3/56 (5%) | 4/51 (8%) | 1.50 | 0.32–7.07 | 0.61 |
| Persistent colonization | 0 | 1/51 (2%) | |||
| Persistent infectiond | 3/53 (6%) | 3/51 (6%) | 1.04 | 0.20–5.42 | 0.96 |
| New organism c | 9/56 (16%) | 11/51 (22%) | 1.44 | 0.54–3.81 | 0.47 |
| Colonizations | 6/53 (11%) | 7/49 (14%) | 1.31 | 0.41–4.19 | 0.65 |
| Infectionsd | 3/53 (6%) | 3/49 (6%) | 1.09 | 0.21–5.66 | 0.92 |
| n (%) | Control Group | PCT/ Pyuria Group | |||
| Total no. of isolates | 13 | 18 | |||
| Gram-negative uropathogen | |||||
| Escherichia coli | 3/13 (23%) | 3/18 (17%) | |||
| Klebsiella pneumoniae | 1/13 (8%) | 1/18 (6%) | |||
| Gram-positive uropathogen | |||||
| Enterococcus faecalis | 6/13 (46%) | 11/18 (61%) | |||
| Enterococcus faecium | 1/13 (8%) | 1/18 (6%) | |||
| Staphylococcus saprophyticus | 1/13 (8%) | 0 | |||
| Non uropathogen | |||||
| Lactobacillus speciesb | 1/13 (8%) | 1/18 (6%) | |||
| Candida albicans | 0 | 1/18 (6%) |
aLogistic regression analysis.
bLactobacillus species were considered as contaminants.
cIn case of contaminated (n = 1 in PCT/Pyuria group) initial urine culture any uropathogen was considered as new organism, in case of missing (n = 2 in PCT/ Pyuria group) initial urine culture the uropathogen was not attributed to persistent or new organism group.
dInfection was assumed if pyuria (>20 leukocytes/μL) was present in concomitant urinalysis.
The rate of persistent symptomatic infection 30 days after enrollment was not significantly different between the PCT-pyuria group and the control group (4% in both groups, OR, 1.07; 95% CI, 0.14–7.90; P = 0.95 in ITT analysis). There were no symptomatic infections with new organisms 30 days after enrollment (Table 7).
Table 7.
Microbiological and clinical outcome 30 days after enrollment
| n (%) | Control group | PCT/Pyuria group | Odds ratio | 95% CI | P value a |
|---|---|---|---|---|---|
| All patients (intention-to-treat) | (n = 64) | (n = 61) | |||
| Missing urinalysis | 10/64 (16%) | 9/61 (13%) | 0.93 | 0.35–2.48 | 0.89 |
| Missing urine cultures | 14/64 (22%) | 11/61 (18%) | 0.79 | 0.33–1.90 | 0.59 |
| Sterile urine cultures | 19/50 (38%) | 8/50 (16%) | 0.31 | 0.12–0.80 | 0.02 |
| Contaminated urine cultures b | 20/50 (40%) | 26/50 (52%) | 1.63 | 0.74–3.59 | 0.23 |
| Urine cultures with pathogen c | 11/50 (22%) | 16/50 (32%) | 1.67 | 0.68–4.08 | 0.26 |
| Colonizations | 3/50 (6%) | 3/49 (6%) | 1.02 | 0.20–5.33 | 0.98 |
| Infectionsd | 8/50 (16%) | 13/49 (27%) | 1.90 | 0.71–5.09 | 0.20 |
| Symptomatic infections | 2/50 (4%) | 3/49 (6%) | 1.57 | 0.25–9.80 | 0.63 |
| Persistence of initial pathogen c | 6/50 (12%) | 8/48 (17%) | 1.47 | 0.47–4.59 | 0.51 |
| Persistent colonizations | 1/50 (2%) | 1/47 (2%) | 1.07 | 0.06–17.53 | 0.97 |
| Persistent infectionsd | 5/50 (10%) | 7/47 (15%) | 1.58 | 0.46–5.36 | 0.47 |
| Persistent symptomatic infectionsd | 2/50 (4%) | 2/47 (4%) | 1.07 | 0.14–7.90 | 0.95 |
| New organism c | 5/50 (10%) | 6/48 (13%) | 1.29 | 0.37–4.53 | 0.70 |
| Colonizations | 2/50 (4%) | 2/47 (4%) | 1.07 | 0.14–7.90 | 0.95 |
| Infectionsd | 3/50 (6%) | 4/47 (9%) | 1.46 | 0.31–6.89 | 0.64 |
| Symptomatic infectionsd | 0 | 0 | |||
| n (%) | Control group | PCT/Pyuria group | |||
| Total no. of isolates e | 17 | 22 | |||
| Gram-negative uropathogen | |||||
| Escherichia coli | 5/17 (29%) | 7/22 (32%) | |||
| Klebsiella pneumoniae | 2/17 (12%) | 1/22 (5%) | |||
| Citrobacter koseri | 1/17 (6%) | 1/22 (5%) | |||
| Enterobacter cloacae | 0 | 1/22 (5%) | |||
| Pseudomonas aeruginosa | 0 | 1/22 (5%) | |||
| Gram-positive uropathogen | |||||
| Enterococcus faecalis | 5/17 (29%) | 9/22 (41%) | |||
| Enterococcus faecium | 1/17 (6%) | 0 | |||
| Staphylococcus saprophyticus | 0 | 1/22 (5%) | |||
| Group B Streptococci | 1/17 (6%) | 0 | |||
| Non-uropathogen | |||||
| Staphylococcus aureus | 1/17 (6%) | 0 | |||
| Coagulase-negative staphylococcib | 0 | 1/22 (5%) | |||
| Lactobacillus speciesb | 1/17 (6%) | 1/22 (5%) | |||
| Streptococcus milleri | 0 | 1/22 (5%) |
aLogistic regression analysis.
bLactobacillus species and Coagulase-negative staphylococci were considered as contaminants.
cIn case of missing initial urine culture (n = 2 in the PCT/Pyuria group) any uropathogen was not attributed to persistent or new organism group.
dInfection was assumed if pyuria (>20 leukocytes/μL) was present in concomitant urinalysis.
eTwo isolates in nine cultures.
Bacteremic patients
As the distribution of patients with bacteremia was not well balanced between the two study arms we performed a stratified analysis of the primary and secondary outcomes for bacteremic and non-bacteremic patients (Additional file 1: Table S1). As a sensitivity analysis for the primary endpoint we also performed median regression analysis adjusted for bacteremia. Adjusted results were robust and showed a significant reduction in antibiotic exposure (coefficient, −3.0; 95% CI, −0.6 to −5.4; P = 0.015). Among bacteremic patients, the initial antibiotic therapy was shorter in the PCT-pyuria group (7.0 vs. 11.0 days, P ≤0.001); overall antibiotic exposure within 90 days was not different. The recurrence rate was higher in the PCT-pyuria group (56% vs. 16% in the control group, OR, 6.67; 95% CI, 0.04–1.10; P = 0.039) but rehospitalization rates were not significantly different.
The rates of persistent infection 7 days after end of therapy were similar in both groups (13% in the PCT-pyuria group vs. 6% in the control group, OR, 2.14; 95% CI, 0.12–39.47; P = 0.61).
There were two symptomatic infections with new organisms 7 days after end of therapy and one persistent symptomatic infection 30 days after enrollment in the control group.
Discussion
As UTIs are one of the most common indications for antibiotic therapy, the impact of a reduction of treatment duration could be enormous. This study provides evidence that guidance of antibiotic therapy in patients with a UTI by a PCT-pyuria algorithm for antibiotic guidance is feasible. The implementation of an algorithm into clinical workflows is practicable as shown by our group in respiratory tract infections [34]. The efficacy of this approach is evidenced by the 90 day observation period for the primary endpoint, which included both the initial and any subsequent antibiotic treatments.
Overall and in most subgroups (except for the small subgroup of patients with uncomplicated simple UTIs), the PCT-pyuria algorithm led to shorter initial duration of antibiotic therapy. The tested algorithm can help to determine the optimal length of antibiotic therapy and avoid antibiotic overuse.
There was an imbalance in randomization of eight patients with uncomplicated simple UTI with only two being randomized to the PCT-pyuria group. Since all six patients in the standard guidelines group were treated according to our algorithm with single-dose fosfomycin, the median duration of the initial antibiotic therapy in this subgroup was similar between both groups.
Only one patient in the PCT-pyuria group, who relapsed with urosepsis and had to be hospitalized for 3 days and treated with intravenous antibiotics, was initially treated with NSAIDs according to the study protocol. Given the small number of outpatients, the safety of NSAIDs for simple uncomplicated UTIs cannot be determined based on our study. Despite recent data with promising results for this approach [32,33], a recent review [13] emphasized the need for immediate antimicrobial therapy rather than delayed treatment or symptomatic management with ibuprofen alone.
Patients with complicated febrile UTI were older and had multiple comorbidities. Especially in this population with the highest disease burden, in whom the longest antibiotic therapy is recommended by current guidelines, our algorithm proved to be effective.
The safety subgroups were small, but no trend for difference in rates of persistent infection was shown at 7 days after end of therapy or at 30 days after enrollment. The slightly higher, but non-significant, rate of bacteriuria and asymptomatic infection in the PCT-pyuria group should not be viewed as an unsuccessful treatment. There is vast evidence that asymptomatic bacteriuria should not be treated [35]. In fact, asymptomatic bacteriuria might be protective against future development of pyelonephritis, as elegantly shown in a prospective Italian study of young women with asymptomatic bacteriuria, who benefited from symptomatic treatment versus antibiotics [36]. There is evidence that in older patients with isolated non-specific signs or non-infectious symptoms, such as delirium, urine testing and subsequent antibiotic therapy should not be ordered [37].
Furthermore, the follow-up mid-stream urine cultures in the PCT-pyuria group yielded in the majority of cases Enterococcus faecalis (Table 2), which has recently been shown to have a low positive predictive value for uropathogen growth in the bladder [38].
The antibiotics chosen in our algorithm, derived from international guidelines, should not deter from the necessity to adapt antibiotic choices to local epidemiology and resistance data [9]. In Switzerland, 18.5% of Escherichia coli were resistant to fluoroquinolones in 2013, compared to 22.3% in the European Union in 2012 [39,40].
A major strength was the innovative study design with antibiotic guidance based on the combination of the systemic and local response against a control group receiving antibiotic therapy according to the low end of currently recommended guidelines.
Potential limitations
Our study has the following limitations. First, the small sample size due to slow recruitment and the heterogeneity of patients within the predefined subgroups limit the power of the analysis, especially regarding safety outcomes. Second, the follow-up mode by telephone interview and by urine samples which were returned by mail harbors potential recall bias and underreporting, which we tried to counteract by contacting the primary care physician and by obtaining discharge letters of subsequent hospitalizations. Third, the analysis of the recurrence rate in the subgroup of patients with bacteremia was limited due to the small numbers. Further studies will have to clarify whether this algorithm needs to be adapted for patients with bacteremia.
Conclusions
An algorithm based on PCT and pyuria significantly reduces antibiotic exposure when compared to current guidelines without apparent negative effects on clinical outcomes, especially in patients with complicated febrile UTI. Further randomized controlled multi-center studies with larger patient numbers are needed to confirm our findings for all subgroups and to proof the feasibility in other settings.
Acknowledgements
We are grateful to all physicians, nurses, social workers, and patients who participated in this study. Especially, we thank Petra Tobias and the staff of the Emergency Department; and Susanne Schirlo and the staff of the Medical University Clinic; Renate Hunziker, Martha Kaeslin, and the staff of the Center of Laboratory Medicine of the Cantonal Hospital of Aarau for their very helpful assistance and technical support. We are grateful to the members of the DSMB: Prof. Uyen Huynh-Do, MD (Inselspital Berne), Prof. Stephan Zimmerli, MD (Inselspital Berne), and PD Matthias Briel (University Hospital, Basel), MD, MPH.
Funding
This work was supported by the research council – “Forschungsrat” of the Kantonsspital Aarau (project number 1410.000.003) and the Department of Health and Social Services of the Canton Aargau, Switzerland.
Abbreviations
- eGFR
Estimated glomerular filtration rate
- ITT
Intention-to-treat
- NSAIDs
Non-steroidal anti-inflammatory drugs
- PCT
Procalcitonin
- PP
Per-protocol
- UTIs
Urinary tract infections.
Additional file
Analysis stratified for presence of bacteremia.
Footnotes
Competing interests
This was an investigator-initiated study. To exclude any conflict of interest, no commercial sponsor had any involvement in the design and conduct of the trial, i.e., collection, management, analysis, and interpretation of the data, or preparation, decision to submit, review, or approval of the manuscript. For other studies unrelated to this trial Werner Albrich, Alexander Kutz, Philipp Schuetz, and Beat Mueller received support from BRAHMS Thermo Fisher and from bioMérieux to attend meetings and fulfilled speaking engagements and served as consultants for BRAHMS Thermo Fisher. Beat Mueller received research support from BRAHMS Thermo Fisher. All other authors have not disclosed any conflicts of interests.
Authors’ contributions
DD, SS, AB, CF, BM, and WA planned and designed the study protocol. KR, US, AC, BR, CO, FB, CB, AH, UB, and PS participated in study design and coordination. DD, PS, AB, CF, BM, and WA were involved in the drafting of the manuscript. DD, AK, EG, AR, DS, KR, US, MG, SH, and CB made substantial contributions to acquisition of data and revised the manuscript. AC, BR, CO, FB, AH, and UB revised the manuscript critically for important intellectual content. DD, WA, and PS performed the statistical analysis. All authors read and approved the final manuscript.
Contributor Information
Daniel Drozdov, Email: daniel.drozdov@ksa.ch.
Stefanie Schwarz, Email: steffyschwarz@gmail.com.
Alexander Kutz, Email: kutz.alexander@gmail.com.
Eva Grolimund, Email: eva.grolimund@ksa.ch.
Anna Christina Rast, Email: rast.annachr@gmail.com.
Deborah Steiner, Email: deborah.steiner@ksa.ch.
Katharina Regez, Email: katharina.regez@ksa.ch.
Ursula Schild, Email: ursula.schild@ksa.ch.
Merih Guglielmetti, Email: merih.guglielmetti@ksa.ch.
Antoinette Conca, Email: antoinette.conca@ksa.ch.
Barbara Reutlinger, Email: barbara.reutlinger@ksa.ch.
Cornelia Ottiger, Email: cornelia.ottiger@ksa.ch.
Florian Buchkremer, Email: florian.buchkremer@ksa.ch.
Sebastian Haubitz, Email: sebastian.haubitz@gmail.com.
Claudine Blum, Email: claudineblum@yahoo.com.
Andreas Huber, Email: andreas.huber@ksa.ch.
Ulrich Buergi, Email: ulrich.buergi@ksa.ch.
Philipp Schuetz, Email: schuetzph@gmail.com.
Andreas Bock, Email: andreas.bock@ksa.ch.
Christoph Andreas Fux, Email: christophandreas.fux@ksa.ch.
Beat Mueller, Email: happy.mueller@unibas.ch.
Werner Christian Albrich, Email: werner.albrich@kssg.ch.
References
- 1.Foxman B. Urinary tract infection syndromes: occurrence, recurrence, bacteriology, risk factors, and disease burden. Infect Dis Clin North Am. 2014;28:1–13. doi: 10.1016/j.idc.2013.09.003. [DOI] [PubMed] [Google Scholar]
- 2.Curns AT, Holman RC, Sejvar JJ, Owings MF, Schonberger LB. Infectious disease hospitalizations among older adults in the United States from 1990 through 2002. Arch Intern Med. 2005;165:2514–20. doi: 10.1001/archinte.165.21.2514. [DOI] [PubMed] [Google Scholar]
- 3.Eells SJ, Bharadwa K, McKinnell JA, Miller LG. Recurrent urinary tract infections among women: comparative effectiveness of 5 prevention and management strategies using a Markov chain Monte Carlo model. Clin Infect Dis. 2014;58:147–60. doi: 10.1093/cid/cit646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tamma PD, Turnbull AE, Milstone AM, Lehmann CU, Sydnor ER, Cosgrove SE. Ventilator-associated tracheitis in children: does antibiotic duration matter? Clin Infect Dis. 2011;52:1324–31. doi: 10.1093/cid/cir203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hooton TM. Clinical practice. Uncomplicated urinary tract infection. N Engl J Med. 2012;366:1028–37. doi: 10.1056/NEJMcp1104429. [DOI] [PubMed] [Google Scholar]
- 6.Wagenlehner FM, Schmiemann G, Hoyme U, Funfstuck R, Hummers-Pradier E, Kaase M, et al. National S3 guideline on uncomplicated urinary tract infection: recommendations for treatment and management of uncomplicated community-acquired bacterial urinary tract infections in adult patients. Urologe A. 2011;50:153–69. doi: 10.1007/s00120-011-2512-z. [DOI] [PubMed] [Google Scholar]
- 7.Spoorenberg V, Hulscher ME, Akkermans RP, Prins JM, Geerlings SE. Appropriate antibiotic use for patients with urinary tract infections reduces length of hospital stay. Clin Infect Dis. 2014;58:164–9. doi: 10.1093/cid/cit688. [DOI] [PubMed] [Google Scholar]
- 8.McQuiston Haslund J, Rosborg Dinesen M, Sternhagen Nielsen AB, Llor C, Bjerrum L. Different recommendations for empiric first-choice antibiotic treatment of uncomplicated urinary tract infections in Europe. Scand J Prim Health Care. 2013;31:235–40. doi: 10.3109/02813432.2013.844410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ulleryd P, Sandberg T. Ciprofloxacin for 2 or 4 weeks in the treatment of febrile urinary tract infection in men: a randomized trial with a 1 year follow-up. Scand J Infect Dis. 2003;35:34–9. doi: 10.1080/0036554021000026988. [DOI] [PubMed] [Google Scholar]
- 10.van Nieuwkoop C, van’t Wout JW, Assendelft WJ, Elzevier HW, Leyten EM, Koster T, et al. Treatment duration of febrile urinary tract infection (FUTIRST trial): a randomized placebo-controlled multicenter trial comparing short (7 days) antibiotic treatment with conventional treatment (14 days) BMC Infect Dis. 2009;9:131. doi: 10.1186/1471-2334-9-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sandberg T, Skoog G, Hermansson AB, Kahlmeter G, Kuylenstierna N, Lannergard A, et al. Ciprofloxacin for 7 days versus 14 days in women with acute pyelonephritis: a randomised, open-label and double-blind, placebo-controlled, non-inferiority trial. Lancet. 2012;380:484–90. doi: 10.1016/S0140-6736(12)60608-4. [DOI] [PubMed] [Google Scholar]
- 12.Eliakim-Raz N, Yahav D, Paul M, Leibovici L. Duration of antibiotic treatment for acute pyelonephritis and septic urinary tract infection – 7 days or less versus longer treatment: systematic review and meta-analysis of randomized controlled trials. J Antimicrob Chemother. 2013;68:2183–91. doi: 10.1093/jac/dkt177. [DOI] [PubMed] [Google Scholar]
- 13.Grigoryan L, Trautner BW, Gupta K. Diagnosis and management of urinary tract infections in the outpatient setting: a review. JAMA. 2014;312:1677–84. doi: 10.1001/jama.2014.12842. [DOI] [PubMed] [Google Scholar]
- 14.Naber KG, Wullt B, Wagenlehner FM. Antibiotic treatment of uncomplicated urinary tract infection in premenopausal women. Int J Antimicrob Agents. 2011;38:21–35. doi: 10.1016/j.ijantimicag.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 15.Gupta K, Hooton TM, Naber KG, Wullt B, Colgan R, Miller LG, et al. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: A 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis. 2011;52:e103–20. doi: 10.1093/cid/ciq257. [DOI] [PubMed] [Google Scholar]
- 16.Kollef MH, Fraser VJ. Antibiotic resistance in the intensive care unit. Ann Intern Med. 2001;134:298–314. doi: 10.7326/0003-4819-134-4-200102200-00014. [DOI] [PubMed] [Google Scholar]
- 17.Hanberger H, Garcia-Rodriguez JA, Gobernado M, Goossens H, Nilsson LE, Struelens MJ. Antibiotic susceptibility among aerobic gram-negative bacilli in intensive care units in 5 European countries. French and Portuguese ICU Study Groups. JAMA. 1999;281:67–71. doi: 10.1001/jama.281.1.67. [DOI] [PubMed] [Google Scholar]
- 18.Neuhauser MM, Weinstein RA, Rydman R, Danziger LH, Karam G, Quinn JP. Antibiotic resistance among gram-negative bacilli in US intensive care units: implications for fluoroquinolone use. JAMA. 2003;289:885–8. doi: 10.1001/jama.289.7.885. [DOI] [PubMed] [Google Scholar]
- 19.Drekonja DM, Rector TS, Cutting A, Johnson JR. Urinary tract infection in male veterans: treatment patterns and outcomes. JAMA Intern Med. 2013;173:62–8. doi: 10.1001/2013.jamainternmed.829. [DOI] [PubMed] [Google Scholar]
- 20.Stalenhoef JE, van Dissel JT, van Nieuwkoop C. Febrile urinary tract infection in the emergency room. Curr Opin Infect Dis. 2015;28:106–11. doi: 10.1097/QCO.0000000000000121. [DOI] [PubMed] [Google Scholar]
- 21.Schuetz P, Albrich W, Mueller B. Procalcitonin for diagnosis of infection and guide to antibiotic decisions: past, present and future. BMC Med. 2011;9:107. doi: 10.1186/1741-7015-9-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schuetz P, Christ-Crain M, Thomann R, Falconnier C, Wolbers M, Widmer I, et al. Effect of procalcitonin-based guidelines vs standard guidelines on antibiotic use in lower respiratory tract infections: the ProHOSP randomized controlled trial. JAMA. 2009;302:1059–66. doi: 10.1001/jama.2009.1297. [DOI] [PubMed] [Google Scholar]
- 23.Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013;41:580–637. doi: 10.1097/CCM.0b013e31827e83af. [DOI] [PubMed] [Google Scholar]
- 24.Schuetz P, Amin DN, Greenwald JL. Role of procalcitonin in managing adult patients with respiratory tract infections. Chest. 2012;141:1063–73. doi: 10.1378/chest.11-2430. [DOI] [PubMed] [Google Scholar]
- 25.van Nieuwkoop C, Bonten TN, van’t Wout JW, Kuijper EJ, Groeneveld GH, Becker MJ, et al. Procalcitonin reflects bacteremia and bacterial load in urosepsis syndrome: a prospective observational study. Crit Care. 2010;14:R206. doi: 10.1186/cc9328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bouadma L, Luyt CE, Tubach F, Cracco C, Alvarez A, Schwebel C, et al. Use of procalcitonin to reduce patients’ exposure to antibiotics in intensive care units (PRORATA trial): a multicentre randomised controlled trial. Lancet. 2010;375:463–74. doi: 10.1016/S0140-6736(09)61879-1. [DOI] [PubMed] [Google Scholar]
- 27.Ottiger C, Schaer G, Huber AR. Time-course of quantitative urinary leukocytes and bacteria counts during antibiotic therapy in women with symptoms of urinary tract infection. Clin Chim Acta. 2007;379:36–41. doi: 10.1016/j.cca.2006.11.023. [DOI] [PubMed] [Google Scholar]
- 28.Gupta K, Hooton TM, Miller L. Managing uncomplicated urinary tract infection–making sense out of resistance data. Clin Infect Dis. 2011;53:1041–2. doi: 10.1093/cid/cir637. [DOI] [PubMed] [Google Scholar]
- 29.Drozdov D, Thomer A, Meili M, Schwarz S, Kouegbe RB, Regez K, et al. Procalcitonin, pyuria and proadrenomedullin in the management of urinary tract infections–‘triple P in UTI’: study protocol for a randomized controlled trial. Trials. 2013;14:84. doi: 10.1186/1745-6215-14-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Regeniter A, Haenni V, Risch L, Kochli HP, Colombo JP, Frei R, et al. Urine analysis performed by flow cytometry: reference range determination and comparison to morphological findings, dipstick chemistry and bacterial culture results–a multicenter study. Clin Nephrol. 2001;55:384–92. [PubMed] [Google Scholar]
- 31.Neuner EA, Sekeres J, Hall GS, van Duin D. Experience with fosfomycin for treatment of urinary tract infections due to multidrug-resistant organisms. Antimicrob Agents Chemother. 2012;56:5744–8. doi: 10.1128/AAC.00402-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bleidorn J, Gagyor I, Kochen MM, Wegscheider K, Hummers-Pradier E. Symptomatic treatment (ibuprofen) or antibiotics (ciprofloxacin) for uncomplicated urinary tract infection?–results of a randomized controlled pilot trial. BMC Med. 2010;8:30. doi: 10.1186/1741-7015-8-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Falagas ME, Kotsantis IK, Vouloumanou EK, Rafailidis PI. Antibiotics versus placebo in the treatment of women with uncomplicated cystitis: a meta-analysis of randomized controlled trials. J Infect. 2009;58:91–102. doi: 10.1016/j.jinf.2008.12.009. [DOI] [PubMed] [Google Scholar]
- 34.Albrich WC, Dusemund F, Bucher B, Meyer S, Thomann R, Kuhn F, et al. Effectiveness and safety of procalcitonin-guided antibiotic therapy in lower respiratory tract infections in “real life”: an international, multicenter poststudy survey (ProREAL) Arch Intern Med. 2012;172:715–22. doi: 10.1001/archinternmed.2012.770. [DOI] [PubMed] [Google Scholar]
- 35.Beveridge LA, Davey PG, Phillips G, McMurdo ME. Optimal management of urinary tract infections in older people. Clin Interv Aging. 2011;6:173–80. doi: 10.2147/CIA.S13423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cai T, Mazzoli S, Mondaini N, Meacci F, Nesi G, D’Elia C, et al. The role of asymptomatic bacteriuria in young women with recurrent urinary tract infections: to treat or not to treat? Clin Infect Dis. 2012;55:771–7. doi: 10.1093/cid/cis534. [DOI] [PubMed] [Google Scholar]
- 37.Nace DA, Drinka PJ, Crnich CJ. Clinical uncertainties in the approach to long term care residents with possible urinary tract infection. J Am Med Dir Assoc. 2014;15:133–9. doi: 10.1016/j.jamda.2013.11.009. [DOI] [PubMed] [Google Scholar]
- 38.Hooton TM, Roberts PL, Cox ME, Stapleton AE. Voided midstream urine culture and acute cystitis in premenopausal women. N Engl J Med. 2013;369:1883–91. doi: 10.1056/NEJMoa1302186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bulletin 31/14. Federal Office of Public Health, Switzerland. http://www.bag.admin.ch/dokumentation/publikationen/01435/13591/index.html?lang=de&download=NHzLpZig7t,lnp6I0NTU042l2Z6ln1acy4Zn4Z2qZpnO2Yuq2Z6gpJCLfYF3gWym162dpYbUzd,Gpd6emK2Oz9aGodetmqaN19XI2IdvoaCUZ,s-.
- 40.Antimicrobial resistance surveillance in Europe 2012. Annual Report of the European Antimicrobial Resistance Surveillance Network (EARS-Net). http://www.ecdc.europa.eu/en/publications/Publications/antimicrobial-resistance-surveillance-europe-2012.pdf.


