Abstract
Purpose
While spouses play a vital role in the care of cancer patients, caregiving exerts a physical and psychological toll. Caregiving burden may not only compromise spouses’ quality of life but also the quality of care and support they are able to provide. Consequently, spousal caregiving burden may also negatively impact patients’ psychological adjustment. However, the effect of caregiving burden on patients’ psychological distress is unknown. Thus, this 6-month longitudinal study examined the associations between caregiving burden and distress in both lung cancer patients and their spouses.
Methods
Patients and their spouses individually completed questionnaires within 1 month of treatment initiation (baseline) and at 3-month and 6-month follow-up. Distress was measured with the Brief Symptom Inventory and caregiving burden with the Caregiver Reaction Assessment.
Results
Multilevel modeling of data from 158 couples revealed that baseline spouses’ reports of caregiving-related health problems were significantly associated with 3-month (p<0.001) and 6-month (p=0.01) follow-up distress in both patients and spouses even when controlling for baseline distress and dyadic adjustment. Further, there was evidence that baseline spouses’ reports of schedule disruption (p=0.05) predicted 3-month patients’ distress and baseline spouses’ reports of financial strain (p<0.05) and lack of support (p<0.10) predicted their own distress at 6-months.
Conclusion
Caregiving burden is problematic for both patients and spouses. Couples in which spouses report caregiving-related health problems may be at particular high risk of long-term elevated distress. Targets of future couple-focused interventions such as self-care and use of social support are discussed.
Keywords: Lung cancer, caregiving reactions, couples, distress, prospective research
INTRODUCTION
Throughout the course of the illness trajectory, cancer not only affects the quality of life (QOL) of patients but also their family members [1]. To successfully cope with the diagnosis and treatment of cancer, patients need support from their close others. Most often, patients’ spouses or partners are the primary [2] and the most valued source of support and care [3]; yet, as spouses deal with patients’ deteriorating health, ongoing caregiving demands, and fear of possible loss of their loved one, they tend to be as distressed as patients themselves [4]. Caregiving exerts both emotional and physical tolls and spousal caregivers of cancer patients are at greater risk of depression, coronary heart disease and stroke compared to population controls [5–8]. Importantly, caregiving burden may undermine the quality of care spouses are able and willing to provide, which may compromise patients’ cancer adjustment and recovery.
Given that cancer profoundly affects the lives of both patients and spouses [9], caregiving burden is likely to be associated with the psychological adjustment of both members of the couple. In fact, research has shown that psychosocial factors such as distress, dyadic adjustment, and overall QOL [4, 10–13] are interdependent processes in couples coping with cancer so that spousal outcomes influence patient outcomes and vice versa. While most studies have focused on identifying antecedents (e.g., patient characteristics) and consequences (e.g., caregiver’s health and QOL) of caregiving burden [14] as well as coping resources (e.g., social support and mastery) aiming to prevent burden [15], the impact of caregiving on patient outcomes is generally unknown. Considering the interdependent nature of couples, this study seeks to examine the associations between caregiving burden and distress in both members of the couple.
It is important to note that, even though caregiving is generally deemed as burdensome (e.g., schedule disruptions, financial strain, health problems, and lack of family support), it may also be considered positively because it may foster one’s self-worth and feelings of closeness [16]. In fact, caregiving has also been linked to health and well-being [17, 18]. A recent qualititative study revealed that, in addition to themes related to distress and unbalance, caregivers expressed themes of gaining strength and perspective [19]. Thus, we also wanted to examine positive reactions (i.e., caregiving esteem) related to caring for a spouse or partner with cancer and its potential buffering association with distress.
The Current Study
The current research seeks to examine the associations between caregiving reactions (i.e., burden and esteem) and psychological distress in lung cancer patients and their spouses. We were interested in this population because lung cancer is not only the most prevalent cancer in the United Sates affecting both men and women, it also leads to more debilitating physical and psychological sequelae than other cancer disease sites [20, 21]. Considering the high symptom burden, it is not surprising that patients’ need for physical care and emotional support are high [22–24] and spouses of lung cancer patients report greater anxiety and depression compared to partners of other cancer sites [25]. Consequently, lung cancer patients and their spouses may be vulnerable to distress as a function of caregiving-related burden.
Research has shown that, while some patients and spouses seem to psychologically adapt to cancer quite well, others may remain distressed across the illness trajectory [19, 25–27]. For instance, group-based trajectory modeling of caregivers’ (90% spouses) adjustment over time revealed that, even though the group with borderline anxiety scores (33%) deceased over a 12-month period, the group with clinical anxiety levels (14%) and borderline or clinical depression levels (30%) remained unchanged across time [25]. Because of previously reported variability in patient and spousal psychological adjustment of over time, we were interested in determining if distress levels at 3-month and 6-month post-treatment initiation are a function of caregiving burden and esteem. Additionally, we were interested in establishing a direction of effect and thus examined prospective analyses with baseline levels of burden and esteem predicting follow-up distress. Lastly, we were interested in examining whether these associations differed for patients and spouses. Considering that caregiving is a spousal construct, the associations between spouses’ reports of their caregiving burden/esteem and their own distress may be stronger than the associations between caregiving reactions and patient distress.
In summary, we examined the following primary hypotheses: we expected that 1) caregiving burden is positively associated with distress and 2) caregiving esteem is negatively associated with distress in both patients and spouses at baseline and follow-up assessments. We also expected that caregiving burden and esteem are associated with distress prospectively over time so that baseline caregiving reactions predict follow-up distress while controlling for baseline distress. Additionally, we conducted exploratory analyses to examine if the prospective associations between caregiving reactions and distress are moderated by social role (patient vs. spouse) so that the strength of these associations is different for spouses and patients.
METHODS
Participants
The current data are part of a longitudinal study of the psychological and relationship functioning of couples coping with lung cancer [4, 12, 13]. Data were collected at baseline (within 1 month of treatment initiation) and 3 and 6 months later. Patients were eligible if they: 1) were within one month of initiating treatment for lung cancer (all types); 2) had a physician-rated Eastern Cooperative Oncology Group performance status score ≤2 meaning, at minimum, patients were up more than 50% of waking hours and ambulatory and capable of all self-care but unable to carry out any work activities [28]; 3) were able to provide informed consent; 4) could speak, read, and understand English; 5) were age 18 years or older; and 6) had a partner (spouse or significant other) with whom they had lived for at least 1 year.
We obtained consent from 270 patients and their spouses; 158 (59%) of these couples returned the baseline questionnaire; there were an additional 11 couples in which only the patient returned a survey and nine couples in which only the spouse returned a survey. Detailed recruitment information was previously described [4]. Two patients who had completed the baseline survey died before the 3-month assessment, so only 156 sets of the 3-month surveys were mailed and returned. Prior to mailing the 6-month assessment, six patients died and 12 couples withdrew so that only 140 sets of surveys were mailed, of which 108 (68% of the original 158 couples) were returned. Detailed information regarding study attrition has been reported elsewhere, demonstrating no significant differences between study completers and non-completers regarding demographic and medical characteristics [12]. Further analyses based on t tests indicated that patients and spouses who did not complete the 6-month follow-up surveys did not significantly differ from completers regarding baseline distress; however, spouses who did not complete the 6-month assessment reported greater caregiving-related health problems and scheduling disruptions (p < 0.05) and marginally greater lack of family support (p < 0.09) at baseline compared to study completers.
Procedure
Study procedures were approved by The University of Texas MD Anderson Cancer Center’s Institutional Review Board. Patients and their spouses were approached during appointments in the Thoracic Clinic and screened for eligibility. After providing informed consent, patients and spouses separately completed paper-pencil questionnaires and returned them in individually sealed postage-paid envelopes. Follow-up surveys were mailed 3 and 6 months later to couples who had completed the baseline questionnaires. Participants received $10 gift cards for survey completion (up to $60 total per couple).
Measures
Psychological distress
Patients and spouses completed the well-validated Brief Symptom Inventory [29], a 53-item self-report measure of psychological functioning over the past week in nine symptom dimensions. It also yields a global severity index. A t-score ≥63 on the global severity index or on two of the Brief Symptom Inventory’s nine primary dimensions defines “caseness” for distress and indicates a need for further clinical evaluation. The primary outcome in this study is the global severity index raw scores.
Caregiving reactions
Spouses completed the Caregiver Reaction Assessment (CRA) [30], which has been validated in cancer caregiving populations [18]. This 24-item instrument measures caregivers’ reactions to caring for the patient across four negative domains: lack of family support (5 items; e.g., “Since caring for my spouse, I feel my family has abandoned me,” alpha = .75); financial strain (3 items; e.g., “caring for my spouse has put a financial strain on the family,” alpha = .82); schedule disruption (5 items; e.g., “I have eliminated things from my schedule since caring for my spouse,” alpha = .68); and health problems (4 items; e.g., “Since caring for my spouse, it seems like I’m tired all the time,” alpha = .72). Spouses were asked to indicate their degree of agreement with each item on a 5-point Likert scale ranging from [1] = “strongly agree” to [5] = “strongly disagree.” Higher scores on each subscale indicated a greater degree of caregiving burden. The instrument also includes one positive reaction: caregiving esteem (6 items; e.g., “I feel privileged to care for my spouse,” alpha = .80). Higher scores denote greater esteem. Consistent with previous recommendations regarding the psychometric quality of this measure [18], we omitted one of the items on the caregiver esteem subscale (“I will never be able to do enough caregiving to repay my partner”) to increase internal consistency from .76 to .80.
Dyadic adjustment
Patients and spouses also completed the 32-item Dyadic Adjustment Scale, which assesses four components of marital adjustment: consensus, satisfaction, cohesion, and affectionate expression [31]. Alpha coefficients for patients’ and spouses’ scores were .91 and .90, respectively.
Demographic/medical factors
At baseline, patients and spouses also provided demographic information including age, sex, level of education, race/ethnicity, marital status, and employment status. Patients were asked questions about their disease, including time since diagnosis, treatments, and disease stage.
Data Analysis Strategy
We calculated descriptive statistics (e.g., means, standard deviations, correlations) for continuous variables and performed paired t tests to determine whether mean scores differed for patients and spouses. Additionally, we performed paired t tests to examine whether participants’ baseline scores differed from the 3-month and 6-month follow-up scores. We performed prospective analyses to examine if caregiving burden (i.e., lack of family support, financial strain, schedule disruptions, and health problem) and caregiving esteem predict follow-up distress while controlling for baseline levels of distress. Because previous work revealed a link between caregiving burden and dyadic adjustment [5], which in turn is linked to distress in couples coping with lung cancer [4, 32], we controlled for dyadic adjustment to isolate caregiving processes from the larger context of the couple’s relationship. Considering that none of the assessed demographic variables (i.e., age, sex, race/ethnicity, level of education, employment status) and patients’ medical factors (i.e., time since diagnosis, Eastern Cooperative Oncology Group performance status, stage of disease, treatment initiation and type of treatment) were significantly associated (p<.05) with the outcome variable (i.e., distress), we did not include them as covariates. We used a multilevel modeling technique in which the couple was the unit of analysis [33] with the Proc MIXED procedure in SAS [34]. As opposed to the general linear model, multilevel modeling allows testing of nonindependent (e.g. dyadic) data without introducing bias to the probability estimates. Additionally, instead of using list-wise deletion for cases with missing data, Proc MIXED uses a likelihood-based estimation method for missing data so that attrition is less of a concern for the prospective analyses [35]. We conducted separate multilevel models for each type of caregiving burden (i.e., lack of family support, financial strain, schedule disruptions, and health problem) and esteem. The predictor variables were centered at their grand mean [33]; dummy coding was used for social role (patient=1 and spouse=0), and effect sizes were calculated using the formula r=[t2/(t2+df)]1/2 [36] for significant effects. Effect sizes were interpreted based on Cohen’s taxonomy [37, 38] (small effect: r=.10; medium effect: r=.30; and large effect: r=.50). Because we were interested in whether these associations differ for patients and spouses, we regressed participants’ 3-month follow-up distress on the interaction between caregiving burden and esteem and social role (i.e., patient or spouse). In case of significant interactions, we used simple slope analyses as outlined by Preacher et al. [39]. We repeated these analyses for the 6-month follow-up.
RESULTS
Descriptive Results
Sample characteristics
Table 1 summarizes baseline demographic and medical characteristics of the sample.
Table 1.
Baseline Demographic and Medical Characteristics of Lung Cancer Patients and their Spouses.
| Characteristic | Patients (N=169) | Spouses (N=167) |
|---|---|---|
| Men (%) | 63.7 | 32.9 |
| White (%) | 89.3 | 91.0 |
| Hispanic or Latino (%) | 4.8 | 2.4 |
| Age (mean ± standard deviation) (range), years | 62.9±10.1 (30.3–86.6) | 60.5±11.1 (30.6–86.4) |
| Married (%) | 95.8 | |
| Length of marriage (mean ± standard deviation), years | 25.57 ± 13.02 | |
| College ≥2 yrs (%) | 61.3 | 57.5 |
| Employment status (%) | ||
| Full-time | 33.9 | 37.5 |
| Part-time | 5.4 | 7.5 |
| Unemployed | 10.1 | 7.5 |
| Retired | 50.6 | 47.5 |
| Time since diagnosis (mean ± standard deviation), months | 2.3 ± 1.7 | |
| Disease stage at initial diagnosis (%) | ||
| I | 16.3 | |
| II | 14.5 | |
| III | 32.5 | |
| IV | 36.7 | |
| Lung cancer type (%) | ||
| NSCLC | 86.8 | |
| SCLC | 9.6 | |
| Other | 3.6 | |
| Had initiated treatment (%) | ||
| Yes | 57.1 | |
| Type of treatment* (%) | ||
| Chemotherapy | 55.8 | |
| Radiotherapy | 24.2 | |
| Chemoradiotherapy | 3.2 | |
| Surgery | 16.8 |
Note: NSCLS, non-small cell lung cancer; SCLC, small-cell lung cancer
percentages of those who had initiated treatment at baseline assessment.
Caregiving burden and esteem
Table 2 shows means and standard deviations of spouses’ caregiving burden and esteem and paired t test results at each assessment. Mean scores for schedule disruption and caregiving esteem remained stable across assessment points. However, spouses reported significantly greater lack of family support (p<0.0001) and more health problems (p<0.05) but less financial strain (p<0.05) at 3-month follow-up compared to baseline. At 6-month follow-up, again, spouses reported greater lack of family support (p<0.01) but less financial strain (p<0.05) compared to baseline.
Table 2.
Means and standard deviations, and paired t tests results for spouses’ caregiving burden and esteem and correlations with patients and spouses’ distress scores at baseline and 3-months and 6-months follow-up.
| Caregiving Reaction |
Mean ± Standard Deviation (Range) |
Paired t testˆ Baseline and |
Correlation Coefficient | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Baseline (N=164) | 3-months | df | 6-months | df | Patient Distress | Spouse Distress | Patient Dyadic Adjustment | Spouse Dyadic Adjustment | |
| Schedule Disruption | 2.99±0.79 (1.2–5) | 0.83 | 115 | 1.65 | 93 | .04 | .20* | .05 | −.18* |
| Lack of Family Support | 1.74±0.68 (1–3.8) | −3.82*** | 113 | −3.19** | 92 | .08 | .19* | −.24** | −.35*** |
| Health Problems | 2.03±0.76 (1–4.5) | −2.43* | 114 | −1.08 | 92 | .04 | .34** | −.27*** | −.42*** |
| Financial strain | 2.61±1.02 (1–5) | 2.46* | 112 | 2.23* | 92 | .21* | .25** | −.19** | −.34*** |
| Caregiver Esteem | 4.31±0.54 (2.71–5) | 1.20 | 115 | 0.84 | 93 | −.00 | .03 | .24** | .47*** |
| 3-month Follow-up (N=119) | |||||||||
|
| |||||||||
| Schedule Disruption | 2.92±0.83 (1.2–5) | .35** | .27** | −.13 | −.30** | ||||
| Lack of Family Support | 1.88±0.71 (1–3.8) | .22* | .44** | −.22* | −.59*** | ||||
| Health Problems | 2.12±0.80 (1–4) | .40** | .44** | −.23* | −.47*** | ||||
| Financial strain | 2.33±0.96 (1–4.) | .16+ | .31** | −.06 | −.39*** | ||||
| Caregiver Esteem | 4.3±0.54 (2.9–5) | .02 | −.22* | .13 | .53*** | ||||
| 6-month Follow-up (N=97) | |||||||||
|
| |||||||||
| Schedule Disruption | 2.79±0.88 (1–4.8) | .12 | .33** | .08 | −.13 | ||||
| Lack of Family Support | 1.91±0.75(1–4) | .16 | .41** | −.14 | −.34*** | ||||
| Health Problems | 2.10±0.79 (1–4) | .03 | .43** | −.03 | −.35*** | ||||
| Financial strain | 2.33±1.01 (1–5) | .03 | .39** | −.03 | −.23* | ||||
| Caregiver Esteem | 4.23±0.54 (2.7–5.0) | −.04 | −.26** | .19 | .35*** | ||||
Note
Paired t test examined differences in baseline and follow-up assessment.
p < 0.10
p<.05.
p<.01.
p<.001.
Psychological distress
Raw global severity scores on the Brief Symptom Inventory were .41 (SD=.37), .40 (SD=.36) and .46 (SD=.51) for patients and .45 (SD=.42), .38 (SD=.36) and .39 (SD=.40) for spouses at baseline, 3-month and 6-month, respectively. Paired t test analyses revealed that the global severity scores did not differ between patients and their spouses at baseline (t(142)=−1.09, p=0.28) or the 3-month (t(111)=0.217, p=0.83) and 6-month (t(84)=1.32, p=0.19) follow-up assessments. Pertaining to change over time, paired t test analyses also revealed that distress scores at baseline did not significantly differ from scores at 3-month for both patients and spouses (t(116)=−0.79, p=0.47; t(109)=1.23, p=0.21, respectively). While scores remained unchanged for patients (t(92)=−0.75, p=0.46) at 6-month follow-up, spouses reported significantly less distress (t(92)=1.95, p=0.05) compared to baseline.
Main Analyses
Primary hypotheses
Caregiving burden is positively associated with distress and caregiving esteem is negatively associated with distress in both patients and spouses.
Cross-sectional associations between caregiving burden and esteem and distress
Table 2 shows correlation coefficients between caregiving burden and esteem, distress and dyadic adjustment scores at each assessment. As expected, for spouses, types of caregiving burden were positively associated with distress and negatively associated with dyadic adjustment. Caregiving esteem was negatively associated with spouses’ distress scores and positively associated with their dyadic adjustment. Based on Cohen’s taxonomy [37, 38], effect sizes fell into the small to medium range. Correlations were less consistent for patients. While at baseline only financial strain was positively correlated with patients’ distress scores (small effect size), each type of caregiving burden was significantly associated with distress at 3-month follow-up (small and medium effect sizes). At 6-month follow-up, none of the caregiving burden subscales were significantly associated with patients’ distress scores. Caregiving esteem was not significantly associated with patient distress at any time point. At baseline and to some extent at 3-month follow-up, caregiving burden/esteem was significantly associated with patients’ dyadic adjustment in the hypothesized direction (small and medium effects sizes).
Prospective associations between caregiving burden and esteem on distress
There was a significant main effect of baseline health problems (t(135)=3.89, p<0.001) predicting 3-month follow-up distress even with baseline distress (t(210)=6.20, p<0.0001) and dyadic adjustment (t(204)=−1.11, p =0.26) in the model. A greater degree of health problems related to caregiving was associated with greater levels of 3-month follow-up distress for both patients and spouses. This main effect (t(98)=2.55, p<0.05) was significantly replicated when predicting 6-month follow-up distress.
Baseline reports of schedule disruption, financial strain and lack of family support as well as caregiving esteem were not significantly associated with the two follow-up assessments of distress.
Exploratory analyses
Do the prospective associations between caregiving burden/esteem and distress differ for spouses and patients?
Schedule Disruption
There was a significant interaction between baseline schedule disruption and social role predicting 3-month follow-up (t(109)=−1.97, p=0.05). Simple slope analyses revealed that for patients, but not spouses (t=−0.07, p=0.95), schedule disruption was significantly associated with later distress (t=5.52, p <0.05) so that patients reported greater distress at 3-month follow-up when spouses had indicated a greater degree of schedule disruption at baseline. Table 3 and Figure 1 illustrate this finding. When predicting 6-month follow-up distress, the interaction was not significant.
Table 3.
Prospective analysis results examining the moderation between spouses’ baseline schedule disruption and social role predicting distress at 3-month follow-up while controlling for baseline distress and dyadic adjustment.
| 3-Month Follow-Up Distress (N=112 Couples) | ||||
|---|---|---|---|---|
| Baseline Variables | B | SE | t | r |
| Intercept | 0.41 | 0.02 | ||
| Distress | 0.40 | 0.06 | 6.56*** | .42 |
| Dyadic Adjustment | −0.00 | 0.00 | −2.50* | |
| Schedule disruption | 0.08 | 0.03 | 2.54* | .18 |
| Role | −0.06 | 0.03 | −1.86+ | .17 |
| Schedule disruption × Role | −0.08 | 0.04 | −1.97* | .19 |
Notes:
p < 0.10
p=0.05
p < 0.05
p < 0.01.
B, raw coefficient; SE, Standard Error, Role, Social Role (patient=1, spouse=0). Effect size r=[t2/(t2+df)]1/2. B, raw coefficient;
Fig. 1.
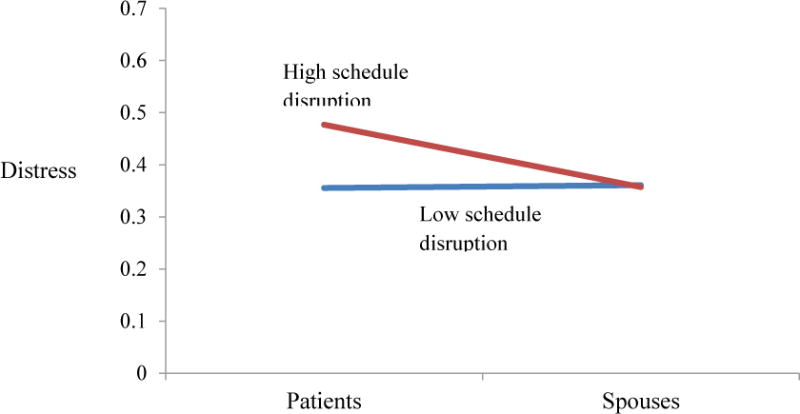
A multilevel model analysis reveals an interaction (p=0.05) depicting 3-month follow-up distress as a function of baseline schedule disruption and social role. Scores are plotted at the mean ±1 standard deviation. Higher scores indicate greater distress.
Financial strain
When predicting 3-month follow-up distress, the interaction of baseline financial strain and social role was not significant. However, when predicting 6-month follow-up distress, the interaction was significant (t (86)=2.49, p < 0.05). Based on simple slope analyses, baseline financial strain was significantly associated with distress at 6-month for spouses (t=2.53, p=0.01) but not patients (t= −0.61, p=0.511). Spouses who reported a greater degree of financial strain at baseline indicated more distress at 6-month. Table 4 and Figure 2 illustrate this finding.
Table 4.
Prospective analyses results examining the moderation between spouses’ baseline caregiving burden (financial strain and lack of family support) and social role predicting distress at 6-month follow-up while controlling for baseline distress and dyadic adjustment.
| Outcome: 6-Month Follow-Up Distress (N=108 Couples) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Financial Strain | Lack of Family Support | ||||||||
|
| |||||||||
| Baseline Variables | B | SE | t | r | Baseline Variables | B | SE | t | r |
| Intercept | 0.43 | 0.03 | Intercept | 0.43 | 0.03 | ||||
| Distress | 0.56 | 0.07 | 8.12*** | .33 | Distress | 0.58 | 0.07 | 8.18*** | .53 |
| Dyadic adjustment | 0.00 | 0.00 | 0.34 | Dyadic adjustment | 0.00 | 0.00 | 0.05 | ||
| Financial strain | −0.02 | 0.03 | −0.58 | Lack of support | −0.01 | 0.05 | −0.27 | ||
| Role | −0.05 | 0.04 | −1.13 | Role | −0.06 | 0.04 | −1.38 | ||
| Financial strain × Role | 0.10 | 0.04 | 2.49* | .26 | Lack of support × Role | 0.11 | 0.06 | 1.64+ | .18 |
Notes:
p < 0.10
p=0.05
p <0.05
p < 0.01.
B, raw coefficient; SE, Standard Error, Role, Social Role (patient=1, spouse=0). Lack of support, Lack of family support; Effect size r=[t2/(t2+df)]1/2. B, raw coefficient;
Fig. 2.
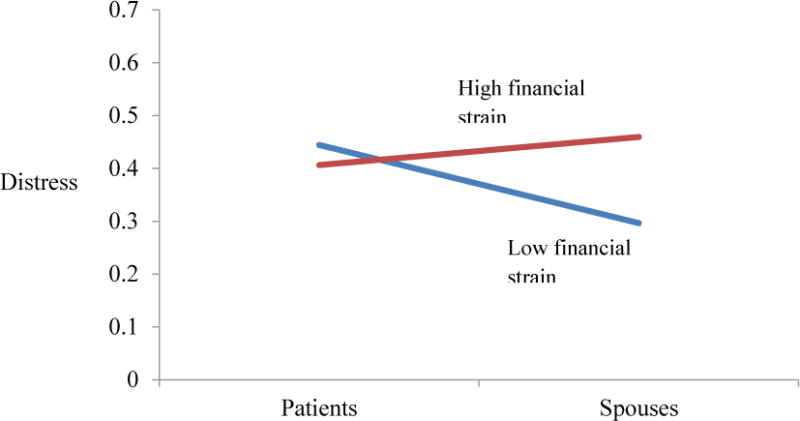
A multilevel model analysis reveals an interaction (p < 0.05) depicting 6-month follow-up distress as a function of baseline financial strain and social role. Scores are plotted at the mean ±1 standard deviation. Higher scores indicate greater distress.
Lack of Family Support
When predicting 3-month follow-up distress, the interaction of baseline lack of family support and social role was not significant. There was a trend in the hypothesized direction (t(83)=1.64, p=0.10) when examining 6-month follow-up distress. Simple slope analyses revealed that lack of family support was associated with 6-month distress for spouses (t= 1.74, p=0.08) but not patients (t= −0.30, p=0.77). Table 4 and Figure 3 illustrate this finding.
Fig. 3.
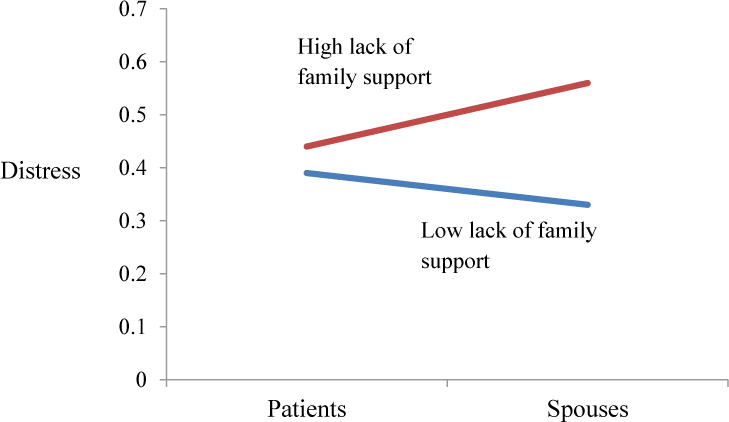
A multilevel model analysis reveals an interaction (p=0.10) depicting 6-month follow-up distress as a function of baseline lack of family support and social role. Scores are plotted at the mean ±1 standard deviation. Higher scores indicate greater distress.
There was no evidence that the prospective associations involving caregiving-related health problems or caregiving esteem were moderated by social role.
DISCUSSION
The results of this prospective dyadic study suggest that caregiving burden is significantly related to both spouse and patient psychological adjustment and some dimensions may differentially affect patients and spouses over an approximately 6 month period after treatment initiation for lung cancer. Spouses’ burden (except for financial strain) did not decrease but rather remained stable (i.e., schedule disruption) or increased (i.e., health problems and lack of family support) over the 6-month assessment period. Regarding psychological adjustment, similarly to previous reports [26, 40], distress levels remained fairly consisted across time for patients yet spouses seemed to improve. Overall, our findings support as well as extend the caregiving literature [5, 14, 15, 17, 18, 41, 42] in several important ways.
Primary findings
First, we identified that both spouses and patients’ psychological adjustment suffers as a result of caregiving strain. Even though distress levels decreased for spouses perhaps indicating their adjustment over time to their loved one’s diagnosis, the cross-sectional associations between caregiver burden and spousal distress became increasingly stronger as time progressed. This finding may demonstrate that caregiver burden may become an increasing source of their distress following the initial adjustment to the stressors associated with the patient’s diagnosis. In contrast, caregiver burden was associated with patient distress at baseline and 3-month follow-up but not at the 6-month assessment. Perhaps, at this point in the illness trajectory, where there may be increased symptom burden, patients’ level of distress may be primarily a function of their illness experience (e.g., prognosis, physical functioning) as others have demonstrated [43, 44]. Nevertheless, spousal baseline reports of their caregiving-related health problems predicted both patients and spouses’ distress scores at 3-month as well as 6-month follow-up. Two items of this 4-item subscale specifically assess fatigue, a common problem among family caregivers [41, 42, 45, 46]. Spouses’ exhaustion may predict patient distress because spouses may be too tired to provide for patients’ physical and emotional needs. Additionally, patients may be distressed due to witnessing the toll their illness takes on their spouses’ wellbeing.
Exploratory findings
Second, we revealed that patients and spouses may be adversely affected by different types of caregiving burden at different time points. We found that schedule disruptions were associated with patients but not spouses’ prospective distress. It is possible that spousal reports on schedule disruptions are more distressing to patients than spouses because disruptions are visible to patients and may trigger feelings of guilt and worthlessness. Yet, at 6-month follow-up, schedule disruption no longer significantly explained the variance of patient distress above the strong predictive effects of baseline distress. For spouses, interestingly, the opposite pattern was observed. Except for health problems, caregiving burden (i.e., lack of family support, financial strain) predicted 6-month but not 3-month distress. Possibly, when controlling for the initial link between caregiving burden and distress, the emotional toll associated with caregiving (e.g., feeling financially overwhelmed and scared as well as socially isolated and abandoned) may become more prominent as time goes on predicting distress above the baseline association at 6-month but not yet at 3-month follow-up. Yet, future research is needed to pinpoint the exact underlying mechanisms of these associations.
Despite cross-sectional beneficial associations between caregiving esteem and spousal distress, caregiving esteem did not provide a buffering effect for subsequent distress. Further, the finding that caregiving esteem is only weakly inversely correlated with spousal distress and not at all with patient distress seems to support a seminal review in the marriage and health literature [47] suggesting that negative dimensions (e.g., behaviors and cognitions) tend to have more direct and reliable health and wellbeing implications compared to positive dimensions. Furthermore, caregiving burden may be distressing for patients because spouses’ problems with finances, scheduling, health and family are external and noticeable whereas caregiving esteem is an internal process of which patients may not be aware.
In the context of patient care, caregiver burden is rarely if ever addressed. Because caregiving burden predicts increased distress in both patients and spouses, this research underscores the need for managing caregiver burden, particularly health problems, in spouses of lung cancer patients. Research revealed that spouses with high caregiving responsibilities, as it is typical among spouses of lung cancer patients, are prone to poor health behaviors such as lack of exercise, inadequate rest in general and when sick, and poor adherence to their own medications [48]. Consequently, supportive care programs that highlight the importance of spouses practicing self-care particularly health behaviors (e.g., exercise, routine physicals, rest, and healthy diet) to manage their fatigue and maintain physical health may be particularly fruitful. Based on our findings, programs that teach practical behavioral skills such as time management and scheduling, balancing work with caregiving activities, coping with financial challenges and accessing support from one’s social network and family members may also be effective in reducing distress. Further, because of the dyadic nature of the stressor, a couple-oriented approach for psychosocial supportive care in lung cancer may be prudent.
This study has a few limitations. First, as with all self-report assessments, responses on the caregiving measure may have been vulnerable to social desirability, which may potentially, explain the ceiling effect of caregiver esteem. Yet, even though the distribution of caregiving esteem scores was negatively skewed, current mean scores were comparable to those of previous reports [14, 18]. Nevertheless, this restricted range may explain the lack of significant prospective findings for caregiving esteem. Also, the prospective finding regarding lack of family support only approached statistical significance. As such, this trend should be interpreted with caution; however, the obtained effect size is comparable to our other study findings that did reach statistical significance highlighting the need for further exploration in future research. Finally, as with all survey data, no causal inferences can be made. Based on prospective analyses, we can be fairly confident regarding the direction of the caregiving burden and distress association; however, a bidirectional association is certainly possible.
In summary, caregiving burden may undermine the long-term psychological adjustment of spouses and to some extent patients coping with lung cancer. The risk of elevated and enduring distress is particularly high for couples in which spouses report caregiving-related health problems. Other negative domains such as schedule disruption and lack of family support may increase distress in patients, and spouses, respectively. This study contributes to caregiving literature because it highlights the dyadic nature of the cancer coping process. The procedure we employed for data analysis enabled us to examine couple-level data within the same model and test for differential associations for patients and their spouses. The study’s prospective design allowed us to confirm the direction of the caregiver burden and distress association over a 6-month period. Future intervention research is encouraged to examine practical behavioral and self-care skills as targets of couple-focused interventions to facilitate patients and spouses’ successful coping with lung cancer.
Footnotes
Conflict of Interest Statement: The authors have no conflict of interest to disclose.
References
- 1.Kim Y, Given BA. Quality of life of family caregivers of cancer survivors: across the trajectory of the illness. Cancer. 2008;112(11 Suppl):2556–68. doi: 10.1002/cncr.23449. [DOI] [PubMed] [Google Scholar]
- 2.Coyne JC, Fiske V. Couples coping with chronic and catastrophic illness. In: Akamatsu TJ, et al., editors. Family Health Psychology. Hemisphere; Washington, DC: 1992. pp. 129–149. [Google Scholar]
- 3.Neuling SJ, Winefield HR. Social support and recovery after surgery for breast cancer: frequency and correlates of supportive behaviours by family, friends and surgeon. Soc Sci Med. 1988;27(4):385–92. doi: 10.1016/0277-9536(88)90273-0. [DOI] [PubMed] [Google Scholar]
- 4.Carmack Taylor CL, et al. Lung cancer patients and their spouses: psychological and relationship functioning within 1 month of treatment initiation. Ann Behav Med. 2008;36(2):129–40. doi: 10.1007/s12160-008-9062-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Braun M, et al. Hidden morbidity in cancer: spouse caregivers. J Clin Oncol. 2007;25(30):4829–34. doi: 10.1200/JCO.2006.10.0909. [DOI] [PubMed] [Google Scholar]
- 6.Kim Y, et al. Levels of depressive symptoms in spouses of people with lung cancer: effects of personality, social support, and caregiving burden. Psychosomatics. 2005;46(2):123–30. doi: 10.1176/appi.psy.46.2.123. [DOI] [PubMed] [Google Scholar]
- 7.Ji J, et al. Increased Risks of Coronary Heart Disease and Stroke Among Spousal Caregivers of Cancer Patients. Circulation. 2012 doi: 10.1161/CIRCULATIONAHA.111.057018. [DOI] [PubMed] [Google Scholar]
- 8.Swore Fletcher BA, et al. Symptom experience of family caregivers of patients with cancer. Oncol Nurs Forum. 2008;35(2):E23–44. doi: 10.1188/08.ONF.E23-E44. [DOI] [PubMed] [Google Scholar]
- 9.Acitelli L, Badr H. My illness or our illness? Attending to the relationship when one partner is ill. In: K K, Revenson TA, Bodenmann G, editors. Couples coping with stress: Emerging perspectives on dyadic coping. American Psychological Association; Washington, DC: 2005. pp. 121–136. [Google Scholar]
- 10.Kim Y, et al. Individual and dyadic relations between spiritual well-being and quality of life among cancer survivors and their spousal caregivers. Psychooncology. 2011;20(7):762–70. doi: 10.1002/pon.1778. [DOI] [PubMed] [Google Scholar]
- 11.Kim Y, et al. Quality of life of couples dealing with cancer: dyadic and individual adjustment among breast and prostate cancer survivors and their spousal caregivers. Ann Behav Med. 2008;35(2):230–8. doi: 10.1007/s12160-008-9026-y. [DOI] [PubMed] [Google Scholar]
- 12.Badr H, Carmack Taylor CL. Effects of relationship maintenance on psychological distress and dyadic adjustment among couples coping with lung cancer. Health Psychol. 2008;27(5):616–27. doi: 10.1037/0278-6133.27.5.616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Milbury K, Badr H, Carmack CL. The role of blame in the psychosocial adjustment of couples coping with lung cancer. Annals of Behavioral Medicine. 2012;44(3):331–40. doi: 10.1007/s12160-012-9402-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nijboer C, et al. Determinants of caregiving experiences and mental health of partners of cancer patients. Cancer. 1999;86(4):577–88. doi: 10.1002/(sici)1097-0142(19990815)86:4<577::aid-cncr6>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 15.Nijboer C, et al. The role of social and psychologic resources in caregiving of cancer patients. Cancer. 2001;91(5):1029–39. [PubMed] [Google Scholar]
- 16.Given CW, et al. The caregiver reaction assessment (CRA) for caregivers to persons with chronic physical and mental impairments. Res Nurs Health. 1992;15(4):271–83. doi: 10.1002/nur.4770150406. [DOI] [PubMed] [Google Scholar]
- 17.Poulin MJ, et al. Does a helping hand mean a heavy heart? Helping behavior and well-being among spouse caregivers. Psychology and Aging. 2010;25(1):108–17. doi: 10.1037/a0018064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nijboer C, et al. Measuring both negative and positive reactions to giving care to cancer patients: psychometric qualities of the Caregiver Reaction Assessment (CRA) Soc Sci Med. 1999;48(9):1259–69. doi: 10.1016/s0277-9536(98)00426-2. [DOI] [PubMed] [Google Scholar]
- 19.Pusa S, Persson C, Sundin K. Significant others’ lived experiences following a lung cancer trajectory: from diagnosis through and after the death of a family member. Eur J Oncol Nurs. 2012;16(1):34–41. doi: 10.1016/j.ejon.2011.02.004. [DOI] [PubMed] [Google Scholar]
- 20.Zabora J, et al. The prevalence of psychological distress by cancer site. Psychooncology. 2001;10(1):19–28. doi: 10.1002/1099-1611(200101/02)10:1<19::aid-pon501>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 21.Degner LF, Sloan JA. Symptom distress in newly diagnosed ambulatory cancer patients and as a predictor of survival in lung cancer. J Pain Symptom Manage. 1995;10(6):423–31. doi: 10.1016/0885-3924(95)00056-5. [DOI] [PubMed] [Google Scholar]
- 22.Ellis J. The impact of lung cancer on patients and carers. Chron Respir Dis. 2012;9(1):39–47. doi: 10.1177/1479972311433577. [DOI] [PubMed] [Google Scholar]
- 23.Stone AM, et al. Caring for a parent with lung cancer: caregivers’ perspectives on the role of communication. Qual Health Res. 2012;22(7):957–70. doi: 10.1177/1049732312443428. [DOI] [PubMed] [Google Scholar]
- 24.Mosher CE, et al. Distressed family caregivers of lung cancer patients: an examination of psychosocial and practical challenges. Support Care Cancer. 2012 doi: 10.1007/s00520-012-1532-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lambert SD, et al. Walking a mile in their shoes: anxiety and depression among partners and caregivers of cancer survivors at 6 and 12 months post-diagnosis. Support Care Cancer. 2012 doi: 10.1007/s00520-012-1495-7. [DOI] [PubMed] [Google Scholar]
- 26.Stommel M, et al. A longitudinal analysis of the course of depressive symptomatology in geriatric patients with cancer of the breast, colon, lung, or prostate. Health Psychol. 2004;23(6):564–73. doi: 10.1037/0278-6133.23.6.564. [DOI] [PubMed] [Google Scholar]
- 27.Choi CW, et al. Group-based trajectory modeling of caregiver psychological distress over time. Ann Behav Med. 2012;44(1):73–84. doi: 10.1007/s12160-012-9371-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Oken MM, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5(6):649–55. [PubMed] [Google Scholar]
- 29.Derogatis LR. Brief Symptom Inventory: Administration, Scoring, and Procedures Manual. 3. Minneapolis, MN: National Computer Systems; 1993. [Google Scholar]
- 30.Given CW, et al. The Caregiver Reaction Assessment (CRA) for caregivers to persons with chronic physical and mental impairments. Research in Nursing and Health. 1992;15:271–283. doi: 10.1002/nur.4770150406. [DOI] [PubMed] [Google Scholar]
- 31.Spanier GB. Measuring Dyadic Adjustment – New Scales for Assessing Quality of Marriage and Similar Dyads. Journal of Marriage and the Family. 1976;38(1):15–28. [Google Scholar]
- 32.Badr H, Acitelli LK, Taylor CL. Does talking about their relationship affect couples’ marital and psychological adjustment to lung cancer? J Cancer Surviv. 2008;2(1):53–64. doi: 10.1007/s11764-008-0044-3. [DOI] [PubMed] [Google Scholar]
- 33.Kenny DA, Kashy DA, Cook WL. Dyadic data analysis. New York: Guilford Press; 2006. [Google Scholar]
- 34.Campbell L, Kashy DA. Estimating Actor, Partner, and Interaction Effects for Dyadic Data Using PROC MIXED and HLM: A User–Friendly Guide. Personal Relationships. 2002;9(3):327–342. [Google Scholar]
- 35.Wolfer R, Sang C. Proceedings of the Twentieth Annual SAS Users Group Conference, Cary, NC. Gary, NC: SAS Institute Inc; 1995. Comparing the SAS GLM and MIXED Procedures for Repeated Measures. [Google Scholar]
- 36.Snijders T, Bosker R. Multilevel analysis. Thousand Oaks, CA: Oaks; 1999. [Google Scholar]
- 37.Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Lawrence Earlbaum Associates; 1988. [Google Scholar]
- 38.Cohen J. A power primer. Psychol Bull. 1992;112(1):155–9. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- 39.Preacher KJ, Curran PJ, Bauer DJ. Computational tools for probing interaction effects in multiple linear regression, multilevel modeling, and latent curve analysis. Journal of Educational and Behavioral Statistics. 2006;31(4):437–448. [Google Scholar]
- 40.Brant JM, et al. Symptom trajectories in posttreatment cancer survivors. Cancer Nurs. 2011;34(1):67–77. doi: 10.1097/NCC.0b013e3181f04ae9. [DOI] [PubMed] [Google Scholar]
- 41.Roca RM, et al. Impact of caregiving on the health of family caregivers. Aten Primaria. 2000;26(4):217–23. doi: 10.1016/S0212-6567(00)78650-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gaston-Johansson F, et al. Psychological distress, fatigue, burden of care, and quality of life in primary caregivers of patients with breast cancer undergoing autologous bone marrow transplantation. Oncol Nurs Forum. 2004;31(6):1161–9. doi: 10.1188/04.ONF.1161-1169. [DOI] [PubMed] [Google Scholar]
- 43.Hopwood P, Stephens RJ. Depression in patients with lung cancer: prevalence and risk factors derived from quality-of-life data. J Clin Oncol. 2000;18(4):893–903. doi: 10.1200/JCO.2000.18.4.893. [DOI] [PubMed] [Google Scholar]
- 44.Graves KD, et al. Distress screening in a multidisciplinary lung cancer clinic: prevalence and predictors of clinically significant distress. Lung Cancer. 2007;55(2):215–24. doi: 10.1016/j.lungcan.2006.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jensen S, Given B. Fatigue affecting family caregivers of cancer patients. Support Care Cancer. 1993;1(6):321–5. doi: 10.1007/BF00364970. [DOI] [PubMed] [Google Scholar]
- 46.Fletcher BA, et al. Trajectories of fatigue in family caregivers of patients undergoing radiation therapy for prostate cancer. Res Nurs Health. 2009;32(2):125–39. doi: 10.1002/nur.20312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kiecolt-Glaser JK, Newton TL. Marriage and health: his and hers. Psychol Bull. 2001;127(4):472–503. doi: 10.1037/0033-2909.127.4.472. [DOI] [PubMed] [Google Scholar]
- 48.Burton LC, et al. Preventive health behaviors among spousal caregivers. Prev Med. 1997;26(2):162–9. doi: 10.1006/pmed.1996.0129. [DOI] [PubMed] [Google Scholar]


