Abstract
Objectives:
Global Self-Rating of Oral Health (GSROH) has numerous benefits, especially in resource-constrained environments with a paucity of dentists thereby potentially limiting administration of oral health surveys and monitoring of dental treatment. The aim of the study was to identify factors that could influence or predict poor self-ratings of oral health.
Materials and Methods:
The study was descriptive in design. Data were collected using structured interviewer-administered questionnaire, which had items on socio-demographic characteristics of the respondents and their GSROH. Oral examination was conducted to identify untreated dental caries, missing teeth, and mobile teeth. Data were analyzed using SPSS, and the P value was set at 0.05.
Results:
There were 600 participants; 400 were teachers constituting the non-patient population and 200 were dental patients with age ranging from 18 to 83 years. A total of 169 (28.1%) participants rated their oral health as poor, including 104 patients (52.0%) and 65 (16.2%) non-patients (P < 0.001). Having had toothache in the preceding 6 months (62.4% vs. 16.0%, P < 0.001), mobile teeth (46.7% vs. 24.2%, P < 0.001), decayed teeth (49.0% vs. 21.3%, P < 0.001), missing teeth (35.0% vs. 26.1%, P = 0.042), or DMFT score greater than zero (41.1% vs. 20.7%, P < 0.001) was associated with poor GSROH. Presence of mobile teeth [odds ratio (OR) = 2.68; 95% confidence interval (CI): 1.29, 4.23; P < 0.001] and carious teeth (OR = 2.25; 95% CI: 1.09, 4.65; P = 0.029) were independent predictors of GSROH.
Conclusion:
The GSROH was able to identify individuals with or without oral conditions in the studied population, and thus may be used in oral health surveys to assess the oral health status and in monitoring of treatment outcome.
Keywords: Oral health surveys, patients, predictors, self-rating of oral health
INTRODUCTION
The Global Self-Ratings of Oral Health (GSROH) status is a tool that provides a simple way of assessing self-perception of oral health.[1] It is time- and cost-effective, of proven validity, and may be utilized when a need arises to understand the views and perceptions of individuals and the larger population as regards oral health.[2,3,4] Furthermore, it has been recognized as a useful adjunct in the identification of health inequalities in populations.[5,6] The GSROH has also been documented as an essential tool in measuring treatment or intervention outcome, as well as a validating tool for other subjective assessment of oral health status, especially the composite instruments, with multiple items.[7,8]
Despite its usefulness in individuals and the population, it remains an understudied tool in both the dental clinic settings and at the community level in developing countries. Moreover, low-income countries present with peculiarities such as limited resources, highly prevalent common oral diseases, for example, periodontal disease, and inadequate professionals who investigate disease burden or assess different treatment outcomes. These peculiarities often make adequate clinical oral examinations in oral health surveys practically difficult and monitoring of treatment outcome in community dental outposts unrealizable due to lack of appropriate instruments and as the personnel are insufficient for the task ahead of them. Quite often, a single-item tool such as the GSROH with the aforementioned advantages will be an appropriate tool to use.[5,6,7,8]
Since dental care is treatment need-driven in low-resource settings and patients typically do not consult dental practitioners until they perceive a need for treatment,[9,10] it will be interesting to know if GSROH is usable in such settings and if it would be able to predict the presence of dental caries and periodontal problems. The aims of the study, therefore, included evaluation of the self-ratings of oral health in a low-resource setting, identification of factors influencing the ratings, and determination of predictors of the GSROH.
MATERIALS AND METHODS
The study was cross sectional in design, and the study population consisted of patients and non-patients to simulate the dental clinic and the community settings. Public primary school teachers in Ibadan constituted the non-patient population, while the patients were recruited from adults attending the Dental Center of the University College Hospital, Ibadan, Nigeria. The teachers were randomly selected prior to commencing oral health promotion at school oral health education programs conducted in the city between September 2011 and June 2012, while the patient population consisted of consecutive patients attending the Oral Diagnosis Clinic of the Dental Center of the hospital between September 2011 and June 2012. A minimum sample size of 379 teachers was estimated using a significance level of 5% and based on the prevalence of dental caries in a population-based (non-hospital) study conducted in Nigeria (44%), to achieve a power of 90% for the study.[11] Two teachers were selected for each patient recruited since the patients were seen at the dental clinic where the prevalence of dental caries is expected to be much higher. Individuals aged 18 years or older who were approached and consented to participate were included in the study. Those who declined to give consent, those younger than 18 years, or presented for routine scaling and polishing at the dental clinic were excluded from the study. The protocol for this study was approved by the joint University of Ibadan and the University College Hospital Ethics Review Committee and the participants gave individual consent.
Data collection procedure
Information was obtained on the socio-demographic characteristics of the study participants and the global self-ratings of their oral health. The GSROH assessed their oral health status through a single question: “How would you consider the condition of your teeth and mouth presently?” The response was provided on a 5-point Likert scale as “very good,” “good,” “neither good nor poor,” “poor,” and “very poor.” They were also asked if they have had toothache within a 6-month period preceding the interview, with the response recorded as “Yes” or “No.” Oral examination was conducted by a trained and calibrated researcher who examined all the study participants using the Community Periodontal Index probe (CPI probe), wooden spatula, and dental mirror. The total number of teeth present/missing, presence or absence of decayed teeth, and presence of periodontal disease were evaluated. The oral examinations were done according to the World Health Organization (WHO) survey guidelines using natural lighting as the source of illumination.[12]
The questions were pre-tested on 20 teachers who volunteered in a school not included in the study and on 10 patients seen at the Periodontology Clinic of the hospital. Intra-examiner variability was calculated for correct and standard measurements: Every tenth participant had a duplicate examination and the intra-examiner Kappa score was 0.92.
Data management
Data collected were entered into and analyzed using SPSS version 21.0 (IBM Corp., Armonk, NY, USA). Categorical variables were summarized using frequencies, percentages, and proportions, while continuous variables were reported using medians and ranges. The GSROH was dichotomized for the purposes of bivariate analyses into “good” (including the original responses of “very good” and “good”) and “poor” (including “neither good nor poor,” “poor,” and “very poor”). Mann–Whitney U test was conducted to compare the oral examination findings between the two groups of participants. The relationship between GSROH and clinical oral examination findings was explored using Chi-square statistics and the level of statistical significance set at P < 0.05. Logistic regression analysis was performed to identify significant predictors of GSROH among clinical oral examination parameters.
RESULTS
A total of 600 respondents participated in the study, which consisted of 400 (66.7%) school teachers (non-patients) and 200 (33.3%) patients with a median age of 48 years (range 18–83 years). The majority (461, 76.8%) were females and 523 (87.2%) were married. A total of 89 (14.8%) participants had university education. Among others, 20 had between 1 and 6 years of formal education (3.3%), 99 had 7–12 years of schooling (16.5%), 383 had >12 years of schooling without university education (63.8%), and 9 had no formal education (1.5%). Twenty-six percent reported having had one or more episodes of toothache within the preceding six months.
GSROH of the study participants
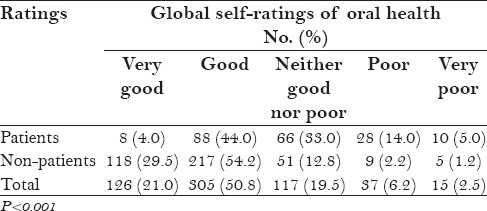
A total of 126 (21.0%) participants rated their oral health as being very good, 305 (50.8%) as good, 117 (19.5%) as neither good nor poor, 37 (6.2%) selected poor, while 15 (2.5%) rated it as very poor. The patients significantly rated their oral health status as poor, compared to non-patients [Table 1].
Table 1.
GSROH of the study participants
Oral examination findings
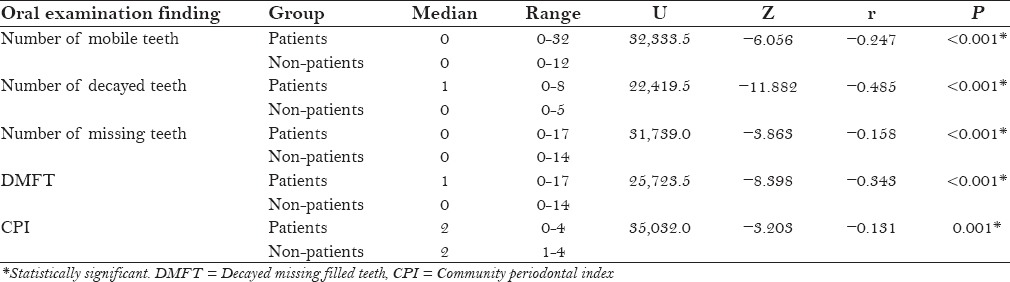
The number of mobile teeth recorded on examination ranged from 0 to 32, and 105 (17.5%) participants had mobile teeth. A total of 149 (24.8%) participants had decayed teeth, with the number of decayed teeth ranging from 0 to 8. One or more teeth were missing from the oral cavity of 137 (22.8%) participants. The total DMFT score ranged from 0 to 17; 219 (36.5%) participants had a DMFT score greater than zero. The CPI scores recorded were: 0 (healthy periodontium) in 1 (0.2%) participant, 1 (bleeding encountered on probing) in 13 (2.2%) participants, 2 (calculus accumulation) in 438 (73.0%) participants, 3 (periodontal pockets 3.5–5.5 mm deep) in 131 (21.8%) participants. and 4 (periodontal pockets deeper than 5.5 mm) in 17 (2.8%) participants.
The patients in the study had higher numbers of mobile teeth, decayed teeth, and missing teeth than the non-patients [Table 2]. The patients also had higher DMFT scores and worse periodontal status.
Table 2.
Oral examination findings of the participants
GSROH and toothache
A total of 98 (62.4%) out of 157 participants who had toothache within the preceding 6 months rated their oral health status as poor, compared to 41 (16.0%) out of 443 participants who had no toothache (P < 0.001).
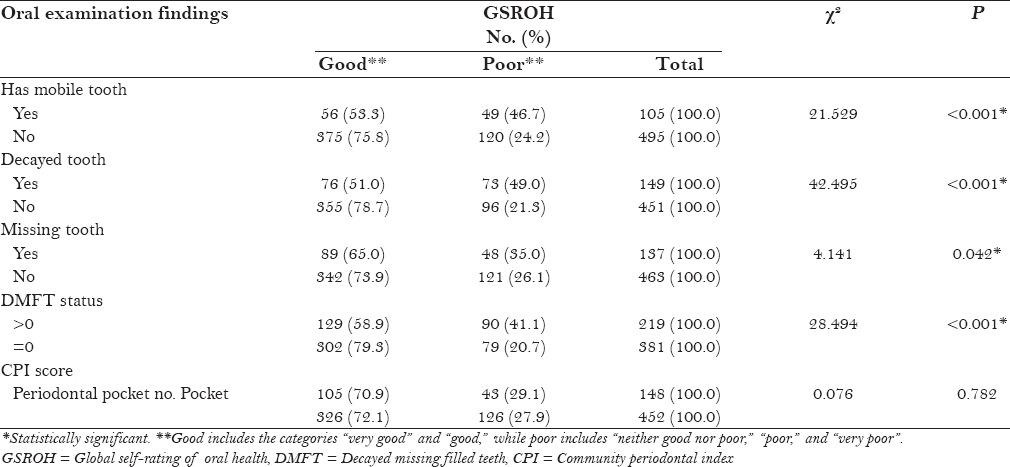
GSROH and oral examination findings
A higher proportion of participants with mobile teeth rated their oral health status as poor than those without mobile teeth (46.7% vs. 24.2%, P < 0.001). The proportion of participants with decayed teeth who rated their oral health status as poor (49.0%) was higher than that of participants without decayed tooth (21.3%, P < 0.001). Similar relationships were found between GSROH and “missing teeth” or DMFT status [Table 3]. There was no statistically significant relationship between the GSROH and CPI scores.
Table 3.
Relationship between GSROH and oral examination findings
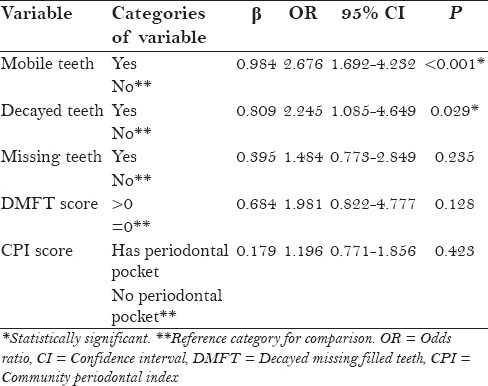
Predictors of GSROH status of participants among normative needs
Participants with mobile teeth were three times more likely to report their oral health status as poor compared to those without mobile tooth [odds ratio (OR) = 2.68; 95% confidence interval (CI): 1.29, 4.23; P < 0.001]. Those with carious tooth/teeth were twice as likely as participants without carious teeth to state that their oral health was poor (OR = 2.25; 95% CI: 1.09, 4.65; P = 0.029). Having “missing” teeth, a DMFT score higher than zero, and presence of periodontal pocket were not significant predictors of global self-rating [Table 4].
Table 4.
Logistic regression analysis of the relationship between GSROH and oral examination findings (with GSROH as the dependent variable and poor as reference)
DISCUSSION
This is the first study in Nigeria to describe the applicability of this single-item tool in summarizing the oral health status in both the population and clinical settings. In addition to the enormous benefits it presents when the subjective and objective assessment of oral health is quickly needed, scores obtained from the GSROH have been found to correlate with multi-item indices like Oral Health Related Quality of Life measure that assesses the perception of individuals on how oral health affects daily activities.[8]
The present study revealed that the majority of the study participants summarized their oral health as good, similar to reports from earlier studies,[4,5,8,13,14] but inconsistent with some.[15,16] Furthermore, a higher proportion of patients compared to non-patients summarized their oral health less favorably as poor, suggesting that demand for oral health care by individuals who perceive a need for it may be important in the ratings of oral health in this environment. The oral diseases prevalent in patients in the present study might have further contributed to this finding. Patients in this region will only consult a dentist if they have complaints, as was also noted by Okunseri et al.[9,10] that in our culture, dental consultation is problem-driven and most people will only visit the dentist when they perceive significant depreciation in their oral health status, usually accompanied by pain. Pain is the leading reason for utilization of dental services in this region.[17] Pain, according to Kim et al.,[16] may lead to physical as well as functional limitation, which impacts on the quality of life of the affected persons invariably, significantly associated with poor ratings of oral health, as was observed in the present study and by some other authors.[18,19]
A poor rating of oral health was associated with presence of oral disease conditions investigated in the study population. Respondents with decayed, missing, or mobile teeth rated their oral health as poor, compared to those without these conditions. The functional and social effects of these disease conditions on those affected may account for the poor ratings of oral health. Less favorable ratings of oral health have been associated with dental problems and treatment needs.[15,16,20] On the other hand, poor global self-rating did not appear to be associated with the presence of periodontal disease in this study. This could be because the prevalence of the disease was nearly 100% and comparison was done between individuals with severe and mild periodontal disease as measured by the presence or absence of periodontal pockets, respectively.
Tooth decay and mobility were predictors of poor ratings of oral health in this study. Untreated dental caries and tooth mobility are almost always accompanied by pain and dysfunction, which could be the explanation for why it was a significant predictor of poorly rated oral health status.[8,15,21,22] Missing tooth, on the other hand, was not a significant predictor of GSROH in this study. The finding, however, is at variance with what Kim and Patton had reported among the elderly in Korea, where missing tooth was noted to be a predictor of poor self-rating of oral health.[15] The different ages of the participants in the two studies may be responsible for this variation. Moreover, the type of tooth loss and the duration of the tooth loss as well as replacement of lost teeth may be important factors to be considered for this difference, as adaptation to the different diets available in our environment may have occurred before the study was done; likewise, the social or psychological effects that may arise as a result of lost teeth may have been overcome either due to the time factor as accounted for by adaptation to it or replacement of the lost teeth. Since the concept of health is context-bound,[14] being able to detect those with oral health compromise in these two population settings by the GSROH makes this instrument a useful tool in analyzing the perceived oral health needs of individuals or the population, an important consideration when any oral health promotion program is to be instituted.
Evaluation of the oral health status as poor using the GSROH as shown by this study indicates presence of oral disease condition and probably a perceived need for treatment, which may be a pointer to the need for an intervention program. Likewise, in a clinical setting, it may be of use when a need arises to determine if the demand of an individual is being met or if the instituted therapy is having a positive response. Since pain and dysfunction are predictors of poor rating of oral health, any change in the patient's condition as evidenced by alleviation of pain and or dysfunction will be noted. It is obvious that the GSROH in these settings is an appropriate tool in evaluating oral health. Further use of the instrument in assessing oral health outcomes is thereby encouraged. In the present study, a major limitation was the inability to identify behavioral influences that could have impacted on the ratings of oral health status by the participants. It will be necessary to study the influence of different levels of disabilities and impairments, as well personalities on GSROH.
CONCLUSION
This study shows that the GSROH is an appropriate tool for summarizing oral health status in a low-resource environment. Poorer rating of oral health was significantly associated with being a patient, having pain, having untreated carious tooth, and having a mobile tooth. The GSROH was able to identify individuals with or without oral health compromise, thus making it a valuable tool that can be used in both population-based oral health surveys as well as clinically to assess the oral health needs of patients and in monitoring progress of their treatment.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Thomson WM, Mejia GC, Broadbent JM, Poulton R. Construct validity of Locker's global oral health item. J Dent Res. 2012;91:1038–42. doi: 10.1177/0022034512460676. [DOI] [PubMed] [Google Scholar]
- 2.Locker D. Applications of self-reported assessments of oral health outcomes. J Dent Educ. 1996;60:494–500. [PubMed] [Google Scholar]
- 3.Pattussi MP, Peres KG, Boing AF, Peres MA, da Costa JS. Self-rated oral health and associated factors in Brazilian elders. Community Dent Oral Epidemiol. 2010;38:348–59. doi: 10.1111/j.1600-0528.2010.00542.x. [DOI] [PubMed] [Google Scholar]
- 4.Lawal FB, Olawole WO, Sigbeku OF. Self rating of oral health status by students dental surgeon assistants in Ibadan, Nigeria-a pilot survey. Ann Ib Postgrad Med. 2013;11:12–7. [PMC free article] [PubMed] [Google Scholar]
- 5.Ravaghi V, Underwood M, Marinho V, Eldridge S. Socioeconomic status and self-reported oral health in Iranian adolescents: The role of selected oral health behaviors and psychological factors. J Public Health Dent. 2012;72:198–207. doi: 10.1111/j.1752-7325.2012.00330.x. [DOI] [PubMed] [Google Scholar]
- 6.Subramanian SV, Ertel K. Self-rated health may be adequate for broad assessments of social inequalities in health. Int J Epidemiol. 2009;38:319–20. doi: 10.1093/ije/dyn241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Locker D, Jokovic A. Three-year changes in self-perceived oral health status in an older Canadian population. J Dent Res. 1997;76:1292–7. doi: 10.1177/00220345970760060901. [DOI] [PubMed] [Google Scholar]
- 8.Locker D, Mscn EW, Jokovic A. What do older adults’ global self-ratings of oral health measure? J Public Health Dent. 2005;65:146–52. doi: 10.1111/j.1752-7325.2005.tb02804.x. [DOI] [PubMed] [Google Scholar]
- 9.Okunseri C, Chattopadhyay A, Lugo RI, McGrath C. Pilot survey of oral health-related quality of life: A cross-sectional study of adults in Benin City, Edo State, Nigeria. BMC Oral Health. 2005;5:7. doi: 10.1186/1472-6831-5-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Okunseri C, Hodges JS, Born D. Self-reported toothache experience in an adult population in Benin City, Edo State, Nigeria. Oral Health Prev Dent. 2005;3:119–25. [PubMed] [Google Scholar]
- 11.Adegbembo AO, el-Nadeef MA, Adeyinka A. National survey of dental caries status and treatment needs in Nigeria. Int Dent J. 1995;45:35–44. [PubMed] [Google Scholar]
- 12.4th ed. Geneva: World Health Organization; 1997. World Health Organization. Oral Health Surveys: Basic Methods; pp. 10–52. [Google Scholar]
- 13.Astrøm AN, Haugejorden O, Skaret E, Trovik TA, Klock KS. Oral impacts on daily performance in Norwegian adults: The influence of age, number of missing teeth, and socio-demographic factors. Eur J Oral Sci. 2006;114:115–21. doi: 10.1111/j.1600-0722.2006.00336.x. [DOI] [PubMed] [Google Scholar]
- 14.Locker D. Self-esteem and socioeconomic disparities in self-perceived oral health. J Public Health Dent. 2009;69:1–8. doi: 10.1111/j.1752-7325.2008.00087.x. [DOI] [PubMed] [Google Scholar]
- 15.Kim HY, Patton LL. Intra-category determinants of global self-rating of oral health among the elderly. Community Dent Oral Epidemiol. 2010;38:68–76. doi: 10.1111/j.1600-0528.2009.00513.x. [DOI] [PubMed] [Google Scholar]
- 16.Kim HY, Patton LL, Park YD. Assessment of predictors of global self-ratings of oral health among Korean adults aged 18-95 years. J Public Health Dent. 2010;70:241–4. doi: 10.1111/j.1752-7325.2009.00160.x. [DOI] [PubMed] [Google Scholar]
- 17.Lawal FB, Taiwo JO, Oke GA. Oral health practices of adult inhabitants of a traditional community in Ibadan, Nigeria. Niger J Med. 2013;22:212–7. [PubMed] [Google Scholar]
- 18.Locker D, Clarke M, Payne B. Self-perceived oral health status, psychological well-being, and life satisfaction in an older adult population. J Dent Res. 2000;79:970–5. doi: 10.1177/00220345000790041301. [DOI] [PubMed] [Google Scholar]
- 19.Martins AM, Barreto SM, Silveira MF, Santa-Rosa TT, Pereira RD. Self-perceived oral health among Brazilian elderly individuals. Rev Saude Publica. 2010;44:912–22. doi: 10.1590/s0034-89102010005000028. [DOI] [PubMed] [Google Scholar]
- 20.Locker D, Maggirias J, Wexler E. What frames of reference underlie self-ratings of oral health? J Public Health Dent. 2009;69:78–89. doi: 10.1111/j.1752-7325.2008.00103.x. [DOI] [PubMed] [Google Scholar]
- 21.Afonso-Souza G, Nadanovsky P, Chor D, Faerstein E, Werneck GL, Lopes CS. Association between routine visits for dental checkup and self-perceived oral health in an adult population in Rio de Janeiro: The Pró-Saúde Study. Community Dent Oral Epidemiol. 2007;35:393–400. doi: 10.1111/j.1600-0528.2006.00343.x. [DOI] [PubMed] [Google Scholar]
- 22.Jones JA, Kressin NR, Spiro A, 3rd, Randall CW, Miller DR, Hayes C, et al. Self-reported and clinical oral health in users of VA health care. J Gerontol A Biol Sci Med Sci. 2001;56:M55–62. doi: 10.1093/gerona/56.1.m55. [DOI] [PubMed] [Google Scholar]


