Summary
Background
Trichobezoar is an uncommon entity observed mostly in young women. Symptoms in presenting patients are usually due to the large mass of the bezoar or malabsorption of nutrients. Trichobezoar is almost always associated with trichotillomania and trichophagia.
Case Report
Three teenage girls, aged 13, 15, and 16, were diagnosed due to palpable epigastric masses. Additionally the oldest patient presented with symptoms of ileus while the other two patients had weight loss and anaemia. Besides the 15-year-old patient complained of paroxysmal abdominal pains. Patients were subjected to plain radiographic examinations of abdomen which revealed large epigastric tumours, with additional calcifications observed in the youngest girl. Subsequent gastroscopy (the 15-year-old patient) or ultrasonographic examination and computed tomography scans (13- and 16-year-old patients) allowed to establish the diagnosis of giant bezoars: trichobezoars in two older patients and tricho-plaster bezoar in the youngest one. All the tumours were surgically resected and psychiatric treatment was undertaken.
Conclusions
1. Trichobezoar should be taken into consideration in differential diagnosis of epigastric tumours in children, especially teenage girls. 2. The conventional ultrasonographic and radiographic examinations of the abdomen are insufficient for determination of the nature of the mass. A thorough medical history interview and clinical examination may give directions regarding the further diagnosis.3. Trichotillomania and trichophagia are obsessive-compulsive disorders, and therefore patients with trichobezoars should be under psychiatric care to prevent recurrence of the disease.
Keywords: Bezoars, Child, Stomach Neoplasms
Background
Bezoars are concrements made of foreign bodies which, undigested by gastric fluids, accumulate within the gastrointestinal tract, most commonly the stomach.
Trichobezoar, i.e. a bezoar made of hair, is an uncommon entity observed mostly in young women.. This article presents case reports of three patients with giant trichobezoars. In one patient, bezoar extended into the small intestine and caused symptoms of gastrointestinal obstruction thus meeting the criteria of Rapunzel syndrome [1]; in the other two patients, bezoars were located exclusively in stomach, with the one in the 13-year-old patient consisting of plaster as well as hair (tricho-plaster bezoar).
Case Report
Case 1
A 15-year-old female patient was admitted to the gastroenterology clinic due to paroxysmal abdominal pain lasting for 2 weeks. Physical examination revealed palpable tumour within the epigastrium as well as evident loss of scalp hair. Other findings included body weight reduction and anaemia. Gastroscopic examination revealed a trichobezoar inside the stomach. The patient was transferred to the Surgery Clinic for approximate estimation of the bezoar size in abdominal radiographic imaging. The examination revealed a large, soft tissue opacity within the mesogastrium and left epigastrium overlapped by the colon (Figure 1). The examination was followed by surgical resection of the trichobezoar sized 30×15×7 cm (Figure 2). The patient was put under psychiatric care.
Figure 1.

Female patient, aged 15 – standing X-ray of the abdomen: a soft tissue opacity mass in the mesogastrium and the right epigastrium overlapped by the colon.
Figure 2.
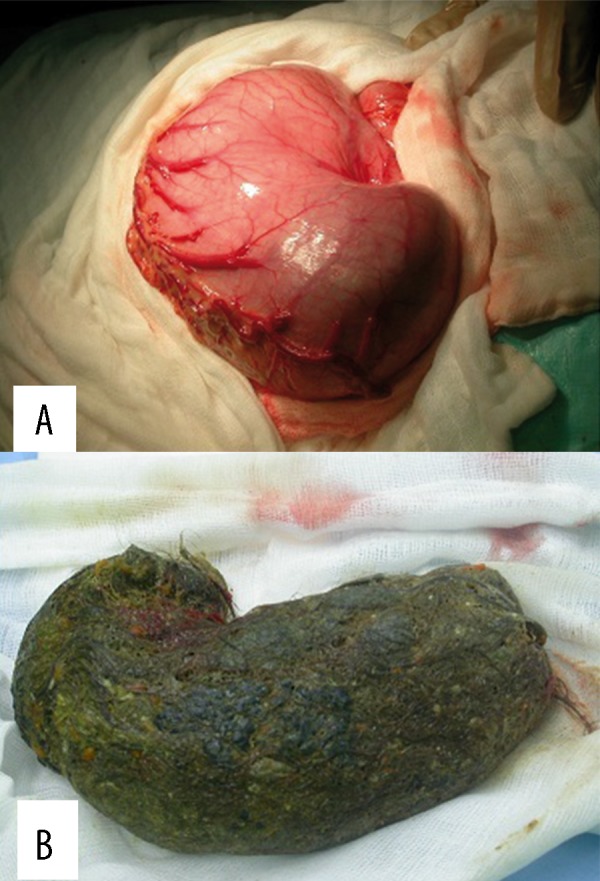
Female patient, aged 15 – intraoperative photographs: giant stomach filled with a bezoar (A); the removed huge trichobezoar reflecting the shape of the stomach (B).
Case 2
A 16-year-old female patient was admitted to the surgery clinic due to an abdominal tumor and symptoms of gastrointestinal obstruction. Physical examination revealed a tumor sized ca. 35×20 cm on the left side of the abdomen (Figure 3). Patient had a history of trichotillomania and trichophagia of ca. 10 years. Abdominal radiography revealed an opacity within the mid-abdominal region with a non-homogeneous, soft tissue opacity mass in the projection of the stomach with two air-fluid levels, most probably at the stomach bottom and prepyloric region as well as several short air-fluid levels within the projection of the right wing of ilium (Figure 4). Ultrasound scan revealed a giant mass with hyperechoic reflections (most probably due to gases). extending from the left epigastrium to the right subcostal region. The remaining organs within the abdominal cavity were unremarkable. A CT was performed following intravenous contrast administration to reveal a large quantity of non-homogeneous content filling a significantly enlarged and extended stomach, extending along duodenum down to the proximal segment of jejunum (Figures 5, 6). A giant bezoar weighing 3 kg extending to the small intestine (Rapunzel syndrome) was resected during the surgery (Figure 7). The patient was put under psychiatric care.
Figure 3.

Female patient, aged 16 – preoperative photograph: a huge mass on the left side of the abdomen, bulging into the abdominal wall.
Figure 4.
Female patient, aged 16 – standing (A) and supine (B) X-ray of the abdomen: a non-homogeneous, soft tissue opacity mass with two air-fluid levels, most probably at the stomach bottom and prepyloric region as well as several short air-fluid levels in the right hypogastrium.
Figure 5.
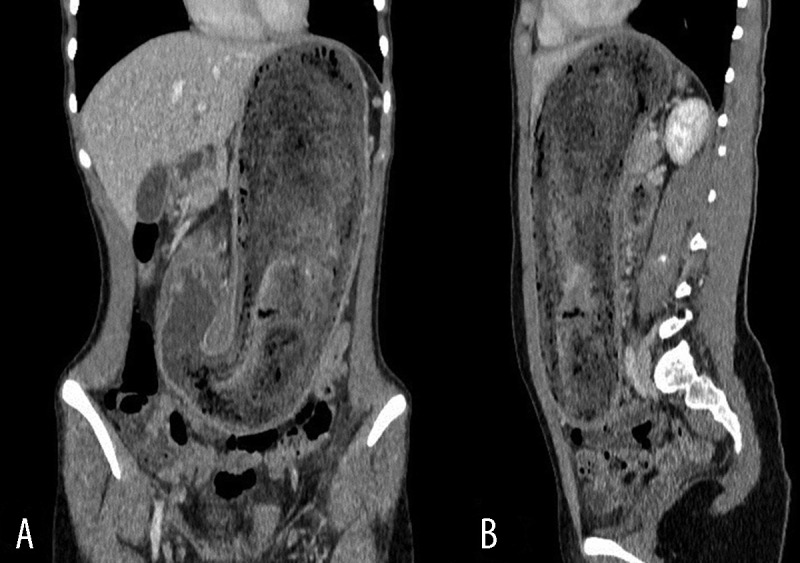
Female patient, aged 16 – coronal (A) and sagittal (B) reformatted CT of the abdomen after intravenous contrast administration: a giant stomach extending from the diaphragm to the hypogastrium with non-homogeneous, non-enhancing content.
Figure 6.

Female patient, aged 16 – transverse CT scan of the abdomen after intravenous contrast administration: giant stomach bulging the outline of the anterior wall of the abdomen, with non-homogeneous, not-enhancing content; distally behind the stomach, the bezoar reaches further down into the small intestine.
Figure 7.

Female patient, aged 16 – the removed trichobezoar, shape reflecting the shape of the stomach and duodenum, with tail extending into the jejunum – Rapunzel syndrome.
Case 3
A 13-year-old female patient growing up in difficult family and socioeconomical conditions was hospitalized in Paediatric Department due to iron deficiency anaemia and left-sided abdominal tumor revealed upon physical examination (ca. 12 cm, hard, only slightly tender). History revealed “very intense hair loss” for about 4 months, abdominal pains and bloating. The patient was treated with iron supplementation, consulted by a dermatologist and an oncologist. Abdominal radiography revealed an opacity and calcifications within the projection of the stomach. The radiologist performing an ultrasound scan suggested a bezoar which was later confirmed by a CT scan. A mass of over 20 cm in length and up to ca. 7 cm in diameter was revealed in the CT scan. Of note were numerous hyperdense elements within and along the outline of the mass (Figure 8). As revealed later on, the patient used to sleep on the upper level of a bunk bed and ingested ceiling plaster as well as own hair; this was responsible for radiological presentation of a tricho-plaster bezoar. The patient was also subjected to surgery (Figure 9) and put under psychiatric care.
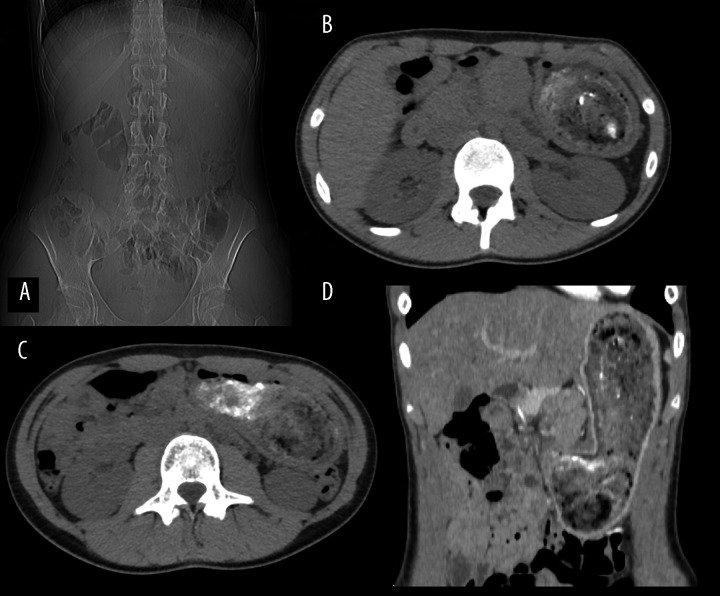
Figure 8.
Female patient aged 13 – invisible gas in the stomach in the pilot sequence of CT (A); a mixture of hair and hyperdense plaster in native scans (B, C); coronal reformatted CT scan after intravenous injection of the contrast medium – stretched stomach containing a non-enhancing mass separated from the stomach wall (D).
Figure 9.

Female patient, aged 13 – intraoperative photograph: a huge trichobezoar with white plaster elements filling the stomach.
Discussion
Bezoars are concrements made of foreign bodies undigested by gastric fluids, accumulated within the gastrointestinal tract, most commonly the stomach. Bezoars are categorized into 4 main groups according to their constituting material: phytobezoars (comprised of undigested fibres from fruit and vegetables), trichobezoars (comprised of hair), lactobezoars (comprised of milk proteins) and pharmacobezoars (comprised of medications) [2]. Phytobezoars are most common, accounting for ca. 40% of all bezoars [3]. The second most common group are trichobezoars, most commonly associated with psychiatric disorders of trichotillomania (urge to pull out one’s hair) and trichophagia (urge to eat one’s hair). However, trichobezoars develop in only about 1% of patients with these disorders [4].
Trichobezoars are diagnosed almost exclusively in adolescent females, although cases of several-years-old children were also reported [4,5]. Trichobezoars are very rarely detected in young male patients [6–8].
Usually, trichobezoars develop within the stomach, although locations within the small intestine are also possible [5,6].
The Rapunzel syndrome [1] (also referred to in Polish literature as Roszpunka syndrome [9] or Raszpunka syndrome [10]) is a rare trichobezoar extending beyond the stomach along the duodenum down to the small intestine. Very scarce reports are available in Polish literature regarding both Rapunzel syndrome [8–10] and bezoars as such [11,12].
Clinical symptoms related to the presence of a trichobezoar within the gastrointestinal tract are characterized by late onset and lack of specificity, causing late diagnosis. Diagnostic procedures are commonly initiated due to acute abdominal symptoms. Most commonly, bezoars are palpable as well-delimited, movable tumors within the left epigastrium. Differential diagnosis of the left-sided epigastric tumors in children is presented in Table 1 [7]. Other common symptoms include abdominal pain, nausea and vomiting, constipation, body weight loss, anorexia, haematemesis (Table 2) [1]. Frequently, patients report due to trichobezoar complications including gastric ulceration, obstructive jaundice, intestinal perforation, acute pancreatitis, stomach dilatation, intestinal intussusception, or peritonitis. Bezoar-related intestinal obstruction is rare [5,6].
Table 1.
The most common left-sided epigastric tumours.
| Left liver-lobe tumour |
| Splenomegaly |
| Neuroblastoma |
| Gastric tumor |
Table 2.
The most common clinical symptoms of trichobezoar [1].
| Symptom | Incidence |
|---|---|
| Palpable tumour in abdominal cavity | 87.7% |
| Abdominal pain | 70.2% |
| Nausea, vomiting | 64.9% |
| Weakness, weight loss | 38.1% |
| Constipation and diarrhea | 32.0% |
| Haematemesis | 6.1% |
Plain radiograms of the abdominal cavity usually reveal a soft tissue mass in an enlarged stomach.
Examination of choice is the contrast-enhanced scan of the upper gastrointestinal tract [6]. The image is that of a mass within the stomach, separated from stomach wall.
Ultrasonography is of limited value in the diagnostics of trichobezoar [6]. Typically, the examination reveals a lesion with hyperechoic reflections; however, the high echogeneity of hair and the presence of numerous acoustic shades due to air bubbles trapped between the hair limits its assessment capabilities. There is a possibility that a bezoar would not be visualized by an ultrasound scan.
Computed tomography is the best tool in the diagnostics of trichobezoars. The image is quite characteristic, consisting of a well-delimited, non-enhanced mass filling the stomach and the small intestine, with a spotted pattern due to air being trapped between hair. CT scans facilitate evaluation of the tumor size, locations, and potential complications [6].
Diagnosis of trichobezoar is easier when the above symptoms are visualized in radiograms and accompanied by an evident loss of hair from patient’s scalp. An additional difficulty may be posed by the presence of trichophagia without trichotillomania – the literature contains a case report of a patient eating hair that was not her own as well as clay [13].
The treatment approaches depend on the size and the location of the bezoar. Small bezoars may be removed by endoscopic techniques, chemical dissolution or fragmentation. Large bezoars should be surgically resected. What’s interesting, literature contains reports of successful treatments of bezoars with Coca-Cola, with the reported doses substantially varying from 1 can of Diet Coke combined with 1 tablet of cellulase two times a day until dissolution of the bezoar which usually takes 6–8 weeks [14]; through 3L administered via a gastric tube over 12 hours [3] up to 4.8 L drank over 12 hours (100 mL every 15 minutes) [15].
Recurrent bezoars as well as recurrent Rapunzel syndrome have been reported, most commonly in patients in whom no psychiatric treatment had been initiated [5,16].
Conclusions
Trichobezoar should be taken into consideration in differential diagnosis of epigastric tumours in children, especially teenage girls.
The conventional ultrasonographic and radiographic examinations of the abdomen are insufficient for the diagnosis of a bezoar. A thorough medical history interview and clinical examination may give directions regarding the further diagnosis.
The obsessive-compulsive nature of trichotillomania and trichophagia require appropriate psychiatric care to prevent the recurrence of the disease.
References
- 1.Naik S, Gupta V, Naik S, et al. Rapunzel syndrome reviewed and redefined. Dig Surg. 2007;24(3):157–61. doi: 10.1159/000102098. [DOI] [PubMed] [Google Scholar]
- 2.Sanders M. Bezoars: from mystical charms to medical and nutritional management. Practical Gastroenterology. 2004;28:37–50. [Google Scholar]
- 3.Eng K, Kay M. Gastrointestinal bezoars: history and current treatment paradigms. Gastroenterol Hepatol (N Y) 2012;8(11):776–78. [PMC free article] [PubMed] [Google Scholar]
- 4.Gonuguntla V, Joshi DD. Rapunzel syndrome: a comprehensive review of an unusual case of trichobezoar. Clin Med Res. 2009;7(3):99–102. doi: 10.3121/cmr.2009.822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khattala K, Boujraf S, Rami M, et al. Trichobezoar with small bowel obstruction in children: two cases report. Afr J Paediatr Surg. 2008;5(1):48–51. doi: 10.4103/0189-6725.41639. [DOI] [PubMed] [Google Scholar]
- 6.Jain M, Solanki SL, Bhatnagar A, et al. An unusual case report of rapunzel syndrome trichobezoar in a 3-year-old boy. Int J Trichology. 2011;3(2):102–4. doi: 10.4103/0974-7753.90820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pace AM, Fearne C. Trichobezoar in a 13 year old Male: A case report and review of literature. Malta Medical Journal. 2003;1:39. [Google Scholar]
- 8.Pytrus T, Sawicz-Birkowska K, Iwańczak F, et al. Zespół Rapunzel – bezoar żołądka i jelita cienkiego u 7-letniego chłopca. Gastroenterol Pol. 2003;10(1):91–94. [in Polish] [Google Scholar]
- 9.Mańkowski P, Rólski M, Derwich K, et al. Zespół Rapunzel – olbrzymi trichobezoar żołądka u 11-letniej dziewczynki. Pediatr Pol. 2006;81(10):768–70. [in Polish] [Google Scholar]
- 10.Taczalska A, Nowosławska-Łuniewska K, Koziarkiewicz M, et al. Bezoars – diagnostic problems based on own observations and literature review. Med Wieku Rozwoj. 2013;17(3):265–69. [PubMed] [Google Scholar]
- 11.Pachana J, Szczerba D. Giant gastro-duodenal trichobezoar – CT appearance. Pol J Radiol. 2004;69(4):118–20. [Google Scholar]
- 12.Raszke K, Domański Z. Obraz rentgenowski grzybów drożdżopodobnych i bezoarów w żołądku po wagotomii i pyloroplastyce. Pol J Radiol. 1976;40(1):17–21. [in Polish] [PubMed] [Google Scholar]
- 13.Mehra A, Avasthi A, Gupta V, Grover S. Trichobezoar in the absence of trichotillomania. J Neurosci Rural Pract. 2014;5:55–57. doi: 10.4103/0976-3147.145204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kramer SJ, Pochapin MB. Gastric phytobezoar dissolution with ingestion of diet coke and cellulase. Gastroenterol Hepatol (NY) 2012;8(1):770–72. [PMC free article] [PubMed] [Google Scholar]
- 15.Mihai C, Mihai B, Drug V, et al. Gastric bezoars – diagnostic and therapeutic challenges. J Gastrointestin Liver Dis. 2013;22(1):111. [PubMed] [Google Scholar]
- 16.Memon SA, Mandhan P, Qureshi JN, et al. Recurrent Rapunzel syndrome – a case report. Med Sci Monit. 2003;9(9):CS92–94. [PubMed] [Google Scholar]