Summary
Abdominal pregnancy is an extremely rare form of ectopic pregnancy, mostly occurring secondarily after tubal rupture or abortion with secondary implantation anywhere in the peritoneal cavity. Massive intra-abdominal hemorrhage is a life threatening complication associated with secondary abdominal pregnancy. Various methods and techniques have been reported in the literature for controlling hemorrhage. Here, we report a case of massive intraperitoneal haemorrhage following placental removal controlled by abdominal packing and review the literature for diagnostic and management challenges.
Keywords: Abdominal pregnancy, abdominal packing, intraperitoneal packing
1. Introduction
Abdominal pregnancy is a rare form ectopic pregnancy occurring in 1 in 10,000 live births to 1 in 30,000 (1). It could be either primary or secondary with the latter being more common. Secondary abdominal pregnancy occurs following a tubal abortion or rupture with secondary implantation in the peritoneal cavity. Primary ectopic pregnancy is diagnosed with studdiford criteria which specifies that both tubes and ovaries should be normal with no tuboperitoneal fistula and an early pregnancy implanted on peritoneal surface which makes the possibility of secondary abdominal pregnancy a rare possibility (2). The main complication of ectopic pregnancy is life threatening hemorrhage. Here, we discuss a case of secondary abdominal pregnancy with profuse intraperitoneal haemorrhage.
2. Case Report
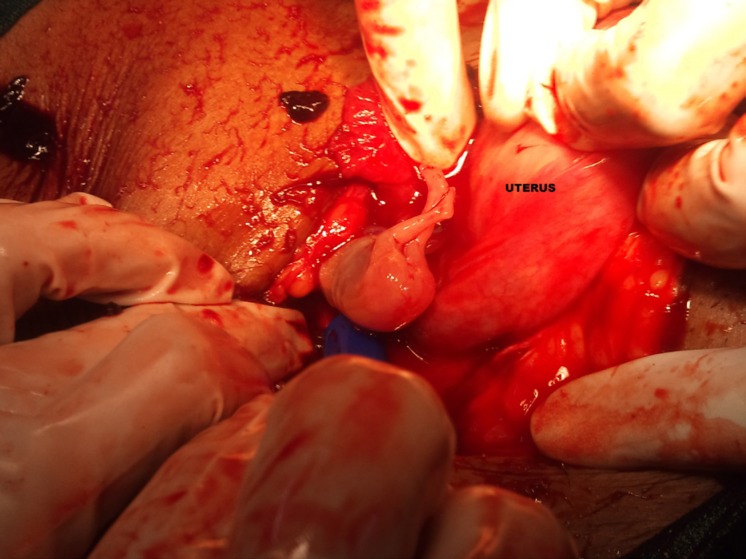
A 28 year lady G2P1LO presented to emergency room with ammenorrhoea for 3 months, lower abdomen pain and bleeding per vaginum for past 7 hours. On examination patient was pale, pulse 120/min, thready and hypovolemic, blood pressure was 90/60 mm Hg. On abdominal examination, there was distention, rigidity and rebound tenderness. On vaginal examination the uterus was normal in size with fullness in all fornices and tenderness in right adenexa. No adnexal lump was present. Urine pregnancy test was positive. Transvaginal Ultrasonography (Figure 1) showed a sac in right adnexa consisting of a 12 weeks old fetus with positive cardiac activity and a collection in the pelvis and abdomen. An empty uterus was seen separately. She was taken up for immediate laparotomy as a suspected case of ruptured ectopic pregnancy in view of her hemodynamic instability. On laparotomy, there was haemoperitoneum, approximately 1.7 litres of blood was drained from abdominal cavity with a live pregnancy within a gestational sac lying in the abdominal cavity. The placenta was found attached to the posterior surface of uterus and posterior leaf of right broad ligament and the peritoneum overlying the ureter (Figure 2). The right tube was distorted, enlarged, edematous and hyperemic with a hole in the mesosalpinx. Right salpingectomy was done as the right tube was distorted and damaged, to prevent recurrence. The placenta was partially separated and its complete removal triggered profuse bleeding from the placental bed, with very friable tissue overlying the peritoneum covering the ureter. Hemostatic sutures were taken to control bleeding from posterior surface of the broad ligament. However bleeding from the peritoneum overlying the ureter continued and a decision to pack the area with ribbon gauze was taken. The packing was limited to posterior surface of uterus and pouch of Douglas. One end of the ribbon gauze was taken out abdominally through the abdominal wound. An abdominal drain was inserted. The opposite fallopian tube and ovary were normal. Patient was transfused 4 units of packed cells and 2 units' fresh frozen plasma and put on antibiotics.
Figure 1.
Ultrasound picture showing live extrauterine pregnancy.
Figure 2.
Per-operative finding of fetus lying in peritoneal cavity.
Pack was removed after 48 hours without any complications. Abdominal drain was removed on third post-operative day. Patient improved and was discharged on sixth post-operative day after stitch removal. However, patient follow up was lost because she failed to report to the outpatient clinic after six weeks.
3. Discussion
Ectopic pregnancy has an average incidence of 1%, however, it accounts for 3–4% of pregnancy related deaths (3). Abdominal pregnancy is rarer and more dangerous with an incidence varying from one per 10,000 births to 1 in 30,000 (1). Abdominal pregnancy is difficult to diagnose and poses a serious risk of morbidity and mortality to the mother and the baby. Maternal mortality ranges between 0 and 30 percent (4). While the perinatal mortality ranges from 40 to 95 percent (5). Clinical diagnosis may be suspected from abdominal pain, vaginal bleeding, adnexal mass, gastrointestinal symptoms, tenderness and in later stages as abnormal lie, superficially palpable fetal parts, painful fetal movements, failed induction of labor and intrauterine fetal death (6–9).
Ultrasound and MRI are helpful in diagnosis when we have a high index of clinical suspicion. The demonstration of an empty uterus adjacent to the bladder, absence of myometrium around the fetus, unusual fetal lie, poor definition of the placenta, and relative oligohydramnios have been described on USG (10,11). Factors such as maternal hemodynamic status, fetal congenital abnormality, fetal viability, gestational age at presentation, and the availability of neonatal facilities should be considered while managing abdominal pregnancies (12). When presenting at an early gestational age the management is laparotomy for removal of the pregnancy because of risk of hemorrhage and association with a much higher incidence of congenital anomalies. With advanced pregnancy when the fetus is at the borderline limits of viability we are faced with the dilemma of continuing the pregnancy at the risk of severe hemorrhage in the mother leading to increased maternal mortality and morbidity versus terminating the pregnancy by elective, well planned laparotomy. It has been reported that if the fetus is surrounded by a normal volume of amniotic fluid, fetal outcome is good and careful wait and watch may be considered until fetal maturity (4). The central controversy in managing abdominal pregnancies is regarding management of the placenta and controlling hemorrhage from the placental bed following placental separation without damage to vital organs like the bowel and is the main clinical challenge (13). Various methods to control hemorrhage have been suggested in the literature. With a confirmed diagnosis of abdominal pregnancy giving pre-operative methotrexate to reduce blood loss at the time of surgery has been suggested (14). Others have preferred leaving the placenta behind (15). But this practice is accompanied by serious risks like secondary hemorrhage, sepsis, failure of lactation, disseminated coagulation, fistulae formation and bowel obstruction due to adhesions (6, 16,17).
Use of post-operative methotrexate for involution of placenta is controversial (18). Selective embolization of placental bed has also been reported in the literature (19). In our patient none of the above procedures were possible because the general condition of the patient was very low at the time of presentation, and profuse bleeding from the bed was continuing. Our institution does not have the facility for embolisation. We resorted to abdominal packing with a successful outcome. One of the main reasons for using abdominal packing in this patient was the friability of the tissue in the placental bed area overlying the ureter with risk of ureteric injury. Abdominal packing has been used effectively for uncontrolled hemorhage following caesarean hysterectomy for morbidly adherent placenta (20) massive hemorrhage during gynecological cancer surgery (21) and for post-partum hemorrhage (22). However, we found no case wherein it has been used to control hemorrhage in secondary abdominal pregnancy. Various types of packs have been described in the literature with the earliest reported being the Logothetopoulos pack (23) others being dry laparotomy packs (23), transcutaneous placement of an inflated condom over a 22 fr catheter (24) or ribbon gauze within a penrose drain (25). Various complications described include a re-laparotomy for removal of pack, post-operative febrile morbidity, sepsis, small bowel obstruction, but no long term complications have been reported.
Intra-abdominal packing proved to be an effective method for controlling hemorrhage and achieving hemostasis in our case.
References
- 1. Badria L, Amarin Z, Jaradat A, Zahawi H, Gharaibeh A, Zobi A. Full-term viable abdominal pregnancy: A case report and review. Arch Gynecol Obstet. 2003; 268:340-342. [DOI] [PubMed] [Google Scholar]
- 2. Studdiford WE. Primary peritoneal pregnancy. Am J Obstet Gynecol. 1942, 44:487-491. [Google Scholar]
- 3. Berg CJ, Callaghan WM, Syverson C, Henderson Z. Pregnancy-related mortality in the United States, 1998 to 2005. Obstet Gynecol. 2010; 116:1302-1309. [DOI] [PubMed] [Google Scholar]
- 4. Martin JN, Jr, McCaul JF., 4th. Emergent management of abdominal pregnancy. Clin Obstet Gynecol. 1990; 33:438-447. [DOI] [PubMed] [Google Scholar]
- 5. Ang LP, Tan AC, Yeo SH. Abdominal pregnancy: A case report and literature review. Singapore Med J. 2000; 41:454-457. [PubMed] [Google Scholar]
- 6. Rahman MS, Al-Suleiman SA, Rahman J, Al-Sibai MH. Advanced abdominal pregnancy — observations in 10 cases. Obstet Gynecol. 1982; 59:366-372. [PubMed] [Google Scholar]
- 7. Kun KY, Wong PY, Ho MW, Tai CM, Ng TK. Abdominal pregnancy presenting as a missed abortion at 16 weeks' gestation. Hong Kong Med J. 2000; 6:425-427. [PubMed] [Google Scholar]
- 8. King M, Bewes PC, Cairns J, Thornton J. Primary Surgery. Volume 1: Chapter 8 nontrauma. On-line edition available at http://www.meb.uni-bonn.de/dtc/primsurg/docbook/html/x5173.html accessed on 4/5/2014 . (accessed December 23, 2014) [Google Scholar]
- 9. Lamina MA, Akinyemi BO, Fakoya TA, Shorunmu TO, Oladapo OT. Abdominal pregnancy: A cause of failed induction of labour. Niger J Med. 2005; 14:213-217. [DOI] [PubMed] [Google Scholar]
- 10. Varma R, Mascarenhas L, James D. Successful outcome of advanced abdominal pregnancy with exclusive omental insertion. Ultrasound Obstet Gynecol. 2003; 21:192-194. [DOI] [PubMed] [Google Scholar]
- 11. Graham D, Johnson TR, Jr, Sanders RC. Sonographic findings in abdominal pregnancy. J Ultrasound Med. 1982; 1:71-74. [DOI] [PubMed] [Google Scholar]
- 12. Shafi SM, Malla MA, Salaam PA, Kirmani OS. Abdominal pregnancy as a cause of hemoperitoneum. J Emerg Trauma Shock. 2009; 2:196-198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Nkusu Nunyalulendho D, Einterz EM. Advanced abdominal pregnancy: Case report and review of 163 cases reported since 1946. Rural Remote Health. 2008; 8:1087. [PubMed] [Google Scholar]
- 14. Gupta P, Sehgal A, Huria A, Mehra R. Secondary abdominal pregnancy and its associated diagnostic and operative dilemma: Three case reports. J Med Case Rep. 2009; 3:7382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hallatt JG, Grove JA. Abdominal pregnancy: A study of twenty-one consecutive cases. Am J Obstet Gynecol. 1985; 152:444-449. [DOI] [PubMed] [Google Scholar]
- 16. Dahab AA, Aburass R, Shawkat W, Babgi R, Essa O, Mujallid RH. Full-term extrauterine abdominal pregnancy: A case report. J Med Case Rep. 2011; 5:531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Pieh-Holder KL, Scardo JA, Costello DH. Lactogenesis failure following successful delivery of advanced abdominal pregnancy. Breastfeed Med. 2012; 7:543-546. [DOI] [PubMed] [Google Scholar]
- 18. Kivikoski AI, Martin C, Weyman P, Picus D, Giudice L. Angiographic arterial embolization to control hemorrhage in abdominal pregnancy: A case report. Obstet Gynecol. 1988; 71:456-459. [PubMed] [Google Scholar]
- 19. Gary Cunningham F, Leveno KJ, Bloom SL, Hauth JC, Rouse D, Spong CY. Williams Obstetrics, 23rd ed., McGraw-Hill Professional, New York, USA, 2009. [Google Scholar]
- 20. Ghourab S, Al-Nuaim L, Al-Jabari A, Al-Meshari A, Mustafa MS, Abotalib Z, Al-Salman M. Abdomino-pelvic packing to control severe haemorrhage following caesarean hysterectomy. J Obstet Gynaecol. 1999; 19:155-158. [DOI] [PubMed] [Google Scholar]
- 21. Finan MA, Fiorica JV, Hoffman MS, Barton DP, Gleeson N, Roberts WS, Cavanagh D. Massive pelvic hemorrhage during gynecologic cancer surgery: “Pack and go back”. Gynecol Oncol. 1996; 62:390-395. [DOI] [PubMed] [Google Scholar]
- 22. Robie GF, Morgan MA, Payne GG, Jr, Wasemiller-Smith L. Logothetopulos pack for the management of uncontrollable postpartum hemorrhage. Am J Perinatol. 1990; 7:327-328. [DOI] [PubMed] [Google Scholar]
- 23. Logothetopoulos K. Eine absolut sichere blutstillungs-methode bei vaginalen undabdominalen gynakologischen operationen. [An absolutely certain method of stopping bleeding during abdominal and vaginal operations]. Zentralbl Gynakol. 1926; 50:3202-3204. [Google Scholar]
- 24. Luijendijk RW, IJzermans JN, Jeekel J, Bruining HA. An inflated condom as a packing device for control of haemorrhage. Br J Surg. 1994; 81:270. [DOI] [PubMed] [Google Scholar]
- 25. Awonuga AO, Merhi ZO, Khulpateea N. Abdominal packing for intractable obstetrical and gynecologic hemorrhage. Int J Gynaecol Obstet. 2006; 93:160-163. [DOI] [PubMed] [Google Scholar]