Abstract
There is an inherited susceptibility to polycystic ovary syndrome (PCOS). Some investigators have suggested that premature male-pattern balding is a male phenotype in PCOS families, but this remains controversial. We recently reported evidence for an autosomal monogenic abnormality in ovarian and adrenal steroidogenesis in the sisters of women with PCOS. We performed this study to determine whether we could identify a clinical or biochemical phenotype in the brothers of women with PCOS. One hundred nineteen brothers of 87 unrelated women with PCOS and 68 weight- and ethnicity-comparable unrelated control men were examined and had fasting blood samples obtained. The odds of balding (Hamilton score ≥ V) did not differ in the brothers of PCOS women compared with control men. Brothers of women with PCOS had significantly elevated dehydroepiandrosterone sulfate (DHEAS) levels [brothers 3035 ± 1132 ng/ml (mean ± SD) vs. control men 2494 ± 1172 ng/ml; P < 0.05]. There was a significant positive linear relationship between DHEAS levels in PCOS probands and their brothers (r = 0.35; P = 0.001). There was no significant bimodal distribution in DHEAS levels, and there were no significant differences in other parameters in brothers of PCOS women with high DHEAS levels compared with those with low DHEAS levels. There is familial clustering of elevated DHEAS levels in the brothers of women with PCOS, suggesting that this is a genetic trait. This might reflect the same underlying defect in steroidogenesis that we found in the sisters of women with PCOS. Balding was not increased in the brothers of women with PCOS. We conclude that there is a biochemical reproductive endocrine phenotype in men in PCOS families.
Polycystic Ovary Syndrome (PCOS) is among the most common endocrinopathies of premenopausal women, affecting 5–10% of this population (1, 2). The syndrome is characterized by hyperandrogenism and chronic anovulation in the absence of specific disorders of the pituitary, ovaries, or adrenal glands (3). Familial aggregation of PCOS consistent with a genetic etiology has been well documented (4, 5). The male reproductive phenotypes that have been proposed in PCOS families include abnormalities in hair distribution, such as increased hair growth (6), and more commonly balding (7–10). This latter phenotype has been further refined to premature male balding defined as balding onset with an age of less than 30 yr (9, 10). Others have noted abnormalities in LH levels in male members of PCOS kindreds (11).
We recently reported elevated T and dehydroepiandrosterone levels in the sisters of women with PCOS (12). There was a bimodal distribution of biologically available T levels in these sisters consistent with a monogenic trait controlled by alleles of a gene at an autosomal locus (12). If there was variation in such a gene regulating steroidogenesis, it was our hypothesis that this should result in a reproductive phenotype in males in PCOS families. Previous studies have not systematically examined male relatives compared with a concurrently studied control group. We performed this study to determine whether we could identify a reproductive phenotype in the brothers of women with PCOS.
Subjects and Methods
Subjects
The brothers of 87 unrelated non-Hispanic white women with PCOS were studied. The diagnosis of PCOS was made in the proband by an elevation of circulating T and/or free and weakly bound T (uT) levels associated with chronic oligomenorrhea (no more than six menses per year) or amenorrhea (12). Women with nonclassical 21-hydroxylase deficiency, hyperprolactinemia, and androgen-secreting tumors were excluded by appropriate tests (12). The clinical features and reproductive hormone levels of the PCOS probands are summarized in Table 1 and have been reported previously in 18 of these women (12).
TABLE 1.
Clinical features and reproductive hormone levels in PCOS sisters
| Variable | Mean ± SD (n) |
|---|---|
| Age (yr) | 29 ± 6 (87) |
| BMI (kg/m2) | 35.6 ± 9.0 (87) |
| T (ng/dl) | 79 ± 38 (87) |
| SHBG (nmol/liter) | 61 ± 42 (78) |
| uT (ng/dl) | 30 ± 24 (87) |
| DHEAS (ng/ml) | 2369 ± 1328 (87) |
| LH (mlU/ml) | 18 ± 22 (84) |
| FSH (mlU/ml) | 11 ± 9 (84) |
To convert T and uT to nanomoles per liter, multiply by 0.03467; to convert DHEAS to micromoles per liter, multiply by 0.002714. n, No. of family units.
There were 156 brothers of the 87 women with PCOS, and 130 brothers were studied. Of the 26 brothers not willing to be studied, one family had four brothers, three families had two brothers, and 16 families had one brother. We limited the age range of brothers studied to 18–55 yr to control for age-related changes in reproductive hormone levels (13, 14). Eleven brothers were excluded because they were younger than 18 yr (n = 9) or older than 55 yr (n = 2). Accordingly, 119 brothers were included in the analysis. Of these 119 brothers, two families had four brothers, five had three brothers, 16 had two brothers, and 64 had a single brother.
Age-, weight-, and ethnicity-comparable unrelated control men (n = 68) without a history of hypertension or diabetes mellitus (either personally or in their first-degree relatives) were studied. Control men were in good health and, for at least 1 month before each study, were not taking any medication known to affect sex hormone metabolism. Control men were recruited concurrently with brothers of PCOS women, and we sought to match primarily on the basis of body mass index (BMI) and secondarily age. The Institutional Review Boards of the Hershey Medical Center and the Brigham and Women’s Hospital approved this study, and all subjects gave written informed consent.
Height, weight, and blood pressure (a single seated determination after a 5-min rest period) were obtained, and BMI (kilograms per square meter) was determined in subjects examined by the investigators. Due to their distance from our study sites, 65 brothers had blood drawn at an outside site. An investigator did not examine these men, and their height and weight were self-reported. They did not have blood pressure determinations. Balding was assessed by the Hamilton scale (15), and waist and hip circumferences were measured in those subjects examined at the Hershey site. A single fasting blood sample was obtained in the morning from each subject. In brothers studied off-site, blood was obtained at a clinical laboratory and immediately separated and aliquoted; the plasma and serum were shipped on ice packs by overnight delivery. All assays were performed in a single central laboratory. We performed validation studies to document that there were minimal differences in self-reported compared with on-site determinations of height and weight. We also documented that there was no significant impact of shipping serum and plasma at 4 C on hormone levels.
Assays
Assays for T, uT, dehydroepiandrosterone sulfate (DHEAS), LH, and FSH were performed as previously reported, and the interassay coefficients of variation were less than 10% for these assays (12). SHBG was determined using Diagnostics Systems Laboratories, Inc. (Webster, TX) reagents. The interassay coefficient of variation was 8% at 24 nmol/liter.
Data analysis
For all analyses, the family unit was the case; in families with multiple brothers, the brothers’ data were averaged to yield one mean value per family. Analysis of covariance models were fit, adjusting for the effect of age, to all continuous clinical features and reproductive hormones to compare brothers of PCOS women to control men. Logarithmic transformations were made, where necessary, to meet modeling assumptions. The ratio of brothers of PCOS women to control men and associated 95% confidence intervals are reported because back-transforming the logarithmic difference between groups to the original units is a ratio. For a binary outcome, a logistic regression model was fit. The logistic regression model also adjusted for the age of the subjects in testing whether the odds of a binary outcome differed significantly between brothers of PCOS women and control men.
Linear associations between PCOS women and their brothers for reproductive hormones were assessed using either the Pearson correlation coefficient or the Spearman correlation coefficient. For these correlations, the brothers’ values were averaged, resulting in one mean value per family, and then paired with their corresponding PCOS sisters. Analyses were performed using SAS statistical software (SAS Institute, Inc., Cary, NC). Descriptive data are reported as the unadjusted mean ± sd.
Results
Clinical features (Tables 1 and 2)
TABLE 2.
Clinical features of PCOS brothers and control men
| Variable | Brothersa | Male controlsa | P |
|---|---|---|---|
| Age (yr) | 30 ± 8 (87) | 33 ± 9 (68) | 0.050 |
| BMI (kg/m2) | 28.6 ± 5.9 (87) | 28.5 ± 5.1 (68) | 0.69 |
| Waist (cm) | 96 ± 18 (49) | 98 ± 18 (48) | 0.88 |
| Waist/hip ratio | 0.91 ± 0.07 (49) | 0.91 ± 0.08 (48) | 0.50 |
| Systolic blood pressure (mmHg) | 124 ± 12 (55) | 122 ± 12 (68) | 0.32 |
| Diastolic blood pressure (mmHg) | 75 ± 10 (55) | 75 ± 9 (68) | 0.97 |
Mean ± SD; numbers in parentheses represent family units. Multiple brothers for a single family are averaged to yield one mean value per family.
The PCOS probands had elevated T, uT, and LH levels consistent with the biochemical profile of the disorder (2) (Table 1). PCOS probands were more obese (35.6 ± 9.0 kg/m2) than their brothers (29.2 ± 6.4 kg/m2). By design, brothers of PCOS women and control men were comparable in terms of BMI (Table 2). The brothers of PCOS women tended to be younger than the control men (P = 0.050). Accordingly, all analyses were adjusted for age to control for its potential confounding effect on outcome variables. There were no significant differences in waist to hip ratio or waist circumference in brothers of PCOS women compared with control men. There was no significant difference in blood pressure in brothers of PCOS women compared with control men. However, the odds of hypertension by Joint National Committee VI guidelines (16) (systolic blood pressure >140 mmHg or diastolic blood pressure >90 mmHg) tended to be higher in PCOS brothers compared with control men, but this did not achieve statistical significance (adjusted odds ratio, 3.2; 95% confidence interval, 0.9, 10.7; P = 0.06). Balding (Hamilton score ≥ V) did not differ significantly in the brothers of PCOS women (5.5%) compared with control men (19%) (14, 15).
Biochemical features (Tables 3 and 4)
Table 3.
Reproductive hormone levels in PCOS brothers and control men
| Variable | Brothers | Male controls | P |
|---|---|---|---|
| T (ng/dl) | 520 ± 216 (86) | 519 ± 183 (68) | 0.67 |
| uT (ng/dl) | 256 ± 156 (86) | 238 ± 106 (67) | 0.85 |
| SHBG (nmol/liter) | 52 ± 27 (77) | 51 ± 31 (67) | 0.23 |
| DHEAS (ng/ml) | 3035 ± 1132 (85) | 2494 ± 1172 (68) | 0.016 |
| LH (mlU/ml) | 4 ± 2 (86) | 5 ± 5 (67) | 0.39 |
| FSH (mIU/ml) | 7 ± 3 (86) | 8 ± 5 (68) | 0.50 |
To convert T and uT to nanomoles per liter, multiply by 0.03467; to convert DHEAS to micromoles per liter, multiply by 0.002714. Data are mean ± SD; numbers in parentheses represent family units. Multiple brothers for a single family are averaged to yield one mean value per family.
TABLE 4.
Linear correlation between PCOS brothers and their PCOS sisters
| PCOS brother | PCOS proband | Pearson correlation coefficient [P value] (n) |
|---|---|---|
| DHEAS | DHEAS | 0.35 [0.001] (85) |
| T | T | −0.005 [0.96] (86) |
| uT | uT | −0.05 [0.67] (86) |
| LH | LH | 0.06 [0.62] (83) |
| FSH | FSH | −0.02 [0.83] (83) |
| SHBG | SHBG | 0.18 [0.13] (70) |
Spearman correlation coefficient. n, No. of family units.
Circulating DHEAS levels were significantly higher in brothers of PCOS women than in control men (P = 0.02) (Fig. 1). Otherwise, there were no significant differences in circulating T, uT, SHBG, LH, or FSH levels in brothers of PCOS women compared with control men. In PCOS probands and their brothers, the correlation between DHEAS levels was significant (r = 0.35; P ≤ 0.001) (Table 4). There were no other statistically significant correlations between the PCOS probands and their brothers. There was no significant bimodal distribution of DHEAS or other hormone levels in the brothers or in control men (Table 4). To further investigate whether we could use DHEAS levels to identify different subgroups of brothers, we compared brothers with DHEAS levels more than 1 sd below the mean to those with DHEAS levels more than 1 SD above the mean (i.e. mean − SD = 1322 ng/ml, and mean + SD = 3666 ng/ml). There were no significant differences in other outcome variables in these groups of brothers.
FIG. 1.
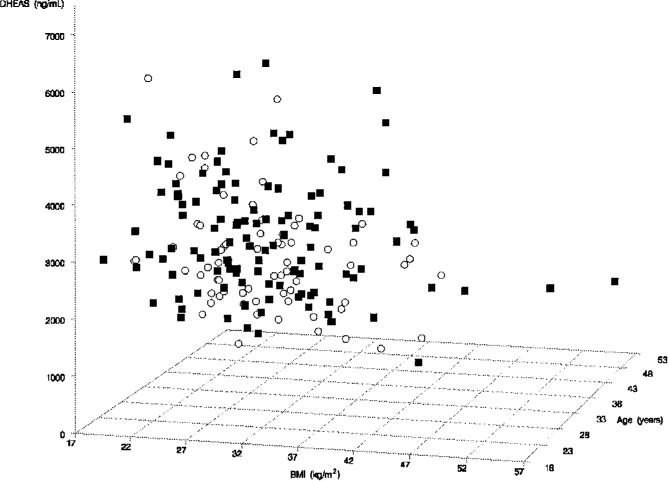
DHEAS levels in the brothers (■) were significantly increased compared with control (○) men after adjusting for age (P = 0.016).
Discussion
Our results suggest that there is a male biochemical reproductive phenotype in PCOS families. Circulating levels of the adrenal androgen DHEAS were significantly increased in brothers of PCOS women compared with control men. Furthermore, DHEAS levels in the brothers were significantly correlated with DHEAS levels in the PCOS probands, consistent with a heritable trait. There were no other significant changes in reproductive hormone levels in the brothers of women with PCOS compared with control men. There was no increase in the prevalence of balding in the brothers of PCOS women. Recently, we reported that hyperandrogenemia with or without menstrual irregularity appeared to be a genetic trait in the reproductive-age sisters of PCOS women (12). Another group has confirmed the high prevalence of hyperandrogenemia in PCOS female first-degree relatives (17).
The increased circulating T and DHEAS levels in affected sisters suggested a defect in a common factor regulating ovarian and adrenal androgen biosynthesis (12). Furthermore, we have found an association of this phenotype with candidate genes for PCOS in an affected sib pair analysis supporting our hypothesis that it had a genetic basis (18, 19). Elevated DHEAS levels in the brothers of PCOS women may reflect this steroidogenic defect (12). We did not find elevated T levels in brothers of PCOS women. This might be because T feeds back on the hypothalamic-pituitary axis to modulate its own secretion in men or because the substantially greater male T production rates made it difficult to discern subtle changes in circulating levels (20, 21). Alternatively, the varying ontogeny of the ovary and testes in PCOS families may obviate the potential abnormality in the testes and preserve it in the adrenal gland, which originates from a common anlage in both males and females.
A study of men with severe acne found significantly increased DHEAS levels (22). This supports the utility of this adrenal androgen as a marker for male hyperandrogenism. We did not assess the presence of acne in this study. DHEAS is a good marker of abnormal steroidogenesis because of its lack of pulsatility and its long half life (23). DHEAS levels within an individual remain stable over time (24). There is a decline in circulating DHEAS levels with age (13, 14, 25), but this phenomenon was controlled for statistically in our analysis. Previous studies have suggested that there is a significant heritable component to circulating DHEAS levels in normal individuals (26–28). The heritability for DHEAS, however, has been found to be much less for men than for women (27), and heritability has also been noted to be stronger for T levels (26, 27, 29).
Premature male balding has been suggested to be a male phenotype in previous studies in PCOS families that ascertained the PCOS index case on the basis of ovarian morphology determined by ultrasonography rather than by endocrine criteria (6–10). No endocrinological marker of male affected status was noted. However, in one study, PCOS male relatives with premature balding had significantly higher total T levels than unaffected male relatives (10). There was no significant increase in DHEAS levels in those male relatives. Our sample size of PCOS brothers with balding was too small to test this hypothesis, but abnormalities in circulating T levels in male-pattern baldness are an infrequent finding (30, 31). Furthermore, control men tended to have more balding than the brothers of PCOS women. A survey of the U.S. male population age 18–49 yr reported high rates of significant male-pattern hair loss (32). The proportion of men with moderate to extensive hair loss increased with increasing age, ranging from 16% for men 18–29 yr of age to 53% of men 40–49 yr of age (32). We conclude that balding is extremely common in the U.S. male population and its prevalence is not increased in the brothers of PCOS women. Recent reports from investigators in the United Kingdom have also suggested that balding is not as reliable a male phenotype in PCOS families as they had originally reported (4).
In the sisters of women with PCOS, approximately 50% appear to have increased ovarian and adrenal steroidogenesis. If this is a monogenic trait, a similar number of brothers should be affected, although there might be sex-specific differences in penetrance (33, 34). However, there was no bimodal distribution of DHEAS levels in the brothers to suggest a monogenic trait (35) as we have found for T levels in the sisters of women with PCOS (12). This suggests a more complex pattern of inheritance for this phenotypic marker in familial PCOS. Individual DHEAS values in the brothers overlapped substantially with those in control men. Furthermore, there were no significant differences in other hormonal parameters in those brothers of PCOS women with high (>mean + 1 SD) DHEAS levels compared with those with low (<1 SD + mean) DHEAS levels. Accordingly, it was not possible to assign affected status on the basis of a DHEAS value in a brother of a PCOS woman.
In summary, we have identified a male reproductive phenotype in the brothers of women with PCOS. This consists of elevations in circulating DHEAS levels. There was no increase in the prevalence of balding in this U.S. population of male first-degree relatives. DHEAS levels were highly correlated between brothers and their proband sisters, consistent with a heritable trait (26–28, 36). The same putative defect in steroidogenesis that we reported in the sisters of women with PCOS (12) could account for the observed DHEAS elevations in the brothers of PCOS probands.
Acknowledgments
We thank the nurses of the Pennsylvania State University College of Medicine and the Brigham and Women’s Hospital General Clinical Research Centers for their excellent care of the study participants; Ms. Sharon Ward for her superb coordination of the study; Drs. J.F. Strauss, R.S. Spielman, and M. Urbanek for critical review of the manuscript; and Ms. Ruth Capella for her skillful preparation of the manuscript.
This work was supported by NIH Grant R01 DK 40605 (to A.D.), Grant K08 HD 0118 (to R.S.L.), The National Center for Infertility Research at University of Pennsylvania-Brigham and Women’s Hospital-University of California at San Francisco-Pennsylvania State University U54 HD 34449 (Project 1 to A.D.), M01 RR 10732 (to Pennsylvania State University College of Medicine General Clinical Research Center), and M01 RR 02635 (to the Brigham and Women’s Hospital General Clinical Research Center).
Abbreviations
- BMI
Body mass index
- DHEAS
dehydroepiandrosterone sulfate
- PCOS
polycystic ovary syndrome
- uT
free and weakly bound T
References
- 1.Knochenhauer ES, Key TJ, Kahsar-Miller M, Waggoner W, Boots LR, Azziz R. Prevalence of the polycystic ovary syndrome in unselected black and white women of the southeastern United States: a prospective study. J Clin Endocrinol Metab. 1998;83:3078–3082. doi: 10.1210/jcem.83.9.5090. [DOI] [PubMed] [Google Scholar]
- 2.Diamanti-Kandarakis E, Kouli CR, Bergiele AT, Filandra FA, Tsianateli TC, Spina GG, Zapanti ED, Bartzis MI. A survey of the polycystic ovary syndrome in the Greek island of Lesbos: hormonal and metabolic profile. J Clin Endocrinol Metab. 1999;84:4006–4011. doi: 10.1210/jcem.84.11.6148. [DOI] [PubMed] [Google Scholar]
- 3.Dunaif A. Insulin resistance and the polycystic ovary syndrome: mechanism and implications for pathogenesis. Endocr Rev. 1997;18:774–800. doi: 10.1210/edrv.18.6.0318. [DOI] [PubMed] [Google Scholar]
- 4.Franks S, Gharani N, Waterworth D, Batty S, White D, Williamson R, McCarthy M. Genetics of polycystic ovary syndrome. Mol Cell Endocrinol. 1998;145:123–128. doi: 10.1016/s0303-7207(98)00178-6. [DOI] [PubMed] [Google Scholar]
- 5.Legro RS. Polycystic ovary syndrome. Phenotype to genotype. Endocrinol Metab Clin North Am. 1999;28:379–96. doi: 10.1016/s0889-8529(05)70075-x. [DOI] [PubMed] [Google Scholar]
- 6.Cooper HE, Spellacy WN, Prem KA, Cohen WD. Hereditary factors in the Stein-Leventhal syndrome. Am J Obstet Gynecol. 1968;100:371–387. doi: 10.1016/s0002-9378(15)33704-2. [DOI] [PubMed] [Google Scholar]
- 7.Ferriman D, Purdie AW. The inheritance of polycystic ovarian disease and a possible relationship to premature balding. Clin Endocrinol (Oxf) 1979;11:291–300. doi: 10.1111/j.1365-2265.1979.tb03077.x. [DOI] [PubMed] [Google Scholar]
- 8.Lunde O, Magnus P, Sandvik L, Hoglo S. Familial clustering in the polycystic ovarian syndrome. Gynecol Obstet Invest. 1989;28:23–30. doi: 10.1159/000293493. [DOI] [PubMed] [Google Scholar]
- 9.Carey AH, Chan KL, Short F, White D, Williamson R, Franks S. Evidence for a single gene effect causing polycystic ovaries and male pattern baldness. Clin Endocrinol (Oxf) 1993;38:653–658. doi: 10.1111/j.1365-2265.1993.tb02150.x. [DOI] [PubMed] [Google Scholar]
- 10.Govind A, Obhrai MS, Clayton RN. Polycystic ovaries are inherited as an autosomal dominant trait: analysis of 29 polycystic ovary syndrome and 10 control families. J Clin Endocrinol Metab. 1999;84:38–43. doi: 10.1210/jcem.84.1.5382. [DOI] [PubMed] [Google Scholar]
- 11.Cohen PN, Givens JR, Wiser WL, Wilroy RS, Summitt RL, Coleman SA. Polycystic ovarian disease, maturation arrest of spermiogenesis, and Klinefelter’s syndrome in siblings of a family with familial hirsutism. Fertil Steril. 1975;26:1228–1238. [PubMed] [Google Scholar]
- 12.Legro RS, Driscoll D, Strauss JF, 3rd, Fox J, Dunaif A. Evidence for a genetic basis for hyperandrogenemia in polycystic ovary syndrome. Proc Natl Acad Sci USA. 1998;95:14956–14960. doi: 10.1073/pnas.95.25.14956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Perry HM, 3rd, Flood JF, Jensen J, Silver AJ, Roberts E. Potentially predictive and manipulable blood serum correlates of aging in the healthy human male: progressive decreases in bioavailable testosterone, dehydroepiandrosterone sulfate, and the ratio of insulin-like growth factor 1 to growth hormone. Proc Natl Acad Sci USA. 1997;94:7537–7542. doi: 10.1073/pnas.94.14.7537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Labrie F, Belanger A, Cusan L, Gomez JL, Candas B. Marked decline in serum concentrations of adrenal C19 sex steroid precursors and conjugated androgen metabolites during aging. J Clin Endocrinol Metab. 1997;82:2396–2402. doi: 10.1210/jcem.82.8.4160. [DOI] [PubMed] [Google Scholar]
- 15.Hamilton JB. Patterned loss of hair in man: types and incidence. Ann N Y Acad Sci. 1951;53:708–728. doi: 10.1111/j.1749-6632.1951.tb31971.x. [DOI] [PubMed] [Google Scholar]
- 16.Anonymous. The sixth report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Arch Intern Med. 1997;157:2413–2446. doi: 10.1001/archinte.157.21.2413. [DOI] [PubMed] [Google Scholar]
- 17.Kahsar-Miller MD, Nixon C, Boots LR, Go RC, Azziz R. Prevalence of polycystic ovary syndrome (PCOS) in first-degree relatives of patients with PCOS. Fertil Steril. 2001;75:53–58. doi: 10.1016/s0015-0282(00)01662-9. [DOI] [PubMed] [Google Scholar]
- 18.Urbanek M, Legro RS, Driscoll DA, Azziz R, Ehrmann DA, Norman RJ, Strauss JF, 3rd, Spielman RS, Dunaif A. Thirty-seven candidate genes for polycystic ovary syndrome: strongest evidence for linkage is with follistatin. Proc Natl Acad Sci USA. 1999;96:8573–8578. doi: 10.1073/pnas.96.15.8573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Urbanek M, Wu XQ, Vickery KR, Kao LC, Christenson LK, Schneyer A, Legro RS, Driscoll DA, Strauss JF, 3rd, Dunaif A, Spielman RS. Allelic variants of the follistatin gene in polycystic ovary syndrome. J Clin Endocrinol Metab. 2000;85:4455–4461. doi: 10.1210/jcem.85.12.7026. [DOI] [PubMed] [Google Scholar]
- 20.Santen RJ. Feedback control of luteinizing hormone and follicle-stimulating hormone secretion by testosterone and estradiol in men: physiological and clinical implications. Clin Biochem. 1981;14:243–251. doi: 10.1016/s0009-9120(81)90964-4. [DOI] [PubMed] [Google Scholar]
- 21.Mooradian AD, Morley JE, Korenman SG. Biological actions of androgens. Endocr Rev. 1987;8:1–28. doi: 10.1210/edrv-8-1-1. [DOI] [PubMed] [Google Scholar]
- 22.Marynick SP, Chakmakjian ZH, McCaffree DL, Herndon JH., Jr Androgen excess in cystic acne. N Engl J Med. 1983;308:981–986. doi: 10.1056/NEJM198304283081701. [DOI] [PubMed] [Google Scholar]
- 23.Baulieu EE, Corpechot C, Dray F. An adrenal secreted androgen: dehydroisoandrosterone sulfate. Its metabolism and a tentative generalization on the metabolism of other steroid conjugates in man. Recent Prog Horm Res. 1965;21:411–500. [PubMed] [Google Scholar]
- 24.Thomas G, Frenoy N, Legrain S, Sebag-Lanoe R, Baulieu EE, Debuire B. Serum dehydroepiandrosterone sulfate levels as an individual marker. J Clin Endocrinol Metab. 1994;79:1273–1276. doi: 10.1210/jcem.79.5.7962319. [DOI] [PubMed] [Google Scholar]
- 25.Orentreich N, Brind JL, Vogelman JH, Andres R, Baldwin H. Long-term longitudinal measurements of plasma dehydroepiandrosterone sulfate in normal men. J Clin Endocrinol Metab. 1992;75:1002–1004. doi: 10.1210/jcem.75.4.1400863. [DOI] [PubMed] [Google Scholar]
- 26.Rotter JI, Wong FL, Lifrak ET, Parker LN. A genetic component to the variation of dehydroepiandrosterone sulfate. Metabolism. 1985;34:731–736. doi: 10.1016/0026-0495(85)90023-x. [DOI] [PubMed] [Google Scholar]
- 27.Rice T, Sprecher DL, Borecki IB, Mitchell LE, Laskarzewski PM, Rao DC. The Cincinnati Myocardial Infarction and Hormone Family Study: family resemblance for dehydroepiandrosterone sulfate in control and myocardial infarction families. Metabolism. 1993;42:1284–1290. doi: 10.1016/0026-0495(93)90126-9. [DOI] [PubMed] [Google Scholar]
- 28.Akamine Y, Kato K, Ibayashi H. Studies on changes in the concentration of serum adrenal androgens in pubertal twins. Acta Endocrinol (Copenh) 1980;93:356–364. doi: 10.1530/acta.0.0930356. [DOI] [PubMed] [Google Scholar]
- 29.Harris JA, Vernon PA, Boomsma DI. The heritability of testosterone: a study of Dutch adolescent twins and their parents. Behav Genet. 1998;28:165–171. doi: 10.1023/a:1021466929053. [DOI] [PubMed] [Google Scholar]
- 30.Legro RS, Carmina E, Stanczyk FZ, Gentzschein E, Lobo RA. Alterations in androgen conjugate levels in women and men with alopecia. Fertil Steril. 1994;62:744–750. doi: 10.1016/s0015-0282(16)56999-4. [DOI] [PubMed] [Google Scholar]
- 31.Demark-Wahnefried W, Lesko SM, Conaway MR, Robertson CN, Clark RV, Lobaugh B, Mathias BJ, Strigo TS, Paulson DF. Serum androgens: associations with prostate cancer risk and hair patterning. J Androl. 1997;18:495–500. [PubMed] [Google Scholar]
- 32.Rhodes T, Girman CJ, Savin RC, Kaufman KD, Guo S, Lilly FR, Siervogel RM, Chumlea WC. Prevalence of male pattern hair loss in 18–49 year old men. Dermatol Surg. 1998;24:1330–1332. doi: 10.1111/j.1524-4725.1998.tb00009.x. [DOI] [PubMed] [Google Scholar]
- 33.Healey CS, Dunning AM, Teare MD, Chase D, Parker L, Burn J, Chang-Claude J, Mannermaa A, Kataja V, Huntsman DG, Pharoah PD, Luben RN, Easton DF, Ponder BA. A common variant in brca2 is associated with both breast cancer risk and prenatal viability. Nat Genet. 2000;26:362–364. doi: 10.1038/81691. [DOI] [PubMed] [Google Scholar]
- 34.de Graaf J, Swinkels DW, de Haan AF, Demacker PN, Stalenhoef AF. Both inherited susceptibility and environmental exposure determine the low-density lipoprotein-subfraction pattern distribution in healthy Dutch families. Am J Hum Genet. 1992;51:1295–1310. [PMC free article] [PubMed] [Google Scholar]
- 35.Weinshilboum RM, Raymond FA. Inheritance of low erythrocyte cate-chol-o-methyltransferase activity in man. Am J Hum Genet. 1977;29:125–135. [PMC free article] [PubMed] [Google Scholar]
- 36.Bull SB, Darlington GA, Greenwood CM, Shin J. Design considerations for association studies of candidate genes in families. Genet Epidemiol. 2001;20:149–174. doi: 10.1002/1098-2272(200102)20:2<149::AID-GEPI1>3.0.CO;2-A. [DOI] [PubMed] [Google Scholar]


